Abstract
Objectives
To investigate the effect of inhaler technique education delivered by a clinical pharmacist to patients hospitalised for asthma, on inhaler technique scores and asthma control at three months post-discharge.
Methods
This pre-post interventional study in Jordan enrolled patients who had been admitted for asthma and were using controller medication by Accuhaler [Diskus] (ACC), Turbuhaler (TH) or Pressurized metered dose inhalers (pMDI). Inhaler technique was assessed using published checklists (score 0–9). Asthma symptom control was assessed by Asthma Control Test (ACT, range 5–25). Patients were assessed on admission (baseline), pre-discharge, and 3 months later. All patients received a ‘Show-and-Tell’ inhaler technique counseling service prior to discharge.
Results
Baseline data were available for 140 patients, 71% females, mean age 52.7 (SD 16.64) years, mean ACT score 10.0 (SD 4.8). Mean inhaler score was 7.5 (SD 1.52) with no significant difference between the inhaler groups (p = 0.174). After pre-discharge training, all patients had correct technique (score 9/9). After 3 months, mean inhaler scores were significantly higher than at baseline (8.14 (SD 0.87, p < 0.001), with mean change significantly higher for TH 1.21 (SD 2.25) and ACC 0.85 (SD 0.97) than pMDI (0.16; SD 0.72), p = 0.001. Symptom control improved significantly for all patients, with a mean increase in ACT score of 7.54 (SD 8.18), with no significant difference between the inhaler device groups (p = 0.326).
Conclusions
Patients hospitalized for asthma achieved correct inhaler technique after training by a pharmacist, and maintained better technique at 3 months than on admission. Significant improvements in ACT scores were documented for all inhaler groups.
Keywords: Inhaler technique, Asthma control, Asthma knowledge, Pharmaceutical care, Hospitalized asthma patients, Jordan
1. Introduction
Asthma is a chronic health condition affecting millions worldwide (Global Initiative for Asthma (GINA) - Global strategy for asthma management and prevention report 2017), and developing countries are no exception (Abu-Ekteish et al., 2009). Current international asthma management guidelines (Global Initiative for Asthma (GINA) - Global strategy for asthma management and prevention report 2017) define asthma control as having no or minimal daytime and nocturnal symptoms, no or minimal use of rescue bronchodilators, no acute exacerbations and normal or near-normal lung function. Nevertheless, many patients with asthma continue to live with uncontrolled symptoms leading to hospitalization, low health-related quality of life (Guilbert et al., 2011) and increased cost of treatment (Dal Negro et al., 2016).
Important reasons for uncontrolled asthma include poor adherence, poor asthma knowledge by patients and poor skills in inhaler technique (Basheti et al., 2016, The British Guideline on the Management of Asthma, 2017). Suboptimal inhaler use is associated with poorer asthma control (Basheti et al., 2007), with obvious consequences on day-to-day lives and exacerbation risk (Giraud and Roche, 2002). This problem appears common across the spectrum of inhaler devices, both dry powder inhalers (DPIs) such as Accuhaler [ACC, Diskus] and Turbuhaler (TH) and Pressurized metered dose inhalers (pMDIs) (van der Palen et al., 1998, Basheti et al., 2011, Bosnic-Anticevich et al., 2010). These devices are used for delivery of inhaled corticosteroids (ICS) alone, or in combination with long-acting β2-agonists (LABA); their correct use is thus a cornerstone in asthma management (Global Initiative for Asthma (GINA) - Global strategy for asthma management and prevention report 2017).
Research in primary health care settings indicates that educating patients in correct use of their inhalers results in mastery of good inhaler technique and improved asthma control (Basheti et al., 2008, Basheti et al., 2007, Melani et al., 2011). In these studies, pharmacists had an important role in providing both initial training for first-time inhaler users and subsequent regular, re-training (Basheti et al., 2009). However, incorrect inhalation technique is still a common problem, not only for patients (Price et al., 2013), but also for healthcare professionals (Basheti et al., 2014b).
Patients with hospitalizations due to asthma exacerbations are at the highest risk and need a higher level of asthma management (Hasegawa et al., 2015). Hospitalization provides an important opportunity to provide asthma education and self-management skills. Inhaler technique is amongst the skills that need optimization for this high-risk population of asthma patients (Press et al., 2011).
The objective of the current study was to investigate the impact of an educational inhaler technique intervention delivered prior to discharge from an asthma hospitalization in Amman, Jordan, on inhaler technique scores and asthma control at three months post-discharge, and to identify factors associated with change in asthma control.
2. Methods
For this prospective pre-post interventional study, patients were recruited from the respiratory wards at two public hospitals in Amman, Jordan. Ethics approval was obtained from the Jordanian Ministry of Health and the study hospitals. The study was preceded by a pilot study at the same hospitals to assess feasibility, recognise and address barriers, and evaluate clarity and readability of the developed questionnaires.
Patients hospitalized for asthma were eligible if they were aged ≥14 years, had a doctor diagnosis of asthma, and had been using ICS-containing medication via ACC, TH or pMDI with no change for ≥1 month prior to study. Patients were excluded if they did not self-administer their inhaled therapy, did not speak and understand the Arabic or English language, were not able to commit to study procedures and a 3-month follow-up visit, or were involved in another clinical study.
As soon as possible after admission (preferably within 24 h), eligible patients were approached by the study researcher (a clinical pharmacist who is an expert in asthma management and inhaler technique education), after confirmation by their treating specialist that asthma was the reason for hospitalization. Participants provided written informed consent.
2.1. Baseline assessments
At baseline, data were collected including demographics, asthma history and medication use (including complementary treatments), hospital admissions and oral corticosteroid use, and past inhaler technique education.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jsps.2018.06.002.
Inhaler technique was assessed by the researcher (baseline assessment) for the patient’s controller device, using placebo inhalers provided by AstraZeneca Pharmaceuticals (Wilmington, Delaware; Amman, Jordan) and GlaxoSmithKline (Philadelphia, Pennsylvania; Amman, Jordan), and standardized inhaler technique checklists (see Online Appendix 1) translated into Arabic (Basheti et al., 2014a, Bosnic-Anticevich et al., 2010). Each checklist consisted of 9 steps (potential score 0–9). A score of 9/9 was classified as correct technique for the TH, four steps were classified as ‘essential’ (without which little or no medication would reach the airway), and for the ACC and pMDI, three steps were classified as essential (Basheti et al., 2014a).
Supplementary material.
Asthma symptom control over the previous 4 weeks was assessed using a published Arabic translation of the 5-item Asthma Control Test (ACT).(Lababidi et al., 2008) ACT scores range between 5 and 25, with higher scores indicating better asthma symptom control; ACT score >19 indicates well controlled asthma, 16–19 not-well-controlled asthma, and 5–15 very-poorly controlled asthma (Schatz et al., 2006).
Asthma knowledge was assessed using the consumer asthma knowledge test questionnaire (AKT) (Kritikos et al., 2005). The original questionnaire comprised 12 questions about asthma and its treatment. Questions ‘4′ and ‘11′ were omitted following feedback from the patients during the pilot study (question ‘4′, about actions in response to asthma triggers, was confusing to many while question ‘11′ was directed at parents of children with asthma). Hence, the maximal (highest) score was 10 (Kritikos et al., 2005).
2.2. Pre-discharge assessment and intervention
Prior to discharge, the questionnaire (see Online Appendix 2) was administered to all participants in face-to-face interviews regarding any inhaler information and training that they received during their hospital stay. The researcher then assessed patients’ inhaler technique (pre-discharge assessment), then used a specialized ‘‘Show and Tell’’ inhaler technique counselling service to optimize inhaler technique (Basheti et al., 2007). The researcher went through each step on the device-specific checklist with the patient in Arabic, to describe and demonstrate correct use, then checked the patient’s technique again. This cycle of assessment and counselling was repeated up to three times if necessary, until the patient demonstrated correct technique on all steps (score 9/9) (Basheti et al., 2007).
Patients were requested by the researcher to come back to the specialist clinic 3–4 months after discharge. At this visit, the researcher met them before they saw their specialist and reassessed their inhaler technique, asthma control, any change in treatment, and asthma knowledge (3-month follow-up assessment).
2.3. Data analysis
The primary outcome was change in ACT score between baseline and 3 months. Data were analysed with the Statistical Package for Social Sciences (SPSS) version 20 (Chicago, Illinois). Proportions were compared with Pearson’s chi-square test. For continuous variables, comparisons between groups were performed by Independent Sample T test, Paired sample t test, Wilcoxon signed-rank test, and Mann–Whitney U test. Differences with p < 0.05 were considered statistically significant.
In order to determine predictors of improved asthma symptom control over the study period, a multiple linear regression analysis was performed after assessment for collinearity. The dependent variable was change in ACT score from baseline to follow-up visit. Independent variables included inhaler type (ACC, TH or pMDI), age, gender, income, smoking status, ACT scores at baseline, AKT scores at baseline and at follow-up, duration of preventer use, patient education level, baseline inhaler technique score and change in inhaler technique score over study period. This analysis was repeated for the dependent variable ACT score at follow-up.
Multiple linear regression modelling including the independent variables mentioned above was conducted for the dependent variable ACT score at baseline, excluding ‘ACT scores at baseline’ from the independent variables’ list’ and including ‘hospital admissions during the past year’.
The same independent variables were used in a multiple linear regression analysis to determine predictors of inhaler technique score at follow-up (the dependent variable), with substitution of final ACT score for final inhaler technique score.
2.4. Sample size calculations
Sample size determination was based on the primary outcome variable of inhaler technique scores improvement pre and post education based on our previous work in this area. (Basheti et al., 2007, Basheti et al., 2008) In order to detect a significantly different change in inhaler technique score of 1 point difference, with a significance level of 5%, and power of 80%, with the standard deviation of the change being 1.4 points (Basheti et al., 2007)., a sample size of 15 patients for each type of inhaler used (Turbuhaler, Diskus, pMDI needs to be recruited into this pre-post designed study. Accounting for a dropout rate of 20%, a sample size of 54 patients would be required. The sample size was increased to 140 to allow for analysis of factors relating to change in ACT score.
3. Results
3.1. Baseline characteristics
A total of 161 subjects were approached to participate in the study, and 140 (87.0%) agreed to be enrolled (Fig. 1). The mean age was 52.70 (SD 16.64) years, and 70.7% were female. No clinically important differences were found in demographic or baseline characteristics between the inhaler groups (Table 1, Fig. 2A). Sixty patients (42.9%) had ≥1 asthma-related admissions in the previous year. Mean asthma knowledge scores were low (6.53 out of 10 (SD 1.68)) across inhaler groups.
Fig. 1.
Flow chart of study participation.
Table 1.
Baseline demographics and characteristics for study participants (n = 140) using a controller medication by Accuhaler, Turbuhaler or Pressurized Metered Dose Inhaler (pMDI) at admission.
| Variable | Accuhaler, n = 41 | Turbuhaler, n = 23 | pMDI, n = 76 | All, n = 140 | P value |
|---|---|---|---|---|---|
| Age, mean (SD) | 52.29 (15.69) | 55.30 (17.27) | 52.13 (17.08) | 52.70 (16.64) | 0.716 |
| Gender, females, n (%) | 27 (65.9) | 16 (72.7) | 56 (73.7) | 99 (70.7) | 0.668 |
| Education level, n (%) | n = 36 | n = 19 | n = 68 | n = 123 | 0.515 |
| Not educated | 10 (27.8) | 4 (21.1) | 15 (22.1) | 29 (23.6) | |
| Elementary school | 8 (22.2) | 6 (31.6) | 21 (30.9) | 35 (28.5) | |
| High school | 11 (30.6) | 6 (31.6) | 22 (32.4) | 39 (31.7) | |
| College | 2 (5.6) | 3 (15.8) | 7 (10.3) | 12 (9.8) | |
| University | 5 (13.9) | 0 (0.0) | 3 (4.4) | 8 (6.5) | |
| Working status, n (%) | n = 39 | n = 20 | n = 71 | n = 130 | 0.553 |
| Employed | 7 (17.9) | 2 (10.0) | 8 (11.3) | 17 (13.1) | |
| Student | 2 (5.1) | 1 (5.0) | 2 (2.8) | 5 (3.8) | |
| Unemployed | 25 (64.1) | 15 (75.0) | 55 (77.5) | 95 (73.1) | |
| Retired | 5 (12.8) | 2 (10.0) | 6 (8.5) | 13 (10.0) | |
| Amman locationa, n (%) West: East: Outside |
n = 41 | n = 22 | n = 75 | n = 138 | 0.233 |
| 5:19:17 (12.2:46.3:41.4) |
5:11:6 (22.7:50.0:27.3) |
7:47:21 (9.3:62.7:28) |
17:77:44 (12.3:55.8:31.9) |
||
| Marital status, n (%) married: widowed: divorced: single |
n = 39 | n = 20 | n = 74 | n = 133 | 0.950 |
| 26:7:2:4 (66.7:17.9:5.1: 10.3) |
14:4:1:1 (70.0:20.0:5.0: 5.0) |
52:11:2:9 (70.3:14.9:2.7: 12.2) |
92:22:5:14 (69.2:16.5:3.8: 10.5) |
||
| Yearly incomeb, mean (SD) | 2780.2 (3647.7) |
1999.6 (1311.1) |
2099.1 (1640.3) |
2297.0 (2419.2) |
0.384 |
| Number of family members, mean (SD) | 5.7 (4.3) | 7.0 (3.6) | 5.5 (2.8) | 5.8 (3.4) | 0.268 |
| Smoking status n (%) Non-smoker: ex- smoker: current smoker |
n = 39 | n = 22 | n = 72 | n = 133 | 0.534 |
| 21:12:6 (53.8:30.8:15.4) |
12:5:5 (54.5:22.7:22.7) |
46:19:7 (63.9:26.4:9.7) |
79:36:18 (59.4:27.1:13.5) |
||
| Age of onset of asthma, n (%) Infant: 2–12:>12 years |
n = 35 | n = 19 | n = 70 | n = 124 | 0.583 |
| 0:2:33 (0.0:5.7:94.3) |
1:0:18 (5.3:0.0:94.7) |
2:2:66 (2.9:2.9:94.3) |
3:4:117 (2.4:3.3:95.1) |
||
| Age at diagnosis, mean (SD) | 37.5 (14.6) | 41.7 (18.6) | 37.8 (18.4) | 38.3 (17.4) | 0.654 |
| Hospital admissions during past year, mean (SD) | 0.76 (1.13) | 0.91 (1.04) | 0.63 (1.03) | 0.71 (1.06) | 0.517 |
| Hospital admissions during past year, n (%) | n = 41 | n = 23 | n = 76 | n = 140 | 0.530 |
| No previous admissions One admission Two admissions Three or more admissions |
24 (58.5) 8 (19.5) 6 (14.6) 3 (7.3) |
10 (43.5) 7 (30.4) 5 (21.7) 1 (4.3) |
46 (60.5) 20 (26.3) 6 (7.9) 4 (5.3) |
80 (57.1) 37 (26.4) 16 (11.4) 7 (5.0) |
|
| Oral corticosteroid use during the previous month to hospital admission, n (%) | 7 (17.1) |
4 (17.4) |
1 (1.3) |
12 (8.6) |
0.394 |
| Asthma Knowledge Test scorec, mean (SD) | 6.52 (1.81) |
6.71 (1.90) |
6.50 (1.60) |
6.53 (1.68) |
0.911 |
| Have you ever used a peak flow meter before? ‘yes’ n (%) | 0/41 (0.0) |
2/22 (9.1) |
1/76 (1.3) |
3/139 (2.2) |
0.052 |
| Do you have a written asthma action plan? ‘yes’ n (%) | 5/41 (14.7) |
2/23 (11.1) |
10/76 (14.9) |
17/140 (14.3) |
0.916 |
| ACT scoredd, mean (SD) | 10.3 (5.0) | 9.7 (5.0) | 10.0 (4.7) | 10.0 (4.8) | 0.863 |
| Asthma controld, n (%) Well controlled: Not-well-controlled: Poorly controlled |
2:5:34 (4.9:12.2:82.9) |
2:1:20 (8.7:4.3:87.0) |
3:6:67 (3.9:7.9:88.2) |
7:12:121 (5.0:8.6:86.4) |
0.730 |
| Asthma medications | |||||
| Reliever used during the past one month, n (%) | 15/41 (36.6) |
15/23 (65.2) |
66/76 (86.8) |
96/140 (68.6) |
<0.001 |
| Duration of controller use (years), mean (SD) | 11.5 (8.4) | 8.4 (6.6) | 12.4 (13.0) | 11.5 (11.0) | 0.370 |
| Controller medication, n (%) ICS; ICS + LABA (combination or separate) |
18/41:23/41 (43.9:56.1) |
9/23:14/23 (39.1:60.9) |
47/63:16/63 (74.6:25.4) |
74/127:53/127 (58.3:41.7) |
0.001 |
| Past inhaler technique education | |||||
| Why did you choose to use this type of inhaler? n (%) | 0.671 | ||||
| Specialist advice | 35/35 (100.0) | 18/18 (100.0) | 66/67 (98.5) | 119/120 (99.2) | |
| Family advice | 0/35 (0.0) | 0/35 (0.0) | 1/67 (1.5) | 1/120 (0.8) | |
| Have you ever been provided with information or advice about how to use your inhaler: ‘yes’ n (%) | 35/41 (85.3) | 18/23 (78.3) | 67/76 (88.2) | 120/140 (85.7) | |
| If yes, was this by: n (%) | n = 38 | n = 22 | n = 74 | n = 134 | |
| Regular doctor | 0 (0.0) | 1 (5.6) | 2 (3.0) | 3 (2.5) | 0.438 |
| Pharmacist | 2 (5.7) | 1 (5.6) | 1 (1.5) | 4 (3.3) | 0.450 |
| Specialist | 35 (100.0) | 17 (94.4) | 67 (100.0) | 119 (99.2) | 0.057 |
| Hospital clinic | 1 (2.9) | 2 (11.1) | 3 (4.5) | 6 (5.0) | 0.408 |
| A medical center | 0 (0.0) | 0 (0.0) | 1 (1.5) | 1 (0.8) | 0.671 |
| Other people | 0 (0.0) | 1 (5.6) | 0 (0.0) | 1 (0.8) | 0.057 |
| Product insert | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| If yes, what was the type of the counseling? n (%) | n = 35 | n = 18 | n = 67 | n = 120 | 0.181 |
| Verbal information | 1 (2.9) | 2 (11.1) | 7 (10.5) | 10 (8.3) | |
| Physical demonstration | 25 (71.4) | 15 (83.3) | 47 (70.1) | 87 (72.5) | |
| Written information | 0 (0.0) | 1 (5.6) | 1 (1.5) | 2 (1.7) | |
| Verbal information and physical demonstration | 9 (25.7) | 0 (0.0) | 12 (17.9) | 21 (17.5) | |
| If yes, when did you receive this information or advice? n (%) | n = 35 | n = 18 | n = 67 | n = 120 | 0.264 |
| When you first got your inhaler | 33 (94.2) | 15 (83.3) | 63 (94.0) | 111 (92.5)120 | |
| After you started using your inhaler | 0 (0.0) | 2 (11.1) | 3 (4.5) | 5 (4.2) | |
| At some other time | 1 (2.9) | 1 (5.6) | 0 (0.0) | 2 (1.7) | |
| After you requested some information on how to use your inhaler | 0 (0.0) | 0 (0.0) | 1 (1.5) | 1 (0.8) | |
| Can't recall | 1 (2.9) | 0 (0.0) | 0 (0.0) | 1 (0.8) | |
| Has anyone ever checked the way you use your inhaler? ‘yes’ n (%) | 14/33 (42.4) | 12/17 (70.6) | 33/66 (50.0) | 59/116 (50.9) | 0.165 |
| Have you received any information or advice about how to use your inhaler in the last 12 months? ‘yes’ n (%) | 5/34 (14.7) | 2/16 (12.5) | 10/65 (15.4) | 17/115 (14.8) | 0.958 |
| In your opinion, whose role is it to educate you on asthma and inhaler use: n (%) | n = 32 | n = 18 | n = 67 | n = 117 | 0.158 |
| Specialist | 19 (59.4) | 9 (50.0) | 48 (71.6) | 76 (65.0) | |
| Pharmacist | 2 (6.3) | 0 (0.0) | 3 (4.5) | 5 (4.3) | |
| Nurse | 2 (6.3) | 0 (0.0) | 3 (4.5) | 5 (4.3) | |
| Regular doctor | 1 (3.1) | 0 (0.0) | 0 (0.0) | 1 (0.85) | |
| Combinations of the above HCPs | 6 (18.8) | 7 (38.9) | 13 (19.4) | 26 (2.2) | |
| Other people | 2 (6.3) | 2 (11.1) | 0 (0.0) | 4 (3.4) | |
| Do you think that you use your inhaler correctly? ‘yes’ n (%) | 14/14 (100) | 10/12 (83.3) | 27/33 (81.8) | 51/59 (86.4) | 0.404 |
East Amman (lower socioeconomic areas); West Amman (higher socioeconomic areas); outside Amman (mixed socioeconomic areas).
(0.71JD = 1USD).
AKT (Asthma knowledge test) questionnaire (score out of 10, higher indicates better asthma knowledge).
ACT: Asthma Control Test (score 5–25, higher indicates better asthma symptom control in the previous 4 weeks. Well controlled asthma (ACT > 19); Not-well-controlled asthma (ACT 16 to 19); poorly controlled asthma ≤ 15). HCPs = Healthcare professionals.
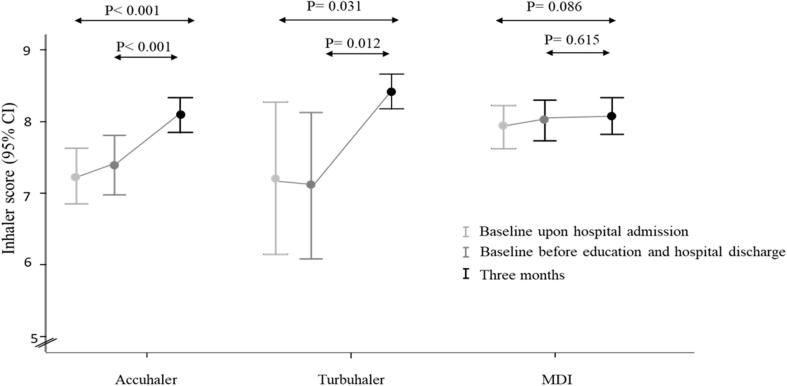
Fig. 2A.
Mean score of inhaler technique for Accuhaler (ACC, n = 41), Turbuhaler (TH, n = 23) and Metered Dose Inhaler (pMDI, n = 76) users at initial assessment, prior education assessment (before hospital discharge) and after 3 months. All patients were trained to correct technique (score 9/9) prior to discharge.
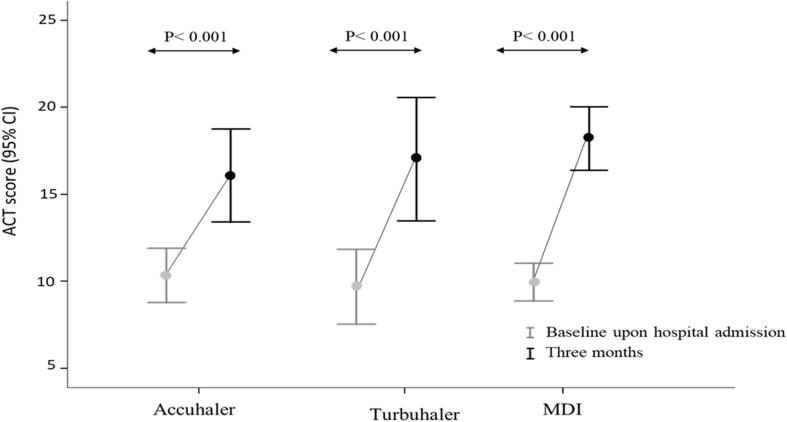
Mean ACT score was 10.0 (SD 4.8), with the majority of patients (121, 86.4%) having very-poorly-controlled asthma (ACT score 5–15), and 12 (8.6%) having not-well-controlled asthma (ACT score 16–19); 7 (5.0%) patients had scores of 20–25 consistent with well-controlled asthma over the previous 4 weeks, suggesting that their exacerbation was sudden-onset. No significant difference in ACT scores was found between the inhaler groups (Table 1, Fig. 2B).
Fig. 2B.
Asthma symptom control, assessed by Asthma Control Test (ACT) for patients using the Accuhaler (ACC, n = 41), Turbuhaler (TH, n = 23) and Metered Dose Inhaler (pMDI, n = 76).
Multiple regression analysis of baseline ACT (R2 = 0.165, p = 0.004) showed that patient income (B = 0.317, t = 3.119, p = 0.002) and AKT at baseline (B = 0.228, t = 2.261, p = 0.026) were the only significantly associated variables (see Online Appendix 3).
At admission, 58.3% of patients were taking ICS-only and 41.7% were taking ICS and LABA (combination or separately). Patients taking ICS alone were more likely to receive it by pMDI than by a dry powder inhaler (63.5% vs 30.2% respectively, p = 0.001). Two-thirds of patients (68.6%) reported using as-needed salbutamol in the previous month; reliever usage was consistent with poorly controlled asthma (mean 6.00 (SD 6.72) puffs/day).
Only 40.4% of patients agreed that they liked using their controller inhalers, and most (79.0%) reported also using herbal treatment to treat their asthma symptoms (59.4%) or to prevent asthma attacks (40.6%). The most common was chamomile, used by 53.6% of patients (Fig. 3). Many patients reported use of other treatments to manage their asthma symptoms (see Online Appendix 4), such as over the counter medications (57.1%) and antibiotics (47.9%).
Fig. 3.
Complementary herbal treatments used by the study patients (n = 140).
3.2. Past inhaler technique education
Most patients (120/140, 85.7%) reported being given information about how to use their inhaler, mostly (92.5%) when first prescribed, and only 14.8% during the previous 12 months. Most patients (65.0%) believed that it was the respiratory specialist’s role to educate them on asthma and inhaler technique and only 4.3% believed it was the pharmacist’s role (Table 1).
3.3. Baseline inhaler technique
Baseline inhaler technique assessment revealed a mean score of 7.54 (SD 1.52), with little difference between inhaler types (Table 2A, Fig. 2A). Few patients demonstrated correct technique (35.0%). However, significantly more ACC (95.1%) and TH (87.0%) users demonstrated correct essential technique compared to pMDI (67.1%) users (p < 0.001, Table 2A).
Table 2.
Inhaler technique: baseline assessment, inhaler technique education during hospitalization, and inhaler technique pre-discharge (before intervention) assessment.
| Variable | Accuhaler, n = 41 | Turbuhaler, n = 23 | pMDI, n = 76 | All, n = 140 | P value |
|---|---|---|---|---|---|
| A. Inhaler technique at baseline (shortly after admission to hospital) | |||||
| Inhaler technique score, mean (SD) | 7.29 (1.12) |
7.26 (2.03) |
7.76 (1.51) |
7.54 (1.52) |
0.174 |
| Correct inhaler technique, n (%) | 9/41 (22.0) |
8/23 (34.8) |
32/76 (42.1) |
49/140 (35.0) |
0.093 |
| Correct essential technique, n (%) | 39/41 (95.1) |
20/23 (87.0) |
51/76 (67.1) |
110/140 (78.6) |
<0.001 |
| B. Patient-reported inhaler technique education during hospitalization (from pre-discharge questionnaire) | |||||
| Were you told what each of your inhalers is used for? ‘yes’ n (%) | 14/30 (46.7) |
4/16 (25.0) |
25/58 (43.1) |
43/104 (41.3) |
0.335 |
| Were you told how often to take each of your inhalers? ‘yes’ n (%) | 30/30 (100.0) |
16/16 (100.0) |
56/58 (96.6) |
102/104 (98.1) |
0.445 |
| Were you told anything about the side effects? ‘yes’ n (%) | 9/30 (30.0) |
3/16 (18.8) |
20/58 (34.5) |
32/104 (30.8) |
0.480 |
| Were you told (verbally) how to use each of your inhalers? ‘yes’ n (%) | 15/30 (50.0) |
11/16 (68.8) |
30/58 (51.7) |
56/104 (53.8) |
0.424 |
| Were you given written information (product insert leaflet)? ‘yes’a n (%) | 4/20 (20.0) |
1/13 (7.7) |
4/36 (11.1) |
9/69 (13.0) |
0.522 |
| Were you shown how to use your inhaler? ‘yes’a | 17/19 (89.5) |
13/15 (86.7) |
28/32 (87.5) |
58/66 (87.8) |
0.245 |
| Who showed you how to use your inhaler?a n (%) | n = 17 | n = 13 | n = 30 | n = 60 | 0.559 |
| Specialist | 15/17 (88.2) |
12/13 (92.3) |
29/30 (96.7) |
56/60 (93.3) |
|
| Specialist and nurse | 2/17 (11.8) |
1/13 (7.7) |
1/30 (3.3) |
4/60 (6.7) |
|
| Were you observed while demonstrating the use of your inhaler? ‘yes’a n (%) | 17/18 (94.4) |
12/13 (92.3) |
28/30 (93.3) |
57/61 (93.4) |
0.972 |
| Were you assessed on your inhaler technique using your own inhaler? ‘yes’a n (%) | 15/17 (88.2) |
13/13 (100.0) |
30/30 (100.0) |
58/60 (96.7) |
0.073 |
| When were you shown how to use your inhaler?a n (%) | n = 17 | n = 13 | n = 30 | n = 60 | 0.603 |
| On admission | 6 (35.3) | 2 (15.4) | 7 (23.3) | 15 (25.0) | |
| During hospital stay | 10 (58.8) | 11 (84.6) | 22 (73.3) | 43 (71.7) | |
| On discharge | 1 (5.9) | 0 (0.0) | 1 (3.3) | 2 (3.3) | |
| C. Inhaler technique – pre-discharge, before intervention was delivered | |||||
| Inhaler technique score, mean (SD) | 7.47 (1.13) |
7.27 (2.05) |
7.99 (1.10) |
7.72 (1.34) |
0.036 |
| Correct inhaler technique, n (%) | 10/38 (26.3) |
8/22 (36.4) |
29/64 (45.3) |
47/124 (37.9) |
0.404 |
| Correct essential technique, n (%) | 35/38 (92.1) |
19/22 (86.4) |
60/71 (84.5) |
114/131 (87.0) |
0.528 |
Not all patients agreed to answer these questions; results are reported as n/N (%) where n is the number of patients who responded with ‘yes’, and N is the number of patients who answered the question.
3.4. Patient-reported inhaler technique education received during hospitalization
Patients spent an average of 9.57 days (SD 7.7) in hospital. At the pre-discharge assessment, some patients declined to answer questions about inhaler technique education provided to them during their hospitalization (Table 2B); of those who responded, the majority (98.1%) said that they had been informed about how often to use their inhalers, but only 43/104 (41.3%) said they were informed what each of their inhalers were used for. About half of patients (53.8%) reported that they were educated on correct inhaler use, and were observed while using their inhalers.
3.5. Inhaler technique assessment pre-discharge, before and after intervention
At the pre-discharge assessment prior to inhaler technique education, reassessment of patients’ inhaler technique revealed slightly improved inhaler technique results compared to baseline (Table 2C, Fig. 2A). The only significant improvement noted was the proportion of patients with pMDI correct essential technique (84.5% vs. 67.1%, p = 0.004).
After receiving inhaler technique training, and prior to discharge, all patients demonstrated correct technique (score 9/9, change in score from pre-education p < 0.001 for all).
3.6. Three month follow-up questionnaires
One hundred and twenty-five patients returned for follow-up (89.3%). Of these, 20 (16.0%) reported a change in medications, which involved addition (n = 3) or removal (n = 1) of LABA; switching from combination inhalers (ICS/LABA) to separate inhalers (n = 9), or vice versa (n = 5); or adding a short acting β2 agonist (n = 2).
Asthma knowledge scores had improved significantly for all patients at follow-up (7.79 (SD 2.18), p < 0.001), with no significant differences between the inhaler groups (ACC: 7.94 (SD 2.18); TH: 8.35 (SD 2.28); pMDI: 7.52 (SD 1.93), p = 0.262).
At follow-up, mean ACT score had increased by 7.54 (SD 8.18, p < 0.001), with no significant difference in increase between the inhaler groups (p = 0.326, Fig. 2B). Overall, at follow-up, 64/125 (51.2%) of patients now had well-controlled asthma; 12/125 (9.6%) not-well-controlled; but 49/125 (39.2%) still had very-poorly-controlled asthma (p < 0.001 for change from baseline), with no significant difference in change between the inhaler groups (p = 0.225). There were no significant differences in ACT or inhaler technique scores at follow-up between patients who did and did not have a medication change.
3.7. Inhaler technique scores at three month follow-up
At follow-up, 116/125 (93.0%) patients demonstrated their inhaler technique. Overall, there was a small but significant difference in inhaler technique scores compared with baseline (mean score 8.14 (SD 0.87), mean difference from baseline 0.53 (SD 1.23), p < 0.001), with a significant difference between change in score for ACC (mean difference 0.85 (SD 0.97), TH (1.21 (SD 2.25)), and pMDI (0.16 (SD 0.72)) users, p = 0.001.
No significant difference was found in the proportion of patients with correct technique at follow-up compared with baseline for ACC (27.3% vs. 22.0%, p = 0.375 for change), TH (47.4% vs. 34.8%, p = 0.774) or pMDI (45.3% vs. 42.1%, p = 1.000, McNemar test). The steps still most commonly incorrect at follow-up for ACC and TH users were “exhale to residual volume before inhalation” and “exhale away from the mouthpiece (before inhalation)” (ACC: 68.4% and 60.5%; TH: 59.1%, 50.0%, respectively). For the pMDI, incorrect steps included “exhale to residual volume before inhalation” (52.1%), “Hold inhaler upright” (21.1%) and “Remove mouthpiece cover and shake” (11.3%).
All ACC and pMDI users, and 94.7% of TH users, demonstrated correct essential technique at follow-up.
Multiple linear regression modelling indicated that higher AKT mean scores at follow-up was the only variable significantly associated (B = 0.319, t = 2.816, p = 0.006) with higher inhaler technique scores at follow-up (R2 = 0.102, p = 0.006).
Multiple linear regression modelling of ACT score at 3-month follow-up indicated that type of inhaler, lower baseline knowledge scores and higher follow-up knowledge scores were the variables significantly associated with higher ACT scores (R2 = 0.391, p < 0.001, Table 3 Model A); change in inhaler technique score over the study period was not a significant factor.
Table 3.
Summary of the regression model (n = 140) obtained for the dependent variable, Asthma Control Test score at 3-month follow-up (Model A) and change in Asthma Control Test score over study period (Model B).
| Model A. Variables | Beta | t | P value |
|---|---|---|---|
| Type of inhaler (ACC, TH and pMDI) | 0.198 | 2.013 | 0.048 |
| Age | −0.075 | −0.584 | 0.561 |
| Gender | 0.000 | 0.000 | 1.000 |
| Incomea | −0.101 | −0.813 | 0.419 |
| Smoking status | 0.005 | 0.038 | 0.970 |
| ACT at baselineb | 0.208 | 2.073 | 0.042 |
| AKT at baselinec | −0.565 | −4.683 | <0.001 |
| AKT at follow-upc | 0.528 | 4.600 | <0.001 |
| Duration of preventer use (years) | −0.135 | −1.305 | 0.196 |
| Patient education | 0.128 | 0.977 | 0.332 |
| Change in inhaler score over study period | 0.084 | 0.829 | 0.410 |
| Follow-up inhaler technique score | −0.061 | −0.619 | 0.538 |
| Model B. Variables | Beta | t | P value |
| Type of inhaler (ACC, TH and pMDI) | 0.287 | 2.384 | 0.020 |
| Age | −0.085 | −0.564 | 0.575 |
| Gender | −0.086 | −0.607 | 0.546 |
| Incomea | 0.119 | 0.805 | 0.424 |
| Smoking status | −0.088 | −0.605 | 0.548 |
| ACT at baselineb | −0.381 | −3.284 | 0.002 |
| AKT at baselinec | −0.377 | −2.709 | 0.009 |
| AKT at follow-upc | 0.290 | 2.049 | 0.045 |
| Duration of preventer use (years) | −0.142 | −1.196 | 0.237 |
| Patient education | −0.070 | −0.451 | 0.654 |
| Baseline inhaler technique score | −0.068 | −0.438 | 0.663 |
| Change in inhaler score over study period | 0.089 | 0.568 | 0.572 |
This table shows the output from a multivariable regression analysis in which ACT score at 3-month follow-up (overall fit of the model was R2 = 0.391, P < 0.001) and change in ACT score over study period (overall fit of the model was R2 = 0.377, P = 0.003) were the dependent variables. “Beta“ is the standardized regression coefficient.
Income (yearly income in Jordanian Dinar; 0.71JD = 1USD).
ACT: Asthma Control Test (score 5–25, higher indicates better asthma symptom control in the previous 4 weeks).
AKT (Asthma knowledge Test) questionnaire (score out of 10, higher indicates better asthma knowledge). Numbers in ‘bold’ indicate significant results.
Multiple linear regression modelling of ACT scores across the study period indicated that type of inhaler, lower baseline ACT scores, lower baseline knowledge scores and higher follow-up knowledge scores were the variables significantly associated with greater increase ACT score difference (R2 = 0.377, p = 0.003, Table 3 Model B); change in inhaler technique score over the study period was not a significant factor.
4. Discussion
This pre-post interventional study found that, among patients hospitalized for asthma, few had correct inhaler technique. Although many patients reported that they had received some inhaler technique training during their admission to the respiratory ward, inhaler technique was still not correct at a pre-discharge assessment. However, inhaler technique was significantly enhanced through a ‘Show-and-Tell’ educational intervention delivered by a clinical pharmacist, and small but significant improvements in inhaler technique were maintained at 3-months post-discharge compared with baseline. Findings at the 3-month follow-up confirm that poor asthma control is common among asthma patients with a recent hospitalization, independent of socioeconomic background and place of living (Global Initiative for Asthma (GINA) - Global strategy for asthma management and prevention report 2017).
In this population, assessed shortly after admission to hospital because of asthma, baseline inhaler technique scores were relatively high (mean score 7.54 out of 9), compared with baseline scores of 4.5–5.5 in our previous studies in community pharmacies (Basheti et al., 2008) and outpatient clinics (Basheti et al., 2017) in Australia and Jordan using the same checklists (Basheti et al., 2011). This suggests that incorrect inhaler technique was not the primary contributor to the present hospitalization; instead, with 42.9% of the patient having one or more hospital admissions in the previous year, higher inhaler technique scores may reflect greater contact with healthcare professionals than by those previously studied. The higher baseline inhaler technique scores also meant that there was limited opportunity to demonstrate any relationship between change in inhaler technique and change in asthma symptom control, due to a ceiling effect.
Considering previous findings, it was not surprising to find that patients’ previous main source of inhaler technique education was their specialist, with little role played by the pharmacist (Basheti et al., 2014b, Clarenbach et al., 2016). In addition, education was mostly delivered when the patients started using their inhalers, and, as also reported by ourselves and others (Basheti et al., 2005, Clarenbach et al., 2016), inhaler technique was generally not checked on a regular basis.
Many effective medications are available on the market to enable patients to better manage their asthma symptoms, however, the demonstrated current levels of asthma control fall short of the treatment goals idealized in many asthma treatment guidelines (Basheti et al., 2016). Many patients in this study reported use of rescue medications and rescue oral corticosteroids, as well as frequent hospitalizations. A recent European Consensus Statement made a call to action to seek solutions to incorrect inhaler use, with a highlight on the opportunity for educational interventions to reduce errors (Papi et al., 2011).
ACT was one of the validated tools used in the assessment of the intervention conducted in this study (Lababidi et al., 2008). At baseline, significant associations were found between lower ACT scores, lower income and lower asthma knowledge scores. Previous studies unveiled associations between uncontrolled asthma and poverty (Burney et al., 2015). Low socioeconomic status has been found to decrease self-efficacy, the confidence an individual has in their ability to control and manage their asthma (Ejebe et al., 2015). Association between Asthma knowledge scores and ACT scores was also revealed at follow-up. Such association was not shown in previous asthma outpatient studies (Basheti et al., 2016, Ozyigit et al., 2015). No former inpatient study has stated this association.
Overall, ACT scores improved substantially for all inhaler groups, with mean improvement between baseline and follow-up more than twice the minimal important difference of 3.0 (Schatz et al., 2009). However, the baseline ACT likely reflected the exacerbation that resulted in the patient’s hospitalization. Improving patients’ inhaler technique skills has been shown previously to reduce lung function variability and improve asthma control, asthma-related quality of life and perceived asthma control (Basheti et al., 2008, Basheti et al., 2007, Giraud et al., 2011), however, no association between change in inhaler technique and change in ACT scores was evident in this study. Significant improvements were also seen in patients’ asthma knowledge (Kritikos et al., 2005), which was significantly associated with ACT improvement. One factor may have been that many patients took the opportunity to ask the researcher questions regarding their asthma treatment.
Complementary treatment for asthma, mainly with chamomile, was highly prevalent among the study patients, as in general in Jordan (Issa and Basheti, 2016). By the inclusion criteria, patients were also taking an ICS treatment (Philp et al., 2012), but only 40% of patients said they liked using their inhaler; corticosteroid phobia (Skoner et al., 2008) and incorrect beliefs (Price et al., 2013) emerged as important creasons through anecdotal comments. Overuse and misuse of OTC medications and antibiotics were also issues of concern.
Strengths of the study were the use of standardized tools, including inhaler technique checklists and ACT and AKT, the assessment of inhaler technique shortly after admission as well as pre-discharge, and follow-up after 3 months. Limitations include the unusually high baseline inhaler scores, and different sample sizes recruited for the different inhalers, suggesting that pMDIs were more familiar to local prescribers. Patient-reported data on inhaler training during hospitalization may have been subject to social desirability bias; indeed, many patients declined to answer these questions. Due to ethical considerations for hospitalized patients, no control group was enrolled; hence, improvements seen at follow-up might be due to factors other than the inhaler intervention, including recovery from the index exacerbation. Nevertheless, the intervention delivered mimics a real life situation, where the pharmacist in the hospital would see the patient prior to discharge and deliver any needed education before they went home.
5. Conclusions
The majority of patients hospitalized for asthma in Jordan have incorrect inhaler technique, poor asthma control and low asthma knowledge. Many patients turn to using herbal treatments, OTC drugs and antibiotics to manage their asthma. Few patients considered pharmacists to have a role in inhaler training, but we found that an intervention on inhaler technique delivered by a clinical pharmacist prior to discharge was feasible, and was successful in significantly maintaining improved inhaler technique at three months following discharge. Further studies are needed to confirm the results obtained in other populations and different geographical areas in Jordan.
6. Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
Acknowledgments
The authors are grateful to the Applied Science Private University Amman, Jordan, for the full financial support granted to this research project. The authors wish to thank the healthcare professionals and patients who participated in this study, and Dr Mohammad Basheti for his valuable contribution.
Funding
The authors are grateful to the Applied Science Private University, Amman, Jordan, for the full financial support granted to this research project.
Conflict of interest
HKR has provided independent medical education at symposia funded by AstraZeneca, GlaxoSmithKline, Mundipharma, Novartis and Teva; has participated in Advisory Boards for AstraZeneca, GlaxoSmithKline, Novartis and Boehringer Ingelheim; has provided consultancy for AstraZeneca and GlaxoSmithKline; is participating in a joint data monitoring committee for studies funded by AstraZeneca, GlaxoSmithKline, Merck and Novartis; and has received unconditional grants from AstraZeneca and GlaxoSmithKline for investigator-sponsored research.
For the other authors, no financial or other potential conflicts of interest exist. Placebo inhalers were provided by AstraZeneca Pharmaceuticals (Wilmington, Delaware; Amman, Jordan) and GlaxoSmithKline (Philadelphia, Pennsylvania; Amman, Jordan).
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Iman A. Basheti, Email: dr_iman@asu.edu.jo.
Helen K. Reddel, Email: helen.reddel@sydney.edu.au.
References
- Abu-Ekteish F., Otoom S., Shehabi I. Prevalence of asthma in Jordan: comparison between Bedouins and urban schoolchildren using the International Study of Asthma and Allergies in Childhood phase III protocol. Allergy Asthma Proc. 2009;30:181–185. doi: 10.2500/aap.2009.30.3208. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Armour C.L., Bosnic-Anticevich S.Z., Reddel H.K. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ. Couns. 2008;72:26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Armour C.L., Reddel H.K., Bosnic-Anticevich S.Z. Long-term maintenance of pharmacists' inhaler technique demonstration skills. Am. J. Pharm. Educ. 2009;73:32. doi: 10.5688/aj730232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basheti I.A., Bosnic-Anticevich S.Z., Armour C.L., Reddel H.K. Checklists for powder inhaler technique: A review and recommendations. Respir. Care. 2014;59:1140–1154. doi: 10.4187/respcare.02342. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Obeidat N.M., Ammari W.G., Reddel H.K. Associations between inhaler technique and asthma control among asthma patients using pressurised MDIs and DPIs. Int. J. Tuberc. Lung Dis. 2016;20:689–695. doi: 10.5588/ijtld.15.0557. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Obeidat N.M., Reddel H.K. Effect of novel inhaler technique reminder labels on the retention of inhaler technique skills in asthma: a single-blind randomized controlled trial. NPJ Prim. Care Respir. Med. 2017;27:9. doi: 10.1038/s41533-017-0011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basheti I.A., Qunaibi E., Bosnic-Anticevich S.Z., Armour C.L., Khater S., Omar M., Reddel H.K. User error with Diskus and Turbuhaler by asthma patients and pharmacists in Jordan and Australia. Respir. Care. 2011;56:1916–1923. doi: 10.4187/respcare.01205. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Qunaibi E.A., Hamadi S.A., Reddel H.K. Inhaler technique training and health-care professionals: effective long-term solution for a current problem. Respir. Care. 2014;59:1716–1725. doi: 10.4187/respcare.02671. [DOI] [PubMed] [Google Scholar]
- Basheti I.A., Reddel H.K., Armour C.L., Bosnic-Anticevich S.Z. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir. Care. 2005;50:617–623. [PubMed] [Google Scholar]
- Basheti I.A., Reddel H.K., Armour C.L., Bosnic-Anticevich S.Z. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J. Allergy Clin. Immunol. 2007;119:1537–1538. doi: 10.1016/j.jaci.2007.02.037. [DOI] [PubMed] [Google Scholar]
- Bosnic-Anticevich S.Z., Sinha H., So S., Reddel H.K. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47:251–256. doi: 10.3109/02770900903580843. [DOI] [PubMed] [Google Scholar]
- Burney P., Jarvis D., Perez-Padilla R. The global burden of chronic respiratory disease in adults. Int. J. Tuberc. Lung Dis. 2015;19:10–20. doi: 10.5588/ijtld.14.0446. [DOI] [PubMed] [Google Scholar]
- Clarenbach C.F., Nicod L.P., Kohler M. Real-world asthma management with inhaler devices in Switzerland-results of the asthma survey. J. Thorac. Dis. 2016;8:3096–3104. doi: 10.21037/jtd.2016.11.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dal Negro R.W., Distante C., Bonadiman L., Turco P., Iannazzo S. Cost of persistent asthma in Italy. Multidiscip. Respir. Med. 2016;11:44. doi: 10.1186/s40248-016-0080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejebe I.H., Jacobs E.A., Wisk L.E. Persistent differences in asthma self-efficacy by race, ethnicity, and income in adults with asthma. J. Asthma. 2015;52:105–113. doi: 10.3109/02770903.2014.947429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraud V., Allaert F.A., Roche N. Inhaler technique and asthma: feasibility and acceptability of training by pharmacists. Respir. Med. 2011;105:1815–1822. doi: 10.1016/j.rmed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Giraud V., Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur. Respir. J. 2002;19:246–251. doi: 10.1183/09031936.02.00218402. [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma (GINA) - Global strategy for asthma management and prevention report 2017. Available online at: http://www.ginasthma.org (Accessed September 2017).
- Guilbert T.W., Garris C., Jhingran P., Bonafede M., Tomaszewski K.J., Bonus T., Hahn R.M., Schatz M. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J. Asthma. 2011;48:126–132. doi: 10.3109/02770903.2010.535879. [DOI] [PubMed] [Google Scholar]
- Hasegawa K., Bittner J.C., Nonas S.A., Stoll S.J., Watase T., Gabriel S., Herrera V., Camargo C.A., Jr. Children and adults with frequent hospitalizations for asthma exacerbation, 2012-2013: A multicenter observational study. J. Allergy Clin. Immunol. Pract. 2015;3:751–758 e751. doi: 10.1016/j.jaip.2015.05.003. [DOI] [PubMed] [Google Scholar]
- Issa R.A., Basheti I.A. Herbal Products Use Among Chronic Patients and its Impact on Treatments Safety and Efficacy: A Clinical Survey in the Jordanian Field. Trends Med. Res. 2016;12:32–44. [Google Scholar]
- Kritikos V., Krass I., Chan H.S., Bosnic-Anticevich S.Z. The validity and reliability of two asthma knowledge questionnaires. J Asthma. 2005;42:795–801. doi: 10.1080/02770900500308627. [DOI] [PubMed] [Google Scholar]
- Lababidi H., Hijaoui A., Zarzour M. Validation of the Arabic version of the asthma control test. Ann. Thorac. Med. 2008;3:44–47. doi: 10.4103/1817-1737.39635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melani A.S., Bonavia M., Cilenti V., Cinti C., Lodi M., Martucci P., Serra M., Scichilone N., Sestini P., Aliani M., Neri M. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir. Med. 2011;105:930–938. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Ozturk A.B., Ozyigit Pur L., Kostek O., Keskin H. Association between asthma self-management knowledge and asthma control in the elderly. Ann. Allergy Asthma Immunol. 2015;114:480–484. doi: 10.1016/j.anai.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Papi A., Haughney J., Virchow J.C., Roche N., Palkonen S., Price D. Inhaler devices for asthma: a call for action in a neglected field. Eur. Respir. J. 2011;37:982–985. doi: 10.1183/09031936.00150910. [DOI] [PubMed] [Google Scholar]
- Philp J.C., Maselli J., Pachter L.M., Cabana M.D. Complementary and alternative medicine use and adherence with pediatric asthma treatment. Pediatrics. 2012;129:e1148–e1154. doi: 10.1542/peds.2011-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press V.G., Arora V.M., Shah L.M., Lewis S.L., Ivy K., Charbeneau J., Badlani S., Nareckas E., Mazurek A., Krishnan J.A. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J. Gen. Intern. Med. 2011;26:635–642. doi: 10.1007/s11606-010-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price D., Bosnic-Anticevich S., Briggs A., Chrystyn H., Rand C., Scheuch G., Bousquet J. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respir. Med. 2013;107:37–46. doi: 10.1016/j.rmed.2012.09.017. [DOI] [PubMed] [Google Scholar]
- Schatz M., Kosinski M., Yarlas A.S., Hanlon J., Watson M.E., Jhingran P. The minimally important difference of the Asthma Control Test. J. Allergy Clin. Immunol. 2009;124(719–723) doi: 10.1016/j.jaci.2009.06.053. [DOI] [PubMed] [Google Scholar]
- Schatz M., Sorkness C.A., Li J.T., Marcus P., Murray J.J., Nathan R.A., Kosinski M., Pendergraft T.B., Jhingran P. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J. Allergy Clin. Immunol. 2006;117:549–556. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Skoner J.D., Schaffner T.J., Schad C.A., Kwon A.Y., Skoner D.P. Addressing steroid phobia: improving the risk-benefit ratio with new agents. Allergy Asthma Proc. 2008;29:358–364. doi: 10.2500/aap.2008.29.3132. [DOI] [PubMed] [Google Scholar]
- The British Guideline on the Management of Asthma. (Available online at: https://www.brit-thoracic.org.uk/standards-of-care/guidelines/. Accessed September 2017).
- van der Palen J., Klein J.J., Schildkamp A.M. Comparison of a new multidose powder inhaler (Diskus/Accuhaler) and the Turbuhaler regarding preference and ease of use. J. Asthma. 1998;35:147–152. doi: 10.3109/02770909809068202. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.