Abstract
A 60-year-old male presented with complaints of dyspnea, intermittent fever, and 40 pounds of weight loss over the previous 9 months and was admitted for acute hypoxemic respiratory failure. Labs demonstrated elevated inflammatory markers, mild anemia, and thrombocytopenia. Fluorodeoxyglucose-positron emission tomography scan demonstrated diffusely increased pulmonary fluorodeoxyglucose uptake without corresponding abnormality on CT images. Excisional lung biopsy demonstrated intravascular large B-cell lymphoma (IV-LBCL). Presentation, imaging findings, and diagnosis of IV-LBCL will be discussed, as well as differential considerations for pulmonary involvement by IV-LBCL.
Keywords: Lymphoma, Intravascular large B-cell lymphoma, FDG-PET, CT, Pulmonary uptake
Abbreviations: IV-LBCL, intravascular large B-cell lymphoma; FDG, fluorodeoxyglucose; PET, positron emission tomography; CT, computed tomography; CTA, computed tomography angiogram; MIP, maximum intensity projection; ARDS, acute respiratory distress syndrome; H&E, hematoxylin-eosin
Case report
A 60-year-old male presented to the emergency department with chief complaint of dyspnea and was admitted for acute hypoxemic respiratory failure. The patient reported intermittent, recurrent fever up to 102 °F and 40 pounds of weight loss over the previous 9 months.
Medical history was significant for recent admission to an outside hospital, 1 month prior to this admission, for pancytopenia and splenomegaly. Splenic biopsy demonstrated marginal zone lymphoma and splenectomy was performed. Bone marrow biopsy performed at that time was negative. Family history revealed similar presentation years earlier by the patient's mother of unknown etiology, despite extensive medical workup in the months prior to her death.
Labs on admission demonstrated mild anemia and thrombocytopenia. Lactate dehydrogenase and inflammatory markers, including C-reactive protein and erythrocyte sedimentation rate, were significantly elevated. White blood cell count and differential were normal and infectious workup was negative. Liver transaminases were mildly elevated. Initial imaging evaluation in the emergency department (ED) included computed tomography (CT) angiogram of the chest, which was negative for pulmonary embolism and demonstrated no significant abnormalities (Fig. 1). Further extensive imaging workup was obtained following admission which included echocardiogram, CT abdomen and pelvis with contrast, and CT maxillofacial. No significant abnormalities were identified.
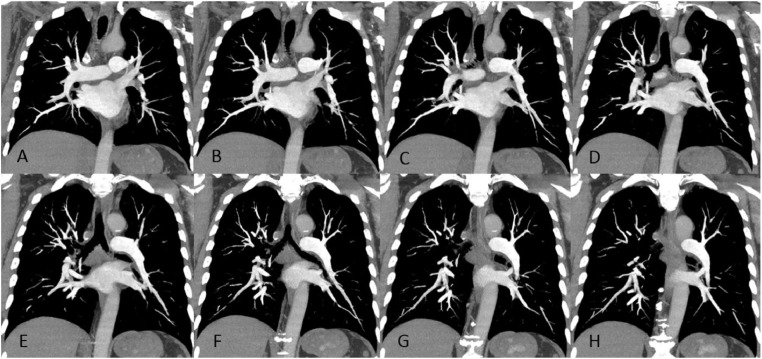
Fig. 1.
Sixty-year-old male with dyspnea and hypoxemia, diagnosed 4 days later with pulmonary involvement by intravascular large B-cell lymphoma. Coronal 10 mm maximum intensity projection computed tomography angiogram images from anterior to posterior (A-H) demonstrate normal caliber pulmonary arteries without evidence of intraluminal filling defect.
Given the history of splenic marginal zone lymphoma, PET-CT was ordered to evaluate for recurrence. PET-CT was obtained on day 4 of admission and demonstrated changes of prior splenectomy without hypermetabolic lymphadenopathy. There was, however, the unusual finding of diffusely increased fluorodeoxyglucose (FDG) uptake throughout both lungs, greater than background hepatic uptake, without corresponding abnormality on CT images (Fig. 2 and Fig. 3). Pneumonitis was considered although there were no pulmonary opacities on CT to support this diagnosis. This prompted a literature search to explain the findings.
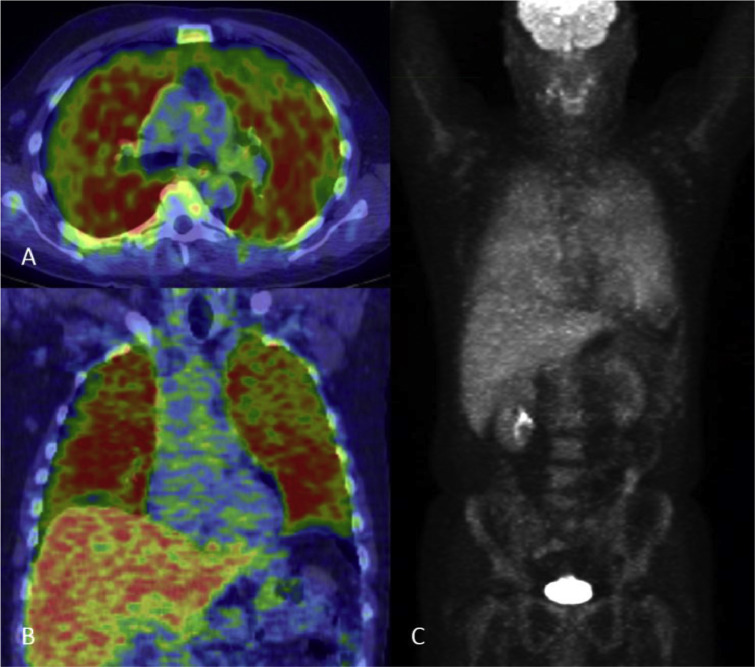
Fig. 2.
Sixty-year-old male with intravascular diffuse large B-cell lymphoma. Axial (A) and coronal (B) fused PET-CT images and 3D attenuation corrected maximum intensity projection (C) obtained 60 minutes after IV administration of 17.7 mCi F-18 FDG demonstrate diffuse hypermetabolic bilateral pulmonary FDG uptake, greater than physiologic hepatic uptake.
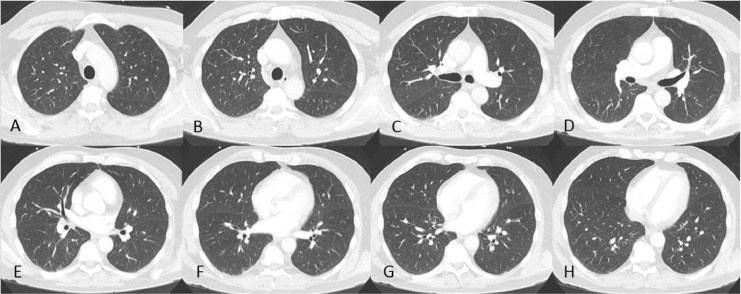
Fig. 3.
Sixty-year-old male with intravascular diffuse large B-cell lymphoma. Axial lung window CT images reconstructed with high spatial frequency algorithm, 1.25 mm slice thickness at 2 cm intervals from superior to inferior (A-H) demonstrate normal lung parenchyma without airspace or interstitial opacities corresponding to hypermetabolic uptake on PET images.
A case report of diffuse pulmonary uptake on FDG-positron emission tomography (PET) with normal CT diagnosed as biopsy-proven intravascular lymphoma was found upon literature review. This study was referenced and differential diagnoses of intravascular lymphoma versus pneumonitis were included in the PET-CT report. Bronchoalveolar lavage was performed and flow cytometry was negative. Due to high clinical suspicion for lymphoma, excisional lung biopsy was performed. Biopsy was interpreted as intravascular large B-cell lymphoma (IV-LBCL) with cell markers positive for CD5, CD20, and CD79a, and negative for CD3 and Pan-CK, supporting this diagnosis (Fig. 4).
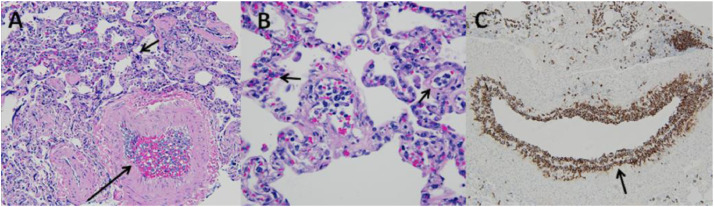
Fig. 4.
Sixty-year-old male with intravascular large B-cell lymphoma. Hematoxylin-eosin (H&E) stain of right middle lobe excisional lung biopsy at 20× magnification (A) and 40× magnification (B) demonstrate atypical lymphocytes within the lumen of a pulmonary artery (long arrow) and within surrounding capillary beds (short arrows). CD-20 immunohistochemical stain (C) demonstrates that the atypical lymphocytes stain positive for CD-20 (arrow).
Discussion
Etiology and demographics
IV-LBCL is a rare type of non-Hodgkin lymphoma, usually B-cell immunophenotype, characterized by preferential growth of malignant lymphocytes within the lumina of small vessels, aggressive behavior, and often fatal course [1]. IV-LBCL usually affects elderly patients with median age at diagnosis in the sixth-seventh decades.
Clinical and imaging findings
Patients with IV-LBCL may present with poor performance status, elevated lactic dehydrogenase serum levels, anemia, and B symptoms (Table 1) [1], [2]. In contrast to other types of lymphoma, the bone marrow, lymph nodes, peripheral blood, and cerebrospinal fluid are often uninvolved in IV-LBCL. Clinical presentation is highly variable with the most pronounced differences related to the geographical origin of the patient, although it often includes organ dysfunction related to obstruction of blood vessels. Fever, skin lesions, and rapidly progressive neurologic symptoms are more common in Western countries, while bone marrow, spleen, and liver involvement are more common in Asia [1], [3], [4]. central nervous system (CNS) involvement may present similar to an ischemic stroke. Pulmonary artery involvement results in dyspnea and hypoxemia, presenting similar to a pulmonary embolism or pulmonary hypertension [5], [6], [7]. Filling defects are usually not identified on computed tomography angiogram [5], [8], [9]. This is presumably due to lymphomatous cells being primarily located in small peripheral pulmonary arteries and capillary beds. Five case reports of isolated pulmonary artery involvement presenting with diffuse or regional increased pulmonary FDG uptake and normal appearance on CT have been published [10], [11], [12], [13], [14]. In 1 study, gallium scintigraphy demonstrated similar increased pulmonary uptake although was less pronounced than FDG uptake [14].
Table 1.
Summary.
| Epidemiology | • Median age at diagnosis is in the sixth to seventh decades, no sex predilection. |
| • True incidence unknown, until recently it was usually only recognized at autopsy. | |
| Clinical presentation | • Western countries: fever, skin lesions, and prominent, rapidly progressive neurologic signs (eg, dementia, progressive cerebral vascular accident, peripheral neuropathy). |
| • Asia: bone marrow, spleen, and liver involvement more common. May present with hemophagocytic syndrome. | |
| Labs | • Elevated lactate dehydrogenase and beta 2 microglobulin (80-90%), anaemia (65%), elevated sediment rate (43%), altered hepatic, renal, or thyroid function, serum monoclonal protein (14%). |
| • Thrombocytopenia and hypoalbuminemia more common in Asia (76% and 84%) than Western countries (29% and 18%). | |
| Treatment | • Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) more effective than CHOP alone. |
| Prognosis (R-CHOP) | • Complete response (82%), 2-year overall survival (66%), 2-year progression free survival (56%). |
Diagnosis
Biopsy is generally required to make the diagnosis since the malignant cells are located within the lumina of small vessels, with percutaneous, transbronchial, and excisional lung biopsies reported in confirmed cases. Multiple cases have reported, successfully confirming the diagnosis by random skin or subcutaneous biopsy, demonstrating proliferating lymphoma cells within the lumina of vessels [11], [15], [16]. B-cell origin is the most common immunophenotype. Immunohistochemistry in almost all cases of IV-LBCL stains positive for surface antigen CD-20, with CD-5 and CD-10 being the next most common [17]. CD-29 and CD-54, surface antigens involved in transvascular migration into organs or lymph nodes, are consistently absent in IV-LBCL, which explains the preferential intravascular growth [18].
Differential diagnosis
Diffusely increased pulmonary FDG uptake has also been reported in cases of inflammatory and infectious pneumonitis, pulmonary contusion, and acute respiratory distress syndrome in which CT findings were initially absent or disproportionately less than FDG-PET findings. In each of these cases, CT findings progressed over 3-5 days with development of ground glass opacities or consolidation corresponding to the areas of increased uptake (Table 2) [19], [20], [21].
Table 2.
Differential diagnosis.
| Differential diagnosis | CT chest/X-ray findings | PET findings |
|---|---|---|
| Intravascular large B-cell lymphoma | X-ray, CT, and CTA normal | Diffuse hypermetabolic FDG uptake |
| Inflammatory or infectious pneumonitis | Ground glass opacity/ consolidation (within 3-5 d) | Focal or diffuse hypermetabolic FDG uptake |
| Pulmonary contusion | Ground glass opacity/ consolidation (within 3-5 d) | Focal or diffuse hypermetabolic FDG uptake |
| Acute respiratory distress syndrome (ARDS) | Ground glass opacity/ consolidation (within 3-5 d) | Diffuse hypermetabolic FDG uptake |
Treatment and prognosis
Nonspecific, variable clinical presentation, and occult radiologic features, including absence of significant lymphadenopathy often results in diagnostic delay, which in combination with its aggressive behavior, result poor prognosis for IV-LBCL [22]. In fact, diagnosis at autopsy is not uncommon [23], [24]. Prognosis was extremely poor prior to the advent of rituximab [25], although, it is now considered that detection and treatment at an early stage can improve survival [25], [26]. In 1 case report of isolated pulmonary involvement by IV-LBCL, diagnosed by PET-CT, complete remission was achieved for over 24 months, supporting the role of PET-CT in early diagnosis [14]. Current standard of treatment is rituximab plus anthracycline-based chemotherapy, which has been shown to be superior to chemotherapy alone. The largest retrospective study demonstrated complete response in 82%, 2-year overall survival in 66%, and 2-year progression-free survival in 56% of patients treated with anthracycline-based chemotherapy plus rituximab [25].
Conclusion
In high-risk patients with suggestive clinical presentation, IV-LBCL should be considered for the finding of diffusely increased pulmonary FDG uptake when there is no corresponding abnormality on CT. The diagnosis requires high degree of suspicion, as scintigraphy may be the only clue to the diagnosis of this aggressive disease, which may otherwise be clinically and radiologically undetectable in its early stages. There are a few differential considerations for the PET-CT findings, although, CT is less likely to remain normal for more than 3-5 days in these conditions. Without alternative explanation, biopsy should be considered and, based on promising results from prior studies, initial attempt at diagnosis via random skin or subcutaneous biopsy may be considered prior to lung biopsy.
Author contributions
Jayden Spencer, MD as primary author.
Reginald Dusing, MD as faculty mentor.
Wendell Yap, MD as faculty mentor.
Jacquelline Hill, MPH as radiology department research director.
Carissa Walter, MPH as radiology department research coordinator.
Footnotes
Acknowledgments: The authors would like to thank Da Zhang, MD of Kansas University Hospital, Department of Pathology–Pathology images.
Competing Interests: The authors have declared that no competing interests exist.
Contributor Information
Jayden Spencer, Email: jspencer2@kumc.edu.
Reginald Dusing, Email: rdusing@kumc.edu.
Wendell Yap, Email: wyap@kumc.edu.
Jacqueline Hill, Email: jhill@kumc.edu.
Carissa Walter, Email: cwalter2@kumc.edu.
References
- 1.Ponzoni M., Ferreri A., Campo E., Facchetti F., Mazzucchelli L., Yoshino T. Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J Clin Oncol. 2007;25(21):3168–3173. doi: 10.1200/JCO.2006.08.2313. PMID 17577023. [DOI] [PubMed] [Google Scholar]
- 2.Ferreri A., Campo E., Seymour J., Willemze R., Ilariucci F., Ambrosetti A. Intravascular lymphoma: clinical presentation, natural history, management and prognostic factors in a series of 38 cases, with special emphasis on the ‘cutaneous variant’. Br J Haematol. 2004;127(2):173–183. doi: 10.1111/j.1365-2141.2004.05177.x. PMID 15461623. [DOI] [PubMed] [Google Scholar]
- 3.Shimada K., Kinoshita T., Naoe T., Nakamura S. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol. 2009;10(9):895–902. doi: 10.1016/S1470-2045(09)70140-8. PMID 19717091. [DOI] [PubMed] [Google Scholar]
- 4.Zuckerman D., Seliem R., Hochberg E. Intravascular lymphoma: the oncologist's “great imitator”. Oncologist. 2006;11(5):496–502. doi: 10.1634/theoncologist.11-5-496. PMID 16720850. [DOI] [PubMed] [Google Scholar]
- 5.Kotake T., Kosugi S., Takimoto T., Nakata S., Shiga J., Nagate Y. Intravascular large B-cell lymphoma presenting pulmonary arterial hypertension as an initial manifestation. Intern Med. 2010;49(1):51–54. doi: 10.2169/internalmedicine.49.2774. PMID 20046001. [DOI] [PubMed] [Google Scholar]
- 6.Aouba A., Diop S., Saadoun D., Trebbia G., Vilde F., Patri B. Severe pulmonary arterial hypertension as initial manifestation of intravascular lymphoma: case report. Am J Hematol. 2005;79(1):46–49. doi: 10.1002/ajh.20300. PMID 15849762. [DOI] [PubMed] [Google Scholar]
- 7.Souza C.A., Quan K., Seely J., Kravcik S., Burns B. Pulmonary intravascular lymphoma. J Thorac Imaging. 2009;24(3):231–233. doi: 10.1097/RTI.0b013e31819724d9. PMID 19704329. [DOI] [PubMed] [Google Scholar]
- 8.Martusewicz-Boros M., Wiatr E., Radzikowska E., Roszkowski-Sliz K., Langfort R. Pulmonary intravascular large B-cell lymphoma as a cause of severe hypoxemia. J Clin Oncol. 2007;25(15):2137–2139. doi: 10.1200/JCO.2007.10.7201. PMID 17513823. [DOI] [PubMed] [Google Scholar]
- 9.Yamashita H., Suzuki A., Takahashi Y., Kubota K., Kano T., Mimori A. Intravascular large B-cell lymphoma with diffuse FDG uptake in the lung by 18FDG-PET/CT without chest CT findings. Ann Nucl Med. 2012;26(6):515–521. doi: 10.1007/s12149-012-0600-9. PMID 22539250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner T., Brechemier D., Dugert E., Le Guellec S., Julian A., Hitzela A. Diffuse pulmonary uptake on FDG-PET with normal CT diagnosed as intravascular large B-cell lymphoma: a case report and a discussion of the causes of diffuse FDG uptake in the lungs. Cancer Imaging. 2012;12:7–12. doi: 10.1102/1470-7330.2012.0002. PMID 22275725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamashita H., Suzuki A., Takahashi Y., Kubota K., Kano T., Mimori A. Intravascular large B-cell lymphoma with diffuse FDG uptake in the lung by 18FDG-PET/CT without chest CT findings. Ann Nucl Med. 2012;26(6):515–521. doi: 10.1007/s12149-012-0600-9. PMID 22539250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitanaka A., Kubota Y., Imataki O., Ohnishi H., Fukumoto T., Kurokohchi K. Intravascular large B‐cell lymphoma with FDG accumulation in the lung lacking CT/67gallium scintigraphy abnormality. Hematol Oncol. 2009;27(1):46–49. doi: 10.1002/hon.876. PMID 18819161. [DOI] [PubMed] [Google Scholar]
- 13.Miura Y., Tsudo M. Fluorodeoxyglucose-PET/CT for diagnosis of intravascular large B-cell lymphoma. Mayo Clin Proc. 2010;85(8):e56–e57. doi: 10.4065/mcp.2009.0716. PMID 20675506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niida T., Isoda K., Miyazaki K., Kanoh S., Kobayashi H., Kobayashi A. Pulmonary intravascular lymphoma diagnosed by 18-fluorodeoxyglucose positron emission tomography-guided transbronchial lung biopsy in a man with long-term survival: a case report. J Med Case Rep. 2011;5(1):295. doi: 10.1186/1752-1947-5-295. PMID 21736708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miura Y., Tsudo M. Fluorodeoxyglucose-PET/CT for diagnosis of intravascular large B-cell lymphoma. Mayo Clin Proc. 2010;85(8):e56–e57. doi: 10.4065/mcp.2009.0716. PMID 20675506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asada N., Odawara J., Kimura S., Aoki T., Yamakura M., Takeuchi M. Use of random skin biopsy for diagnosis of intravascular large B-cell lymphoma. Mayo Clin Proc. 2007;82(12):1525–1527. doi: 10.1016/s0025-6196(11)61097-5. PMID 18053461. [DOI] [PubMed] [Google Scholar]
- 17.Kazuyuki S., Kinoshita T., Naoe T., Nakamura S. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol. 2009;10(9):895–902. doi: 10.1016/S1470-2045(09)70140-8. PMID 19717091. [DOI] [PubMed] [Google Scholar]
- 18.Ponzoni M., Arrigoni G., Gould V.E., Del Curto B., Maggioni M., Scapinello A. Lack of CD 29 (β1 integrin) and CD 54 (ICAM-1) adhesion molecules in intravascular lymphomatosis. Hum Pathol. 2000;31(2):220–226. doi: 10.1016/s0046-8177(00)80223-3. PMID 10685637. [DOI] [PubMed] [Google Scholar]
- 19.Yamane T., Daimaru O., Ito S., Nagata T., Yoshiya K., Fukaya N. Drug-induced pneumonitis detected earlier by 18 F-FDG-PET than by high-resolution CT: a case report with non-Hodgkin's lymphoma. Ann Nucl Med. 2008;22(8):719–722. doi: 10.1007/s12149-008-0183-7. PMID 18982476. [DOI] [PubMed] [Google Scholar]
- 20.Rodrigues R., Miller P., Bozza F., Marchiori E., Zimmerman G., Hoffman J. FDG-PET in patients at risk for acute respiratory distress syndrome: a preliminary report. Intensive Care Med. 2008;34(12):2273. doi: 10.1007/s00134-008-1220-7. PMID 18682917. [DOI] [PubMed] [Google Scholar]
- 21.Rohr L., Klaeser B., Joerger M., Kluckert T., Cerny T., Gillessen S. Increased pulmonary FDG uptake in bleomycin-associated pneumonitis. Oncol Res Treat. 2007;30(6):320–323. doi: 10.1159/000101517. PMID 17551256. [DOI] [PubMed] [Google Scholar]
- 22.Murase T., Yamaguchi M., Suzuki R., Okamoto M., Sato Y., Tamaru J.I. Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood. 2007;109(2):478–485. doi: 10.1182/blood-2006-01-021253. PMID 16985183. [DOI] [PubMed] [Google Scholar]
- 23.Domizio P., Hall P.A., Cotter F., Amiel S., Tucker J., Besser G.M. Angiotropic large cell lymphoma (ALCL): morphological, immunohistochemical and genotypic studies with analysis of previous reports. Hematol Oncol. 1989;7(3):195–206. doi: 10.1002/hon.2900070303. PMID 2651272. [DOI] [PubMed] [Google Scholar]
- 24.Demirer T., Dail D.H., Aboulafia D.M. Four varied cases of intravascular lymphomatosis and a literature review. Cancer. 1994;73(6):1738–1745. doi: 10.1002/1097-0142(19940315)73:6<1738::aid-cncr2820730631>3.0.co;2-u. PMID 8156502. [DOI] [PubMed] [Google Scholar]
- 25.Shimada K., Matsue K., Yamamoto K., Murase T., Ichikawa N., Okamoto M. Retrospective analysis of intravascular large B-cell lymphoma treated with rituximab-containing chemotherapy as reported by the IVL study group in Japan. J Clin Oncol. 2008;26(19):3189–3195. doi: 10.1200/JCO.2007.15.4278. PMID 18506023. [DOI] [PubMed] [Google Scholar]
- 26.Baumann T.P., Hurwitz N., Karamitopolou-Diamantis E., Probst A., Herrmann R., Steck A.J. Diagnosis and treatment of intravascular lymphomatosis. Arch Neurol. 2000;57:374–377. doi: 10.1001/archneur.57.3.374. PMID 10714664. [DOI] [PubMed] [Google Scholar]