Abstract
Hyperkeratosis presents as thickened skin. It can be congenital or acquired. Typically, it affects the palms and soles; the distribution of epidermal involvement is either diffuse, focal, or punctate. Microscopically, the pathologic signature of hyperkeratosis is marked orthokeratosis of the stratum corneum. Topical treatments provide the mainstay of therapy for hyperkeratosis. These include keratolytics (such as urea, salicylic acid, and lactic acid) and retinoids; physical debridement, topical corticosteroids, and phototherapy (using topical psoralen and ultraviolet A phototherapy) are other local therapeutic modalities. Selenium is a non-metallic essential element; its water-insoluble salt, selenium sulfide, is an active ingredient that is used (in either a foam, lotion, or shampoo) to treat not only seborrheic dermatitis but also tinea versicolor. Three individuals with hyperkeratosis involving their palms and/or soles are described; the hyperkeratosis was successful treated with topical selenium sulfide in either a 2.5% lotion/shampoo or a 2.75% foam. The response to topical selenium sulfide was not only rapid but also complete and sustained; none of the patients experienced any adverse events secondary to the therapy. In conclusion, we recommend that topical selenium sulfide be added to the therapeutic armamentarium for congenital or acquired hyperkeratosis—particularly for those patients with involvement of their palms and soles.
Keywords: Foot, Hand, Hyperkeratosis, Keratoderma, Palm, Plantar, Selenium, Soles, Sulfide, Topical
Introduction
Hyperkeratosis presents as thickening of the skin. Selenium sulfide is an agent that is topically used for the management of seborrheic dermatitis and tinea versicolor. Three individuals with hyperkeratosis of their plantar feet, whose thickened skin was successfully treated with topical selenium sulfide, are described. Informed consent was obtained from the participants for inclusion in the study.
Case Reports
Case 1
A 38-year-old African American woman presented for treatment of plantar hyperkeratosis. Her past medical history was significant for spina bifida. However, she was otherwise healthy.
Four years earlier, she was seen for evaluation and management of a left trochanteric pressure ulcer. At that time, her cutaneous examination revealed scaling and ulcers on her feet. She also had an ulcer overlying the left trochanter. In addition, she had bilateral lower extremity edema.
Her leg edema was successfully managed with lower extremity dynamic compression therapy. The pressure ulcer on her left trochanter completely healed. The ulcers on her feet underwent serial debridement; during these treatments, she also required a brief course of oral antibiotics. In addition, weekly topical management of the foot ulcers included antimicrobial dressings along with white petroleum moisturizer. Also, antifungal cream was applied twice daily to her toes. Subsequently, the ulcers on her feet healed; however, the hyperkeratosis on her feet persisted.
Four years after her initial presentation, she returned for treatment of her plantar hyperkeratosis. She also had calluses on her palms that developed secondary to the use of her manual wheelchair. Cutaneous examination of the plantar surface of her bilateral feet showed thickening of the skin (Fig. 1).
Fig. 1.
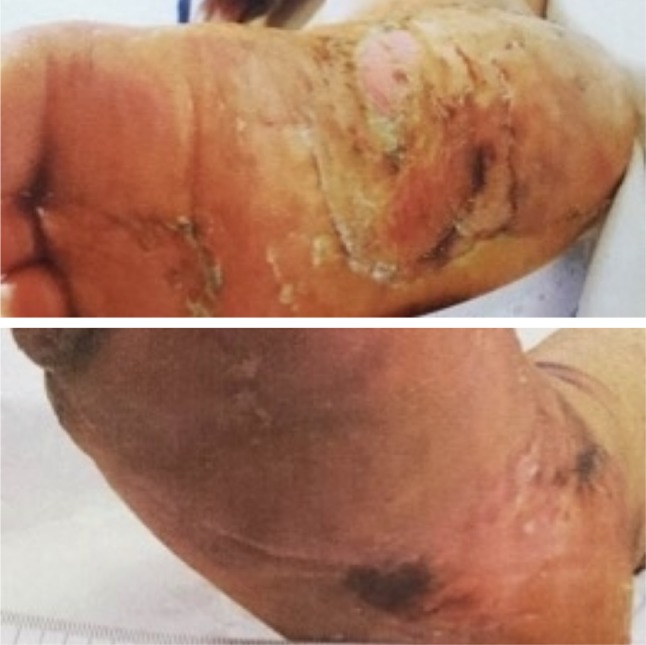
The right plantar foot of a 38-year-old African American woman. There is prominent hyperkeratosis on the medial aspect of the plantar foot (top). Complete resolution of the plantar hyperkeratosis is observed 2 weeks after the initiation of daily treatment with selenium sulfide foam 2.75% (bottom). The foam was applied to the area for 10 min prior to being rinsed off; after rinsing, Aquaphor ointment was also applied daily
Initially, her feet were treated with salicylic acid ointment 3% applied topically twice daily. There was no improvement. The salicylic acid topical therapy was discontinued and she began daily treatment with selenium sulfide foam 2.75%.
She was instructed to apply the selenium sulfide foam onto her feet and continue to rub the area so that the selenium sulfide was in a lather form. The foam remained present on her feet for 10 min prior to being rinsed off. She also continued to apply Aquaphor ointment daily, as she had previously done.
She achieved an excellent result with the selenium sulfide therapy; there was complete resolution of her plantar hyperkeratosis within 2 weeks (Fig. 1). Subsequently, she was instructed to taper the selenium sulfide therapy—every other day for 3 weeks and then as needed if the hyperkeratosis reappeared. She continued to use Aquaphor ointment daily.
Her feet remained clear of the hyperkeratotic skin. Therefore, she decided to discontinue the Aquaphor ointment and began topical treatment with ammonium lactate cream 12%. The plantar hyperkeratosis recurred; she stopped the ammonium lactate cream 12% and treated her feet with the selenium sulfide foam 2.75%. Promptly, the plantar hyperkeratosis resolved.
Case 2
A 32-year-old Caucasian man presented for evaluation and treatment of congenital hyperkeratosis with fissures on his palms and soles. His sister also had a similar congenital palmoplantar hyperkeratosis; correlation of the clinical history and lesion morphology established a diagnosis of Unna–Thost disease. In addition, the patient’s past medical history was significant for poorly controlled diabetes mellitus and severe coronary artery disease with several prior myocardial infarctions and placement of coronary stents.
Cutaneous examination of the plantar surface of his feet showed hyperkeratosis with multiple fissures (Fig. 2). Prior unsuccessful topical therapies had included salicylic acid ointment, urea cream, ammonium lactate cream, and high-potency corticosteroid creams and ointments. Therefore, a decision was made to implement selenium sulfide shampoo 2.5%.
Fig. 2.

The left plantar foot of a 32-year-old Caucasian man who had Unna–Thost syndrome and congenital hyperkeratosis of his palms and soles. There is confluent hyperkeratosis of the mid and distal plantar foot (top). There is complete resolution of the plantar hyperkeratosis within 2 weeks after initiating daily topical therapy with selenium sulfide shampoo 2.5% (bottom). The shampoo remained on the foot for 10 min after it had been rubbed into the foot and was in a lather form; it was then rinsed off and Aquaphor ointment was applied
He applied the shampoo daily and rubbed it into his feet until it was in a lather form. Then he allowed the shampoo to remain present for 10 min prior to rinsing it off. He also applied Aquaphor ointment daily.
He had excellent results. There was complete resolution of the plantar hyperkeratosis within 2 weeks after initiating therapy (Fig. 2).
Prompted by the effectiveness of the topical selenium sulfide treatment after 1 week of application to his feet, he began to apply it for 30 min daily not only to his feet, but also to his hyperkeratotic hands. He tolerated this regimen and noted significant improvement. Therefore, the following week, he kept the shampoo lather on his hands for up to 2 h.
Follow-up examination revealed that his palmar hyperkeratosis had also almost completely resolved. The patient enthusiastically discussed that none of his prior treatments had worked this well. He was instructed to use the selenium sulfide 2.5% shampoo on an as-needed basis and to continue to apply Aquaphor ointment daily.
Case 3
An 80-year-old African American man presented for evaluation and treatment of extensive hyperkeratosis of his lower legs and feet. His past medical history was significant for chronic bilateral lymphedema of his distal lower extremities. He also had ongoing issues with compliance to medical therapy.
Three and one-half years earlier, he was initially seen for his lower extremity lymphedema and associated numerous verrucous keratoses on his distal legs and feet. His management required bilateral lower extremity compression therapy—including manual lymphatic drainage massage therapy—coupled with extensive debridement of the hyperkeratotic scaly skin of both legs. These interventions proved useful in managing the lymphedema along with achieving a marked improvement in the extent of papillomatous skin lesions of legs and feet.
The application of white petroleum prior to each compression wrap to his legs was continued weekly. However, follow-up examination showed that the hyperkeratosis of his legs and feet persisted. Yet, most of the hyperkeratosis responded to weekly labor-intensive superficial curette debridement of the skin, which resulted in the shedding of a substantial amount of scales.
Subsequently, two and one-quarter years ago, he was again evaluated for the management of his lower-extremity hyperkeratosis. Ammonium lactate cream 12% was recommended; however, the patient was unable to tolerate the cream because of extensive burning. When the dosage was reduced to 5%, he had the same problem and had to discontinue the treatment with ammonium lactate. After 2 weeks, he also complained of burning with the 5% version.
He resumed daily Aquaphor ointment application to his legs. In addition, he continued his maintenance compression therapy. However, during the subsequent 2 years, the hyperkeratotic lesions recurred on his legs and prompted further debridement.
Cutaneous examination showed extensive hyperkeratosis on his legs and feet (Fig. 3). Daily application of selenium sulfide shampoo 2.5% was started. He applied the shampoo to both legs and feet daily in a lather form. The shampoo was allowed to remain present for 10–20 min each day prior to rinsing it off. Afterwards, he continued to apply Aquaphor ointment daily to his lower extremities.
Fig. 3.
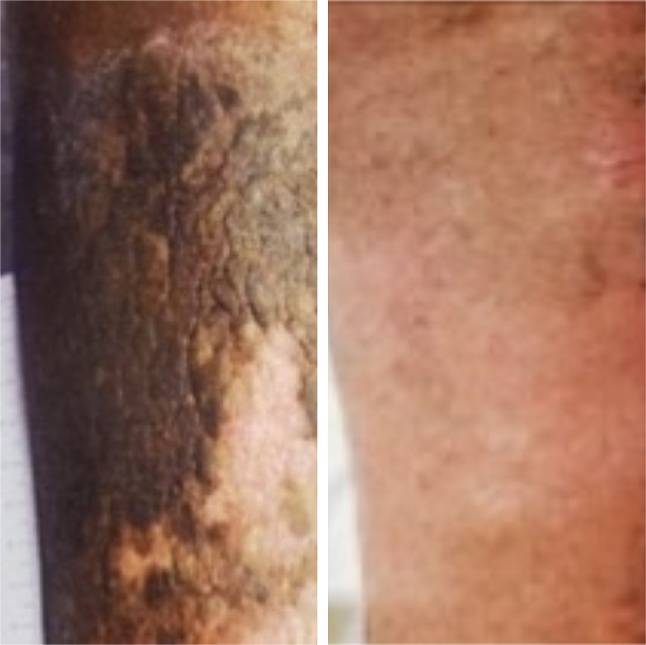
The right distal leg of an 80-year-old African American man with a history of chronic lymphedema of his lower extremities. There was extensive hyperkeratosis on the distal right pretibial leg (left). The hyperkeratosis was completely resolved after 2 weeks of applying selenium sulfide shampoo 2.5% daily for 10–30 min; after rinsing off the shampoo, Aquaphor was applied (right)
He achieved excellent results. There was complete resolution of his bilateral lower extremity hyperkeratosis (Fig. 3). The daily application of selenium sulfide shampoo 2.5% has become part of his maintenance routine; in addition, he has not required any debridement of hyperkeratosis. However, he continues to struggle with lymphedema management, and the verrucous skin changes correlate inversely with his edema control: more lesions are present when his lymphedema control is worse.
Discussion
Hyperkeratosis, also often referred to as keratoderma, can be an acquired condition or an inherited disorder. It frequently affects the palms and soles. It typically presents as thickening of the skin; fissures and ulceration may develop [1, 2].
The classification of hyperkeratosis may be determined by its manifestations of epidermal involvement: diffuse or focal or punctate. Categories of acquired palmoplantar hyperkeratosis include chemically induced, dermatoses-related, drug-related, idiopathic, infection-related, keratoderma climactericum, malignancy-associated, malnutrition-associated, and systemic-disease-related. Hereditary palmoplantar keratoderma may be limited to persistent thickening of the palms and soles or may be associated with syndromes characterized by additional extracutaneous manifestations, such as cardiomyopathy, deafness, inborn errors of metabolism, internal organ involvement, mucosal lesions, or sexual development disorders [1, 2].
Hyperkeratosis is histologically defined by marked orthokeratosis: an increased thickness of the stratum corneum. Other epidermal pathologic changes that may be present include parakeratosis (demonstrated by retained nuclei in the stratum corneum), acanthosis (in which there is thickening of the entire epidermis) and hyperplasia of the granular layer and stratum spinosum; a perivascular lymphocytic infiltrate may also be seen in the dermis. Congenital hyperkeratosis can also have additional changes in the epidermis, such as epidermolysis of the granular layer [1, 2].
The initial treatment of acquired hyperkeratosis (particularly of the palms and soles) is to identify and treat the underlying cause of the associated condition. For those individuals with idiopathic acquired hyperkeratosis and patients with hereditary hyperkeratosis, there are several potential conservative treatment options that have each been associated with variable success for any given individual; they include topical keratolytics (such as urea, salicylic acid, and lactic acid), repeated physical debridement, topical retinoids, topical psoralen and ultraviolet A phototherapy, and topical corticosteroids. Systemic retinoid therapy (such as acitretin) has also been utilized for patients with severe hyperkeratosis that does not respond to conservative measures. We report our observations of successful hyperkeratosis management using topical selenium sulfide [1–4].
Selenium is a member of group IVa of the periodic table; other elements in this group include oxygen, sulfur, polonium, and tellurium. It is a nonmetallic element that has four natural oxidative states. However, the water-soluble selenite and selenate salts are toxic [5].
Selenium has a role in preventing oxidative degradation of lipids in polysaturated membranes. Selenium is an essential component of the antioxidant enzyme glutathione peroxidase. Indeed, selenium deficiency has been linked to endemic diseases in the Chinese population: Keshan disease and Kashin–Beck disease [6, 7].
Keshan disease results in cardiac enlargement, congestive heart failure, cardiogenic shock, and death. It occurs secondary to multifocal necrosis of the myocardium. Keshan disease primarily occurs in children and young women [6].
The main feature of Kashin–Beck disease is shortened stature. Multiple focal areas of necrosis in the tubular bone growth plates cause it. The endemic chronic osteoarthropathy results from atrophy, degeneration and necrosis of cartilage. Kashin–Beck disease has been observed not only in China, but also in Russia and Korea [7].
However, excess selenium can be associated with acute and chronic toxicity. Acute ingestion of selenious acid (which is usually fatal) results in garlic odor breath and red pigmentation of the hair, nails, and teeth [8]. Garlicky breath and nail changes (transverse ridges), in addition to a metallic taste in the mouth, have been observed following inhalation of hydrogen selenide [9, 10]. Residents of geographic areas with high levels of selenium may develop chronic selenium poisoning; changes characteristically involve the skin (erythema and red discoloration, pruritic scalp rash, vesicles, and secondary infections), hair (which becomes brittle and breaks easily), and nails (which become brittle and develop yellowish-white or red longitudinal lines or transverse streaks) [11].
Selenium sulfide (SeS2 or Se=S) is a selenium salt. At room temperature, it is a yellow-orange tablet or powder. In contrast to the water-soluble selenium salts, selenium sulfide is not only insoluble in water but also nontoxic when taken orally. Indeed, it has been found to be safe in animal studies and not carcinogenic when applied topically [12–14].
Selenium sulfide is used as a therapeutic agent in dermatological conditions. It is the active ingredient in anti-dandruff shampoo [14–16]. In addition, it is also used to treat tinea versicolor [14, 17, 18].
Selenium sulfide can be an effective agent for the treatment of hyperkeratosis—not only for the soles of the feet and palms of the hands, but also for thick skin on the distal legs. Either the 2.5% lotion/shampoo or the 2.75% foam preparation of selenium sulfide can be used. The treatment protocol is simple and can readily be performed by the patient or a caregiver. The selenium sulfide is applied topically and then continuously rubbed into the affected area of skin for at least 10 min; longer treatment durations—ranging from 20 min to 2 h—can also be used. Thereafter, the treated area is cleaned with water and dried. Improvement can be observed within 2 weeks.
All of our patients had plantar hyperkeratosis. One man had congenital hyperkeratosis of the palms and soles consistent with Unna–Thost disease [19, 20]. The other patients both had lower extremity edema and acquired hyperkeratosis; the woman had spina bifida and hyperkeratosis of her plantar feet whereas the man’s hyperkeratosis was idiopathic and he had hyperkeratosis of his hands, feet, and distal legs.
Prior to using topical selenium sulfide for their hyperkeratosis, all of our patients had tried several other topical therapies, all of which failed. Indeed, after initiating treatment with selenium sulfide, all of the patients had rapid, complete, and sustained improvement of their hyperkeratosis. In addition, none of them experienced any adverse events from the therapy.
Investigators have suggested that the mechanism of action of selenium sulfide in the management of seborrheic dermatitis and tinea versicolor is secondary to its anti-Pityrosporum effect [15–17, 21]. However, the antiseborrheic properties of selenium sulfide are also the result of it significantly reducing the mitotic rate and cell turnover of the epidermis basal layer due to a cytostatic effect it has not only on the epidermal cells but also the follicular epithelium, thereby diminishing the formation rate of the stratum corneum [22, 23]. These latter effects of selenium sulfide may, in part, contribute to its effectiveness in the treatment of hyperkeratosis.
In addition, selenium sulfide has been associated with an increased sebum excretion rate [23, 24]. This clinical observation corresponds to an increase in the size of the existing sebaceous glands [23]. However, since the palms and soles have no sebaceous glands, hyperplasia of the sebaceous gland and subsequent increased sebum secretion probably did not play a role in the resolution of our patients’ hyperkeratosis.
Topical selenium sulfide has also been demonstrated to effectively treat psoriasis, an immunologically driven hyperproliferative disorder of the epidermis. The researchers treated more than 100 patients with psoriasis; similar to our methodology, they applied selenium sulfide shampoo (25 mg/ml) to the affected sites and allowed the shampoo to remain on the skin surface for 15 min before washing it off. There was prompt and sustained improvement of the psoriatic plaques—even in those individuals who had been refractory to topical tar or high-potency corticosteroids or both [25]. It is reasonable to speculate a similar mechanism of action of selenium sulfide in our patients who were treated for hyperkeratosis and those individuals who were treated for psoriasis.
Conclusions
Hyperkeratosis can be congenital or acquired. Clinically it presents as thickened skin, often affecting the palms and soles. Pathologic changes in affected skin uniformly show marked orthokeratosis of the stratum corneum. Currently, topical treatment options include keratolytics and retinoids; other local therapeutic modalities that have been initiated are physical debridement, topical corticosteroids, and phototherapy (using topical psoralen and ultraviolet A phototherapy). Selenium is a nonmetallic essential element; deficiency can result in systemic diseases. However, acute and chronic toxicity have been associated with excess ingestion. The water-insoluble selenium salt selenium sulfide is a safe active ingredient in foam, lotion, and shampoo; it has been used to treat not only seborrheic dermatitis but also tinea versicolor. The successful use of topical selenium sulfide (as a 2.5% lotion/shampoo or a 2.75% foam) to treat either congenital or acquired hyperkeratosis—particularly of the palms and/or soles—is described for three patients. All of these individuals had a rapid, complete, and sustained response to treatment, without any adverse events. In conclusion, we recommend that topical selenium sulfide be added to the therapeutic armamentarium for hyperkeratosis, especially of the palms and soles.
Acknowledgements
We thank the participants of the study.
Funding
No funding was received for the publication of this article. The authors are fully responsible for all content and editorial decisions, and received no financial support or other form of compensation related to the development of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Philip R. Cohen and Caesar A. Anderson have nothing to disclose with regards to the publication of this article.
Compliance with Ethics Guidelines
Informed consent was obtained from the participants for inclusion in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.7022126.
References
- 1.Patel S, Zirwas M, English JC., 3rd Acquired palmoplantar keratoderma. Am J Clin Dermatol. 2007;8:1–11. doi: 10.2165/00128071-200708010-00001. [DOI] [PubMed] [Google Scholar]
- 2.Guerra L., Castori M., Didona B., Castiglia D., Zambruno G. Hereditary palmoplantar keratodermas. Part II: syndromic palmoplantar keratodermas - Diagnostic algorithm and principles of therapy. Journal of the European Academy of Dermatology and Venereology. 2018;32(6):899–925. doi: 10.1111/jdv.14834. [DOI] [PubMed] [Google Scholar]
- 3.Okulicz JF, Schwartz RA. Hereditary and acquired ichthyosis vulgaris. Int J Dermatol. 2003;42:95–98. doi: 10.1046/j.1365-4362.2003.01308.x. [DOI] [PubMed] [Google Scholar]
- 4.Patel N, Spencer LA, English JC, 3rd, Zirwas MJ. Acquired ichthyosis. J Am Acad Dermatol. 2006;55:647–656. doi: 10.1016/j.jaad.2006.04.047. [DOI] [PubMed] [Google Scholar]
- 5.Barceloux DG. Selenium. J Toxicol Clin Toxicol. 1999;37:145–172. doi: 10.1081/CLT-100102417. [DOI] [PubMed] [Google Scholar]
- 6.Xu G-I, Wang S-C, Gu B-Q, et al. Further investigation of the role of selenium deficiency in the aetiology and pathogenesis of Keshan disease. Biomed Environ Sci. 1997;10:316–326. [PubMed] [Google Scholar]
- 7.Allander E. Kashin–Beck disease, an analysis of research and public health activities based on a bibliography 1849–1992. Scand J Rheumatol. 1994;23(Suppl 99):1–36. doi: 10.3109/03009749409117126. [DOI] [PubMed] [Google Scholar]
- 8.Ruta DA, Haider S. Attempted murder by selenium poisoning. Br Med J. 1989;299:316–317. doi: 10.1136/bmj.299.6694.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schecter A, Shanske W, Stenzler A, Quintilian H, Steinberg H. Acute hydrogen selenide inhalation. Chest. 1980;77:554–555. doi: 10.1378/chest.77.4.554. [DOI] [PubMed] [Google Scholar]
- 10.Alderman LC, Bergin JJ. Hydrogen selenide poisoning: an illustrative case with review. Arch Environ Health. 1986;41:354–358. doi: 10.1080/00039896.1986.9935778. [DOI] [PubMed] [Google Scholar]
- 11.Wilber CG. Toxicology of selenium: a review. J Toxicol Clin Toxicol. 1980;17:171–230. doi: 10.3109/15563658008985076. [DOI] [PubMed] [Google Scholar]
- 12.Cummins LM, Kimura ET. Safety evaluation of selenium sulfide antidandruff shampoos. Toxicol Appl Pharmacol. 1971;20:89–96. doi: 10.1016/0041-008X(71)90092-5. [DOI] [PubMed] [Google Scholar]
- 13.Millikan LE. The safety of selenium sulfide, and other news from Washington. J Am Acad Dermatol. 1980;3:430–431. doi: 10.1016/S0190-9622(80)80339-2. [DOI] [PubMed] [Google Scholar]
- 14.National Toxicology Program Selenium sulfide. Rep Carcinog. 2002;10:214–215. [PubMed] [Google Scholar]
- 15.Rapaport M. A randomized, controlled clinical trial of four anti-dandruff shampoos. J Int Med Res. 1981;9:152–156. doi: 10.1177/030006058100900213. [DOI] [PubMed] [Google Scholar]
- 16.Danby FW, Maddin WS, Margesson LJ, Rosenthal D. A randomized, double-blind, placebo-controlled trial of ketoconazole 2% shampoo versus selenium sulfide 2.5% shampoo in the treatment of moderate to severe dandruff. J Am Acad Dermatol. 1993;29:1008–1012. doi: 10.1016/0190-9622(93)70282-X. [DOI] [PubMed] [Google Scholar]
- 17.Van Cutsem J, Van Gerven F, Fransen J, Schrooten P, Janssen PA. The in vitro antifungal activity of ketoconazole, zinc pyrithione, and selenium sulfide against Pityrosporum and their efficacy as a shampoo in the treatment of experimental pityrosporosis in guinea pigs. J Am Acad Dermatol. 1990;22:993–8. [DOI] [PubMed]
- 18.Kalivas J. Lack of serum selenium rise after overnight application of selenium sulfide. Arch Dermatol. 1993;129:646–648. doi: 10.1001/archderm.1993.01680260118023. [DOI] [PubMed] [Google Scholar]
- 19.Stypczynska E, Placek W, Zegarska B, Czajkowski R. Keratinization disorders and genetic aspects in palmar and plantar keratodermas. Acta Dermatovenerol Croat. 2016;24:116–123. [PubMed] [Google Scholar]
- 20.Loh TH, Yosipovitch G, Tay YK. Palmar-plantar keratoderma of Unna Thost associated with atopic dermatitis: an underrecognized entity? Pediatr Dermatol. 2003;20:195–198. doi: 10.1046/j.1525-1470.2003.20302.x. [DOI] [PubMed] [Google Scholar]
- 21.Shuster S. The aetiology of dandruff and the mode of action of therapeutic agents. Br J Dermatol. 1984;111:235–242. doi: 10.1111/j.1365-2133.1984.tb04050.x. [DOI] [PubMed] [Google Scholar]
- 22.Sanfilippo A, English JC., 3rd An overview of medicated shampoos used in dandruff treatment. P T Community. 2006;31:394–400. [Google Scholar]
- 23.Goldschmidt H, Kligman AM. Increased sebum secretion following selenium sulfide shampoos. Acta Derm Venereol. 1968;48:489–491. [PubMed] [Google Scholar]
- 24.Piérard-Franchimont C. Subjects using anti-dandruff shampoos. Journal of the European Academy of Dermatology and Venereology. 1995;5(1):S153. doi: 10.1016/0926-9959(95)96394-N. [DOI] [Google Scholar]
- 25.Borglund E, Enhamre A. Treatment of psoriasis with topical selenium sulphide. Br J Dermatol. 1987;117:665–666. doi: 10.1111/j.1365-2133.1987.tb07503.x. [DOI] [PubMed] [Google Scholar]


