Abstract
This was a retrospective, observational chart review conducted on a convenience sample of 537 outpatients, aged 16–60 years, referred to an Italian Dietetic and Nutrition University Center. The study aimed to look at the association between a history of childhood obesity and dieting behaviors with development of eating disorders (EDs) at a later age. Subjects with a history of EDs (n = 118), assessed using both self-report and health records, were compared with those with no EDs (n = 419), who were attending the clinic mainly for primary prevention of metabolic and cardiovascular risk. Logistic regression analysis was performed to assess the association of childhood-onset obesity with development of an ED at a later age. Childhood-onset obesity, gender, maternal history of eating disorders, and dieting were associated with a positive history of EDs at a later age (p <.05). It is important to raise professional awareness of early symptoms of EDs in children with a history of obesity and treat them accordingly.
Childhood obesity is one of the major public health issues throughout the world. Its prevalence has reached epidemic proportions, with an increasingly younger age of onset. Preventing and managing childhood-onset obesity is one of the most important public health goals for both industrialized and developing countries (Howe, Firestone, Tilling, & Lawlor, 2015). It is well recognized that childhood obesity is a strong predictor of chronic diseases such as the metabolic syndrome, type 2 diabetes mellitus, hypertension, and other cardiovascular diseases (Cena et al., 2015; Howe et al., 2015), which contribute to a significant decrease in quality of life and life expectancy (Rendón-Macías, Rosas-Vargas, Villasís-Keever, & Pérez-García, 2014).
Previous research confirms that childhood obesity is likely to persist into adulthood, particularly when children are older at the time of evaluation, have severe obesity, or have a family history of obesity (Nadeau, Maahs, Daniels, & Eckel, 2011). However, inadequate attention is paid to the sub-sequent psychological impact of childhood obesity (Russell-Mayhew, McVey, Bardick, & Ireland, 2012). Modern society, in fact, perceives obesity as unattractive (Rees, Caird, Dickson, Vigurs, & Thomas, 2014), which strengthens the widespread opinion that slimness is necessary for success and respect. The media emphasizes thinness and often portrays those with obesity as having a lack of self-control and willpower. Children with obesity are often teased about their weight by peers or family members which decreases their self-esteem (Loth, Wall, Larson, & Neumark-Sztainer, 2010). Parents’ obesity-related behavior and their confidence and motivation to support behavioral change plays an important role in supporting children with obesity (Arsenault, Xu, Taveras, & Hacker, 2014).
There is increasing evidence that childhood-onset obesity is not only a risk factor for metabolic complications in adulthood, but also associated with an increased risk of developing eating disorders (EDs) during adolescence (Micali et al., 2015; Rancourt & McCullough, 2015; Sahoo et al., 2015; Sim, Lebow, & Billings, 2013; Villarejo et al., 2012). To assess this association and establish the temporal pattern of development of EDs, prospective longitudinal studies are necessary. However, so far, there are few prospective studies that have addressed this question. Recently, Berkowitz et al. (2016) conducted a prospective longitudinal study in Sweden on 51 individuals with adolescent-onset anorexia nervosa (AN), using a unique longitudinal dataset to investigate differences in early body weight or weight trajectories over time between individuals who later did or did not develop AN. The authors observed elevated premorbid body mass indexes (BMIs) during childhood in those who developed AN later in life, reporting on average a BMI that was 1.42 units higher than in age, sex and school matched healthy controls. Moreover, subjects who subsequently developed AN also showed higher childhood BMIs compared to population norms.
EDs are more common than type 2 diabetes in childhood and adolescence (Campbell & Peebles, 2014) and are associated with high morbidity and mortality; yet they continue to be underdiagnosed by pediatric professionals. There are many factors that contribute to the development of EDs, including perceived pressure for thinness, thin-ideal internalization, body dissatisfaction, and negative affect (Stice, Ng, & Shaw, 2010). Research also suggests that dietary restraint and weight stigma may constitute prodromal stages and be strong predictors for development of EDs (O’Hara, Tahboub-Schulte, & Thomas, 2016; Stice et al., 2010). During adolescence, when teenagers are the most vulnerable and often unprepared to deal with the physiological changes that accompany growth, attempts to lose weight may lead to an increased risk for eating pathology that is further reinforced by misuse of social media sites (Mabe, Forney, & Keel, 2014). Besides, findings from a 10-year longitudinal study indicate that disordered eating behaviors throughout adolescence set the stage for EDs among young adults (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). While there is great variability of dieting behaviors, most individuals with EDs acknowledge self-imposed diet attempts in the past (Stice et al., 2010). If these behaviors are not supervised and controlled, they may lead to negative emotions that increase the risk of binge eating and the use of inappropriate compensatory behaviors, which raises concerns of the impact of anti-obesity efforts in the pediatric population leading to eating disorders.
We anticipate that childhood obesity will be associated with development of ED at a later age based on previous research showing associations and overlapping presentations of EDs and childhood obesity (Micali et al., 2015; Rancourt & McCullough, 2015; Sahoo et al., 2015; Sim et al., 2013) and data which indicate that dieting and unhealthy weight control behaviors increase the risk for EDs (Stice, Gau, Rohde, & Shaw, 2017). To our knowledge, this is the first single Italian center study to investigate the association of a history of childhood-onset obesity and dieting with a history of EDs in adolescence and adulthood. This issue is of great interest to professionals engaged in prevention and treatment of childhood onset obesity and EDs (Neumark-Sztainer, 2016; Tanas, Caggese, & Marucci, 2015).
Method
Participants
The study population included 537 individuals attending the Dietetics and Clinical Nutrition outpatient Laboratory (DCNL) at the University of Pavia, between January 2013 and March 2015. This retrospective chart review (RCR) compared a group of patients with a history of EDs (n = 118), diagnosed using both self-report and medical records according to the criteria for diagnosis of EDs as defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013), with a group with no EDs (NED; n = 419). The NED group included anyone who did not have an ED, and received care and nutritional counselling at the outpatient clinic mainly for primary prevention of metabolic and cardiovascular risk. The prevalence of overweight and obesity in this group was around 60%. This RCR was performed on a convenience sample, a limitation of the study that we acknowledge in the Discussion section.
Since the DSM-5 was released in mid-2013 (APA, 2013), the diagnosis of all ED patients enrolled prior to this date has been reformulated according to the new DSM-5 criteria by three doctors (MDs) experienced in the diagnosis and treatment of EDs, who established consensus DSM-5 diagnoses by reviewing the medical records of the patients enrolled prior to the DSM-5 release. Each clinical record was reviewed independently by two out of three MDs. The revision was done carefully by examining all relevant information available in the case notes recorded by the interviewers at the time of diagnosis.
In order to improve reliability, besides their clinical experience and employing the same diagnostic criteria, the MDs were invited to use reference definitions and data derived from structured interviews as well as clinical records according to the DR.SED paradigm, which stands for diagnostic criteria, reference definitions, structuring the interview, clinical experience, and data (Aboraya, Rankin, France, El-Missiry & John, 2006).
We included patients of both sexes, aged 16–60 years, who had documentation of weight and height during puberty. We excluded patients with genetic pathologies (such as Prader-Willi Syndrome, Down syndrome, Achondroplasia, and Kabuki Syndrome) and intellectual disabilities.
Procedure
Prior to study initiation, we developed standardized data abstraction forms, explicit inclusion and exclusion criteria, and well-defined research questions. Once the study variables were defined, a single data abstractor was trained to identify pertinent information from patients’ records. Accurate record keeping was essential for the validity and reliability of the data. Data abstracted for the current study included birthdate, weight history, dieting attempts, family history of obesity, maternal history of EDs, educational level, and sports activity. We addressed intra-rater reliability by conducting a pilot test on 10% of a randomly selected sample by correlating multiple scores extracted by our data abstractor.
In our institution, clinical patients are routinely provided with a consent form at the time of their visit addressing privacy and confidentiality. Further all patients who consecutively attended the clinic between January 2013 and March 2015 were invited to sign a data use agreement that would allow the use of their medical records for research purposes. Ninety-two percent of patients authorized the use of their medical records for this purpose. The study was performed according to the Declaration of Helsinki, and institutional review board approval for the retrospective data collection was obtained per institutional guidelines.
Educational status
Educational level (EL) was dichotomized into lower (secondary education, levels 2 and 3 according to the International Standard Classification of Education [ISCED]) and higher EL (tertiary education: level 4, 5 and 6 according to ISCED) (UNESCO, 2012). In many education systems with compulsory education legislation, the end of lower secondary education coincides with the end of compulsory (general) education (levels 2 and 3). Post-secondary education (ISCED level 4) prepares individuals for both labor market entry as well as tertiary education, while tertiary education (ISCED levels 5–6) includes advanced vocational or professional education. For adolescents included in this analysis, we assessed their parents’ EL.
Weight history
Weight data were abstracted from the records. All subjects were weighed at their first visit to the clinic. The minimum and maximum weight in adult-hood as well as the weight trend in childhood was acquired from the medical records or growth charts. In the few patients who did not have past medical records, data were self-reported in real-time.
BMI during the pubertal years (between 9 and 12 years in females and 10–13 years in males) (Burgio, Martini, Nespoli, & Notarangelo, 2012) was calculated for all patients, and evaluated according to Cole and Lobstein’s (2012) cut-off point reference standards for BMI. Childhood overweight was defined as a BMI at or above the 85th percentile and below the 95th percentile while obesity is defined as a BMI at or above the 95th percentile for children and teens of the same age and sex, as reported by the Centers for Disease Control and Prevention (CDC, 2015), according to the Italian growth charts (Cacciari et al., 2006).
Dieting behavior
Dieting was defined as any intentional food intake change aimed at losing weight. Attempts to lose weight can be associated with behavioral changes such as alterations in eating habits and/or exercise frequency. There is consistency in defining self-induced emesis, and use of laxatives and diet pill use as unhealthy or extreme dieting (Canadian Pediatric Society, 2004), and as disordered eating if the behaviors were not sufficiently severe to warrant a diagnosis of an ED. We have categorized this kind of behavior into three main practices: dieting as nutritional therapy prescription, such as a weight-loss balanced diet; dieting as self-restriction; and dieting as self-restriction with inappropriate compensatory behaviors to avoid weight gain. To this end, the following questions that are asked as standard of care to screen for dieting or disordered eating behavior, were abstracted:
“Have you ever undergone a nutritional therapy prescription by nutrition professionals (physicians with residency in Nutrition, dieticians or nutritionists), during your adolescence?”
“Have you ever gone on a weight loss diet during your adolescence, without any professional support?”
“Have you ever used the following inappropriate compensatory behaviors in order to avoid weight gain (self-induced vomiting, use of laxatives, diuretics or other medications, fasting or excessive physical activity, smoking), during your adolescence?”
Eating disorders (ED) diagnosis
ED diagnosis reported in the charts was either abstracted from the patient’s medical records documentation or made at time of clinic intake by the multidisciplinary clinical team supervised by a psychologist and a senior MD with training in Clinical Nutrition and expertise in ED. Patient data are recorded in electronic medical records in our institution following the Subjective, Objective, Assessment, and Plan approach (Jacobs, 2009). Each patient routinely undergoes assessment of history, lifestyle and eating habits, dietary intake assessment, as well as a physical examination including anthropometric measurements and body composition analysis, and laboratory tests. DSM-5 standard criteria are used for the classification of EDs (APA, 2013). The records include the differential diagnosis and management plan, which are based on valid primary data and national or international guidelines.
Family history of obesity and maternal history of EDs
Positive family history of obesity (defined as at least one parent with obesity) as well as a maternal past history of eating disorders (MPHEDs), was abstracted from the patient’s medical records. In the few cases in which this information was lacking, specific questions were asked to the patients, or to his/her representative, during the family history recording. All mothers of minors were asked if they had ever experienced EDs (Micali et al., 2015).
Sports activity
Participation in sports was assessed as standard of care with the question “Have you ever practiced any sports activity during adolescence at a competitive level?” This question was included as part of a questionnaire on life-style, nutrition knowledge and habits, and was administered to all subjects (Turconi et al., 2003).
Statistical analysis
Data from this systematic sampling were prepared and analyzed using STATA version 11.1 MP (College Station, TX). Descriptive statistics are presented as means, standard deviations (SD) and percentages. Because we did not have sufficient sample size to perform a matched case-control study, we adjusted for sex, age, and educational level by including these variables in a multivariate logistic regression model. This was used to assess whether a history of childhood obesity was associated with a history of an ED after controlling for these possible confounders. Furthermore, multivariate logistic regression was used to determine whether obesity was a potential risk factor for EDs after controlling for other potential risk factors such as MPHEDs, dieting, sports activity, and EL.
Results
The characteristics of the study population as well as the Eating Disorders classification within the ED group are reported in Table 1. The convenience sample was divided into an ED group or NED group based on the presence or absence of a history of an ED, based on DSM-5 criteria (APA, 2013). The NED group included anyone without EDs receiving care and nutritional counselling at the outpatient clinic mainly for chronic metabolic and cardiovascular disease risk factors. The prevalence rate of overweight and obesity in this group was around 60%. The ED group was significantly younger than the NED group (p <.0001) with a higher prevalence of females (93% vs 74%) (Table 1).
Table 1.
Characteristics of the study population (n = 537) and classification of the ED group (n = 118), according to the diagnostic criteria in DSM 5.
| Number of participants (%) | Age (yrs) Mean ± SD | Males n | Females n | |
|---|---|---|---|---|
| TOTAL | 537 (100) | 40 ± 16.8 | 118 | 419 |
| NED | 419 (78) | 43.6 ± 16.4 | 110 | 309 |
| ED | 118 (22) | 26.9 ± 10.9 | 8 | 110 |
| ANr | 41 (34.7) | 22.0 ± 9.4 | 2 | 39 |
| ANp | 13 (11) | 24.8 ± 7.7 | 0 | 13 |
| BN | 7 (5.9) | 29.3 ± 8.2 | 1 | 6 |
| BNnp | 13 (11) | 28.5 ± 9.4 | 2 | 11 |
| BED | 19 (16.1) | 29.6 ± 11.1 | 1 | 18 |
| ARFID | 25 (21.2) | 32.5 ± 13.5 | 2 | 23 |
Note. Data are presented as number (n) and proportion (%) of participants or mean ± standard deviation (SD). ‘Age’ refers to age at the initial visit.
ED: Group with Eating Disorders; NED: Group with no Eating Disorders (control group).
ANr: Anorexia Nervosa restricting type; ANp: Anorexia Nervosa purging type; BN: Bulimia Nervosa; BNnp: Bulimia Nervosa non-purging type; BED: Binge Eating Disorder; ARFID: Avoidant/Restrictive Food Intake Disorder.
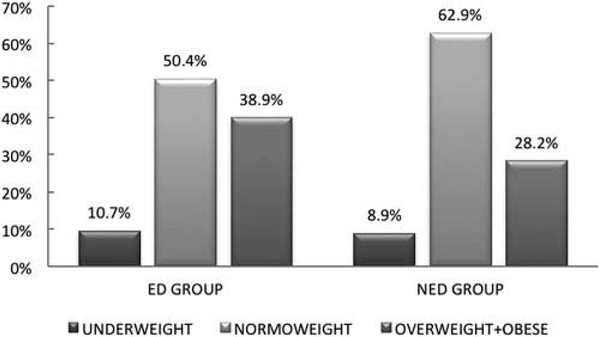
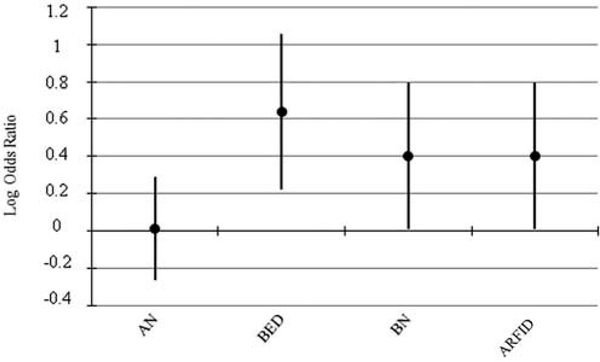
A positive history of childhood overweight and obesity, defined as the presence of overweight or obesity during puberty, was significantly higher in the ED group than in the NED group (38.9% vs. 28.2% of participants; p =.033) (Figure 1). Multivariate logistic regression showed that participants who reported childhood obesity had a two times higher odds of a positive history of ED (p =.017), compared with normal and underweight participants (Table 2). Particularly, the risk of developing binge eating disorder (BED) and bulimia nervosa (BN) later was respectively three times (p =.018) and 2.6 times (p =.031) higher, adjusting for sex and weight) (Figure 2).
Figure 1.
Weight status at pubertal age in ED and NED groups. Childhood obesity was defined as the presence of overweight or obesity at puberty and ages 9–12 years in females and 10–13 years in males (38.9% of participants in the ED group vs. 28.2% of participants in the NED group; p = 0.033, Chi square test analysis).</P/> ED: Eating disorders group; NED: Group with no eating disorders (comparison group).
Table 2.
Risk factors for eating disorders.
| Odds Ratio | 95% CI | p | |
|---|---|---|---|
| Females | 5 | 2.3–10.8 | <.001 |
| Childhood obesity | 1.7 | 1.1–2.8 | .017 |
| MPHEDs | 10.8 | 2–59.1 | .006 |
| Educational level (EL) | 1.7 | 1.1–2.6 | .026 |
| Competitive sports activity | 4 | 1.5–10.4 | .004 |
| Family history of obesity | 0.8 | 0.5–1.3 | .329 |
Note. Childhood obesity was defined as the presence of overweight or obesity at pubertal age and ages 9–12 years in females and 10–13 years in males.
Significance was defined at p <.05 (Multiple logistic regression analysis). MPHEDs: maternal positive history of eating disorders.
Figure 2.
Logistic regression for different eating disorders (ED). Log OR for a history of childhood obesity versus underweight/normal weight being associated with different EDs (along with 95% CI) are shown on a logarithmic scale. Reference categories for independent categorical variables are underweight/normal weight (log OR = 0). Childhood obesity was defined as the presence of overweight or obesity at puberty, ages 9–12 years in females and 10–13 years in males. AN: Anorexia Nervosa; BED: Binge Eating Disorder; BN: Bulimia Nervosa; ARFID: Avoidant/ Restrictive Food Intake Disorder.
Females and participants with MPHEDs had five times (p <.001) and 10 times (p =.006) higher odds of a positive history of ED respectively, compared to males and participants with a negative maternal history for EDs. Also, participants of a high EL had double the odds (p =.026) of developing an ED compared to those of a lower EL (Table 2). Further, we investigated the involvement of sports activity and its association with EDs, and found that participants who practiced sports at a competitive level during childhood had a four times higher odds ratio of later developing EDs (p =.004) compared to those who did not (Table 2). No significant association was found between family history of obesity and EDs.
With regard to dieting behaviors, we found a positive association between dieting and childhood obesity (p <.001). Sixty-seven percent (n = 356) of the sample had experienced dieting (Table 2) and the prevalence of EDs in dieters is reported in Table 3. Dieters had 3.3 times higher odds of a positive history of ED compared with non-dieters (OR = 3.3, p <.001, 95% C.I.: 1.9– 5.8). Among participants who had dieted and had a positive history of childhood overweight/obesity (n = 138), 32% (n = 44) had a positive history of EDs. Among dieters (n = 356), 33% (n = 119) and 67% (n = 237) respectively either self-restricted food intake or were prescribed nutritional therapy by nutrition professionals, respectively. Using sex-adjusted logistic regression, we found that those who had self-restricted their diet in the past had a higher odds of a positive history of ED (OR = 8.2; 95% C.I.: 4.8–14; p <.001), while simple dietary modifications or therapeutic diets prescribed by a professional appeared to be protective (OR = 0.2; 95% C.I.: 0.1–0.4; p <.001).
Table 3.
Prevalence of eating disorders in participants who had previously dieted.
| Males |
Females |
||||
|---|---|---|---|---|---|
| NED dev.°. n (%) | ED dev.° n (%) | NED dev.° n (%) | ED dev.° n (%) | Total n | |
| Normal weight | 33 (97.1)^ | 1 (2.9)^ | 111(71.6)§ | 44 (28.4)§ | 189 |
| Overweight | 24 (88.9)^ | 3 (11.1)^ | 70 (71.4)§ | 28 (28.6)§ | 125 |
| Obese | 0 (0)^ | 1 (100)^ | 0 (0)§ | 12 (100)*§ | 13 |
| Underweight | 0 (0)^ | 1 (100)^ | 20 (71.4)§ | 8 (28.6)§ | 29 |
| Total | 57 (90.5)^ | 6 (9.5)^^ | 201(68.6)§ | 92 (31.4)§§ | 356 |
Note. BMI was assessed at puberty (ages 9–12 years in females and 10–13 years in males).
° dev = development; ED: Eating Disorders; NED: no Eating Disorders.
refers to the proportion of males within any weight category sample for males (normal weight n = 34; overweight n = 27; obese n = 1; underweight n = 1), who did not or did develop an Eating Disorder (NED and ED respectively).
refers to the proportion of males within all weight categories taken together (n = 63) who did not or did develop an Eating Disorder (NED and ED respectively).
refers to the proportion of females within any weight category (normal weight n = 155; overweight n = 98; obese n = 12; underweight n = 28), who did not or did develop an Eating Disorder (NED and ED respectively).
refers to the proportion of females within all weight categories taken together (n = 293), who did not or did develop an Eating Disorder (NED and ED respectively).
p <.0001 (Chi square test analysis)
Finally, we analyzed the association between weight status during puberty and self-restriction with or without purging. Purging was assessed by self-report through questions asking how often participants made themselves sick, or used laxatives, diuretics or other medications to lose weight or avoid gaining weight. We found a significant association (p <.0001) between childhood obesity and self-restriction with purging.
Discussion
Our data show that childhood obesity was associated with the presence of EDs later in adolescence or adulthood in this sample of patients referred to the DCNL at the University of Pavia for nutritional and dietetic support. Consistent with previous research (Babio, Canals, Pietrobelli, Pérez, & Arija, 2009; Villarejo et al, 2012), we found a high prevalence of EDs (38.9%) in those with a history of childhood obesity, particularly BED (p =.018) and BN.
We also investigated the association between dieting and EDs and identified that 84% of participants with a positive history of childhood obesity (N = 138) had dieted before, and that in 32% (N = 44) there was a robust association with the development of ED at a later age. In fact, participants who had previously dieted were three times more likely to have a positive history of ED subsequently than those who had never dieted. In addition, we found that participants who followed self-restricted diets had eight times higher odds of a subsequent positive history of ED, compared to those who had been prescribed dietary modifications or therapeutic diets by a professional. This confirms previous findings in which assignment to a therapeutic diet by a professional did not worsen but rather improved eating pathology during the dieting intervention (Stice et al., 2010). These results suggest that earlier referral to an inter-professional team trained in behavior-change strategies for weight management could potentially be beneficial in teaching safe strategies to get to a healthier weight (Dietz et al., 2015).
In this study, we also found a strong association between MPHEDs and later EDs as already reported in previous research, suggesting a higher likelihood of developing EDs in the children with maternal EDs (Easter et al., 2013; Stein et al., 2006). Maternal ED may influence the offspring’s dietary patterns and macronutrient intake and be predictive of high levels of body dissatisfaction and weight and shape concern in girls and dieting in boys (Easter et al., 2013; Micali et al., 2015).
Gender is another important risk factor for EDs. Although evidence indicates that EDs are more common in females, the prevalence in males, especially younger males, may be underreported (Hepworth, 2010; Vo, Lau & Rubinstein, 2016). In our sample, the odds of having an ED was five times higher in females than in males, confirming previous research showing that women are more influenced by the emphasis of society on extreme thinness as the ideal of feminine beauty, as well as by family criticism regarding weight, shape, and eating behavior, with negative emotional consequences over time (Micali et al., 2015; Striegel-Moore & Bulik, 2007).
On exploring other “lifestyle” risk factors for EDs we found an association between competitive sports activity and development of ED at a later age. Those involved in competitive sports activity had three times higher odds of developing an ED, confirming that individuals involved in competitive sports may be vulnerable to pressure from trainers, peers, or friends regarding ideal body weight, and may modify their eating habits in order to improve performance (Joy, Kussman, & Nattiv, 2016). Data on specific sports performed were available only for a small portion of the sample and so are not discussed. It would have been important to define what specific sports activities the participants with EDs were engaged in to determine whether new sports activities should be added to the list of known “high-risk” sports for EDs (e.g., gymnastics, ice skating, dancing, swimming, track, wrestling) (Joy et al., 2016; Matzkin, Curry, & Whitlock, 2015).
Limitations
Data sets based on a RCR simulate reality but do have their limitations. Medical records are meant primarily for clinical practice rather than for research purposes. Also the sample considered for this RCR is a convenience sample; however, while this method presents limitations with respect to the generalizability of results, it is a practical method that allows researchers to use medical information at their disposal for research purposes (Vassar & Holzmann, 2013). Further, it is important to acknowledge that a positive history of eating disorders was assessed both via self-report and through medical records, and that the NED group is not a typical compassion group in that it includes individuals referred to our clinic for metabolic risk management. As we did not have sufficient sample size to conduct a matched case-control study, we adjusted for sex, age, and educational level by including them in the multiple logistic regression model. Although we had a large sample, the use of a clinical population within a specific geographic area may limit the extrapolation of the results to the greater population.
Conclusion
Despite the limitations acknowledged above, this is the first Italian study confirming the correlation between childhood obesity onset, self-restrictive diets, and development of ED at a later age. The prevalence of EDs and the delayed diagnosis suggest the need to increase awareness amongst clinicians who treat children and adolescents with overweight and obesity. It is important to emphasize that eating disordered behaviors should be evaluated not only in the presence of weight changes but also if behavioral changes are identified such as inappropriate eating habits, body image misperception or uneasiness, and lifestyle or social withdrawal (Sim et al., 2013). In addition, because general practitioners and pediatricians usually provide primary health care for teenagers in Italy, these results suggest the importance of setting up specific services for teenagers, and to seek to increase the evidence for country specific health policy making.
Acknowledgments
The authors would like to thank A. Passerini, registered dietitian, for her help with data collection, and Dr. L. Fiechtner for her guidance and support.
References
- Aboraya A, Rankin E, France C, El-Missiry A, & John C (2006). The reliability of psychiatric diagnosis revisited: The clinician’s guide to improve the reliability of psychiatric diagnosis. Psychiatry (Edgmont), 3(1), 41–50. [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Arsenault LN, Xu K, Taveras EM, & Hacker KA (2014). Parents’ obesity-related behavior and confidence to support behavioral change in their obese child: Data from the STAR study. Academic Pediatrics, 14(5), 456–462. doi:10.1016/j.acap.2014.03.001 [DOI] [PubMed] [Google Scholar]
- Babio N, Canals J, Pietrobelli A, Pérez S, & Arija V (2009). A two-phase population study: Relationships between overweight, body composition and risk of eating disorders. Nutrición Hospitalaria, 24(4), 485–491. [PubMed] [Google Scholar]
- Berkowitz SA, Witt AA, Gillberg C, Råstam M, Wentz E, & Lowe MR (2016). Childhood body mass index in adolescent-onset anorexia nervosa. International Journal of Eating Disorders, 49. doi:10.1002/eat.22584 [DOI] [PubMed] [Google Scholar]
- Burgio R, Martini A, Nespoli L, & Notarangelo LD (2012). Pediatria essenziale. Milano, Italia: Edi-ermes editore. [Google Scholar]
- Cacciari E, Milani S, Balsamo A, Spada E, Bona G, Cavallo L,…Cicognani A (2006). Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). Journal of Endocrinological Investigation, 29, 581–593. doi:10.1007/BF03344156 [DOI] [PubMed] [Google Scholar]
- Campbell K, & Peebles R (2014). Eating disorders in children and adolescents: State of the art review. Pediatrics, 134(3), 582–592. doi:10.1542/peds.2014-0194 [DOI] [PubMed] [Google Scholar]
- Canadian Paediatric Society. (2004). Dieting in adolescence. Position statement (AH 2004–01). Paediatrics & Child Health, 9(7), 487–491. Retrieved from http://www.cps.ca/en/documents/position/dieting-adolescence [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cena H, Fonte ML, Casali PM, Maffoni S, Roggi C, & Biino C (2015). Epicardial fat thickness: Threshold values and lifestyle association in male adolescents. Pediatric Obesity, 10(2), 105–111. doi:10.1111/ijpo.227 [DOI] [PubMed] [Google Scholar]
- Centers for Chronic Disease Prevention and Health Promotion (CDC). (2015). Defining childhood obesity. Retrieved from https://www.cdc.gov/obesity/childhood/defining.html
- Cole TJ, & Lobstein T (2012). Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatric Obesity, 7(4), 284–294. doi:10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed] [Google Scholar]
- Dietz WH, Baur LA, Hall K, Puhl RM, Taveras EM, Uauy R, & Kopelman P (2015). Management of obesity: Improvement of health-care training and systems for prevention and care. The Lancet, 385(9986), 2521–2533. doi:10.1016/S0140-6736(14)61748-7 [DOI] [PubMed] [Google Scholar]
- Easter A, Naumann U, Northstone K, Schmidt U, Treasure J, & Micali N (2013). A longitudinal investigation of nutrition and dietary patterns in children of mothers with eating disorders. The Journal of Pediatrics, 163(1), 173–178. doi:10.1016/j.jpeds.2012.11.092 [DOI] [PubMed] [Google Scholar]
- Hepworth K (2010). Eating disorders today–not just a girl thing. Journal of Christian Nursing: A Quarterly Publication of Nurses Christian Fellowship, 27(3), 236–241. doi:10.1097/CNJ.0b013e3181dd7976 [DOI] [PubMed] [Google Scholar]
- Howe LD, Firestone R, Tilling K, & Lawlor DA (2015). Trajectories and transitions in childhood and adolescent obesity In Burton-Jeangros C, Cullati S, Sacker A, & Blane D (Eds.), A life course perspective on health trajectories and transitions. Cham CH: Springer; Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK385368/ [PubMed] [Google Scholar]
- Jacobs L (2009). Interview with Lawrence Weed, MD—The father of the problem-oriented medical record looks ahead. The Permanente Journal, 13(3), 84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joy E., Kussma A., & Natti A. (2016). 2016 update on eating disorders in athletes: A comprehensive narrative review with a focus on clinical assessment and management. British Journal of Sports Medicine, 50(3), 154–162. doi:10.1136/bjsports-2015-095735 [DOI] [PubMed] [Google Scholar]
- Loth K, Wall M, Larson N, & Neumark-Sztainer D (2010). Disordered eating and psychological well-being in overweight and nonoverweight adolescents: Secular trends from 1999 to 2010. International Journal of Eating Disorders, 48(3), 323–327. doi:10.1002/eat.22382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabe AG, Forney KJ, & Keel PK (2014). Do you “like” my photo? Facebook use maintains eating disorder risk. International Journal of Eating Disorders, 47(5), 516–523. doi:10.1002/eat.v47.5 [DOI] [PubMed] [Google Scholar]
- Matzkin E, Curry EJ, & Whitlock K (2015). Female athlete triad: Past, present, and future. The Journal of the American Academy of Orthopaedic Surgeons, 23(7), 424–432. doi:10.5435/JAAOS-D-14-00168 [DOI] [PubMed] [Google Scholar]
- Micali N, De Stavola B, Ploubidis G, Simonoff E, Treasure J, & Field AE (2015). Adolescent eating disorder behaviours and cognitions: Gender-specific effects of child, maternal and family risk factors. The British Journal of Psychiatry: The Journal of Mental Science, 207(4), 320–327. doi:10.1192/bjp.bp.114.152371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeau KJ, Maahs DM, Daniels SR, & Eckel RH (2011). Childhood obesity and cardiovascular disease: Links and prevention strategies. Nature Reviews. Cardiology, 14(8), 513–525. doi:10.1038/nrcardio.2011.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D (2016). Eating disorders prevention: Looking backward, moving forward; Looking inward, moving outward. Eating Disorders, 24(1), 29–38. doi:10.1080/10640266.2015.1113825 [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, & Loth K (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association, 111(7), 1004–1011. doi:10.1016/j.jada.2011.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara L, Tahboub-Schulte S, & Thomas J (2016). Weight-related teasing and internalized weight stigma predict abnormal eating attitudes and behaviours in Emirati female university students. Appetite, 102, 44–50. doi:10.1016/j.appet.2016.01.019 [DOI] [PubMed] [Google Scholar]
- Rancourt D, & McCullough MB (2015). Overlap in eating disorders and obesity in adolescence. Current Diabetes Reports, 15(10), 78. doi:10.1007/s11892-015-0645-y [DOI] [PubMed] [Google Scholar]
- Rees RW, Caird J, Dickson K, Vigurs C, & Thomas J (2014). “It’s on your conscience all the time”: A systematic review of qualitative studies examining views on obesity among young people aged 12–18 years in the UK. BMJ Open, 4(4), e004404. doi:10.1136/bmjopen2013-004404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendón-Macías ME, Rosas-Vargas H, Villasís-Keever MA, & Pérez-García C (2014). Children’s perception on obesity and quality of life: A Mexican survey. BMC Pediatrics, 14 (1), 131. doi:10.1186/1471-2431-14-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell-Mayhew S, McVey G, Bardick A, & Ireland A (2012). Mental health, wellness, and childhood overweight/obesity. Journal of Obesity, 281–801. doi:10.1155/2012/281801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, & Bhadoria AS (2015). Childhood obesity: Causes and consequences. Journal of Family Medicine and Primary Care, 4(2), 187–192. doi:10.4103/2249-4863.154628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim LA, Lebow J, & Billings M (2013). Eating disorders in adolescents with a history of obesity. Pediatrics, 132(4), e1026–e1030. doi:10.1542/peds.2012-3940 [DOI] [PubMed] [Google Scholar]
- Stein A, Woolley H, Cooper S, Winterbottom J, Fairburn CG, & Cortina-Borja M (2006). Eating habits and attitudes among 10-year-old children of mothers with eating disorders: Longitudinal study. The British Journal of Psychiatry, 189, 324–329. doi:10.1192/bjp.bp.105.014316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Gau JM, Rohde P, & Shaw H (2017). Risk factors that predict future onset of each DSM–5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology, 126(1), 38–51. doi:10.1037/abn0000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Ng J, & Shaw H (2010). Risk factors and prodromal eating pathology. Journal of Child Psychology and Psychiatry, 51(4), 518–525. doi:10.1111/j.1469-7610.2010.02212.x [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, & Bulik CM (2007). Risk factors for eating disorders. The American Psychologist, 62(3), 181–198. doi:10.1037/0003-066X.62.3.181 [DOI] [PubMed] [Google Scholar]
- Tanas R, Caggese G, & Marucci S (2015). Future directions in prevention and treatment of children obesity and eating disorders. Italian Journal of Pediatrics, 41(S2), A72. doi:10.1186/1824-7288-41-S2-A72 [Google Scholar]
- Turconi G, Celsa M, Rezzani C, Biino G, Sartirana MA, & Roggi C (2003). Reliability of a dietary questionnaire on food habits, eating behaviour and nutritional knowledge of adolescents. European Journal of Clinical Nutrition, 57(6), 753–763. doi:10.1038/sj.ejcn.1601607 [DOI] [PubMed] [Google Scholar]
- UNESCO. (2012). International standard classification of education: ISCED 2011. Eds UNESCO institute for statistics. Retrieved from http://unesdoc.unesco.org/images/0021/002116/211619e.pdf
- Vassar M, & Holzmann M (2013). The retrospective chart review: Important methodological considerations. Journal of Educational Evaluation for Health Professions, 10, 12. doi:10.3352/jeehp.2013.10.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarejo C, Fernández-Aranda F, Jiménez-Murcia S, Peñas-Lledó E, Granero R, Penelo E,…Menchón JM (2012). Lifetime obesity in patients with eating disorders: Increasing prevalence, clinical and personality correlates. European Eating Disorders Review, 20(3), 250–254. doi:10.1002/erv.2166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vo M, Lau J, & Rubinstein M (2016). Eating disorders in adolescent and young adult males: Presenting characteristics. The Journal of Adolescent Health, 59(4) 397–400. doi:10.1016/j.jadohealth.2016.04.005 [DOI] [PubMed] [Google Scholar]