Abstract
Although the last decade has seen a proliferation of research on mental illness stigma, lack of consistency and clarity in both the conceptualization and measurement of mental illness stigma has limited the accumulation of scientific knowledge about mental illness stigma and its consequences. In the present article, we bring together the different foci of mental illness stigma research with the Mental Illness Stigma Framework (MISF). The MISF provides a common framework and set of terminology for understanding mechanisms of mental illness stigma that are relevant to the study of both the stigmatized and the stigmatizer. We then apply this framework to systematically review and classify stigma measures used in the past decade according to their corresponding stigma mechanisms. We identified more than 400 measures of mental illness stigma, two thirds of which had not undergone any systematic psychometric evaluation. Stereotypes and discrimination received the most research attention, while mechanisms that focus on the perspective of individuals with mental illness (e.g., experienced, anticipated, or internalized stigma) have been the least studied. Finally, we use the MISF to discuss the strengths and weaknesses of mental illness stigma measurement, identify gaps in the literature, and provide recommendations for future research.
Keywords: stigma, mental illness stigma, Mental Illness Stigma Framework
“A sustainable, coherent theory of stigma can improve…stigma research and intervention planning because how we define stigma structures our understanding of how to measure it, and how to design and evaluate interventions”
(Deacon, 2006 pg. 419)
“The terminology we use…should be clear, precisely defined, and used consistently to aid unambiguous clinical and scientific communication and promote clearer appraisal of, and generalizations from, empirical findings”
(Kelly, 2004 pg. 80)
Mental illness stigma is as a major obstacle to well-being among people with mental illness (PWMI). According to findings from the most recent nationally representative study of public attitudes toward mental illness in the U.S., only 42% of Americans aged 18–24 believe PWMI can be successful at work, 26% believe that others have a caring attitude toward PWMI, and 25% believe that PWMI can recover from their illness (NAMI-GC, 2013; Substance Abuse and Mental Health Services Administration [SAMHSA], 2008). A robust body of evidence demonstrates that PWMI experience discrimination in nearly every domain of their lives, including employment (Farina & Felner, 1973; Link, 1987; Stuart, 2006), housing (Corrigan et al., 2003; Farina, Thaw, Lovern, & Mangone, 1974), and medical care (Thornicroft, Rose, & Kassam, 2007). Experiences of stigma are associated with increased symptom severity (e.g., Boyd, Adler, Otilingham, & Peters, 2014), decreased treatment seeking (e.g., Corrigan, 2004) and treatment non-adherence (e.g., Sirey et al., 2001).
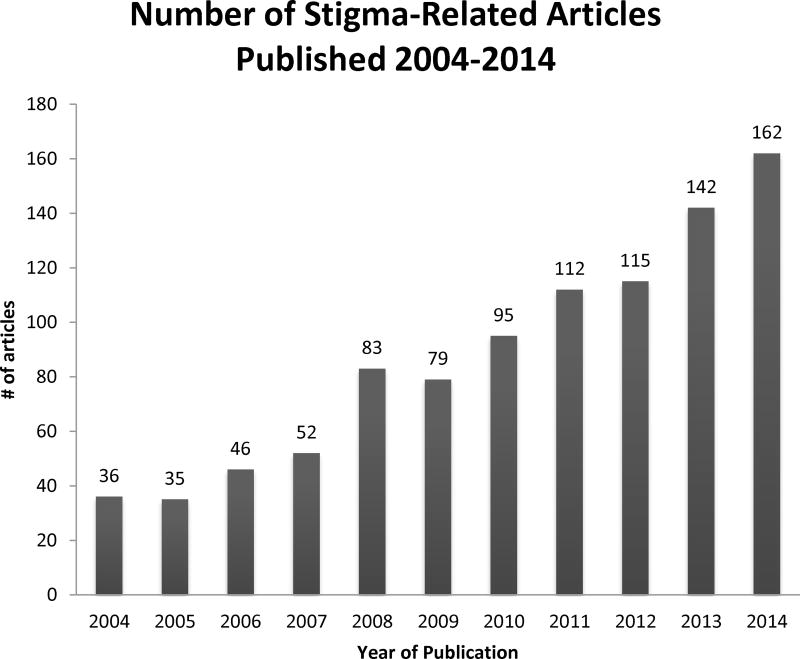
Given the prevalence of mental illness and the deleterious effects of stigma, mental illness stigma has been a widely studied research topic in a variety of disciplines, including psychology, sociology, public health, and medicine. Beginning with Erving Goffman’s (1963) seminal essay Stigma: Notes on the Management of Spoiled Identity, research on stigma has continued to grow each year, with the majority of stigma research occurring in the last decade (Bos, Pryor, Reeder & Stutterheim, 2013). Across disciplines, but especially within the field of psychology, researchers have been primarily concerned with examining mental illness stigma at the individual level (Link & Phelan, 2001). As Figure 1 demonstrates, the number of published, peer-reviewed mental illness stigma articles appearing in searches of PubMed, PsycInfo/EBSCO, and Web of Science has steadily increased each year for the past ten years. As the psychological research on mental illness stigma has progressed, the stigma construct has been parsed into a number of different constructs, or mechanisms. Borrowing from the work of Link (2001), we use the term “stigma mechanism” throughout the present article to emphasize that these different constructs represent ways in which individuals respond to having, or not having, a mental illness (Earnshaw & Chaudoir, 2009; Link, 2001).
Figure 1.
Number of Stigma-Related Peer-Reviewed Publications appearing in searches of EBSCO/PsycInfo databases, PubMed, and Web of Science, 2004–2014
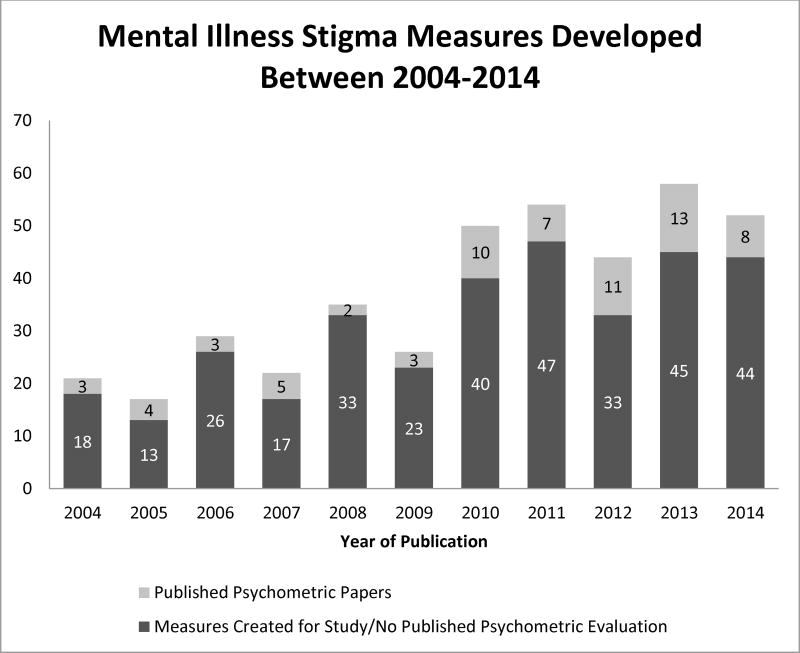
The proliferation of research on mental illness stigma mechanisms in the psychological literature has been accompanied by a sharp increase in stigma measures. In 2004, Link and colleagues published a review of mental illness stigma measures, with guidelines and suggestions for researchers interested in studying and measuring mental illness stigma. In addition to describing the already substantial number of stigma measures that existed at that time, they identified a number of gaps in stigma measurement, including the need for measures related to the experiences of PWMI (e.g., internalized stigma). As Figure 2 demonstrates, more than 400 new measures of mental illness stigma have been developed since 2004. The overabundance of measures may be attributed, in part, to the lack of consistency in how stigma mechanisms are defined, which may make it difficult for researchers to identify existing measures that meet their needs. Such inconsistencies in terminology and measurement make it difficult to evaluate the state of the field, and in turn, may hinder efforts to develop interventions to reduce or eliminate mental illness stigma.
Figure 2.
Mental Health Stigma Measures Identified in searches of EBSCO/PsycInfo databases, PubMed, and Web of Science, 2004–2014
Aims of the Review
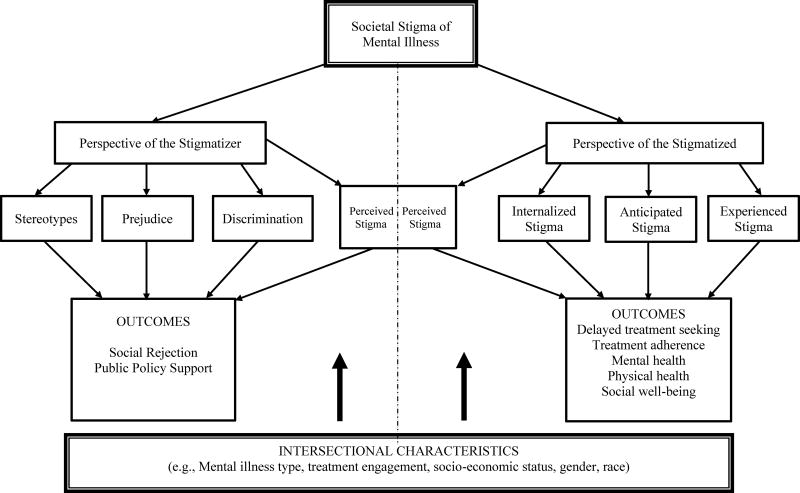
In the present article, we first review existing limitations and challenges currently facing the mental illness stigma literature with a primary focus on the psychological literature. Next, we bring together the different foci of mental illness stigma research in an overarching conceptual framework for understanding how individuals experience stigma, the Mental Illness Stigma Framework (Figure 3). After overviewing key aspects of this framework—and their associated benefits for organizing mental illness stigma research, we demonstrate the usefulness of this framework by applying it— to systematically review and classify mental illness stigma measures that have appeared in the literature since Link and colleagues’ (2004) previous measure review. We then identify gaps in the literature and limitations with the measurement of mental illness stigma, and provide recommendations for future research.
Figure 3.
The Mental Illness Stigma Framework
Because stigma is a social process that manifests at multiple levels, researchers in fields such as sociology and anthropology have also developed theoretical perspectives on mental illness stigma. Many of these theories consider the processes whereby mental illness stigma is socially constructed and reinforced. Consequently, researchers from other fields have studied other forms of stigma including structural stigma (e.g., Hatzenbuehler, Phelan, & Link, 2013) as well as cultural manifestations of stigma (e.g., Abdullah & Brown, 2011; Yang et al., 2007). In the present review, we focus our attention on individual-level experiences of stigma, and draw from a substantial body of primarily psychological literature to further understanding of how individuals experience, and are impacted by, mental illness stigma. In the discussion section, we briefly consider how other forms of stigma may contribute to our larger understanding of how mental illness stigma operates.
Limitations and Challenges of the Mental Illness Stigma Literature
Clear and consistent terminology is important to all fields of inquiries. A number of researchers have pointed out the confusion, complexity, and/or lack of clarity in the mental illness stigma literature (e,g., Angermeyer & Dietrich, 2006; Brohan et al., 2010; Livingston & Boyd, 2010; Thornicroft, 2008). This lack of conceptual clarity is not unique to mental illness stigma research. In reference to the HIV/AIDS stigma literature, Deacon (2006) noted that “the concept of stigma has suffered from ‘conceptual inflation’ and a consequent lack of analytical clarity” (pg. 419). For example, the term “stigma” is often used to refer to “both the stigmatizing beliefs themselves and the effects of these stigmatization processes” (p. 419). The same can be said for the mental illness stigma literature, and even the broader stigma construct itself, which has been criticized for its complexity and variability in definitions both within and across disciplines (Link & Phelan, 2001; Pescosolido & Martin, 2015; Phelan, Link, & Dovidio, 2008).
A prominent issue within the mental illness stigma literature is that researchers frequently use different terms to describe the same stigma concepts and the same terms to refer to different constructs. For example, the term perceived stigma is sometimes used to refer to what others term experienced stigma or internalized stigma. The concept of anticipated stigma, as we define it in this article, is sometimes referred to as stigma concerns, stigma apprehension, or stigma consciousness. And the terms internalized stigma and self-stigma are often used interchangeably. This proliferation of terminologies and definitions of mental illness stigma represent a critical barrier to the advancement of mental illness stigma research. A search for articles on experienced stigma may not reveal important research on perceived stigma; a search for anticipated stigma may not reveal articles on stigma concerns, and a search for studies of perceived stigma could produce studies of not only perceived stigma, but also studies of stereotypes, prejudice, and discrimination, as well as experienced or internalized stigma.
Another challenge to the field has been the siloing of research based on the particular type of mental disorder under study. Mental illness encompasses a broad and diverse set of disorders and it is possible that mental illness stigma may manifest slightly differently depending on the type of disorder with which an individual has been labeled. For example, an individual diagnosed with Schizophrenia may be viewed as more dangerous than someone diagnosed with an anxiety or depressive disorder (Feldman & Crandall, 2007). Likewise, because the cause of posttraumatic stress disorder is typically believed to be external rather than internal (i.e., trauma exposure), an individual diagnosed with this disorder is likely to be considered less responsible for their mental illness than an individual diagnosed with a personality disorder.
While a disorder–specific approach to the study of mental illness stigma has a number of benefits, in the present review we have taken a broader approach for several reasons. First, a broad approach can bring together the common threads of the experiences of mental illness stigma. Second, such an approach is consistent with macro-level theories of stigma that cross-cut stigmatized identities (Link & Phelan, 2001; Phelan, Link & Dovidio, 2008; Pescosolido & Martin, 2015), as well as meta-analyses demonstrating that the effects of stigma are similar across a variety of stigmatized conditions (Pascoe & Smart Richman, 2009) and different mental health disorders (Mak, Poo, Pun, & Cheung, 2007). Third, the feasibility of a broad approach is evidenced by the finding that stigmatization of PWMI is driven by three core stereotypes—dangerousness, rarity, and responsibility—and disorders can be ranked in terms of their level of social rejection (Feldman & Crandall, 2007; Silton, Flannelly, Milstein, & Vaaler, 2011). Finally, van Brakel (2006) argues that the impact of stigma is similar across a variety of health conditions, suggesting that generic stigma measures can provide an accurate assessment of how people experience stigma. This work suggests that a macro-level framework of mental illness stigma could provide much needed clarity to the field of mental illness stigma research.
Another limitation of mental illness stigma literature is that most of the existing stigma models and frameworks do not incorporate stigma concepts that are relevant to both research on the stigmatizer and the stigmatized. Yet, such an approach has important benefits, as the inclusion of the perspective of both individuals who have and do not have mental illness recognizes that experiences and outcomes of stigma are fundamentally shaped by whether the individual possesses the socially devalued characteristic. Classic theories of stigma (Link & Phelan, 2001), as well as theories of intergroup relations (Allport, 1954; Brewer, 2007) emphasize that “separation” is an important component of stigma. The distinction between “us” and “them” is what allows stigma to unfold (Link & Phelan, 2001).
To address some of the limitations of the mental illness stigma literature and guide our review of mental illness stigma measures, we developed the Mental Illness Stigma Framework (MISF; Figure 3). The development of the MISF was informed by a number of prominent mental illness stigma theories, conceptualizations and definitions, including modified labeling theory (Link, Cullen, Struening, Shrout, & Dohrenwend, 1989), Link and Phelan’s (2001) definition of stigma, social cognitive theory of public and self-stigma (Corrigan & Watson, 2002; Corrigan, Watson, & Barr, 2006; Corrigan, Kerr, & Knudson, 2005), Pryor and Reeder’s (2011) four manifestations of stigma, the constructs of anticipated and experienced discrimination (Brohan et al., 2013; Thornicroft et al., 2007), and the construct of internalized stigma (Boyd Ritsher, Otilingam, & Grajales, 2003). Our proposed framework is meant to complement, not replace, existing frameworks, models, or theories. A key benefit of the framework is that by integrating existing definitions and conceptualizations of mental illness stigma through common terminology, we tie together the immense and varied body of mental illness stigma research and delineated the types of stigma that are most important to outcomes for people with and without mental illness, regardless of the specific condition under study.
The Mental Illness Stigma Framework
The top box of the MISF represents the identification of mental illness as a culturally-situated and socially devalued identity. How do individuals understand, respond to, and experience mental illness stigma? The answer to this question depends on whether an individual has experienced a mental illness. Existing research on mental illness stigma at the individual level can be broken down into two major categories: Research focused on the perspective of those doing the stigmatizing, typically the general public, and research focused on those who are on the receiving end of stigmatization, individuals with mental illness (or a history of mental illness). Thus, the MISF separates stigma mechanisms accordingly. Separating stigma mechanisms based on perspective is consistent with existing theories and definitions of stigma, (Bos, et al., 2013; Clement et al., 2015; Corrigan & Watson, 2002; Corrigan, Rafacz, & Rusch, 2011; Link & Phelan, 2001; Martin, Pescosolido, Olafsdottir, & McLeod, 2007; Pescosolido & Martin, 2015; Pryor & Reeder, 2011; van Brakel, 2006).
Perspective of the Stigmatizer
Drawing from the social psychological (Allport,1954; Brewer, 2007; Dovidio, Glick, & Rudman, 2005; Nelson, 2009), mental illness (Corrigan et al., 2005; Corrigan & Watson, 2002; Thornicroft, Rose, Kassam, & Sartorius, 2007), and broader stigma literature (Bos, Pryor, & Reeder, 2013; Pryor & Reeder, 2011), the three mechanisms that are most relevant to individuals who do not have (or have never had) a mental illness are stereotypes, prejudice, and discrimination. These three mechanisms represent the cognitive, affective, and behavioral responses people may have to someone who possesses a devalued identity. Stereotypes are beliefs, or “cognitive schemas” about the characteristics and behaviors of groups of individuals (Corrigan, 2005; Dovidio, Hewstone, Glick, & Esses, 2010; Stangor, 2009) and represent the cognitive response to someone with mental illness stigma. The core stereotypes associated with mental illness include dangerousness, rarity, responsibility, incompetence, weakness of character, and dependence (Feldman & Crandall, 2007; Taylor & Dear, 1981).
The affective component of mental illness stigma is reflected in prejudice, defined as the emotional reaction or feelings that people have toward a group or member of a group (Stangor, 2009). Most often, these feelings are negative, although they do not necessarily need to be. The most common forms of prejudice toward PWMI are fear, pity, and anger (Corrigan, 2005; Corrigan, Watson, Warpinksi, & Garcia, 2004). Prejudice is strongly connected to stereotypes. As examples, the stereotype of dangerousness may lead to feelings of fear and the stereotype of incompetence may lead to feelings of pity. Prejudice toward PWMI may also be expressed or experienced as anxiety, leading to awkward interactions (Hebl, Tickle, & Heatherton, 2000) and/or serve as a precursor to the behavioral aspect of stigma, discrimination. Discrimination is defined as the unfair or unjust behaviors directed at PWMI (Allport, 1954; Brewer, 2007). Discriminatory behaviors exist along a continuum from subtle to overt, but which result in the “differential and disadvantaged treatment of the stigmatized” (Pescosolido & Martin, 2015). There are four common types of discrimination directed towards PWMI described in the literature: withholding help, avoidance, segregation, and coercion (Corrigan & Rüsch, 2002; Corrigan & Watson, 2002).
Stereotypes, prejudice, and discrimination lead to a range of outcomes that affect both people living with and without mental illness. Individuals who endorse stigmatizing attitudes toward PWMI are less likely to support insurance parity (i.e., covering mental illness at the same level as other medical conditions) and increased government funding for mental health treatment (Barry & McGinty, 2014). In the workplace, discrimination can limit the economic opportunities of PWMI. Additionally, these mechanisms prevent people without diagnoses of mental illness from seeking mental health support to avoid gaining the label of mental illness (Corrigan, 2004).
Perspective of the Stigmatized
Three stigma mechanisms are most relevant to PWMI (or people with a history of mental illness): experienced stigma, anticipated stigma, and internalized stigma. Experienced stigma is defined as experiences of stereotypes, prejudice, and discrimination from others in the past or present (Cechnicki, Angermeyer & Bielańska, 2011; Quinn & Earnshaw, 2011; Wahl, 1999) and is sometimes referred to as enacted stigma (Bos et al., 2013). Experienced stigma includes both chronic, day-to-day experiences of unjust or unfair treatment (e.g., interpersonal slights) as well as acute, major experiences (e.g., fired from one’s job), both of which are related to a range of deleterious outcomes among people with stigmatized identities (Williams, Neighbors, & Jackson, 2003). Anticipated stigma, sometimes referred to as felt stigma (Bos et al., 2013), is defined as the extent to which a person with mental illness expects to be the target of stereotypes, prejudice, or discrimination in the future (Quinn & Chaudoir, 2009; Quinn & Earnshaw, 2011). Because PWMI are likely aware of the negative stereotypes associated with mental illness and negative ways in which PWMI are treated, they may worry about people viewing them as weak or dangerous, being afraid or avoiding them, or being denied work. PWMI may therefore anticipate stigma even if they have never personally experienced stigma. Finally, we define internalized stigma as the extent to which people endorse the negative beliefs and feelings associated with the stigmatized identity for the self (Bos et al., 2013; Boyd Ritsher et al., 2003; Corrigan, Watson, & Barr, 2006; Link, 1987; Quinn & Earnshaw, 2011). In other words, internalized stigma represents the application of negative stereotypes and prejudice to the self. For PWMI, this may involve perceiving that they are dangerous, to be blamed for their illness, are incompetent, or childlike (Taylor & Dear, 1981). Internalized stigma is sometimes referred to as self-stigma, a term which reflects the application of mental illness stigma to the self (Corrigan, Rafacz, & Rüsch, 2011; Corrigan & Rao, 2012). When an individual applies negative stereotypes of mental illness to the self, they may believe they are devalued (Quinn & Earnshaw, 2013), which in turn may lead to increased psychological distress (Ritsher & Phelan, 2004) or decreased self-esteem (Corrigan, et al., 2011; Corrigan & Rao, 2012).
Experienced, anticipated, and internalized stigma are associated with negative outcomes for PWMI. Perceived and anticipated stigma undermine mental illness treatment adherence and initiation (Corrigan, 2004; Sirey et al., 2001). Anticipated and experienced stigma are stressors (Link & Phelan, 2006), which may elicit psychological and physiological stress responses that impact mental and physical health. Internalized stigma is associated with depression, decreased self-esteem, and increased symptom severity (Boyd et al., 2014).
Perceived Stigma
Perceived stigma is the one stigma mechanism in the framework that is shared by both people with and without mental illness. We define perceived stigma as perceptions of societal beliefs (stereotypes), feelings (prejudice), and behaviors (discrimination) toward PWMI (Bos et al., 2013; Griffiths, Christensen, Jorm, Evans, & Groves, 2004; Link, 1987). Perceived stigma is distinct from an individual’s own beliefs, feelings, and behaviors about PWMI, which Griffiths and colleagues refer to as personal stigma (and which is captured by the mechanisms of stereotypes and discrimination in the MISF). Research has established the importance of treating personal and perceived stigma as distinct constructs. Griffiths et al. (2008) found that whereas people’s own stigma-related beliefs were associated with greater psychological distress, less previous contact with people with depression, and lower depression literacy, perceived stigma was only associated with psychological distress. Additionally, demographic variables (e.g., gender, age, education, experience with someone with depression, country of birth) explained 22% of the variance in individual’s own stigma-related beliefs, while only explaining 1.6% for perceived stigma.
The extent to which people perceive the stigma of mental illness is shaped by whether they have experienced mental illness. For example, studies have shown a positive relationship between mental illness symptom severity and perceived stigma (Freidl, Piralic, Spitzl, & Aigner 2008; Golberstein, Eisenberg, & Gollust, 2008; Griffiths et al., 2008). Further, perceived stigma is associated with negative outcomes for PWMI. In Link’s (1987) seminal paper examining the negative labeling effects of mental illness, he showed that for PWMI who have been labeled as mentally ill, perceived discrimination and devaluation were associated with a number of negative outcomes associated with employment, earnings, and demoralization (Link, 1987; Link et al., 2004), but this was not the case for PWMI who had never received the label.
Intersectionality
Finally, the MISF recognizes that there is intersectionality in experiences of stigma, a perspective that emphasizes that individuals also live with other characteristics representing privilege and marginalization, and that it is important to take these other characteristics into account in order to understand their lived experiences and outcomes (Cole, 2009; Crenshaw, 1991; hooks, 1990). This perspective therefore allows for commonality in experiences of stigma across all PWMI, while simultaneously emphasizing that individual experiences of mental illness stigma may vary depending on one’s specific mental illness diagnosis, treatment engagement, socio-economic status, gender, race, culture, and/or other characteristics.
Application of the Mental Illness Stigma Framework to Measurement
The proliferation of research on mental illness stigma has been accompanied by a stark increase in stigma measures. While the availability of multiple measures is not inherently problematic, the development of new measures may be inefficient when validated measures of the same construct already exist. The availability and use of so many measures can also present difficulties for researchers trying to draw broad conclusions from the literature. In their meta- analysis of stigma change programs, Corrigan and colleagues (2012) noted that there were 22 different outcome measures in their analysis, assessing a range of attitudes, affects, and behavior intentions. As the choice of measures is tied to how researchers define constructs, the use of so many measures can make it difficult to draw firm conclusions about mental illness research.
Additionally, to the extent that the mental illness stigma measures in use today do not differentiate between stigma mechanisms, researchers may miss opportunities to examine the implications of different stigma mechanisms and may inadvertently dilute or amplify the effects of one particular mechanism by failing to acknowledge that their measure reflects multiple mechanisms. For example, Livingston and Boyd (2010) found a robust negative relationship between internalized stigma, hope, self-esteem and treatment adherence, and a positive association between internalized stigma and symptom severity in their meta-analysis. However, their broad definition of internalized stigma incorporated measures of experienced stigma, anticipated stigma, stereotypes, and perceived stigma. While their findings present a broad picture of the relationship between mental illness stigma and various outcomes, they cannot inform conclusions about the role of internalized stigma as defined by other researchers (Corrigan et al., 2006; Quinn & Earnshaw, 2011).
Understanding which stigma mechanisms are being assessed in any given measure is vitally important. Each stigma mechanism may impact people uniquely. For example, a recent meta-analysis of stigma and help-seeking found that internalized stigma predicted help-seeking, whereas perceived, experienced, and anticipated stigma did not (Clement et al., 2015). To move the study of mental illness stigma forward, we need to identify measures that can be used to reliably and validly measure different mechanisms of mental illness stigma (Corrigan & Shapiro, 2010). In the next section, we use MISF to guide a systematic review and evaluation of mental illness stigma measures. We focused our review on the ten year period following Link et al.’s (2004) review of mental illness stigma measures. Unlike previous reviews (e.g., Brohan et al., 2010; Corrigan & Shapiro, 2010; Link et al., 2004), we provide a broad review of measures of mental illness stigma, whether validated or unvalidated, in order to present a comprehensive overview of the state of mental illness stigma measurement.
Method
We conducted a literature search on articles published between 2004 and 2014 using PubMed, EBSCO databases (PsycInfo, Academic Search Premier, Education Full Text, General Science Full Text, PsycArticles, Psychology and Behavioral Sciences Collection, Social Sciences Full Text, Women’s Studies International), and Web of Science. The search was limited to peer-reviewed, quantitative or empirical manuscripts published in English. Using titles, abstracts, and keywords, we searched for articles containing the keyword stigma and any of the following: mental health, mental illness, schizo*, depress*, anxiety, PTSD, posttraumatic, eating disorder*, anorexia, bulimia, or personality* disorder. We excluded the following keywords: epilepsy, HIV, AIDS, dementia. Next, we checked the reference sections of reviews and meta-analyses articles published in the past ten years (Brohan et al., 2010; Clement et al., 2015, Livingston & Boyd, 2010; Mak, Poon, Pun, & Cheung, 2007; Schomerus & Angermeyer, 2008) and our personal libraries for additional articles.
Screening of Studies
An initial screening of the titles and abstracts of 3901 articles resulted in the identification of 1282 articles that were potentially relevant to our review. The first author reviewed all 3901 articles and a second coder reviewed 1086 articles (35%) to ensure reliability. Coders agreed 95% of the time and all disagreements (n =51) were included in the full-text review. The full-text of each of the 1282 articles was then reviewed to determine if the study contained a mental illness stigma measure. After the full-text review, an additional 326 articles were excluded. In total, 957 articles contained at least one stigma measure. Supplemental Figure S1 contains the PRISMA diagram with the literature search details (Moher, Liberati, Tetzlaff, Altman, & The PRISMA Group, 2009).
Organizing Measures
For each of the 957 articles, we identified the stigma measure(s) that was used and classified it into one of two categories. The first category represents measures that have been cited in at least one study (not including the study in which the measure was originally published) and/or measures that have documented psychometrics. Measures in this category can be found in Table 1 (n = 140).
Table 1.
Mental Illness Stigma Measures and their Corresponding Mechanisms according to the Mental Illness Stigma Framework
| Year | Authors | Measure or Scale Name | Psychometric Characteristics |
Subscales | MI Stigma Mechanism |
N cites* |
Sample | |
|---|---|---|---|---|---|---|---|---|
| 1 | 1933 | Bogardus | Social Distance Scale | R, WE | D | 213 | Community | |
| 2 | 1987 | Link et al. | R | Community | ||||
|
| ||||||||
| 3 | 1962 | Cohen & Struening | Opinions about MI | DI, P, R, V, WE | Authoritarianism | S | 13 | Hospital personnel |
| 1963 | Struening & Cohen | Benevolence | S | |||||
| Hygiene | S | |||||||
| Social restrictiveness | S, D | |||||||
| Interpersonal etiology | S | |||||||
|
| ||||||||
| 4 | 1981 | Taylor & Dear | Community Attitudes Toward the Mentally Ill | DI, P, R, V, WE | Authoritarianism | S, D | 43 | Community/Undergrad |
| Benevolence | S, P | |||||||
| Social restrictiveness | S, D | |||||||
| Community MH ideology | S, P | |||||||
| 5 | 1996 | Wolff et al. | Community Attitudes Toward the Mentally Ill | DI | Fear and exclusion | S, P, D | Community | |
| Social control | S, D | |||||||
| Goodwill | P, D | |||||||
|
| ||||||||
| 6 | 2012 | Hogberg et al | New CAMI-S (Swedish) | DI, P, R | Intention to Interact | S, D | ||
| Fearful and avoidant | P, D | |||||||
| Open-minded and pro-integration | S, D | |||||||
| Community MH ideology | PD | |||||||
|
| ||||||||
| 7 | 1985 | Stephan & Stephan | Intergroup anxiety | DI, R, V, WE | P | 2 | Hispanic college students | |
| 2012 | Stathi et al. | Mental illness version | ||||||
|
| ||||||||
| 8 | 1986 | Link & Cullen | Perceived Dangerousness | R | S | 10 | Community | |
| 1987 | Link et al. | |||||||
|
| ||||||||
| 9 | 1987 | Kelly et al. | Social Interaction Scale | R, WE | D | 1 | Medical students | |
|
| ||||||||
| 10 | 1987 | Link | Perceived Devaluation-Discrimination Scale | R, V, WE | PS, PD | 124 | Community & Psychiatric | |
| 1989 | Link et al. | |||||||
| 1991 | Link et al. | |||||||
| 1997 | Link et al. | |||||||
| 11 | 2007 | Bjorkman et al. | Swedish version | P, R | PWMI | |||
| 12 | 2009 | Moses | Adolescent version | P, R, V | Adolescent MH | |||
|
| ||||||||
| 13 | 1988 | Weller & Grunes | Attitudes toward the Mentally Ill | R | S, P, D | 1 | Nurses | |
|
| ||||||||
| 14 | 1991 | Link et al. | Secrecy Scale | R, WE | Secrecy | AS | 10 | Psychiatric |
| 1997 | Link et al. | |||||||
| 2002 | Link et al. | |||||||
|
| ||||||||
| 15 | 1992 | Botega et al. | Depression Attitude Questionnaire | DI, P, R, WE | Antidepressant/ psychotherapy | 3 | Doctors | |
| Professional unease | ||||||||
| Inevitable course of depression | S | |||||||
| Identification of depression | S | |||||||
|
| ||||||||
| 16 | 1994 | Penn et al. | Penn Affective Reactions | R, WE | P | 9 | Undergraduates | |
| 17 | Penn Characteristics | R | S | 6 | ||||
| 18 | Penn Dangerousness | R | S | 4 | ||||
|
| ||||||||
| 19 | 1996 | Wolff et al. | Fear and behavioral intentions | Not reported | Fear | P | 1 | Community |
| 20 | 2011 | Svensson et al. | Fear and behavioral intentions | P, R (no support) | Behavioral intentions | D | ||
|
| ||||||||
| 21 | 1997 | Angermeyer and Matschinger | Emotional Reactions | DI, R | Feelings of anxiety | P | 5 | General population |
| Aggressive emotions | P | |||||||
| Prosocial reactions | ||||||||
|
| ||||||||
| 22 | 1997 | Batson et al. | Attitudes toward people with AIDS | R | S, P, D, PD | 1 | College students | |
| 2010 | Kalyanaraman et al. | Adapted for schizophrenia | ||||||
|
| ||||||||
| 23 | 1997 | Link et al. | Link Rejection | R, V, WE | Rejection experiences | ES | 15 | MH patients |
| 24 | 2007 | Björkman et al. | Rejection Experiences-Swedish | P, R | ES | |||
|
| ||||||||
| 25 | 1997 | Raguram, & Weiss | Explanatory Model Interview Catalogue-Stigma Scale | R, WE | PD | 4 | MH | |
| 1997 | Weiss | |||||||
| 1992 | Weiss et al. | |||||||
|
| ||||||||
| 26 | 1997 | Williams et al. | Everyday discrimination scale | R | D | 1 | Community | |
|
| ||||||||
| 27 | 1998 | Singh et al. | Attitudes To Mental Illness Questionnaire | Not reported | S | 2 | Medical students | |
|
| ||||||||
| 28 | 1999 | Magliano et al. | Questionnaire of Family Opinions | DI, P, R, V | Social restrictions | D | 3 | Family members |
| 2004 | Magliano et al. | Questionnaire on the Opinions about MI | Social distance | D | General public | |||
| Utility of treatments | ||||||||
| Biopsychosocial causes | S | |||||||
|
| ||||||||
| 29 | 1999 | Pinel | Stigma Consciousness Scale | DI, P, R, V, WE | AS | 3 | Undergraduates, Gay/Lesbian | |
|
| ||||||||
| 30 | 1999 | Wahl | Consumer experiences of discrimination | V, WE | AS, ES | 16 | MH Consumers | |
| 31 | 2013 | Switaj et al. | Polish version | DI, P, R, V | ||||
|
| ||||||||
| 32 | 2000 | Corrigan et al. | Psychiatric Disability Attribution Questionnaire | DI, R | Stability | S | 2 | Community |
| Controllability | S, D | |||||||
|
| ||||||||
| 33 | 2000 | Crisp | Attitudes to MI ("Changing Minds") | Not reported | S | 11 | Community | |
| 34 | 2011 | Svensson et al. | P, R (No support) | |||||
|
| ||||||||
| 35 | 2000 | Fife & Wright | Social Impact Scale | DI, R, WE | Social rejection | ES | 10 | Consumers (HIV/Cancer) |
| Financial insecurity | Depression, HIV/AIDS, Schizophrenia | |||||||
| Internalized shame | IS, AS | |||||||
| Isolation | IS | |||||||
| 36 | 2007 | Pan et al. | DI, P, R | Unidimensional | AS, ES, IS | |||
|
| ||||||||
| 37 | 2000 | Hirai & Clum | Beliefs Toward MI Scale | DI, P, R, V | Dangerousness | S, P | 1 | Undergraduates |
| Poor interpersonal and social skills | S; AS | |||||||
| Incurability | ||||||||
| 38 | 2013 | Royal & Thompson | DI, P, R, V | Unidimensional | Protestant service goers | |||
|
| ||||||||
| 39 | 2000 | Lauber et al. | Stereotype endorsement scale | Not reported | S | 5 | General population | |
| Social restrictions scale | D | 3 | ||||||
|
| ||||||||
| 40 | 2000 | Ng & Chan | Opinion about Mental Illness in Chinese Community | DI, R | Benevolence | S, D | students | |
| Attitude Scale for MI | Separation | S | ||||||
| Stereotyping | S | |||||||
| Restrictiveness | D | |||||||
| Pessimistic prediction | D, PD | |||||||
| Stigmatization | S, D | |||||||
|
| ||||||||
| 41 | 2001 | Corrigan et al. | Attribution Questionnaire (AQ--27) | DI, R, WE | Personal responsibility | S | 48 | Undergraduate (community college) |
| 2002 | Corrigan et al. | Dangerousness | S | |||||
| 2003 | Corrigan et al | AQ-9 (blame, anger, pity, help, dangerousness, fear, avoidance, segregation, coercion) | Anger | P | ||||
| 2004 | Corrigan et al. | Concern | P | |||||
| 42 | 2012 | Pingani et al. | Italian Version | DI, P, R, V | Fear | P | ||
| 43 | 2012 | Pinto et al. | r-AQ (5 items, unidimensional) | DI, P, R | Helping-avoidance | D | Adolescents | |
| 44 | 2004 | Watson et al. | r-AQ (9 items, for adolescents) | R | Segregation-coercion | D | Adolescents | |
| Fear/dangerousness | S, P | |||||||
| Help/interact | D | |||||||
|
| ||||||||
| 45 | 2008 | Brown | Attribution Questionnaire | DI, P, R, V | Responsibility | S | 2 | Undergraduates |
| Forcing treatment | D | |||||||
| Empathy | P | |||||||
| Negative emotions | P | |||||||
|
| ||||||||
| 46 | 2001 | Harvey | Stigmatization Scale | DI, P, R, V, WE | ES | 2 | Stigmatized group members | |
|
| ||||||||
| 47 | 2001 | Lai et al. | Stigma Questionnaire | DI | Social rejection | AS, ES | 1 | MH Patients |
| 2005 | Chee et al. | Negative Media perceptions | PD | Outpatient MH | ||||
| Shame | IS | |||||||
| Social discrimination | AS | |||||||
|
| ||||||||
| 48 | 2001 | Struening et al. | Devaluation of Consumers Scale | DI, R | Status reduction | PS | 3 | Caregivers |
| Role restriction | PD | |||||||
| Friendship refusal | PD | |||||||
|
| ||||||||
| 49 | 2001 | Read & Harre | Questionnaire on Attitudes towards MH | R | Predicted response items | D | 1 | Undergraduates |
| Semantic differentials | S | |||||||
|
| ||||||||
| 50 | 2012 | Dalky | Stigma-Devaluation Scale, Jordan | DI, P, R, V | Status reduction | PS, PD | ||
| Role restriction | PD | |||||||
| Community rejection | PS, PD | |||||||
|
| ||||||||
| 51 | 2002 | Christison et al. | Medical Condition Regard Scale | DI, P, R, V, WE | S, P, D | 4 | Medical Students | |
|
| ||||||||
| 52 | 2002 | Thompson et al. | Attitudes toward people with mental illness | Not reported | S | 4 | Community, medical, students, members of Schizophrenia advocacy group | |
|
| ||||||||
| 53 | 2003 | Pinfold et al. | Stigma Questionnaire | Not reported | S | 2 | Students | |
|
| ||||||||
| 54 | 2003 | Angermeyer & Matschinger | Emotional Reactions to MI Scale | DI, R | Fear | P | 8 | General public |
| Pity | P | |||||||
| Anger | P | |||||||
| 55 | Personal Attributes Scale | DI, R | Dangerousness | S | 5 | |||
| Dependency | S | |||||||
|
| ||||||||
| 56 | 2003 | Boyd Ritsher et al. | Internalized Stigma of MI Scale | DI, P, R, V, WE | Alienation | IS | 91 | MH outpatients |
| 57 | 2013 | Sibitz et al. | German version | DI, P, R, V | Stereotype endorsement | S, IS | ||
| 58 | 2014 | Boyd et al. | Brief version | DI, P, R, V | Discrimination experiences | ES | ||
| 2014 | Chang et al | DI, P, R, V | Social withdrawal | IS | ||||
| 59 | 2014 | Ociskova et al. | Czech version | DI, P, R, V | Stigma resistance | |||
|
| ||||||||
| 60 | 2003 | Schulze et al. | Questionnaire on Social Distance | R | Stereotypes | S | 8 | Students |
| Social distance | D | |||||||
|
| ||||||||
| 61 | 2004 | Austin et al. | Child Stigma Scale | P, R, V | ES, AS | 2 | Parents | |
| 2009 | Moses | |||||||
|
| ||||||||
| 62 | 2004 | Fortney et al. | Community Stigma | Not reported | Community judgment of drinking | PS, IS | 1 | At-risk drinkers |
| Community judgment about treatment seeking | ||||||||
| Community judgment of specialty treatment services | ||||||||
| Primary care provider judgment | ||||||||
| Specialty provider judgment | ||||||||
| Specialty care lack of privacy | ||||||||
|
| ||||||||
| 63 | 2004 | Angermeyer & Matschinger | Stereotypes of Schizophrenia | DI, R | Dangerousness | S | 6 | General public |
| Attribution of responsibility | S | |||||||
| Creativity | S | |||||||
| Unpredictability/incompetence | S | |||||||
| Poor prognosis | S | |||||||
|
| ||||||||
| 64 | 2004 | Griffiths et al. | Depression Stigma Scale | DI, R, WE | Personal stigma | S, D | 56 | Depressed |
| 2008 | Griffiths et al. | Perceived stigma | PS, PD | Community, General Pop, Depressed subset | ||||
|
| ||||||||
| 65 | 2004 | Sanders Thompson et al. | Experience of Discrimination Scale | V | ES | 1 | Mental illness | |
|
| ||||||||
| 66 | 2004 | Tanaka et al. | Mental Disorder Prejudice Scale | DI, P, R | Rejection | S, D | General public | |
| Peculiarity | S | |||||||
| Human right alienation | D | |||||||
|
| ||||||||
| 67 | 2005 | Baker et al. | Attitudes Toward Acute Mental Health Scale | DI, P, R | Care of control | S | Nursing staff | |
| semantic differentials | S | |||||||
| therapuetic perspectives | S, D | |||||||
| hard to help | S | |||||||
| positive attitudes | S | |||||||
| 68 | 2014 | Gang | Korean version | DI, P, R, V | Professional perspective | 1 | Korean nursing staff | |
| semantic differentials | S | |||||||
| positive attitude | S | |||||||
|
| ||||||||
| 69 | 2005 | Haghighat | Standardized Stigmatization Questionnaire | DI, P, R, V | Social self-interest | PD | 2 | Patients and Relatives |
| Psychological self-interest | PD | |||||||
| Evolutionary self-interest | PS, PD | |||||||
|
| ||||||||
| 70 | 2005 | Watson et al. | Attitudes Toward Serious MI Scale– | DI, P | Threat | S, P, D, AS† | Adolescent | |
| Adolescent Version | Social construction/concern | S | ||||||
| Wishful thinking | S | |||||||
| Categorical thinking | S, D | |||||||
| Out of control | S | |||||||
|
| ||||||||
| 71 | 2005 | Wrigley et al. | Perceived Stigma Scale | Not reported | PS, PD | 5 | Community | |
|
| ||||||||
| 72 | 2005 | Yen et al. | Self-Stigma Assessment Scale, Chinese Version | R | IS | 3 | MH outpatients | |
|
| ||||||||
| 73 | 2005 | Kira et al. | Stigma Consciousness | Not reported | PS, PD, D, AS | 2 | MH clients | |
|
| ||||||||
| 74 | 2006 | Bowers & Allan | Attitudes Toward Personality Disorder Scale | DI, P, R, V | Enjoyment v. loathing | P | 1 | Nurses, prison officers, psychiatric professionals |
| Security v. vulnerability | P | |||||||
| Acceptance v rejection | P | |||||||
| Purpose v. futility | ||||||||
| Exhaustion v. enthusiasm | ||||||||
|
| ||||||||
| 75 | 2006 | Corrigan et al. | Self-Stigma of MI Scale | P, R, V, WE | Stereotype awareness | S | 24 | Psychiatric disabilities |
| 76 | 2007 | Fung et al. | Chinese Version | DI, P, R, V | Stereotype agreement | S | Severe MI | |
| 77 | 2012 | Corrigan et al. | Short Form | P, R, V | Self-concurrence | IS | ||
| Self-esteem decrement | IS | |||||||
|
| ||||||||
| 78 | 2006 | Kroska & Harkness | Stigmatized Sentiments | V | Evaluation (good v bad) | P | 2 | PWMI |
| Potency (powerful v weak) | ||||||||
| Activity (active v weak) | ||||||||
| 79 | 2006 | Kroska & Harkness | Stigmatized Identity Meanings | V | Evaluation (good v bad) | IS | PWMI | |
| Potency (powerful v weak) | ||||||||
| Activity (active v weak) | ||||||||
|
| ||||||||
| 80 | 2006 | Luty et al. | Attitudes Toward Mentally Ill Questionnaire | DI, P, R, V, WE | S, D | 16 | General population | |
|
| ||||||||
| 81 | 2006 | Ucok et al. | Attitudes Toward Schizophrenia | DI | S, D | 2 | General practitioners | |
|
| ||||||||
| 82 | 2006 | Wood & Wahl | IOOV Attitudes and Knowledge | Not reported | Attitudes | D, P | Undergraduates | |
|
| ||||||||
| 83 | 2007 | Day et al. | MI Stigma Scale | DI, R | Anxiety | P | 4 | College Students |
| Relationship disruption | S, D | Community | ||||||
| Hygiene | S | |||||||
| Visibility | S | |||||||
| Treatability | S | |||||||
| Professional efficacy | ||||||||
| Recovery | S | |||||||
|
| ||||||||
| 84 | 2007 | Gilbert et al. | Attitudes Toward Mental Health Problem Scale | R | Attitudes toward MH problems | PS, PD | Female university students | |
| External Shame/Stigma awareness | AS† | |||||||
| Internal shame | IS | |||||||
| Reflected Shame 1 | ||||||||
| Reflected Shame 2 | ||||||||
|
| ||||||||
| 85 | 2007 | King et al. | The Stigma Scale | DI, P, R | Discrimination | ES | 2 | MH service users |
| Disclosure | AS | |||||||
| Positive aspects | S (1 item) | |||||||
|
| ||||||||
| 86 | 2007 | Luoma et al. | Substance Abuse Perceived Stigma Scale | DI, V | Self-devaluation | IS | 3 | Substance abusers in Tx |
| Fear of enacted stigma | AS | |||||||
| Stigma avoidance | AS | |||||||
| Values disengagement | ||||||||
|
| ||||||||
| 87 | 2007 | Marcks et al. | Vignette Questionnaire | DI, R, V | Social rejection | D | 1 | College students |
| 2013 | Cathey & Witterneck | Modified for OCD | Hiding a drug/alcohol problem | S | ||||
| Psychological/Medical problem | S | |||||||
| Concern | P | |||||||
|
| ||||||||
| 88 | 2007 | Happell & Gough | Mental Health Nursing Education Survey | DI, R | Negative Stereotypes | S | 1 | Nursing students |
| Preparedness for MH field | ||||||||
| Valuable contribution | ||||||||
| Anxiety surrounding MI | P | |||||||
| Interest in MH nursing as a career | ||||||||
|
| ||||||||
| 89 | 2008 | Collins et al. | Stigma in Psychiatric Illness and Sexuality Among Women | R | Mental illness stigma | ES | 1 | Serious MI |
| Relationship stigma | S | |||||||
| Ethnic stigma | ||||||||
| Perceived attractiveness | ||||||||
| Discrimination | ES | |||||||
|
| ||||||||
| 90 | 2008 | Eack and Newhill | Attitudes Toward Individuals with Schizophrenia | DI, R | General attitudes | S, D | 1 | Social workers |
| Attitudes about working with individuals with Schizophrenia | D | |||||||
|
| ||||||||
| 91 | 2008 | Kanter et al. | Depression Self-Stigma Scale | DI, P, R, V | General self-stigma | ES, AS | 7 | Depressed undergrads and community |
| Secrecy | AS | |||||||
| Public stigma | S, D | |||||||
| Treatment stigma | ||||||||
| Stigmatizing experiences | ES | |||||||
|
| ||||||||
| 92 | 2009 | Magliano et al. | User Opinions Questionnaire | P, R, V | Affective problems | P | 1 | Schizophrenia patients |
| Social distance | S, D | |||||||
| Usefulness of drug and psychosocial treatments | ||||||||
| Right to be informed | ||||||||
| Recognizability | S, P | |||||||
| Social equality | D | |||||||
|
| ||||||||
| 93 | 2009 | Masuda et al. | Stigmatizing Attitudes-Believability | R | S | 4 | Undergraduates | |
|
| ||||||||
| 94 | 2009 | Quinn & Chaudoir | Anticipated Stigma Scale | R | AS | 1 | College students | |
|
| ||||||||
| 95 | 2010 | Aromaa et al. | Attitudes towards people with mental disorders | DI, P, R | Depression is a matter of will | S | 2 | General population |
| Mental problems have negative consequences | S | |||||||
| One should be careful with antidepressants | ||||||||
| You never recover from mental problems | S | |||||||
|
| ||||||||
| 96 | 2010 | Barney et al. | Self-Stigma of Depression Scale | DI, P, R, V | Shame | IS, AS† | Undergraduate, Internet, Depressed, General pop Depressed | |
| Self-blame | IS, AS† | |||||||
| Social inadequacy | IS, AS† | |||||||
| Help-seeking inhibition | IS, AS | |||||||
|
| ||||||||
| 97 | 2010 | Bell et al. | Stereotypic Beliefs | Not reported | S | 1 | Pharmacy Students | |
|
| ||||||||
| 98 | 2010 | Evans-Lacko et al. | Mental Health Knowledge Schedule | P, R, V, WE | S | 16 | General public | |
|
| ||||||||
| 99 | 2010 | Fresan et al. | Public Conception of Aggressiveness Questionnaire | DI, P, R | Aggressiveness | S | General public | |
| Mental disease | S | |||||||
|
| ||||||||
| 100 | 2010 | Gabriel & Violato | Attitudes towards depression and its treatments | DI, P, R, V | Acceptance of treatment | Depressed | ||
| Perceived stigma and shame | IS, ES | |||||||
| Negative attitudes toward antidepressants | ES | |||||||
| Self-stigma | S, ES | |||||||
| Preference for psychotherapy | ||||||||
|
| ||||||||
| 101 | 2010 | Karidi et al. | Self-Stigmatization Questionnaire | Not reported | ES, AS, IS | 1 | Schizophrenia outpatients | |
|
| ||||||||
| 102 | 2010 | Kassam et al. | MI: Clinicians' Attitudes Scale | DI, P, R, V | S, D, AS† | 5 | Medical students | |
| 103 | 2013 | Gabbidon et al. | MI: Clinicians' Attitudes Scale (healthcare professions version) | DI, R, V | Views of health/social care field and MI | D | Healthcare Professionals | |
| Knowledge of MI | S | |||||||
| Disclosure | AS† | |||||||
| Distinguishing mental and physical health | ||||||||
| Patient care for people with MI | D | |||||||
|
| ||||||||
| 104 | 2010 | Kellison et al. | ADHD Stigma Questionnaire | DI, P, R, V | Disclosure concerns | 3 | Community adolescents | |
| Negative self-image | S; IS | |||||||
| Concern with public attitudes | PS, ES, AS | |||||||
|
| ||||||||
| 105 | 2010 | Kobau et al. | Generic Scale for Public Health Surveillance of MI Associated Stigma (HealthStyles Survey 2006) | DI, P, R, V | Negative stereotypes | S | General public | |
| Recovery and outcomes | S | |||||||
|
| ||||||||
| 106 | 2010 | Luoma et al. | Perceived Stigma of Addiction Scale | DI, P, R, V | PS, PD | Substance abuse tx | ||
|
| ||||||||
| 107 | 2010 | Mak & Cheung | Self-Stigma Scale–Short Form | DI, P, R, V | Affective | IS | 2 | MH consumers |
| Behavioral | IS | Immigrants | ||||||
| Cognitive | IS | Sexual minorities | ||||||
|
| ||||||||
| 108 | 2011 | Brown | Social Distance Scale for Substance Users | P, R, V | D | undergraduates | ||
| 109 | Dangerous Scale for Substance Users | P, R, V (no support) | S | |||||
| 110 | Affect Scale for Substance Users | P, R, V | P | |||||
|
| ||||||||
| 111 | 2011 | Clayfield et al. | Mental Health Attitude Survey for police | DI, P, R | Positive attitudes toward EDPs | S,D | Police | |
| Negative attitudes toward community responsibility for EDPs | D | |||||||
| Not adequately prepared to deal with EDPs | ||||||||
| Positive attitudes toward EDPs living in the community | P,D | |||||||
|
| ||||||||
| 112 | 2011 | Evans-Lacko et al. | Reported and Intended Behaviour Scale | P, R, V, WE | Reported behavior | D | 17 | General population |
| 113 | 2014 | Yamaguchi et al. | Japanese version | DI, P, R, V | Intended behavior | D | ||
|
| ||||||||
| 114 | 2011 | Griffiths et al. | Generalized Anxiety Stigma Scale | DI, P, R, V | Personal stigma | S, D | 3 | General population |
| Perceived stigma | PS, PD | |||||||
|
| ||||||||
| 115 | 2011 | Palamar | Drug Use Stigmatization Scale | DI, P, R, V | Stigma of drug users scale | S | 3 | Adults |
| Drug use stigmatization scale | PS, PD | |||||||
|
| ||||||||
| 116 | 2011 | Scheerder | Attitudes Toward Depression | Not reported | S | 2 | Community and Health Professionals | |
|
| ||||||||
| 117 | 2011 | Wahl et al. | Knowledge and Attitudes about MI | R | Knowledge | S | 1 | Adolescents |
| Attitudes | S, P, D, AS† | |||||||
|
| ||||||||
| 118 | 2012 | Birchwood et al. | Personal Beliefs about Illness Questionnaire-Revised | DI, P, R, V | Entrapment | IS | 6 | MH Patients |
| 1993 | Birchwood et al. | Personal Beliefs about Illness Questionnaire | Loss | IS | MH Patients | |||
| Social marginalization | IS | |||||||
| Shame | IS | |||||||
| Control | IS | |||||||
|
| ||||||||
| 119 | 2012 | Fuermaier et al. | Adult ADHD Stigma Scale | DI, P, R | Reliability and social functioning | S, D | 1 | Undergraduates, community |
| Malingering and misuse of medication | S | |||||||
| Ability to take responsibility | S, D | |||||||
| Norm-violating and externalizing behavior | S | |||||||
| Consequences of diagnostic disclosure | S | |||||||
| Etiology | S | |||||||
|
| ||||||||
| 120 | 2012 | Kassam et al. | Opening Minds Scale for Health Care Providers | DI, P, R, V | Attitudes of healthcare providers | S, P | 4 | Healthcare providers |
| Attitudes toward disclosure | AS | |||||||
| Attitudes of healthcare providers toward PWMI | ||||||||
| Disclosure/help-seeking | ||||||||
| Social distance | D | |||||||
| 121 | 2014 | Modgill et al. | 15-item version | DI, P, R, V | Attitudes | S, P | Healthcare providers | |
| Disclosure/help-seeking | AS | |||||||
| Social distance | D | |||||||
|
| ||||||||
| 122 | 2012 | Madianos et al. | Public Attitudes Toward MI Greece | DI, P, R, V | Stereotyping | S | General population | |
| Optimism | S | |||||||
| Coping | ||||||||
| Understanding | PS, PD | |||||||
|
| ||||||||
| 123 | 2012 | Scocco et al. | Stigma of Suicide Attempt | DI, P, R | Supportive/respectful/caring attitudes | D | Gen Pop, MH patients, attempters, SO who lost someone to suicide | |
| Stigmatizing attitudes and beliefs | S, D | |||||||
|
| ||||||||
| 124 | 2012 | Siu et al. | Attitudes Toward Mental Disorders | Not reported | S, P, D | 2 | Secondary school, community (elderly,public and private housing) | |
|
| ||||||||
| 125 | 2012 | van der Heijden | Nurses’ Perceptions of MH Care | DI, P, R, V | Student s' views on psychiatric patients | S, PS | students | |
| Students' views on a career in mental health care | ||||||||
|
| ||||||||
| 126 | 2013 | Batterham et al. | Stigma of Suicide Scale | DI, P, R, V | Stigma | S | 4 | University student and staff (community) |
| 127 | Short Form | DI, P, R, V | Isolation/depression | S | ||||
| Glorification/normalization | S | |||||||
|
| ||||||||
| 128 | 2013 | Brohan et al. | Discrimination and Stigma Scale | DI, P, R, V, WE | Unfair treatment | ES | 19 | Community MH service users |
| Stopping self | AS | |||||||
| Overcoming stigma | ||||||||
| Positive treatment | ||||||||
|
| ||||||||
| 129 | 2013 | Gabbidon et al. | Questionnaire on Anticipated Discrimination | P, R, V | AS | 1 | Community MH service users | |
|
| ||||||||
| 130 | 2013 | Glass et al. | Perceived Alcohol Stigma Scale | DI, P, V | PS, PD | General population | ||
|
| ||||||||
| 131 | 2013 | Hirsch | Biases Toward Children with Psychological and Behavioral Problems Scale | DI, P, R,V | S | Professionals and students | ||
|
| ||||||||
| 132 | 2013 | Ilic et al. | Multifaceted Stigma Experiences Scale | DI, P, R, V | Hostile discrimination | ES | 1 | MH Tx seekers |
| Benevolent discrimination | ES | |||||||
| Taboo | ES | |||||||
| Denial | ES | |||||||
|
| ||||||||
| 133 | 2013 | Luoma et al. | Substance Abuse Self-Stigma Scale | DI, P, R, V | Self-devaluation | IS | Substance abusers | |
| Fear of enacted stigma | AS | |||||||
| Stigma avoidance | AS, IS | |||||||
| Values disengagement | ||||||||
|
| ||||||||
| 134 | 2013 | Michaels & Corrigan | Knowledge Test | P, R, V | S | 2 | Undergraduates, MH Providers, MH consumers | |
|
| ||||||||
| 135 | 2013 | Mileva et al. | Inventory of Stigmatizing Experiences | P, R | Stigma experiences scale | AS, IS, ES | 7 | MH patients |
| 2005 | Stuart et al. | Stigma impact scale | ES | |||||
|
| ||||||||
| 136 | 2013 | Segal et al. | Attitudes Toward Persons With MI Scale | DI, R | Rejection-- intimate contact | D | 1 | Community mental health clients |
| Rejection-- competence/trustworthiness | S, D | |||||||
| Rejection--severity of illness | S, D | |||||||
|
| ||||||||
| 137 | 2014 | Heflinger et al. | Attitudes about Child Mental Health Questionnaire | DI, P, R, V | Child dangerousness/incompetence | S | Community | |
| General stereotypes | S | |||||||
| Community devaluation/discrimination | PS, PD | |||||||
| Personal attitudes | P, D | |||||||
|
| ||||||||
| 138 | 2014 | Karidi et al | Stigma Inventory for Mental Illness | DI, P, R, V | Perceptions of Social Stigma | AS | Schizophrenia outpatients | |
| Self-efficacy | ||||||||
|
| ||||||||
| 139 | 2014 | Mak et al. | Stigma and Acceptance Scale | DI, R | Public stigma | S, P, D | 1 | Community |
| Stigma acceptance | D | |||||||
|
| ||||||||
| 140 | 2014 | Vogt et al. | Endorsed and Anticipated Stigma Inventory | DI, P, R, V | Negative beliefs about MH treatment | 1 | Veterans | |
| Negative beliefs about MH treatment seeking | S | |||||||
| Negative beliefs about mental illness | S | |||||||
| Concerns about stigma-- family/friends | AS† | |||||||
| Concerns about stigma-- workplace | AS† | |||||||
Notes.
Number of citations in the current review; MI = mental illness; MH = mental health; For psychometric evaluation: DI = dimensionality examined, R = at least one form of reliability reported (e.g., internal consistency, test-retest), P = published psychometric paper, V = at least one form of validity examined (e.g., construct, convergent, divergent, concurrent, discriminant, predictive),WE = well-established measure in the literature with 10+ citations in the past ten years. For stigma mechanisms: D = discrimination, S = stereotypes, P = prejudice, PS = perceived stereotypes, PD = perceived discrimination, AS= anticipated stigma, AS
AS† indicates an anticipated stigma measure that can be administered to the general population, IS = internalized stigma, ES = experienced stigma
The second category consisted of measures described as being specifically created for the study, measures where no citation information was provided, measures that were created by pulling items from multiple measures, and newly developed measures of stigma that had not yet been cited or psychometrically validated in other studies. We refer to this set of measures as “study-created measures” and although they are not included in Table 1, we classified the stigma mechanisms assessed in each measure and summarize the findings. In total, we identified 304 study-created measures (reference list of articles containing study-created measures is available from the first author).
Not included in either category of measures are national or international “indicator” measures of stigma (n = 8). These measures were typically one or two items and were designed to be easily administered in population-level studies to gauge overall levels of stigma in a particular country or context (e.g., General Social Survey, National Survey Study-Children, National Comorbidity Study). A list and description of these measures is available from the first author.
Classifying Measures
We attempted to obtain a copy of each measure included in Table 1. We were not able to obtain original copies of two measures that were not published in English (Sibitz et al., 2013; Zeng et al., 2009). If the article in which the original measure was cited provided the items or enough detail to classify the type of stigma measured, we kept it in Table 1. Our final list included 140 measures of stigma, comprising 330 scales or subscales. For each measure, we recorded the psychometric properties described in the paper and the number of times it was cited in our search. We examined the items included in the measure and classified the stigma mechanism(s) the measure captured at the factor or subscale level. For some measures, there were multiple versions or adaptations available (e.g., validated in a different language or for a different population than the original measure). If an alternative version of a measure had a published psychometric paper available, we counted it as a separate measure when determining the total number of measures we identified and when examining the psychometric characteristics available for the measures. However, in order to avoid over-inflating the totals for the stigma mechanisms contained in the measures, we grouped multiple versions of measures together and only classified the stigma mechanisms once for all versions of the measure (assuming they shared the same items and factor structure). Operational definitions and example items for each stigma mechanism are included in Supplemental File 2.
Psychometric Evaluation of Measures
Information regarding the availability of psychometric properties of each measure is included in Table 1 and a more detailed evaluation of the quality of the evidence for these measurement properties is included in Supplemental File 3. In Table 1, measures were given an “R” if details about at least one form of reliability (e.g., internal consistency, test-retest) were available and a “V” if details about at least one form of validity (e.g., construct, convergent, predictive, concurrent) were available. Measures were given a “D” if the underlying dimensionality (i.e., factor structure) of the measure was reported. We gave a rating of “P” if there was a published paper specifically describing the development of the measure. A measure was considered well-established in the literature and given a rating of “WE” if it had been cited at least 10 times. For measures that were developed before 2004, we checked PsycInfo to see if it had been cited more than 10 times.
In Supplemental File 3, we evaluated measures using the quality criteria developed by Terwee et al. (2007). As part of the COSMIN initiative (Consensus-based Standards for the selection of health Measurement Instruments), Terwee, Mokkink, and colleagues developed a set of standard measurement quality criteria in order to facilitate comparisons of health outcomes questionnaires (Mokkink et al., 2010a, 2010b; Terwee et al., 2007). Terwee et al. provide guidelines for assessing the quality of evidence for content validity, internal consistency, criterion validity, construct validity, reproducibility, responsiveness, floor and ceiling effects, and interpretability. For each measurement property, measures are given a “+”, “−,” “indeterminate,” or “no information available” rating. A full description of each rating is provided in Supplemental File 3. Within the stigma literature, the COSMIN criteria have been used to evaluate measures of internalized stigma (Stevelink, Wu, Voorend, & van Brekel, 2012) and measures of experiences of mental illness stigma (Brohan et al., 2010). In the present study, we followed the same procedures as Brohan et al. (2010) and evaluated measures based on a subset of the COSMIN criteria most relevant to measures of stigma: content validity, internal consistency, construct validity, test-retest reliability, and floor-ceiling effects.
Results
Overview of mental illness stigma measures
Figure 2 presents the number of stigma measures that have been developed in the past decade, broken down by whether the measure has been psychometrically validated for its intended use. The findings are striking. On average, 36 measures of stigma have been developed per year since 2004. On average since 2004, measures without established psychometrics have appeared in the literature about six times as often as new validated measures. Measures have been developed to assess every stigma mechanism, and for a wide range of mental illnesses, including depression (e.g., Griffiths et al., 2004; Griffiths et al., 2008), alcohol and substance use disorders (e.g., Brown, 2011; Glass, Kristjansson, & Bucholz, 2013; Luoma, O’Hair, Kohlenberg, Hayes, & Fletcher, 2010; Luoma et al., 2007; Luoma et al., 2013), schizophrenia (e.g., Ucok et al., 2006), suicide (e.g., Batterham, Calear, & Christensen, 2013), suicide attempts (e.g., Scocco, Castriotta, Toffol, & Preti, 2012), generalized anxiety disorder (e.g., Griffiths, Batterham, Barney, & Parsons, 2011), and attention deficit hyperactivity disorder (e.g., Fuermaier et al., 2012).
Overall Psychometric Summary of Mental Illness Measures
The fifth column of Table 1 contains a description of the psychometric characteristics of each measure. In total, 55.0% (n = 77) of measures had a published psychometric paper available (i.e., a paper describing the development of the measure and its psychometric characteristics) and 17.1% (n = 24) had been cited at least ten times. Information regarding the dimensionality of the measure was described for 58.6% (n = 82), and 48.6% (n = 68) had information about at least one form of validity. The majority of scales (n = 115, 82.1%) had information regarding the reliability of the measure. Fourteen measures did not report any psychometric properties and three measures were found to have no psychometric support.
Of the measures with a psychometric paper available, 61.0% (n = 47) included an examination of at least one form each of reliability, validity, and dimensionality. A total of eight of those measures have been cited at least 10 times in the past decade (although we acknowledge that the 14 measures published since 2012 that have all three psychometric characteristics available may not have been in the literature long enough to be cited 10 times). While there were at least two psychometric characteristics available for most measures in Table 1 (n = 91, 65.0%), 34 measures (24.3%) had only one type of psychometric data available.
Mental Illness Stigma Mechanisms
Before examining the measures associated with each of the stigma mechanisms in the MISF, we began by looking at the number of measures that were associated with the perspective of the stigmatizer versus those associated with the perspective of the stigmatized. Of all the measures we identified, 39 (28%) addressed the perspective of the stigmatized and 100 (72%) were developed from the perspective of the stigmatizer. In the broader literature search, 327 articles (34.2%) were focused on the perspective of the stigmatized (i.e., PWMI).
Stereotypes
Stereotypes were the most widely measured stigma mechanism in our review, with 418 of the 957 articles (43.5%) containing a measure of the extent to which people endorse stereotypical beliefs about mental illness. Among the measures we identified, stereotypes were captured in 128 different scales or subscales. Of those 128 different scales or subscales, 63.3% (n = 81) solely measured stereotypes. The remaining scales or subscales (n = 47) included items assessing at least one other stigma mechanism, with discrimination being the most common mechanism to co-occur within the scale (n = 35).
In terms of their psychometric properties, 28 measures reported information on reliability, validity and dimensionality, and another 29 measures reported only two of those three characteristics. Fifteen measures only reported information on one psychometric characteristic, and eight measures did not provide any psychometric information. In total, 45 measures had a psychometric paper available, and 9 measures were classified as well-established.
The most widely used measure containing stereotypes was the ISMI scale (Boyd Ritsher et al., 2003; n = 89), followed by the Depression Stigma Scale (DSS; Griffiths et al., 2004; 2008; n = 56), the Attribution Questionnaire (AQ; Corrigan, Green, Lundin, Kubiak, & Penn, 2001; n = 48), and the Community Attitudes Toward the Mentally Ill Scale (CAMI; Taylor & Dear, 1981; n = 43). Both the ISMI and CAMI are well-validated measures, with psychometric information available regarding their reliability, validity and dimensionality (although only the ISMI has a published psychometric paper). Reliability and dimensionality have been examined with the AQ and DSS.
The most common stereotypes addressed in the stereotype measures were that PWMI are weak, dangerous, unpredictable, violent, and that they are responsible for their condition. Some measures focus on the stereotypes associated with specific disorders. For example, the “personal stigma” subscale of the DSS asks people the extent to which they think that people with depression can snap out of it. Although the ADHD stigma scale (Kellison, Bussing, Bell & Garvan, 2010) focuses on ADHD, the items were adapted from an HIV stigma scale and could be adapted for other mental illnesses. The “personal stigma” subscale of the Generalised Anxiety Stigma Scale (Griffiths et al., 2011) also addresses stereotypes that could be applied to other mental disorders. Thus, although numerous measures have focused on a specific disorder, for the most part, the stereotypes included could apply to any disorder.
Prejudice
Prejudice was the least measured stigma mechanism, measured in 141 articles (14.7%), and captured in 42 scales or subscales. Twenty measures or subscales also included items assessing other stigma mechanisms, with stereotypes being the most common co-occurring mechanism. The most cited measures of prejudice were the AQ and the CAMI. A total of ten measures had information related to all three psychometric characteristics, 13 measures presented two psychometric characteristics, and nine measures reported just one. Two measures did not provide any psychometric information. Three measures were well-established, and 16 had a psychometric paper.
Fear and anger appear to be the most common forms of prejudice captured in the measures. The AQ contains a fear subscale, and the CAMI includes items that address fear (e.g., It is frightening to think of people with mental problems living in residential neighborhoods) and lack of sympathy (e.g., The mentally ill do not deserve our sympathy).
Discrimination
Discrimination was the second most widely measured stigma mechanism in our review, with 43.1% (n = 412) of articles containing a measure of discrimination. Among the measures we identified, discrimination was captured in 69 different scales or subscales, and was the sole stigma mechanism measured in 29 (42.0%) of the scales or subscales. Stereotypes were the most common co-occurring stigma mechanism.
In terms of psychometric characteristics of the measures, eight measures were rated as well-established and 15 measures had information available regarding reliability, validity and dimensionality. A total of 19 measures reported two psychometric characteristics, 13 measures reported only one, and four measures did not provide any psychometric information.
The most cited measure of discrimination was also the most cited overall—social distance. Social distance was measured in 213 of 957 articles (22.3%). The original social distance scale (SDS) was a type of Guttman scale developed by Bogardus (1933) and contains seven equidistant items related to people’s willingness to engage in social contact with people from other social groups. Participants are asked to read each statement and indicate whether they would be willing to engage in that type of social relationship (yes/no). However, many researchers use modified versions of the SDS or created their own. For example, Link et al. (1987) modified the Bogardus SDS so that the seven items were no longer necessarily equidistant, and participants respond to each of seven items using a 0 to 3 Likert scale. Others tie the social distance scale to a vignette describing someone with mental illness (e.g., Boyd, Katz. Link & Phelan, 2010; Yap, Reavley, & Jorm, 2013). Given the variability in how social distance is measured, it is challenging to assess the psychometric characteristics of the measure. However, reliability information is available for both the Bogardus and Link versions of the scales.
Other concepts that were captured in the discrimination measures include avoidance, social restrictiveness, and willingness to help. For example, the AQ contains subscales that assess willingness to help someone with mental illness as well as the extent to which people agree that PWMI should be segregated from the general population (i.e., put in mental hospitals).
Experienced Stigma
Experienced stigma was captured in 17.2% (n =165) of the articles and we identified 27 scales or subscales measuring experienced stigma. The majority of measures exclusively focused on experienced stigma (63.0%). However, ten subscales also captured other mechanisms, with anticipated or internalized stigma co-occurring most often. In terms of psychometrics, nine measures reported all three psychometric characteristics, four measures reported two forms, six reported only one form, and one did not present any. Six measures were well-established, and 12 measures had psychometric papers available.
The most cited measure of experienced stigma was the ISMI, which includes an experienced stigma subscale that assesses day-to-day discrimination experienced by PWMI. The next most cited measures of experienced stigma were the CESQ, Link et al.’s (1997) Rejection Experiences Scale, and Fife & Wright’s (2000) Social Impact Scale (SIS), all of which include items assessing both day-to-day discrimination (e.g., being avoided), as well as more acute forms of discrimination (e.g., being denied a job).
Anticipated Stigma
In total, 10.0% (n = 96) of articles cite measures that assesses anticipated stigma, and we identified 37 anticipated stigma scales or subscales. Fifteen measures provided information regarding reliability, validity, and dimensionality, and twelve of those also included a published psychometric paper. Six measures presented two forms of psychometrics, eight presented only one form, and two did not present any psychometric information.
Interestingly, 19 of the 37 scales or subscales (51.4%) that assessed anticipated stigma also include items that address at least one other stigma mechanism, with internalized stigma and experienced stigma co-occurring most often. Additionally, the most cited measures of anticipated stigma are primarily measures of experienced stigma that include items that also assess anticipated stigma: the SIS (n = 10) and CESQ (n = 16). One recently developed measure, the Questionnaire on Anticipated Discrimination (QUAD; Gabbidon et al., 2013), is entirely focused on anticipated stigma and appears to be a psychometrically valid and promising measure.
In our framework, anticipated stigma is one of the mechanisms specific to PWMI. Therefore, one needs to have a mental illness in order to anticipate stigma related to mental illness. However, 27.0% (n = 10) scales or subscales identified as assessing anticipated stigma were designed to be completed by people who may or may not have mental illness. In some of these measures, individuals are asked to report how they think they would feel (e.g., If I had a mental illness, I would feel bad about myself) if they were to have a mental illness. For PWMI, these items may be capturing aspects of anticipated or internalized stigma (or both). For people who do not have mental illness, it is unclear what mechanism is being tapped.
Some of these measures assess how they think others would react to them if they had a mental illness (e.g., “If I had a mental illness, friends and family would think I am weak”). For PWMI, these measures are likely tapping anticipated stigma because they are asking to what extent people expect to be the target of stereotyping and discrimination. For people who do not have mental illness, these measures are likely tapping perceived stigma—how do people think others will react to PWMI.
Internalized Stigma
Of articles in the broader search, 150 (15.7%) include a measure of internalized stigma. A total of 29 scales or subscales assess internalized stigma. More than one-third (34.5%) of internalized stigma measures also included items that address other stigma mechanisms (n = 10), with anticipated stigma co-occurring the most often.
In terms of the psychometric characteristics, eight measures provided information on reliability, validity, and dimensionality, and all of them were accompanied by a published psychometric evaluation. However, only three measures were categorized as well-established, and only one of those three had a published psychometric paper (ISMI). Four measures provided two psychometric characteristics, five provided only one, and two measures did not have any psychometric information provided.
The most cited measure of internalized stigma was the ISMI (90 citations in the broader search). The ISMI is a well-cited, validated measure with five subscales: alienation, stereotype endorsement, discrimination experiences, social withdrawal, and stigma resistance. Scores on the five scales can be summed for a total ISMI score, or the scales can be treated individually. However, by generating a total ISMI score, the effect of internalized stigma is conflated with other stigma constructs. Importantly, only two of the subscales—alienation and social withdrawal, assess internalized stigma as conceptualized in the current article. For example, while the stereotype endorsement scale addresses internalized stigma, it also includes items that reflect endorsement of personal stereotypes. The discrimination experiences subscale measures experienced stigma. The stigma resistance scale was intended to reflect how much an individual feels they resist internalizing the stigma of mental illness (e.g., I can have a good, fulfilling life, despite my mental illness). However, psychometric support for the reliability of the scale is quite low, with some researchers finding internal consistency reliability estimates as low as 0.15 (Werner, Stein-Shvachman, & Heinik, 2009). Others have found support for stigma resistance as a separate construct (Sibitz, Unger, Woppmann, Zidek, & Amering 2011). Nevertheless, more than half (n = 50, 55.6%) of the articles citing the ISMI include stigma resistance in their analyses.
Recently, the authors of the ISMI reviewed international applications of the ISMI since its development (Boyd et al., 2014). There are more than 50 versions of the ISMI in existence. It has been translated to multiple languages, and modified for use with specific mental (e.g., depression, schizophrenia, eating disorders) and physical health conditions (e.g., epilepsy, inflammatory bowel disorder). Reliability and validity for the overall scale and subscales are consistently high (with the exception of the stigma resistance subscale). Chang and colleagues (2014) recently conducted additional psychometric analyses on the ISMI, demonstrating that ISMI shows good internal consistency, test-retest, and concurrent validity, as well as measurement invariance across time (again with the exception of the stigma resistance subscale).
Perceived Stigma
Perceived stereotypes and discrimination were measured in 200 and 203 articles (20.9 and 21.2%, respectively) in the broader search, respectively. Of the scales and subscales we identified, 19 measured perceived stereotypes, and 22 measured perceived discrimination. None of the measures were classified as assessing perceived prejudice. Only two of the perceived stigma measures were classified as well-established, and neither of those had a published psychometric paper available. Nine measures presented information regarding reliability, validity, and dimensionality; seven measures presented two psychometric characteristics, five presented one, and three did not present any psychometric information.
Link’s (1987) Perceived-Devaluation Discrimination (PDD) measure was the most cited measure of both perceived stereotypes and discrimination, and was the second most used stigma measure overall (n = 123, 12.9%). The PDD is a well-established measure, having been cited over 100 times in the past decade with good internal consistency. However, the original PDD has never undergone a full psychometric evaluation.
As a perceived stigma measure, the PDD asks what people think other people feel and act towards PWMI. Because the measure is designed to be completed by people both with and without mental illness, the items are written more generally, and ask the extent to which people agree or disagree about what “most people” believe about PWMI. An important benefit of asking people about others’ beliefs is the avoidance of socially desirable responding, as participants may feel more comfortable reporting that others view PWMI negatively, rather than endorsing those views themselves. Nevertheless, it is important to keep in mind that although personal beliefs may be correlated with perceived beliefs, they are distinct constructs that differentially impact outcomes for PWMI.
Although we classified the PDD as a measure of perceived stigma, there was variability in how the PDD was used. Some authors refer to the PDD as a measure of self- or internalized stigma (e.g., Jung and Kim, 2012; Kondrat, 2012; Livingston & Boyd, 2010; Vauth, Kliem, Wirtz, & Corrigan, 2007).
The DSS was also a common measure of both of perceived stereotypes and discrimination and includes two subscales: personal stigma and perceived stigma. The DSS has been adapted for other mental health conditions, including addiction, alcohol use, and generalized anxiety. The perceived stigma subscale also asks participants the extent to which they believe most people hold negative beliefs about people with depression and whether they feel most people discriminate against people with depression.
Study-Created Measures
Study-created measures were used in 239 of the 957 articles (25.0%) for a total of 304 measures. Measures assessing stereotypes were the most common (n =156, 51.3%), followed by personal discrimination (n = 83, 27.3%), personal prejudice (n = 50, 16.5%), anticipated stigma (n = 29, n =9.5%), perceived discrimination (n = 26, 8.6%), experienced stigma (n = 21, 6.9%), perceived stereotypes (n = 15, 4.9%), internalized stigma (n =14, 4.6%), and finally, perceived prejudice (n = 6, 2.0%).
General Discussion
In the present article, we present a comprehensive framework for organizing research on the mechanisms through which individuals experience mental illness stigma, and apply it to evaluate the current state of measurement with respect to those mechanisms. This framework – the Mental Illness Stigma Framework – is not meant to replace existing conceptual models of stigma mechanisms. Instead, it was designed to capture the most common ways that individuals experience stigma, address key aspects of mental illness stigma that are relevant to a broad range of mental illnesses, and differentiate between mechanisms that are most relevant for people who do not have mental illness—stereotypes, prejudice, and discrimination—versus those that are most important for those who do have mental illness—experienced, anticipated, and internalized stigma. Most importantly, it ties together a substantial body of mental illness stigma research through common language and terminology, which can guide communication about relevant research findings, inform future research efforts, and aid researchers in selecting measures that correspond to the mental illness stigma mechanisms in which they are interested.
Current State of Mental Illness Stigma Measurement
The application of the MISF to systematically review mental illness stigma measures revealed that a striking number of measures—more than 400—have been used since 2004. Notably, more than two thirds of these measures were created for a particular study and had not undergone systematic psychometric validation. And yet, this review revealed that there is at least one well-validated measure of mental illness stigma for each of the mechanisms in the MISF. This begs the question of why researchers continue to create their own measures rather than use existing measures. There are several potential explanations. First, the complexity and multidimensionality of mental illness stigma likely plays a role. The interdisciplinary nature of mental illness stigma research is also likely an important factor, with researchers in different disciplines varying in their use of terminology and measurement. However, probably one of the biggest reasons for the large number of stigma measures is the lack of a unified conceptual framework that provides common terminology and definitions for mental illness stigma researchers. The MISF was designed to address this limitation by integrating the core mental illness stigma mechanisms that have been examined in this literature.
Through the application of the MISF, we were able to determine which stigma mechanisms have received the most, and the least, attention in the literature. By far, the most widely studied stigma mechanisms were stereotypes and discrimination, which were measured in 43.5% and 43.1% of the articles we identified, respectively. The research emphasis on stereotypes and discrimination parallels international efforts to reduce stigmatizing attitudes in the general public. The widespread prevalence of stereotypes and discrimination contributes to a cultural context in which individuals with mental illness may come to anticipate and experience stigma (Link & Phelan, 2001). Ideally, efforts to reduce and eliminate stereotypes and prejudice can create a cultural shift that would ultimately improve the lives of PWMI.
Less research exists on anticipated stigma (10% of the 957 articles). Compared to other mechanisms in the MISF, there appears to be less consistency in how researchers define and assess anticipated stigma. Several anticipated stigma measures we identified required participants to take the perspective of someone who has mental illness when (i.e., “If I had a mental illness…”). However, it is difficult to determine which stigma construct is being assessed when items are written this way. They may be picking up on anticipated, internalized, or perceived stigma, or a combination of all of these mechanisms. Because anticipated stigma is inherently tied to having a mental illness, it is often appropriate to limit the assessment of anticipated stigma to PWMI. However, there may be some research questions that benefit from asking individuals who do not have a confirmed mental illness these types of questions. For example, there may be assessment contexts in which individuals are reluctant to acknowledge mental health problems and therefore limiting the sample to those with a priori mental illness may not be feasible. There may also be assessment contexts in which it is not possible to limit the sample to PWMI before data collection. In such instances, care should be taken in carefully defining the stigma mechanisms under study.
Another issue we identified in our review is that many stigma measures assess multiple constructs within a single scale or subscale. This was particularly true for anticipated stigma and discrimination, where it occurred in more than half of their respective scales. Anticipated stigma was often included as a subscale (or part of a subscale) of measures addressing internalized or experienced stigma. In fact, we identified only four measures in which anticipated stigma was the sole stigma mechanism assessed (QUAD, Pinel’s (1999) Stigma Consciousness Scale, Link et al.’s (1991) secrecy scale, and Quinn & Chaudoir's (2009) anticipated stigma measure). Similarly, discrimination was the sole mechanism measured in in about half of the discrimination scales, with stereotypes most commonly co-occurring.
Including items that assess multiple constructs within a scale or subscale is not inherently problematic if one is interested in capturing a broader conceptualization of stigma. However, it is important not to conflate stigma mechanisms by including items that measure multiple stigma mechanisms within the same scale or subscale because they may be related to important outcomes in different ways. For example, the ISMI scale includes five subscales. Although researchers can generate a total ISMI score by summing across all items, some of the ISMI scales do not measure internalized stigma (e.g., the stereotype endorsement subscale addresses stereotypes, and the discrimination experiences subscale measures experienced stigma). By generating a total ISMI score, it appears that the effect of internalized stigma is conflated with other stigma constructs. We recommend that researchers who use the ISMI, or any other measure assessing multiple stigma mechanisms, consider the value of using the subscales independently.
The sheer volume of mental illness stigma measures we identified, and in particular, the use of unvalidated measures, suggests that we may be close to a saturation point when it comes to the development of mental illness stigma measures. Instead of continuing to use unvalidated measures in new studies, we suggest that researchers carefully consider the stigma mechanism they are interested in examining, and whenever possible, identify a preexisting measure that meets their needs. Additionally, research should focus on validating some of the more promising measures of mental illness stigma with population(s) for which the measure was intended—i.e., those measures that are well-cited but have not yet undergone a psychometric evaluation. In cases where researchers would like to focus their attention on a specific disorder, there are a number of options. They can use existing measures that were designed for broad application to mental illness. The benefit of such an approach is that it facilitates future comparisons across disorders using the same measure. Another option is to use one of the many well-validated measures developed or adapted for a specific disorder. Finally, if needed, researchers can adapt an existing well-validated measure to fit their needs, being sure to provide information regarding reliability, validity, and dimensionality of their adapted measure.
Directions for Future Research
Our application of the MISF to review stigma measures provides valuable information regarding gaps in the mental illness stigma literature. In general, stigma mechanisms that are most relevant to the experiences of PWMI—experienced, anticipated, and internalized stigma—have been the least studied, and were measured in less than 20% of the studies in our review. There is a still a great deal of work to be done to explore these mechanisms and their corresponding outcomes for PWMI. For example, research is needed to understand relationships between stigma mechanisms, as research on other stigmatized identities (e.g., chronic physical illnesses) suggests that experienced and internalized stigma may lead to anticipated stigma, which in turn negatively impact healthcare access and overall quality of life (Earnshaw & Quinn, 2012). Understanding how PWMI experience stigma through mechanisms such as anticipated, internalized, or experienced stigma can also pave the way for the development of strategies to resist or reduce stigma. How people who possess a socially devalued identity experience these identities can vary greatly (Crocker & Major, 1989). PWMI may respond to stigmatization with righteous anger (Corrigan & Watson, 2002), feelings of empowerment (Rusch, Lieb, Bohus, & Corrigan, 2006), or by resisting stigma (Sibitz et al., 2011). These responses may impact the wellbeing of PWMI. Although research in this area is somewhat limited, the existing evidence suggests that empowerment is associated with decreased internalized stigma (Brohan et al., 2010; Sibitz et al., 2011).
Importantly, this review underscores the need for additional longitudinal research to better understand how mental illness stigma impacts individuals. The majority of studies we reviewed were cross-sectional, which necessarily limits their generalizability. The call for more longitudinal stigma research is not new. Ten years ago in his review of mental illness stigma measures, Link et al. (2004) also encouraged researchers to take prospective view of mental illness stigma. Yet, we have not seen a marked increase in longitudinal work in this area. Of course, longitudinal research presents its own sets of challenges, namely cost and time. But if we want to advance our understanding of mental illness stigma, longitudinal studies are essential.
We hope the MISF can be a starting point for other researchers by delineating the most common ways in which people experience stigma and providing common terminology that can guide measurement selection. We also hope that researchers will be able to build upon the MISF to advance our understanding of mental illness stigma. How stigma mechanisms influence one another and how individuals respond to stigmatization (i.e., stigma resistance or coping) are two important ways in which the MISF could be elaborated upon.
Understanding the multidimensionality of stigma is key to advancing both theory and research (Pescosolido & Martin, 2015). An essential future direction for the MISF will be to examine the dimensionality of the stigma mechanisms themselves. For example, Quinn, Williams, & Weisz (2015) recently argued for a distinction between acute experiences of discrimination such as getting fired for having a mental illness, versus “day-to-day” discrimination such as being disrespected or avoided due to one’s mental illness. Both of these types of behaviors are captured in the discrimination mechanism of the MISF; however, different forms of discrimination may differentially impact PWMI. The same may be true with respect to other mechanisms in the MISF.
It is also important to acknowledge that our framework is just one way of conceptualizing mental illness stigma and there may be other informative conceptualizations. The MISF may be used in tandem with other conceptualizations of stigma to move the field forward. For example, Pescosolido and Martin (2015) propose a systems-level conceptualization of stigma, the stigma complex. Their conceptualization of stigma is based on the Framework Integrating Normative Influences on Stigma (FINIS; Pescosolido, Martin, Lang, & Olafsdottir, 2008). The FINIS is a broad theoretical model positing that stigma is the result of the dynamic interplay of both individual and community level factors. However, unlike the MISF, the FINIS does not identify the specific stigma mechanisms that capture the different ways in which people experience mental illness stigma. Future stigma researchers might examine ways in which these two theoretical frameworks work together to better understand how the different components of stigma (at both the individual and community level) interact.
Most of the theoretical and empirical work on mental illness stigma has focused on the individual level, which is also the emphasis of the MISF. However, future research can build upon and expand the MISF to include other important manifestations of stigma, including courtesy stigma, structural stigma, and cultural stigma. Courtesy stigma is the stigma experienced by people associated with those who possess a devalued identity, and is sometimes referred to as stigma-by-association (Goffman, 1963), family stigma (Corrigan &Miller 2004; Larson & Corrigan, 2008) or affiliate stigma (Mak & Cheung, 2008). Family members, friends, caregivers, and service providers may all be the target of stigma (i.e., stereotyping, prejudice, or discrimination), or they may experience, anticipate, or internalize stigma (Mak & Cheung, 2008) because of their relationship to the stigmatized person. Structural stigma occurs when laws, policies, procedures, and cultural norms intentionally or unintentionally restrict the opportunities of those individuals who possess a stigmatized identity (Corrigan, et al., 2005; Link & Phelan, 2001; Hatzenbuehler & Link, 2014; Pugh, Hatzenbuehler, & Link, 2015). Structural stigma focuses on macro-level social forces that negatively impact the lives and well-being of PWMI (or any other stigmatized identity). Although research on structural stigma as it relates to mental illness is limited, two comprehensive reviews describe the state of current research on structural stigma and provide suggestions for future research (Livingston, 2013; Pugh et al., 2015). An important limitation of existing research on structural stigma is that it tends to be descriptive in nature, and consequently, there is a need for research examining the causal relationship between structural stigma and outcomes for PWMI (Pugh et al., 2015).
The integration of intersectionality theory may also help to further focus and unite the mental illness stigma literature. Intersectionality theory suggests that experiences and outcomes of mental illness stigma may be shaped by other characteristics of the stigmatized or stigmatizer, including the type of mental illness, treatment engagement, socio-economic status, gender, race, and others. For example, at the intersection of gender and mental illness, some Latina women living with mental illness define themselves as “good girls” and “church ladies” in opposition to stigmatizing labels (e.g., “loca”) (Collins, von Unger, & Armbrister, 2008). Identifying with cultural identities that are well-respected is a way of resisting the stigma associated with mental illness (Collins et al., 2008). Additionally, some work at the intersection of race/ethnicity, culture, and mental illness suggests that there is variability in the extent to which different racial and ethnic groups endorse stigmatizing beliefs about mental illness, and these differences may be attributed to different socialization and cultural values related to mental illness (Abdullah & Brown, 2011; Rao, Fienglass, & Corrigan, 2007; Whaley, 1997). Understanding how race and ethnicity impact people’s conceptualizations and experiences of mental illness stigma has important implications for individuals’ overall health and well-being, especially because racial and ethnic minorities are more likely to have unmet mental healthcare needs (Wang et al., 2007).
Finally, it is important to recognize culture as a lens through which we can better understand how stigma impacts individuals (Yang et al., 2007). The extent to which culture has been incorporated into measurements of stigma was recently examined in a measure review by Yang and colleagues (2014). The majority of cultural measures they identified involved adapting an existing measure to a specific culture, with very few measures being developed specifically for a particular culture. Yang et al. (2014) call for the development of culture-specific stigma measures, as they may have stronger predictive value over generic measures. Importantly, such measures should consider the cultural values that matter the most and therefore threaten people’s ability to successfully function in their social worlds (Yang et al., 2007).
Mental Illness Treatment Stigma
One area of mental illness stigma measurement that we excluded from our review was treatment stigma. There is a substantial body of literature examining the stigma associated with seeking treatment or help for mental health problems, and a number of treatment stigma scales have also been developed (e.g., Elhai, Schweinle, & Anderson, 2008; Skopp et al., 2012; Vogel, Wade, & Haake, 2006; Vogt et al., 2014). Some researchers treat mental illness stigma and treatment stigma as synonymously, including treatment and help-seeking items among other items assessing mental illness stigma. Others view treatment-seeking as a behavioral cue that identifies someone as mentally ill. Because mental illness can be concealed, seeking treatment may signal to others that the individual has a mental illness, and these individuals may become the target of stereotyping, prejudice, and discrimination.
A study conducted by Tucker and colleagues (2013) demonstrated that the internalized stigma of seeking treatment and the internalized stigma of mental illness are distinct constructs (they refer to these constructs as self-stigma of treatment and mental illness, respectively). Further, they each uniquely predicted outcomes such as shame, self-blame, social inadequacy, and help-seeking. Understanding the differences between the two constructs may have important implications for designing stigma interventions. For example, interventions targeting mental illness stigma mechanisms might focus on changing stereotypes of PWMI, or reducing internalized stigma (Lucksted et al., 2011). Interventions targeting treatment stigma might focus on negative beliefs about the efficacy of therapies and medications (Schomerus & Angermeyer, 2008), or challenging the belief that seeking treatment makes one weak.
Given the evidence supporting the distinction between treatment stigma and mental illness stigma, researchers should avoid conflating the two constructs in their conceptualization and measurement of mental illness stigma. Additional research is needed to fully understand the similarities and differences between these constructs, and how they work together to impact individuals with mental illness. For example, it is possible that treatment stigma may serve as a mediator between mental illness stigma and treatment-related outcomes. As previously mentioned, seeking treatment may also serve as a moderator of mental illness stigma mechanisms, affecting how PWMI experience mental illness stigma.
Conclusions
In their 2004 review of stigma measures, Link et al. proposed six questions that researchers should consider when selecting measures of stigma: (1) What is the research question, and what are the variables one must measure to answer the question posed? (2) Is there an existing measure available, (3) Is it suitable for the population under examination (or can it be modified to make it appropriate)? (4) Is the measure appropriate to the study methodology in use? (5) Is the measure reliable and valid, and could social desirability influence responses to the measure? (6) Is the administration of the measure feasible for participants? Despite the inherent wisdom of this guidance, there has been a proliferation in use of both validated and unvalidated mental illness stigma measures over the past 10 years, with little signs of slowing down. The field of mental illness stigma research has reached a point where there needs to be convergence across researchers with respect to both terminology and measurement to move forward. We believe the MISF can help researchers articulate their constructs of interest with shared terminology, and that our review of mental illness stigma measures can help researchers identify validated scales that can be used to study those constructs.
One of the most important implications of the MISF and our review of the field’s measurement of mental illness stigma is its potential to inform stigma reduction interventions. As Bos et al. (2013) note, many stigma interventions lack a theoretical foundation and sound methodology. They recommend that stigma reduction interventions identify and target specific stigma mechanisms and use measures that correspond to those mechanisms. The MISF and our review of measures can help researchers do exactly that. We hope that the next decade of mental illness stigma research is characterized by a greater synthesis of existing and newly discovered knowledge, and that researchers leverage that knowledge to reduce stigma and ultimately, improve the lives of those who experience mental illness.
Supplementary Material
Acknowledgments
Dr. Earnshaw’s efforts were supported by NIH grant K12 HS022986.
Footnotes
VA Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
*indicates reference for a stigma measure described in Table 1.
- Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clinical Psychology Review. 2011;31:934–948. doi: 10.1016/j.cpr.2011.05.003. [DOI] [PubMed] [Google Scholar]
- Allport GW. Basic and Applied Social Psychology. Vol. 35. Cambridge, MA: Perseus Books. and research; 1954/1979. The nature of prejudice; pp. 1–9. [DOI] [Google Scholar]
- Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: A review of population studies. Acta Psychiatrica Scandinavica. 2006;113:163–179. doi: 10.1111/j.1600-0447.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- *.Angermeyer MC, Matschinger H. Social distance towards the mentally ill: Results of representative surveys in the Federal Republic of Germany. Psychological Medicine. 1997;27:131–141. doi: 10.1017/S0033291796004205. [DOI] [PubMed] [Google Scholar]
- *.Angermeyer MC, Matschinger H. The stigma of mental illness: Effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatrica Scandinavica. 2003;108:304–308. doi: 10.1034/j.1600-0447.2003.00150.x. [DOI] [PubMed] [Google Scholar]
- *.Angermeyer MC, Matschinger H. The stereotype of Schizophrenia and its impact on discrimination against people with Schizophrenia: Results from a representative survey in Germany. Schizophrenia Bulletin. 2004;30:1049–1061. doi: 10.1093/oxfordjournals.schbul.a007120. [DOI] [PubMed] [Google Scholar]
- *.Aromaa E, Tolvanen A, Tuulari J, Wahlbeck K. Attitudes towards people with mental disorders: The psychometric characteristics of a Finnish questionnaire. Social Psychiatry and Psychiatric Epidemiology. 2010;45:265–273. doi: 10.1007/s00127-009-0064-y. [DOI] [PubMed] [Google Scholar]
- *.Austin JK, MacLeod J, Dunn DW, Shen J, Perkins SM. Measuring stigma in children with epilepsy and their parents: Instrument development and testing. Epilepsy & Behavior. 2004;5:472–482. doi: 10.1016/j.yebeh.2004.04.008. [DOI] [PubMed] [Google Scholar]
- *.Baker JA, Richards DA, Campbell M. Nursing attitudes towards acute mental health care: Development of a measurement tool. Journal of Advanced Nursing. 2005;49:522–529. doi: 10.1111/j.1365-2648.2004.03325.x. [DOI] [PubMed] [Google Scholar]
- *.Barney LJ, Griffiths KM, Christensen H, Jorm AF. The Self-Stigma of Depression Scale (SSDS): Development and psychometric evaluation of a new instrument. International Journal of Methods in Psychiatric Research. 2010;19:243–254. doi: 10.1002/mpr.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, McGinty EE. Stigma and public support for parity and government spending on mental health: A 2013 national opinion survey. Psychiatric Services. 2014;65:1265–1268. doi: 10.1176/appi.ps.201300550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Batson CD, Polycarpou MP, Harmon-Jones E, Imhoff HJ, Mitchener EC, Bednar LL, Highberger L. Empathy and attitudes: Can feeling for a member of a stigmatized group improve feelings toward the group? Journal of Personality and Social Psychology. 1997;72:105–118. doi: 10.1037//0022-3514.72.1.105. [DOI] [PubMed] [Google Scholar]
- *.Batterham PJ, Calear AL, Christensen H. The Stigma of Suicide Scale: Psychometric properties and correlates of the stigma of suicide. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2013;34:13–21. doi: 10.1027/0227-5910/a000156. [DOI] [PubMed] [Google Scholar]
- Bell JS, Aaltonen SE, Airaksinen MS, Volmer D, Gharat MS, Muceniece R, Chen TF. Determinants of mental health stigma among pharmacy students in Australia, Belgium, Estonia, Finland, India and Latvia. International Journal of Social Psychiatry. 2010;56:3–14. doi: 10.1177/0020764008097621. [DOI] [PubMed] [Google Scholar]
- *.Birchwood M, Jackson C, Brunet K, Holden J, Barton K. Personal Beliefs about Illness Questionnaire-revised (PBIQ-R): Reliability and validation in a first episode sample. British Journal of Clinical Psychology. 2012;51:448–458. doi: 10.1111/j.2044-8260.2012.02040.x. [DOI] [PubMed] [Google Scholar]
- *.Birchwood M, Mason R, MacMillan F, Healy J. Depression, demoralisation and control over psychotic illness: A comparison of depressed and non-depressed patients with a chronic psychosis. Psychological Medicine. 1993;23:387–395. doi: 10.1017/s0033291700028488. [DOI] [PubMed] [Google Scholar]
- *.Björkman T, Svensson B, Lundberg B. Experiences of stigma among people with severe mental illness. Reliability, acceptability and construct validity of the Swedish versions of two stigma scales measuring devaluation/discrimination and rejection experiences. Nordic Journal of Psychiatry. 2007;61:332–338. doi: 10.1080/08039480701642961. [DOI] [PubMed] [Google Scholar]
- *.Bogardus ES. A social distance scale. Sociology & Social Research. 1933;17:265–271. [Google Scholar]
- Bos AE, Pryor JB, Reeder GD, Stutterheim SE. Stigma: Advances in theory and research. Basic and Applied Social Psychology. 2013;35:1–9. doi: 10.1080/01973533.2012.746147. [DOI] [Google Scholar]
- *.Botega N, Mann A, Blizard R, Wilkinson O. General practitioners and depression-First use of the Depression Attitude Questionnaire. International Journal of Methods in Psychiatric Research. 1992;2:169–180. [Google Scholar]
- *.Bowers L, Allan T. The Attitude to Personality Disorder Questionnaire: Psychometric properties. Journal of Personality Disorders. 2006;20:281–293. doi: 10.1521/pedi.2006.20.3.281. [DOI] [PubMed] [Google Scholar]
- *.Boyd Ritsher J, Otilingam PG, Grajales M. Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Boyd JE, Adler EP, Otilingam PG, Peters T. Internalized Stigma of Mental Illness (ISMI) scale: A multinational review. Comprehensive Psychiatry. 2014;55:221–231. doi: 10.1016/j.comppsych.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Boyd JE, Katz EP, Link BG, Phelan JC. The relationship of multiple aspects of stigma and personal contact with someone hospitalized for mental illness, in a nationally representative sample. Social Psychiatry and Psychiatric Epidemiology. 2010;45:1063–1070. doi: 10.1007/s00127-009-0147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Boyd JE, Otilingam PG, DeForge BR. Brief version of the Internalized Stigma of Mental Illness (ISMI) scale: Psychometric properties and relationship to depression, self-esteem, recovery orientation, empowerment, and perceived devaluation and discrimination. Psychiatric Rehabilitation Journal. 2014;37:17–23. doi: 10.1037/prj0000035. [DOI] [PubMed] [Google Scholar]
- Brewer MB. The social psychology of intergroup relations: Social categorization, ingroup bias, and outgroup prejudice. In: Kruglanski AW, Higgins ET, editors. Social psychology: Handbook of basic principles. 2. New York, NY: Guilford Press; 2007. pp. 695–715. [Google Scholar]
- *.Brohan E, Clement S, Rose D, Sartorius N, Slade M, Thornicroft G. Development and psychometric evaluation of the Discrimination and Stigma Scale (DISC) Psychiatry Research. 2013;208:33–40. doi: 10.1016/j.psychres.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Brohan E, Clement S, Rose D, Sartorius N, Slade M, Thornicroft G. Development and psychometric evaluation of the Discrimination and Stigma Scale (DISC) Psychiatry Research. 2013;208:33–40. doi: 10.1016/j.psychres.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice, and discrimination: A review of measures. BMC Health Services Research. 2010;10:80–91. doi: 10.1186/1472-6963-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Brown SA. Factors and measurement of mental illness stigma: A psychometric examination of the Attribution Questionnaire. Psychiatric Rehabilitation Journal. 2008;32:89–94. doi: 10.2975/32.2.2008.89.94. [DOI] [PubMed] [Google Scholar]
- *.Brown SA. Standardized measures for substance use stigma. Drug and Alcohol Dependence. 2011;116:137–141. doi: 10.1016/j.drugalcdep.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Brown SA. Standardized measures for substance use stigma. Drug and Alcohol Dependence. 2011;116:137–141. doi: 10.1016/j.drugalcdep.2010.12.005. [DOI] [PubMed] [Google Scholar]
- *.Cathey AJ, Wetterneck CT. Stigma and disclosure of intrusive thoughts about sexual themes. Journal of Obsessive-Compulsive and Related Disorders. 2013;2:439–443. [Google Scholar]
- Cechnicki A, Angermeyer MC, Bielańska A. Anticipated and experienced stigma among people with schizophrenia: Its nature and correlates. Social Psychiatry And Psychiatric Epidemiology. 2011;46:643–650. doi: 10.1007/s00127-010-0230-2. [DOI] [PubMed] [Google Scholar]
- Chang CC, Wu TH, Chen CY, Wang JD, Lin CY. Psychometric evaluation of the Internalized Stigma of Mental Illness Scale for patients with mental illnesses: Measurement invariance across time. PloS One. 2014;9:e98767. doi: 10.1371/journal.pone.0098767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Chee CI, Ng TP, Kua EH. Comparing the stigma of mental illness in a general hospital with a state mental hospital: A Singapore study. Social Psychiatry And Psychiatric Epidemiology. 2005;40:648–653. doi: 10.1007/s00127-005-0932-z. [DOI] [PubMed] [Google Scholar]
- *.Christison GW, Haviland MG, Riggs ML. The Medical Condition Regard Scale: Measuring reactions to diagnoses. Academic Medicine. 2002;77:257–262. doi: 10.1097/00001888-200203000-00017. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7:309–319. doi: 10.1037/1040-3590.7.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Clayfield JC, Fletcher KE, Grudzinskas AJ. Development and validation of the Mental Health Attitude Survey for Police. Community Mental Health Journal. 2011;47(6):742–751. doi: 10.1007/s10597-011-9384-y. [DOI] [PubMed] [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Thornicroft G. What is the impact of mental health-related stigma on help- seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine. 2015;45:11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- *.Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. Journal of Abnormal and Social Psychology. 1962;64:349–360. doi: 10.1037/h0045526. [DOI] [PubMed] [Google Scholar]
- Cole ER. Intersectionality and research in psychology. American Psychologist. 2009;64:170–180. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- *.Collins PY, Elkington KS, von Unger H, Sweetland A, Wright ER, Zybert PA. Relationship of stigma to HIV risk among women with mental illness. American Journal of Orthopsychiatry. 2008;78:498–506. doi: 10.1037/a0014581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, von Unger H, Armbrister A. Church ladies, good girls, and locas: Stigma and the intersection of gender, ethnicity, mental illness, and sexuality in relation to HIV risk. Social Science & Medicine. 2008;67:389–397. doi: 10.1016/j.socscimed.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW. How stigma interferes with mental health care. American Psychologist. 2004;59:614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan PW. On the stigma of mental illness: Implications for research and social change. Washington, DC: American Psychological Association Press; 2005. [Google Scholar]
- *.Corrigan PW, Green A, Lundin RK, Kubiak MA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatric Services. 2001;52:953–958. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kerr A, Knudsen L. The stigma of mental illness: Explanatory models and methods for change. Applied and Preventive Psychology. 2005;11:179–190. doi: 10.1016/j.appsy.2005.07.001. [DOI] [Google Scholar]
- *.Corrigan PW, Michaels PJ, Vega E, Gause M, Watson AC, Rüsch N. Self-Stigma of Mental Illness Scale—Short Form: Reliability and validity. Psychiatry Research. 2012;199:65–69. doi: 10.1016/j.psychres.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Miller FE. Shame, blame, and contamination: A review of the impact of mental illness stigma on family members. Journal of Mental Health. 2004;13:537–548. doi: 10.1037/0893-3200.20.2.239. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: A meta-analysis of outcome studies. Psychiatric Services. 2012;63:963–973. doi: 10.1176/appi.ps.201100529. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Rafacz J, Rüsch N. Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Research. 2011;189:339–343. doi: 10.1016/j.psychres.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Rao D. On the self-stigma of mental illness: Stages, disclosure, and strategies for change. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 2012;57:464–469. doi: 10.1177/070674371205700804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Corrigan PW, River LP, Lundin RK, Wasowski KU, Campion J, Mathisen J, Kubiak MA. Stigmatizing attributions about mental illness. Journal of Community Psychology. 2000;28:91–102. [Google Scholar]
- Corrigan PW, Rüsch N. Mental illness stereotypes and clinical care: Do people avoid treatment because of stigma? Psychiatric Rehabilitation Skills. 2002;6:312–334. doi: 10.1080/10973430208408441. [DOI] [Google Scholar]
- Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clinical Psychology Review. 2010;30:907–922. doi: 10.1016/j.cpr.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Thompson V, Lambert D, Sangster Y, Noel JG, Campbell J. Perceptions of discrimination among persons with serious mental illness. Psychiatric Services. 2003;54:1105–1110. doi: 10.1176/appi.ps.54.8.1105. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002;9:35–53. [Google Scholar]
- *.Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. Journal of Social and Clinical Psychology. 2006;25:875–884. doi: 10.1521/jscp.2006.25.8.875. [DOI] [Google Scholar]
- *.Corrigan PW, Watson AC, Warpinkski AC, Garcia G. Stigmatizing attitudes about mental illness and allocation of resources to mental health services. Community Mental Health Journal. 2004;40:297–307. doi: 10.1023/B:COMH.0000035226.19939.76. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, Gracia G, Slopen N, Rasinski K, Hall LL. Newspaper stories as measures of structural stigma. Psychiatric Services. 2005;56:551–556. doi: 10.1176/appi.ps.56.5.551. [DOI] [PubMed] [Google Scholar]
- Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review. 1991;43:1241–1299. doi: 10.2307/1229039. [DOI] [Google Scholar]
- *.Crisp AH. Stigmatisation of people with mental illnesses. The British Journal of Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B. Social stigma and self-esteem: The self-protective properties of stigma. Psychological Review. 1989;96:608–630. [Google Scholar]
- *.Dalky HF. Arabic translation and cultural adaptation of the stigma-devaluation scale in Jordan. Journal of Mental Health. 2012;21:72–82. doi: 10.3109/09638237.2011.629238. [DOI] [PubMed] [Google Scholar]
- *.Day EN, Edgren K, Eshleman A. Measuring stigma toward mental illness: Development and application of the Mental Illness Stigma Scale. Journal of Applied Social Psychology. 2007;37:2191–2219. doi: 10.1111/j.1559-1816.2007.00255.x. [DOI] [Google Scholar]
- Deacon H. Towards a sustainable theory of health-related stigma: Lessons from the HIV/AIDS literature. Journal of Community & Applied Social Psychology. 2006;16:418–425. doi: 10.1002/casp.900. [DOI] [Google Scholar]
- Dovidio JF, Glick PE, Rudman LA. On the nature of prejudice: Fifty years after Allport. Malden, MA: Blackwell; 2005. [Google Scholar]
- Dovidio JF, Hewstone M, Glick P, Esses VM. Prejudice, stereotyping and discrimination: Theoretical and empirical overview. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. SAGE Handbook of Prejudice, Stereotyping, and Discrimination. Thousand Oaks, CA: Sage Publications; 2010. pp. 3–28. [Google Scholar]
- *.Eack SM, Newhill CE. An investigation of the relations between student knowledge, personal contact, and attitudes toward individuals with schizophrenia. Journal of Social Work Education. 2008;44:77–96. doi: 10.5175/JSWE.2008.200700009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. Journal of Health Psychology. 2012;17:157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Schweinle W, Anderson SM. Reliability and validity of the Attitudes Toward Seeking Professional Psychological Help Scale-short form. Psychiatry Research. 2008;159:320–329. doi: 10.1016/j.psychres.2007.04.020. [DOI] [PubMed] [Google Scholar]
- *.Evans-Lacko S, Little K, Meltzer H, Rose D, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the Mental Health Knowledge Schedule. The Canadian Journal of Psychiatry / La Revue Canadienne de Psychiatrie. 2010;55:440–447. doi: 10.1177/070674371005500707. [DOI] [PubMed] [Google Scholar]
- *.Evans-Lacko S, Rose D, Little K, Flach C, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the Reported and Intended Behaviour Scale (RIBS): A stigma-related behaviour measure. Epidemiology and Psychiatric Sciences. 2011;20:263–271. doi: 10.1017/S2045796011000308. [DOI] [PubMed] [Google Scholar]
- Farina A, Felner RD. Employment interviewer reactions to former mental patients. Journal of Abnormal Psychology. 1973;82:268–272. doi: 10.1002/1520-6629(197404)2:2. [DOI] [PubMed] [Google Scholar]
- Farina A, Thaw J, Lovern JD, Mangone D. People's reactions to a former mental patient moving to their neighborhood. Journal of Community Psychology. 1974;2:108–112. [Google Scholar]
- Feldman DB, Crandall CS. Dimensions of mental illness stigma: What about mental illness causes social rejection? Journal of Social and Clinical Psychology. 2007;26:137–154. doi: 10.1521/jscp.2007.26.2.137. [DOI] [Google Scholar]
- *.Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and Cancer. Journal of Health and Social Behavior. 2000;41:50–67. doi: 10.2307/2676360. [DOI] [PubMed] [Google Scholar]
- *.Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. Journal of Behavioral Health Services and Research. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- Freidl M, Piralic Spitzl S, Aigner M. How depressive symptoms correlate with stigma perception of mental illness. International Review of Psychiatry. 2008;20:510–514. doi: 10.1080/09540260802565422. [DOI] [PubMed] [Google Scholar]
- *.Fresan A, Robles-Garcia R, de Benito L, Saracco R, Escamilla R. Development and psychometric properties of a brief instrument to measure the stigma of aggressiveness in Schizophrenia. Actas Españolas de Psiquiatría: Acepsi. 2010;38:340–344. [PubMed] [Google Scholar]
- *.Fuermaier AB, Tucha L, Koerts J, Mueller AK, Lange KW, Tucha O. Measurement of stigmatization towards adults with attention deficit hyperactivity disorder. PloS One. 2012;7:e51755. doi: 10.1371/journal.pone.0051755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Fung KMT, Tsang HWH, Corrigan PW, Lam CS, Cheng W-M. Measuring self-stigma of mental illness in China and its implications for recovery. International Journal of Social Psychiatry. 2007;53:408–418. doi: 10.1177/0020764007086524. [DOI] [PubMed] [Google Scholar]
- *.Gabbidon J, Brohan E, Clement S, Henderson C, Thornicroft G, Group MS. The development and validation of the Questionnaire on Anticipated Discrimination. BMC Psychiatry. 2013;13:297–311. doi: 10.1186/1471-244X-13-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbidon J, Brohan E, Clement S, Henderson C, Thornicroft G, Group MS. The development and validation of the Questionnaire on Anticipated Discrimination. BMC Psychiatry. 2013;13:297–311. doi: 10.1186/1471-244X-13-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gabbidon J, Clement S, van Nieuwenhuizen A, Kassam A, Brohan E, Norman I, Thornicroft G. Mental illness: Clinicians' Attitudes (MICA) Scale: Psychometric properties of a version for healthcare students and professionals. Psychiatry Research. 2013;206:81–87. doi: 10.1016/j.psychres.2012.09.028. [DOI] [PubMed] [Google Scholar]
- *.Gabriel A, Violato C. The development and psychometric assessment of an instrument to measure attitudes towards depression and its treatments in patients suffering from non-psychotic depression. Journal of Affective Disorders. 2010;124:241–249. doi: 10.1016/j.jad.2009.11.009. [DOI] [PubMed] [Google Scholar]
- *.Gang M, Song Y, Park SY, Yang S. Psychometric evaluation of the Korean version of the attitudes toward acute mental health scale. Journal of Psychiatric Mental Health Nursing. 2014;21:939–948. doi: 10.1111/jpm.12164. [DOI] [PubMed] [Google Scholar]
- *.Gilbert P, Bhundia R, Mitra R, McEwan K, Irons C, Sanghera J. Cultural differences in shame-focused attitudes towards mental health problems in Asian and non-Asian student women. Mental Health, Religion & Culture. 2007;10:127–141. [Google Scholar]
- *.Glass JE, Kristjansson SD, Bucholz KK. Perceived alcohol stigma: Factor structure and construct validation. Alcoholism, Clinical and Experimental Research. 2013;37(Suppl 1):E237–246. doi: 10.1111/j.1530-0277.2012.01887.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster Inc.; 1963. [Google Scholar]
- Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatric Services. 2008;59:392–399. doi: 10.1176/ps.2008.59.4.392. [DOI] [PubMed] [Google Scholar]
- *.Griffiths KM, Batterham PJ, Barney L, Parsons A. The Generalised Anxiety Stigma Scale (GASS): Psychometric properties in a community sample. BMC Psychiatry. 2011;11:184–193. doi: 10.1186/1471-244x-11-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Griffiths KM, Christensen H, Jorm AF. Predictors of depression stigma. BMC Psychiatry. 2008;8:25–36. doi: 10.1186/1471-244X-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths KM, Christensen H, Jorm AF. Predictors of depression stigma. BMC Psychiatry. 2008;8:25–36. doi: 10.1186/1471-244X-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatising attitudes to depression: Randomised controlled trial. British Journal of Psychiatry. 2004;185:342–349. doi: 10.1192/bjp.185.4.342. [DOI] [PubMed] [Google Scholar]
- *.Haghighat R. The development of an instrument to measure stigmatization: Factor analysis and origin of stigmatization. The European Journal of Psychiatry. 2005;19:144–154. doi: 10.4321/S0213-61632005000300002. [DOI] [Google Scholar]
- *.Happell B, Gough K. Undergraduate nursing students' attitudes towards mental health: Understanding the influencing factors. Contemporary Nurse: A Journal for the Australian Nursing Profession. 2007;25:72–81. doi: 10.5172/conu.2007.25.1-2.72. [DOI] [PubMed] [Google Scholar]
- *.Harvey RD. Individual differences in the phenomenological impact of social stigma. The Journal of Social Psychology. 2001;141:174–189. doi: 10.1080/00224540109600545. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Social Science & Medicine. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebl MR, Tickle J, Heatherton TF. Awkward moments in interactions between nonstigmatized and stigmatized individuals. The Social Psychology of Stigma. 2000:275–306. [Google Scholar]
- *.Heflinger CA, Wallston KA, Mukolo A, Brannon AM. Perceived stigma toward children with emotional and behavioral problems and their families: The attitudes about child mental health questionnaire (ACMHQ) Journal of Rural Mental Health. 2014;38:9–19. doi: 10.1037/rmh0000010. [DOI] [Google Scholar]
- *.Hirai M, Clum GA. Development, reliability, and validity of the Beliefs Toward Mental Illness Scale. Journal of Psychopathology and Behavioral Assessment. 2000;22:221–236. doi: 10.1023/A:1007548432472. [DOI] [Google Scholar]
- *.Hirsch JA. Development of the biases toward children with psychological and behavioral disorders scale. Psychological Reports. 2013;113:855–873. doi: 10.2466/08.07.PR0.113x26z0. [DOI] [PubMed] [Google Scholar]
- Hogberg T, Magnusson A, Lutzen K, Ewalds-Kvist B. Swedish attitudes towards persons with mental illness. Nordic Journal of Psychiatry. 2012;66:86–96. doi: 10.3109/08039488.2011.596947. [DOI] [PubMed] [Google Scholar]
- hooks bell. Yearning: Race, gender, and cultural politics. Boston, MA: South End Press; 1990. [Google Scholar]
- *.Ilic M, Reinecke J, Bohner G, Röttgers H-O, Beblo T, Driessen M, Corrigan PW. Belittled, avoided, ignored, denied: Assessing forms and consequences of stigma experiences of people with mental illness. Basic and Applied Social Psychology. 2013;35:31–40. doi: 10.1080/01973533.2012.746619. [DOI] [Google Scholar]
- Jung SH, Kim HJ. Perceived stigma and quality of life of individuals diagnosed with schizophrenia and receiving psychiatric rehabilitation services: A comparison between the clubhouse model and a rehabilitation skills training model in South Korea. Psychiatric Rehabilitation Journal. 2012;35:460–465. doi: 10.1037/h0094580. [DOI] [PubMed] [Google Scholar]
- Kalyanaraman S, Penn DL, Ivory JD, Judge A. The virtual doppelganger: Effects of a virtual reality simulator on perceptions of Schizophrenia. Journal of Nervous and Mental Disease. 2010;198:437–443. doi: 10.1097/NMD.0b013e3181e07d66. [DOI] [PubMed] [Google Scholar]
- *.Kanter JW, Rusch LC, Brondino MJ. Depression self-stigma: A new measure and preliminary findings. Journal of Nervous and Mental Disease. 2008;196:663–670. doi: 10.1097/NMD.0b013e318183f8af. [DOI] [PubMed] [Google Scholar]
- *.Karidi MV, Stefanis CN, Theleritis C, Tzedaki M, Rabavilas AD, Stefanis NC. Perceived social stigma, self-concept, and self-stigmatization of patient with Schizophrenia. Comprehensive Psychiatry. 2010;51:19–30. doi: 10.1016/j.comppsycha.2009.01.001. [DOI] [PubMed] [Google Scholar]
- *.Karidi MV, Vasilopoulou D, Savvidou E, Vitoratou S, Rabavilas AD, Stefanis CN. Aspects of perceived stigma: The Stigma Inventory for Mental Illness, its development, latent structure and psychometric properties. Comprehensive Psychiatry. 2014;55:1620–1625. doi: 10.1016/j.comppsych.2014.04.002. [DOI] [PubMed] [Google Scholar]
- *.Kassam A, Glozier N, Leese M, Henderson C, Thornicroft G. Development and responsiveness of a scale to measure clinicians' attitudes to people with mental illness (medical student version) Acta Psychiatrica Scandinavica. 2010;122:153–161. doi: 10.1111/j.1600-0447.2010.01562.x. [DOI] [PubMed] [Google Scholar]
- *.Kassam A, Papish A, Modgill G, Patten S. The development and psychometric properties of a new scale to measure mental illness related stigma by health care providers: The Opening Minds Scale for Health Care Providers (OMS-HC) BMC Psychiatry. 2012;12:62–73. doi: 10.1186/1471-244x-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kellison I, Bussing R, Bell L, Garvan C. Assessment of stigma associated with Attention-Deficit Hyperactivity Disorder: Psychometric evaluation of the ADHD Stigma Questionnaire. Psychiatry Research. 2010;178:363–369. doi: 10.1016/j.psychres.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kelly JA, St Lawrence JS, Smith S, Hood HV, Cook DJ. Medical Students' Attitudes toward AIDS and Homosexual Patients. Journal of Medical Education. 1987;62:549–556. doi: 10.1097/00001888-198707000-00003. [DOI] [PubMed] [Google Scholar]
- Kelly JF. Toward an Addictionary: A proposal for more precise terminology. Alcoholism Treatment Quarterly. 2004;22:79–87. doi: 10.1300/J020v22n02_07. [DOI] [Google Scholar]
- *.King M, Dinos S, Shaw J, Watson R, Stevens S, Passetti F, Serfaty M. The Stigma Scale: Development of a standardised measure of the stigma of mental illness. British Journal of Psychiatry. 2007;190:248–254. doi: 10.1192/bjp.bp.106.024638. [DOI] [PubMed] [Google Scholar]
- *.Kira IA, Hammad A, Simaan A. The effects of stigma consciousness on mental health. Ethnicity and Disease. 2005;15(Suppl 1):S1–104. [PubMed] [Google Scholar]
- *.Kobau R, DiIorio C, Chapman D, Delvecchio P. Attitudes about mental illness and its treatment: Validation of a generic scale for public health surveillance of mental illness associated stigma. Community Mental Health Journal. 2010;46:164–176. doi: 10.1007/s10597-009-9191-x. [DOI] [PubMed] [Google Scholar]
- Kondrat DC. Do treatment processes matter more than stigma? The relative impacts of working alliance, provider effects, and self-stigma on consumers' perceived quality of life. Best Practices in Mental Health: An International Journal. 2012;8:85–103. [Google Scholar]
- *.Kroska A, Harkness SK. Stigma sentiments and self-meanings: Exploring the modified labeling theory of mental illness. Social Psychology Quarterly. 2006;69:325–348. doi: 10.1177/019027250606900403. [DOI] [Google Scholar]
- *.Lai YM, Hong CPH, Chee CYI. Stigma of mental illness. Singapore Medical Journal. 2001;42:111–114. [PubMed] [Google Scholar]
- Larson JE, Corrigan P. The stigma of families with mental illness. Academic Psychiatry. 2008;32:87–91. doi: 10.1176/appi.ap.32.2.87. [DOI] [PubMed] [Google Scholar]
- *.Lauber C, Nordt C, Falcato L, Rössler W. Public acceptance of restrictions on mentally ill people. Acta Psychiatrica Scandinavica. 2000;102(s407):26–32. doi: 10.1034/j.1600-0447.2000.00005.x. [DOI] [PubMed] [Google Scholar]
- *.Link BG. Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review. 1987;52:96–112. [Google Scholar]
- Link BG. Stigma: Many mechanisms require multifaceted responses. Epidemiologia e Psichiatria Sociale. 2001;10:8–11. doi: 10.1017/S1121189X00008484. [DOI] [PubMed] [Google Scholar]
- *.Link BG, Cullen FT. Contact with the mentally ill and perceptions of how dangerous they are. Journal of Health and Social Behavior. 1986;27:289–303. doi: 10.2307/2136945. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. doi: 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. The Lancet. 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- *.Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: Understanding why labels matter. The American Journal of Sociology. 1987;92:1461–1500. [Google Scholar]
- *.Link BG, Cullen FT, Struening EL, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review. 1989;54:400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- *.Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: Can negative consequences of mental illness labeling be avoided? Journal of Health and Social Behavior. 1991;32:302–320. [PubMed] [Google Scholar]
- *.Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. On describing and seeking to change the experience of stigma. Psychiatric Rehabilitation Skills. 2002;6:201–231. doi: 10.1080/10973430208408433. [DOI] [Google Scholar]
- *.Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior. 1997;38:177–190. doi: 10.2307/2955424. [DOI] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophrenia Bulletin. 2004;30:511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Livingston JD. Mental illness-related structural stigma: The downward spiral of systemic exclusion. 2013 Retrieved from http://www.mentalhealthcommission.ca/sites/default/files/MHCC_OpeningMinds_MentalIllness RelatedSructuralStigmaReport_ENG_0_0.pdf.
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Lucksted A, Drapalski A, Calmes C, Forbes C, DeForge B, Boyd J. Ending self-stigma: Pilot evaluation of a new intervention to reduce internalized stigma among people with mental illnesses. Psychiatric Rehabilitation Journal. 2011;35:51–54. doi: 10.2975/35.1.2011.51.54. [DOI] [PubMed] [Google Scholar]
- *.Luoma JB, Nobles RH, Drake CE, Hayes SC, O'Hair A, Fletcher L, Kohlenberg BS. Self-stigma in substance abuse: Development of a new measure. Journal of Psychopathology and Behavioral Assessment. 2013;35:223–234. doi: 10.1007/s10862-012-9323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Nobles RH, Drake CE, Hayes SC, O'Hair A, Fletcher L, Kohlenberg BS. Self-Stigma in substance abuse: Development of a new measure. Journal of Psychopathology and Behavioral Assessment. 2013;35:223–234. doi: 10.1007/s10862-012-9323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Luoma JB, O'Hair AK, Kohlenberg BS, Hayes SC, Fletcher L. The development and psychometric properties of a new measure of perceived stigma toward substance users. Substance Use and Misuse. 2010;45:47–57. doi: 10.3109/10826080902864712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, Fisher G. An investigation of stigma in individuals receiving treatment for substance abuse. Addictive Behaviors. 2007;32:1331–1346. doi: 10.1016/j.addbeh.2006.09.008. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, Fisher G. An investigation of stigma in individuals receiving treatment for substance abuse. Addictive Behaviors. 2007;32:1331–1346. doi: 10.1016/j.addbeh.2006.09.008. [DOI] [PubMed] [Google Scholar]
- *.Luty J, Fekadu D, Umoh O, Gallagher J. Validation of a short instrument to measure stigmatised attitudes towards mental illness. Psychiatric Bulletin. 2006;30:257–260. doi: 10.1192/pb.30.7.257. [DOI] [Google Scholar]
- *.Madianos M, Economou M, Peppou LE, Kallergis G, Rogakou E, Alevizopoulos G. Measuring public attitudes to severe mental illness in Greece: Development of a new scale. European Journal of Psychiatry. 2012;26:55–67. [Google Scholar]
- *.Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M. Beliefs about Schizophrenia in Italy: A comparative nationwide survey of the general public, mental health professionals, and patients' relatives. Canadian Journal of Psychiatry. 2004;49:322–330. [PubMed] [Google Scholar]
- *.Magliano L, Fiorillo A, Del Vecchio H, Malangone C, De Rosa C, Bachelet C, Maj M. Development and validation of a self-reported questionnaire on users' opinions about schizophrenia: a participatory research. International Journal of Social Psychiatry. 2009;55:425–441. doi: 10.1177/0020764008099414. [DOI] [PubMed] [Google Scholar]
- *.Magliano L, Marasco C, Malangone G, Lacrimini G, Zanus P, Maj M. A new questionnaire assessing the opinions of the relatives of patients with Schizophrenia on the causes and social consequences of the disorder: Reliability and validity. European Psychiatry. 1999;14:71–75. doi: 10.1016/S0924-9338(99)80720-2. [DOI] [PubMed] [Google Scholar]
- Mak WWS, Cheung RYM. Affiliate stigma among caregivers of people with intellectual disability or mental illness. Journal of Applied Research in Intellectual Disabilities. 2008;21:532–545. [Google Scholar]
- *.Mak WWS, Cheung RYM. Self-stigma among concealable minorities in Hong Kong: Conceptualization and unified measurement. American Journal of Orthopsychiatry. 2010;80:267–281. doi: 10.1111/j.1939-0025.2010.01030.x. [DOI] [PubMed] [Google Scholar]
- *.Mak WW, Chong ES, Wong CC. Beyond attributions: Understanding public stigma of mental illness with the common sense model. American Journal of Orthopsychiatry. 2014;84:173–181. doi: 10.1037/h0099373. [DOI] [PubMed] [Google Scholar]
- Mak WW, Poon CY, Pun LY, Cheung SF. Meta-analysis of stigma and mental health. Social Science & Medicine. 2007;65:245–261. doi: 10.1016/j.socscimed.2007.03.015. [DOI] [PubMed] [Google Scholar]
- *.Marcks BA, Berlin KS, Woods DW, Davies WH. Impact of Tourette Syndrome: A preliminary investigation of the effects of disclosure on peer perceptions and social functioning. Psychiatry. 2007;70:59–67. doi: 10.1521/psyc.2007.70.1.59. [DOI] [PubMed] [Google Scholar]
- Martin JK, Pescosolido BA, Olafsdottir S, McLeod JD. The construction of fear: Americans' preferences for social distance from children and adolescents with mental health problems. Journal of Health and Social Behavior. 2007;48:50–67. doi: 10.1177/002214650704800104. [DOI] [PubMed] [Google Scholar]
- *.Masuda A, Price M, Anderson PL, Schmertz SK, Calamaras MR. The role of psychological flexibility in mental health stigma and psychological distress for the stigmatizer. Journal of Social and Clinical Psychology. 2009;28:1244–1262. [Google Scholar]
- *.Michaels PJ, Corrigan PW. Measuring mental illness stigma with diminished social desirability effects. Journal of Mental Health. 2013;22:218–226. doi: 10.3109/09638237.2012.734652. [DOI] [PubMed] [Google Scholar]
- *.Mileva VR, Vazquez GH, Milev R. Effects, experiences, and impact of stigma on patients with bipolar disorder. Neuropsychiatric Disease and Treatment. 2013;9:31–40. doi: 10.2147/NDT.S38560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Modgill G, Patten SB, Knaak S, Kassam A, Szeto AC. Opening minds stigma scale for health care providers (OMS-HC): examination of psychometric properties and responsiveness. BMC Psychiatry. 2014;14:120. doi: 10.1186/1471-244X-14-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, de Vet HCW. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: A clarification of its content. BMC Medical Research Methodology. 2010a;10:22. doi: 10.1186/1471-2288-10-22. http://dx.doi.org/10.1186/1471-2288-6-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, de Vet HCW. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. Journal of Clinical Epidemiology. 2010b;63:737–745. doi: 10.1016/j.jclinepi.2010.02.006. http://dx.doi.org/10.1016/j.jclinepi.2010.02.006 [DOI] [PubMed] [Google Scholar]
- *.Moses T. Stigma and self-concept among adolescents receiving mental health treatment. American Journal of Orthopsychiatry. 2009;79:261–274. doi: 10.1037/a0015696. [DOI] [PubMed] [Google Scholar]
- National Alliance for the Mentally Ill—Greater Chicago. Mental Health 2013: An important public health issue. [Retrieved March 3, 2015];2013 Retrieved from http://www.namigc.org/wp-content/uploads/2013/01/MentalIllnessFactSheet-July-2013.pdf.
- Nelson TD, editor. Handbook of prejudice, stereotyping, and discrimination. New York: Psychology Press; 2009. [Google Scholar]
- *.Ng P, Chan K. Sex differences in opinion towards mental illness of secondary school students in Hong Kong. International Journal of Social Psychiatry. 2000;46:79–88. doi: 10.1177/002076400004600201. [DOI] [PubMed] [Google Scholar]
- *.Palamar JJ, Kiang MV, Halkitis PN. Development and psychometric evaluation of scales that assess stigma associated with illicit drug users. Substance Use & Misuse. 2011;46:1457–1467. doi: 10.3109/10826084.2011.596606. [DOI] [PubMed] [Google Scholar]
- *.Pan AW, Chung L, Fife BL, Hsiung PC. Evaluation of the psychometrics of the Social Impact Scale: A measure of stigmatization. International Journal of Rehabilitation Research. 2007;30:235–238. doi: 10.1097/MRR.0b013e32829fb3db. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Penn DL, Guynan K, Dally T, Spaulding WD, Garbin CP, Sullivan M. Dispelling the stigma of Schizophrenia: What sort of information is best? Schizophrenia Bulletin. 1994;20:567–578. doi: 10.1093/schbul/20.3.567. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Martin JK. The stigma complex. Annual Review of Sociology. 2015;41:87–116. doi: 10.1146/annurev-soc-071312-145702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido BA, Martin JK, Lang A, Olafsdottir S. Rethinking theoretical approaches to stigma: A framework integrating normative influences on stigma (FINIS) Social Science & Medicine. 2008;67:431–440. doi: 10.1016/j.socscimed.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: One animal or two? Social Science & Medicine. 2008;67:358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Pinel EC. Stigma Consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037/0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- *.Pinfold V, Toulmin H, Thornicroft G, Huxley P, Farmer P, Graham T. Reducing psychiatric stigma and discrimination: Evaluation of educational interventions in UK secondary schools. British Journal of Psychiatry. 2003;182:342–346. doi: 10.1192/bjp.182.4.342. [DOI] [PubMed] [Google Scholar]
- *.Pingani L, Forghieri M, Ferrari S, Ben-Zeev D, Artoni P, Mazzi F, Corrigan PW. Stigma and discrimination toward mental illness: Translation and validation of the Italian version of the Attribution Questionnaire-27 (AQ-27) Social Psychiatry and Psychiatric Epidemiology. 2012;47:993–999. doi: 10.1007/s00127-011-0407-3. [DOI] [PubMed] [Google Scholar]
- *.Pinto MD, Hickman R, Logsdon MC, Burant C. Psychometric evaluation of the revised attribution questionnaire (r-AQ) to measure mental illness stigma in adolescents. Journal of Nursing Measurement. 2012;20:47–58. doi: 10.1891/1061-3749.20.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pryor JB, Reeder GD. HIV-related stigma. In: Hall JC, Hall BJ, Cockerell CJ, editors. HIV/AIDS in the Post-HAART Era: Manifestations, treatment, and Epidemiology. Shelton, CT: PMPH-USA; 2011. pp. 790–806. [Google Scholar]
- Pugh T, Hatzenbuehler M, Link B. Structural Stigma and Mental Illness. Commissioned paper for Committee on the Science of Changing Behavioral Health Social Norms. 2015 Retrieved from http://sites.nationalacademies.org/cs/groups/dbassesite/documents/webpage/dbasse_170045.pdf.
- *.Quinn DM, Chaudoir SR. Living with a concealable stigmatized identity: The impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology. 2009;97(4):634. doi: 10.1037/a0015815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Earnshaw VA. Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes. Social Issues and Policy Review. 2011;5:160–190. doi: 10.1111/j.1751-2409.2011.01029.x. [DOI] [Google Scholar]
- Quinn DM, Earnshaw VA. Concealable stigmatized identities and psychological well-being. Social and Personality Psychology Compass. 2013;7:40–51. doi: 10.1111/spc3.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Williams MK, Weisz BM. From discrimination to internalized mental illness stigma: The mediating roles of anticipated discrimination and anticipated stigma. Psychiatric Rehabilitation Journal. 2015;38:103–108. doi: 10.1037/prj0000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Raguram R, Weiss MG. EMIC interview for outpatient psychiatry and stigma. Instrument for collaborative research. National Institute of Mental Health and Neuro Sciences, Bangalore, India and Swiss Tropical Institute, Basel, Switzerland 1997 [Google Scholar]
- Rao D, Feinglass J, Corrigan P. Racial and ethnic disparities in mental illness stigma. Journal of Nervous and Mental Disease. 2007;195:1020–1023. doi: 10.1097/NMD.0b013e31815c046e. [DOI] [PubMed] [Google Scholar]
- *.Read J, Harre N. The role of biological and genetic causal beliefs in the stigmatisation of ‘mental patients’. Journal of Mental Health. 2001;10:223–235. doi: 10.1080/09638230020023778. [DOI] [Google Scholar]
- Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Research. 2004;129:257–265. doi: 10.1016/j.psychres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- *.Royal KD, Thompson JA. A psychometric validation of the Beliefs Toward Mental Illness Scale. Journal of Nursing Measurement. 2013;21:516–524. doi: 10.1891/1061-3749.21.3.516. doi: 1061-3749.21.3.516. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Lieb K, Bohus M, Corrigan PW. Brief reports: Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatric Services. 2006;57:399–402. doi: 10.1176/appi.ps.57.3.399. [DOI] [PubMed] [Google Scholar]
- *.Sanders Thompson VL, Noel JG, Campbell J. Stigmatization, discrimination, and mental health: The impact of multiple identity status. American Journal of Orthopsychiatry. 2004;74:529–544. doi: 10.1037/0002-9432.74.4.529. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Angermeyer MC. Stigma and its impact on help-seeking for mental disorders: What do we know? Epidemiologia e Psichiatria Sociale. 2008;17:31–37. doi: 10.1017/s1121189x00002669. [DOI] [PubMed] [Google Scholar]
- *.Schulze B, Richter-Werling M, Matschinger H, Angermeyer MC. Crazy? So what! Effects of a school project on students’ attitudes towards people with Schizophrenia. Acta Psychiatrica Scandinavica. 2003;107:142–150. doi: 10.1034/j.1600-0447.2003.02444.x. [DOI] [PubMed] [Google Scholar]
- *.Scheerder G, Van Audenhove C, Arensman E, Bernik B, Giupponi G, Horel AC, Hegerl U. Community and health professionals' attitude toward depression: a pilot study in nine EAAD countries. International Journal of Social Psychiatry. 2011;57:387–401. doi: 10.1177/0020764009359742. [DOI] [PubMed] [Google Scholar]
- *Scocco P, Castriotta C, Toffol E, Preti A. Stigma of Suicide Attempt (STOSA) scale and Stigma of Suicide and Suicide Survivor (STOSASS) scale: Two new assessment tools. Psychiatry Research. 2012;200:872–878. doi: 10.1016/j.psychres.2012.06.033. [DOI] [PubMed] [Google Scholar]
- *.Segal SP, Silverman CJ, Temkin TL. Self-stigma and empowerment in combined-CMHA and consumer-run services: Two controlled trials. Psychiatric Services. 2013;64:990–996. doi: 10.1176/appi.ps.201200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Sibitz I, Friedrich ME, Unger A, Bachmann A, Benesch T, Amering M. Internalized stigma of Schizophrenia: Validation of the German version of the Internalized Stigma of Mental Illness-Scale (ISMI) Psychiatrische Praxis. 2013;40:83–91. doi: 10.1055/s-0032-1332878. [DOI] [PubMed] [Google Scholar]
- Sibitz I, Unger A, Woppmann A, Zidek T, Amering M. Stigma resistance in patients with schizophrenia. Schizophrenia Bulletin. 2011;37:316–323. doi: 10.1093/schbul/sbp048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silton NR, Flannelly KJ, Milstein G, Vaaler ML. Stigma in America: has anything changed?: Impact of perceptions of mental illness and dangerousness on the desire for social distance: 1996 and 2006. The Journal of Nervous and Mental Disease. 2011;199:361–366. doi: 10.1097/NMD.0b013e31821cd112. [DOI] [PubMed] [Google Scholar]
- *.Singh SP, Baxter H, Standen P, Duggan C. Changing the attitudes of `tomorrow's doctors' towards mental illness and psychiatry: A comparison of two teaching methods. Medical Education. 1998;32:114–120. doi: 10.1046/j.1365-2923.1998.00162.x. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Raue P, Friedman SJ, Meyers BS. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. American Journal of Psychiatry. 2001;158:479–481. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- *.Siu BW, Chow KK, Lam LC, Chan WC, Tang VW, Chui WW. A questionnaire survey on attitudes and understanding towards mental disorders. East Asian Archives of Psychiatry. 2012;22:18–24. [PubMed] [Google Scholar]
- Skopp NA, Bush NE, Vogel DL, Wade NG, Sirotin AP, McCann RA, Metzger-Abamukong MJ. Development and initial testing of a measure of public and self-stigma in the military. Journal of Clinical Psychology. 2012;68:1036–1047. doi: 10.1002/jclp.21889. [DOI] [PubMed] [Google Scholar]
- Stangor C. The study of stereotyping, prejudice, and discrimination within social psychology. In: Nelson TD, editor. Handbook of Prejudice, Stereotyping and Discrimination. New York. NY: Psychology Press; 2009. pp. 1–22. [Google Scholar]
- *.Stathi S, Tsantila K, Crisp RJ. Imagining intergroup contact can combat mental health stigma by reducing anxiety, avoidance and negative stereotyping. The Journal of Social Psychology. 2012;152:746–757. doi: 10.1080/00224545.2012.697080. [DOI] [PubMed] [Google Scholar]
- *.Stephan WG, Stephan CW. Intergroup anxiety. Journal of Social Issues. 1985;41:157–175. doi: 10.1111/j.1540-4560.1985.tb01134.x. [DOI] [Google Scholar]
- Stevelink SAM, Wu IC, Voorend CG, van Brakel WH. The psychometric assessment of internalized stigma instruments: A systematic review. Stigma Research and Action. 2012;2:100–118. [Google Scholar]
- *.Stuart H, Milev R, Koller M. The Inventory of Stigmatizing Experiences. World Psychiatry. 2005;4:33–37. [Google Scholar]
- *.Struening EL, Cohen J. Factorial invariance and other psychometric characteristics of five opinions about mental illness factors. Educational and Psychological Measurement. 1963;23:289–298. doi: 10.1177/001316446302300206. [DOI] [Google Scholar]
- *.Struening EL, Perlick DA, Link B, Hellman F, Herman D, Strey JA. Stigma as a barrier to recovery: The extent to which caregivers believe most people devalue consumers and their families. Psychiatric Services. 2001;52:1633–1638. doi: 10.1176/appi.ps.52.12.1633. [DOI] [PubMed] [Google Scholar]
- Stuart H. Mental illness and employment discrimination. Current Opinion in Psychiatry. 2006;19:522–526. doi: 10.1097/01.yco.0000238482.27270.5d. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) What a difference a friend makes. [Retrieved April 14, 2015];2008 from https://store.samhsa.gov/shin/content/SMA07-4257/SMA07-4257.pdf.
- *.Svensson B, Markström U, Bejerholm U, Björkman T, Brunt D, Eklund M, Östman M. Test-retest reliability of two instruments for measuring public attitudes towards persons with mental illness. BMC Psychiatry. 2011;11 doi: 10.1186/1471-244X-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Switaj P, Grygiel P, Wciorka J, Humenny G, Anczewska M. The Stigma subscale of the Consumer Experiences of Stigma Questionnaire (CESQ): A psychometric evaluation in Polish psychiatric patients. Comprehensive Psychiatry. 2013;54:713–719. doi: 10.1016/j.comppsych.2013.03.001. [DOI] [PubMed] [Google Scholar]
- *.Tanaka G, Inadomi H, Kikuchi Y, Ohta Y. Evaluation stigma against mental disorder and related factors. Psychiatry and Clinical Neurosciences. 2004;58:558–566. doi: 10.1111/j.1440-1819.2004.01300.x. [DOI] [PubMed] [Google Scholar]
- *.Taylor SM, Dear MJ. Scaling Community Attitudes Toward the Mentally Ill. Schizophrenia Bulletin. 1981;7:225–240. doi: 10.1093/schbul/7.2.225. [DOI] [PubMed] [Google Scholar]
- Terwee CB, Bot SDM, De Boer MR, van der Windt DAWM, Knol DL, Dekker J, de Vet HCW. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. http://dx.doi.org/10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- *.Thompson AH, Stuart H, Bland RC, Arboleda-Florez J, Warner R, Dickson RA Association, W. P. A. W. P. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Social Psychiatry and Psychiatric Epidemiology. 2002;37:475–482. doi: 10.1007/s00127-002-0583-2. [DOI] [PubMed] [Google Scholar]
- Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiologia e Psichiatria Sociale. 2008;17:14–19. doi: 10.1017/S1121189X00002621. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Rose D, Kassam A. Discrimination in health care against people with mental illness. International Review of Psychiatry. 2007;19:113–122. doi: 10.1080/09540260701278937. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: Ignorance, prejudice or discrimination? The British Journal of Psychiatry. 2007;190:192–193. doi: 10.1192/bjp.bp.106.025791. [DOI] [PubMed] [Google Scholar]
- Tucker JR, Hammer JH, Vogel DL, Bitman RL, Wade NG, Maier EJ. Disentangling self-stigma: Are mental illness and help-seeking self-stigmas different? Journal of Counseling Psychology. 2013;60:520–531. doi: 10.1037/a0033555. [DOI] [PubMed] [Google Scholar]
- *.Ucok A, Soygur H, Atakli C, Kuscu K, Sartorius N, Duman ZC, Erkoc S. The impact of antistigma education on the attitudes of general practitioners regarding Schizophrenia. Psychiatry and Clinical Neurosciences. 2006;60:439–443. doi: 10.1111/j.1440-1819.2006.01529.x. doi: 10.1111/j.1440- [DOI] [PubMed] [Google Scholar]
- Van Brakel WH. Measuring health-related stigma--a literature review. Psychology, Health & Medicine. 2006;11:307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- *.van der Heijden A, van der Bijl J, Latour CHM, Hoekstra H, van Meijel B. Student nurses' perceptions of mental health care: Validation of a questionnaire. Nurse Education Today. 2012;32:373–377. doi: 10.1016/j.nedt.2011.05.013. [DOI] [PubMed] [Google Scholar]
- Vauth R, Kleim B, Wirtz M, Corrigan PW. Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Research. 2007;150:71–80. doi: 10.1016/j.psychres.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology. 2006;53:325–337. [Google Scholar]
- *.Vogt D, Di Leone BAL, Wang JM, Sayer NA, Pineles SL, Litz BT. Endorsed and Anticipated Stigma Inventory (EASI) A tool for assessing beliefs about mental illness and mental health treatment among military personnel and veterans. Psychological Services. 2014;11:105–113. doi: 10.1037/a0032780. [DOI] [PubMed] [Google Scholar]
- Vogt D, Di Leone BAL, Wang JM, Sayer NA, Pineles SL, Litz BT. Endorsed and Anticipated Stigma Inventory (EASI) A tool for assessing beliefs about mental illness and mental health treatment among military personnel and veterans. Psychological Services. 2014;11:105–113. doi: 10.1037/a0032780. [DOI] [PubMed] [Google Scholar]
- *.Wahl OF. Mental health consumers' experiences of stigma. Schizophrenia Bulletin. 1999;25:467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- *Wahl OF, Susin J, Kaplan L, Lax A, Zatina D. Changing knowledge and attitudes with a middle school mental health education curriculum. Stigma Research in Action. 2011;1:44–53. doi: 10.5463/sra.v1i1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, Gureje O. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. The Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Watson AC, Miller FE, Lyons JS. Adolescent attitudes toward serious mental illness. The Journal of Nervous and Mental Disease. 2005;193:769–772. doi: 10.1097/01.nmd.0000185885.04349.99. [DOI] [PubMed] [Google Scholar]
- *.Watson AC, Otey E, Westbrook AL, Gardner AL, Lamb TA, Corrigan PW, Fenton WS. Changing middle schoolers' attitudes about mental illness through education. Schizophrenia Bulletin. 2004;30:563–572. doi: 10.1093/oxfordjournals.schbul.a007100. [DOI] [PubMed] [Google Scholar]
- *.Weiss M. Explanatory Model Interview Catalogue (EMIC): Framework for comparative study of illness. Transcultural Psychiatry. 1997;34:235–263. doi: 10.1177/136346159703400204. [DOI] [Google Scholar]
- *.Weiss MG, Doongaji DR, Siddhartha S, Wypij D, Pathare S, Bhatawdekar M, Fernandes R. The Explanatory Model Interview Catalogue (EMIC). Contribution to cross-cultural research methods from a study of leprosy and mental health. The British Journal of Psychiatry. 1992;160:819–830. doi: 10.1192/bjp.160.6.819. [DOI] [PubMed] [Google Scholar]
- *.Weller L, Grunes S. Does contact with the mentally ill affect nurses’ attitudes to mental illness? British Journal of Medical Psychology. 1988;61:277–284. doi: 10.1111/j.2044-8341.1988.tb02789.x. [DOI] [PubMed] [Google Scholar]
- Werner P, Stein-Shvachman I, Heinik J. Perceptions of self-stigma and its correlates among older adults with depression: A preliminary study. International Psychogeriatrics. 2009;21:1180–1189. doi: 10.1017/s1041610209990470. [DOI] [PubMed] [Google Scholar]
- Whaley AL. Ethnic and racial differences in perceptions of dangerousness of persons with mental illness. Psychiatric Services. 1997;48:1328–1330. doi: 10.1176/ps.48.10.1328. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93:200–208. doi: 10.2105/AJPH.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial Differences in Physical and Mental Health. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- *.Wolff G, Pathare S, Craig T, Leff J. Community attitudes to mental illness. British Journal of Psychiatry. 1996;168:183–190. doi: 10.1192/bjp.168.2.183. [DOI] [PubMed] [Google Scholar]
- *.Wood AL, Wahl OF. Evaluating the effectiveness of a consumer-provided mental health recovery education presentation. Psychiatric Rehabilitation Journal. 2006;30:46–53. doi: 10.2975/30.2006.46.53. [DOI] [PubMed] [Google Scholar]
- *.Wrigley S, Jackson H, Judd F, Komiti A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Australian and New Zealand Journal of Psychiatry. 2005;39:514–521. doi: 10.1080/j.1440-1614.2005.01612.x. [DOI] [PubMed] [Google Scholar]
- *.Yamaguchi S, Koike S, Watanabe K, Ando S. Development of a Japanese version of the Reported and Intended Behaviour Scale: Reliability and validity. Psychiatry and Clinical Neurosciences. 2014;68:448–455. doi: 10.1111/pcn.12151. [DOI] [PubMed] [Google Scholar]
- Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: Utilizing 'what matters most' to identify culture-specific aspects of stigma. International Journal of Epidemiology. 2014;43:494–510. doi: 10.1093/ije/dyu039. [DOI] [PubMed] [Google Scholar]
- Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: Adding moral experience to stigma theory. Social Science & Medicine. 2007;64:1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Reavley NJ, Jorm AF. Associations between stigma and help- seeking intentions and beliefs: findings from an Australian national survey of young people. Psychiatry Research. 2013;210:1154–1160. doi: 10.1016/j.psychres.2013.08.029. [DOI] [PubMed] [Google Scholar]
- Zeng QZ, He YL, Tian H, Miu JM, Yu WL, Wang XD. Development of stigma scale towards people with mental illness. Shanghai Archives of Psychiatry. 2009;21:217–220. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.