Abstract
Background:
The meaning of unconscious dreaming has been assigned varying degrees of historical significance throughout the ages and across different cultures including in major psychological theories of psychopathology. While dreams’ meaning and implications have remained controversial, not disputed is the occurrence of drinking/drug-using dreams (DDUD) when people enter recovery from a significant alcohol and other drug (AOD) problem. Typically taking the form of a relapse scenario followed by relief on awakening, such dreams can be profoundly unnerving. Beyond common anecdotal reports of these phenomena, however, very little is known about the prevalence, predictors, and decay of such dreams with time in recovery. Greater knowledge could help inform patients and providers about what to anticipate in recovery.
Method:
Nationally-representative cross-sectional study of US adults (N=39,093) who had resolved a significant AOD problem (weighted n=2,002). Measures: DDUD prevalence/time since last DDUD; demographics; measures of clinical history.
Results:
Approximately one third (31.9%) reported experiencing DDUD which were predicted by more severe clinical history variables (earlier age of onset; prior treatment/mutual-help participation). A significant linear decay of DDUD occurrence was observed with time in recovery.
Conclusions:
DDUD appear to occur among a substantial minority of US adults resolving significant AOD problems and are related to a more pronounced and deleterious AOD history. DDUD attenuate in frequency over time in recovery which plausibly may be indicative of increased biopsychosocial stability that reduces neurocognitive reverberation and psychological angst regarding relapse risk. Further prospective research is needed to understand the frequency, topography, content variability, and influence such dreams may have on intermediate (e.g., abstinence self-efficacy) and ultimate (substance use) outcomes.
Introduction
The phenomenology and meaning behind dreams and dreaming have a rich history in human cultures and civilizations. In psychology and psychiatry, more specifically, they have been a focus of much debate with varying degrees of psychological significance placed upon them. Ranging from Freud’s emphasis as dreams being the “royal road to the unconscious” allowing people to gain liberating, even curative, insights that are normally obscured by psychological defenses during waking hours (Freud, 1913), through biological psychiatry’s more straightforward neurochemical and neuro-psychological explanations (Hobson, 2009), dreams often arouse curiosity if not strong opinions and debate.
In the world of addiction and recovery from it, while there may be similar discussion regarding dreams’ meaning and impact, based on our clinical and clinical research experience there is little debate as to the phenomenology of the actual experience of having vivid drinking and drug-using dreams when people stop using substances and begin to enter remission and recovery. These often take the form intense portrayals of a relapse to their primary substance, with often simultaneous disbelief during the dream that a relapse has occurred, and which, on awakening, elicits initial intense fear, guilt, and remorse. This is followed by an immediate sense of relief once the individual realizes it has been merely a dream.
Modern neuroscientific study of dreaming reveals most dreams occur during rapid-eye movement (REM) or slow delta wave/stage 4 sleep (Louie & Wilson, 2001) and suggest dreaming reflects a process of memory consolidation, reorganization, and reprocessing of emotion laden content involving limbic and prefrontal brain regions (Hobson, 2009). This mind-brain process may reflect a psycho-biological interplay whereby memories are restructured in a process involving past experiences and biologically determined goals (Reiser, 2001). It is plausible, therefore, that during addiction recovery this memory recoding and reorganization during REM/slow-wave sleep may reflect a process of psychobiological deconditioning whereby the overlearned and automated processes involved in alcohol/drug consumption begin to be recoded and reorganized within an often lucid and intensely emotion-laden context, involving fear, anxiety, and remorse. This negatively valanced emotional intensity that is reported in drinking/drug-using relapse dreams gradually serves to deepen the disassociation between alcohol/drug use and functioning.
In our clinical work and related research experience, while these types of dreams are commonly experienced and often reported by people in treatment and recovery support service settings and anecdotal observations suggest these dreams become less frequent with more time in remission, little is known about the prevalence or natural history of these relapse dreams, which individuals in particular may be more likely to experience them (i.e., what demographic or clinical history factors predict their occurrence), and the rate at which they change in frequency and intensity when people enter recovery. Given the experience of these phenomena can be deeply unnerving among those in recovery and for their families, more information about these dreams and their natural history of decay could help inform treatment providers and those in or entering recovery about what to expect going forward in recovery.
To this end, using a national sample of U.S. adults who reported resolving a significant alcohol or other drug (AOD) problem (Kelly et al, 2017), this study examines 1. the overall prevalence of the experience of drinking/drug-using dreams in recovery, 2. investigates who, in particular, appears to experience such dreams (using demographic and clinical correlates of their occurrence) and, 3. documents their decay in occurrence with time in recovery.
2. Method
2.1. Procedure
The study sample was recruited using address-based sampling to randomly select individuals from 97% of U.S. households based on the U.S. Postal Service’s Delivery Sequence File. Eligible participants were individuals 18 years or older who answered yes to the screening question “Did you used to have a problem with drugs or alcohol, but no longer do?”. Of the 39,809 individuals selected for participation, 25,229 responded to the screening question (63.4%). In order to produce unbiased estimates of population parameters from these respondents, survey data were weighted according to nonresponse and to reflect the distribution of the U.S. adult, non-institutionalized population according to gender, age, race, education, geographic region, household income, home ownership and metropolitan area as determined by the Current Population Survey (CPS; U.S. Bureau of Labor Statistics, 2018). These weights were computed using the method of “iterative proportional fitting”, which is commonly referred to as “raking” (Battaglia, Hoaglin, & Frankel, 2009). More details are available elsewhere (e.g., Kelly, Greene, & Bergman, 2018; Kelly et al., 2017).
IRB Statement.
All study procedures were approved by the Partners HealthCare Institutional Review Board.
2.2. Measures
The survey was first piloted on 20 individuals over 3 days in July 2016 to estimate time to completion and address potential pitfalls in the survey. The official survey was administered over 19 days in July-August 2016. Non-responders to the screening question were sent e-mail reminders on days 3, 6, and 12 of the survey period.
Drinking/drug-using dreams.
Participants were asked if they’d ever had a drinking/drug using dream in recovery and if so, were asked how recently last dream occurred: 1) It has been so long I can’t remember; 2) More than 24 months ago; 3) 12–24 months ago; 4) 6–12 months ago; 5) 3–6 months ago; or 6) in the past 3 months.
Substance use history.
Participants answered a series of questions about 15 substances/classes of substances based on items from the Global Appraisal of Individual Needs (GAIN-I) (Dennis, Titus, White, Unsicker, & Hodkgins, 2002): 1) alcohol, 2) marijuana, 3) cocaine, 4) heroin, 5) narcotics other than heroin (e.g., pharmaceutical opioids), 6) methadone, 7) buprenorphine and its formulations (e.g., “suboxone”), 8) amphetamines (including methylenedioxymethamphetamine, or MDMA), 9) methamphetamine (“crystal meth”), 10) benzodiazepines, 11) barbiturates, 12) hallucinogens, 13) synthetic drugs (e.g., synthetic cannabinoid like “K2” and synthetic cathinones such as “bath salts”), 14) inhalants, and 15) steroids, as well as other (specified by participant). First, participants reported which of these substances they used 10 or more times in their life. Then for each substance endorsed, they provided information on the following: a) Age of first use; b) age of first regular use (i.e., at least once per week); c) whether the substance was a perceived problem for them (yes/no); d) whether they were still using the substance (yes/no); and e) if they were no longer using the substance, age at which they stopped using it. Finally, from the list of substances they deemed to be a problem, participants chose their primary substance (“drug of choice”).
Treatment and other recovery support services.
The questionnaire assessed history of participation in the following psychosocial treatment and recovery support services (Institute of Behavioral Research, 2002): 1) Inpatient or residential treatment; 2) outpatient addiction treatment; and 3) mutual-help organizations (MHOs). We assessed for lifetime attendance to help with their AOD problem at 11 different 12-step and non-12-step MHOs, with an “other” option specified by participant (Kelly, Myers, & Brown, 2011): 1) Alcoholics Anonymous (AA); 2) Narcotics Anonymous (NA); 3) Marijuana Anonymous; 4) Cocaine Anonymous; 5) Crystal Methamphetamine Anonymous; 6) SMART Recovery; 7) LifeRing Secular Recovery; 8) Moderation Management; 9) Celebrate Recovery; 10) Women for Sobriety; and 11) Secular Organization for Sobriety (S.O.S.). For each MHO attended, participants reported a) whether they ever attended and, if so, whether they had attended in the past 90-days.
Recovery history.
Participants reported whether they currently consider themselves to be “in recovery” (yes/no). If not, they reported whether they ever considered themselves to be “in recovery” (yes/no).
2.3. Analytic Plan.
We calculated the prevalence of drinking or drug using dreams after AOD problem resolution and how recently these dreams had occurred. We then examined correlates of any and recent drug using dreams using multinomial regression controlling for years since AOD problem resolution. Correlates included age, sex, race/ethnicity, number of substances used 10 or more times, age of onset (primary substance), years since AOD problem resolution, primary substance, inpatient treatment history, outpatient treatment history, mutual help attendance (any and 12-step), and whether the participant currently or has ever considered themselves to be in recovery. To examine the association between time in recovery and recency of dreams we calculated a Spearman rank correlation coefficient describing the relationship between years since AOD problem resolution and time since most recent drinking or drug using dream (6 categories described in 2.2 Measures). This relationship was displayed visually using a locally weighted scatterplot and smoothing (LOWESS) plot. We then compared the median years since problem resolution in each dreams recency group and calculated the relative risk of more distal drug using dreams with increased years since AOD problem resolution. For this analysis we recoded the variable describing recency of drinking or drug using dreams into the following categories: 1) more than 24 months; 2) 3–24 months; or 3) less than 3 months, and examined the distribution of drinking or drug using dream recency among people who have reported having these dreams since AOD problem resolution. We included the response “it’s been so long I can’t remember” in the more than 2 years ago recency group. To account for potential biases in assessing recency of drinking/drug-using dreams among people with limited time since AOD problem resolution, we replicated the analyses in a sample restricted to individuals with three or more years since problem resolution to assess the robustness of the results. Three years was selected given that it makes it possible for all participants to be able to report a potential drinking/drug-using dream that occurred over two years ago, which was the largest numerical category included in the recency variable. All models incorporated survey weights and were conducted in Stata, version 14 (StataCorp, 2015).
3. Results
3.1. Prevalence of drinking and drug using dreams after AOD problem resolution
Of the 2,002 participants resolving a significant AOD problem, 1,994 provided information on whether they had experienced a drinking or drug using dream since AOD problem resolution. In this sample, 31.9% reported experiencing a drinking or drug using dream since AOD problem resolution. Almost ten percent (9.6%) reported experiencing a drinking or drug using dream so long ago that they can’t remember. The remainder of the sample reported experiencing their most recent drinking or drug using dream more than two years ago (3.9%), one to two years ago (4.5%), six to twelve months ago (3.6%), three to six months ago (2.2%) or in the past three months (8.1%; Table 1).
Table 1.
Prevalence of drinking and drug using dreams since AOD problem resolution
| Drinking/drug using dreams since AOD problem resolution | |
|---|---|
| % | |
| No | 68.09 |
| Yes, but been so long I can’t remember | 9.56 |
| Yes, more than 2 years ago | 3.91 |
| Yes, 1–2 years ago | 4.49 |
| Yes, 6–12 months ago | 3.57 |
| Yes, 3–6 months ago | 2.24 |
| Yes, in the past 3 months | 8.14 |
3.2. Correlates of drinking and drug using dreams (Table 2)
Table 2.
Correlates of drinking and drug using dreams controlling for years since AOD problem resolution
| Recency | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Ever (vs. Never) | More than 24 months ago (vs. past 3-months) |
3–24 months (vs. past 3-months) |
|||||||||
| RR | SE | t | p | RR | SE | t | p | RR | SE | t | p | |
| Age (in years) | 0.99 | 0.01 | −1.64 | 0.101 | 0.98 | 0.01 | −1.63 | 0.105 | 1.00 | 0.01 | −0.44 | 0.661 |
| Male | 0.86 | 0.12 | −1.09 | 0.274 | 1.36 | 0.43 | 0.98 | 0.326 | 0.61 | 0.20 | −1.54 | 0.125 |
| Race/Ethnicity (ref=White) | ||||||||||||
| Black, non-Hispanic | 0.99 | 0.23 | −0.03 | 0.973 | 1.38 | 0.66 | 0.67 | 0.504 | 1.67 | 0.78 | 1.10 | 0.270 |
| Other, non-Hispanic | 2.02 | 0.71 | 2.02 | 0.043 | 1.05 | 0.70 | 0.08 | 0.936 | 0.81 | 0.57 | −0.30 | 0.761 |
| Hispanic | 0.83 | 0.19 | −0.80 | 0.421 | 1.67 | 0.80 | 1.08 | 0.282 | 1.07 | 0.55 | 0.13 | 0.894 |
| Multiracial | 1.56 | 0.63 | 1.11 | 0.269 | 5.14 | 5.69 | 1.48 | 0.140 | 5.49 | 6.48 | 1.44 | 0.149 |
| Number of substances used | 1.17 | 0.03 | 5.89 | 0.000 | 1.02 | 0.05 | 0.47 | 0.642 | 1.00 | 0.05 | −0.08 | 0.933 |
| Age of onset (primary substance) | 0.98 | 0.01 | −1.68 | 0.093 | 0.95 | 0.02 | −2.21 | 0.028 | 0.99 | 0.02 | −0.51 | 0.609 |
| Years since AOD problem resolution1 | 0.98 | 0.01 | −3.66 | 0.000 | 1.12 | 0.03 | 4.55 | 0.000 | 1.05 | 0.03 | 2.03 | 0.042 |
| Primary substance (ref=Cannabis) | ||||||||||||
| Alcohol | 0.64 | 0.16 | −1.75 | 0.080 | 1.40 | 0.70 | 0.67 | 0.500 | 0.73 | 0.39 | −0.60 | 0.548 |
| Other Drug | 1.27 | 0.34 | 0.88 | 0.378 | 1.10 | 0.58 | 0.17 | 0.862 | 0.90 | 0.50 | −0.19 | 0.851 |
| Inpatient treatment | 2.99 | 0.52 | 6.25 | 0.000 | 0.84 | 0.30 | −0.50 | 0.618 | 1.09 | 0.36 | 0.26 | 0.795 |
| Outpatient treatment | 3.03 | 0.54 | 6.18 | 0.000 | 0.83 | 0.28 | −0.56 | 0.575 | 0.62 | 0.21 | −1.40 | 0.163 |
| Mutual Help Attendance (ref=Never) | ||||||||||||
| Former | 2.54 | 0.42 | 5.63 | 0.000 | 0.82 | 0.31 | −0.53 | 0.594 | 0.79 | 0.30 | −0.62 | 0.535 |
| Past 3-Mo | 8.39 | 2.02 | 8.85 | 0.000 | 0.86 | 0.35 | −0.38 | 0.704 | 0.92 | 0.38 | −0.21 | 0.836 |
| 12-Step Mutual Help Attendance (ref=Never) | ||||||||||||
| Former | 2.42 | 0.39 | 5.42 | 0.000 | 0.75 | 0.28 | −0.78 | 0.436 | 0.75 | 0.28 | −0.78 | 0.438 |
| Past 3-Mo | 9.35 | 2.48 | 8.45 | 0.000 | 0.79 | 0.33 | −0.58 | 0.563 | 0.80 | 0.34 | −0.54 | 0.591 |
| Do you consider yourself to be in recovery? (ref=No) | ||||||||||||
| Yes | 2.46 | 0.36 | 6.13 | 0.000 | 0.96 | 0.31 | −0.11 | 0.911 | 1.22 | 0.40 | 0.60 | 0.550 |
| Did you ever consider yourself to be in recovery? (ref=No) | ||||||||||||
| Yes | 1.90 | 0.43 | 2.82 | 0.005 | 0.69 | 0.37 | −0.68 | 0.497 | 1.56 | 0.80 | 0.86 | 0.392 |
Bivariate association between years since problem resolution and drinking/drug-using outcomes
Participant report of experiencing a drinking or drug using dream after AOD problem resolution was more likely with an increasing number of substances used 10 or more times (RR=1.17, SE=003, p<.001), among non-Hispanics reporting a race other than White or Black (ref=White, non-Hispanic, RR=2.02, SE=0.71, p=0.043), among individuals who reported inpatient treatment (RR=2.99, SE=0.52, p<.001), outpatient treatment (RR=3.03, SE=0.54, p<.001), previous MHO attendance (RR=2.54, SE=0.42, p<.001), past 3-month MHO attendance (RR=8.39, SE=2.02, p<.001), previous 12-step MHO attendance (RR=2.42, SE=0.39, p<.001), past 3-month 12-step MHO attendance (RR=9.35, SE=2.48, p<.001), individuals who currently consider themselves to be in recovery (RR=2.46, SE=0.36, p<.001), and individuals who have ever considered themselves to be in recovery (RR=1.90, SE=0.43, p=0.005). Current age, sex, age of AOD onset and primary substance were not significantly associated with the probability of experiencing drinking or drug using dreams.
With regard to recency of drinking or drug using dreams among individuals who reported experiencing drinking or drug using dreams after AOD problem resolution, age of onset was associated with more recent drinking and drug using dreams. More specifically, older age of onset was associated with a lower probability of experiencing a drinking or drug using dream over two years ago relative to in the past 3-months controlling for years since problem resolution (RR=0.95, SE=0.02, p=0.028); however there was no difference in whether someone experienced their last drinking or drug using dream in the past 3–24 or less than 3-months by age of onset. Other correlates assessing demographics, substance use history, treatment and recovery service utilization and whether one considers themselves to currently or have ever been in recovery were not associated with recency of drinking or drug using dreams among those that reported having these dreams since AOD problem resolution.
3.3. Association between time in recovery and recency of drinking or drug using dreams
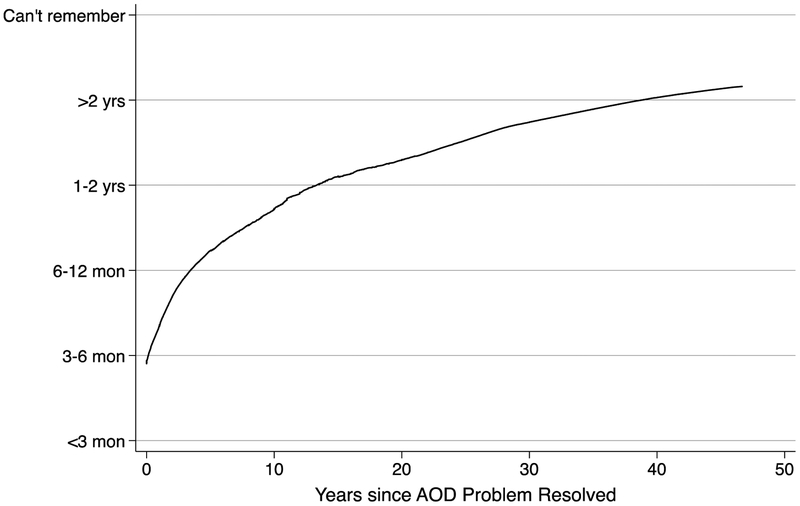
Additional time since AOD problem resolution was associated with significantly more distal drinking and drug using dreams (r=−0.399, p<0.001; Figure 1). More specifically, each additional year of problem resolution was associated with a 5% increase in the probability that the most recent dream occurred 3–24 months ago (vs. less than 3-months, p=0.042), and a 12% increase in the probability that the most recent dream occurred over two years ago (vs. less than 3-months, p=0.000). Median years since AOD problem resolution was greatest for individuals whose last drinking or drug using dream was over 2 years ago (Median=11 years, IQR = 6.0–20.0) and shorter for individuals whose last drinking or drug using dream was 3–24 months (Median=6.6 years, IQR=2.3–12.8) or less than 3 months ago (Median=2.3 years, IQR=1.0–9.0).
Figure 1a.
Association between time in recovery and time since most recent drinking/drug-using dreams (full sample)
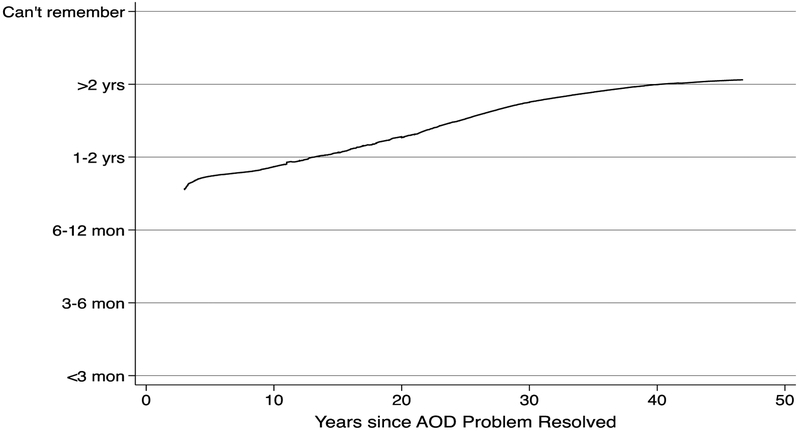
3.4. Sensitivity Analyses
The analyses reported in sections 3.2 and 3.3 were replicated in a sample restricted to participants with three or more years since problem resolution. As shown in Figure 2, the Spearman rank order correlation describing the relationship between recency of drinking/drug-using dreams and years since AOD problem resolution was attenuated, but remained significant (r=−0.21, p=0.002). Analysis of correlates of whether participants reported having drinking/drug-using dreams after AOD problem resolution and, if so, how recently these occurred displayed similar patterns in this subsample as what were reported in the full sample, suggesting that these analyses are perhaps robust to possible immortal time biases that could qualitatively modify the inferences reported above.
4. Discussion
Anecdotally, having “drinking/drug-using dreams” are common experiences among individuals in recovery who have suffered significant alcohol or other drug problems. These experiences are often highly unsettling among those experiencing them with the content of the dream following the common scenario of a return to substance use/relapse. Of note, these dreams occur while individuals are otherwise in the midst of concerted conscious efforts to stay abstinent and may have many months or even years of continuous remission. Despite the perceived commonality of this phenomenon, little was known from an empirical standpoint regarding the prevalence and correlates of their occurrence, and whether and when these unsettling dream experiences begin to diminish. In this nationally-representative sample of individuals resolving a significant drug or alcohol problem, approximately one third reported ever having experienced such a dream, and participants that did, were those with more severe substance use histories as evidenced by a greater variety and intensity of substances used and greater use of treatment and recovery support services. As anticipated, a significant linear decay in the prevalence of the occurrence of these dreams was also observed with greater time in recovery associated with increasing time since the last such experience.
While reports of these dream phenomena are commonly heard in clinical and recovery support services settings, of note was the finding here that the majority of individuals in this sample never experienced such dreams. This is perhaps reflective of the breadth of the sample in this study as it included the population of individuals in the US who subjectively self-defined once having a drug or alcohol problem and no longer doing so and did not include solely the more severe objectively defined clinical cases, as we have found in prior analyses (Kelly, Abry, Milligan, Bergman, & Hoeppner, 2018; Kelly et al., 2017). This notion is supported by the finding that the major correlates of the drinking/drug using dream experience reflected greater alcohol/drug involvement and impairment, and treatment and recovery support service use. Another potential reason why DDUD may seem like a more common phenomenon than we found here, is because these tend to happen more frequently in early recovery, and despite recognition that addiction tends to be a chronic disorder requiring ongoing disease management and recovery monitoring for several years to ensure stable remission (Kelly and White, 2011), this is the only time when most treatment professionals encounter those in recovery. Consequently, this may produce a biased, inflated, prevalence estimate (commonly known as Berkson’s Bias(Westreich, D. (2012).
Also noteworthy was the finding of the decay in the recency of these dreams with longer time in recovery. In the early months and years of recovery, prodigious deconditioning processes and neuronal re-calibrations occur in the brain that reflect abstinence-based neuroadaptations (Buhler & Mann, 2011; Niciu & Mason, 2014) and these rearrangements may create reverberations for some time. Although anecdotal, and this study did not systematically gather information on the exact nature and content of experienced drinking/drug-using dreams, the common theme of these dreams are striking in that they invariably are comprised of a vivid relapse scenario, which on awakening is met with great relief that it was only a dream. It has been postulated that dreams in REM sleep provide a virtual reality model of the world that may be of functional use to the development and maintenance of waking consciousness (Hobson, 2009). In other words, there may be an adaptive function to drinking-drug using dreams that help bolster motivation and heighten vigilance against relapse. The adaptive and functional need for drinking-drug using dreams thus would be expected to decay over time with greater biopsychosocial stabilization and greater psycho-emotional and functional stabilization appears to occur with greater remission lengths (Kelly et al., 2018).
Indeed, these dreams have not been observed to be associated with relapse risk; rather, they are often met with great relief and are not reported as increasing desire to re-engage with substances - in fact quite the opposite. Nevertheless, from an empirical standpoint, the effect of experiencing such dreams on intermediate variables (e.g., abstinence self-efficacy) or ultimate, substance use/relapse, variables is not currently formally understood.
4.1. Limitations
There are several limitations inherent in the design and scope of this study which should be considered when interpreting and making generalizations from these findings. First, this is a cross-sectional study and while longitudinal inferences may be insinuated it is important to confirm cross-sectional findings with future prospective studies. Furthermore, the measurement of the drinking/drug-using dream experiences was limited and the ordinal categorization of the variable measuring time since experiencing DDUD is limited and not ideal. These limitations prevented the application of a time-to-event analysis that could protect against immortal time bias, which could explain, in part, the relationship between time in recovery and time since last drinking/drug-using dream. To begin to account for this, we controlled for years since AOD problem resolution in all models. Furthermore, although our study is highly likely to contain many individuals with formal alcohol or other drug use disorder diagnoses (since many attended treatment and such diagnoses are typically required to justify treatment entry), we did not formally conduct such diagnostic assessments ourselves, thus the relationship between such diagnoses and the occurrence DDUD is unknown but should be investigated. Future research also should examine the DDUD construct in more detail, including the actual nature, temporal topography, and content of such dreams, and the impact that such dreams may have on individuals experiencing them including future relapse risk.
4.2. Conclusion
Very little is known from an epidemiological or phenomenological standpoint about the prevalence, correlates, and natural history of drinking/drug-using dreams among people in recovery from significant alcohol/drug problems. This study suggests that in the broad population of individuals who report resolving a significant alcohol/drug problem, about one third will report occurrence of at least one drinking/drug-using dream, and these individuals appear to be those who have accessed help from treatment and mutual-help organizations, possibly reflecting a more serious clinical course of the disorder and its impact on the central nervous system. Also, the observed association between decreased incidence of DDUD and longer time in recovery suggests a psycho-biological interrelationship whereby increasing psychosocial stability and neuroplastic adaptations to abstinence and a recovery lifestyle may be helping to diminish psychological angst about relapse. Future research should examine these phenomena prospectively. Future research should examine also the variability in the frequency, topography, and content of such dreams and how such dreams may be related to the experience of normalization of sleep patterns and REM/slow delta wave sleep in particular.
Figure 1b.
Association between time in recovery and time since most recent drinking/drug-using dreams (sensitivity analysis restricted to participants with 3 or more years since AOD problem resolution)
JSAT Highlights.
Anecdotally drinking and drug-using dreams are perceived as common occurrences among people entering recovery from significant alcohol/drug problems, but little is known about their actual prevalence or phenomenology
This study found that about one third of U.S. adults resolving a significant alcohol/drug problem report having had drinking/drug using dreams after stopping substance use
Drinking/drug-using dreams appear to occur among those more seriously impacted by alcohol/drug use.
Significant declines in drinking/drug-using dreams occur with greater time in recovery
Acknowledgments
Funding: JFK is supported by K24AA022136; MCG is supported by the National Institute on Drug Abuse (T32DA007292). This study was funded by an anonymous donation to the MGH Recovery Research Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Battaglia MP, Hoaglin DC, & Frankel MR (2009). Practical Considerations in Raking Survey Data. Survey Practice, 2(5), 1–10. [Google Scholar]
- Buhler M, & Mann K (2011). Alcohol and the human brain: a systematic review of different neuroimaging methods. Alcoholism: Clinical and Experimental Research, 35(10), 1771–1793. doi:10.1111/j.1530-0277.2011.01540.x [DOI] [PubMed] [Google Scholar]
- Dennis M, Titus J, White M, Unsicker J, & Hodkgins D (2002). Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures Retrieved from www.chestnut.org/li/gain/gadm1299.pdf
- Freud S (1913). The Interpretation of Dreams (Third ed.). New York: The Macmillan Company. [Google Scholar]
- Hobson JA (2009). REM sleep and dreaming: towards a theory of protoconsciousness. Nature Reviews. Neuroscience, 10(11), 803–813. doi:10.1038/nrn2716 [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research. (2002). TCU Comprehensive Intake (TCU CI). Fort Worth: Texas Christian University, Institute of Behavioral Research; Available at ibr.tcu.edu. [Google Scholar]
- Kelly JF, Abry AW, Milligan CM, Bergman BG, & Hoeppner BB (2018). On being “in recovery”: A national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychology of Addictive Behaviors. http://dx.doi.org/10.1037/adb0000386 [DOI] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2018). Beyond Abstinence: Changes in Indices of Quality of Life with Time in Recovery in a Nationally Representative Sample of U.S. Adults. Alcoholism: Clinical and Experimental Research 42(4), 770–780. doi:10.1111/acer.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JFB, Bergman BG, Hoeppner B, Vilsaint CL, White WL (2017). Recovery from substance use disorder in the United States: Prevalence, characteristics, and pathways from the first national probability-based sample. Drug Alc Dep, December 1;181:162–169. doi: 10.1016/j.drugalcdep.2017.09.028. [Google Scholar]
- Kelly JF, Urbanoski KA, Hoeppner BB, Slaymaker V (2011). Facilitating comprehensive assessment of 12-step experiences: A Multidimensional Measure of Mutual-Help Activity. Alcoholism Treatment Quarterly, January 1;29(3):181–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, White WL (2011) Addiction Recovery Management: Theory, Research, and Practice, Springer Science, Human Press, New York, NY. [Google Scholar]
- Louie K, & Wilson MA (2001). Temporally structured replay of awake hippocampal ensemble activity during rapid eye movement sleep. Neuron, 29(1), 145–156. [DOI] [PubMed] [Google Scholar]
- Niciu MJ, & Mason GF (2014). Neuroimaging in Alcohol and Drug Dependence. Curr Behav Neurosci Rep, 1(1), 45–54. doi:10.1007/s40473-013-0005-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiser MF (2001). The dream in contemporary psychiatry. American Journal of Psychiatry, 158(3), 351–359. doi:10.1176/appi.ajp.158.3.351 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- U.S. Bureau of Labor Statistics (2018). Labor force statistics from the current population survey. United States Deparmtent of Labor; www.bls.gov/cps, Washington, DC. [Google Scholar]
- Westreich D (2012). Berkson’s bias, selection bias, and missing data. Epidemiology (Cambridge, Mass.), 23(1), 159–164. http://doi.org/10.1097/EDE.0b013e31823b6296 [DOI] [PMC free article] [PubMed] [Google Scholar]