Abstract
HIV incidence and mortality are high among adolescents and young adults (AYA) in sub-Saharan Africa, but testing rates are low. Understanding how support people (SP), such as peers, partners, or parents, influence AYA may improve HIV testing uptake. AYA aged 14–24 seeking HIV testing at a referral hospital in Nairobi, Kenya completed a post-test survey assessing the role of SP. Among 1,062 AYA, median age was 21. Overall, 12% reported their decision to test was influenced by a parent, 20% by a partner, and 22% by a peer. Young adults (20–24 years old) were more likely than adolescents (14–19 years old) to be influenced to test by partners (23% vs 12%, p<0.001), and less likely by parents (6.6% vs 27%, p<0.001), healthcare workers (11% vs 16%, p<0.05), or counselors (9.4% vs 19%, p<0.001). Half of AYA were accompanied for testing (9.9% with parent, 11% partner, 23% peer, 4.3% others, and 2.1% multiple types). Young adults were more likely than adolescents to present alone (58% vs 32%, p<0.001) or with a partner (12% vs 6.7%, p<0.001), and less likely with a parent (1.6% vs 31%, p<0.001). Similar proportions of adolescents and young adults came with a peer or in a group. Correlates of presenting with SP included: younger age (aRR=1.55 [95%CI=1.30–1.85]), female sex (aRR=1.45 [95%CI=1.21–1.73]), and school enrollment (aRR=1.41 [95%CI=1.05–1.88]). SP play an important role in AYA’s HIV testing and varies with age. Leveraging SP may promote uptake of HIV testing and subsequent linkage care for AYA.
Keywords: adolescent, young adult, HIV, support people, testing
Introduction
UNAIDS estimates that 4 million adolescents and young adults (AYA) aged 15–24 were living with HIV in 2016 (Joint United Nations Programme on HIV/AIDS [UNAIDS], 2016). In Kenya, AYA aged 15–24 have the highest HIV incidence rates compared to other age strata, and an estimated 50% of AYA aged 15–19 and 81% of AYA aged 20–24 have ever been tested for HIV (National AIDS Control Council [NASCOP], 2016). Accessing HIV testing services (HTS) can be challenging for AYA due to knowledge, economic, legal, and psychological barriers (World Health Organization [WHO], 2002, 2014).
Studies have found that support people (SP), defined as parents, partners, or peers, can positively influence HIV testing among AYA (MacPhail et al., 2009). HIV-related partner communication has been associated with an increase in AYA testing uptake (Talib et al., 2013), and peer recruiters can increase acceptability and demand for HTS (Boyer et al., 2013). Conversely, a perceived lack of support from SP exacerbates AYA fears of HIV testing (Strauss et al., 2015). In one study, untested young adults were twice as likely to report fears of family or partner rejection compared to those tested for HIV (Bhoobun et al., 2014).
SP also play an important role in HIV treatment; SP have been utilized to improve adherence to antiretroviral treatment (ART) (Chaiyachati et al., 2014), increase knowledge of reproductive health and HIV (Bastien et al., 2011; Mwale et al., 2017; Puffer et al., 2016), and support lifestyle changes (Ramchand et al., 2017; Siceloff et al., 2014). There is also evidence of higher retention of AYA in HIV treatment programs in clinics offering AYA support groups (Lamb et al., 2014).
Given the potential for SP to support AYA in HIV testing and linkage to care, we evaluated the role SP play in the AYA decision to test for HIV and within each stage of the HIV voluntary counseling and testing (VCT) visit, including pre-test counseling, finger prick/blood draw, disclosure of results, post-test counseling. We describe characteristics of SP, and their role by AYA age group, to inform the development of interventions utilizing support systems.
Methods
Study design
This secondary cross-sectional analysis was nested within the Developing Adolescent Strategies for HIV Testing (DASH) Study, which assessed the use of a quality improvement intervention to optimize AYA HTS (Wagner et al., 2017). Data collected 6 months prior to and during the intervention were used in this analysis. The intervention focused on optimizing facility-level HTS procedures and is not expected to have influenced SP involvement in the AYA decision to test, SP accompaniment, or SP involvement in the HTS visit.
Study location and population
This study was conducted from October 2015 to June 2016 at the Kenyatta National Hospital (KNH) HIV VCT clinics in Nairobi, Kenya. AYA exiting HTS were recruited from 3 separate areas; Main VCT serving a mostly adult clientele, Youth Center, and VCT Tents stationed near the hospital gate. AYA ages 14 to 24 who completed HIV testing within the study period in any of the 3 clinics were eligible for the study and referred by clinic staff to study staff for screening; however, newly diagnosed AYA were escorted directly to the HIV care clinic following diagnosis and were thus excluded (Wagner et al., 2017). AYA were not reimbursed for participation in this study.
Data collection
Participants completed a short Audio Computer-Assisted Self-Interview (ACASI) survey that assessed sociodemographic information, satisfaction with services and SP involvement. The survey tool was developed by the study team with input from local HTS providers. The survey was conducted in English with audio-recorded questions and numbered answers to enable participation by AYA with incomplete literacy. Headphones were provided to maintain privacy. Study participants completed the survey in a private room at KNH, and the survey took an estimated 20 minutes to complete. A study counselor was also available to answer any questions.
Measures
All exposures and outcomes were self-reported by enrolled AYA. Exposures in this analysis included age (14–19/20–24 years and linear continuous), sex (female/male), highest level of education completed (primary, secondary, polytechnic, and university/college), current enrollment in school (yes/no), and first time presenting for an HIV test (yes/no). AYA could indicate multiple SP who influenced their decision to test; categories of SP included: parents, peers, partners, health care workers (HCW), counselors, and other SP (includes other family, church members, and unspecified other). If an AYA selected multiple SP, that AYA was included in the numerator of each of the proportions of the SP that they indicated. The primary outcome of this analysis was whether the adolescent presented for testing accompanied by SP. We reported the proportion of AYA who came with parent(s), peer(s), and partner(s), those who selected multiple groups (e.g. parent and peer), and those who came with others (e.g. other family and church members). AYA were also asked to identify whether SP were present for pre-test counselling, finger prick/blood draw, disclosure of results, and/or post-test counseling. All questions were required by the electronic data tool. SP attendance and characteristics were stratified by age interval based on the WHO definition of adolescence (adolescents=14–19 and young adults=20–24) (World Health Organization [WHO], 2014).
Data analysis
Analyses were conducted using Stata 14 (StataCorp, College Station, TX), all tests were 2-sided with alpha=0.05. Proportions were used to describe the role of SP in AYAs’ decision to test, the proportion of AYA accompanied by SP, and SP participation in the HIV test visit. Chi-squared tests of binomial proportions were used to compare proportions between different age intervals and determine whether AYA were more likely to present for HTS accompanied by SP or unaccompanied. Relative risk regression (generalized linear models using a log link and Poisson family) yielded prevalence ratios, which were used to evaluate the association between exposures and the primary outcome (SP accompanied/unaccompanied). Education was collinear with age, thus age, not level of education, was adjusted for in this analysis.
Ethical Considerations
This study was approved by the Kenyatta National Hospital Ethics and Research Committee (KNH ERC #P281/05/2015) and the University of Washington Institutional Review Board (UW IRB #48627). Participants were identified by VCT staff after completing the test session, and referred to study staff for enrollment and oral consent. AYA ≥18 years and mature minors (14–17 years) provided oral informed consent. Adolescents age 14–17 years who were accompanied by a caregiver provided assent and the caregiver provided consent. A waiver of parental permission was granted for this minimal risk, anonymous survey for unaccompanied AYA.
Results
Participant characteristics
Among 1,062 AYA surveyed, median age was 21 (IQR: 19–23); 306 (29%) were adolescents (ages 14–19) and 756 (71%) were young adults (ages 20–24) (Table 1). Half (49%) of AYA were accompanied by SP. AYA in this sample were highly educated, with over 95% of participants having completed secondary school and 87% currently enrolled in school. There were approximately equal proportions of males and females. Two thirds (63%) of participants were visiting this clinic for the first time and one third (32%) of participants were receiving their first HIV test (Table 1).
Table 1:
Characteristics of adolescents and young adults enrolled at Kenyatta National Hospital, Nairobi, Kenya.
| N=1,062 n (%) or median (IQR) |
|
|---|---|
| Demographics | |
| Age | 21 (19, 23) |
| 14–19 | 306 (29%) |
| 20–24 | 756 (71%) |
| Female | 554 (52%) |
| Highest level of education completed | 17 (12, 19) |
| Primary | 44 (4.1%) |
| Secondary | 310 (29%) |
| Polytechnic | 33 (3.1%) |
| University/college | 675 (64%) |
| Currently enrolled in school | 920 (87%) |
| Characteristics of testing visit | |
| Site | |
| Upstairs VCT | 315 (30%) |
| Youth Centre | 583 (55%) |
| Tents | 164 (15%) |
| Reason for coming to VCT (N=969) | |
| HIV test | 731 (75%) |
| General health information or counseling | 180 (19%) |
| Family planning, STI test (not HIV), pregnancy test | 12 (0.1%) |
| Other | 46 (4.8%) |
| First time visiting clinic (N=969) | 611 (63%) |
| First HIV test (N=969) | 306 (32%) |
| Knowledge of HIV | |
| Correct knowledge of HIV prevention | 600 (57%) |
| Correct knowledge of HIV transmission | 596 (54%) |
| People involved in testing decision | |
| No one | 398 (38%) |
| Peer | 232 (22%) |
| Partner | 209 (20%) |
| Parent | 132 (12%) |
| Health care worker | 133 (13%) |
| Counselor | 129 (12%) |
| Other family member | 65 (6.1%) |
| Church member/Youth group member | 28 (2.6%) |
| Other | 81 (7.6%) |
|
People who accompanied adolescent to the clinic for testing (N=1049) |
|
| Unaccompanied | 530 (51%) |
| Accompanied | 519 (49%) |
| Peer | 238 (23%) |
| Partner | 110 (11%) |
| Parent | 104 (9.9%) |
| Multiple groups | 22 (2.1%) |
| Other | 45 (4.3%) |
|
Portion of testing experience for which SP were present, among adolescents who presented with SP (N=519) |
|
| Pre-test counseling | 296 (57%) |
| Finger prick/blood draw | 330 (64%) |
| Disclosure of results | 169 (33%) |
| Post-test counseling | 171 (33%) |
| None of these, waited in waiting room | 87 (17%) |
Role of SP in decision to test for HIV
Most AYA (63%) reported being influenced to test for HIV by SP. Adolescents were more likely than young adults to be influenced to test for HIV by parents (27% vs 6.6%, p<0.001), healthcare workers (16% vs 11%, p<0.05) and counselors (19% vs 9.4, p<0.001; Figure 1A). Young adults were more likely to be influenced to test by a partner compared to adolescents (23% vs 12%, p<0.001; Figure 1A). Twenty-two percent of AYA were influenced to test by a peer; this was similar between adolescents and young adults AYA (18% vs 23%, p=0.075; Figure 1A).
Figure 1:
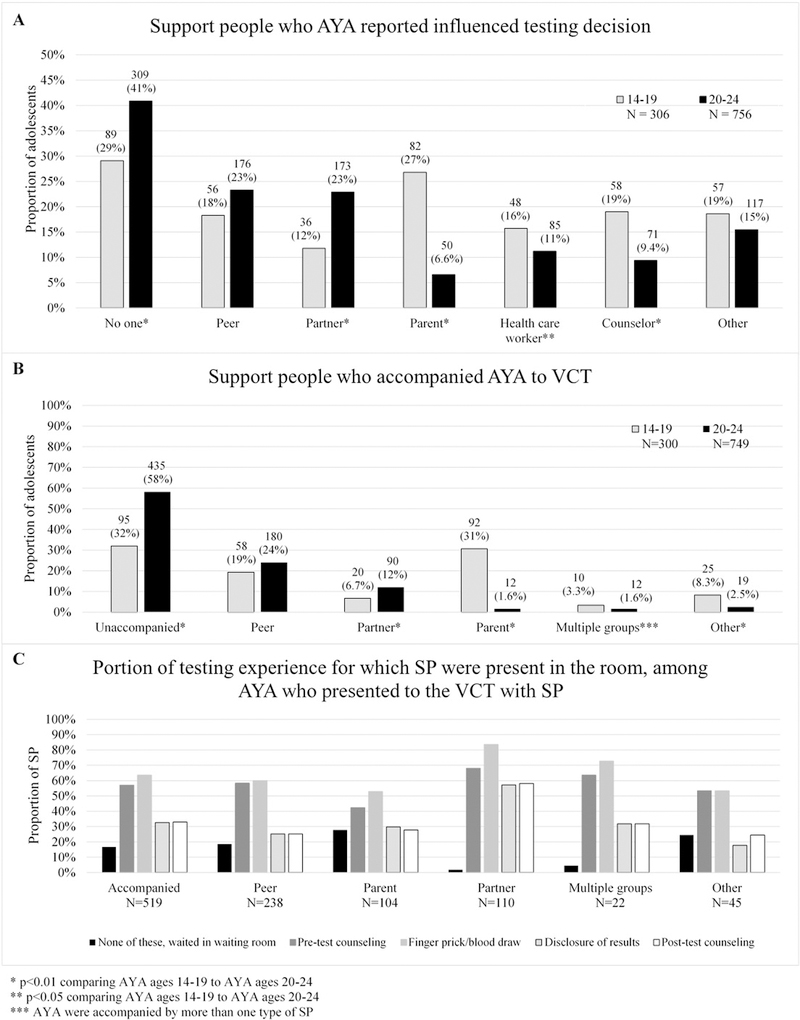
Role of support people in adolescent and young adult HIV testing experience.
Support person involvement in the HIV testing visit
Over half of AYA presented to the VCT alone (Table 1), though it was more common for young adults than adolescents to present alone (58% vs 32%, p<0.001; Figure 1B). Young adults were more likely to present with a partner (12% vs 6.7%, p<0.001) than adolescents, while adolescents were more likely to present with a parent (31% vs 1.6%, p<0.001) compared to young adults (Figure 1B). Adolescents and young adults were equally likely to present with a peer (19% vs 24%, p=0.101; Figure 1B), or in a group (3.3% vs 1.6%, p=0.077; Figure 1B).
Role of SP in test experience
Among the 519 AYA who were accompanied to the VCT by a support person, 17% waited in the waiting room for AYA to complete testing, 57% were present for pre-test counseling, 64% were present for the finger prick/blood draw, 33% were present for disclosure of results, and 33% were present for post-test counseling (Table 1). This was similar between adolescents and young adults for pre-test counseling, finger prick/blood draw, and disclosure of results. SP accompanying young adults were more likely to be present for post-test counseling compared to adolescents (p=0.04).
Partners were more involved in all parts of the testing visit compared to peers and parents. Of partners who accompanied the AYA to the clinic, 2% stayed in the waiting room during the entire AYA testing experience, whereas 18% of peers and 28% of parents waited (Figure 1C). Fifty-seven percent of partners, 30% of parents and 25% of peers were present for disclosure of HIV results (Figure 1C).
Cofactors for presenting with SP
Correlates of presenting with a support person included younger age (aRR: 1.55 [95%CI: 1.30–1.85]), female sex (aRR: 1.45 [95%CI: 1.21–1.73]), and school enrollment (aRR: 1.41 [95% CI: 1.05–1.88]). Among AYA enrolled in school, females were more likely than males to present with peers for HIV testing in both the adolescents (25% vs. 13%, p=0.019) and young adults (35% vs. 18%, p<0.001). Female and male AYA enrolled in school were equally as likely to present with parents (adolescents: 31% vs 32%, p=0.750; young adults: 1.6% vs. 1.9%, p=0.801) and partners (adolescents: 7.8% vs 4.8%, p=0.329; young adults: 14% vs 9.0%, p=0.058) after stratifying by age group.
Discussion
Our findings revealed age-specific differences in patterns of SP accompanying AYA to the clinic for testing and influencing their decision to test for HIV. Our data suggest that SP play an important role in AYA HIV testing and may be an under-utilized resource to promote AYA HIV testing in Africa.
UNAIDS has set 90–90-90 goals, aiming by 2020 for 90% of people living with HIV to know their HIV status, 90% of people with diagnosed HIV infection receiving sustained ART, and 90% of people receiving ART to be virally suppressed for all age strata, but AYA lag behind (NASCOP, 2016). To reach the first “90” goal, scaling up HTS for AYA is critical; HTS provides an opportunity to identify and link HIV-positive AYA to care and also to link HIV-negative AYA to prevention services and promote repeat testing. However, AYA have historically low levels of proactive care-seeking and low utilization of prevention services (WHO, 2002, 2014). To increase uptake of HTS, it is important to simultaneously generate demand for HTS and make HTS more accessible and acceptable for AYA.
One possible strategy to increase uptake may be to leverage SP to influence AYA to test and making HTS more accessible by accompanying adolescents to a clinic, providing emotional and/or financial/logistical support. SP may also be critical in reaching the second and third “90s” by supporting HIV-positive AYA to engage and remain in care and treatment (Chaiyachati et al., 2014; Ruria et al., 2017). Many interventions to improve AYA health are intended to be delivered by overburdened healthcare workers; SP could be utilized to promote HIV testing and care for AYA by providing appropriate knowledge and support outside of the healthcare setting.
AYA are a diverse population in terms of emotional and financial autonomy, thus it is critical to understand the evolving role that different SP play at different AYA ages to inform more effective and targeted interventions. For example, a VCT clinic might approach demand creation differently for adolescents and young adults; to increase demand among adolescents, counselors might target parents or caregivers to bring their children for HTS (Ahmed et al., 2017) while they might use a social network approach to increase demand for young adults among their peer and partner networks (Latkin et al., 2013). Similarly, visual promotional materials to encourage HTS, such as posters or pamphlets, might depict young adults with partners or peers and adolescents being accompanied by a caregiver.
Our data support earlier reports noting the importance of family and peer influence in AYA decision-making around sexual and reproductive health services and HIV testing (Bastien et al., 2011; Bhoobun et al., 2014; Boyer et al., 2013; Lamb et al., 2014; MacPhail et al., 2009; Mwale et al., 2017; Strauss et al., 2015; Talib et al., 2013). In our study, authoritative figures, such as parents, healthcare workers, and counselors, were more likely to have informed the decision to test for HIV in adolescents compared to young adults. Adolescents were also most likely to be accompanied by parents than by any other type of SP. These data suggest that parental communication, which has been associated with AYA HIV testing in a different setting (Balaji et al., 2017) could impact uptake of HIV testing among adolescents. Additionally, HCW prompted HTS could be a key intervention for uptake of HIV testing among adolescents outside of inpatient settings, which is where provider-initiated HIV testing and counseling is most commonly delivered to children and adolescents, and linkage to care among HIV-positive adolescents.
Young adults were primarily influenced by peers and partners to test and were more likely to be accompanied by partners compared to adolescents. Partner involvement in the testing experience was common; 57% of partners were present for disclosure of results, suggesting that the test visit is an important interventional opportunity for counselors to assist with early disclosure and building social and emotional support from the moment of learning one’s results. Group testing is also common in this clinic, where many students present together for testing after school but complete testing individually. Promotion of group presentation for testing may be an intervention that merits further investigation to increase uptake of AYA HTS.
Many participants reported that SP were present during the pretest counseling, blood draw/prick, and post-test counseling. SP were most frequently present during the blood draw period, which could suggest that this is the most fearful component of HTS, requiring more support. Consistent with this need for support, qualitative research performed among AYA in the parent study found some AYA desired concurrent HIV testing with their parents, and found this to be an appropriate emotional environment in which to learn their own HIV status (Wilson et al., 2017).
While there has been little research to date focused specifically on the role of SP in the AYA HIV testing visit, our results are relatively consistent with existing literature that has examined HIV testing behaviors in AYA. In 1998, the Horizons Program, which studied facilitators, barriers, and perceptions among young adults presenting at VCT Centers in Nairobi, reported that 36% of AYA aged 14–21 were unaccompanied to the clinic for testing and AYA were most likely to be accompanied to the clinic by peers (Horizons Program, 2001). Our study found that half of AYA were unaccompanied but that young adults were most likely to be accompanied by peers and adolescents were more likely to present with parents than peers, differing slightly from the Horizons study.
Our study has some limitations. This was a cross-sectional study; therefore, we cannot assume a temporal relationship or infer causality between exposures and outcomes. For example, it is difficult to determine whether an AYA decided to get his/her HIV test and then was accompanied to the clinic by SP or whether SP accompanied an AYA to KNH and then the AYA received his/her HIV test. KNH is a referral hospital in Nairobi; people tend to travel far to receive care here and may thus have socioeconomic status or stigma concerns that are distinct from the general population. Additionally, a large proportion of participants were young adults and university students. Among those enrolled, approximately two thirds of AYA enrolled had previously been tested for HIV (Wagner et al., 2017). The data, therefore, may not be generalizable to other settings, for instance, in rural Kenya. Our study did not assess AYA motivations for HIV testing or whether AYA or SP were the primary agents who initiated the HIV test; in our formative studies, healthcare workers cited conflicting parent/AYA desires to test for HIV to be a challenge (Wilson et al., 2017). However, programs and counseling procedures should account for the possibility for conflicting child/parent wishes and seek to balance the need for AYA autonomy and confidentiality with the important role SP can play while still providing critical health information and treatment.
Peers, partners, and parents play an important role in a Kenyan AYAs’ testing decisions and experience. Defining the role of SP in the HIV testing visit and AYA care-seeking behaviors can inform strategies that leverage this support to increase demand and uptake of AYA HIV testing and linkage to care. Further research on how SP can be utilized to promote AYA HIV testing is necessary. Understanding AYA motivations for testing for HIV may also be important to further define the role of SP in AYA HIV testing and to target age-appropriate interventions to promote uptake of HTS services and earlier linkage to care.
Table 2:
Comparing accompanied and unaccompanied adolescents and young adults presenting for HIV testing.
| Accompanied (Unaccompanied is referent) N=1,049 |
||||||
|---|---|---|---|---|---|---|
| Cofactors | Accompanied N=519 n (%) |
Unaccompanied N=530 n (%) |
RR | p-value | aRR | p-value |
| Age (in years) | 0.89 (0.86, 0.92) | <0.001 | 0.90 (0.87, 0.93)* | <0.001 | ||
| 14–19 | 205 (40%) | 95 (18%) | 1.63 (1.37, 1.94) | <0.001 | 1.55 (1.30, 1.85) * | <0.001 |
| 20–24 | 314 (61%) | 435 (82%) | REF | REF | REF | REF |
| Female | 329 (63%) | 220 (42%) | 1.58 (0.32, 1.89) | <0.001 | 1.45 (1.21, 1.73)** | <0.001 |
|
Highest level of education completed |
0.96 (0.94, 0.98) | <0.001 | 1.58 (1.32, 1.89)* | <0.001 | ||
| Primary | 24 (4.6%) | 18 (3.4%) | 1.27 (0.84, 1.92) | 0.264 | 1.28 (0.84, 1.94)* | 0.246 |
| Secondary | 178 (34%) | 125 (24%) | 1.30 (1.08, 1.57) | 0.005 | 1.33 (1.10, 1.60)* | 0.003 |
| Polytechnic | 14 (2.7%) | 18 (3.4%) | 0.97 (0.57, 1.66) | 0.912 | 1.06 (0.62, 1.81)* | 0.834 |
| University/college | 303 (58%) | 369 (70%) | REF | REF | REF | REF |
|
Currently enrolled in school |
469 (90%) | 441 (83%) | 1.43 (1.07, 1.92) | 0.016 | 1.41 (1.05, 1.88)* | 0.021 |
|
First time receiving an HIV test (N=490) |
174 (37%) | 130 (27%) | 1.28 (1.06, 1.54) | 0.011 | 1.01 (0.83, 1.24)*** | 0.895 |
Adjusted for sex; age and education were collinear
Adjusted for age as a continuous linear term; age and education were collinear
Adjusted for age as a continuous linear term and sex; age and education were collinear
Acknowledgements
The authors thank the DASH study participants and their families, without whom this research would not be possible. We thank the Kenyatta National Hospital staff at the VCT, Youth Center, and tents for their tremendous efforts. We thank the DASH administrative and data team for their dedication and support. We thank the Kenyan National AIDS and STI Control Programme (NASCOP) for valuable input during study design, conduct, and dissemination. We thank members of the Kizazi Working Group (UW Global Center for Integrated Health of Women, Adolescents and Children (Global WACh)) and Kenya Research & Training Center (KRTC) for their support during the preparation of this article.
Funding
This research was funded by National Institutes of Health (Supplement to P30 AI027757). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Funding sources were not involved in the analyses or interpretation of data.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ahmed S, Sabelli RA, Simon K, et al. Index case finding facilitates identification and linkage to care of children and young persons living with HIV/AIDS in Malawi. Trop Med Int Health 2017;22(8):1021–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaji AB, Oraka E, Fasula AM, et al. Association between parent-adolescent communication about sex-related topics and HIV testing, United States. 2006–2013. AIDS Care 2017;29(3):344–349 [DOI] [PubMed] [Google Scholar]
- Bastien S, Kajula LJ, Muhwezi WW. A review of studies of parent-child communication about sexuality and HIV/AIDS in sub-Saharan Africa. Reprod Health 2011;8:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhoobun S, Jetty A, Koroma MA, et al. Facilitators and barriers related to voluntary counseling and testing for HIV among young adults in Bo, Sierra Leone. J Community Health 2014;39:514–520. [DOI] [PubMed] [Google Scholar]
- Boyer CB, Hightow-Weidman L, Bethel J, et al. An assessment of the feasibility and acceptability of a friendship-based social network recruitment strategy to screen at-risk African American and Hispanic/Latina young women for HIV infection. JAMA Pediatr 2013;167:289–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaiyachati KH, Ogbuoji O, Price M, et al. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS 2014;28 Suppl 2:S187–204. [DOI] [PubMed] [Google Scholar]
- Horizons Program. HIV Voluntary Counseling and Testing Among Youth. Kenya Project Partners and Uganda Project Partners, ed. Results from an exploratory study in Nairobi, Kenya and Kampala and Masaka, Uganda The Population Council Inc; 2001. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Data Sheet: Number of People Living with HIV AIDSinfo; 2016. [Google Scholar]
- Lamb MR, Fayorsey R, Nuwagaba-Biribonwoha H, et al. High attrition before and after ART initiation among youth (15–24 years of age) enrolled in HIV care. AIDS 2014;28:559–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Davey-Rothwell MA, Knowlton AR, et al. Social Network Approaches to Recruitment, HIV Prevention, Medical Care, and Medication Adherence. J Acquir Immune Defic Syndr 2013;63 Suppl 1:S54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPhail C, Pettifor A, Moyo W, Rees H. Factors associated with HIV testing among sexually active South African youth aged 15–24 years. AIDS Care 2009;21(4):456–467. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and National AIDS Control Council. Kenya AIDS Response Progress Report 2016 Nairobi, 2016. [Google Scholar]
- Mwale M, Muula AS. Systematic review: a review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-Saharan Africa. BMC Public Health 2017;17(1):718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Green EP, Sikkema KJ, et al. A church-based intervention for families to promote mental health and prevent HIV among adolescents in rural Kenya: Results of a randomized trial. J Consult Clin Psychol 2016;84(6):511–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R, Ahluwalia SC, Xenakis L, et al. A systematic review of peer-supported interventions for health promotion and disease prevention. Prev Med 2017;101:156–170. [DOI] [PubMed] [Google Scholar]
- Ruria EC, Masaba R, Kose J, et al. Optimizing linkage to care and initiation and retention on treatment of adolescents with newly diagnosed HIV infection. AIDS 2017;31 Suppl 3:S253–S260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siceloff ER, Wilson D, Van Horn L. A Longitudinal Study of the Effects of Instrumental and Emotional Social Support on Physical Activity in Underserved Adolescents in the ACT Trial. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine 2014;48(1):71–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss M, Rhodes B, George G. A qualitative analysis of the barriers and facilitators of HIV counselling and testing perceived by adolescents in South Africa. BMC Health Serv Res 2015;15:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talib HJ, Silver EJ, Coupey SM, Bauman LJ. The influence of individual, partner, and relationship factors on HIV testing in adolescents. AIDS Patient and Care STDs 2013;27:637–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner AD, Mugo C, Bluemer-Miroite S, et al. Continuous quality improvement intervention for adolescent and young adult HIV testing services in Kenya improves HIV knowledge. AIDS 2017;31 Suppl 3:S243–S252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KS, Beima-Sofie KM, Moraa H, et al. “At our age, we would like to do things the way we want: “ a qualitative study of adolescent HIV testing services in Kenya. AIDS 2017;31 Suppl 3:S213–S220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). Adoelescence: a period needing special attention. Health for the World’s Adolescents: A second chance in the second decade 2014.
- World Health Organization (WHO). Towards adolescent-responsive health systems. Health for the World’s Adolescents: A second chance in the second decade 2014.
- World Health Organization (WHO). Adolescent Friendly Health Services Geneva, 2002. [Google Scholar]


