Abstract
Toxoplasmosis is a cosmopolitan zoonotic infection, caused by a unicellular protozoan parasite known as Toxoplasma gondii (T. gondii) that belongs to the phylum Apicomplexa. The present investigation was aimed to evaluate the seroprevalence of T. gondii infection in the general population of Abadan city. In this cross-sectional study, a total of 496 subjects were participated. Anti-T. gondii IgG and IgM antibodies were tested using commercially available enzyme-linked immunosorbent assay (ELISA). Moreover, a structured questionnaire was completed for each person. Out of 496 subjects, 188 (37.9%) and 30 (6.05%) samples were seropositive for IgG and IgM, respectively. The more seroprevalence was found during spring season, among female subjects, in rural inhabitants, in persons with the education level of diploma or lower, from the subjects with a history of contact with cat, in individuals who consumed raw/undercooked meat, and amongst who drink unpurified water. The results showed that inhabitants of tropical areas, may be moderately exposed to T. gondii. Increase of knowledge of people about toxoplasmosis, certainly affects in reduction of the infection.
Keywords: Toxoplasma gondii, Seroprevalence, ELISA, Abadan, Iran
Introduction
Toxoplasmosis is a cosmopolitan zoonotic infection, caused by a unicellular protozoan parasite known as Toxoplasma gondii (T. gondii) that belongs to the phylum Apicomplexa (Dubey 2008). In general, Toxoplasma needs two hosts to complete its life cycle in the environment. For this purpose, cats (Family: Felidae) are the definitive hosts, while the majority of warm-blooded animals serve as intermediate hosts (Dubey 2008; Foroutan et al. 2018a; Khademvatan et al. 2017).
The infection is predominantly transmitted through the following routes: consumption of raw/undercooked meat contaminated with tissue cysts, drinking water or ingestion of raw/unwashed vegetables contaminated by mature oocysts, and vertically from mother to the fetus (Dubey 2008; Foroutan-Rad et al. 2016a; Foroutan et al. 2018a). However, transmission through blood transfusion and organ transplantation are less frequent (Foroutan-Rad et al. 2016b; Foroutan and Majidiani 2018; Yousefi et al. 2017). In humans, the infection is often subclinical and asymptomatic in immunocompetent persons, although in immunocompromised subjects such as patients with malignancies, HIV-positive individuals, and organ transplant recipients may be causes severe and progressive complications with poor prognosis, including brain abscess, encephalitis, chorioretinitis, myocarditis, etc. or even may result in death if not treated (Fallahi et al. 2017; Foroutan et al. 2018a; Majidiani et al. 2016; Rostami et al. 2018; Wang et al. 2017). Moreover, T. gondii infection may cause severe complications for the fetus in those seronegative pregnant mothers that acquired the infection during their pregnancy period (Fallahi et al. 2018; Foroutan-Rad et al. 2016a). Despite of continuous attempts of scientists and great advances during three past decades, there is no commercial licensed vaccine against toxoplasmosis for medical application in humans (Foroutan and Ghaffarifar 2018; Foroutan et al. 2018b, d).
Based on recent systematic review papers with meta-analysis approach in Iran, the seroprevalence of toxoplasmosis were estimated among different human groups. The pooled exposure to T. gondii was relatively high in various populations including: cancer patients 45% (95% CI = 39–51), HIV/AIDS subjects 50% (95% CI = 37–63), transplant recipients 55% (95% CI = 43– 67), general population 39% (95% CI = 33–46), pregnant women 41% (95% CI = 36–45), apparently healthy blood donors 33% (95% CI = 24–42), and hemodialysis patients 58% (95% CI = 46–70) (Daryani et al. 2014; Foroutan et al. 2018a, c).
Numerous published papers have determined the seroprevalence of toxoplasmosis in different human groups of Khuzastan province, southwest of Iran, indicating the people of this area has relatively moderate to high exposure to T. gondii. The majority of previous investigations have been performed in high risk populations, including pregnant women, immunosuppressed individuals, premarital women, hemodialysis patients, diabetic subjects, and multi-transfused thalassemia patients (Ghasemian et al. 2007; Maraghi et al. 2013a, b; Saki et al. 2013, 2015, 2016, 2017; Soltani et al. 2013; Yad Yad et al. 2014; Yousefi et al. 2017). Since there is a lack of an epidemiological data showing the prevalence of toxoplasmosis in human general population during recent years, thus, the current study was aimed to determine the seroprevalence of anti-Toxoplasma IgG and IgM antibodies in those subjects who referred to the Taleghani hospital, affiliated to Abadan School of Medical Sciences, southwest of Iran.
Materials and methods
Study area
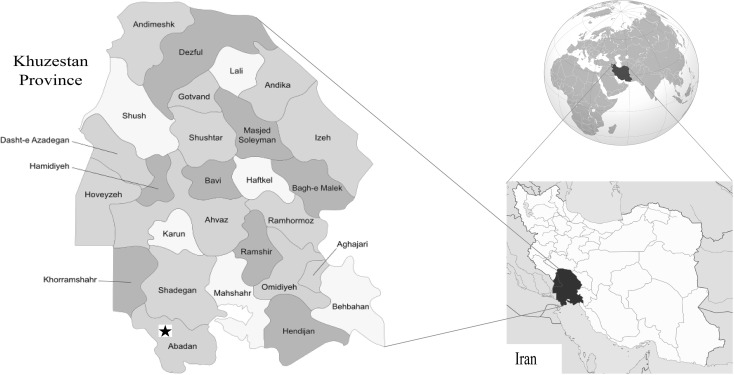
Abadan city is located in the southwest of Iran (Khuzestan province) (Fig. 1). Abadan is confined in the East by the Bahmanshir outlet of the Karun River (the Arvand Rood) and in the West by the Arvand waterway, near the Iraq-Iran border. Its population today has reached about 350,000 people. Weather temperature is highly varied throughout the year, ranged from 53 °C in summer to − 4 °C in winter. This city has a mean temperature of 25.5 °C, average relative humidity of 45%, and mean annual precipitation of 153.3 mm (https://en.wikipedia.org/wiki/Abadan,_Iran).
Fig. 1.
Location of Abadan city. The study region is shown with black asterisk
Study population
In this cross-sectional study, venous blood samples were taken from 496 participants who were referred to Taleghani hospital affiliated to Abadan School of Medical Sciences between July 2017 and June 2018 for routine checkups. A written informed consent was obtained from adult persons and parent or guardian of children less than 15 years old. This study received the approval from the Abadan School of Medical Sciences Ethical Committee (1396.239).
Serology
From each person who agreed to participate in this study, 5 mL of venous blood was collected. All blood specimens were transferred to the central laboratory of the Abadan School of Medical sciences. Firstly, the blood samples were centrifuged at 4000 rpm for 5 min. Then the sera were separated and stored in − 20 °C until examined. The specific anti-T. gondii IgM and IgG antibodies were tested by commercial available enzyme-linked immunosorbent assay (ELISA) kit (Torch-IgG, IgM-Trinity Biotech Company) based on the manufacturer’s instruction. The samples with international units (IU)/mL of < 0.9, 0.9–1.1, and > 1.1 were considered as negative, borderline, and positive, respectively.
Questionnaire
A questionnaire was completed for each individual containing some demographic information, including gender (Male or Female), age (10–25, 25–40, 40–55, and 55–72), place of residence (Urban or Rural), season (Spring, Summer, Autumn, and Winter), education level (Diploma or lower and University degree), contact with cat (Yes or No), consumption of raw/undercooked meat (Yes or No), and source of drinking water (Purified or Unpurified water).
Statistical analysis
Data analysis was performed using SPSS version 22 and Chi square test.
Results
Participants
In the current study, 496 individuals were participated from July 2017 to June 2018. Of these, 243 (49%) and 253 (51%) were male and female, respectively. The age range of the subjects was 10–72 years old. In terms of place of residence, 357 (72%) of participants were from urban areas and the rest were from rural regions (28%; 139/496).
Seroprevalence of anti-T. gondii antibodies
Four hundred and ninety six persons were tested for the presence of anti-T. gondii IgG and IgM antibodies using ELISA. The overall prevalence of toxoplasmosis was 43.95% (218/496) in Abadan city. Of these, 188 (37.9%) and 30 (6.05%) samples were identified positive for IgG and IgM, respectively.
Risk factors
During this investigation, we recorded eight risk factors related to T. gondii infection. In terms of gender, 55% (139/253) and 7% (18/253) of female were seropositive for IgG and IgM antibodies, respectively. While, these antibodies were identified in 20% (49/243) and 5% (12/243) of male, respectively. The overall prevalence between two genders was statistically significant (62% vs. 25%). In terms of residence, 39.2% (140/357) and 56.1% (78/139) of the subjects of urban and rural communities were seropositive for T. gondii, respectively. We divided all participants into four groups including 10–25, 25–40, 40–55, and 55–72 years and the exposure to T. gondii was estimated as 44.9% (58/129), 58.05% (75/129), 35.43% (44/124), and 35.96% (41/114), respectively. Also, the higher seroprevalence rate was observed during spring season (64.5%; 80/124), in subjects with the education level of diploma or lower (51.8%; 176/340), from the persons who had contact with cat (49.3%; 69/140), in individuals who consumed raw/undercooked meat (49.3%; 37/75), and amongst who drink unpurified water (52.45%; 32/61). More details are listed in Table 1.
Table 1.
Demographic characteristics and risk factors related to seroprevalence of T. gondii
| Characteristic | Number tested | IgG positive | IgM positive | Total | |||
|---|---|---|---|---|---|---|---|
| Number | Percent (%) | Number | Percent (%) | Number | Percent (%) | ||
| Gender | |||||||
| Male | 243 (49%) | 49 | 20 | 12 | 5 | 61 | 25 |
| Female | 253 (51%) | 139 | 55 | 18 | 7 | 157 | 62 |
| Age | |||||||
| 10–25 | 129 (26%) | 50 | 38.7 | 8 | 6.2 | 58 | 44.9 |
| 25–40 | 129 (26%) | 65 | 50.3 | 10 | 7.75 | 75 | 58.05 |
| 40–55 | 124 (25%) | 38 | 30.6 | 6 | 4.83 | 44 | 35.43 |
| 55–72 | 114 (23%) | 35 | 30.7 | 6 | 5.26 | 41 | 35.96 |
| Residence | |||||||
| Uraban | 357 (72%) | 122 | 34.2 | 18 | 5 | 140 | 39.2 |
| Rural | 139 (28%) | 66 | 47.5 | 12 | 8.6 | 78 | 56.1 |
| Season | |||||||
| Spring | 124 (25%) | 70 | 37.2 | 10 | 8 | 80 | 64.5 |
| Summer | 124 (25%) | 25 | 13.3 | 4 | 3.2 | 29 | 23.4 |
| Autumn | 124 (25%) | 65 | 34.6 | 11 | 8.8 | 76 | 61.3 |
| Winter | 124 (25%) | 28 | 14.9 | 5 | 4 | 33 | 26.6 |
| Education level | |||||||
| Diploma or lower | 340 (68.5%) | 152 | 44.7 | 24 | 7.06 | 176 | 51.8 |
| University degree | 156 (31.5%) | 36 | 23.07 | 6 | 3.8 | 42 | 26.9 |
| Contact with cat | |||||||
| Yes | 140 (28.2%) | 60 | 42.8 | 9 | 6.4 | 69 | 49.3 |
| No | 356 (71.8%) | 128 | 35.9 | 21 | 5.9 | 149 | 41.8 |
| Consumption of raw/undercooked meat | |||||||
| Yes | 75 (15.1%) | 30 | 40 | 7 | 9.3 | 37 | 49.3 |
| No | 421 (84.9%) | 158 | 37.5 | 23 | 5.5 | 181 | 43 |
| Source of drinking water | |||||||
| Purified water | 435 (87.7%) | 163 | 37.5 | 23 | 5.3 | 186 | 42.75 |
| Unpurified water | 61 (12.3%) | 25 | 41 | 7 | 11.5 | 32 | 52.45 |
Discussion
The prevalence rate of toxoplasmosis in the Iranian general population was defined 39% (95% CI = 33–46), ranged from 12% to 87.5% with more endemicity in the northern provinces of the country (Daryani et al. 2014). Our knowledge is poor about the epidemiology of T. gondii infection and public health significance of urban and rural communities in Abadan city, southwest of Iran. Hence, the present study is the first survey to assess the seroprevalence rate of toxoplasmosis and related risk factors among human general population who were referred to the Taleghani hospital of Abadan city. Anti-Toxoplasma IgG and IgM antibodies were found in 37.9% and 6.05% of participants, and the overall prevalence was determined as 43.95%. The seroprevalence of our study was a little higher than the average seroprevalence of the Iranian general population (Daryani et al. 2014). Our findings are in agreement with other studies such as Mostafavi et al. in Isfahan province 41.4% (248/599) (Mostafavi et al. 2011) and Keshavarz et al. in Karzj city 45.5% (Keshavarz et al. 1998). In some studies such as Salahi-Moghaddam and Hafizi in Tehran province (Salahi-Moghaddam and Hafizi 2009) and Shahmoradi et al. in Gilan province (Shahmoradi et al. 1998) seropositivity in human general population were reported more than 50%, while the lower seroprevalence of T. gondii infection was reported from Chaharmahal & Bakhtiyari province (34.2%) (Manouchehri Naeini et al. 2012), Kermanshah province (36.3%) (Mansouri et al. 2003), Meshkin-Shahr city (18.3%) (Soltan Mohammad Zadeh et al. 2003), Shiraz city (27.6%) (Razavi et al. 2003), and Tabriz city (29.87%) (Fatollahzadeh et al. 2016). The discordance between studies could be justified by study region, study population, environment status, type of sampling, number of participants, cultural habits of the subjects, the methodologies, different cutoff values or antibody titers, etc.
Several behavioral and ecological risk factors are involved in the epidemiological distribution of toxoplasmosis. Many probable risk factors have been determined for acquiring the T. gondii infection, however inconsistent results are abundant (Daryani et al. 2014; Foroutan-Rad et al. 2016a, b; Gebremedhin and Tadesse 2015; Mansouri et al. 2017; Rostami et al. 2016; Wang et al. 2018). In this study, eight potential risk factors related to toxoplasmosis were assessed. The ELISA results showed 62% (157/253) and 25% (61/243) of female and male were seropositive for anti-T. gondii antibodies, respectively. Based on recent systematic review paper among Iranian general population, a non-significant association was observed between toxoplasmosis and gender (P > 0.05). The authors reported a slightly higher prevalence in male 44.08% (95% CI = 34.5–53.9) than female 42.06% (95% CI = 32.04–52) (Daryani et al. 2014). Besides, the same association was observed from Iranian and Chinese apparently healthy blood donors (Mansouri et al. 2017; Wang et al. 2018).
In order to assess the seroprevalence of toxoplasmosis among different age groups, the participants were categorized into four groups, including 10–25, 25–40, 40–55, and 55–72 years. The seroprevalence rate was 44.9, 58.05, 35.43, and 35.96% in these groups, respectively. In this case, Daryani et al. among the Iranian general population of Iran (Daryani et al. 2014) and Gebremedhin and Tadesse in humans from Ethiopia (Gebremedhin and Tadesse 2015) reported a significant association between T. gondii infection and age, while Wang et al. among Chinese blood donors failed to show the same association (Wang et al. 2018). As it was predictable, seroprevalence tended to increase with age. The older subjects have a higher seroprevalence of toxoplasmosis than younger groups. Its reason could be explained due to increased exposure to T. gondii via one the following transmission routes: ingestion of raw/undercooked meat, consumption of raw/unwashed vegetables, contact with contaminated soil, contact with cats, etc. (Daryani et al. 2014; Gebremedhin and Tadesse 2015).
In the current study, T. gondii infection was higher in individuals who had a history of contact with cats. Cats are serving as definitive hosts for parasites and due to their close contact with humans, especially in rural regions, there is a general consensus that contact with cat could be a potential risk factor for acquiring the infection. Stray and domestic cats are one of the main sources of T. gondii infection. They can release millions of oocysts through feces of infected cats into the environment. Sporulated oocysts may survive for a long time in moist soils, ranged from months to years (Dubey 2008; Foroutan et al. 2018a). Accordingly, exposure to soil could play a main role in T. gondii infection. In this case, Cong et al. revealed that exposure to soil is associated with prevalence of toxoplasmosis in the study population (Cong et al. 2015), while Yousefi et al. failed to show the association (Yousefi et al. 2017). As it was said in study area section, Abadan city had proper humidity and average temperature, which are necessary for oocysts sporulation. In Iran, 34% (95% CI = 22–46) of cats were found infected with T. gondii during 1975–2013 (Foroutan et al. 2018a). Previously published articles, among the Iranian general population (P < 0.05), and Iranian pregnant women (P = 0.002) have reported that contact with cat is significantly associated with seroprevalence of T. gondii infection (Daryani et al. 2014; Foroutan-Rad et al. 2016a).
Consumption of raw/undercooked meat is considered as a potential risk factor regarding the infection (Belluco et al. 2016). In the present study, the more prevalence rate was seen among subject who consumed raw/undercooked meat (49.3% vs. 43%). Although, in many papers no association between toxoplasmosis and this risk factor was shown (Foroutan-Rad et al. 2016a; Gebremedhin and Tadesse 2015; Yousefi et al. 2017), but some others are believed eating raw/undercooked meat can significantly increase the rate of infection in societies (Daryani et al. 2014; Foroutan-Rad et al. 2016b). Transmission of the parasite through meat consumption depended upon the cultural habits of people in a certain area (Belluco et al. 2016; Daryani et al. 2014). Recently, was reported that 2.6%, 12.3%, and 14.7% of cattle, pigs, and sheep were positive for T. gondii using different diagnostic methods from a global perspective. The authors confirmed the role of meat and other meat products as T. gondii sources. Increase in consumer knowledge surely influences in reduction of the infection (Belluco et al. 2016).
In the current study, 39.2% and 56.1% of participants from urban and rural regions were seropositive for toxoplasmosis, respectively. The villagers habits such as direct exposure to soil, livestock, pets, etc. could make this condition predictable, as earlier reported in the majority of published articles (Foroutan-Rad et al. 2016a, b; Gebremedhin and Tadesse 2015). In the Iranian general population, risk factor analysis highlighted that by increasing the level of education, T. gondii infection can be reduced (P < 0.0001) (Daryani et al. 2014). In this study, the same association was observed. As it is evident, lack of awareness about the main transmission routes and sources of infection as well as poor hygienic status are extremely important factors to acquiring toxoplasmosis.
In conclusion, our study revealed a moderate seroprevalence of T. gondii in the general population of southwest of Iran. A single risk factor may have a little importance on the seroepidemiological pattern of toxoplasmosis in a certain region on its own, but the above-discussed risk factors can change the distribution figure of infection in different geo-locations. Increase of knowledge of people about toxoplasmosis, the main transmission routes, and the related risk factors surely affects in reduction of the infection, especially in rural communities.
Acknowledgements
The authors would like to thank all staff of Abadan School of Medical Sciences.
Authors’ contributions
S. Soltani, M. Foroutan, H. Afshari, M. Hezarian, and M. Sagha Kahvaz conceived, designed and drafted the manuscript; S. Soltani, H. Afshari, and M. Hezarian involved in data acquisition; S. Soltani, M. Foroutan, and M. Sagha Kahvaz involved in statistical analysis and critically revised the text. All authors read and approved the final version of the manuscript.
Funding
This study was financially supported by Grant No. 96ST-0135 from Student Research Committee, Abadan School of Medical Sciences, Abadan, Iran.
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical statement
This study received the approval from the Abadan School of Medical Sciences Ethical Committee (1396.239). A written informed consent was obtained from adult persons and parent or guardian of children less than 15 years old. Ethical issues (Including plagiarism, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Contributor Information
Shahrzad Soltani, Email: shahrzadsoltani225@yahoo.com.
Masoud Foroutan, Email: m.foroutan@modares.ac.ir.
Hamed Afshari, Email: afshari.h@ajums.ac.ir.
Maryam Hezarian, Email: maryamhezarian1996@gmail.com.
Mehdi Sagha Kahvaz, Email: mehdikahvazi@gmail.com.
References
- Belluco S, Mancin M, Conficoni D, Simonato G, Pietrobelli M, Ricci A. Investigating the determinants of Toxoplasma gondii prevalence in meat: a systematic review and meta-regression. PLoS ONE. 2016;11(4):e0153856. doi: 10.1371/journal.pone.0153856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cong W, et al. Toxoplasma gondii infection in pregnant women: a seroprevalence and case-control study in Eastern China. Biomed Res Int. 2015;2015:170278. doi: 10.1155/2015/170278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daryani A, et al. Seroprevalence of Toxoplasma gondii in the Iranian general population: a systematic review and meta-analysis. Acta Trop. 2014;137:94–185. doi: 10.1016/j.actatropica.2014.05.015. [DOI] [PubMed] [Google Scholar]
- Dubey JP. The history of Toxoplasma gondii—the first 100 years. J Eukaryot Microbiol. 2008;55(6):75–467. doi: 10.1111/j.1550-7408.2008.00345.x. [DOI] [PubMed] [Google Scholar]
- Fallahi S, Rostami A, Birjandi M, Zebardast N, Kheirandish F, Spotin A. Parkinson’s disease and Toxoplasma gondii infection: sero-molecular assess the possible link among patients. Acta Trop. 2017;173:97–101. doi: 10.1016/j.actatropica.2017.06.002. [DOI] [PubMed] [Google Scholar]
- Fallahi S, Rostami A, Nourollahpour Shiadeh M, Behniafar H, Paktinat S. An updated literature review on maternal-fetal and reproductive disorders of Toxoplasma gondii infection. J Gynecol Obstet Hum Reprod. 2018;47(3):133–140. doi: 10.1016/j.jogoh.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Fatollahzadeh M, et al. Study of anti-Toxoplasma IgG and IgM seropositivity among subjects referred to the central laboratory in Tabriz, Iran, 2013-2014. Avicenna J Clin Microbiol Infect. 2016;3(3):e35975. doi: 10.17795/ajcmi-35975. [DOI] [Google Scholar]
- Foroutan M, Ghaffarifar F. Calcium-dependent protein kinases are potential targets for Toxoplasma gondii vaccine. Clin Exp Vaccine Res. 2018;7(1):24–36. doi: 10.7774/cevr.2018.7.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foroutan M, Majidiani H. Toxoplasma gondii: are there any implications for routine blood screening? Int J Infect. 2018;5(1):e62886. doi: 10.5812/iji.62886. [DOI] [Google Scholar]
- Foroutan M, et al. Rolling up the pieces of a puzzle: a systematic review and meta-analysis of the prevalence of toxoplasmosis in Iran. Alex J Med. 2018;54(3):189–196. doi: 10.1016/j.ajme.2017.06.003. [DOI] [Google Scholar]
- Foroutan M, Ghaffarifar F, Sharifi Z, Dalimi A, Pirestani M. Bioinformatics analysis of ROP8 protein to improve vaccine design against Toxoplasma gondii. Infect Genet Evol. 2018;62:193–204. doi: 10.1016/j.meegid.2018.04.033. [DOI] [PubMed] [Google Scholar]
- Foroutan M, et al. A systematic review and meta-analysis of the prevalence of toxoplasmosis in hemodialysis patients in Iran. Epidemiol Health. 2018;40:e2018016. doi: 10.4178/epih.e2018016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foroutan M, Zaki L, Ghaffarifar F. Recent progress in microneme-based vaccines development against Toxoplasma gondii. Clin Exp Vaccine Res. 2018;7(2):93–103. doi: 10.7774/cevr.2018.7.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foroutan-Rad M, Khademvatan S, Majidiani H, Aryamand S, Rahim F, Malehi AS. Seroprevalence of Toxoplasma gondii in the Iranian pregnant women: a systematic review and meta-analysis. Acta Trop. 2016;158:160–169. doi: 10.1016/j.actatropica.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Foroutan-Rad M, et al. Toxoplasmosis in blood donors: a systematic review and meta-analysis. Transfus Med Rev. 2016;30(3):22–116. doi: 10.1016/j.tmrv.2016.03.002. [DOI] [PubMed] [Google Scholar]
- Gebremedhin EZ, Tadesse G. A meta-analysis of the prevalence of Toxoplasma gondii in animals and humans in Ethiopia. Parasit Vectors. 2015;8(1):291. doi: 10.1186/s13071-015-0901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghasemian M, Maraghi S, Saki J, Pedram M. Determination of antibodies (IgG, IgM) against Toxoplasma gondii in patients with cancer. Iran J Parasitol. 2007;2(4):1–6. [Google Scholar]
- Keshavarz H, Nateghpour M, Zibaei M. Seroepidemiologic survey of toxoplasmosis in Karaj district. Iran J Public Health. 1998;27(3–4):73–82. [Google Scholar]
- Khademvatan S, et al. Toxoplasmosis in rodents: a systematic review and meta-analysis in Iran. J Infect Public Health. 2017;10(5):487–493. doi: 10.1016/j.jiph.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Majidiani H, Dalvand S, Daryani A, Galvan-Ramirez ML, Foroutan-Rad M. Is chronic toxoplasmosis a risk factor for diabetes mellitus? A systematic review and meta-analysis of case-control studies. Braz J Infect Dis. 2016;20(6):605–609. doi: 10.1016/j.bjid.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manouchehri Naeini K, Mortazaei S, Zebardast N, Kheiri S. Seroprevalence and some of risk factors affecting Toxoplasma infection in Chaharmahal va Bakhtiyari province, Iran. J Share Univ Med Sci. 2012;13(6):8–18. [Google Scholar]
- Mansouri F, Hatami H, Mahdavian B, Hashemian AH. Epidemiology of toxoplasmosis in Kermanshah province. J Kermanshah Univ Med Sci. 2003;7(2):12–19. [Google Scholar]
- Mansouri A, et al. Epidemiology of Toxoplasma gondii among blood donors in Iran: a systematic review and meta-analysis. Transfus Apher Sci. 2017;56(3):404–409. doi: 10.1016/j.transci.2017.03.011. [DOI] [PubMed] [Google Scholar]
- Maraghi S, YadYad M, Sheikhi M, LatifiS M. Frequency of anti-Toxoplasma antibodies in midwifery and nursing students of Abadan Islamic Azad University students in 2011. Armaghane Dan. 2013;18(4):327–336. [Google Scholar]
- Maraghi S, Yadyad MJ, Sheikhi M, Shamakhteh F, Latifi SM. Study the anti-Toxoplasma antibodies (IgG and IgM) in hemodialysis patients of Abadan and Khoramshahr cities Southwest Iran in 2011 using ELISA. Jundishapur J Microbiol. 2013;6(7):e7113. doi: 10.5812/jjm.7113. [DOI] [Google Scholar]
- Mostafavi SN, Ataei B, Nokhodian Z, Yaran M, Babak A. Seroepidemiology of Toxoplasma gondii infection in Isfahan province, central Iran: a population based study. J Res Med Sci. 2011;16(4):496–501. [PMC free article] [PubMed] [Google Scholar]
- Razavi S, Esnaashari H, Gheysari H. Seroepidemiological survey of toxoplasmosis by IFA technique in the students of Faculty of Veterinary Medicine, University of Shiraz. J Vet Res. 2003;58(2):163–167. [Google Scholar]
- Rostami A, et al. Seroprevalence and risk factors associated with Toxoplasma gondii infection among rural communities in Northern Iran. Rev Inst Med Trop Sao Paulo. 2016;58:70. doi: 10.1590/S1678-9946201658070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostami A, Karanis P, Fallahi S. Advances in serological, imaging techniques and molecular diagnosis of Toxoplasma gondii infection. Infection. 2018;46(3):303–315. doi: 10.1007/s15010-017-1111-3. [DOI] [PubMed] [Google Scholar]
- Saki J, Khademvatan S, Soltani S, Shahbazian H. Detection of toxoplasmosis in patients with end-stage renal disease by enzyme-linked immunosorbent assay and polymerase chain reaction methods. Parasitol Res. 2013;112(1):8–163. doi: 10.1007/s00436-012-3120-6. [DOI] [PubMed] [Google Scholar]
- Saki J, Mohammadpour N, Moramezi F, Khademvatan S. Seroprevalence of Toxoplasma gondii in women who have aborted in comparison with the women with normal delivery in Ahvaz, southwest of Iran. Sci World J. 2015;2015:764369. doi: 10.1155/2015/764369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saki J, Shafieenia S, Foroutan-Rad M. Seroprevalence of toxoplasmosis in diabetic pregnant women in southwestern of Iran. J Parasit Dis. 2016;40(4):1586–1589. doi: 10.1007/s12639-015-0735-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saki J, Tavakoli S, Pedram M. Seroprevalence and molecular evaluation of toxoplasmosis in children with cancer in Khuzestan province, Southwest of Iran. J Parasit Dis. 2017;41(4):947–951. doi: 10.1007/s12639-017-0916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salahi-Moghaddam A, Hafizi A. A serological study on Toxoplasma gondii infection among people in south of Tehran, Iran. Korean J Parasitol. 2009;47(1):3–61. doi: 10.3347/kjp.2009.47.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahmoradi A, Daryani A, Hajizadeh A. Seroepidemiological survey of toxoplasmosis in individuals referred to Health Center of Roodsar, Gilan. J Shahid Beheshti Univ Med Sci. 1998;4:7–12. [Google Scholar]
- Soltan Mohammad Zadeh M, Keshavarz H, Mohebali M, Holakouie Naieni K, Arshi S. Seroepidemiologic study of human Toxoplasma infection in residents of Meshkin-Shahr. J Sch Public Health Inst Public Health Res. 2003;1(4):57–72. [Google Scholar]
- Soltani S, Khademvatan S, Saki J, Shahbazian H. Detection of toxoplasmosis in renal transplant recipients by ELISA and PCR methods in Ahvaz, Southwest of Iran. Jundishapur J Microbiol. 2013;6(9):e7642. doi: 10.5812/Jjm.7642. [DOI] [Google Scholar]
- Wang ZD, et al. Toxoplasma gondii infection in immunocompromised patients: a systematic review and meta-analysis. Front Microbiol. 2017;8:389. doi: 10.3389/fmicb.2017.00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T, Han Y, Pan Z, Wang H, Yuan M, Lin H. Seroprevalence of Toxoplasma gondii infection in blood donors in mainland China: a systematic review and meta-analysis. Parasite. 2018;25:36. doi: 10.1051/parasite/2018037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yad Yad MJ, Jomehzadeh N, Jafar Sameri M, Noorshahi N. Seroprevalence of anti-Toxoplasma gondii antibodies among pregnant woman in South Khuzestan, Iran. Jundishapur J Microbiol. 2014;7(5):e9998. doi: 10.5812/jjm.9998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousefi E, Foroutan M, Salehi R, Khademvatan S. Detection of acute and chronic toxoplasmosis amongst multi-transfused thalassemia patients in southwest of Iran. J Acute Dis. 2017;6(3):120–125. doi: 10.12980/jad.6.2017JADWEB-2017-0008. [DOI] [Google Scholar]