Abstract
Objective
This study was designed to verify the association between dementia and mortality in the elderly undergoing hip fracture surgery, and assessed the mortality of patients with dementia after hip fracture surgery.
Material and methods
PubMed, Embase, and Web of Science were searched until April, 2018 without language restrictions. Two reviewers selected related studies, assessed study quality, and extracted data independently. Risk ratios (RRs) with 95% confidence intervals (CI) were derived using random-effects model throughout all analyses. The endpoints included 30-day, 6-month, 1-year, and more than 1-year mortality. This meta-analysis was performed following PRISMA statement and carried out by using stata14.0 software.
Results
Dementia significantly increased postoperative mortality of patients suffered from hip fracture in 30-day [RR = 1.57, 95% CI (1.29, 1.90), P<0.00], 6-month [RR = 1.97, 95% CI (1.47, 2.63), P<0.00], 1-year [RR = 1.77, 95% CI (1.54, 2.04), P<0.00], and more than 1-year follow up [RR = 1.60, 95% CI (1.30, 1.96), P<0.00] respectively. The mortality of dementia patients after hip fracture surgery in 30-day [ES = 12%, 95% CI (8%, 15%)], 6-month [ES = 32%, 95% CI (17%, 48%)], 1-year [ES = 39%, 95% CI (35%, 43%)], and more than 1-year follow up [ES = 45%, 95% CI (32%, 58%)].
Conclusions
Our meta-analysis demonstrated that the mortality of patients with dementia suffered from hip fracture surgery is 12%, 32%, 39%, and 45%, and dementia increased 1.57, 1.97, 1.77, and 1.60-fold mortality in patients undergoing hip fracture surgery in 30-day, 6-month, 1-year, and more than 1-year follow up respectively.
Keywords: Hip fracture, Mortality, Dementia, Meta-analysis
Introduction
Hip fractures are being paid more attention due to higher morbidity and mortality. These patients usually have poor body compensatory capacity and comorbidities, such as dementia. Dementia is a syndrome characterized by persistent impairment in cognitive function or behavioral abnormalities. Due to the progress of aging society, dementia prevalence increases exponentially with age, it is estimated that the number of patients with dementia may reach 65.7 million in 2030 and 115.4 million in 2050 [1].
Dementia is not as fatal as deep vein thrombosis or pulmonary embolism in the short term, so it did not cause clinicians to pay enough attention, and it is unclear that the mortality of patients with dementia suffered from hip fracture surgery. Therefore, we performed a meta-analysis based on plenty of previous achievements in current research, to identify the effects of dementia on postoperative mortality of hip fracture, and the incidence of death in patients with dementia undergoing hip fracture surgery in 30 days, 6 months, 1 year, and more than 1 year follow up, and provided more convincing evidences for clinicians.
Materials and methods
We carried out this meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [2] and Cochrane Collaboration guidelines strictly [3].
Search strategy
We searched PubMed, Embase, and Web of Science until April, 2018, without language restrictions. In addition, the references of the included studies were manual searched to identify any additional articles. The following keywords were adopted in the database search: “hip fracture,” “mortality,” and “dementia.” The Boolean operators were used to combine them.
Study selection and eligibility criteria
The inclusion criteria are as follows: (1) studies examined the relationship between dementia and mortality among elderly patients undergoing hip fracture surgery; (2) the sample size was more than 200; (3) study designs were cohort study; (4) the mean age is greater than 60 years. The exclusion criteria are as follows: (1) other types of fractures included; (2) studies provided insufficient data; (3) case report, review, commentary, and study just included an abstract; (4) dementia with other psychiatric disorders.
Data extraction
Two reviewers (JZ B and P Z) independently extracted the following information from each study: first author, year of publication, country, study design, sample size, mean age, diagnostic criteria for dementia, and duration of follow-up (in-hospital, perioperative setting, 30-day, 6-month, 1-year and more than 1-year). Any discrepancies were resolved following discussion. All extracted data were entered into a predefined standardized Excel (Microsoft Corporation, USA) file carefully.
Quality assessment
We evaluated the quality of studies by Newcastle-Ottawa Scale (NOS), which is a risk of bias assessment tool for observational studies [4]. This scale contains a number of answers per question ranging from two to five. High-quality responses earn a star, totaling up to nine stars. We set scores of 0–3, 4–6, and 7–9 for low, moderate, and high quality of studies, respectively [5].
Statistical analysis
Statistical analyses were performed by using STATA 14.0 (StataCorp LP). The association between dementia and mortality was described as risk ratios (RR) with 95% confidence intervals (CI) by using random models. P ≤ 0.05 was regarded as statistically significant. Statistical heterogeneity was assessed by the Cochran Q test and quantified by the I2 statistic [6], and an I2 value greater than 50% indicates significant heterogeneity. When significant heterogeneity existed, heterogeneity analysis would be conducted to make a further explanation. We divided the follow-up time into four timepoints: 30-day, 6-month, 1-year, and more than 1-year follow-up. We classified the in-hospital and perioperative mortality as 30-day mortality.
Results
Study characteristics and quality assessment
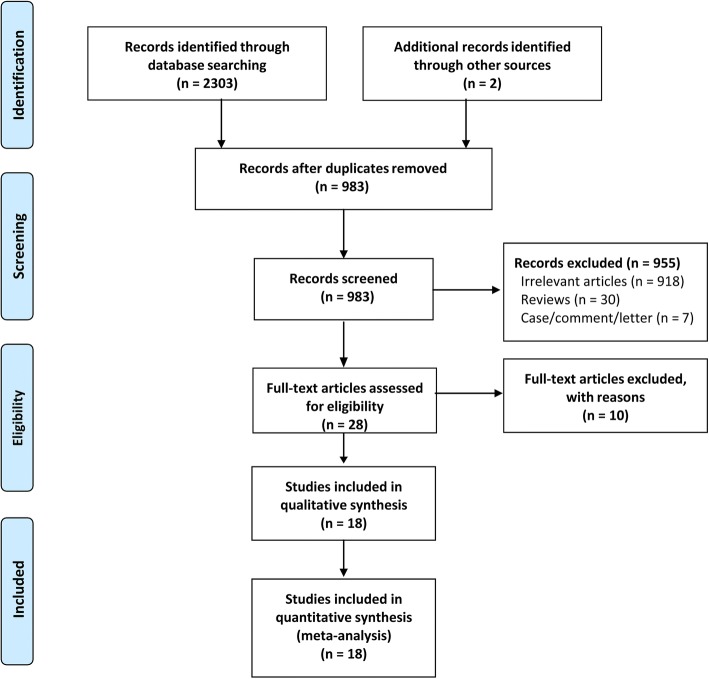
Two reviewers (JZ B and P Z) independently undertook the searches. Endnote X8 (version 18.0.0.10063) was used to remove duplicate studies. Additionally, we deleted irrelevant articles through the full text. Finally, 18 articles were included. The study selection process was shown in Fig. 1, and the main characteristics of the included trials were summarized in Table 1. Fourteen of 18 were prospective cohort studies [7–20], and four were retrospective cohort studies [21–24]. These studies enrolling 295,285 subjects were published between 2000 and 2018, with a sample size ranging from 272 to 134,144. The average scores of the quality assessment were 7.3 (range, 7–9). Details of the quality assessment were available in Table 2.
Fig. 1.
The flow chart of studies selecting
Table 1.
Characteristics of the included studies
| Studies | Country/design | Sample size | Mean age (years) | Follow-up (months) | 30-day/6-month mortality | 1-year/>1-year mortality |
|---|---|---|---|---|---|---|
| Holmes 2000 [8] | UK/PC | 731 | 82.1 | 24 | 6 m D: 118/294 ND:93/409 | 1y D: 143/294 ND:121/409 > 1y D: 181/294 ND:159/409 |
| Hannan 2001 [11] | USA/PC | 571 | ≥70* | 6 | 6 m D: 34/141 ND:43/430 | NR |
| Mortimore 2008 [9] | USA/PC | 674 | 81.1 | 24 | NR | > 1y D: 49/120 ND:120/554 |
| Pretto 2010 [10] | Switzerland/PC | 272 | 84 | 12 | NR | 1y D:33/91 ND:24/172 |
| Hershkovitz 2010 [12] | Israel /PC | 376 | 82.3 | 24 | NR | > 1y D: 59/237 ND:9/137 |
| Julieb 2010 [14] | Norway/PC | 331 | 85.1 | 12 | NR | 1y D: 14/50 ND:14/138 |
| Frost 2011 [7] | Australia/ PC | 1504 | 80.2 | 1 | 30d D: 20/214 ND:63/1290 | NR |
| Khan 2013 [15] | UK/PC | 467 | 80.2 | 1 | 30d D: 14/110 ND:21/357 | NR |
| Kim 2013 [24] | Korea/RC | 506 | 77.2 | 1 | 30d D: 0/40 ND:11/466 | NR |
| Lee 2013 [16] | Korea/PC | 790 | 77.8 | 72 | NR | > 1y D: 51/78 ND:321/712 |
| Cenzer 2016 [23] | USA/RC | 857 | 84 | 12 | NR | 1y D: 49/133 ND:186/724 |
| Tolppanen 2016 [20] | Finland/PC | 134,144 | 79.9 | 36 | NR | > 1y D: 22240/67072 ND:17771/67072 |
| Ruggiero 2017 [17] | Italy/PC | 514 | 83.1 | 12 | NR | 1y D: 20/102 ND:56/412 |
| Reig 2017 [18] | Spain/PC | 331 | 83 | 1 | 30d D: 9/92 ND:29/239 | NR |
| Sheikh 2017 [19] | UK/PC | 1356 | 81.4 | 1 | 30d D: 9/97 ND:109/1259 | NR |
| Karres 2018 [21] | Netherlands/RC | 1050 | 80 | 1 | 30d D: 15/131 ND:49/615 | NR |
| Mitchell 2017 [22] | Australia /RC | 27,888 | ≥ 65 | 12 | NR | 1y D: 2970/7132 ND:3977/19219 |
| Jantzen 2018 [13] | Denmark /PC | 122,923 | 80.6 | 12 | 30d D: 849/5230 ND:11372/117693 | 1y D:2334/5230 ND:32048/117693 |
PC prospective cohort study, RC retrospective cohort study, D dementia, ND non-dementia, NR no report; *calculated result
Table 2.
Methodological quality assessment of included studies by Newcastle–Ottawa scales
| Study | Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Exposed Cohort | Nonexposed Cohort | Ascertainment of exposure | Outcome of interest | Assessment of outcome | Length of follow-up | Adequacy of follow-up | Total score | ||
| Holmes et al. | * | * | * | * | * | * | * | * | 8 |
| Hannan et al. | * | * | * | * | * | * | – | * | 7 |
| Mortimore et al. | * | * | * | * | * | * | * | * | 8 |
| Pretto et al. | * | * | * | * | * | * | – | * | 7 |
| Julieb et al. | * | * | * | * | * | * | – | * | 7 |
| Hershkovitz et al | * | * | * | * | * | * | * | * | 8 |
| Frost et al. | * | * | * | * | * | * | – | * | 7 |
| Lee et al. | * | * | * | * | * | * | * | * | 8 |
| Khan et al. | * | * | * | * | * | * | – | * | 7 |
| Kim et al. | * | * | * | * | * | * | – | * | 7 |
| Cenzer et al. | * | * | * | * | * | * | – | * | 7 |
| Tolppanen et al. | * | * | * | * | ** | * | * | * | 9 |
| Ruggiero et al. | * | * | * | * | * | * | – | * | 7 |
| Reig et al. | * | * | * | * | * | * | – | * | 7 |
| Sheikh et al. | * | * | * | * | * | * | – | * | 7 |
| Karres et al. | * | * | * | * | * | * | – | * | 7 |
| Mitchell et al. | * | * | * | * | * | * | – | * | 7 |
| Jantzen et al. | * | * | * | * | * | * | – | * | 7 |
Single asterisk indicates 1 score; double asterisk indicates 2 scores, and dash indicates 0 scores
Thirty-day mortality
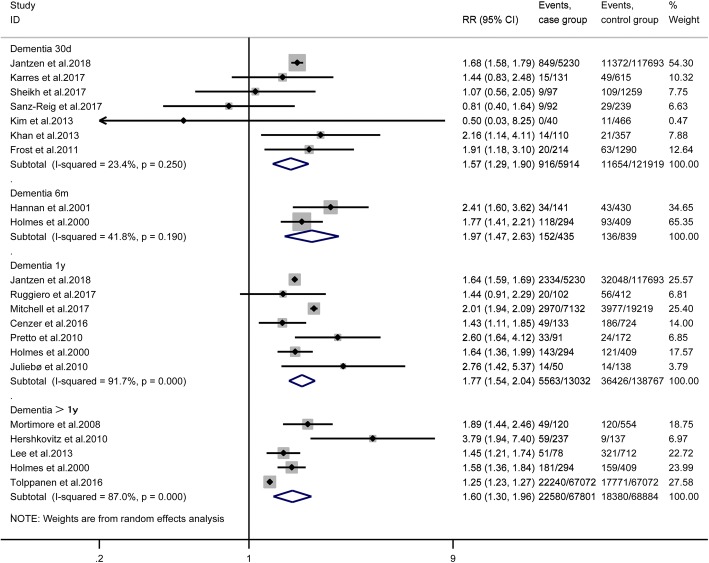
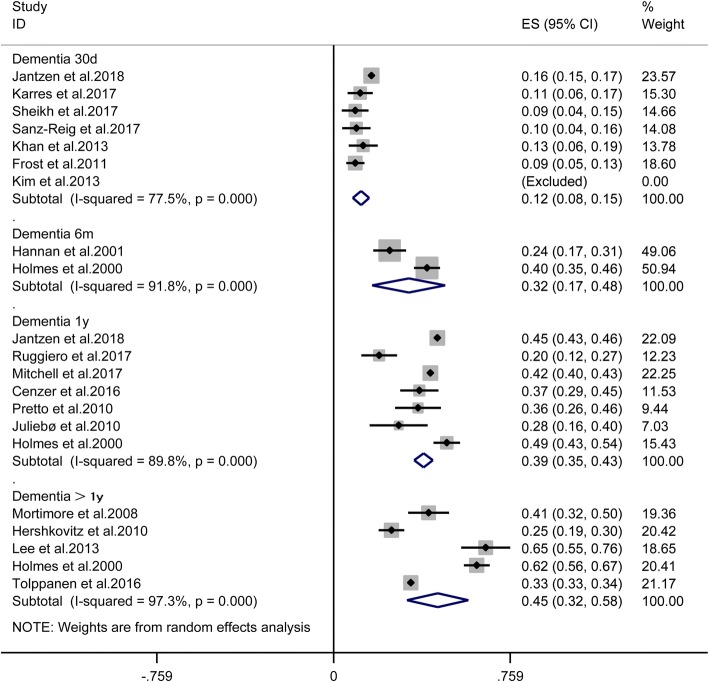
Seven studies [7, 13, 15, 18, 19, 21, 24] provided available data, and the pooled results suggested that dementia significantly increased the mortality of patients undergoing hip fracture surgery [RR = 1.57, 95% CI (1.29, 1.90), P < 0.001, I2 = 23.4%; Fig. 2], and the mortality of patients with dementia suffered from hip fracture surgery [ES = 12%, 95% CI (8%, 15%), I2 = 77.5%; Fig. 3].
Fig. 2.
The effect of dementia on the mortality of patients after hip fracture surgery
Fig. 3.
The mortality of dementia patients after hip fracture surgery
Six-month mortality
Only two studies [8, 11] provided available data in 6-month follow-up. The pooled outcomes suggested that dementia significantly increases the mortality of patients after hip fracture surgery [RR = 1.97, 95% CI (1.47, 2.63), P > 0.001, I2 = 41.8%; Fig. 2], and the mortality of the dementia patients suffered from hip fracture surgery [ES = 32%, 95% CI (17%, 48%), I2 = 91.8%; Fig. 3].
One-year mortality
Seven studies [8, 10, 13, 14, 17, 22, 23] provided available data, and the pooled results suggested that dementia significantly increases the mortality of patients undergoing hip fracture surgery in 1-year follow up[RR = 1.77, 95% CI (1.54, 2.04), P < 0.001, I2 = 91.7%; Fig. 2], and the mortality of the dementia patients suffered from hip fracture surgery [ES = 39%, 95% CI (35%, 43%), I2 = 89.8%; Fig. 3].
More than one-year mortality
Five studies [8, 9, 12, 16, 20] reported more than 1-year mortality. The pooled outcomes suggested that dementia significantly increases the mortality of patients undergoing hip fracture surgery [RR = 1.60, 95% CI (1.30, 1.96), P < 0.001, I2 = 87%; Fig. 2], and the mortality of the dementia patients suffered from hip fracture surgery [ES = 45%, 95% CI (32%, 58%), I2 = 97.3%; Fig. 3].
Discussion
Main findings
Our meta-analysis demonstrated that the mortality of patients with dementia suffered from hip fracture surgery is 12%, 32%, 39%, and 45%, and dementia increased 1.57, 1.97, 1.77, and 1.60-fold mortality in patients undergoing hip fracture surgery in 30-day, 6-month, 1-year, and more than 1-year follow-up. A previous meta-analysis included 75 studies, and involving 64,316 patients [25], the pooled outcomes demonstrated that the overall inpatient or 1 month mortality was 13.3%, 3 to 6 months was 15.8%, 1 year 24.5%, and 2 years 34.5% in generally patients, which mortality was significantly lower than patients with dementia who underwent hip fracture surgery.
Comparison with other studies
To the best of our knowledge, there are three meta-analyses that described risk factors for postoperative mortality after hip fracture surgery [25–27], which dementia is one of these risk factors. However, these meta-analyses included fewer literatures for the indicator of dementia, and inconsistent follow-up time made conclusions less convincing. Therefore, we performed an update meta-analysis to evaluate the effects of dementia on postoperative mortality of patients undergoing hip fracture surgery and the incidence of death in patients with dementia undergoing hip fracture surgery in 30 days, 6 months, 1 year, and more than 1 year follow-up.
Implications for clinical practice
Dementia has not received enough attention compared with deep vein thrombosis and pulmonary embolism in patients with hip fracture. However, our pooled results demonstrated that more than one third of people with dementia will die after hip fracture surgery in a 1-year follow-up and about one in two in more than 1-year follow-up. Patients with dementia usually have less activity and poor self-care ability, which increased postoperative complications, such as surgical site infection, urinary tract infection, and respiratory complications [28]. Therefore, orthopedists should attach great importance to this age-related disease, instead of just focusing on hip fracture problems. Besides, they should fully assess whether the dementia patients are suitable for surgical treatment after suffering from a hip fracture. Can surgical treatment improve the quality of life and prolong life span of patients, especially for patients with severe dementia? For patients with dementia who underwent hip fracture surgery, we should establish a multidisciplinary model of diagnosis and treatment to improve the postoperative outcomes [29]. Besides, nursing cares are necessary to prevent the adverse outcomes of dementia postoperatively [30], such as aspiration, pressure sore, deep vein thrombosis, and pneumonia. Further, rehabilitate exercises are needed to restore function as much as possible after discharge.
Call for future studies
Our results show that patients with dementia have very high mortality rates after undergoing hip fracture surgery. Mortality will be higher for patients with severe dementia. It is unclear whether surgical treatment could improve quality of life and prolong life-span of patients with severe dementia. Until recently, there is no relevant meta-analysis or clinical guidelines to elaborate on this issue. We recommend that future studies should focus on which one is better for the treatment of patients with severe dementia who suffered from hip fracture, surgery, or conservative treatment. Besides, clinical decision makers should formulate relevant clinical guidelines to guide clinicians in the treatment of patients with dementia suffered from hip fracture.
Heterogeneity analysis
The pooled results indicated that significant heterogeneity was found in some indicators. For the prevalence of death of patients with dementia after hip fracture surgery, (1) we conducted a sensitivity analysis through the deletion of Jantzen et al’s study [13], and the heterogeneity was reduced from 77.5 to 0.0% in 30-day mortality; (2) we excluded each study of the outcomes one at a time in 1-year mortality, but the heterogeneity was still very high. Unequal levels of regional medical care and significant sample size difference in the included studies may be the major sources of heterogeneity. For the effect of dementia on postoperative mortality, there was significant heterogeneity in 1-year mortality. The heterogeneity was reduced from 91.7 to 33.8% after the removal of Mitchell et al’s study [22]. Only two studies were included in 6-month mortality, which may be the main source of heterogeneity. In terms of more than 1-year mortality, the inconsistency of follow-up time and obvious sample size differences, which may be major sources of higher heterogeneity.
Strengths and limitations of this meta-analysis
The major strengths of this study were the following: (1) our study was restricted to the elderly dementia patients undergoing hip fracture surgery, which were higher homogeneous and selective; (2) we designed our meta-analysis into four timepoints: 30-day, 6-month, 1-year, and more than 1-year follow up, and follow-up time is consistent; (3) we calculated the mortality of patients with dementia suffered from hip fracture surgery.
Limitations of this meta-analysis must be considered. First, although the patients we included in the study were elderly patients, it is difficult to make the confounding variables among the studies exactly the same. Second, we did not classify dementia into mild, moderate, and severe dementia because no related data were available in the original studies. Third, there was a great difference in the sample size of the included studies, which may affect the accuracy of our results to some extent. Fourth, significant heterogeneity was found in some outcomes. Last, although we conducted a comprehensive search of literature, it was hard to rule out the existence of publication bias.
Conclusions
Our meta-analysis demonstrated that the mortality of people with dementia suffered from hip fracture surgery is 12%, 32%, 39%, and 45%, and dementia increased 1.57-, 1.97-, 1.77-, and 1.60-fold mortality in patients undergoing hip fracture surgery in 30-day, 6-month, 1-year, and more than 1-year follow-up. Future large-volume, well-designed studies, and the outcomes of multivariable analysis with extensive follow-up are awaited to confirm and update the findings of our analysis.
Acknowledgements
We thank the authors of the included studies for their helping.
Funding
This study was supported by the project foundation of Northern Jiangsu People’s Hospital: (yzucms201623), (fcjs201715); National Natural Science Foundation of China: (81772332)
Availability of data and materials
All data are fully available without restriction.
Abbreviations
- CI
Confidence interval
- D
Dementia
- ND
Non-dementia
- NOS
Newcastle-Ottawa Scale
- NR
No report
- PC
Prospective cohort study
- RC
Retrospective cohort study
- RR
Risk ratio
Authors’ contributions
JCW, YL, and JZB conceived of the design of the study. JZB and PZ participated in the literature search, study selection, data extraction, and quality assessment. XYL and ZPW performed the statistical analysis. JZB finished the manuscript. All authors read and approved the final manuscript.
Authors’ information
The author information can be found in the title page.
Ethics approval and consent to participate
All analyses were based on previously published studies; thus, no ethical approval and patient consent are required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jianzhong Bai, Email: 327265214@qq.com.
Pei Zhang, Email: 505557001@qq.com.
Xinyu Liang, Email: 595980334@qq.com.
Zhipeng Wu, Email: 2287288158@qq.com.
Jingcheng Wang, Phone: +86 13301456789, Email: wangjcyangzhou@163.com.
Yuan Liang, Phone: +86 18051063817, Email: 464156241@qq.com.
References
- 1.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75.e62. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Higgins J, Green S: Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. Cochrane Collab 2011. Available at: www.handbook.cochrane.org. Accessed 24 Apr 2016.
- 4.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 5.Gu WJ, Wu XD, Zhou Q, et al. Relationship between annualized case volume and mortality in sepsis: a dose-response meta-analysis. Anesthesiology. 2016;125(1):168–179. doi: 10.1097/ALN.0000000000001133. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 7.Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV. Risk factors for in-hospital post-hip fracture mortality. Bone. 2011;49(3):553–558. doi: 10.1016/j.bone.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Holmes J, House A. Psychiatric illness predicts poor outcome after surgery for hip fracture: a prospective cohort study. Psychol Med. 2000;30(4):921–929. doi: 10.1017/S0033291799002548. [DOI] [PubMed] [Google Scholar]
- 9.Mortimore E, Haselow D, Dolan M, et al. Amount of social contact and hip fracture mortality. J Am Geriatr Soc. 2008;56(6):1069–1074. doi: 10.1111/j.1532-5415.2008.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pretto M, Spirig R, Kaelin R, Muri-John V, Kressig RW, Suhm N. Outcomes of elderly hip fracture patients in the Swiss healthcare system: a survey prior to the implementation of DRGs and prior to the implementation ofa geriatric fracture Centre. Swiss Med Wkly. 2010;140:w13086. doi: 10.4414/smw.2010.13086. [DOI] [PubMed] [Google Scholar]
- 11.Hannan EL, Magaziner J, Wang JJ, et al. Mortality and locomotion 6 months after hospitalization for hip fracture - risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285(21):2736–2742. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 12.Hershkovitz A, Polatov I, Beloosesky Y, Brill S. Factors affecting mortality of frail hip-fractured elderly patients. Arch Gerontol Geriatr. 2010;51(2):113–116. doi: 10.1016/j.archger.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Jantzen Christopher, Madsen Christian M, Lauritzen Jes B, Jørgensen Henrik L. Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthopaedica. 2018;89(2):170–176. doi: 10.1080/17453674.2018.1428436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Juliebø V, Krogseth M, Skovlund E, Engedal K, Ranhoff AH, Wyller TB. Delirium is not associated with mortality in elderly hip fracture patients. Dement Geriatr Cogn Disord. 2010;30(2):112–120. doi: 10.1159/000318819. [DOI] [PubMed] [Google Scholar]
- 15.Khan MA, Hossain FS, Ahmed I, Muthukumar N, Mohsen A. Predictors of early mortality after hip fracture surgery. Int Orthop. 2013;37(11):2119–2124. doi: 10.1007/s00264-013-2068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SR, Ha YC, Kang H, Park YG, Nam KW, Kim SR. Morbidity and mortality in Jeju residents over 50-years of age with hip fracture with mean 6-year follow-up: a prospective cohort study. J Korean Med Sci. 2013;28(7):1089–1094. doi: 10.3346/jkms.2013.28.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruggiero C, Bonamassa L, Pelini L, et al. Early post-surgical cognitive dysfunction is a risk factor for mortality among hip fracture hospitalized older persons. Osteoporos Int. 2017;28(2):667–675. doi: 10.1007/s00198-016-3784-3. [DOI] [PubMed] [Google Scholar]
- 18.Sanz-Reig J, Salvador Marin J, Perez Alba JM, Ferrandez Martinez J, Orozco Beltran D, Martinez Lopez JF. Risk factors for in-hospital mortality following hip fracture. Rev Esp Cir Ortop Traumatol. 2017;61(4):209–215. doi: 10.1016/j.recot.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Sheikh HQ, Hossain FS, Aqil A, Akinbamijo B, Mushtaq V, Kapoor H. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg. 2017;9(1):10–18. doi: 10.4055/cios.2017.9.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tolppanen AM, Taipale H, Tanskanen A, Tiihonen J, Hartikainen S. Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer's disease - exposure-matched cohort study. BMC Geriatr. 2016;16(1):204. doi: 10.1186/s12877-016-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karres J, Kieviet N, Eerenberg JP, Vrouenraets BC. Predicting early mortality after hip fracture surgery: the hip fracture estimator of mortality Amsterdam. J Orthop Trauma. 2018;32(1):27–33. doi: 10.1097/BOT.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 22.Mitchell R, Harvey L, Brodaty H, Draper B, Close J. One-year mortality after hip fracture in older individuals: the effects of delirium and dementia. Arch Gerontol Geriatr. 2017;72:135–141. doi: 10.1016/j.archger.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 23.Cenzer IS, Tang V, Boscardin WJ, et al. One-year mortality after hip fracture: development and validation of a prognostic index. J Am Geriatr Soc. 2016;64(9):1863–1868. doi: 10.1111/jgs.14237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim SD, Park SJ, Lee DH, Jee DL. Risk factors of morbidity and mortality following hip fracture surgery. Korean J Anesthesiol. 2013;64(6):505–510. doi: 10.4097/kjae.2013.64.6.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–685. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 26.Norring-Agerskov D, Laulund AS, Lauritzen JB, et al. Metaanalysis of risk factors for mortality in patients with hip fracture. Dan Med J. 2013;60(8):A4675. [PubMed] [Google Scholar]
- 27.Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43(4):464–471. doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 28.Tsuda Y, Yasunaga H, Horiguchi H, Ogawa S, Kawano H, Tanaka S. Association between dementia and postoperative complications after hip fracture surgery in the elderly: analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg. 2015;135(11):1511–1517. doi: 10.1007/s00402-015-2321-8. [DOI] [PubMed] [Google Scholar]
- 29.Stenvall M, Berggren M, Lundstrom M, Gustafson Y, Olofsson B. A multidisciplinary intervention program improved the outcome after hip fracture for people with dementia--subgroup analyses of a randomized controlled trial. Arch Gerontol Geriatr. 2012;54(3):e284–e289. doi: 10.1016/j.archger.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 30.Kim SK, Park M. Effectiveness of person-centered care on people with dementia: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:381–397. doi: 10.2147/CIA.S117637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are fully available without restriction.