Abstract
Objective
To assess patients’ weight management needs and experiences across multiple sites within the Learning Health System Network.
Patients and Methods
A total of 19,964 surveys were sent to patients identified with overweight or obesity through medical record query at 5 health care systems throughout 11 states. The survey collected patients’ experiences with and opinions about weight management in clinical care from October 27, 2017, through March 1, 2018.
Results
Among the 2380 responders, being younger, female, nonwhite, and single and having some college education or less were all significantly associated with higher body mass index (BMI). The most frequent weight loss barriers included food cravings (30.7%-49.9%) and having a medical condition limiting physical activity (17.7%-47.1%) (P<.001). Higher BMI was associated with a higher frequency of comorbidities and lower health status (P<.001). Higher BMI was also associated with a higher belief that primary care providers (PCPs) should be involved in weight loss management (P=.01) but lower belief that the PCP had the necessary skills and knowledge to help (P<.001). Responders with a higher BMI were more likely to feel judged (P<.001) and not always respected (P<.001) by their PCP. In addition, those with a higher BMI more frequently reported avoiding health care visits because of weight gain, not wanting to undress or be weighed, and not wanting to discuss their weight with their PCP (P<.001).
Conclusion
Physician involvement in weight management is important to patients whose needs and experiences differ by BMI. These data may inform clinical weight management efforts and create greater alignment with patient expectations.
Abbreviations and Acronyms: BMI, body mass index; CDM, common data model; IRB, institutional review board; LHSNet, Learning Health System Network; OR, odds ratio; PCP, primary care provider
Overweight and obesity result from energy imbalances caused by a combination of genetic, behavioral, and environmental factors.1, 2, 3, 4 In the United States, the prevalence of adults with obesity is approximately 45.4%, an increase of 10% since 2005 and 600% since the 1980s.5 Taking into consideration the economic burden of obesity on the individual and direct medical expenditures (up to $147 billion) and productivity loss (up to $6.38 billion) on society, obesity is a far-reaching public health crisis.6, 7
The US Preventive Services Task Force, the Centers for Medicare and Medicaid Services, and the Obesity Expert Panel have independently recommended and published guidelines for clinicians to screen for obesity, offer intensive counseling and behavioral interventions, and delineate requirements for behavioral therapy for obesity8 and address weight management.9 Despite the consistency of these guidelines and evidence that adhering to guidelines increases patient motivation for weight loss, these guidelines are not always followed by health care providers.10, 11, 12, 13 Furthermore, few studies have rigorously examined patients’ experiences with and expectations about weight management in primary care.14, 15, 16 One of the few studies that did so was a survey of patients previously conducted by our study team in a primary care setting.14 A conclusion from this previous study was that patients’ conversations with their primary care provider (PCP) concerning weight loss were less likely to motivate patients to lose weight.14 This study, however, did not address the tone and content of these interactions. Evidence suggests that PCPs spend less time building rapport and providing information to patients with obesity.17 Patients who feel judged by their PCP are less motivated to attempt to lose weight.18 A large body of evidence has shown that implicit and explicit biases negatively affect interpersonal behavior in ways that are detectable to patients.19, 20, 21, 22 Health care providers from all specialties, including primary care specialties, have been found to hold strong negative implicit and explicit attitudes and beliefs about their patients with obesity, which may influence their communication with patients with obesity.23, 24 In one study, PCPs were randomized to evaluate an otherwise identical patient with or without obesity. Those who evaluated the patient with obesity rated the patient as a greater waste of their time, as someone who would make them like their jobs less, and indicated that they would spend less time with them.25 Studies confirm that patients with overweight or obesity feel stigmatized and disrespected by PCPs, but less is known about patients’ preferences about and experiences with weight management in clinical settings and how these perceptions differ by BMI status.
To address these limitations and better understand patient needs, experiences, and expectations about weight management in primary care, our team conducted a survey of primary care patients within the Learning Health Systems Network (LHSNet) Clinical Data Research Network.14 The LHSNet is 1 of 13 Clinical Data Research Network partners with 20 patient-powered research networks to create the National Patient-Centered Clinical Research Network, funded by the Patient-Centered Outcomes Research Institute to support clinical trials and outcome research.26, 27, 28, 29
This survey aimed to identify barriers to successful weight loss and patients’ expectations regarding PCP assistance in weight management. Data obtained from this large sociodemographic sample of patients across diverse health systems provide unique and important knowledge to guide continued training and support for PCPs to initiate respectful and motivating conversations regarding obesity and obesity treatment with patients.
Patients and Methods
The LHSNet is composed of 9 sites and includes data on approximately 10 million patients. Details of the LHSNet structure and sites are found elsewhere.30, 31 The LHSNet sites each host a local common data model (CDM) and share common data elements across sites. The LHSNet CDM contains outcome data and consists of patient cohorts, one of which is the weight cohort. The building of the weight cohort centered on cohorts of children and adults across the LHSNet that were assembled and identified as overweight or obese on the basis of the PCORnet obesity algorithm, focusing on individuals with at least one other height and weight measurement in the previous 5 years. Weights of pregnant women were excluded from 6 months before to 3 months after the delivery date. The patients within this cohort served as the sampling population for the current study.
The Mayo Clinic Institutional Review Board (IRB) served as the IRB of record for the relying participating study sites: Mayo Clinic, Allina Health System, Essentia Health, Intermountain Health Care, University of Michigan, and Ohio State University. Upon review, the IRB, which had ethical oversight for this study, determined this study to be exempt under 45 CFR 46.101, item 2. In addition, the authors assert that all procedures contributing to this work comply with the ethical standards of the Mayo Clinic IRB guidelines on human experimentation in accordance with the Declaration of Helsinki of 1975, as revised in 2008. Protocol-approved passive consent was obtained from all study participants before study initiation. During the project, all changes to study design and procedures continued to be appropriately filed with the IRB.
Survey Development
A survey was developed by the LHSNet weight cohort work group,30 based on previously developed questions/scales of patient beliefs, behaviors, and experiences.18, 32, 33, 34, 35, 36, 37, 38, 39 The 5 overarching components of the survey were (1) patient’s health care experience18, 32, 33, 37; (2) Brief Stigmatizing Situation Inventory34; (3) patients’ health care experience; (4) self-esteem38; and (5) patient sociodemographic characteristics.35, 36, 39
The survey was purposefully developed to be brief and low-burden for participants to complete. It was anonymous (did not include patient identifiers), and all surveys were delivered and returned via US Postal Service. It was essential to design the survey in such a way that would maximize participation and trust from the first, and only, survey mailing.
Pilot Testing
The survey structure and process was tested by engaging 20 patients with body mass index (BMI; calculated as the weight in kilograms divided by the height in meters squared) of greater than or equal to 25 in cognitive testing. Of the 20 distributed survey packets, 55% were returned anonymously over a period of 10 weeks. The average time for completing the survey was about 11 minutes and 100% felt the length was “about right.” There were no consistent concerns/issues reported regarding the survey questions. This pilot test study was also deemed to be exempt by IRB under 45 CFR 46.101, item 2.
Data Collection and Response Rate
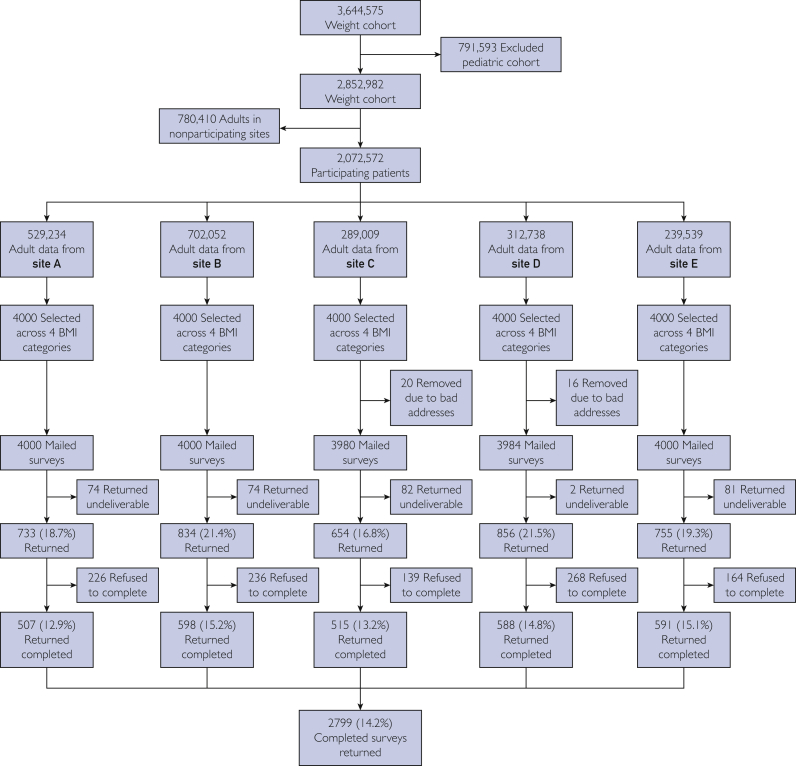
The LHSNet CDM consists of 3.6 million patients with overweight or obesity, of which 2.85 million (78.3%) are adults. For this project, 5 of the 6 sites with 2.07 million (72.6%) eligible adult patients with overweight or obesity participated. A detailed breakdown of study participation is found in the Figure.
Figure.
Consort diagram for patient data flow. BMI = body mass index.
Each participating site ran a query on its local data CDM to select patients from this larger LHSNet weight cohort, who fit the entry criteria but with an added stratification factor. For the query to be able to successfully run, all patients had to be older than 18 years, had to have existing weight and height (for which the program calculated a BMI), and the site had to be approved by the LHSNet steering committee and Mayo Clinic IRB (overseeing regulatory body) to participate in this project. The query randomly selected 4000 patients per site who met the criteria but with the added stratification of having 1000 patients selected per BMI category (overweight [BMI, 25-29.9 kg/m2], obesity class I [BMI, 30-34.9 kg/m2], obesity class II [BMI, 35-39.9 kg/m2], obesity class III or morbidly obese [BMI, >40 kg/m2]), totaling 4000 per site. This helped increase the representation of BMI category for patients invited into our study.
Once sites identified the patients who met entry criteria through their site CDM, they matched patients with their last known address. From the 20,000 patients selected to receive surveys for this study, 19,964 surveys were mailed during a 4-week period from October 27, 2017, through November 22, 2017, and data were collected from October 27, 2017, through March 1, 2018. Survey packets consisted of the survey, a cover letter, and a return stamped mailed envelope addressed to Mayo Clinic Survey Research Center.40 Returned surveys were accepted through March 1, 2018. The United States Postal Service returned 313 mailed surveys as “undeliverable.” Of the remaining 19,652 delivered surveys, 2799 (14.2%) were returned as completed and an additional 1033 (5.2%) refusal to participate. The Mayo Clinic Survey Research Center40 received, collated, and entered the data from all returned surveys using a dual data entry system.
Data Analysis
Continuous variables were summarized using mean ± SD and compared across BMI categories using analysis of variance. Categorical variables were summarized using frequency counts and percentages and compared across BMI categories using the χ2 test. To assess characteristics associated with the respondents’ perceptions of PCP behavior, a multivariable analysis was performed using logistic regression. The 3 multivariate models tested evaluated the following outcomes: “judged because of your weight,” “not always treated with respect,” and “not always treated as an equal.” The explanatory variables used in our 3 multivariate models included age, sex, race, marital status, education, multimorbidity, and BMI. In all cases, 2-tailed tests were performed, with P values of less than .05 considered statistically significant. All analyses were performed using SAS software, version 9.4 (SAS Institute).41
Results
Among the 2799 completed surveys, 419 (15.0%) were excluded from the analysis: 58 (2.1%) had incomplete sociodemographic data, 211 (7.5%) did not report current height and/or weight, and 150 (5.4%) reported height/weight consistent with BMI less than 25 kg/m2. Among 2380 evaluable surveys, 685 (27.0%) were for respondents with overweight, 656 (26.4%) obesity class I, 498 (20.0%) obesity class II, and 541 (21.9%) obesity class III.
As noted in Table 1, being younger, female, nonwhite, single, and having some college education or less were all associated with a higher BMI. The most frequent barriers to weight loss included food cravings (30.7%-49.9% for overweight to obesity class III, respectively) and the presence of a medical condition that limited physical activity (17.7%-47.1% for overweight to obesity class III, respectively). The percentage of respondents endorsing a given barrier increased with higher BMI for all the barriers assessed, with the exception of “not having enough time for physical activity.”
Table 1.
Respondent Characteristics
| Characteristic | Body mass index (kg/m2) |
P value | |||
|---|---|---|---|---|---|
| 25.0-29.9 (N=685a) | 30.0-34.9 (N=656a) | 35.0-39.9 (N=498a) | ≥40.0 (N=541a) | ||
| Age (y), mean ± SD | 62.1±14.9 | 60.9±13.7 | 58.8±13.3 | 54.3±14.1 | <.001 |
| Sex, No. (%) | <.001 | ||||
| Male | 326 (47.6) | 299 (45.6) | 177 (35.5) | 138 (25.5) | |
| Female | 359 (52.4) | 357 (54.4) | 321 (64.5) | 403 (74.5) | |
| Race, No. (%) | .02 | ||||
| White, non-Hispanic | 623 (93.4) | 584 (92.9) | 439 (90.9) | 468 (88.6) | |
| Other | 44 (6.6) | 45 (7.1) | 44 (9.1) | 60 (11.4) | |
| Marital status, No. (%) | <.001 | ||||
| Married/living as married | 511 (75.0) | 492 (75.5) | 354 (71.5) | 327 (61.0) | |
| Other | 170 (25.0) | 160 (24.5) | 141 (28.5) | 209 (39.0) | |
| Education, No. (%) | <.001 | ||||
| High school graduate or less | 134 (19.8) | 129 (20.0) | 103 (21.1) | 122 (23.1) | |
| Some college | 217 (32.1) | 222 (34.5) | 179 (36.7) | 234 (44.2) | |
| Four-year college degree or more | 325 (48.1) | 293 (45.5) | 206 (42.2) | 173 (32.7) | |
| Barriers to losing weight,b No. (%) | |||||
| Food cravings that prevent me from losing weight | 210 (30.7) | 248 (37.8) | 236 (47.4) | 270 (49.9) | <.001 |
| Medical condition that limits ability to do physical activity | 121 (17.7) | 200 (30.5) | 171 (34.3) | 255 (47.1) | <.001 |
| Cannot afford a gym membership | 56 (8.2) | 110 (16.8) | 116 (23.3) | 176 (32.5) | <.001 |
| Not enough time to do physical activity | 120 (17.5) | 118 (18.0) | 97 (19.5) | 95 (17.6) | .82 |
| Not sure which foods to eat to help lose weight | 53 (7.7) | 104 (15.9) | 70 (14.1) | 93 (17.2) | <.001 |
| Do not have access to a facility to do physical activity | 35 (5.1) | 58 (8.8) | 43 (8.6) | 81 (15.0) | <.001 |
| Do not have access to healthy food choices | 16 (2.3) | 22 (3.4) | 21 (4.2) | 47 (8.7) | <.001 |
| Pressure from my family or peers to not lose weight | 8 (1.2) | 9 (1.4) | 8 (1.6) | 17 (3.1) | .05 |
In all cases, data were missing for <5% of respondents. Because of missing data, the sum of the response categories for a given characteristic may not equal the total number of respondents.
Respondents may have indicated multiple barriers.
Higher BMI was significantly (P<.001) associated with reported comorbidities (Table 2), with the exception of heart disease (P=.61). Multimorbidity was self-reported in 53.1%, 68.0%, 70.9%, and 77.8% of respondents with overweight, obesity class I, obesity class II, and obesity class III, respectively (P<.001). Higher BMI was also associated with depression (9.1%, 14.0%, 16.0%, and 28.7%, overweight, obesity classes I, II, and III, respectively; P<.001), as well as being associated with worse self-reported current health (P<.001). In addition, percentage of respondents who reported that they avoided seeking health care in the previous 12 months for a given weight-related reason was found to increase with higher BMI (P<.001).
Table 2.
Medical Historya
| Characteristic, No. (%) | Body mass index (kg/m2) |
P value | |||
|---|---|---|---|---|---|
| 25.0-29.9 (N=685b) | 30.0-34.9 (N=656b) | 35.0-39.9 (N=498b) | ≥40.0 (N=541b) | ||
| Comorbidities | |||||
| Arthritis | 230 (33.6) | 277 (42.2) | 212 (42.6) | 259 (47.9) | <.001 |
| Diabetes mellitus | 85 (12.4) | 130 (19.8) | 119 (23.9) | 154 (28.5) | <.001 |
| High cholesterol | 279 (40.7) | 318 (48.5) | 242 (48.6) | 211 (39.0) | <.001 |
| High blood pressure | 275 (40.2) | 347 (52.9) | 297 (59.6) | 316 (58.4) | <.001 |
| Heart disease | 105 (15.3) | 108 (16.5) | 74 (14.9) | 74 (13.7) | .60 |
| Obstructive sleep apnea | 84 (12.3) | 153 (23.3) | 160 (32.1) | 245 (45.3) | <.001 |
| Depression | 137 (20.0) | 185 (28.2) | 170 (34.1) | 251 (46.4) | <.001 |
| Asthma | 66 (9.6) | 96 (14.6) | 73 (14.7) | 137 (25.3) | <.001 |
| Multimorbidityc | 364 (53.1) | 446 (68.0) | 353 (70.9) | 421 (77.8) | <.001 |
| Positive screen for current depression (PHQ-2) | 57 (9.1) | 83 (14.0) | 74 (16.0) | 145 (28.7) | <.001 |
| How would you describe your current health? | <.001 | ||||
| Very good/excellent | 343 (50.3) | 215 (33.2) | 119 (24.0) | 71 (13.3) | |
| Good | 255 (37.4) | 291 (44.9) | 243 (49.0) | 228 (42.5) | |
| Fair/poor | 84 (12.3) | 142 (21.9) | 134 (27.0) | 237 (44.2) | |
| Reasons for delaying health care visit in the previous 12 mo? | |||||
| Gained weight | 21 (3.2) | 54 (8.6) | 75 (15.5) | 113 (21.7) | <.001 |
| Were told to lose weight | 13 (2.0) | 40 (6.4) | 44 (9.2) | 91 (17.5) | <.001 |
| Thought you would be weighed | 42 (6.4) | 51 (8.1) | 64 (13.3) | 92 (17.7) | <.001 |
| Thought you would discuss your weight with your primary health care provider | 24 (3.7) | 45 (7.1) | 46 (9.5) | 71 (13.6) | <.001 |
| Thought you would be asked to undress | 18 (2.8) | 26 (4.1) | 24 (5.0) | 45 (8.7) | <.001 |
| Thought you could get rid of a medical problem by losing weight | 47 (7.2) | 113 (18.0) | 120 (25.0) | 154 (29.6) | <.001 |
PHQ-2 = Patient Health Questionnaire-2.
Data were missing for <5% of respondents for all characteristics with the exception of the PHQ-2 depression questions, which were missing for 8%.
Multimorbidity is defined as the presence of 2 or more of the comorbidities listed.
The participants’ experience with their PCPs is summarized in Table 3. The respondents’ interactions with their PCPs and their expectations of their PCPs differed across BMI categories. The percentage of respondents indicating that they and their PCP discussed their weight as a health concern increased with higher BMI (P<.001), ranging from 39.5% (overweight) to 87.2% (obesity class III). The percentage of respondents who reported that their PCP currently has a role in their weight management also increased with BMI (P<.001), ranging from 17.4% (overweight) to 29.6% (obesity class III). Increasing BMI was also associated with a decreased perception that their PCP has the knowledge/skills to help manage their weight (P<.001), ranging from 65.2% (overweight) to 53.0% (obesity class III). Respondents’ perception that their PCP was able to spend enough time to give them good weight loss advice (P<.001) also decreased with increasing BMI, ranging from 57.9% (overweight) to 43.9% (obesity class III). The percentage of respondents feeling judged by their PCP because of their weight increased with higher BMI (P<.001), ranging from 2.3% (overweight) to 12.1% (obesity class III). The percentage of respondents who felt that their PCP treated them with respect also differed by BMI (P<.001); the percentage of respondents who reported that they “always” felt respected by their PCP decreased from 87.7% among those who were overweight to 79.3% among those with obesity class III.
Table 3.
Interactions With Providers and Respondent Perception of Provider Behavior
| Question, No. (%) | Body mass index (kg/m2) |
P value | |||
|---|---|---|---|---|---|
| 25.0-29.9 (N=685a) | 30.0-34.9 (N=656a) | 35.0-39.9 (N=498a) | ≥40.0 (N=541a) | ||
| Not including mental health professionals, is there a primary health care provider that you see most often? | .75 | ||||
| Yes | 610 (92.9) | 581 (93.9) | 443 (94.1) | 486 (92.8) | |
| No | 47 (7.1) | 38 (6.1) | 28 (5.9) | 38 (7.2) | |
| In the past, have you and your health care provider ever discussed your weight as a health concern? | <.001 | ||||
| Yes | 262 (39.5) | 417 (65.4) | 373 (76.9) | 455 (87.2) | |
| No | 402 (60.5) | 221 (34.6) | 112 (23.1) | 67 (12.8) | |
| Do you believe your primary health care provider should have a role in your weight management? | .01 | ||||
| Yes | 497 (76.2) | 437 (69.3) | 352 (72.7) | 391 (74.8) | |
| No | 54 (8.3) | 45 (7.1) | 31 (6.4) | 25 (4.8) | |
| Not sure | 101 (15.5) | 149 (23.6) | 101 (20.9) | 107 (20.5) | |
| Does your primary health care provider currently have a role in your weight management? | <.001 | ||||
| Yes | 113 (17.4) | 138 (21.9) | 125 (25.9) | 154 (29.6) | |
| No | 500 (76.8) | 453 (71.9) | 321 (66.5) | 313 (6.2) | |
| Not sure | 38 (5.8) | 39 (6.2) | 37 (7.7) | 53 (10.2) | |
| Do you believe your primary health care provider has the necessary knowledge and skills to help you manage your weight? | <.001 | ||||
| Yes | 426 (65.2) | 360 (57.0) | 270 (55.8) | 278 (53.0) | |
| No | 42 (6.4) | 56 (8.9) | 48 (9.9) | 71 (13.6) | |
| Not sure | 185 (28.3) | 216 (34.2) | 166 (34.3) | 175 (33.4) | |
| Do you believe your primary health care provider is able to spend enough time to give you good weight loss advice? | <.001 | ||||
| Yes | 377 (57.9) | 319 (50.4) | 242 (49.9) | 229 (43.9) | |
| No | 108 (16.6) | 141 (22.3) | 123 (25.4) | 156 (29.9) | |
| Not sure | 166 (25.5) | 173 (27.3) | 120 (24.7) | 137 (26.2) | |
| Do you believe you could ask your primary health care provider for weight loss advice? | <.001 | ||||
| Yes | 588 (90.2) | 551 (86.9) | 403 (83.1) | 420 (80.5) | |
| No | 29 (4.4) | 37 (5.8) | 34 (7.0) | 50 (9.6) | |
| Not sure | 35 (5.4) | 46 (7.3) | 48 (9.9) | 52 (10.0) | |
| In the last 12 mo, did you ever feel that your primary health care provider judged you because of your weight? | <.001 | ||||
| Yes | 15 (2.3) | 30 (4.7) | 47 (9.7) | 63 (12.1) | |
| No | 621 (95.1) | 569 (89.9) | 403 (83.3) | 411 (78.7) | |
| Not sure | 17 (2.6) | 34 (5.4) | 34 (7.0) | 48 (9.2) | |
| In the last 12 mo, how often did you feel that your primary health care provider treated you with respect? | <.001 | ||||
| Never/rarely | 11 (1.7) | 6 (1.0) | 1 (0.2) | 9 (1.7) | |
| Sometimes | 6 (0.9) | 20 (3.1) | 15 (3.1) | 31 (5.9) | |
| Often | 63 (9.7) | 68 (10.7) | 58 (12.1) | 68 (13.0) | |
| Always | 571 (87.7) | 540 (85.2) | 407 (84.6) | 414 (79.3) | |
| In the last 12 mo, how often did your primary health care provider treat you as an equal? | .06 | ||||
| Never/rarely | 19 (2.9) | 23 (3.7) | 18 (3.8) | 27 (5.2) | |
| Sometimes | 26 (4.0) | 32 (5.1) | 30 (6.3) | 37 (7.1) | |
| Often | 106 (16.4) | 106 (16.8) | 80 (16.7) | 105 (20.3) | |
| Always | 496 (76.7) | 469 (74.4) | 350 (73.2) | 349 (67.4) | |
Because of missing data, the sum of the response categories for a given characteristic may not equal the total number of respondents.
Multivariable analysis (Table 4) demonstrates that the likelihood of feeling judged by their PCP decreased with age (odds ratio [OR], 0.77 [95% CI, 0.67-0.88] per 10 years; P<.001) and was higher among females (OR, 1.52 [95% CI, 1.02-2.25]; P=.04), those with multiple morbidities (OR, 1.73 [95% CI, 1.13-2.66]; P=.01), and those with higher BMI (OR, 2.38 [95% CI, 1.22-4.63], 4.62 [95% CI, 2.45-8.74], and 5.26 [95% CI, 2.78-9.96] for obesity classes I, II, and III compared with overweight; P<.001). The likelihood of not always feeling as though they were treated with respect was found to decrease with increasing age (OR, 0.80 per 10 years [95% CI, 0.73-0.87]; P<.001) and education level (OR, 0.66 [95% CI, 0.48-0.91] for those with 4-year college degree or more compared with those with a high school education or less; P=.01).
Table 4.
Multivariable Analysis of Characteristics Associated With Respondent’s Perception of Provider Behaviora
| Characteristic | Judged because of your weight |
Not always treated with respect |
Not always treated as an equal |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age, per 10 y | 0.77 | 0.67-0.88 | <.001 | 0.80 | 0.73-0.87 | <.001 | 0.88 | 0.82-0.95 | <.001 |
| Sex | .04 | .82 | .40 | ||||||
| Male | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Female | 1.52 | 1.02-2.25 | 1.03 | 0.80-1.33 | 1.09 | 0.89-1.34 | |||
| Race | .10 | .30 | .12 | ||||||
| White, non-Hispanic | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Other | 1.55 | 0.91-2.62 | 0.23 | 0.83-1.82 | 0.75 | 0.52-1.08 | |||
| Marital status | .61 | .38 | .28 | ||||||
| Married/living as married | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Other | 0.91 | 0.62-1.33 | 1.12 | 0.87-1.46 | 1.13 | 0.91-1.40 | |||
| Education | .19 | .01 | .87 | ||||||
| High school graduate or less | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Some college | 0.95 | 0.58-1.55 | 0.99 | 0.72-1.35 | 1.05 | 0.81-1.37 | |||
| Four-year college degree or more | 1.33 | 0.83-2.14 | 0.66 | 0.48-0.91 | 0.99 | 0.76-1.29 | |||
| Multimorbidity | .01 | .91 | .05 | ||||||
| No | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| Yes | 1.73 | 1.13-2.66 | 0.98 | 0.75-1.30 | 1.26 | 1.00-1.58 | |||
| Body mass index (kg/m2) | <.001 | .10 | .12 | ||||||
| 25.0-29.9 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | |||
| 30.0-34.9 | 2.38 | 1.22-4.63 | 1.24 | 0.89-1.74 | 1.06 | 0.81-1.38 | |||
| 35.0-39.9 | 4.62 | 2.45-8.74 | 1.10 | 0.76-1.57 | 1.05 | 0.79-1.40 | |||
| ≥40.0 | 5.26 | 2.78-9.96 | 1.51 | 1.07-2.14 | 1.37 | 1.03-1.82 | |||
Each of the questions listed in Table 4 was analyzed using logistic regression. For the question assessing whether the respondent felt judged because of their weight those who responded “Not sure” were excluded from the analysis. For the questions assessing whether respondents felt they were treated with respect and treated as an equal, response categories were combined so that the dependent variable was “Always” vs “Not always.”
Discussion
In a survey of nearly 2500 patients with overweight or obesity, we found that although most patients reported generally positive experiences of clinical weight management, perceptions of their experiences and expectations were markedly different depending on their BMI. Although most patients did not feel judged by their PCP and felt respected by their PCP, those with a higher BMI were less likely to report feeling respected and more likely to feel judged by their PCP. Although expectations that PCPs would help patients lose weight and had the knowledge and skills for this task were generally high, they decreased with higher BMI. These beliefs may contribute to the self-reported barriers to weight loss and delays in seeking health care.
Practice guidelines for the management of adults with overweight or obesity that call for PCPs to identify, counsel, and offer treatment (ie, ask, advise, treat) have been well established.9 Although our survey responders expressed a belief that their PCP should have a role in their weight management, they also indicated that their PCP may not necessarily have the skills to help them. This is consistent with evidence that PCPs also do not feel that they have the skills to treat obesity.11 In our study, patients with a higher BMI (>40 kg/m2) felt that they were less respected and increasingly judged compared with their counterparts with a lower BMI (25-39 kg/m2). Both “lack of respect” and “increased judgment” have been previously linked to delaying/avoiding seeking medical advice.11, 16, 42, 43 Results of our study predominantly identified as white race were similar to those described in a study15 with a large African American patient population. The similar experiences expressed by these sociodemographically different patient populations point to a critical need to raise awareness of patient experiences and develop clinical practice strategies for effectively engaging patients with overweight or obesity in empathetic and respectful ways.
A previous survey, conducted by our study team at a single primary care clinic, found that as the BMI increased, patients did not wish to receive any weight loss messages from their PCPs and if they received any such messages, they felt less motivated to act.14 In this current study, responders with a higher BMI indicated delaying their health care visit because they “did not want to receive weight loss advice from their PCP.” The tone and delivery of the message is just as important as the message itself. On the basis of the current study, if the patient perceives the content of the message delivered to be disrespectful or judgmental, it can have a negative impact on patients’ perceptions and follow-through.10 As demonstrated by our results, this negative impact could be the result of feeling that their PCP lacked the necessary skills to help them with their weight management or behaved in a disrespectful or judgmental manner. These exact reasons for delaying/canceling health care appointments have been self-reported by patients in previous studies.16, 42, 43 A recent survey has shown that 55% of health care professionals did not feel adequately trained to care for patients with obesity and although physicians had a higher level of knowledge, compared with nurses, they also exhibited more negative attitudes toward patients with obesity; in contrast, nurses had more difficulties engaging patients in conversations about weight.11 In this study, physicians also admitted that their increased workload made taking care of patients with overweight and obesity difficult and questioned whether weight management should be a team objective.11 This is consistent with calls to shift weight management counseling away from PCPs to individuals with adequate training.23 This has been confirmed by a series of focus groups44 where it was found that patients were interested in specific and tailored guidance and instructions around weight management. Within these focus groups, the top 3 strategies identified as having the most impact included referrals to a dietitian, medications, and exercise.44
Despite high interest by patients in receiving weight management resources from their PCP,15 many PCPs do not broach the subject with their patients45, 46, 47 and less than a third of respondents in our survey indicated that their PCP had a role in their weight management. Primary care practitioners may see weight management as outside of their expertise, and patients may be seeking weight management support from other health care providers (eg, specialists and dietitians) or from commercial sources. The importance of addressing weight loss is evident in the improvement in chronic disease risk factors with sustained weight loss of 5% to 10%.48 The positive role of the PCP messaging was reinforced in a study comparing 2 interventions (Web-based and in-person coaching programs) to a control group and found that the 2 intervention groups, both including PCP participation, have twice the weight loss as the control (38.2%, 41.4% vs 18.8%) at the end of 24 months. However, this study did not consider the confounding role of the PCP in both intervention groups.49
Although patients indicate that one of the biggest contributions a PCP can make in helping them reduce their weight is to simply ask them about their interest in losing weight,15 many PCPs may be under the impression that asking about weight negatively affects their patient-provider rapport. Although this is a possibility, asking about interest in discussing weight is what patients want. Not engaging in such a discussion may give the impression of lack of knowledge and interest. If this is an unmet expectation for patients, it may lead to patients’ decision to delay further contact with their PCP. In our study, we found that 4 of the 8 (50%) barriers named by our responders could be overcome with education by the PCP or PCP office staff (ie, “food cravings,” “not sure which foods to eat,” “access to healthy food choices,” “access to physical activity facility”). This was corroborated by a recent systematic review of 13 weight loss interventions whereby it was demonstrated that patient education about weight loss is possible.50
Our study has several strengths and limitations. One of the strengths is the generalizability by the inclusion of 5 diverse sites throughout 11 states.30 An additional strength was our effort to establish patients’ trust and reduce barriers to survey participation by anonymizing the surveys. But there were several downsides to this action: (1) the participants’ data could not be linked to any health data/experience on record; (2) there could only be 1 mailing; and (3) we could not trace reasons for nonresponse. Although the 14.2% response rate may have resulted in a study sample not being representative of the general population of patients with overweight and obesity receiving health care at study sites, it should be noted that response rates of mailed surveys have been steadily declining in recent years.51, 52, 53, 54, 55, 56 In addition, our surveys had a one-time mailing during the US holiday season with a generic cover letter (data collection for this survey occurred from October 27, 2017, through March 1, 2018). It should be noted that the return rate of 14.2% is comparable to that in another study using this database that had a rare disease focus and had a similar approach to data collection. For that data collection, the return rate was 18%. We are also limited in the knowledge of reasons for nonparticipation between those returning surveys and those who actively opted out by returning refusals, and we have no information on those who did not respond to our survey. A final limitation is that although we surveyed patients from 5 diverse institutions, our respondents were predominantly non-Hispanic white (93%). Despite the uniformity of the race and ethnicity of our population, the self-reported experiences and attitudes toward their PCP are similar to those identified by study samples of differing race/ethnicity.15
Conclusion
Although many patients with overweight and obesity report comfort and a desire to discuss weight management with their PCP, barriers still exist to patients receiving obesity screening and care that meet clinical recommendations and patients’ needs. These barriers are higher among individuals with higher BMI; among individuals with BMIs of greater than or equal to 40, several barriers to seeking health care exist, and delay of health care due to concerns about weight are common. Patients and providers would benefit from additional education and resources to create positive health care experiences in which all patients are able to receive evidence-based care and resources and referrals to strategies known to be supportive of individuals with obesity.
Acknowledgments
We thank the grant principal investigator, Dr Veronique Roger, for her endless support and advice during the entire study process and the entire LSHNet investigative team for providing help and support to make this endeavor possible.
We take this time to also thank Drs Irina Haller (Essentia Health), Ramona DeJesus (Mayo Clinic), David Williams (University of Michigan), Stephanie Schroeder (Arizona State University), Mr Nathan Tesch (Mayo Clinic), and Mr Scott Brue (Mayo Clinic), as well as Ms Meaghan Ridler (Olmsted County Health Department). In addition, special thanks to Lisa Ferguson (University of Michigan), Allise Taran (Essentia Health), Cassandra Rodgers (Allina Health), and Tameka Sama (Arizona State University) for cofacilitating the site process by obtaining site regulatory readiness, identifying patients who met study criteria, and mailing the study surveys. An additional thank-you is extended to the Mayo Clinic Department of Medicine Clinical Research Office Coordinator staff that was instrumental in pilot testing the survey instrument used in this study and a sincere thanks to the Mayo Clinic Survey Research Center, especially Libby Hammond, without whom this study would not have been possible.
Finally, a special thanks to all the survey participants throughout Mayo Clinic, Ohio State University, University of Michigan, Essentia Health Systems, and Allina Health Systems who took the time to complete this survey.
Footnotes
Grant Support: This research was supported by grant CDRN-1501-26638 from the Patient-Centered Outcomes Research Institute (Principal Investigator: Veronique L. Roger, MD).
Potential Competing Interests: The authors report no competing interests.
References
- 1.Abdelaal M., le Roux C.W., Docherty N.G. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161. doi: 10.21037/atm.2017.03.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grunvald E. Medical management of obesity: a comprehensive review. Clin Obstet Gynecol. 2014;57(3):465–484. doi: 10.1097/GRF.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Obesity. Fact Sheet N. 311. http://www.wpro.who.int/mediacentre/factsheets/obesity/en/
- 4.Hruby A., Hu F.B. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673–689. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahan S.I. Practical strategies for engaging individuals with obesity in primary care. Mayo Clin Proc. 2018;93(3):351–359. doi: 10.1016/j.mayocp.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein E.A., Trogdon J.G., Cohen J.W., Dietz W. Annual medical spending attributable to obesity: payer and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 7.Hammond R.A., Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes. 2010;3:285–295. doi: 10.2147/DMSOTT.S7384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services Decision memo for intensive behavioral therapy for obesity (CAG-00423N) https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?&NcaName=Intensive%20Behavioral%20Therapy%20for%20Obesity&bc=ACAAAAAAIAAA&NCAId=253&
- 9.Jensen M.D., Ryan D.H., Apovian C.M., et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25, pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Koball A.M., Mueller P.S., Craner J., et al. Crucial conversations about weight management with healthcare providers: patients’ perspectives and experiences. Eat Weight Disord. 2018;23(1):87–94. doi: 10.1007/s40519-016-0304-6. [DOI] [PubMed] [Google Scholar]
- 11.Bucher Della Torre S., Courvoisier D.S., Saldarriaga A., Martin X.E., Farpour-Lambert N.J. Knowledge, attitudes, representations and declared practices of nurses and physicians about obesity in a university hospital: training is essential. Clin Obes. 2018;8(2):122–130. doi: 10.1111/cob.12238. [DOI] [PubMed] [Google Scholar]
- 12.Turner M., Jannah N., Kahan S., Gallagher C., Dietz W. Current knowledge of obesity treatment guidelines by health care professionals. Obesity (Silver Spring) 2018;26(4):665–671. doi: 10.1002/oby.22142. [DOI] [PubMed] [Google Scholar]
- 13.Wadden T.A., Butryn M.L., Hong P.S., Tsai A.G. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA. 2014;312(17):1779–1791. doi: 10.1001/jama.2014.14173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Croghan I.T., Huber J.M., Hurt R.T., et al. Patient perception matters in weight management. Prim Health Care Res Dev. 2018;19(2):197–204. doi: 10.1017/S1463423617000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tucker C.M., Williams J.L., Wippold G.M., et al. Views of diverse primary care patients on the roles of healthcare providers and staff and the influence of other variables in their weight management. Clin Obes. 2018;8(1):11–20. doi: 10.1111/cob.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edmunds L.D. Parents’ perceptions of health professionals’ responses when seeking help for their overweight children. Fam Pract. 2005;22(3):287–292. doi: 10.1093/fampra/cmh729. [DOI] [PubMed] [Google Scholar]
- 17.Gudzune K.A., Beach M.C., Roter D.L., Cooper L.A. Physicians build less rapport with obese patients. Obesity (Silver Spring) 2013;21(10):2146–2152. doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gudzune K.A., Bennett W.L., Cooper L.A., Clark J.M., Bleich S.N. Prior doctor shopping resulting from differential treatment correlates with differences in current patient-provider relationships. Obesity (Silver Spring) 2014;22(9):1952–1955. doi: 10.1002/oby.20808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penner L.A., Dovidio J.F., West T.V., et al. Aversive racism and medical interactions with black patients: a field study. J Exp Soc Psychol. 2010;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McConnell A.R., Leibold J.M., Sherman S.J. Within-target illusory correlations and the formation of context-dependent attitudes. J Pers Soc Psychol. 1997;73(4):675–686. doi: 10.1037//0022-3514.73.4.675. [DOI] [PubMed] [Google Scholar]
- 21.Dovidio J.F., Kawakami K., Gaertner S.L. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol. 2002;82(1):62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- 22.Greenwald A.G., Poehlman T.A., Uhlmann E.L., Banaji M.R. Understanding and using the Implicit Association Test: III, meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 23.Phelan S.M., Puhl R.M., Burke S.E., et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ. 2015;49(10):983–992. doi: 10.1111/medu.12770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sabin J.A., Marini M., Nosek B.A. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One. 2012;7(11):e48448. doi: 10.1371/journal.pone.0048448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hebl M.R., Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- 26.Selby J.V., Krumholz H.M., Kuntz R.E., Collins F.S. Network news: powering clinical research. Sci Transl Med. 2013;5(182):182fs13. doi: 10.1126/scitranslmed.3006298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corley D.A., Feigelson H.S., Lieu T.A., McGlynn E.A. Building data infrastructure to evaluate and improve quality: PCORnet. J Oncol Pract. 2015;11(3):204–206. doi: 10.1200/JOP.2014.003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins F.S., Hudson K.L., Briggs J.P., Lauer M.S. PCORnet: turning a dream into reality. J Am Med Inform Assoc. 2014;21(4):576–577. doi: 10.1136/amiajnl-2014-002864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fleurence R.L., Curtis L.H., Califf R.M., Platt R., Selby J.V., Brown J.S. Launching PCORnet, a national patient-centered clinical research network. J Am Med Inform Assoc. 2014;21(4):578–582. doi: 10.1136/amiajnl-2014-002747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finney Rutten L.J., Alexander A., Embi P.J., et al. Patient-Centered Network of Learning Health Systems: developing a resource for clinical translational research. J Clin Transl Sci. 2017;1(1):40–44. doi: 10.1017/cts.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.LHSNet LHSNet: Patient Centered Network of Learning Health Systems. 2017. https://www.lhsnet.org/
- 32.Potter M.B., Vu J.D., Croughan-Minihane M. Weight management: what patients want from their primary care physicians. J Fam Pract. 2001;50(6):513–518. [PubMed] [Google Scholar]
- 33.Drury C.A., Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 34.Myers A., Rosen J.C. Obesity stigmatization and coping: relation to mental health symptoms, body image, and self-esteem. Int J Obes Relat Metab Disord. 1999;23(3):221–230. doi: 10.1038/sj.ijo.0800765. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K., Spitzer R.L., Williams J.B. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 36.Saltzer E.B. The weight locus of control (WLOC) scale: a specific measure for obesity research. J Pers Assess. 1982;46(6):620–628. doi: 10.1207/s15327752jpa4606_11. [DOI] [PubMed] [Google Scholar]
- 37.National Cancer Institute HINTS: Health Information Trends Survey. https://hints.cancer.gov
- 38.Heatherton T.F., Polivy J. Development and validation of a scale for measuring state self-esteem. J Pers Soc Psychol. 1991;60(6):895–910. [Google Scholar]
- 39.Centers for Disease Control and Prevention Adverse childhood experiences (ACEs) https://www.cdc.gov/violenceprevention/acestudy/index.html
- 40.Mayo Clinic Survey Research Survey Research Center. http://surveyresweb.mayo.edu/
- 41.SAS Institute Inc . SAS Institute; Cary, NC: 2017. SAS/STAT User’s Guide—Version 9.4. [Google Scholar]
- 42.Bertakis K.D., Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13(9):1615–1623. doi: 10.1038/oby.2005.198. [DOI] [PubMed] [Google Scholar]
- 43.Meisinger C., Heier M., Loewel H. The relationship between body weight and health care among German women. Obes Res. 2004;12(9):1473–1480. doi: 10.1038/oby.2004.184. [DOI] [PubMed] [Google Scholar]
- 44.Kennedy B.M., Kennedy K.B., Sarpong D.F., Katzmarzyk P.T. Perceptions of obesity treatment options among healthcare providers and low-income primary care patients. Ochsner J. 2016;16(2):158–165. [PMC free article] [PubMed] [Google Scholar]
- 45.Huang J., Yu H., Marin E., Brock S., Carden D., Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156–161. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 46.Look AHEAD Research Group Eight-year weight losses with an intensive lifestyle intervention: the Look AHEAD study. Obesity (Silver Spring) 2014;22(1):5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bennett W.L., Gudzune K.A., Appel L.J., Clark J.M. Insights from the POWER practice-based weight loss trial: a focus group study on the PCP’s role in weight management. J Gen Intern Med. 2014;29(1):50–58. doi: 10.1007/s11606-013-2562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Heart, Lung, and Blood Institute Managing overweight and obesity in adults: systematic evidence review from the Obesity Expert Panel 2013. https://www.nhlbi.nih.gov/sites/default/files/media/docs/obesity-evidence-review.pdf
- 49.Appel L.J., Clark J.M., Yeh H.C., et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Faruqi N., Spooner C., Joshi C., et al. Primary health care-level interventions targeting health literacy and their effect on weight loss: a systematic review. BMC Obes. 2015;2:6. doi: 10.1186/s40608-015-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bradburn N.M. Proceedings of the Forty-Seventh Annual Conference of the American Association for Public Opinion Research: Presidential address: a response to the nonresponse problem. Public Opin Q. 1992;56(3):391–397. [Google Scholar]
- 52.Groves R.M. John Wiley & Sons; Hoboken, NJ: 2004. Survey Errors and Survey Costs. [Google Scholar]
- 53.Curtin R., Presser S., Singer E. Changes in telephone survey nonresponse over the past quarter century. Public Opin Q. 2005;69(1):87–98. [Google Scholar]
- 54.Nohr E.A., Frydenberg M., Henriksen T.B., Olsen J. Does low participation in cohort studies induce bias? Epidemiology. 2006;17(4):413–418. doi: 10.1097/01.ede.0000220549.14177.60. [DOI] [PubMed] [Google Scholar]
- 55.Forthofer R.N. Investigation of nonresponse bias in NHANES II. Am J Epidemiol. 1983;117(4):507–515. doi: 10.1093/oxfordjournals.aje.a113568. [DOI] [PubMed] [Google Scholar]
- 56.Bradshaw L., Sumner J., Delic J., Henneberger P., Fishwick D. Work aggravated asthma in Great Britain: a cross-sectional postal survey. Prim Health Care Res Dev. 2018:1–9. doi: 10.1017/S1463423618000063. [DOI] [PMC free article] [PubMed] [Google Scholar]