Abstract
Background
Successfully transitioning patients from hospital to home is a complex, often uncertain task. Despite significant efforts to improve the effectiveness of care transitions, they remain a challenge across health care systems. The lens of complex adaptive systems (CAS) provides a theoretical approach for studying care transition interventions, with potential implications for intervention effectiveness. The aim of this study is to examine whether care transition interventions that are congruent with the complexity of the processes and conditions they are trying to improve will have better outcomes.
Methods
We identified a convenience sample of high-quality care transition intervention studies included in a care transition synthesis report by Kansagara and colleagues. After excluding studies that did not meet our criteria, we scored each study based on (1) the presence or absence of 5 CAS characteristics (learning, interconnections, self-organization, co-evolution, and emergence), as well as system-level interdependencies (resources and processes) in the intervention design, and (2) scored study readmission-related outcomes for effectiveness.
Results
Forty-four of the 154 reviewed articles met our inclusion criteria; these studies reported on 46 interventions. Nearly all the interventions involved a change in interconnections between people compared with care as usual (96% of interventions), and added resources (98%) and processes (98%). Most contained elements impacting learning (67%) and self-organization (69%). No intervention reflected either co-evolution or emergence. Almost 40% of interventions were rated as effective in terms of impact on hospital readmissions. Chi square testing for an association between outcomes and CAS characteristics was not significant for learning or self-organization, however interventions rated as effective were significantly more likely to have both of these characteristics (78%) than interventions rated as having no effect (32%, p = 0.005).
Conclusions
Interventions with components that influenced learning and self-organization were associated with a significant improvement in hospital readmissions-related outcomes. Learning alone might be necessary but not be sufficient for improving transitions. However, building self-organization into the intervention might help people effectively respond to problems and adapt in uncertain situations to reduce the likelihood of readmission.
Electronic supplementary material
The online version of this article (10.1186/s12913-018-3712-7) contains supplementary material, which is available to authorized users.
Keywords: Complex adaptive systems, Hospital readmissions, Care transitions, Health care interventions, Patient education, Self-organization
Background
Successfully transitioning patients from the hospital to home is a complex task. As hospital readmission rates have been adopted as markers of quality with financial penalties for poor performance, care transition improvement efforts have multiplied.
Over the last 30 years, a variety of care transition interventions have been implemented, including those with differing types and numbers of components; some have proven effective but many have not [1–3]. There is a lack of information about which components or combinations of components are critical to reducing early (30 day) hospital readmissions [4, 5]. We believe that one source of this variability in effectiveness is due to a mismatch between the inherent complexity of care transitions and the health care organizations in which they occur, and the types of interventions being attempted.
Health care organizations have been studied as complex adaptive systems (CAS) for many years [6–8], contributing insights about the importance of interdependencies among different parts of the system, the role of learning, and the impact of local interactions in self-organization (stable but dynamic patterns of interaction among system components), emergence (system level behaviors that cannot be explained by examining the individual components of the system), and co-evolution (patterned changes that take place as a system and its environment react to each other over time) [9]. Using the lens of CAS provides a theoretical approach for describing and understanding care transition interventions.
Effective care transitions from inpatient to outpatient require multiple diverse individuals (providers [inpatient and outpatient, multiple professions, multiple specialties], patients and caregivers) to interact, share their expertise, learn together, and depend on each other to make sense of what is happening in real time to prevent rehospitalization. CAS theory helps us understand both the complexity of care transitions and the difficulty in predicting which processes or approaches will most likely contribute to success. There is a high degree of uncertainty in predicting a patient’s trajectory of recovery after hospitalization, and therefore their specific transitional needs [10].
CAS theory brings focus to the inherent uncertainty in many clinical tasks, and in clinical systems [10]. CAS theory also suggests that for interventions to be successful, they must be congruent with the uncertainties and contextual differences that people face when they deliver care. For example, interventions that rely on a strict application of a new process from one clinical setting to another may not be as successful as one that allows for local adaptation that reflects differences in the ways that people organize themselves across systems. Interventions that foster interconnections between individuals may be more likely to improve communication and support local potential for co-evolution [11], thus increasing implementation success. Moreover, in complex interventions like those required for improving care transitions, the line between intervention and implementation is often blurred [12], as activities aimed at increasing coordination between inpatient and outpatient care teams (intervention strategy) may also function to educate providers about local care transitions resources (implementation strategy) [13].
This paper is the third in a series of articles examining the association between the degree to which interventions to improve complex care delivery activities are consistent with CAS and their degree of effectiveness. In the first of these papers [14], we found type II diabetes intervention effectiveness was positively associated with (a) the number of CAS characteristics inherent in intervention designs and (b) the degree to which the intervention impacted CAS characteristics of interconnections between individuals, and the degree to which the intervention allowed for evolution in its implementation over time. In the second paper [15], congestive heart failure intervention effectiveness was related to (a) the number of CAS characteristics present in the intervention design and (b) the CAS characteristics of learning, self-organization, and co-evolution, again suggesting the need for interventions to adapt and evolve with local patterns of care organization. We hypothesized that observed differences across our two analyses were due to differences in the ways that diabetes and heart failure lead to uncertainty for patients in their daily lives. These differences require emphasis on different CAS characteristics for successful interventions.
This paper extends this work by examining care transition interventions that move patients across complex microsystems from hospital to home. Such transitions are characterized by uncertainty and dynamic change, and frequently involve changes in patients’ functional capacities, requiring them to learn new acute and chronic self-care practices. These transitions also require successful transfer of information between medical providers and between medical providers and informal caregivers.
Our objective is to explore whether care transition intervention designs that reflect the complexity of processes and conditions they are trying to improve are associated with better outcomes. We also aim to identify key characteristics of interventions that are related to better hospital readmissions outcomes. We hypothesize that care transition interventions with elements that are congruent with the nature of CAS will be more likely to have improved readmission outcomes. We do not suggest that interventions were developed with CAS in mind, but that they vary in their degree of congruence with important CAS principles.
Methods
Because of the extensive literature on care transitions, we used Kansagara et al.’s report [4], “Transitions of Care from Hospital to Home” as our starting point. This report was prepared for the Department of Veterans Affairs Evidence-based Synthesis Program and represented a comprehensive assessment of the literature on care transitions.
Kansagara et al. identified systematic reviews of care transitions, screening them for quality (e.g., the review clearly reported their search criteria, evaluated the internal validity of included trials). Eighty-three systematic reviews met their initial criteria. They further narrowed this group to 17 of the most recent and broadly scoped systematic reviews that fit pre-identified categories. Ten of those systematic reviews focused on different types of care transition interventions (e.g., enhanced access to primary care, telephone-based follow-up) and 7 focused on specific patient populations. All included reviews contained hospital readmissions as a reported outcome, though it may not have been the primary outcome and not all studies included in the reviews reported hospital readmissions as an outcome [4]. This approach provided us a high quality, diverse set of care transition intervention types upon which to test our research question.
Inclusion and exclusion criteria
As our interest was in care transition interventions that could be applied to a wide variety of patient populations and not unique to a given disease state, we excluded the 7 targeted patient population reviews included in the Kansagara et al. review [4]. Two researchers (JP and LP) reviewed the remaining reviews in Kansagara et al. and determined that one additional review [16] could be excluded based on the review’s inclusion of studies of low quality and its limited scope (i.e. post-operative care after pancreatic surgery), leaving 154 studies from 9 reviews to be assessed for inclusion in our review. One researcher (LP) reviewed the list to exclude articles for which we could not obtain full text, that were not written in English, and that were duplicates of articles found in one of the other eight reviews, yielding 148 unique publications that were screened for inclusion and exclusion criteria (see Table 1).
Table 1.
Inclusion criteria
| Criterion | Definition |
|---|---|
| Randomized Controlled Trial | The study is a randomized controlled trial. |
| Readmissions Outcome | The individual article reports hospital readmissions. |
| Possibility of Readmission | Every subject/participant in the study has the possibility of being readmitted. |
| Intervention to Improve Care Transitions | The intervention is aimed at improving one or more care transition processes |
| Adults | Participants in the study are adults >age 18 |
| Superiority Trial | The study is a superiority trial AND includes tests of significance for the readmissions outcome measure(s). |
We limited our studies to randomized controlled trials as one proxy of quality (in addition to the quality inclusion criteria in the original reviews). To have a consistent outcome to associate with intervention characteristics, we only included articles that reported hospital readmissions as an outcome. We also excluded studies in which not every participant had the possibility of being readmitted to the hospital (e.g., studies that recruited some participants from the emergency room). We included only studies for which interventions were focused on improving some aspect of care transition processes, as defined by Kansagara et al. [4]. These included processes such as anticipatory discharge planning and care coordination, psychosocial needs assessment, transmitting discharge summaries to outpatient providers, and discharge medication reconciliation. The final inclusion criteria were that study participants be adults and that the study be a superiority trial, with tests of significance performed on the readmission outcome measure(s). Each article was independently reviewed by 2 researchers (see Fig. 1). After scoring for inclusion and exclusion criteria, pairs met to discuss discrepancies. The full research team conferred about and resolved any unresolved discrepancies.
Fig. 1.
Flow chart of review process. Legend: Steps taken in the initial selection, review, and abstraction of articles
Assessment of leveraging of characteristics of CAS
As described in our prior studies of diabetes and congestive heart failure [14, 15], interventions were categorized based on the presence or absence of 5 CAS characteristics. For this analysis, we added additional dimensions of complexity to our assessment based on evolution of the CAS literature since our original studies. This work has emphasized the interdependencies between the people (relationships), processes, and infrastructure (affordances) in the system (Table 2). We felt this was particularly important because care transition processes typically cross more than one part of a health care organization. Because relationships were already accounted for in the original CAS characteristic of interconnections, we added processes and affordances. Definitions were drawn from our previous work and refined when the group had scored 5 test articles.
Table 2.
CAS characteristic and interdependencies’ scoring criteria
| Definition | |
|---|---|
| CAS Characteristic | |
| Learning | People can and will process information, as well as react to changes in information. Education occurred explicitly or there is a new strategy for information uptake. |
| Interconnections | Change in pattern of interactions, including nonverbal communication, among agents. Introducing new agents into the system. |
| Self-organization | Order is created in a system without explicit hierarchical direction. Interventions explicitly allow for modifications, tailoring, adjustments, and negotiations based on patient characteristics, situations, circumstances, and uniqueness of patients, at the level of patients. |
| Co-evolution | The system and the environment influence each other’s development. Adaptations, additions or changes to the intervention or implementation of the intervention that affect more than one patient typically in response to new information or interim evaluation of intervention. |
| Emergence | Intervention is leveraging the fact that non-linearities will occur in the system—Specifically plans to look (e.g., scanning, monitoring) for unintended consequences to try to use them to own advantage. |
| Interdependencies | |
| Affordances | Something new (e.g., staff, process) was brought to the care transition under focus. New resources have been brought in to change an outcome of interest. This might include new staff but could be old staff doing a new thing (i.e. reallocation of old resources or allocation of new resources). |
| Processes | Any standard workflow change or work standardization could be in the form of a process checklist. |
After the scoring guide was finalized (see Table 2), each article was assigned to be read and independently scored by two researchers. For each intervention described in the included studies, each CAS characteristic was scored as either 0 (absent) or 1 (present). Pairs who had independently scored the studies met to identify and resolve discrepancies in scoring, and to ensure intercoder reliability. Scoring that could not be decided among the pairs was discussed in group meetings and final decisions about scoring were made by the group.
After scoring was completed, pairs also abstracted the articles to document sample size, readmission-related outcome unit(s), readmission-related results, and overall project success. Outcome units were described in terms of the timeframe (e.g., 30 days, 1 year) and the measurement (e.g., incidence of readmissions, length of stay of readmissions). Researchers described results in terms of whether there were statistically significant differences between the study groups on the readmission-related outcome measures. Because of the heterogeneity of outcome measurement, overall intervention success was scored dichotomously as either 0 (not effective) and 1 (effective) as described below in Table 3.
Table 3.
Scores for intervention effectiveness
| Score | Description | Criteria |
|---|---|---|
| 0 | No effect | None of the readmission-related outcomes were significantly better for the intervention group |
| 1 | Intervention effective | At least one readmission-related outcome was significantly better in the intervention group |
Analysis
We examined the distribution of CAS characteristics and outcomes among the studies. From this, we identified the CAS characteristics that were most variable in terms of presence or absence in the intervention design (e.g., the CAS characteristic was neither rarely nor nearly always present). We conducted chi squared tests to investigate the significance of the relationship between each of those characteristics and outcomes.
We conducted a second statistical analysis using Fisher’s exact test extension developed by Mehta and Patel [17], to test the relationship between the total number of variable CAS characteristics each intervention had and its effectiveness. Studies were scored with a 0, 1, or 2 based on how many of the CAS characteristics with the most variability were reflected in their intervention design. All statistical analyses were performed using Stata 14 [18].
Results
Included studies
We initially reviewed 154 publications from the 9 systematic reviews [19–27] for potential inclusion in our analysis. Eight publications were immediately excluded because we could not obtain full text copies (n = 4), the full text was not written in English (n = 2), or contained duplicate data from another publication included in the Kansagara review(n = 2). After screening full text of the remaining 146 articles, 102 publications were excluded for not meeting inclusion criteria (see Fig. 2). The majority (67%) were excluded for not having a hospital readmissions outcome.
Fig. 2.
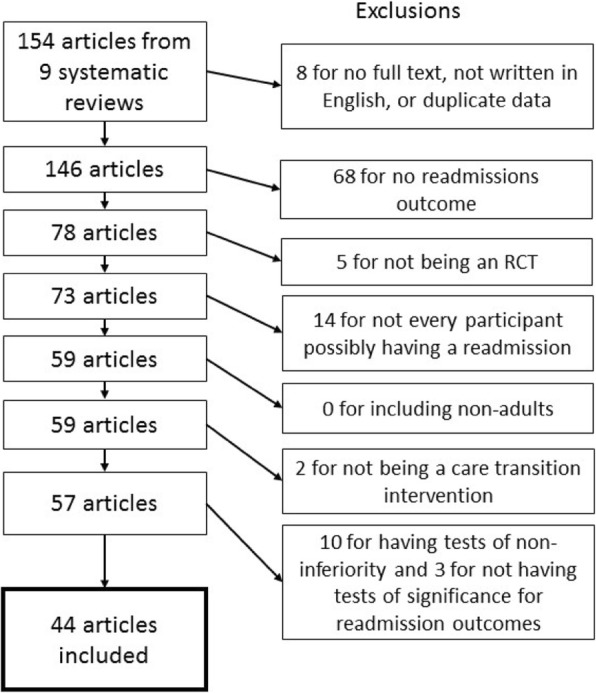
Procedure for selecting articles. Legend: Flow chart depicting details of articles which were excluded from this analysis based on inclusion criteria
Forty-four publications were included in our analysis [28–71] (see Additional file 1). Studies had a mean sample size of 420 people (range: 24 to 2353). There was heterogeneity in readmissions outcomes, including, percent of patients readmitted within 30 days, duration of all cause rehospitalizations at 180 days, the incidence of unexpected admissions at 5 weeks, and the proportion of participants readmitted at 6 months. The number of readmission-related outcomes reported also varied, ranging from 1 to 18. On average, studies reported 3 readmission related outcomes, however the majority (65%) reported 1 or 2 readmissions-related outcomes.
Assessment of interventions
Two publications described three armed studies, with two interventions apiece. All other studies described a single intervention. Each of the 46 interventions described in the 44 included publications was scored separately for their use of the five CAS characteristics and two interdependencies (see Additional file 2). The types of interventions reported varied from implementation of new discharge forms, to use of alerts, to multi-pronged interventions that included new post-discharge contacts between patients and healthcare providers. Almost all the interventions involved a change in interconnections from care as usual (96% of interventions), and added affordances (98%) and processes (98%) (see Table 4). The majority (67%) of interventions included learning and 69% allowed for self-organization. No intervention reflected qualities of either co-evolution or emergence, meaning that none allowed for adaptation of the intervention over time, or planned to look for results that could then be used to update the intervention.
Table 4.
Score distribution for CAS characteristics, interdependencies, and outcomes
| n (percent) | Examples | |
|---|---|---|
| CAS Characteristic | ||
| Learning | 31 (67%) | • Nurses used behavior skill training strategies with patients and encouraged their self-monitoring and use of external cognitive supports. • Nurses provided patients education on such things as vital signs, activities of daily living, coping skills, and signs and symptoms. |
| Interconnections | 44 (96%) | • Advanced practice nurses contacted patients after discharge. • Case managers met with patients after each physician visit. |
| Self-organization | 32 (69%) | • Physicians were alerted if patient values went outside normal range; if deemed necessary, physicians could ask patients to adjust medication use. • Nurses could modify or tailor the frequency of patient follow-up calls based on patient symptoms, knowledge, and needs. |
| Co-evolution | 0 (0%) | (none) |
| Emergence | 0 (0%) | (none) |
| Interdependencies | ||
| Affordances | 45 (98%) | • Patients were provided personal telecare units. • Patients were given discharge forms in one of three languages. |
| Processes | 45 (98%) | • An appointment reminder was mailed to patients 10 days prior to each appointment. • Patient discharge forms were electronically transferred to primary care nurses. |
| Positive Intervention Effect Reported | 18 (39%) | (not applicable) |
Sixty-one percent of the interventions included in our analysis did not lead to statistically significant improvements in any reported hospital readmission-related outcomes (i.e., between intervention and control groups). Thirty-nine percent of interventions had at least one readmission-related outcome that was significantly better for the intervention group than the control.
Learning and self-organization, by outcomes
Because 95% or more of the interventions incorporated the CAS characteristics of interconnections, affordances, and processes, we did not analyze the association of those characteristics with outcomes. Instead, we restricted our analyses to learning and self-organization, which had greater variability in their distribution across interventions (67 and 69%, respectively). Interventions that influenced learning, such as those that taught self-management skills, or allowed for self-organization, such as allowing providers and patients to change frequency of communication based on patient needs, were more likely to report one or more significant readmission outcomes than interventions that did not (see Tables 5 and 6). The association between readmission outcomes and CAS characteristics was not significant (p = 0.064 for learning and p = 0.104 for self-organization). Although interventions with the properties of self-organization were more likely to have significant outcomes than interventions that lacked self-organization (47% vs. 21%, respectively), this association was not significant.
Table 5.
Score distribution and chi square test results by outcome for selected CAS characteristics
| Selected CAS Characteristic Score | Rating of Intervention Effectiveness, n (row %) | Chi square | |
|---|---|---|---|
| Not Effective (n = 28) | Effective (n = 18) | ||
| Learning – 0 | 12 (80%) | 3 (20%) | 3.42, p = 0.064 |
| Learning – 1 | 16 (52%) | 15 (48%) | |
| Self-Organization – 0 | 11 (79%) | 3 (21%) | 2.65, p = 0.104 |
| Self-Organization – 1 | 17 (53%) | 15 (47%) | |
Table 6.
Score distribution by outcome and combined selected CAS characteristics
| Absence (0) or Presence (1) of Selected CAS Characteristics | Rating of Intervention Effectiveness | Fisher’s exact test | |||
|---|---|---|---|---|---|
| Learning | Self-Organization | Not Effective (n = 28) | Effective (n = 18) | Percent Effective | p = 0.005 |
| 0 | 0 | 4 | 2 | 33% | |
| 1 | 0 | 7 | 1 | 12% | |
| 0 | 1 | 8 | 1 | 11% | |
| 1 | 1 | 9 | 14 | 61% | |
When scores for learning and self-organization were combined, we identified a significant relationship among the variables. Interventions rated as effective were significantly more likely to have both characteristics of learning and self-organization (61%) than interventions rated as having no effect (39%; p = 0.005).
Discussion
We assessed whether care transition interventions whose design was congruent with CAS characteristics were more likely to report reduction in early readmissions. We found that nearly all the interventions assessed contained elements reflecting the 3 CAS characteristics of interconnections, affordances and processes, and none of the interventions displayed coevolution or emergence. The CAS characteristics that were most inconsistently reflected in our group of included studies were learning and self-organization. When both of these characteristics were present, interventions were associated with significantly fewer readmissions.
These results complement those reported by Leppin et al.’s work, in which early hospital readmission interventions were analyzed using the cumulative complexity model framework [3]. Their review included 42 trials compared to our 46, nine of which we shared in common. At least five of their included trials would have been excluded from ours because they were conducted on surgical patients. Leppin et al.’s analysis identified that interventions that were more complex (defined as involving more people or components), and those that increased patient capacity for self-care, were more likely to be effective. While that framework appears to share some similarities to CAS (e.g. attention to feedback loops, emergence), it focuses on workload-capacity imbalances and patient complexity, and considers intervention complexity in terms of component parts rather than their impact on characteristics of the complex systems in which the interventions are applied [72]. Whereas Leppin et al’s work was directed toward the intervention components, our CAS-grounded work was more focused on the interdependencies among the components in the systems of intervention. It is possible that their findings regarding self-care are related to learning, and that interventions with more components might be more likely to change interdependencies or self-organization. Future work might look at how the two approaches could be synthesized to enhance our understanding of applying complex interventions in complex adaptive systems.
Our findings have some important differences from our previous work examining the relationships between interventions’ congruence with CAS characteristics and outcomes in two complex chronic diseases: diabetes and chronic heart failure. In the case of type 2 diabetes interventions [14], interconnections and co-evolution were positively associated with outcomes. In our present analysis, 96% of the interventions changed interconnections, typically through approaches such as post-discharge calls or novel handoff practices. The fact that most of the interventions were designed to change the way people interacted with each other but were associated with varied results suggests that interconnections alone were not sufficient for improving outcomes. Additionally, in this group of studies, most of the changes in interaction patterns focused on providers (e.g., patient-provider, provider-provider). Changing other types of interconnections (e.g. between patients and their family caregivers) might influence different aspects of care delivery that is highly dependent on patient and family actions.
Similar to our current findings, in our review of chronic heart failure interventions [15], learning, self-organization, and co-evolution were significantly related to intervention effectiveness. In our analysis of care transition interventions, learning alone was not significantly associated with effective outcomes; when combined with self-organization, its association on readmissions was significant. This finding suggests that learning might be necessary to consider when trying to decrease readmissions, but perhaps is not sufficient. Returning home after a hospital stay involves many life changes, not all which can be anticipated and prepared for through patient education. As in the case of interconnections, different types of learning might also need to be distinguished to determine which approaches are more effective.
Care transitions may lead to a higher degree of uncertainty for patients and providers than other aspects of care delivery, including chronic disease management. After hospitalization, patients may experience medical, functional, social, and spiritual changes. While the interventions we studied made changes to the clinical or healthcare system, they frequently did not address the home context to which patients were returning. Learning and self-organization may be particularly important in this situation as they may help patients effectively respond to problems that might arise after they have returned home, reducing their likelihood of readmission. For example, interventions that include an aspect of patient education (like teaching congestive heart failure patients to manage weight and adjust diuretics) may help patients to know what to expect and respond.
One commonality between our studies of diabetes, congestive heart failure, and care transitions is that, in each study, interventions that had an adaptive element were more successful, whether it be through allowing local self-organization among individuals in the system, or recognizing that implementation is an evolutionary process that requires change over time. We found few descriptions of how interventions were modified or adapted over time, and no examples of co-evolution in the interventions we reviewed. This may spring from a desire for intervention fidelity, or typical word count limitations in the medical literature. Our findings across our three studies speak to the importance of the need for adaptive approaches. The complex and dynamic nature of clinical systems, and of patients’ trajectories over time, speaks to the need for adaptive approaches in which individuals can better tailor the intervention and implementation strategy to the ways they have organized care over time. More details of these adaptive approaches (such as detailed protocol papers) should be reported in the literature regarding these interventions. Increased interest in adaptation in the implementation science literature (e.g., [73, 74]) is helping expose the importance of both carefully documenting modifications as they happen and understanding adaptations as important for intervention success.
Limitations
This project has several limitations. Our assessment of CAS characteristics was limited by the published descriptions of the interventions, which may be inadequate for understanding intervention context and adaptations. In addition, we defined CAS characteristics in broad terms, with each characteristic potentially encompassing an array of diverse intervention practices. Thus, many studies may appear similar in terms of the CAS characteristics, but the specifics of the interventions and the contexts in which they were implemented may contain important differences. For example, our definition of learning is both limited (e.g. interventions had to explicitly describe an educational component or learning, not inclusive of implicit learning that occurs during interpersonal interactions) and possibly overly expansive (e.g. does giving a patient a handout really count as learning?). Future research should consider how best to assess how learning occurs in complex healthcare interventions, particularly in the context of high uncertainty. Our dichotomous assessment of effectiveness was possibly also too generous, as any intervention could be scored as effective if at least one of the reported readmission outcomes was significant. Having a more nuanced classification scheme for study outcomes might have yielded different results.
The breadth of our dataset is both a strength and limitation. The articles reviewed are from a large span of time during which this literature evolved rapidly and expectations for the description of study methodology and intervention details changed significantly. Finally, our starting point was articles identified in a review of reviews, and we relied upon the original reviews to have assessed for methodological quality. Different systematic reviews used different methods for assessing quality. If we had started de novo with a search for all interventions addressing readmissions as an outcome, we may have identified additional studies.
Conclusion
Transitional care interventions with characteristics of complex adaptive systems, particularly learning and self-organization, are associated with a greater reduction in early readmissions. New study designs allowing for adaptation are needed to better address interventions in the complex clinical systems in which they are implemented.
Additional file
Intervention description. Characteristics of included studies of care transition interventions, as described in Penney, et al., Interventions to Reduce Readmissions: Can complex adaptive system theory explain the heterogeneity in effectiveness? A systematic review. (DOCX 45 kb)
Complexity scoring. Ratings of eligible studies by complex adaptive system characteristics (CAS), interdependencies, and project success, as described in Penney, et al., Interventions to Reduce Readmissions: Can complex adaptive system theory explain the heterogeneity in effectiveness? A systematic review. (DOCX 44 kb)
Acknowledgements
Not applicable
Funding
Not applicable
Availability of data and materials
The data for this paper was derived from published manuscripts, each of which is referenced here. The dataset supporting the conclusions of this article is included within the article’s additional files.
Abbreviations
- CAS
Complex adaptive systems
Authors’ contributions
LSP and JP designed the project. LSP and MN downloaded the articles, created the review tables, managed the data through the independent reviews, and conducted initial data analysis. LSP, MN, LKL, HJL, PHN, EF, and JP contributed to article review and scoring, as well as manuscript preparation. LSP drafted the manuscript, and coordinated and submitted the revisions. LSP, MN, LKL, HJL, PHN, EPF, and JP have read and approved this manuscript.
Authors’ information
Not applicable
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors have no competing interests to declare.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lauren S. Penney, Email: Lauren.Penney@va.gov
Musarrat Nahid, Email: nahid@uthscsa.edu.
Luci K. Leykum, Email: leykum@uthscsa.edu
Holly Jordan Lanham, Email: Lanham@uthscsa.edu.
Polly H. Noël, Email: noelp@uthscsa.edu
Erin P. Finley, Email: finleye@uthscsa.edu
Jacqueline Pugh, Email: Jacqueline.Pugh@va.gov.
References
- 1.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day Rehospitalization: a systematic review. Ann Intern Med. 2011;155:520. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 2.Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
- 3.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kansagara D, Chiovaro JC, Kagen D, Jencks S, Rhyne K, O’Neil M, et al. Transitions of care from hospital to home: a summary of systematic evidence reviews and recommendations for transitional care in the veterans health administration: Department of Veterans Affairs; 2015. https://www.ncbi.nlm.nih.gov/books/NBK311349/. [PubMed]
- 5.Naylor Mary D., Shaid Elizabeth C., Carpenter Deborah, Gass Brianna, Levine Carol, Li Jing, Malley Ann, McCauley Kathleen, Nguyen Huong Q., Watson Heather, Brock Jane, Mittman Brian, Jack Brian, Mitchell Suzanne, Callicoatte Becky, Schall John, Williams Mark V. Components of Comprehensive and Effective Transitional Care. Journal of the American Geriatrics Society. 2017;65(6):1119–1125. doi: 10.1111/jgs.14782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson RA, Issel LM, McDaniel RR. Nursing homes as complex adaptive systems: relationship between management practice and resident outcomes. Nurs Res. 2003;52:12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Begun JW, Zimmerman B, Dooley K. Health care organizations as complex adaptive systems. In: Mick SS, Wyttenbach ME, editors. Advances in health care organization theory. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- 8.Plsek P. Redesigning health care with insights from the science of complex adaptive systems. Crossing Qual Chasm New Health Syst 21st Century. 2001:309–22.
- 9.McKenna K, Leykum LK, RR MD. The role of improvising in patient care. Health Care Manage Rev. 2013;38:1–8. doi: 10.1097/HMR.0b013e31823ea9c7. [DOI] [PubMed] [Google Scholar]
- 10.Leykum LK, Lanham HJ, Pugh JA, Parchman M, Anderson RA, Crabtree BF, et al. Manifestations and implications of uncertainty for improving healthcare systems: an analysis of observational and interventional studies grounded in complexity science. Implement Sci. 2014;9. 10.1186/s13012-014-0165-1. [DOI] [PMC free article] [PubMed]
- 11.Lanham HJ, Leykum LK, Taylor BS, McCannon CJ, Lindberg C, Lester RT. How complexity science can inform scale-up and spread in health care: understanding the role of self-organization in variation across local contexts. Soc Sci Med. 2013;93:194–202. doi: 10.1016/j.socscimed.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 12.Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, et al. Making sense of complexity in context and implementation: the context and implementation of complex interventions (CICI) framework. Implement Sci. 2017;12. 10.1186/s13012-017-0552-5. [DOI] [PMC free article] [PubMed]
- 13.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. 2015;10:21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leykum LK, Pugh J, Lawrence V, Parchman M, Noël PH, Cornell J, et al. Organizational interventions employing principles of complexity science have improved outcomes for patients with type II diabetes. Implement Sci IS. 2007;2:28. doi: 10.1186/1748-5908-2-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leykum LK, Parchman M, Pugh J, Lawrence V, Noël PH, McDaniel RR. The importance of organizational characteristics for improving outcomes in patients with chronic disease: a systematic review of congestive heart failure. Implement Sci. 2010;5:66. doi: 10.1186/1748-5908-5-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kagedan DJ, Ahmed M, Devitt KS, Wei AC. Enhanced recovery after pancreatic surgery: a systematic review of the evidence. HPB. 2015;17:11–16. doi: 10.1111/hpb.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta CR, Patel NR. A network algorithm for performing Fisher’s exact test in rxc contingency tables. J Am Stat Assoc. 1983;78:427–434. [Google Scholar]
- 18.StataCorp . Stata Statistical Software: Release 14. College Station: StataCorp LP; 2015. [Google Scholar]
- 19.Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of “hospital in the home.”. Med J Aust. 2012;197:512–519. doi: 10.5694/mja12.10480. [DOI] [PubMed] [Google Scholar]
- 20.Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for Postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915–921. doi: 10.1016/j.amjmed.2012.01.035. [DOI] [PubMed] [Google Scholar]
- 21.Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553. doi: 10.1136/bmj.d6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huntley AL, Thomas R, Mann M, Huws D, Elwyn G, Paranjothy S, et al. Is case management effective in reducing the risk of unplanned hospital admissions for older people? A systematic review and meta-analysis. Fam Pract. 2013;30:266–275. doi: 10.1093/fampra/cms081. [DOI] [PubMed] [Google Scholar]
- 23.Jackson GL, Powers BJ, Chatterjee R, Prvu Bettger J, Kemper AR, Hasselblad V, et al. The patient-centered medical home: a systematic review. Ann Intern Med. 2013;158:169. doi: 10.7326/0003-4819-158-3-201302050-00579. [DOI] [PubMed] [Google Scholar]
- 24.Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5_Part_2):397. doi: 10.7326/0003-4819-158-5-201303051-00006. [DOI] [PubMed] [Google Scholar]
- 25.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006. 10.1002/14651858.CD004510.pub3. [DOI] [PMC free article] [PubMed]
- 26.Pandor A, Gomersall T, Stevens JW, Wang J, Al-Mohammad A, Bakhai A, et al. Remote monitoring after recent hospital discharge in patients with heart failure: a systematic review and network meta-analysis. Heart. 2013;99:1717–1726. doi: 10.1136/heartjnl-2013-303811. [DOI] [PubMed] [Google Scholar]
- 27.Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. In: The Cochrane collaboration, editor. Cochrane database of systematic reviews. Chichester: Wiley; 2013. [DOI] [PubMed] [Google Scholar]
- 28.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23:1228–1233. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith DM, Weinberger M, Katz BP, Moore PS. Postdischarge care and readmissions. Med Care. 1988;26:699–708. doi: 10.1097/00005650-198807000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Fitzgerald JF. A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154:1721. doi: 10.1001/archinte.1994.00420150095009. [DOI] [PubMed] [Google Scholar]
- 31.Kircher TTJ, Wormstall H, Muller PH, Schwarzler F, Buchkremer G, Wild K, et al. A randomised trial of a geriatric evaluation and management consultation services in frail hospitalised patients. Age Ageing. 2006;36:36–42. doi: 10.1093/ageing/afl102. [DOI] [PubMed] [Google Scholar]
- 32.Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of Care in a Hospital Medical Unit Especially Designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 33.Reuben DB, Borok GM, Wolde-Tsadik G, Ershoff DH, Fishman LK, Ambrosini VL, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995;332:1345–1350. doi: 10.1056/NEJM199505183322007. [DOI] [PubMed] [Google Scholar]
- 34.White S, Powers J, Knight J, Harrell D, Varnell L, Vaughn C, et al. Effectiveness of an inpatient geriatric service in a university hospital. J Tenn Med Assoc. 1994;87:425–428. [PubMed] [Google Scholar]
- 35.Asplund K, Gustafson Y, Jacobsson C, Bucht G, Wahlin A, Peterson J, et al. Geriatric-based versus general wards for older acute medical patients: a randomized comparison of outcomes and use of resources. J Am Geriatr Soc. 2000;48:1381–1388. doi: 10.1111/j.1532-5415.2000.tb02626.x. [DOI] [PubMed] [Google Scholar]
- 36.Winograd CH. A negative trial of inpatient geriatric consultation: lessons learned and recommendations for future research. Arch Intern Med. 1993;153:2017. doi: 10.1001/archinte.1993.00410170101010. [DOI] [PubMed] [Google Scholar]
- 37.Thomas DR, Brahan R, Haywood BP. Inpatient community-based geriatric assessment reduces subsequent mortality. J Am Geriatr Soc. 1993;41:101–104. doi: 10.1111/j.1532-5415.1993.tb02040.x. [DOI] [PubMed] [Google Scholar]
- 38.Nikolaus T. A randomized trial of comprehensive geriatric assessment and home intervention in the care of hospitalized patients. Age Ageing. 1999;28:543–550. doi: 10.1093/ageing/28.6.543. [DOI] [PubMed] [Google Scholar]
- 39.Lim WK, Lambert SF, Gray LC. Effectiveness of case management and post-acute services in older people after hospital discharge. Med J Aust. 2003;178:262–266. doi: 10.5694/j.1326-5377.2003.tb05191.x. [DOI] [PubMed] [Google Scholar]
- 40.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 41.Avlund K, Jepsen E, Vass M, Lundemark H. Effects of comprehensive follow-up home visits after hospitalization on functional ability and readmissions among old patients. A randomized controlled study. Scand J Occup Ther. 2002;9:17–22. doi: 10.1080/110381202753505827. [DOI] [Google Scholar]
- 42.Melin AL, Bygren LO. Efficacy of the rehabilitation of elderly primary health care patients after short-stay hospital treatment. Med Care. 1992;30:1004–1015. doi: 10.1097/00005650-199211000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Jack BW. A reengineered hospital discharge program to decrease Rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tranmer JE, Parry MJE. Enhancing postoperative recovery of cardiac surgery patients: a randomized clinical trial of an advanced practice nursing intervention. West J Nurs Res. 2004;26:515–532. doi: 10.1177/0193945904265690. [DOI] [PubMed] [Google Scholar]
- 45.Beckie T. A supportive-educative telephone program: impact on knowledge and anxiety after coronary artery bypass graft surgery. Heart Lung J Crit Care. 1989;18:46–55. [PubMed] [Google Scholar]
- 46.Bostrom J, Caldwell J, McGuire K, Everson D. Telephone follow-up after discharge from the hospital: does it make a difference? Appl Nurs Res. 1996;9:47–52. doi: 10.1016/S0897-1897(96)80402-2. [DOI] [PubMed] [Google Scholar]
- 47.Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001;111:26–30. doi: 10.1016/S0002-9343(01)00966-4. [DOI] [PubMed] [Google Scholar]
- 48.Jerant AF, Azari R, Nesbitt TS. Reducing the cost of frequent hospital admissions for congestive heart failure: a randomized trial of a home telecare intervention. Med Care. 2001;39 https://insights.ovid.com/pubmed?pmid=11606877. [DOI] [PubMed]
- 49.Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, et al. Effect of home-based Telemonitoring using Mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res. 2009;11:e34. doi: 10.2196/jmir.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL, et al. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed E-Health. 2008;14:753–761. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 51.Capomolla S, Pinna G, Larovere M, Maestri R, Ceresa M, Ferrari M, et al. Heart failure case disease management program: a pilot study of home telemonitoring versus usual care. Eur Heart J Suppl. 2004;6:F91–F98. doi: 10.1016/j.ehjsup.2004.09.011. [DOI] [Google Scholar]
- 52.Laramee AS, Levinsky SK, Sargent J, Ross R, Callas P. Case Management in a Heterogeneous Congestive Heart Failure Population: a randomized controlled trial. Arch Intern Med. 2003;163:809. doi: 10.1001/archinte.163.7.809. [DOI] [PubMed] [Google Scholar]
- 53.Woodend AK, Sherrard H, Fraser M, Stuewe L, Cheung T, Struthers C. Telehome monitoring in patients with cardiac disease who are at high risk of readmission. Heart Lung J Acute Crit Care. 2008;37:36–45. doi: 10.1016/j.hrtlng.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 54.Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162:705. doi: 10.1001/archinte.162.6.705. [DOI] [PubMed] [Google Scholar]
- 55.Barth V. A nurse-managed discharge program for congestive heart failure patients: outcomes and costs. Home Health Care Manag Pract. 2001;13:436–443. doi: 10.1177/108482230101300604. [DOI] [Google Scholar]
- 56.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, et al. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dar O, Riley J, Chapman C, Dubrey SW, Morris S, Rosen SD, et al. A randomized trial of home telemonitoring in a typical elderly heart failure population in north West London: results of the home-HF study. Eur J Heart Fail. 2009;11:319–325. doi: 10.1093/eurjhf/hfn050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.DeBusk RF, Miller NH, Parker KM, Bandura A, Kraemer HC, Cher DJ, et al. Care management for low-risk patients with heart failure: a randomized, controlled trial. Ann Intern Med. 2004;141:606. doi: 10.7326/0003-4819-141-8-200410190-00008. [DOI] [PubMed] [Google Scholar]
- 59.Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, Elegeert I, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of heart failure) study. Eur J Heart Fail. 2012;14:333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 60.Goldberg LR, Piette JD, Walsh MN, Frank TA, Jaski BE, Smith AL, et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the weight monitoring in heart failure (WHARF) trial. Am Heart J. 2003;146:705–712. doi: 10.1016/S0002-8703(03)00393-4. [DOI] [PubMed] [Google Scholar]
- 61.Kulshreshtha A, Kvedar JC, Goyal A, Halpern EF, Watson AJ. Use of remote monitoring to improve outcomes in patients with heart failure: a pilot trial. Int J Telemed Appl. 2010;2010:1–7. doi: 10.1155/2010/870959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cleland JGF, Louis AA, Rigby AS, Janssens U, Balk AHMM. Noninvasive home Telemonitoring for patients with heart failure at high risk of recurrent admission and death. J Am Coll Cardiol. 2005;45:1654–1664. doi: 10.1016/j.jacc.2005.01.050. [DOI] [PubMed] [Google Scholar]
- 63.Tsuyuki RT, Fradette M, Johnson JA, Bungard TJ, Eurich DT, Ashton T, et al. A multicenter disease management program for hospitalized patients with heart failure. J Card Fail. 2004;10:473–480. doi: 10.1016/j.cardfail.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 64.Angermann CE, Stork S, Gelbrich G, Faller H, Jahns R, Frantz S, et al. Mode of action and effects of standardized collaborative disease management on mortality and morbidity in patients with systolic heart failure: the interdisciplinary network for heart failure (INH) study. Circ Heart Fail. 2012;5:25–35. doi: 10.1161/CIRCHEARTFAILURE.111.962969. [DOI] [PubMed] [Google Scholar]
- 65.Antonicelli R, Testarmata P, Spazzafumo L, Gagliardi C, Bilo G, Valentini M, et al. Impact of telemonitoring at home on the management of elderly patients with congestive heart failure. J Telemed Telecare. 2008;14:300–305. doi: 10.1258/jtt.2008.071213. [DOI] [PubMed] [Google Scholar]
- 66.Rainville EC. Impact of pharmacist interventions on hospital readmissions for heart failure. Am J Health Syst Pharm. 1999;56:1339–1342. [PubMed] [Google Scholar]
- 67.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334:1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 68.Evans RL, Hendricks RD. Evaluating hospital discharge planning: a randomized clinical trial. Med Care. 1993;31:358. doi: 10.1097/00005650-199304000-00007. [DOI] [PubMed] [Google Scholar]
- 69.Naylor M. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann Intern Med. 1994;120:999. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 70.Shaw H, Mackie CA, Sharkie I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int J Pharm Pract. 2000;8:144–153. doi: 10.1111/j.2042-7174.2000.tb00999.x. [DOI] [Google Scholar]
- 71.Nazareth I, Burton A, Shulman S, Smith P, Haines A, Timberall H. A pharmacy discharge plan for hospitalized elderly patients—a randomized controlled trial. Age Ageing. 2001;30:33–40. doi: 10.1093/ageing/30.1.33. [DOI] [PubMed] [Google Scholar]
- 72.Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012;65:1041–1051. doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 73.Chambers David A., Norton Wynne E. The Adaptome. American Journal of Preventive Medicine. 2016;51(4):S124–S131. doi: 10.1016/j.amepre.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implement Sci. 2013;8. 10.1186/1748-5908-8-65. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intervention description. Characteristics of included studies of care transition interventions, as described in Penney, et al., Interventions to Reduce Readmissions: Can complex adaptive system theory explain the heterogeneity in effectiveness? A systematic review. (DOCX 45 kb)
Complexity scoring. Ratings of eligible studies by complex adaptive system characteristics (CAS), interdependencies, and project success, as described in Penney, et al., Interventions to Reduce Readmissions: Can complex adaptive system theory explain the heterogeneity in effectiveness? A systematic review. (DOCX 44 kb)
Data Availability Statement
The data for this paper was derived from published manuscripts, each of which is referenced here. The dataset supporting the conclusions of this article is included within the article’s additional files.



