Abstract
Toxoplasmosis is a very common and asymptomatic infection caused by Toxoplasma gondii. Pregnant women can develop serious complications if the infection passes to the developing fetus. Primary infection in the pregnant women during the gestation period will result in the development of severe systemic disease with temporary parasitemia and will affect the developing fetus. Several clinical complications can be observed in the congenitally infected children which include mild disease to serious health defects such as mental retardation. The aim of the current study was to determine the seroprevalence among pregnant women in District Charsadda, KP, Pakistan. From various maternity homes and other health care centers 200 random samples were collected. Serum was extracted from the blood and was subjected to the specific serological technique by using Latex Agglutination Kit. Out of 200 random samples collected from pregnant women, 69 (34.5%) were detected positive for the parasite and the remaining 131 (65.5%) were found negative. The seroprevalence of the parasite was also determined in the pregnant women based on various age groups. The infection was more prevalent in the age group of 26–40 years with a total of 54.55% of the total studied population while low seroprevalence of the parasite was recorded in the age group 41–55 years with about 21.87%. However, the age group 15–25 years showed a moderate infection of about 23.63%. Abnormalities were also observed in the newborns of the pregnant women infected with the parasite. From Charsadda 76.1%, 45.1% from Tangi and 72.1% babies from tehsil Shabqadar were born with congenital abnormalities. With proper health care, development and utilization of effective diagnostic and therapeutic strategies the epidemics of the infection can be significantly reduced. The routine serological test is recommended for all the pregnant women.
Keywords: Toxoplasmosis, T. gondii, Sero-prevalence, Abnormalities
Introduction
Toxoplasma gondii is an obligate parasite and the causative agent of the zoonotic disease, toxoplasmosis. From various regions of Africa, Middle East, Europe and South East Asia, a high prevalence of the parasitic infection has been reported in pregnant women. Primary infection with the parasite leads to the development of congenital infection in pregnant women. While the active parasitic infection often leads to severe complications in the fetus and newborn infant. The consequences comprised of the brain, eye damage or even death of the fetus (Torgerson and Mastroiacovo 2013). The congenital toxoplasmosis also leads to the severe birth defects including nervous and ocular complications, hydrocephaly, encephalitis, epilepsy, blindness and internal calcification (Khan et al. 2011; Pappas et al. 2009). Besides with the severe complications, the pregnant women also suffer from several health defects including abortion, dermatitis, headache, myalgia, and malaise (Koppe et al. 1986).
Individuals having low socioeconomic status, routine contact with domestic animals, poor hygienic habits are more prone to the infection. Besides the risk is also associated with age of the people (Alvarado-Esquivel et al. 2017; Sroka et al. 2010). Generally, the pregnant women acquires the parasitic infection during the first and second trimester of their pregnancy. Usually, infection at that stage leads to a severe degree of illness in the fetus. However, the possibilities for transplacental infection are very less during the first trimester of the pregnancy (Jones et al. 2001).
Sero-epidemiological reports from various regions of the world have shown a higher occurrence of the infection. As generally in Southern European countries about 54% of the pregnant women population has been reported to be affected with parasitic infection. Whereas, in Sub-Saharan Africa, 92% of the pregnant women were affected by the parasitic infection (Ayi et al. 2009). Comparatively, increase in the occurrence frequencies of T. gondii in pregnant women was observed in Africa, Middle East and South-East Asian region (Sakikawa et al. 2012).
Few studies have been reported on high seroprevalence of T. gondii in pregnant women from various areas of Pakistan as according to one study, 63% from Punjab, 38% from KP and 48% prevalence from AJK were reported in 2011 (Khan et al. 2011). Very few studies have been reported on seroprevalence of the parasite in pregnant women and risk factors associated with the infection from Pakistan. The reported data from various areas of Pakistan is variable and exist in a range from less than 1% to highest prevalence up to 92% in pregnant women. The aim of the current study was to determine the seroprevalence of T. gondii among pregnant women in District Charsadda, KP, Pakistan.
Materials and methods
Subjects
The current study was conducted in District Charsadda, KP. 200 random samples were collected from the pregnant women population in 3 tehsils of the district including Charsadda, Shabqadar, and Tangi. The parasite T. gondii detection was done with Toxoplasmosis Latex Agglutination Test (Latex Agglutination Kit, Fortress diagnostics). The duration of the sampling was from September 2017 to December 2017. The age of the pregnant women varied from 15 to 55 years. The research facilities were provided by Mardan Medical Complex.
Serological technique
The parasite was detected with “Latex agglutination kit”. Blood was taken Bronchial artery of pregnant women and was centrifuged at 8000 rpm for 1 min. Then serum was taken with a pipette and added to fresh microfuge tubes. From the tubes 60 μl of the serum was added on a glass slide followed by the addition of 30 μl Latex reagent. The two components were gently mixed and left for 3 min at room temperature. Agglutination of the samples indicated the presence of the parasite while the remaining smooth samples were negative for the parasite.
Statistical analysis
The data was recorded on the basis of age of the patients, hygienic conditions and abnormalities observed in the babies born to the infected mothers. The data from each tehsil was analysed with Epi Info 7 (Center for Disease Control, GA, USA).
Results
The overall seroprevalence of T. gondii in District Charsadda
Out of 200 random samples collected from pregnant women, 69 (34.5%) were detected positive for the parasite. Remaining 131 (65.5%) were found negative as shown in Table 1.
Table 1.
Overall seroprevalence of T. gondii
| Total samples | Positive | Negative | Prevalence (%) |
|---|---|---|---|
| 200 | 69 | 131 | 34.5 |
Tehsil wise seroprevalence of T. gondii in District Charsadda
The total samples were randomly collected from 3 different tehsils including Charsadda, Tangi, and Shabqadar as shown in Table 2. The samples were received from pregnant women in hospitals, maternity homes and also during a survey of the pregnant women’s homes.
Table 2.
Tehsil wise seroprevalence of T. gondii
| Tehsil | Total samples | Positive | Negative | Prevalence (%) |
|---|---|---|---|---|
| Charsadda | 110 | 42 | 68 | 38.1 |
| Tangi | 40 | 16 | 24 | 40 |
| Shabqadar | 50 | 11 | 39 | 22 |
Age wise seroprevalence of T. gondii
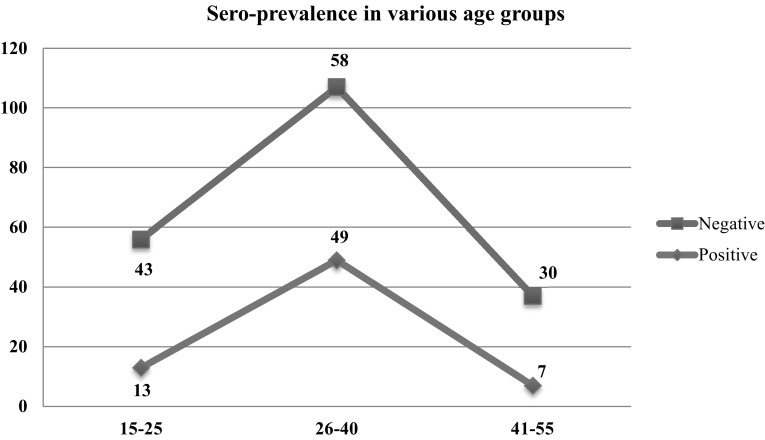
The seroprevalence of the parasite was also determined in various age groups. The age group of 26–40 years was highly affected by the infection with a total of 49 (54.55%) of the total studied population. Low seroprevalence of the parasite was recorded in the age group 41–55 years with about 7 (21.87%). However, the age group 15–25 years showed a moderate infection of about 13 (23.63%) as shown in Fig. 1.
Fig. 1.
Seroprevalence in various age groups. This figure shows the seroprevalence of T. gondii in various age groups of the pregnant women. The parasitic infection was more prevalent in the age group 26–40 years, followed by age group 15–25 and 41–55 years
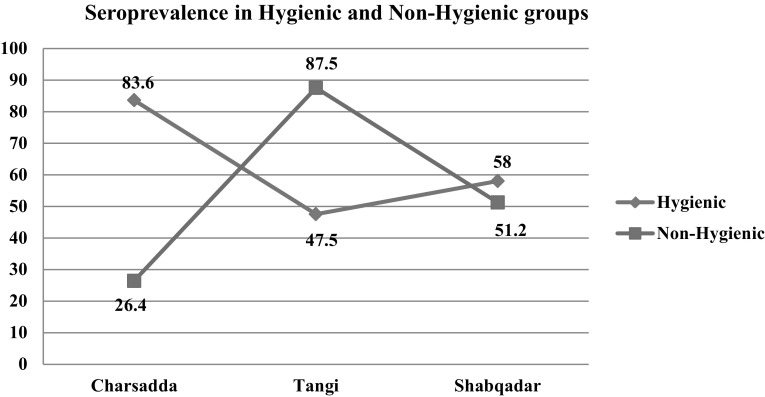
Seroprevalence on the basis of Hygienic conditions
The prevalence of the parasite was also determined on basis of hygienic conditions as shown in Fig. 2. The classification of the routine habits was based on the questionnaire filled from the pregnant women during the survey.
Fig. 2.
Seroprevalence in hygienic and non-hygienic groups. This figure shows the seroprevalence of the infection based on the hygienic and non-hygienic habits of the pregnant women. Each tehsil was divided into two sections. The prevalence was determined based on the questions asked from the women
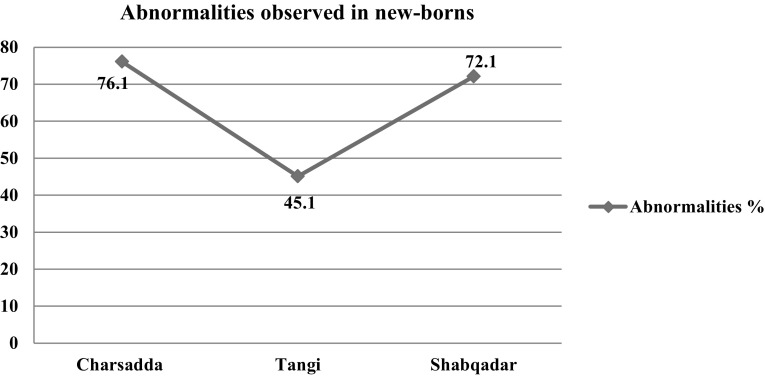
Abnormalities observed in the new-borns of infected mothers
A questionnaire was filled consisting of questions regarding the abnormalities observed in new-borns of those mothers which were pre-disposed to the infection as shown in Fig. 3.
Fig. 3.
Mothers giving birth to abnormal babies. This figure shows the frequency of the abnormal babies born to infected women. It was based on the questionnaire filled from mothers during the survey
Discussion
The epidemiological studies of T. gondii have been used as an indicator for the endemicity of the parasite in humans and animals (Ades et al. 1993; Jones et al. 2001; Sousa et al. 1988; Studeničová et al. 2006). There is very scarce data documented on the seroprevalence of the parasite. Adequate information on the prevalence and transmission routes would give proper risk assessment options in pregnant women and would assist in the planning and implementation of the control and preventive strategies for the parasitic infection. The aim of the current study was to determine the seroprevalence of the T. gondii in pregnant women in District Charsadda, KP.
Out of 200 random samples collected from pregnant women, 69 (34.5%) were detected positive and 131 (65.5%) were negative for the parasite. A similar study was conducted in 2011 in Kohat, KP in order to evaluate the seroprevalence and the risk factors of toxoplasmosis in pregnant women. The overall seroprevalence was determined to be 14.4% (26 out of 180) (Khan et al. 2011). Another similar study from the same region was conducted in 2016 in which 733 random samples were collected from the antenatal maternity centers. Overall seropositivity was detected in 81.41% in the studied population of pregnant women (Majid et al. 2016).
In the current study, the age group of 26–40 years was highly affected from the infection with a total of 54.55% of the total studied population while low seroprevalence of the parasite was recorded in the age group 41–55 years with about 21.87%. However, the age group 15–25 years showed a moderate infection of about 23.63%. Abnormalities were also observed in the newborns of the pregnant women infected with the parasite. From tehsil Charsadda 76.1%, from Tangi 45.1% and 72.1% of the babies from tehsil Shabqadar were born with congenital abnormalities.
With the presence of the domestic animals and also because of the favorable environmental conditions the parasite can survive and transmit easily from one host to another (Hill and Dubey 2018; Pal et al. 2014). There was no adequate data available on the T. gondii infection in the studied area and in the surrounding areas. The high prevalence of the infection was mainly because of the inadequate diagnostic facilities for pregnant women in the area and in the surrounding rural areas.
Conclusion
The risks and damages associated with the congenital toxoplasmosis require serious concerns and also the implementation of the health programs to escort pregnant women is very crucial. The women should undergo various serological tests every three months and should be continued until one month after birth. Neonatal screening programs are of utmost importance and should be added in concordance with the toxoplasmosis serological examination. It is significant for the detection of the parasite whenever it is not detected in the mother and it is mainly required to reduce the possible complications in the new-born. Basic training and educational programs should be encouraged and supported to educate the health professionals about the infection, possible transmission routes and preventive strategies. Awareness campaigns should be conducted for educating the pregnant women about the preventive measures and also the prenatal screening.
Acknowledgements
The authors are thankful to Mardan Medical Complex for providing research facilities.
Authors’ contributions
SF and HJ participated in the design of study. MTK and FUJ helped in the collection of data/samples. TI, AK and MS did the experimental work. MH analyzed the data and prepared the manuscript. All the authors read and approved the final manuscript.
Compliance with ethical standards
Conflict of interest
The authors of this paper have no conflict of interest.
References
- Ades A, et al. Maternal prevalence of Toxoplasma antibody based on anonymous neonatal serosurvey: a geographical analysis. Epidemiol Infect. 1993;110:127–133. doi: 10.1017/S0950268800050755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarado-Esquivel C, et al. Toxoplasma gondii exposure and neurological disorders: an age-and gender-matched case-control pilot study. Eur J Microbiol Immunol. 2017;7:303–309. doi: 10.1556/1886.2017.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayi I, Edu S, Apea-Kubi K, Boamah D, Bosompem K, Edoh D. Sero-epidemiology of toxoplasmosis amongst pregnant women in the greater Accra region of Ghana. Ghana Med J. 2009;43:107–114. doi: 10.4314/gmj.v43i3.55325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill D, Dubey J (2018) Toxoplasma gondii. In: Foodborne parasites. Springer, pp 119–138
- Jones JL, Kruszon-Moran D, Wilson M, McQuillan G, Navin T, McAuley JB. Toxoplasma gondii infection in the United States: seroprevalence and risk factors. Am J Epidemiol. 2001;154:357–365. doi: 10.1093/aje/154.4.357. [DOI] [PubMed] [Google Scholar]
- Khan SN, et al. Seroprevalance and risk factors of toxoplasmosis among pregnant women in District Kohat, Khyber Pakhtunkhwa, Pakistan. World Appl Sci J. 2011;14:1032–1036. [Google Scholar]
- Koppe J, Loewer-Sieger D, de Roever-Bonnet H. Results of 20-year follow-up of congenital toxoplasmosis. Lancet. 1986;327:254–256. doi: 10.1016/S0140-6736(86)90785-3. [DOI] [PubMed] [Google Scholar]
- Majid A, Khan S, Jan AH, Taib M, Adnan M, Ali I, Khan SN. Chronic toxoplasmosis and possible risk factors associated with pregnant women in Khyber Pakhtunkhwa. Biotechnol Biotechnol Equip. 2016;30:733–736. doi: 10.1080/13102818.2016.1175966. [DOI] [Google Scholar]
- Pal M, Alem B, Gar G, Tuli G. Toxoplasmosis in animals and humans, its diagnosis, epidemiology and control. Int J Livest Res. 2014;4:1–10. [Google Scholar]
- Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol. 2009;39:1385–1394. doi: 10.1016/j.ijpara.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Sakikawa M, et al. Anti-Toxoplasma antibody prevalence, primary infection rate, and risk factors in a study of toxoplasmosis in 4,466 pregnant women in Japan. Clin Vaccine Immunol. 2012;19:365–367. doi: 10.1128/CVI.05486-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa OE, Saenz RE, Frenkel JK. Toxoplasmosis in Panama: a 10-year study. Am J Trop Med Hyg. 1988;38:315–322. doi: 10.4269/ajtmh.1988.38.315. [DOI] [PubMed] [Google Scholar]
- Sroka S, et al. Prevalence and risk factors of toxoplasmosis among pregnant women in Fortaleza, Northeastern Brazil. Am J Trop Med Hyg. 2010;83:528–533. doi: 10.4269/ajtmh.2010.10-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studeničová C, Benčaiová G, Holková R. Seroprevalence of Toxoplasma gondii antibodies in a healthy population from Slovakia. Eur J Intern Med. 2006;17:470–473. doi: 10.1016/j.ejim.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Torgerson PR, Mastroiacovo P. The global burden of congenital toxoplasmosis: a systematic review. Bull World Health Organ. 2013;91:501–508. doi: 10.2471/BLT.12.111732. [DOI] [PMC free article] [PubMed] [Google Scholar]