Abstract
We report a case of patient who presented to the hospital due to shoulder pain and was later diagnosed with ruptured thymoma. Shortly after being admitted to the hospital for the work up patient developed respiratory distress and underwent emergent endotracheal intubation. CT scan of the chest showed anterior mediastinal mass with associated right sided hemothorax. He subsequently underwent medial sternotomy with resection of the mass which turned out to be thymoma.
1. Case
A 51-year-old male presented to the hospital due to right-sided shoulder pain. Patient reported that pain awakened him from sleep, was localized to the right shoulder, was sharp and was radiating down the arm. The pain was associated with vague tingling in the right arm. The pain seemed to be slightly worsened with shoulder movement. There was no associated nausea, palpitations, lightheadedness or dyspnea.
His pas medical history is significant for hypertension, hyperlipidemia and single episode of atrial fibrillation several years ago.
When the patient initially arrived at the hospital, his only physical exam abnormality was diaphoresis and “not looking well”. Due to the fact that the patient didn't appear well, he was admitted to the hospital for further work up.
Soon after arrival to the general medical floor, he started to complain of pleuritic chest pain and developed respiratory distress which required an emergent endotracheal intubation.
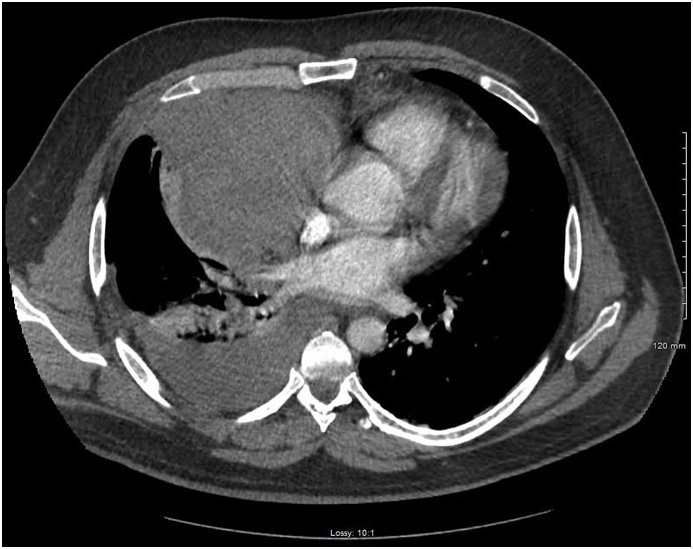
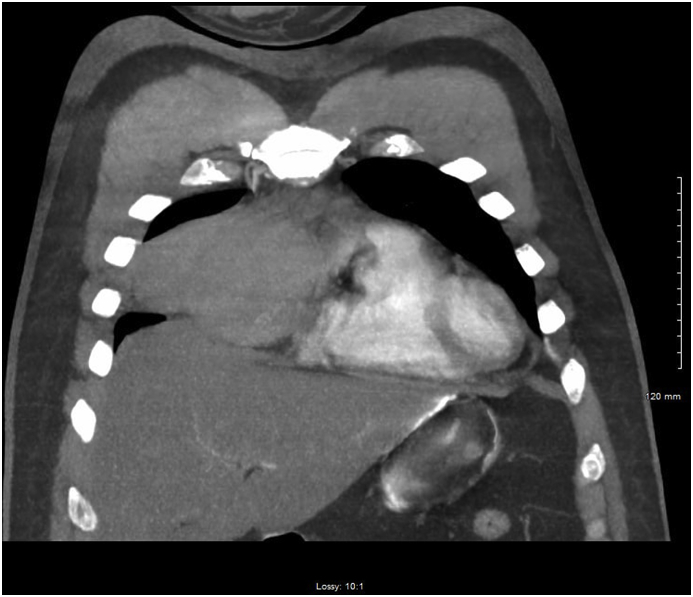
At the time of clinical deterioration vital signs were as following-temperature was 98.3 °F, HR 120 BPM, BP 154/93 mm Hg, respiratory rate 26 breaths per minute and SpO2 on 11 L per nasal cannula was 92%. At that time, he appeared to be in respiratory distress. There was no JVD. Chest examination revealed decreased breath sounds on the right; there was no crackles, rales or wheezing. He was tachycardic, and there was no murmurs, rubs or gallops. EKG showed new onset RBBB. There was a concern for pulmonary embolism and subsequently he underwent CT of the chest which showed a mass along the right anterior mediastinum, resulting in mass effect upon the distal right superior vena cava, and right atrium with associated right-sided hemothorax (Fig. 1, Fig. 2, Fig. 3, Fig. 4). CBC was significant for hemoglobin 13.5 g/dl. A right-sided chest tube was inserted which immediately drained one liter of blood. Over the next 24 hours, there was a minimal drainage through the chest tube. Patient subsequently had MRI of the chest which identified 8.8 cm low T1 and low T2 signal mass closely related to the right pericardium, containing multiple foci of cystic fluid without enhancement. AFP, B- HCG and TSH were within normal limits (see Fig. 5, Fig. 6, Fig. 7, Fig. 8).
Fig. 1.
Computerized tomography of the chest showing right anterior mediastinal mass.
Fig. 2.
Computerized tomography of the chest with lung window revealing associated right hemithorax.
Fig. 3.
Computerized tomography of the chest showing right hemithorax.
Fig. 4.
Computerized tomography of the chest demonstrating the tumor with mass effect on the superior vena cava and the right atrium.
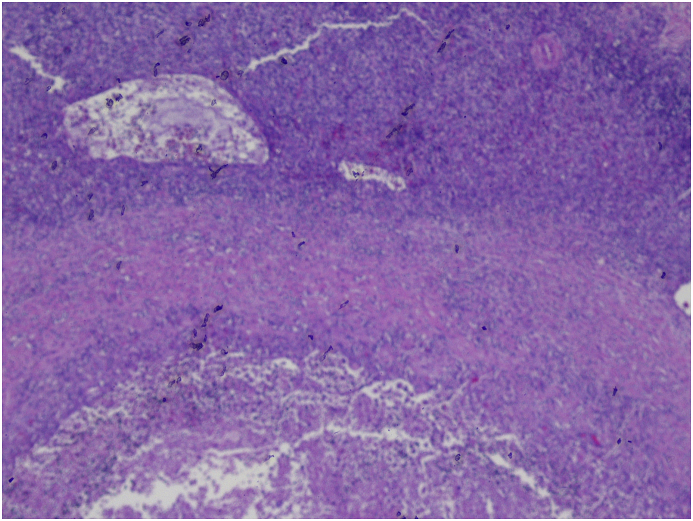
Fig. 5.
H&E stain demonstrating that most of the tumor was necorsed. In this low power image, the outer layer represent thymoma, middle layer shows fibrosis and eventually transitioning to necrosis in the inner most layer.
Fig. 6.
H&E stain, high power field; The large cells with lightly stained nuclei represent epithelial cells (tumor cells) which are interspersed with lymphocytes(cells with large and darkly stained nuclei).
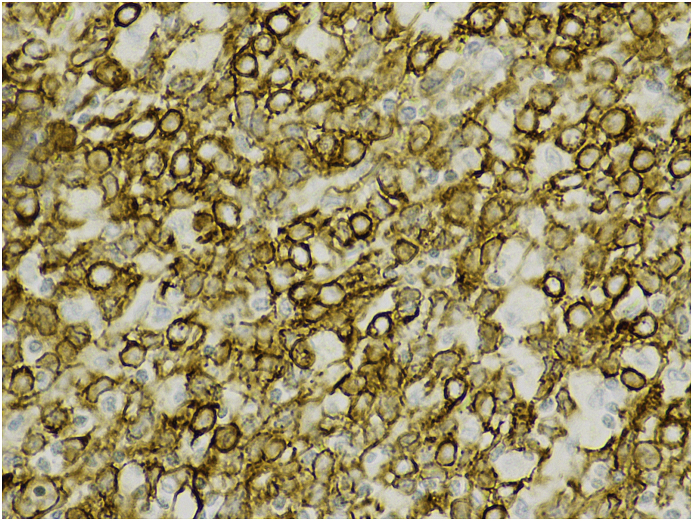
Fig. 7.
Cytokeratin stain; The epithelial cells (tumor cells) are stained with dark brown cell membranes. The admixed lymphocytes have not been stained and appear lighter in color.
Fig. 8.
H&E stain demonstrating thymoma type B2, necrotic tissue surrounded by rim of thymic epithelial cells and lymphocytes.
The patient underwent median sternotomy with exploration and complete resection of thymic mass. Pathology confirmed that the mass was truly representing thymoma type B2.
2. Discussion
Thymoma is a common primary neoplasm found in the anterior mediastinum with the estimated incidence of 0.13 per 100,000 person-year.
Thymoma has no gender preference; its peak incidence at ages 40 to 60 and its unlikely to be seen in children, young adults and elderly [1].
Thymomas are slowly growing tumors and commonly found accidentally on variety of imaging techniques [2]. There are multiple specific presentations of thymoma which can be divided into the two major subgroup.
The first group is related to the paraneoplastic syndromes. The most common paraneoplastic syndromes associated with thymoma include myasthenia gravis (MG), pure red cells aplasia, and hypogammaglobulinemia [3,4].
Myasthenia gravis is the most prevalent of them and occurs in about 30% of the patient with thymoma. About fifty percent of patients with thymoma present with MG, whereas 10–15% of patient with MG have thymoma [5]. It's generally recommended to evaluate all patients with thymoma for the presence of MG because of its association with higher preoperative mortality [6].
The second group consists of symptoms which are caused by growth of the tumor.
These include superior vena cava syndrome, chest pain or coughing and spontaneous rupture [7].
Rupture of thymoma is rare phenomenon, Case reports described shock and hemothorax as presenting features. Cases which were previously published in the literate did not demonstrate an impact on mortality [8,9,16,17].
Diagnostic approach to a patient with an anterior mediastinal mass consists of cross sectional imaging (MRI or CT) and laboratory studies.
CT of the chest is considered to be an imaging modality of choice. Usually, thymomas are located in the close proximity to the superior pericardium, however, they can still appear anywhere. The tumor is usually well defined, round, homogenous and enhances after contrast administration. Yet, in our patient tumor was heterogenous because of areas of hemorrhage and necrosis. One of the crucial thymoma characteristics on the CT is the invasiveness since it has been shown to strongly correlate with prognosis [10].
Another imaging modality is MRI. Thymoma has similar or higher signal intensity than muscle on T1 or T2 – weighted images. The main advantage of the MRI is when the patient is unable to undergo CT scan with contrast. In that situation, MRI can provide high resolution image and assess the local invasiveness [11].
Laboratory work up is mainly focused on the ruling out other pathology in the anterior mediastinum and excluding MG. As the result, it should include serum beta-HCG, alpha fetoprotein (AFP), complete blood count, thyroid stimulating hormone (TSH), triiodothyronine (T3) and thyroxine (T4) [12]. Beta-HCG and AFP levels can be used to rule out germ cell tumors, and TSH, T3, and T4 levels to rule out mediastinal goiter CT guided biopsy can sometimes a provide a diagnosis, however, in many cases aspirated sample is difficult to distinguish from other tumors and, as the result, reported sensitivity is around 60%. Biopsy must not violate pleural space because of the risk of dissemination of the tumor [13,14]. The cornerstone of the treatment of thymoma remains complete surgical resection [15].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2018.11.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Engels E.A. Epidemiology of thymoma and associated malignancies. J. Thorac. Oncol. 2010;5:S260–S265. doi: 10.1097/JTO.0b013e3181f1f62d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strollo D.C., Rosado de Christenson M.L., Jett J.R. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest. 1997;112:511–522. doi: 10.1378/chest.112.2.511. [DOI] [PubMed] [Google Scholar]
- 3.Venuta F., Rendina E.A., Longo F. Long-term outcome after multimodality treatment for stage III thymic tumors. Ann. Thorac. Surg. 2003;76:1866–1872. doi: 10.1016/s0003-4975(03)01020-8. [DOI] [PubMed] [Google Scholar]
- 4.Lewis J.E., Wick M.R., Scheithauer B.W. Thymoma. A clinicopathologic review. Cancer. 1987;60:2727–2743. doi: 10.1002/1097-0142(19871201)60:11<2727::aid-cncr2820601125>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 5.Detterbeck F.C., Parsons A.M. Management of stage I and II thymoma. Thorac. Surg. Clin. 2011;21:59–67. doi: 10.1016/j.thorsurg.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Shamji F., Pearson F.G., Todd T.R., Ginsberg R.J., Ilves R., Cooper J.D. Results of surgical treatment for thymoma. J. Thorac. Cardiovasc. Surg. 1984;87:43–47. [PubMed] [Google Scholar]
- 7.Regnard J.F., Magdeleinat P., Dromer C. Prognostic factors and long-term results after thymoma resection: a series of 307 patients. J. Thorac. Cardiovasc. Surg. 1996;112:376–384. doi: 10.1016/S0022-5223(96)70265-9. [DOI] [PubMed] [Google Scholar]
- 8.Shimokawa S., Watanabe S., Sakasegawa K., Tani A. Ruptured thymoma causing mediastinal hemorrhage resected via partial sternotomy. Ann. Thorac. Surg. 2001;71:370–372. doi: 10.1016/s0003-4975(00)02234-7. [DOI] [PubMed] [Google Scholar]
- 9.Fukuse T., Matsukura T., Nakamura A., Kosaka S., Tamada J. Mediastinal hematoma due to thymoma hemorrhage—a case report. Nippon Kyobu Geka Gakkai Zasshi. 1991;39:930–934. [PubMed] [Google Scholar]
- 10.Marom E.M. Imaging thymoma. J. Thorac. Oncol. 2010;5:S296–S303. doi: 10.1097/JTO.0b013e3181f209ca. [DOI] [PubMed] [Google Scholar]
- 11.Yanagawa M., Tomiyama N. Prediction of thymoma histology and stage by radiographic criteria. Thorac. Surg. Clin. 2011;21:1–12. doi: 10.1016/j.thorsurg.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Marchevsky A., Marx A., Strobel P. Policies and reporting guidelines for small biopsy specimens of mediastinal masses. J. Thorac. Oncol. 2011;6:S1724–S1729. doi: 10.1097/JTO.0b013e31821ea57c. [DOI] [PubMed] [Google Scholar]
- 13.Mehran R., Ghosh R., Maziak D. Surgical treatment of thymoma. Can. J. Surg. 2002;45:25–30. [PMC free article] [PubMed] [Google Scholar]
- 14.Murakawa T., Nakajima J., Kohno T. Results from surgical treatment for thymoma. 43 years of experience. Jpn. J. Thorac. Cardiovasc. Surg. 2000;48:89–95. doi: 10.1007/BF03218097. [DOI] [PubMed] [Google Scholar]
- 15.Pennathur A., Qureshi I., Schuchert M.J. Comparison of surgical techniques for early-stage thymoma: feasibility of minimally invasive thymectomy and comparison with open resection. J. Thorac. Cardiovasc. Surg. 2011;141:694–701. doi: 10.1016/j.jtcvs.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Templeton P.A., Vainright J.R., Rodriguez A., Diaconis J.N. Mediastinal tumors presenting as spontaneous hemothorax, simulating aortic dissection. Chest. 1988;93:828–830. doi: 10.1378/chest.93.4.828. [DOI] [PubMed] [Google Scholar]
- 17.Santoprete S., Ragusa M., Urbani M., Puma F. Shock induced by spontaneous rupture of a giant thymoma. Ann. Thorac. Surg. 2007 Apr;83(4):1526–1528. doi: 10.1016/j.athoracsur.2006.10.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.