Abstract
Objective. In China, the method of clearing heat and removing dampness medicine of Chinese traditional medicine has been widely used on gout. However, the clinical effects are various and not summarized systematically. Methods. In this study, a large number of randomized controlled clinical trials were reviewed and analyzed and the clinical efficacy and adverse reactions of traditional Chinese medicine with clearing heat and removing dampness effects for the treatment of gout were systematically evaluated. A comprehensive search of databases including pubMed, China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database, Wanfang Data, and SinoMed was performed. Results. There are 69 randomized controlled trials with 5915 sample sizes meeting the criteria in the study. The results of the meta-analysis indicate that the effects of clearing heat and removing dampness medicine were slightly better than western medicine in the treatment of gout based on the following parameters: serum uric acid (standardized mean difference (SMD):-62.14, 95% confidence interval (CI): -78.12 to-46.15), C reactive protein (SMD: -4.21, 95% CI: -6.19 to -2.23), erythrocyte sedimentation rate (SMD: -6.23, 95% CI: -8.39 to-4.06), and overall clinical response (relative risk (RR): 1.11, 95% CI: 1.08 to 1.15) and, in the profile of adverse drug reactions, the clearing heat and removing dampness medicine showed less adverse reactions than traditional Western medicine (RR: 0.18, 95% CI: 0.10 to 0.32). Conclusions. Through a systemic evaluation of the clinical efficacy of the clearing heat and removing dampness medicine of traditional Chinese medicine and western medicine on gout, the clearing heat and removing dampness medicine and western medicine possessed similar clinical efficacy, but traditional Chinese medicine treatments are superior to western medicine in controlling adverse reactions.
1. Introduction
With the change of lifestyle and dietary factor, gout has been the global burden [1], mainly because of its high incidence in not only elderly people but also younger people [2]. Gout is a crystal deposition disease which results from local uric acid supersaturation as a consequence of systemic uric acid overload, leading to the formation of monosodium urate (MSU) crystals in the around joints, which caused severe pain and had a strong impact on quality of life. The most common clinical manifestation of gout is recurrent attacks of acute arthritis involving one joint at a time [3]; in some cases, joint injury and renal insufficiency will even occur in patient with gout.
In clinical, western medicines including corticosteroids, allopurinol, and NSAIDs are widely used in treating acute attack of gout [4]. But they all possessed various degrees of side-effect such as gastrointestinal tract reaction, tissue and organ damage, and other adverse reactions. In recent years, IL-1R antagonists appeared and was used for the patients who have contraindications to colchicine and nonsteroidal anti-inflammatory drugs and hormones (oral or injection) [5]. However, the mechanism was unclear and the side effect was also not mentioned. Traditional Chinese medicine (TCM) has been used for preventing and treating gout with unique clinical effects since 200AD in China [6]. Clearing heat and removing dampness is a special medical method for treating patients with gout based on the theory of Chinese traditional medicine, which indicated that the pathogenesis of gout disease is closely related to the heat evil and wetness evil attacking [7]. Many randomized controlled trials (RCTs) in clinical published have selected heat and removing dampness method of Traditional Chinese Medicine to treat gout, and most have clearly shown that Traditional Chinese Medicine have achieved positive results in treating gout.
Meta-analysis, which is the statistical synthesis of relative literature to develop evidence-based conclusions, is able to systematically evaluate and summarize the consistency of multiple studies on the same topic [8]. To the best of our knowledge, there is no meta-analysis of the treatment of gout with heat and removing dampness method of Traditional Chinese Medicine. We need to have a clearer understanding of the application of heat and removing dampness method of Traditional Chinese Medicine in the treatment of gout and to evaluate its effectiveness of in the treatment of gout. The efficacy and side effect of clearing heat and removing dampness medicine and western medicine in the treatment of gout were compared using meta-analysis method in this study. The results will lay a foundation for the treatment of gout with clearing heat and removing dampness methods.
2. Methods
2.1. Experimental Design
The clinical designs in all reports selected in this study were clinical randomized controlled trials (RCTs). Based on the intervention method, the trials were divided into experimental and control groups, oral administration of Chinese herbal decoction and disposition with other methods of traditional Chinese medicine were included in the experimental group, while oral administration of western medicine was regarded as the control group. The publication time was restricted to the period from January 2000 to May 2017, and the journals' languages were restricted in Chinese and English.
2.2. Subjects
According to the diagnostic criteria created by the 1977 American College of Rheumatology classification criteria and Guidelines for the diagnosis and treatment of primary gout established by the Chinese Rheumatology Association, etc., all subjects selected in the study were diagnosed with primary gout in the phase of acute arthritis. Subjects with other comorbidities were excluded.
2.3. Database Search Strategy
The titles of “Clearing heat and removing dampness” and “hyperuricemia” or “Clearing heat and removing dampness” and “gout” were searched from the databases including PubMed, China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database, Wanfang Data, and China Biology Medicine disc during the period from January 2000 to May 2017.
2.4. Data Analysis
Three investigators who participated in the study extracted data from all publications selected in this study. The information of the first author, the year of publication, the number of cases in the experimental group and the control group, the intervention method, the end point evaluation index, and the Jadad score were included. One investigator did the first data extraction, the second investigator reviewed the literatures and confirmed the results afterwards, and the third investigator participated in the discussion when the disagreement occurred and reached a consensus with the other two finally.
2.5. Endpoint Indicators
The evaluations of effective and ineffective were reached artificially based on the indicators of measurement data, such as Serum uric acid (SUA), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). And the evaluations of SUA, CRP, and ESR were collected after the period of gout attack. The reducing of blood uric acid, ESR, and CRP and the relieving of the clinical symptoms were regarded as effective. On the contrary, it was ineffective. The respective measurement data of blood uric acid, ESR, and CRP were also regarded as the primary indicators.
2.6. Assessment of Methodological Quality
Assessment of methodological quality is based on the validated Jadad scale by two reviewers (XN and CH) and the Jadad scale has three scoring points. The first is if the study was described as randomized, and with detailed descriptions. The second is if the blind method was adopted in the study and with detailed descriptions. And the third is if there was a description of withdrawals and dropouts. A paper reporting could therefore receive a Jadad score from 0 to 7, in which the scores with 1-3 and 4-7 were considered as low and high quality, respectively.
2.7. Statistical Methods
The measurement data were evaluated using the mean difference (MD) and 95% confidence interval (CI), or the relative risk (RR) and 95% confidence interval. If the heterogeneity of the study was within the acceptable range (I2≤ 50%), the fixed effect model was used. Otherwise, the random effects model was used. The collected data in clinical research were analyzed by RevMan 5.0 software.
3. Results
3.1. Selection of Studies
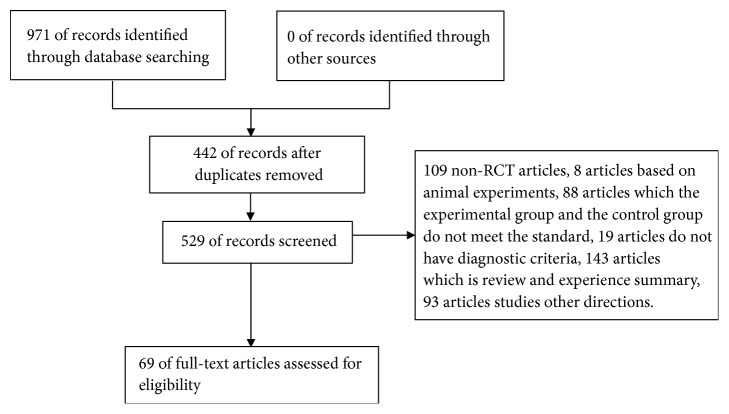
971 articles about the treatment of gout using clearing heat and removing dampness medicine of Chinese traditional medicine were retrieved from five electronic databases, in which 442 duplicated publications articles were excluded. Then two reviewers independently screened the full texts of the remaining 529 articles. 109 non-RCT articles, 8 articles based on animal experiments, 88 articles had inconformity to inclusion standard but included the experimental group or the control group, 19 articles without diagnostic criteria, 143 articles about review and experience summary, and 93 articles about other directions. Finally, 69 articles were included in this study [9–77] (Figure 1). The characteristics of these studies were shown in Tables 1 and 2.
Figure 1.
Flow diagram of study selection.
Table 1.
Characteristics of included studies.
| Author, year | Sample size | Age | Intervention methods | Duration treatment | Effective number | Jadad scale | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| EG | CG | EG | CG | EG | CG | EG | CG | EG | CG | ||
| Yan Zhang, 2016 |
27 | 25 | 47.04±12.92 | 47.72±8.69 | Qingrelishi side | Low purine diet + meloxicam | 14 | 14 | 25 | 23 | 3 |
| Fang Zuo, 2001 |
58 | 30 | N/A | N/A | BaiHuGuiZhi Decoction+ Simiao Powder |
allopurinol | 14 | 14 | 52 | 22 | 1 |
| Yihui Yan, 2006 |
36 | 36 | N/A | N/A | BiNing Decoction | allopurinol | 28 | 28 | 33 | 28 | 1 |
| Xubin Zhao, 2014 |
25 | 25 | N/A | N/A | Blood-letting puncture and cupping+ Microwave therapy | Colchicine +Diclofenac Sodium Sustained Release Capsules |
3~7 | 1~7 | 25 | 23 | 1 |
| Li Cheng, 2009 |
32 | 30 | N/A | N/A | Danghuiniantong Decoction |
Meloxicam | 7 | 7 | 31 | 29 | 1 |
| Guicai Sun, 2007 |
65 | 65 | N/A | N/A | Compound xiqiancao capsule | Voltaren+ allopurinol | 21 | 21 | 58 | 54 | 1 |
| Yuhong Zhang, 2003 |
45 | 43 | N/A | N/A | Modified Sanmiao Powder |
Colchicine | 21 | 21 | 39 | 42 | 1 |
| Shengyun Wu, 2017 |
34 | 34 | 35.9±6.1 | 35.9±6.1 | Simiao Powder+ Xinhuang Tablet(external) |
Colchicine | 14 | 14 | 33 | 18 | 1 |
| Qingsheng He, 2016 |
50 | 50 | 34.5±4.7 | 32.7±3.2 | Modified Simiao Powder+ Xinhuang Tablet(external) |
Colchicine | 7 | 7 | 49 | 44 | 3 |
| Lixin Wang, 2001 |
69 | 35 | N/A | N/A | Modified Simiao pill | Colchicine | N/A | N/A | 67 | 33 | 1 |
| Zhonghua Yang, 2007 |
60 | 30 | N/A | N/A | Jianpi qingrelishi Tongluo Decoction |
Colchicine | 15 | 15 | 55 | 27 | 1 |
| Wenping Cao, 2008 |
44 | 43 | N/A | N/A | JunHu analgesic powder(external)+ acupuncture treatment |
colchicine | 3 | 3 | 44 | 38 | 1 |
| Yanhong Zou, 2010 |
40 | 40 | N/A | N/A | Lizhuodingtong decoction | Nimesulide | 10 | 10 | 34 | 32 | 1 |
| Jincheng Cai, 2006 |
54 | 46 | N/A | N/A | Niantongxiaofeng prescription | colchicine | 15 | 15 | 52 | 43 | 1 |
| Wei Li, 2016 |
58 | 58 | N/A | N/A | Qingrechushi prescription | Etoricoxib Tablets | 14 | 14 | N/A | N/A | 3 |
| Yingxu Wang, 2014 |
33 | 31 | 46.97±9.65 | 41.16±9.72 | Discriminate treatment of Chinese medicine by clearing away heat and resolving turbid | Diclofenac Sodium Sustained Release Tablets+ Benzbromarone Tablets |
31 | 31 | 31 | 27 | 1 |
| Wei Liu, 2016 | 36 | 35 | 46.73±16.25 | 47.06±15.82 | Compound Chinese medicine decoction of Clearing heat-toxin and eliminating dampness method | Diclofenac Sodium Sustained Release Tablets |
14 | 14 | 30 | 29 | 3 |
| Feng Yue, 2005 |
30 | 30 | N/A | N/A | Clearing heat-toxin and eliminating dampness method+ Gold paste(external) | colchicine | 7 | 7 | 30 | 30 | 1 |
| Yanming Ren, 2007 |
60 | 30 | N/A | N/A | Acid fat clear capsule | colchicine | 7 | 7 | 52 | 27 | 1 |
| Huilian Wang, 2012 |
40 | 40 | 48.4±12.8 | 49.1±13.1 | Gouty granule | Nimesulide | 10 | 10 | 34 | 33 | 1 |
| Wei Jin, 2013 |
32 | 32 | C | N/A | Self-prepared gout recipe+ Jiawei Jinhuang powder | colchicine | 7 | 7 | 30 | 24 | 1 |
| Hong Tu, 2015 |
30 | 30 | 44.9±9.1 | 45.1±8.1 | Gout clear granules | Diclofenac Sodium Sustained Release Tablets | 7 | 7 | 29 | 24 | 1 |
| Binchu Wang, 2000 |
52 | 38 | N/A | N/A | Gout decoction | Ibuprofen+ Probenecid52 |
10 | 10 | 49 | 33 | 1 |
| Haifeng Li, 2012 |
73 | 80 | 45.6±10.1 | 47.2±12.4 | Xuanbi decoction | allopurinol | 30 | 30 | 67 | 69 | 1 |
| Hongtao Yan, 2006 |
20 | 20 | N/A | N/A | Xuanbi decoction | Indomethacin | 7 | 7 | 18 | 16 | 3 |
| Weigang Zeng, 2010 |
55 | 50 | N/A | N/A | Yushantongfeng decoction 2 | allopurinol | 7 | 7 | 54 | 32 | 1 |
| Weigang Zeng, 2007 |
120 | 116 | N/A | N/A | Yushantongfeng decoction | colchicine | N/A | N/A | 118 | 108 | 1 |
| Jiang Wu, 2015 |
36 | 36 | 51.34±6.28 | 52.46±7.4 | Acupuncture+Sanren decoction and Sijunzi decoction | Diclofenac Sodium Sustained Release Tablets | 7 | 7 | 33 | 30 | 1 |
| Jing Chen, 2017 |
61 | 55 | 52.1±1.2 | 51.5±1.4 | Chinese medicine and acupuncture | Colchicine+ allopurinol |
7 | 7 | 58 | 47 | 1 |
| Minghai Zhou, 2014 |
20 | 20 | N/A | N/A | Simiao powder and acupuncture | Ibuprofen Sustained-release Capsules | 7 | 7 | 19 | 15 | 1 |
| Guangheng Cui, 2011 |
60 | 60 | N/A | N/A | Hoveniaacerbalindl Tongfeng Decoction |
Meloxicam | 7 | 7 | 55 | 56 | 1 |
| Yangang Wang, 2005 |
35 | 35 | 45.0±6.5 | 46.0±5.7 | Compound decoction of Chinese herbal medicine | Colchicine+ allopurinol | 7 | 7 | N/A | N/A | 1 |
| Hai Lu, 2013 |
30 | 30 | N/A | N/A | Simiao pill and Gouty ointment | Allopurinol+ Sodium Bicarbonate Tablets(oral)+ Qingpeng Paste(external) |
7 | 7 | 29 | 25 | 2 |
| Bo Duan, 2016 |
54 | 54 | 40.26±10.98 | 42.31±11.77 | Oral administration of Chinese medicine decoction+Rebiqing granules(oral)+Chinese medicine(external) | Colchicine Tablets | 7 | 7 | 47 | 46 | 2 |
| Guoying Han, 2010 |
42 | 39 | N/A | N/A | Rabdosia rubescens, coix seed, Poria cocos, Shi Wei, Rhizoma Atractylodis, Cortex Phellodendri, Achyranthes bidentata, rhubarb, Eupatorium adenophorum | Allopurino+Celecoxib | 31 | 31 | 39 | 29 | 1 |
| Min Dai, 2015 |
39 | 39 | 35±2.5 | 35±2.5 | Atractylodes rhizome, Achyranthes bidentata, Smilax glabra, Cortex Phellodendri, honeysuckle vine, liquorice, 2corydalis tuber, astragalus root and coix seed | Diclofenac Sodium Sustained Release Tablets | 14 | 14 | 36 | 29 | 1 |
| Xiaohong He, 2008 |
28 | 26 | 42.5±7.7 | 46±11.8 | Simiao powder+Sihuang powder | Colchicine | 3 | 3 | 27 | 20 | 1 |
| Xiaoxia Wang, 2010 |
30 | 30 | 48.5±15.5 | 49.1±13.7 | Self-made prescription: Mountain arrowhead, clematis, peach, Atractylodes, Poria, Alisma, Adenophora, Polygonum cuspidatum, rice, Bixie | Colchicine | 10 | 10 | 28 | 29 | 1 |
| Huijuan Yao, 2010 |
56 | 54 | N/A | N/A | Modified Guizhishaoyaozhimu decoction |
Colchicine | 10 | 10 | 51 | 52 | 1 |
| Lei Zhang, 2016 |
37 | 37 | 44.43±11.29 | 45.02±12.1 | Oral administration of Bixie decoction | Diclofenac Sodium Sustained Release Tablets | 7 | 7 | 33 | 31 | 1 |
| Bo Shi, 2010 |
45 | 40 | 49±16 | 48±14 | Clearing heat and dmp elimination tongluo +Relieving stasis and pain |
Colchicine | 10 | 10 | 38 | 25 | 1 |
| Liping Yan, 2012 |
38 | 31 | N/A | N/A | Clearing heat and dmp elimination prescription | Colchicine | 7 | 7 | 35 | 23 | 1 |
| Yulei Wu, 2015 |
38 | 38 | N/A | N/A | Clearing heat and removing dampness and activating blood circulation method | Sodium Bicarbonate Tablets+ Diclofenac Sodium Sustained Release Tablets | N/A | N/A | 38 | 32 | 1 |
| Yueqi Wang, 2013 |
32 | 32 | N/A | N/A | Chinese medicine of Clearing heat and removing dampness and activating blood circulation method | Diclofenac acid enteric coated tablets | 7 | 7 | 30 | 29 | 1 |
| Rong Li, 2014 |
75 | 75 | 50.24±12.37 | 49.15±13.06 | Bixieshenshi decoction and Taohongsiwu decoction | Celecoxib+ Sodium Bicarbonate Tablets | 10 | 10 | 69 | 62 | 1 |
| Shanshan Yu, 2008 |
40 | 40 | 48.2±8.6 | 46±9.7 | Dampness detoxification method | Nimesulide tablets | N/A | N/A | 38 | 34 | 1 |
| Weidong Qian, 2007 |
60 | 40 | N/A | N/A | Xitong Granule | Colchicine | 7 | 7 | 53 | 34 | 1 |
| Zheng Huang, 2013 |
32 | 30 | N/A | N/A | Qingrelishi Tongluo Decoction |
Nimesulide tablets | 10 | 10 | 28 | 27 | 1 |
| Chongyu Tan, 2013 |
52 | 46 | N/A | N/A | Self-made Clearing heat and dmp elimination tongluo prescription | Colchicine+ Fenbid | 7 | 7 | 48 | 34 | 2 |
| Chun Kang, 2012 |
30 | 30 | 70.2±5.3 | 69.9±6.1 | Self-made Clearing heat and dmp elimination tongluo decoction | Ibuprofen Sustained-release Capsules+ Sodium Bicarbonate Tablets |
7 | 7 | 28 | 24 | 2 |
| Xiaowu Fan, 2013 |
50 | 48 | N/A | N/A | Clearing heat and dmp elimination tongluo decoction | Fenbid | 7 | 7 | 48 | 38 | 2 |
| Jianchong Shen, 2014 |
61 | 61 | 45.78±7.45 | 46.47±8.35 | Laoshitongfeng prescription+acupuncture | Colchicine+ Sodium Bicarbonate Tablets | 7 | 7 | 57 | 49 | 1 |
| Guiqiong Huang, 2016 |
60 | 60 | 53.82±10.95 | 54.05±12.31 | Clearing heat and dmp elimination tongluo prescription | Colchicine | 7 | 7 | 55 | 38 | 1 |
| Xin Ouyang, 2004 |
30 | 30 | 57.77±6.62 | 56.37±6.74 | Bixiehuadu decoction | Butazolidin | 14 | 14 | 28 | 25 | 1 |
| Zhimin Qi, 2016 |
105 | 105 | 45.3±9.2 | 44.1±9.6 | Qingrelishi Zhuyu Decoction |
Colchicine+ Dexketoprofen Trometamol Tablets |
7 | 7 | 101 | 93 | 2 |
| Yaping Chen, 2014 |
45 | 43 | N/A | N/A | Clearing heat and dredging collaterals to clear turbid decoction | Diclofenac Sodium Sustained Release Tablets | 14 | 14 | 40 | 37 | 1 |
| Demei Li, 2012 |
40 | 40 | N/A | N/A | Clearing heat and dampness, blood stasis, relieving pain Tongluo Decoction; Qingre Tongluo releasing pain prescription | Colchicine+ Celecoxib Capsules+ Votalin(external) | 7 | 7 | 38 | 34 | 1 |
| Yanzhi Lin, 2009 |
30 | 30 | 53.55±10.67 | 55.73±11.92 | Self-made Sanjin decoction and Sanmiao powder | Colchicine+ allopurinol |
30 | 30 | 28 | 22 | 2 |
| Dehe Li, 2007 |
40 | 36 | 44.3±5.2 | 43.1±4.5 | Shandayanhesimiao decoction | Colchicine | 14 | 14 | 36 | 26 | 1 |
| Jun Hao, 2014 |
30 | 30 | 46±8.03 | 45.16±7.97 | Gout mixture | Colchicine | 15 | 15 | 29 | 23 | 1 |
| Chongqing Yang, 2006 |
30 | 30 | N/A | N/A | Gout prescription | Votalin | 7 | 7 | 27 | 28 | 3 |
| Lin Wang, 2011 |
29 | 29 | N/A | N/A | Tongbi prescription | Diclofenac Sodium Sustained Release Tablets | 7 | 7 | 26 | 27 | 4 |
| Ayijiaman, 2012 |
56 | 44 | 44.3±4.3 | 44.9±3.9 | Tanrebi decoction | Sodium acetate | 14 | 14 | 54 | 37 | 1 |
| Chifeng Wang, 2014 |
36 | 36 | 51.7±3.2 | 52.1±2.9 | Simiao pill | Meloxicam | N/A | N/A | 33 | 30 | 1 |
| Jianping Luo, 2010 |
30 | 30 | N/A | N/A | Modified Simiao Powder |
Diclofenac Sodium Enteric-coated Tablets+ Colchicine |
3 | 3 | N/A | N/A | 1 |
| Xianzhang Zeng, 2013 |
60 | 58 | N/A | N/A | Modified Simiao Powder |
Colchicine+ allopurinol |
14 | 14 | 58 | 51 | 1 |
| Jinjin Jia, 2010 |
28 | 26 | 43±10.8 | 44±11.3 | Modified Simiao Powder |
Colchicine | 14 | 14 | 26 | 23 | 1 |
| Xiaozhong Yu, 2013 |
32 | 30 | N/A | N/A | Simiao powder | Ibuprofen+ Colchicine | 14 | 14 | 31 | 28 | 1 |
| Jinfeng Li, 2013 |
35 | 35 | N/A | N/A | Simiaomaqian powder | Diclofenac Sodium Sustained Release Tablets | 7 | 7 | 34 | 33 | 1 |
Table 2.
Outcome of the meta-analyses for the comparison between clearing heat and removing dampness method of Chinese traditional medicine and western medicine, according to study design.
| Author, year | Effective number | SUA | CRP | ESR | Adverse reactions | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| EG | CG | EG | CG | EG | CG | EG | CG | EG | CG | |
| Yan Zhang, 2016 | 25 | 23 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Fang Zuo, 2001 | 52 | 22 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Yihui Yan, 2006 | 33 | 28 | 487.27± 98.88/374.88± 95.48 | 469.26± 114.41/414.52± 102.13 | N/A | N/A | N/A | N/A | N/A | N/A |
| Xubin Zhao, 2014 | 25 | 23 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Li Cheng, 2009 | 31 | 29 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 9 |
| Guicai Sun, 2007 | 58 | 54 | 568.6±21.2/397.2±36.7 | 572.5±27.6/385.8±30.2 | N/A | N/A | 59.2±7.4/17.1±4.6 | 53.7±8.7/15±4.3 | N/A | N/A |
| Yuhong Zhang, 2003 | 39 | 42 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Shengyun Wu, 2017 | 33 | 18 | N/A | N/A | 35.5±3.5/8.9±1.1 | 35.7±3.3/10.1±1.2 | 45.7±9.3/14.6±9.4 | 46.9±9.1/21.8±9.2 | N/A | N/A |
| Qingsheng He, 2016 | 49 | 44 | 511±47.77/370±21.56 | 497±50.12/476±19.57 | 31.34±9.12/8.04±1.29 | 29.77±8.9/9.26±2.55 | 45±11.26/17±6.78 | 47±12.57/21±5.91 | 0 | 5 |
| Lixin Wang, 2001 | 67 | 33 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 32 |
| Zhonghua Yang, 2007 | 55 | 27 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Wenping Cao, 2008 | 44 | 38 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Yanhong Zou, 2010 | 34 | 32 | 442.15±60.12/399.76±38.27 | 438.58±67.45/417.12±41.45 | 67.12±30.23/33.46±15.23 | 60.58±29.40 | 64.12±25.78/34.28±12.21 | 60.10±23.69/40.79±13.08 | N/A | N/A |
| Jincheng Cai, 2006 | 52 | 43 | 585±155/458±162 | 592±142/587±148 | N/A | N/A | N/A | N/A | N/A | N/A |
| Wei Li, 2016 | N/A | N/A | 536.24±54.16/316.49±48.28 | 529.75±52.67/376.62±35.39 | 32.94±5.84/13.26±8.49 | 33.18±5.63/20.17±9.64 | 24.21±9.64/10.26±5.35 | 23.68±9.71/14.86±5.47 | N/A | N/A |
| Yingxu Wang, 2014 | 31 | 27 | 605.21±132/474.63±85.4 | 601.16±114.2/454.51±92.2 | N/A | N/A | N/A | N/A | N/A | N/A |
| Wei Liu, 2016 | 30 | 29 | 548.25±96.31/394.34±32.69 | 541.45±48.11/46 | N/A | N/A | N/A | N/A | N/A | N/A |
| Feng Yue, 2005 | 30 | 30 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Yanming Ren, 2007 | 52 | 27 | 544.36±86.27/341.25±79.34 | 567.74±91.13/387.32±64.64 | N/A | N/A | 52.61±12.35/28.37±9.36 | 48.22±11.79/42.72±0.24 | N/A | N/A |
| Huilian Wang, 2012 | 34 | 33 | N/A | N/A | 49.7±11.6/18.5±6.4 | 47.6±12.6/18.2±5.7 | 9.0±3.0/3.9±1.2 | 8.9±2.9/4.0±2.0 | N/A | 6 |
| Wei Jin, 2013 | 30 | 24 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Hong Tu, 2015 | 29 | 24 | N/A | N/A | 26.28±7.89/5.47±3.01 | 24.16±6.99/12.12±4.21 | 39.62±16.51/14.71±8.97 | 37.74±14.63/24.07±12.61 | 1 | 5 |
| Binchu Wang, 2000 | 49 | 33 | 489±23.1/345±20.1 | 486±21.5/371±19.1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Haifeng Li, 2012 | 67 | 69 | 287.6±56.4 | 426.1±89.2 | N/A | N/A | 21.1±5.4 | 38.3±10.0 | N/A | N/A |
| Hongtao Yan, 2006 | 18 | 16 | 537.85±39.72/425.3±16.24 | 558.5±31.27/550.8±25.09 | N/A | N/A | 45.30±7.97/40±5.39 | 44.55±8.11/43.95±5.85 | 1 | 8 |
| Weigang Zeng, 2010 | 54 | 32 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 2 |
| Weigang Zeng, 2007 | 118 | 108 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 60 |
| Jiang Wu, 2015 | 33 | 30 | 528.46±78.42/436.14±83.27 | 521.47±80.12/446.72±67.46 | 26.24±12.08/10.37±2.58 | 27.18±11.83/12.43±3.19 | 40.72±13.06/16.87±2.26 | 39.24±13.27/24.35±4.03 | 2 | 6 |
| Jing Chen, 2017 | 58 | 47 | 542.15±36.79/384.20±47.28 | 538.76±42.53/437.21±42.13 | N/A | N/A | N/A | N/A | N/A | N/A |
| Minghai Zhou, 2014 | 19 | 15 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 3 |
| Guangheng Cui, 2011 | 55 | 56 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Yangang Wang, 2005 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Hai Lu, 2013 | 29 | 25 | 564±80.5/326±20.3 | 518±75.4/349±34.7 | 36.1±4.3/14.6±5.6 | 34.2±6.8/18.4±3.9 | 65.7±18.5/22.6±7.3 | 63.4±11.7/29.6±6.9 | 2 | 1 |
| Bo Duan, 2016 | 47 | 46 | 673.31±25.26/421.43±58.90 | 666.42±31.54/432.27±70.11 | 36.83±9.62/15.42±8.94 | 34.56±10.11/17.02±7.78 | 20.52±9.98/8.23±5.83 | 18.95±10.01/8.99±6.37 | 19 | 24 |
| Guoying Han, 2010 | 39 | 29 | 568.6±92.5/412.5±94.7 | 581.7±102.4/483.4±107.6 | N/A | N/A | N/A | N/A | N/A | N/A |
| Min Dai, 2015 | 36 | 29 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Xiaohong He, 2008 | 27 | 20 | 508.0±63.6/276.1±23.2v | 512.2±57.6/408.3±30.9 | N/A | N/A | 56.5±10.2/17.4±5.7 | 54.9±11.5/30.6±8.3 | N/A | N/A |
| Xiaoxia Wang, 2010 | 28 | 29 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Huijuan Yao, 2010 | 51 | 52 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Lei Zhang, 2016 | 33 | 31 | 546.69±34.23/393.02±62.69 | 542.43±43.65/479.81±71.81 | N/A | N/A | 28.59±6.69/17.54±4.74 | 29.59±5.59/23.22±6.08 | 0 | 0 |
| Bo Shi, 2010 | 38 | 25 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Liping Yan, 2012 | 35 | 23 | 573.4±113.6/369.1±117.2 | 587.5±109.7/421.8±121.3 | N/A | N/A | N/A | N/A | N/A | N/A |
| Yulei Wu, 2015 | 38 | 32 | 573.7±102.9/428.5±122.5 | 582.7±112.5/368.4±117.8 | N/A | N/A | N/A | N/A | N/A | N/A |
| Yueqi Wang, 2013 | 30 | 29 | 542.36±54.55/351.12±43.92 | 534.99±58.81/424.73±56.79 | 30.90±10.15/6.70±5.11 | 31.45±10.75/12.65±5.26 | 28.90±6.53/6.74±3.14 | 29.45±11.58/7.67±4.11 | 0 | 7 |
| Rong Li, 2014 | 69 | 62 | 525.68±114.85/308.30±50.96 | 537.01±126.46/375.60±61.17 | N/A | N/A | N/A | N/A | N/A | N/A |
| Shanshan Yu, 2008 | 38 | 34 | 552.80±92.76/284.43±58.39 | 560.48±89.37/363.22±63.21 | N/A | N/A | N/A | N/A | 1 | 11 |
| Weidong Qian, 2007 | 53 | 34 | N/A | N/A | N/A | N/A | N/A | N/A | 1 | 5 |
| Zheng Huang, 2013 | 28 | 27 | 477.16±97.33/430.65±88.97 | 465.52±90.13/451.91±89.48 | N/A | N/A | N/A | N/A | N/A | N/A |
| Chongyu Tan, 2013 | 48 | 34 | 568.73±38.29/326.81±38.14 | 573.77±39.87/371.90±38.39 | N/A | N/A | N/A | N/A | 4 | 16 |
| Chun Kang, 2012 | 28 | 24 | 485.65±53.11/303.22±46.35 | 489.18±52.61/396.43±41.91 | N/A | N/A | N/A | N/A | 1 | 9 |
| Xiaowu Fan, 2013 | 48 | 38 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Jianchong Shen, 2014 | 57 | 49 | 495.99±50.73/312.78±54.03 | 485.50±47.58/378.07±50.89 | N/A | N/A | N/A | N/A | 1 | 5 |
| Guiqiong Huang, 2016 | 55 | 38 | 547.48±50.93/304.28±60.14 | 546.37±46.65/415.96±51.86 | 26.17±10.28/5.98±1.45 | 25.94±9.45/16.05±1.76 | 35.18±8.82/15.79±4.21 | 34.95±7.88/23.57±4.52 | N/A | 17 |
| Xin Ouyang, 2004 | 28 | 25 | 492.54±76.03/287.53±93.04 | 498.00±83.46/367.53±93.81 | N/A | N/A | 54.65±11.78/23.43±16.71 | 53.10±10.82/32.03±17.42 | 0 | 18 |
| Zhimin Qi, 2016 | 101 | 93 | 515.13±118.04/318.57±76.12 | 508.67±121.38/392.06±78.39 | 24.60±7.68/8.82±2.58 | 23.86±7.44/12.26±2.71 | 48.91±12.68/17.58±5.22 | 48.36±12.27/22.14±6.15 | 4 | 16 |
| Yaping Chen, 2014 | 40 | 37 | N/A | N/A | N/A | N/A | N/A | N/A | 15 | 32 |
| Demei Li, 2012 | 38 | 34 | 496±66.9/266±48.6 | 498±49.6/562±51.6 | 35.4±6.5/15.6±5.2 | 38.5±7.8/21.9±6.1 | 68.3±15.6/21.5±12.5 | 64.9±12.6/30.2±7.9 | 5 | 16 |
| Yanzhi Lin, 2009 | 28 | 22 | 506.57±119.90/352.41±79.93 | 548.70±83.98/402.42±85.53 | 8.15±1.25/4.64±0.97 | 8.52±1.23/6.32±1.09 | 32.62±13.82/17.9±5.2 | 32.40±13.93/26.4±10.87 | N/A | 17 |
| Dehe Li, 2007 | 36 | 26 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Jun Hao, 2014 | 29 | 23 | N/A | N/A | N/A | N/A | N/A | N/A | 0 | 11 |
| Chongqing Yang, 2006 | 27 | 28 | 487.27±98.87/404.88±95.48 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Lin Wang, 2011 | 26 | 27 | 498.33±87.25/491.13±86.89 | 498.28±128.18/482.23±116.51 | 29.94±22.06/9.24±5.7 | 52.46±56.82/18.16±28.10 | N/A | N/A | 0 | 1 |
| Ayijiaman, 2012 | 54 | 37 | 539.16±34.49/376.3±52.85 | 552.29±46.15/425.79±48.69 | N/A | N/A | N/A | N/A | N/A | N/A |
| Chifeng Wang, 2014 | 33 | 30 | 482.5±51.3/388.3±50.4 | 481.5±50.9/420.2±55.9 | 24.4±3.6/15±2.6 | 24.34±3.7/16±2.9 | 26.3±4.3/13.6±7.2 | 26.2±4.5/15.8±6.8 | N/A | N/A |
| Jianping Luo, 2010 | N/A | N/A | 545.1±5.1/501.2±5.2 | 546.9±4.9/518.1±5 | N/A | N/A | N/A | N/A | N/A | N/A |
| Xianzhang Zeng, 2013 | 58 | 51 | 589.35±92.87/317.26±89.23 | 578.34±95.31/323.44±92.59 | N/A | N/A | N/A | N/A | N/A | N/A |
| Jinjin Jia, 2010 | 26 | 23 | 488.3±78.4/285.75±75.6 | 490.2±72.5/433.5±77.5 | N/A | N/A | N/A | N/A | 0 | 5 |
| Xiaozhong Yu, 2013 | 31 | 28 | 556±23.1/216.12.6 | 552.±21.8/221±15.2 | N/A | N/A | N/A | N/A | 1 | 15 |
| Jinfeng Li, 2013 | 34 | 33 | 468.39±100.28/342.47±90.26 | 452.28±98.75/437.65±94.57 | N/A | N/A | N/A | N/A | N/A | N/A |
aEG: experimental group, CG: control group; bSUA: serum uric acid; cCRP: C-reactive protein; dESR: Erythrocyte Sedimentation Rate; eN/A: not applicable.
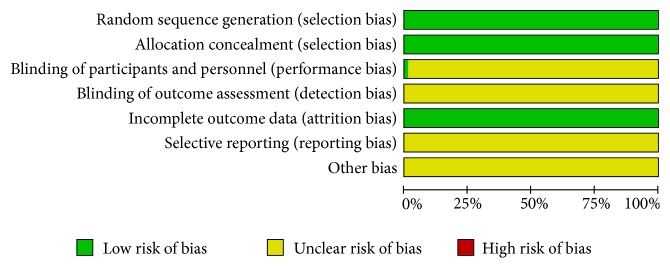
3.2. Risk of Bias
All of the selected trials adopted the method of randomization [9–77], which involved sealed envelopes11, randomized block [9, 10, 12, 13, 15, 17–33, 36–38, 40–51, 53–77], and random number table [14, 16, 34, 35, 39, 52]. Therefore, those trials were considered low risks in terms of selection bias. Only one trial involved the method of blinding [36]. These parameters were considered low risk in terms of incomplete outcome data. Detection bias, reporting bias, and other potential biases were unclear in all studies (Figures 2 and 3).
Figure 2.
Risk of bias summary.
Figure 3.
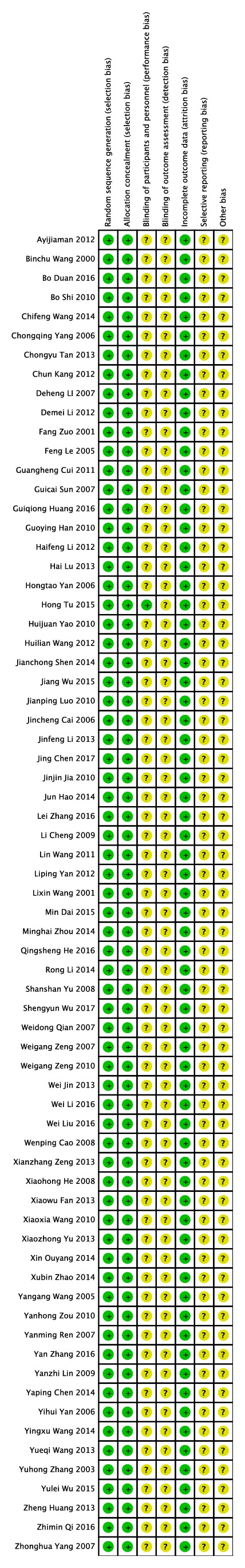
Risk of bias graph.
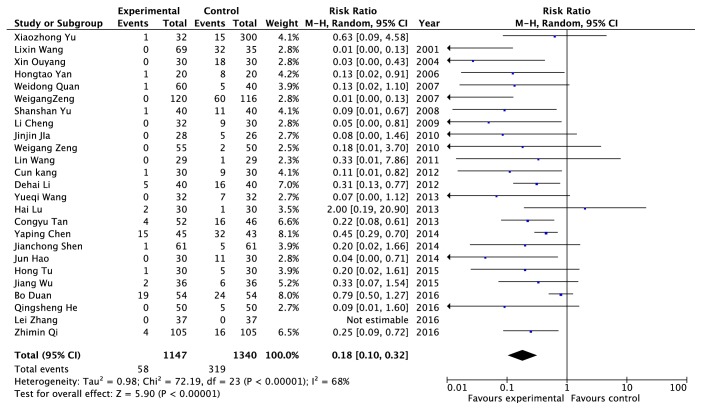
3.3. Adverse Reactions
Adverse reactions data were provided from twenty-five RCTs, including 2217 patients (1147 cases in the experimental group and 1070 cases in the control group) [11, 20, 23, 24, 27, 30, 32, 34–36, 38–40, 42, 47, 48, 53–59]. The random model was applied finally because of its heterogenicity with I2 = 68% (Figure 4). The results indicated that the adverse reactions rate of patients taking Chinese herb and (or) receiving other traditional Chinese medicine treatment was lower than that of patients who take western medicine (0.18 times), and the difference was statistically significant (P < 0.00001).
Figure 4.
An analysis of the adverse reactions caused by clearing heat and removing dampness method and western medicine in the treatment of gout.
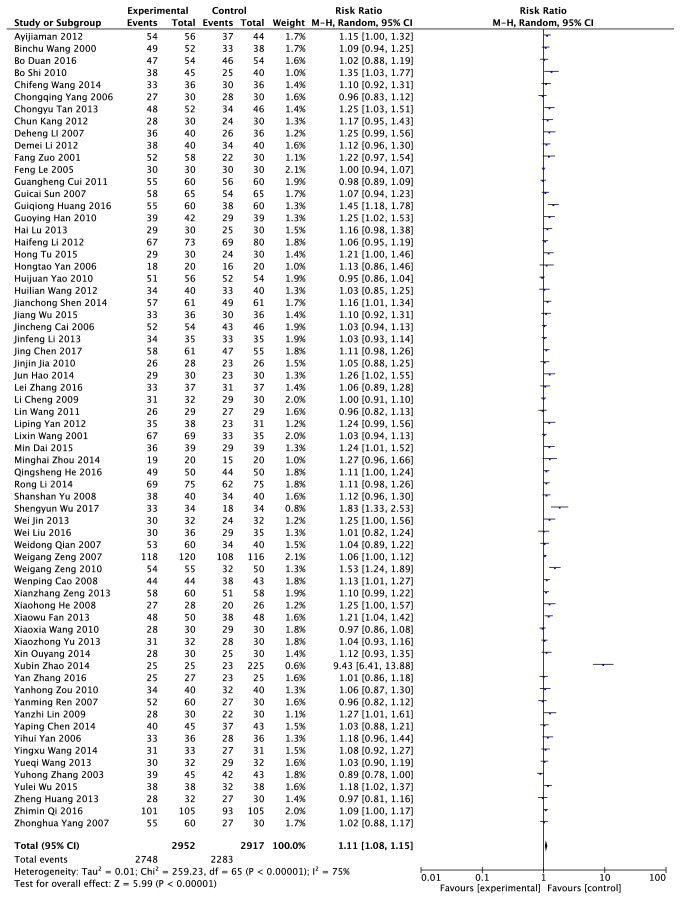
3.4. Efficacy
The effective rate data were provided from sixty-six RCTs, including 5669 patients (2952 cases in the experimental group and 2717 cases in the control group) [9–13, 15–44, 46–69, 71–77]. The random model was used because of its heterogeneity with I2 = 75% (Figure 5). The results indicated that the effective rate of patients who took Chinese herb and (or) treated with other traditional Chinese medicine methods were higher than that of those who used Western Medicine (1.11 times). The difference was statistically significant (P < 0.00001).
Figure 5.
An analysis of the effective of clearing heat and removing dampness method and western medicine in the treatment of gout.
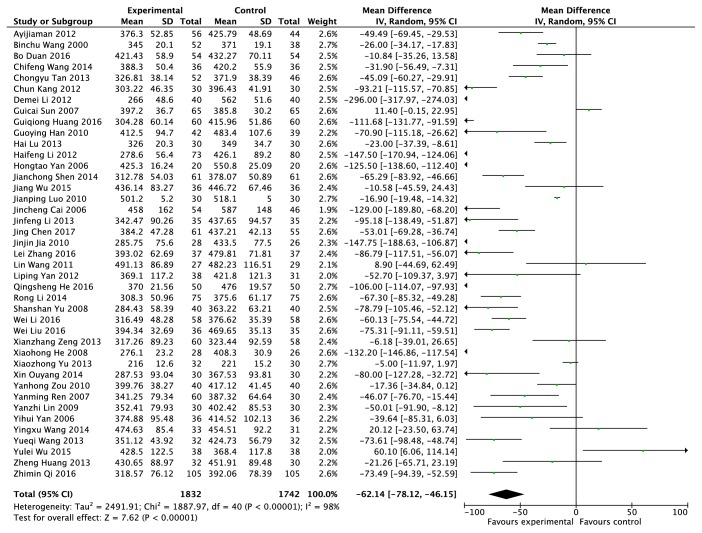
3.5. Serum Uric Acid Concentration (μmol/L)
The serum uric acid concentration data were provided from forty-one RCTs, including 3549 patients (1834 cases in the experimental group and 1715 cases in the control group) [9–49]. The random model was adopted according to I2 = 98% (Figure 6). Compared with the patients in the control group who only took western medicine, the level of serum uric acid concentration was reduced by 62.14% in patients who took traditional Chinese herb and (or) treated with other traditional Chinese medicine methods. The results were statistically significant (P < 0.00001).
Figure 6.
Effects of clearing heat and removing dampness method and western medicine on serum uric acid in the treatment of gout.
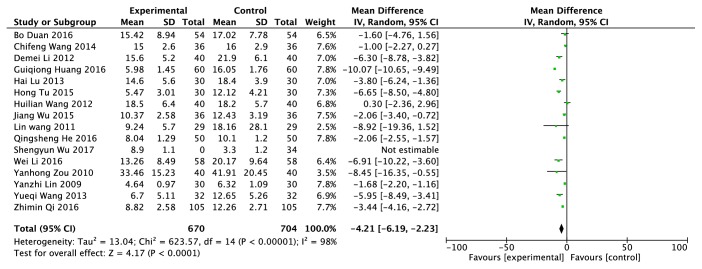
3.6. C-Reactive Protein (mg/L)
The C-reactive protein data was provided from sixteen RCTs, including 1408 patients (704 cases in the experimental group and 704 cases in the control group) [12, 14, 21, 23, 24, 30, 37–42, 44, 50–52]. A random model was adopted according to I2 = 98% (Figure 7). Compared with the patients in the control group who only took western medicine, the level of C-reactive protein was reduced by 4.21% in patients who took traditional Chinese herb and (or) treated with other traditional Chinese medicine methods. They were statistically significant on the difference of two intervention methods to reduce C-reactive protein levels ( P <0.0001).
Figure 7.
Effects of clearing heat and removing dampness method and western medicine on C-reactive protein in the treatment of gout.
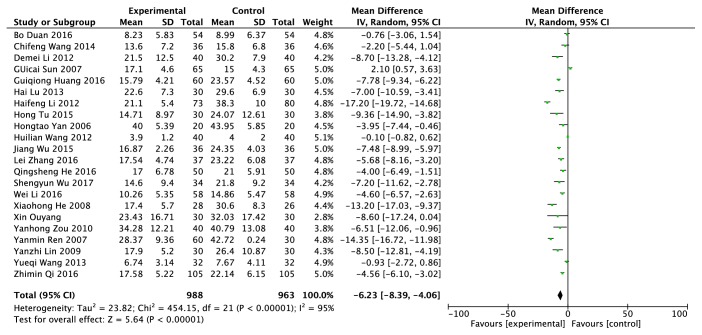
3.7. Erythrocyte Sedimentation Rate (ESR) (mm/h)
The Erythrocyte sedimentation rate data was provided from twenty-two RCTs, including 1951 patients (988 cases in the experimental group and 963 cases in the control group) [10–12, 14, 17, 19, 20, 23, 24, 26, 27, 30, 37–41, 44, 50–52]. A random model was adopted according to I2 = 95% (Figure 8). Compared with the patients in the control group who only took western medicine, the level of Erythrocyte sedimentation rate was reduced by 6.23% in patients who took traditional Chinese herb and (or) treated with other traditional Chinese medicine methods. There was significant difference between the experimental group and the control group on ESR (P < 0.00001).
Figure 8.
Effects of clearing heat and removing dampness method and western medicine on ESR in the treatment of gout.
4. Discussion
With the continuous improvement of people's living standard, the change of dietary structure and the influence of environmental factors, the incidence of gout has been gradually increased every year all over the world. Nowadays, the patient with gout could only be alleviated but not cured with existing clinical treatments; thus searching for a better therapeutic method has been appeared to be very important. Our current study analyzed data from 69 RCTs that aimed to assess the therapeutic effect and safety of heat and removing dampness method of Traditional Chinese Medicine for gouty arthritis.
In respect of adverse reaction rate, clearing heat and removing dampness method with or without other traditional Chinese medicine therapy are better than western medicine treatment (RR = 0.18). The adverse reactions often occurred during the process of using drugs, such as abdominal pain, diarrhea, vomiting, and inappetence, and even causing damage of liver and kidney in severe cases. Compared with western medicine, clearing heat and removing dampness method was shown to be more effective to the patients with gout, with less adverse reactions mentioned above at the same time, probably due to the synergistic action of multicomponents and multitargets in the traditional Chinese medicine and the integrity of human body. The clearing heat and removing dampness method which is the unique medical method based on Chinese traditional medicine has a good effect to treat patients with gout, mainly because of the pathogenesis of gout disease which is that the meridian is blocked by a pathogenic factor formed by blending of heat and wetness evils [7].
According to our results, the clearing heat and removing dampness method of Chinese traditional medicine adjuvant treatment of Chinese medicine such as acupuncture and cupping could effectively reduce uric acid, C-reactive protein, and ESR in patients with gout. Different researchers have chosen different modalities of the clearing heat and removing dampness method of Chinese traditional medicine, such as Si Miao San [29–31], Xuan Bi Fang [38, 39], acupuncture and Chinese medicine combination [41, 59, 76], etc. Among them, the types of Chinese medicine, the dose, and the acupoint selection of acupuncture and acupuncture techniques are inconsistent. Therefore, our results cannot get a clear conclusion, we do not know which treatment method has the best effect on gout and the least adverse reactions.
In this study, there are many shortcomings: a lot of randomized controlled trials are not amply descripted in grouping; it is not sufficient to prove that the randomization program is executed correctly. The overall methodological quality is poor, which limits the value of the effect of the clearing heat and removing dampness method of Chinese traditional medicine in the treatment of gout. Therefore, an indepth investigation and further extensive study were need in the future.
Acknowledgments
This work was supported by National Natural Science Foundation of China (No. 81873195), the China Postdoctoral Science Foundation [2017M611241], Liaoning Undergraduate Program for Innovation and Entrepreneurship [2017101610100051], the project of Dalian Young Star on science and Technology in 2016 (2017RQ122), and Dalian Medical University Undergraduate Program for Innovation and Entrepreneurship.
Contributor Information
Jia-Lin Qu, Email: jialin_qu@126.com.
Li-Na Liang, Email: lianglina304@163.com.
Lin Zhang, Email: zhl8247@163.com.
Disclosure
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Nan Xiao and Hao Chen contributed equally to this work.
References
- 1.Stewart S., Dalbeth N., Vandal A. C., Rome K. The first metatarsophalangeal joint in gout: A systematic review and meta-analysis. BMC Musculoskeletal Disorders. 2016;17(1) doi: 10.1186/s12891-016-0919-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou L., Liu L., Liu X., et al. Systematic review and meta-analysis of the clinical efficacy and adverse effects of Chinese herbal decoction for the treatment of gout. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0085008.e85008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jyaysi D., Stefanie S., Hans-Joachim A. Molecular pathophysiology of gout. Trends in Molecular Medicine. 2017;23(8):756–768. doi: 10.1016/j.molmed.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Barry L. H., Eric M., Travis Wilkes R. Diagnosis, treatment, and prevention of gout. American Family Physician. 2014;90(12):831–836. [PubMed] [Google Scholar]
- 5.Chen G. L., Zhou Y. F., Zhang Y. Research progress in medicine for treating gout and hyperuricemia. Chinese Journal of Clinical Pharmacology and Therapeutics. 2017;22(1):104–109. [Google Scholar]
- 6.Liu S.-H., Chuang W.-C., Lam W., Jiang Z., Cheng Y.-C. Safety surveillance of Traditional Chinese Medicine: current and future. HHS Public Access. 2015;38(2):117–128. doi: 10.1007/s40264-014-0250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang J. Y., Zhang Y. FAN Yong-sheng’s experience in treating acute gout by using Qingre Lishi Formula. China Journal of Traditional Chinese Medicine and Pharmacy. 2016;31(1):135–137. [Google Scholar]
- 8.Althea A., Eric B., Rebecca K., et al. Formalizing the definition of meta-analysis in Molecular Ecology. Molecular Ecology. 2015;24:4042–4051. doi: 10.1111/mec.13264. [DOI] [PubMed] [Google Scholar]
- 9.Zhao X. B. Clinical observation on the treatment of gout with pricking blood cupping combined with microwave. World Latest Medicine Information. 2014;(29):p. 353. [Google Scholar]
- 10.Sun G. C., Yu X. F., Li D. G., et al. Clinical observation of the effect of Compound Herba Siegesbeckiae Capusles treating recurrent gouty arthritis. Chinese Journal of Information on Traditional Chinese Medicine. 2007;(2):34–35+64. [Google Scholar]
- 11.He Q. S. 50 cases of Modified Simiao Decoction with XinHuangPian external treating acute gouty arthritis. Guangxi Journal of Traditional Chinese Medicine. 2016;39(2):37–38. [Google Scholar]
- 12.Zou Y. H., Li Z. G., Zhang S. J. Clinical observation of LizhuoDingtong Yin treating damp heat stasis type gout. Acta Chinese Medicine and Pharmacology. 2010;38(3):113–114. [Google Scholar]
- 13.Cai J. C., Zheng R. J. Observation of curative effect of gouty arthritis treated by NiantongXiaofeng prescription. Jiangxi Journal of Traditional Chinese Medicine. 2006;(3):28–29. [Google Scholar]
- 14.Li W., Yin Y. W., Li Z. G. Clinical study on the treatment of acute gouty arthritis by QingreChushi prescription. Acta Chinese Medicine and Pharmacology. 2016;44(5):117–119. [Google Scholar]
- 15.Wang Y. X., Liu D. B., Zhou X. L., et al. Clinical study on the treatment of gouty arthritis by QingreHuazhuoSanjie Method. Guangming Journal of Chinese Medicine. 2014;29(4):724–727. [Google Scholar]
- 16.Liu W., Wu Y. H., Zhang L., et al. Clinical RCTs of QingreJieduLishiHuazhuo method for treating gout. China Journal of Traditional Chinese Medicine and Pharmacy. 2016;31(3):1113–1116. [Google Scholar]
- 17.Ren Y. M., Wen S. D., Sa Y. P., et al. Clinical observation of treatment of acute gouty arthritis by Clearing heat and removing dampness, Huayu Quzhuo Method. Journal of Sichuan of Traditional Chinese Medicine. 2007;(9):45–46. [Google Scholar]
- 18.Yan L. P., Zhou Z. Q. Clinical observation of 38 cases of Clearing heat and removing dampness Decoction in the treatment of acute gouty arthritis. Jilin Journal of Traditional Chinese Medicine. 2012;32(6):600–601. [Google Scholar]
- 19.Wu Y. L., Lv Y., Xu Z. H. Clinical study of Qingrelishihuoxue method in the treatment of acute gouty arthritis. Medical Information. 2015;29:98–99. [Google Scholar]
- 20.Wang Y. Q. Clinical Study on Treatment of Acute Gouty Arthritis of Qingrelishihuoxue Method. Beijing University of Chinese Medicine; 2013. [Google Scholar]
- 21.Qian W. D., Qian X. Q. 60 cases of QingrelishiTongluo therapy in the treatment of gouty arthritis of damp heat. Jiangxi Journal of Traditional Chinese Medicine. 2008;(1):p. 34. [Google Scholar]
- 22.Huang Z., Wang Y. F., Zhang M. Clinical observation on 32 cases of QingreLishiTongluo Decoction in treating acute gouty arthritis. Journal of New Chinese Medicine. 2013;45(12):85–87. [Google Scholar]
- 23.Shen J. C., Mo J. X., Cai S. Q. Clinical observation of 60 cases of QingrelishiTongluozhitong treatment of acute gouty arthritis with damp heat blockage syndrome. Zhejiang Journal of Traditional Chinese Medicine. 2014;49(11):797–798. [Google Scholar]
- 24.Huang G. Q., Chen H., Liu Q. R., et al. Observation of curative effect of QingrelishiTongluozhitong treatment for acute gouty arthritis. Shaanxi Journal of Traditional Chinese Medicine. 2016;37(11):1483–1485. [Google Scholar]
- 25.Ouyang X. Clinical observation of QingrelishiXieduhuayu method in the treatment of acute persisting gout. Journal of Emergency in Traditional Chinese Medicine. 2004;13(4):211–212. [Google Scholar]
- 26.Chen Y. P. 45 cases of the treatment of acute gouty arthritis by Qingretongluoxiezhuo decoction. Zhejiang Journal of Integrated Traditional Chinese and Western Medicine. 2014;24(3):259–260. [Google Scholar]
- 27.Li D. H., Yu T. 40 cases of Sanjinsanmiao decoction combined with western medicine treating gout. Shaanxi Journal of Traditional Chinese Medicine. 2007;(4):428–429. [Google Scholar]
- 28.Li J. F., Song T. B. The effects of Simiao Maqian decoction in the treatment of gouty arthritis. Guangming Journal of Chinese Medicine. 2013;28(6):1161–1162. [Google Scholar]
- 29.Yu X. Z., Hong D. G., Wang X. Z. Curative effect observation of 32 cases of Simiao powder and Auricular point sticking treating acute gouty arthritis. Journal Gansu University of Traditional Chinese Medicine. 2013;30(3):69–71. [Google Scholar]
- 30.Jia J. J. Compared modified Simiao decoction with colchicine in the treatment of gout. Journal of Emergency in Traditional Chinese Medicine. 2010;19(1):47–48. [Google Scholar]
- 31.Zeng X. Z., Song Y. M. 60 cases of acute gouty arthritis treated with Modified Simiao powder. Hunan Journal of Traditional Chinese Medicine. 2013;29(2):68–69. [Google Scholar]
- 32.Luo J. P., Tang C. Q. Observation of the curative effect of Modified Simiao pills treating gout. Journal of Liaoning University of Traditional Chinese Medicine. 2010;12(11):156–157. [Google Scholar]
- 33.Aigaman A., Hu C. G. Clinical observation of 100 cases of Tongbi Decoction in the treatment of gout. Xinjiang Journal of Traditional Chinese Medicine. 2012;30(3):27–28. [Google Scholar]
- 34.Wang L. Clinical observation of gout decoction in the treatment of acute gouty arthritis. Beijing University of Chinese Medicine; 2011. [Google Scholar]
- 35.Yang C. Q., Cao K. G. Clinical observation of 30 cases of acute gouty arthritis treated with gout mixture. China Journal of Traditional Chinese Medicine and Pharmacy. 2006;(8):474–475. [Google Scholar]
- 36.Tu H., Bao J. W., Tu R. F., et al. 30 cases of gouty arthritis treated with gout clear granule. Chinese Medicine Modern Distance Education of China. 2015;13(24):35–37. [Google Scholar]
- 37.Wang B. C. Treatment of 52 cases of gouty arthritis with gout Decoction. Hunan Guiding Journal of TCMP. 2000;(3):28–29. [Google Scholar]
- 38.Li H. F. Clinical observation of 73 cases of Xuanbitang Decoction for the treatment of gouty arthritis. Guiding Journal of Traditional Chinese Medicine and Pharmacology. 2012;18(3):83–84. [Google Scholar]
- 39.Yan H. T. Clinical observation of curative effect of Xuanbi Decoction in the treatment of acute gouty arthritis. Heilongjiang University of Chinese Medicine; 2006. [Google Scholar]
- 40.Zeng W. G. Yushan gout Decoction in the treatment of gouty arthritis in 120 cases. Journal of Traditional Chinese Medicine. 2007;(1):58–59. [Google Scholar]
- 41.Wu J., Xu Y. Clinical observation of acupuncture combined with Qingrelishi decoction in the treatment of acute gouty arthritis. Journal of Emergency in Traditional Chinese Medicine. 2015;24(4):717–719. [Google Scholar]
- 42.Wang Y. G., Miao Z. M., Yan S. L., et al. A Randomized Parallel Clinical Study on the Treatment of Gout with Chinese Herbal Medicine. Vol. 4. ActaAcademiaeMedicinae Qingdao Universitatis; 2005. [Google Scholar]
- 43.Lu H., Wei L. F., Xie G. P. Clinical study on the treatment of gouty arthritis with Chinese herbal medicine and Western medicine. Clinical Journal of Chinese Medicine. 2013;5(1):16–17. [Google Scholar]
- 44.Duan B., Lv X. Evaluation of clinical efficacy of triple therapy for acute gout. Clinical Journal of Chinese Medicine. 2016;8(27):73–74. [Google Scholar]
- 45.Han G. Y. Observation of 42 cases of the treatment of gouty arthritis by traditional Chinese medicine. Journal of Practical Traditional Chinese Medicine. 2010;26(7):467–468. [Google Scholar]
- 46.Dai M., Zhang Y. Clinical observation of 39 cases of gouty arthritis treated with Chinese medicine. Chinese Journal of Ethnomedicine and Ethnopharmacy. 2015;24(7):49–50. [Google Scholar]
- 47.He X. H., Huang H. Y. Observation of curative effect of Chinese medicine combined therapy on acute gouty arthritis. Proceedings of the Twelfth National Symposium on rheumatic diseases of Chinese Medicine; 2008; pp. 176–177. [Google Scholar]
- 48.Wang X. X. 30 cases of acute gouty arthritis treated with self-made Shancigu decoction. Zhejiang Journal of Traditional Chinese Medicine. 2010;45(6):p. 430. [Google Scholar]
- 49.Yao H. J., Luo J. M., Fang H. T. 56 cases of comprehensive therapy for acute gouty arthritis. Journal of Emergency in Traditional Chinese Medicine. 2011;20(9):p. 1504. [Google Scholar]
- 50.Wu S. Y. Clinical observation of 34 cases of Modified Simiao Decoction with XinHuangPian external treating acute gouty arthritis. Chinese Journal of Ethnomedicine and Ethnopharmacy. 2017;26(4):127–128. [Google Scholar]
- 51.Zhang L., Wang Z. X., Gao J. Y. Clinical observation of 74 cases on the treatment of acute gout by QingrelishiHuoxuetongluo method. Chinese Medicine in Tianjin. 2016;33(7):394–397. [Google Scholar]
- 52.Zhang Y., Huang J. Y. The observation of the curative effect of Qingrelishi prescription in treatment of acute gout. Chinese Journal of General Practice. 2016;14(6):1030–1033. [Google Scholar]
- 53.Yuan Y. J. Fu Huang cream applied in combination with Modified Simiao Decoction for treating acute gouty arthritis. Journal of Practical Traditional Chinese Internal Medicine. 2010;24(12):82–83. [Google Scholar]
- 54.Wang L. X. RCTs observation of Modified Simiao pills and colchicine in the treatment of acute attack of gouty arthritis. Modern Rehabilitation. 2001;(17):p. 125. [Google Scholar]
- 55.Li R. Clinical observation of QingrelishiHuoxuehuayu therapy treating gouty arthritis in high altitude area. Journal of New Chinese Medicine. 2014;46(9):84–86. [Google Scholar]
- 56.Yu S. S., Huang Y. R. Clinical observation of curative effect of treatment on acute gouty arthritis by Qingrelishijiedu method. Hubei Journal of Traditional Chinese Medicine. 2008;30(9):p. 32. [Google Scholar]
- 57.Wang C. F., Liu R., Wang X. Y. Analysis of therapeutic effect of Tanrebi decoction for treating acute gouty arthritis. Journal of Practical Traditional Chinese Mdicine. 2014;30(7):595–596. [Google Scholar]
- 58.Zeng W. G., Zhou L., Xiao Y. H. YushanTongfengyin No. 2 in the treatment of hyperuricemia in 55 cases. Shandong Journal of Traditional Chinese Medicine. 2010;29(9):p. 607. [Google Scholar]
- 59.Zhou M. H. Clinical observation of 20 cases of combined treatment of gouty arthritis with acupuncture and medicine. Nei Mongol Journal of Traditional Chinese Medicine. 2014;33(14):p. 44. [Google Scholar]
- 60.Zuo F., Liu W., Wang H. Decoction Combined with Simiao powder for treating 58 cases of gouty arthritis. Tianjin Journal of Traditional Chinese Medicine. 2001;(1):p. 13. [Google Scholar]
- 61.Yan Y. H., Wang L. Y., Li Y. Clinical observation of Bi Ning decoction in the treatment of 36 cases of acute gouty arthritis. Chinese Journal of Information on Traditional Chinese Medicine. 2006;(6):20–21. [Google Scholar]
- 62.Cheng L., Lu L. J., Jiang X. F. Clinical experience of treatment of acute gouty arthritis with Chinese Angelica Decoction for treating pain. Journal of Emergency in Traditional Chinese Medicine. 2009;18(11):1892–1893. [Google Scholar]
- 63.Zhang Y. H., Song Y. J., Jia Y., et al. Observation of 45 cases of acute gouty arthritis treated with modified Sanmiao powder. Yunnan Journal of Traditional Chinese Medicine and Materia Medica. 2003;(4):5–6. [Google Scholar]
- 64.Yang Z. H., Wang H. M., Cui Q., et al. Clinical analysis of JianpiqingrelishiTongluo Method in treating 60 cases of acute gouty arthritis. Modern Medicine Journal of China. 2007;(11):82–83. [Google Scholar]
- 65.Cao W. P., Luo X. W., Duan L. Y. Observation of curative effect of 44 cases of acute gouty arthritis treated with JunhuZhitong powder and acupuncture. Yunnan Journal of Traditional Chinese Medicine and Materia Medica. 2008;(7):p. 25. [Google Scholar]
- 66.Feng Y., Qian Y., Zhang X. G. Clinical study on the treatment of acute attack of primary gout by QingreJieduLishi method. Hebei Journal of Traditional Chinese Medicine. 2005;(7):501–502. [Google Scholar]
- 67.Shi B., An F. M. Clinical observation of 45 cases of qingrelishi Decoction treating acute gout. Chinese Journal of Modern Drug Application. 2010;4(20):127–128. [Google Scholar]
- 68.Qin C. N., He J., Wei W. B. RCTs of Heat and dampness Tongluo Decoction in treating acute gouty arthritis. Journal of Practical Traditional Chinese Internal Medicine. 2013;27(11):37–39. [Google Scholar]
- 69.Kang C. RCTs of QingrelishiTongluo Decoction in the treatment of acute gouty arthritis. Journal of Practical Traditional Chinese Internal Medicine. 2012;26(16):35–37. [Google Scholar]
- 70.Fan X. W. RCTs of QingrelishiTongluo Decoction in the treatment of gouty arthritis. Journal of Practical Traditional Chinese Internal Medicine. 2013;27(12):22–23. [Google Scholar]
- 71.Qi Z. M., Mou C. L., Wang H. Clinical observation of QingrelishiZhuyu Decoction in the treatment of gouty arthritis. Chinese Journal of Experimental Traditional Medical Formulae. 2016;22(21):147–151. [Google Scholar]
- 72.Li D. M., Li J. H., Cai L. L., et al. Clinical observation on the treatment of acute gouty arthritis in the elderly with oral and external application of QingreZhitong Fang. Chinese Journal of Information on Traditional Chinese Medicine. 2012;19(7):77–78. [Google Scholar]
- 73.Lin Y. Z. Clinical Study of Qingxiaoyitong Decoction in the Treatment of Gouty Arthritis with Kidney Deficiency and Damp Heat. Nanjing University of Chinese Medicine; 2009. [Google Scholar]
- 74.He J., Li L. H., He B., et al. Observation of curative effect of ShandayanheSimiao Decoction in the treatment of acute gouty arthritis. Chinese Journal of Traditional Medical Science and Technology. 2014;21(1):p. 30. [Google Scholar]
- 75.Wang H. L., Wang J. H., Zhou Q., et al. Clinical observation of 40 cases of acute gouty arthritis treated with Gouty granule. World Journal of Integrated Traditional and Wastern Medicine. 2012;7(7):599–600+603. [Google Scholar]
- 76.Chen J., Deng X. H., Liu L. S. Clinical observation of combined treatment of gouty arthritis with acupuncture and medicine. Journal of Emergency in Traditional Chinese Medicine. 2017;26(2):317–319. [Google Scholar]
- 77.Cui G. H., Li Z. R., Tan X. J. Clinical observation of Zhiju gouty Decoction in the treatment of Shireyunjiexing acute gouty arthritis. Guide of China Medicine. 2011;9(3):p. 123. [Google Scholar]