Abstract
Objective
To analyse the increase of self-referral patients at the Emergency Department of Riotinto District Hospital (in Huelva, Spain) during a short period. The study focused on patients’ profiles to identify key factors that explained the increase of self-referrals.
Material and methods
Retrospective descriptive study using patient’s data from a hospital emergency department between 2003–2015, excluding the period 2012–14 due to the lack of records. Socio-demographic variables, type of referral, access to health services, hospital route, transfer time and organisational changes were analysed, among other factors. Descriptive statistics, chi-square test, and binary logistic regression analysis were used.
Results
Self-referral patients to the hospital emergency department revealed a growing trend. Logistic regression model showed that the variables that best predict its occurrence were the health system changes from 2008 and the time it takes to get to the Extra-hospital Emergency Services, where those changes act as modifiers of the effect. From 2008, the likelihood of self-referral in towns with an Extra-hospital Emergency Service over 2 minutes away by car was of 76.43%. When including the triage level, the logistic regression model showed that 83.1% of patients referred themselves.
Conclusions
Changes in the health system and in the time for patients to get to the reference hospital from their origin, affect the likelihood of self-referral to the emergency department. Once the patient's severity level was included, this variable, along with the time to get to the emergency department, modified the probability of self-referral to the emergency department. We found an increase in hospital services together with a reduction of resources in the primary care emergency system. This may have led to inefficiencies in the public health system, together with an increase in self-referrals and greater problems to service users.
Introduction
Patients who attend the Emergency Department (ED) by their own initiative, without being referred by any health professional or institution, are known as self-referral patients [1]. According to the literature, this is one of the causes for the improper use of services [2] which results in ED overcrowding [3]. Factors influencing self-referral include socio-cultural and organisational changes [4], age, sex, socioeconomic status, accessibility to primary care, doctor-patient relationship, geographical area, and health condition or severity of the episode [5]. As Brezzi et al. stated, self-referral is increasing in developed countries and is attributed to different causes such as lack of accessibility or lack of trust in other levels of care, perceived severity, etc. [6].
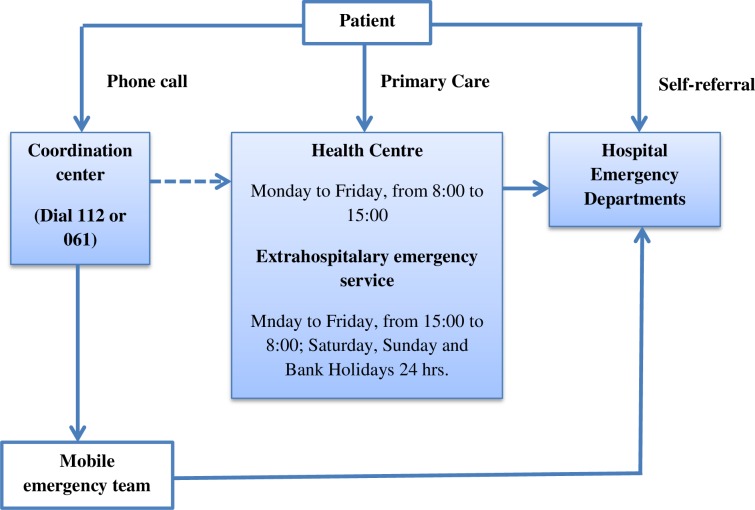
The Spanish National Health System is built on public founding, full coverage, free and equal accessibility and almost full benefits. It has three levels of care provision to respond to emergency situations: primary health care centres, Extra-hospital Emergency Services (EHES) and hospital ED, and a coordination centre that responds to telephone consultations. Individuals have different ways to request and receive health care in emergency situations. Fig 1 shows a diagram of these routes. In Spain, self-referral is the most frequent form of attendance to ED, representing 75.4% of the cases [7].
Fig 1. The Spanish National Health System levels of care provision to respond to emergency situations.
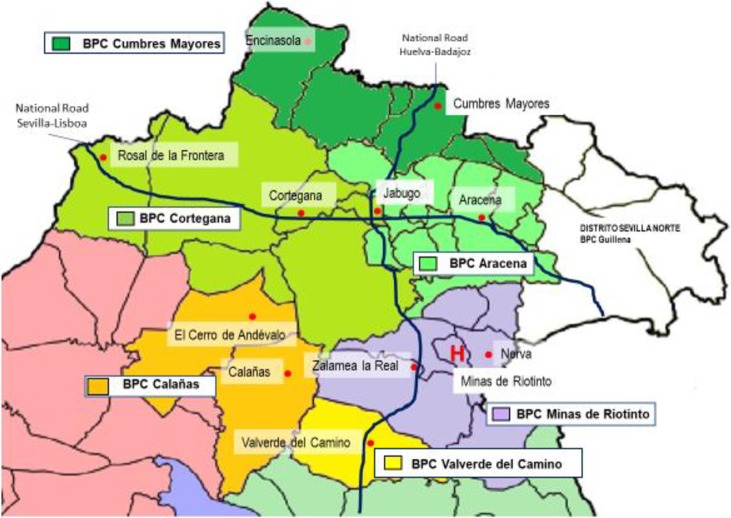
The Northern Huelva Health Area is a predominantly rural and remote region, with over 50% of the population living in rural municipalities of less than 10,000 inhabitants. The area is mostly mountainous, has 3,707 km2 and a population of 69,921 inhabitants. The population density is low (18.6 inhabitants / km2). As a consequence, communications are difficult, which means that more than half of the population needs more than 45 minutes to reach the nearest city [7]. Northern Huelva Health Area has six basic primary care areas and 11 EHES with mobile equipment for urgent care. Specialised assistance, including urgent and critical care, is provided at the Riotinto Hospital [7]. Fig 2 shows the location of the different resources of the Northern Huelva Health Area.
Fig 2. Location of the Basic Primary Care Areas, Extra-hospital Emergency Services and Riotinto Hospital.
The increase of self-referral patients in the Riotinto Hospital ED, from 24.28% (5261) in 2003 up to 70.20% (17912) in 2011 and 62.63% (16915) in 2015, led us to investigate the factors that were involved in these changes.
As a hospital located in a rural area, as described above, ED receives patients referred predominantly from primary care centres. However, during the period of this study, self-referrals reached similar percentages similar to national figures.
During the period referred in this study, the organisational and functional structure of Northern Huelva Health Area had an unequal distribution of quotas for primary care level. The general practitioner/health centre ratio was 1.02, with only one doctor in 9 out of the 11 EHES and in the 18 health centres. These doctors were responsible for a high demand work of around 1,450 emergencies per 1,000 inhabitants in the EHES. There was also a shortage of paediatricians in the health centres, which affected their normal activity. Furthermore, critical care transport equipment was not available in the area.
Between 2006 and 2009, there was a public employment and transfer tender that involved the dismissal of 29 of the 61 medical general practitioners. From the structural point of view, there were two important events: cessation of the afternoon activity in three health centres (2009), and closing of the Minas de Riotinto EHES, without an increase in the resources of those centres to cope with the demand (2008).
Aim of the study
The aim of this study is to assess the possible factors that have contributed to the increase of self-referral patients at Riotinto Hospital Emergency Department.
Material and methods
Design and sample
This study followed a retrospective observational design. A total of 242,475 patients that referred themselves to the Riotinto Hospital ED were included. Out of them, 215,639 patients were assisted between January 2003 and December 2011, and 26,869 patients were assisted during 2015. Although it was recorded, the data from 2012 to 2014 was excluded due to an error on the registration programme and its codification. During this period, item “self-referral” was renamed as “transport by own means”, including every patient who was not transferred by an arranged ambulance, even in those cases where they were referred by a general practitioner. Patients were recorded and classified according to the mean of transport instead of type of referral. So, the research team decided to exclude information from 2012–2014 as it could confound results and conclusions. In 2015, the item “transport by own means” was renamed “self-referral” again.
The manuscript has been checked using the STROBE Statement for observational studies.
Variables
Socio-demographic variables (sex, age, origin) were analysed, as well as type of referral (self-referral or referred), the hospital route, transfer time (higher or lower than the median value), availability of the EHES in town, access to daily general practitioners (GP) consultation, triage (only in data form 2015), destination (admission or discharge) and period (due to organisational changes occurred in 2008). Regarding the hospital route, there was a difference between the patients who lived in a town with EHES (or on their way to the hospital), and patients who lived in a location with the same distance from EHES and from the hospital.
Instruments and analysis
Descriptive study by distribution of frequencies and percentages. The chi-square test, along with the odd ratios (OR) and associated confidence intervals, and a logistic regression analysis were calculated to identify those variables that played an important role. As well as to build an assessment model for the type of referral (self-referral or referred), identifying the possible modifying and/or confounding effects of the variables. Coefficients were estimated by maximum likelihood, with forward selection. Measures for goodness of fit verified the model as appropriate. Hosmer-Lemeshow test percentage of correctly classified values, sensitivity, and specificity. The model with most precision of effects and most quality advantages in the final variables, importance, and simplicity was chosen.
Due to a significant period during which data was excluded (because of the codifying error), the data from 2003–2011 was analysed and reported separately from the 2015 data. IBM statistical software SPSS Statistics 20.0 was used. Data was obtained from the Hospital Admission Aurora and DIRAYA-Emergencies software, regarding the Northern Huelva Health Area. Transfer time and distance between the different locations and the out-of-hospital emergency services or the hospital, were estimated with Google Maps taking into consideration the shortest route.
Ethics approval and consent to participate
The data was provided by the Area Department of Statistics and, both this and its processing, stuck to the guidelines of the Organic Law on Protection of Personal Data (15/1999, December 13).
Results
The total number of patients assisted at the Riotinto Hospital ED between the years 2003 and 2011 and in the year 2015 was 242,508, out of which 125,446 (51.7%) attended on self-referral.
Women recorded more frequent visits to the ED (51.5%), and the mean age of patients assisted was 43.69 years (SD “standard deviation” 26.85), being the largest group those between 15 and 65 years of age. 66.5% of patients came from basic health areas non-adjacent to Riotinto Hospital. 52.2% of them did not have EHES in their town, 4.2% did not have access to daily GP consultations, and in 25.5% of the cases the hospital route was shorter than the EHES route. Out of the total patients treated, 84.3% were discharged directly from the area of consultation.
The mean time of access to the EHES was 6.88 minutes (SD 6.55), taking less than 2 minutes for 50% of the patients. Regarding the transfer time to the hospital, the mean transfer time was 28.44 minutes (SD 19.55); for 50% of the patients, it took a maximum of 27 minutes.
Self-referral patients attending the ED increased from 5% between 2003–07 to 62.2% in 2008, 70.4% in 2011, and 62.9% in 2015. The increase of self-referral contrasted with the decrease of referrals from EHES, which decreased from more than 50% to below 20%. Referrals from general practitioners (GP) were constant (10.6 ± 2.85%).
From 2003 to 2011, 215,639 patients were treated in the hospital emergency department and 50.3% of them were self-referral. Table 1 shows statistical significant differences between self-referral patients versus patients referred by a health professional. Not having a daily GP, consultation is at the limit of the OR = 1.044 (1–1.090). In addition, the self-referral is higher among those who are eventually discharged versus those requiring hospitalisation and further care from 2008 onwards (after organisational changes mentioned above), presenting a risk 3.861 times higher than that of the patients previously assisted (OR = 3.861 (3.793–3.931)).
Table 1. Bivariate analysis, years 2003–2011.
| TOTAL | DECISION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Self-referral | Referred | |||||||||
| N | % | N | % | N | % | x2 | P-value | OR | 95% IC for OR | |
| Total | 215,639 | 100% | 108,531 | 50.3% | 107,108 | 49.7% | ||||
| Sex | ||||||||||
| 0. *Male | 105,056 | 48.7% | 51,522 | 49.0% | 53,534 | 51.0% | 135.404 | <0.001 | 1.106 | 1.087–1.124 |
| Female | 110,535 | 51.3% | 56,980 | 51.5% | 53,555 | 48.5% | ||||
| Age | ||||||||||
| 0. 65 years or more (Elder people) | 62,637 | 29.0% | 25,716 | 41.1% | 36,921 | 58.9% | 3,037.43 | <0.001 | 1.694 | 1.662–1.726 |
| < 65 years | 153,002 | 71.0% | 82,815 | 54.1% | 70,187 | 45.9% | ||||
| 0. < 15 and ≥ 65 years | 100,712 | 46.7% | 46,550 | 46.2% | 54,162 | 53.8% | 1,276.28 | <0.001 | 1.362 | 1.339–1.385 |
| Between 15 and 64 years (adults) | 114,927 | 53.3% | 61,981 | 53.9% | 52,946 | 46.1% | ||||
| 0. ≥ 15 years | 177,568 | 82.3% | 87,699 | 49.4% | 89,869 | 50.6% | 356.24 | <0.001 | 1.238 | 1.211–1.266 |
| From 0 to 14 years (children) | 38,071 | 17.7% | 20,832 | 54.7% | 17,239 | 45.3% | ||||
| Basic Health Area | ||||||||||
| 0. Non-adjacent | 143,665 | 66.6% | 66,403 | 46.2% | 77,262 | 53.8% | 2,907.38 | <0.001 | 1.642 | 1.613–1.672 |
| Adjacent | 71,974 | 33.4% | 42,128 | 58.5% | 29,846 | 41.5% | ||||
| Extrahospital Emergency Service—Riotinto Hospital Emergency Department | ||||||||||
| 0. Not returning | 160,863 | 74.6% | 74,908 | 46.6% | 85,955 | 53.4% | 3,588.25 | <0.001 | 1.824 | 1.788–1.860 |
| Returning | 54,776 | 25.4% | 33,623 | 61.4% | 21,153 | 38.6% | ||||
| Extrahospital Emergency Service in town | ||||||||||
| 0. YES | 88,785 | 44.1% | 37,865 | 42.6% | 50,920 | 57.4% | 2,641.76 | <0.001 | 1.590 | 1.563–1.619 |
| NO | 112,381 | 55.9% | 60,894 | 54.2% | 51,487 | 45.8% | ||||
| Daily consultation | ||||||||||
| 0. YES | 192,435 | 95.7% | 94,383 | 49.0% | 98,052 | 51.0% | 3.85 | 0.05 | 1.044 | 1–1.090 |
| 1. NO | 8,731 | 4.3% | 4,376 | 50.1% | 4,355 | 49.9% | ||||
| Time to Extrahospital Emergency Service | ||||||||||
| 0. ≤ 2 minutes | 114,762 | 57.0% | 50,100 | 43.7% | 64,662 | 56.3% | 3,161.23 | <0.001 | 1.664 | 1.635–1.694 |
| > 2 minutes | 86,404 | 43.0% | 48,659 | 56.3% | 37,745 | 43.7% | ||||
| Time to Riotinto Hospital Emergency Department | ||||||||||
| 0. > 27 minutes | 97,159 | 48.3% | 42,573 | 43.8% | 54,586 | 56.2% | 2,092.63 | <0.001 | 1.506 | 1.480–1.533 |
| ≤27 minutes | 104,007 | 51.7% | 56,186 | 54.0% | 47,821 | 46.0% | ||||
| Destination | ||||||||||
| 0. Admission | 31,610 | 14.7% | 14,696 | 46.5% | 16,914 | 53.5% | 210.33 | <0.001 | 1.193 | 1.165–1.222 |
| Discharge | 183,537 | 85.3% | 93,434 | 50.9% | 90,103 | 49.1% | ||||
| Period | ||||||||||
| 0. 2003–2007 | 112,568 | 52.2% | 39,152 | 34.8% | 73,416 | 65.2% | 22,777.21 | <0.001 | 3.861 | 3.793–3.931 |
| 2008–2011 | 103,071 | 47.8% | 69,379 | 67.3% | 33,692 | 32.7% | ||||
The total of cases per variable does not always correspond with the total of patients, as there is no data record for some patients. *Value “0” or “1” before the modality of each variable indicates the codification used for the analysis, assigning value “1” to the category exposed to risk and “0” to the basal or reference category.
The probability of attending the emergency department by self-referral from 2003 to 2011 from the binary regression model follows the following formula:
where T_EHES indicated whether the time from the town of origin to the EHES of reference is lower, equal or greater than the median; and Period assessed if the patient attended before or after 2008.
The period had a modifying effect, homogeneity test with a 44.47 chi-square statistic (p-value<0.001). The Wald test assessed the individual statistical significance of each of the estimated coefficients (p-value<0.001 in all cases), and the omnibus test, with the statistic of the likelihood ratio LR = 25393.902 (p-value<0.001), allowed to affirm that the variables included in the model effectively contributed to explaining the modifications that took place in the probability of attending ED on the patients’ self-referral. The Hosmer and Lemeshow test did not reject the logistic regression model (p-value = 1). The selected model obtained a sensitivity of 62.8% and a specificity of 69.2%, correctly classifying 66% of the patients. The probability of attending on self-referral depending on the period and whether the town is more than 2 minutes away from the EHES is collected in Table 2.
Table 2. Estimated values of the logistic regression model.
2003–2011.
| Time to the Extra-hospital Emergency Service | Period | Self-referral Probability |
|---|---|---|
| Less than or equal to 2 minutes | Attends between 2003 and 2007 | 29.09% |
| Less than or equal to 2 minutes | Attends between 2008 and 2011 | 60.68% |
| More than 2 minutes | Attends between 2003 and 2007 | 39.27% |
| More than 2 minutes | Attends between 2008 and 2011 | 73.46% |
Regarding analysis from data obtained in 2015, 26,869 patients were assisted at the ED, 63% of them on self-referral. As a novelty, it was possible to analyse the severity levels classified by the Spanish System of Triage, consolidated that same year. Among the patients with lower severity (triage 4 and 5) the self-referral predominated, 10,646 cases (70%). However, this percentage decreased to 53.6% (6,254 patients) in the highest levels of severity (triage 1, 2, and 3).
The bivariate contrasts made to study the association between different factors and the fact of attending ED on self-referral or referral in the year 2015 were significant. Table 3 collects the statistics of the chi-square test, odd ratios and confidence intervals, together with the information relative to the total frequencies and by category.
Table 3. Bivariate analysis.
Year 2015.
| TOTAL | DECISION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Self-referral | Referral | |||||||||
| N | % | N | % | N | % | x2 | P-value | OR | 95% CI for OR | |
| 26,869 | 100% | 16,915 | 63.0% | 9,954 | 37.0% | |||||
| Sex | ||||||||||
| 0. *Male | 12,476 | 46.4% | 7,581 | 60.8% | 4,895 | 39.2% | 47.93 | <0.001 | 1.192 | 1.134–1.252 |
| Female | 14,386 | 53.6% | 9,330 | 64.9% | 5,056 | 35.1% | ||||
| Age | ||||||||||
| 0. 65 years or more (Elder people) | 7,742 | 28.8% | 3,773 | 48.7% | 3,969 | 51.3% | 942.88 | <0.001 | 2.310 | 2.188–2.438 |
| < 65 years | 19,127 | 71.2% | 13,142 | 68.7% | 5,985 | 31.3% | ||||
| 0. < 15 y ≥ 65 years | 12,419 | 46.2% | 7,058 | 56.8% | 5,361 | 43.2% | 371.02 | <0.001 | 1.630 | 1.551–1.713 |
| Between 15 and 64 years (adults) | 14,450 | 53.8% | 9,857 | 68.2% | 4,593 | 31.8% | ||||
| 0. ≥ 15 years | 22,192 | 82.6% | 13,630 | 61.4% | 8,562 | 38.6% | 128.82 | <0.001 | 1.482 | 1.385–1.587 |
| From 0 to 14 years (children) | 4,677 | 17.4% | 3,285 | 70.2% | 1,392 | 29.8% | ||||
| Basic Health Area | ||||||||||
| 0. Non-adjacent | 17,640 | 65.7% | 10,113 | 57.3% | 7,527 | 42.7% | 696.41 | <0.001 | 2.086 | 1.974–2.204 |
| Adjacent | 9,229 | 34.3% | 6,802 | 73.7% | 2,427 | 26.3% | ||||
| Route Extra-hospital Emergency Department-Riotinto Hospital Emergency Department | ||||||||||
| 0. Not returning | 19,876 | 74.0% | 11,541 | 58.1% | 83,350 | 41.9% | 782.56 | <0.001 | 2.397 | 2.252–2.551 |
| Returning | 69,93 | 26.0% | 5,374 | 76.8% | 1,619 | 23.2% | ||||
| Extra-hospital Emergency Services in town | ||||||||||
| 0. YES | 10,017 | 41.4% | 5,366 | 53.6% | 4,651 | 46.4% | 460.05 | <0.001 | 1.775 | 1.684–1.871 |
| NO | 14,189 | 58.6% | 9,533 | 67.2% | 4,656 | 32.8% | ||||
| Daily consultation | ||||||||||
| 0. YES | 22,720 | 93.9% | 13,933 | 61.3% | 8,787 | 38.7% | 7.99 | 0.005 | 1.172 | 1.050–1.308 |
| NO | 1,486 | 6.1% | 966 | 65.0% | 520 | 35.0% | ||||
| Time to Extra-hospital Emergency Services | ||||||||||
| 0. ≤ 2 minutes | 13,338 | 55.1% | 7,315 | 54.8% | 6,023 | 45.2% | 564.77 | <0.001 | 1.901 | 1.803–2.006 |
| > 2 minutes | 10,868 | 44.9% | 7,584 | 69.8% | 3,284 | 30.2% | ||||
| Transfer time | ||||||||||
| 0. >27 minutes | 11,072 | 45.7% | 6,031 | 54.5% | 5,041 | 45.5% | 432.23 | <0.001 | 1.738 | 1.649–1.831 |
| ≤ 27 minutes | 13,134 | 54.3% | 8,868 | 67.5% | 4,266 | 32.5% | ||||
| Destination | ||||||||||
| 0. Admission | 5,656 | 21.2% | 2,916 | 51.8% | 2,710 | 48.2% | 380.96 | <0.001 | 1.803 | 1.698–1.913 |
| Discharge | 20,931 | 78.8% | 13,811 | 66.0% | 712 | 34.0% | ||||
| Priority** | ||||||||||
| 0. Triage 1.2 o 3 | 11,659 | 43.4% | 6,254 | 53.6% | 5,405 | 46.4% | 756.26 | <0.001 | 2.016 | 1.917–2.120 |
| Triage 4 o 5 | 15,210 | 56.6% | 10,646 | 70.0% | 4,564 | 30.0% | ||||
The total of cases per variable does not always correspond with the total of patients, as there is no data record for some patients.
*Value “0” or “1” before the modality of each variable indicates the codification used for the analysis, assigning value “1” to the category exposed to risk and “0” to the basal or reference category.
**The priority distinguishes the severity level or triage performed with the Spanish Triage System (STS).
To determine if the new variable was confounding in the model, a bivariate analysis was carried out, stratified according to the priority of the patient and obtaining a higher risk (OR = 2.143) for those less serious patients (triage 4 and 5).
The homogeneity test between the OR values of the two strata determined the existing differences, with the statistic 9.489 (p-value = 0.002), and the interaction was considered when studying the model.
The selected model in 2015 can be summarised in the equation:
where PRIORITY indicates the level of triage or severity.
For the proposed model, the Wald test assessed the individual statistical significance of the coefficients (p-value<0.001 in all cases). The variables in the model contributed to explain the probability changes for a patient to attend the hospital ED on his/her self-referral as the omnibus test is rejected, with statistic 1467.676 (p-value<0.001). The model adjustment and the Hosmer and Lemeshow test were accepted (p-value = 1). Finally, the proposed model correctly classified 64.4% of the patients, with a sensitivity of 32.8% and a specificity of 83.1%. Table 4 collected the probabilities associated with the model, depending on the time to arrive to the EHES and the patient classification by the Spanish Triage System.
Table 4. Estimated values of the logistic regression model.
2015.
| Time to the Extra-hospital Emergency Service | Priority | Self-referral Probability |
|---|---|---|
| Less than or equal to 2 minutes | Triage 1.2 o 3 | 46.61% |
| Less than or equal to 2 minutes | Triage 4 o 5 | 61.73% |
| More than 2 minutes | Triage 1.2 o 3 | 61.42% |
| More than 2 minutes | Triage 4 o 5 | 77.56% |
Discussion
The analysis of self-referral increase in the Riotinto Hospital ED has helped us to understand better the profile and patterns of patients who attend it, and thus, to identify the factors that would allow us to plan health resources more efficiently, showing a very similar behaviour–in particular regarding self-referral-, to the described in the literature (age, sex, distance, time, etc.) [8,9,10,11].
As previously mentioned, in the years excluded from the study, from 2012 to 2014, the figures of self-referral were excessively high (80–85%). This could be caused by a misinterpretation in the assignment of the origin of the patients, an error in the coding when recording the data. For this reason, it was decided not to include them since they could distort the results with a "false positive".
The increase of self-referrals seems to be due to the loss of accessibility to health resources [12,13]. This is explained by structural causes, inherent to the socio-demographic context and the dispersion of the Northern Huelva Health Area which, with its mountainous geography, causes longer transfer times between towns and health resources. This affected negatively the timeliness of emergency services response and the distribution of human resources, which together with the absence of specific critical care transport equipment, affected the activity of the EHES in those places with a single doctor, forcing their closure, and increasing self-referrals.
Geographic accessibility and EHES availability have been regarded as facilitating variables. In fact, the absence of EHES in the local area was influential when deciding whether to attend the hospital on a self-referral basis, as well as the route the patient had to perform to receive emergency care. Patients whose EHES was in the opposite direction to that of the hospital or in an alternative route, were more likely to attend the Riotinto hospital ED on self-referral. Furthermore, when quantifying the time, it was found that self-referrals at the hospital were favoured because of the proximity to the centre (EHES) due to greater transfer times from the town to the EHES. This outcome coincides with previous studies that found that a larger distance to their primary health care centre is associated with an increased attendance to the hospital ED [14,15]. In addition, people who lived closer to the hospital [16,17] and in urban areas [18,19] made a greater use of the hospital ED and self-referral. Even so, in the period after 2008–2015, 55% of those living more than 50 minutes away referred themselves; twice the percentage than that of 2003–2007.
From the organisational point of view, we need to consider the possible influence produced by the cessation of afternoon activity in some health centres and the closing of the “Minas de Riotinto” EHES, since this has an impact on the demand to the health area and the hospital ED. It has been described that the increase in the use of EHES does not reduce hospital emergencies [20], that the use of health services is seen globally, and there is no replacement of primary care and hospital health care levels [21]. However, in our study, we found a decrease of these extrahospital resources. The number of patients who attended the Riotinto Hospital Emergency Department, who belonged to the area EHES, had a 20% increase between the years 2008 and 2011, from 7500 to 9000 patients, with a peak in 2009 of 10500 patients. Of these patients, 80% attended on self-referral. The number of patients coming from other EHES showed very stable figures and, although there was a general increase in self-referral, this was lower (50%-60%).
Similarly, another factor that could have had an influence is the reduction in number of physicians, which was caused by the long periods of no transfer possibilities, and the modifications of their form of recruitment. This affected the physician-patient relationship. Changes were also made in the assignment of contracts; in the doctors’ replacements, where no fixed assignment of quotas was made and with a decrease in the number of replacements regarding the days (-29,9%) and the number of contracts (-47,2%) [22,23].
At the same time, the introduction of improvements and innovations in the hospital service portfolio could increase the confidence and expectations regarding the ED [24]. Note that for patients who lived far from the hospital or in rural populations, the quality of the service was the major factor that influenced the decision making over attending the Riotinto hospital [25]. To this we must add the low accessibility to specialised attention (barriers between different organisation levels) [26].
The adjustment of our data to a binary logistic regression model emphasised the fact that the changes produced in the health system in 2008 and the time to get to the emergency department simultaneously affected the probability of attending on self-referral, where the first element acts as an effect modifier factor. Once the structural and organisational changes were saved and a quantifiable variable of the patient's priority was introduced, in the year 2015, the level of severity or triage and the time to get to the EHES were the factors that influenced the probability of attending the ED on the patients’ self-referral. At the same time, forcing those patients with more severity levels (triage 1–3) and with a greater distance to the EHES to attend the ED on their self-referral, with greater probability than those who live near their EHES (61.4% vs 46.6%); this probability is similar to that of patients with lower severity levels (triage 4–5) and who live closer to the EHES (61.7%).
Apart from analysing each variable of the health system and its repercussion in the increase of self-referral to the Riotinto Hospital ED, we assessed the set of modifications that have enhanced the Hospital's Health Services portfolio with the creation of an ICU, day hospital and palliative care services, pacemaker implantation service, etc., and those modifications that have reduced the Primary Care Emergency System services, with the cessation of activity in some health centres, the closing of the Minas de Riotinto EHES and the loss of the referring physician as examples of these effects. The increase in self-referrals to the hospital ED is a sign of inefficiency of the system that generates greater health expenses and service difficulties, due to the need of transfer to this ED and the subsequent care delay. However, there is another vision through which the user gets a higher quality of health care that compensates for such inefficiency.
Conclusions
This work has allowed us to describe factors regarding the demand for emergency care of a specific population, with particular socio-demographic characteristics, population dispersion, resources, and a health care system that influences the behaviour of patients attending the Riotinto Hospital ED. We have seen in this study that the probability of self-referring to ED is influenced by the changes in the health system and the time it takes for the patient to get from their town to the EHES. Once the patient's severity level was introduced, it was this variable, along with the time to get to the emergency department, which modified the probability of self-referring to the emergency department. Secondly, it allowed us to use trend analysis to better anticipate future population behaviour, if the conditions remain unchanged.
The changes in the organisation and health care must be studied from the point of view of its impact, not only in terms of morbidity and mortality, but also taking into account the patients’ behaviour when using resources and the accessibility that these resources have. Thus, the studied population, rural and remote, changed the pattern of origin of the patients who come to the hospital ED from being predominantly referred from primary care to self-referred [8]. These findings coincide with previous studies in which the lower Index Multiple Deprivation (IMD) is the main predictive factor for the use of emergency services [27].
The great population dispersion, represented by the time of access to the health services, is a determining element that has acted as a necessary factor to expand and maintain the effects of the changes produced in the health system of the Northern Huelva Health Area.
Study limitations
The reasons for consultation and the final diagnosis could not be analysed due to their lack of coding. Diagnosis codes might help tackle this issue in the study. Patients may often be unable to judge the severity of their condition and may have considered non-urgent symptoms as urgent. Health problems are the main motivation for patients to attend the ED on self-referral, even for patients with non-urgent symptoms, and a health professional can refer these patients to either a GP or the ED [28]. In addition, the level of triage of the Aurora software could not be obtained, and in the Diraya-Emergencies a variation was identified in the model used. The year’s range “2012–2014” was discarded because of changes in the origin consignment items in the Emergency Admissions program, substituting the “self-referral” item for "transportation by own means" thus including all except those derived by ambulance. Another limitation was the absence of some demographic data not found in the records: marital status, employment situation, level of education, socioeconomic status, and ethnic background.
Supporting information
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information file.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Bezzina AJ, Smith PB, Cromwell D, Eagar K. Primary care patients in the emergency department: who are they? A review of the definition of the “primary care patient” in the emergency department. Emerg Med Australas. 2005; 17(5–6):472–9. 10.1111/j.1742-6723.2005.00779.x [DOI] [PubMed] [Google Scholar]
- 2.Sempere-Selva T, Peiró S, Sendra-Pina P, Martínez-Espín C, López- Aguilera I. Inappropiate use of an accident and emergency department: Magnitude, associated factors, and reasons. An approach with explicit criteria. Ann Emerg Med. 2001;37:568–79. 10.1067/mem.2001.113464 [DOI] [PubMed] [Google Scholar]
- 3.Tudela P, Mòdol JM. La saturación en los servicios de urgencias hospitalarios. Emergencias. 2015;27:113–20. [PubMed] [Google Scholar]
- 4.Moreno Millán E. ¿Y si adaptáramos los servicios hospitalarios de urgencias a la demanda social y no a las necesidades de salud? Emergencias. 2008;20:276–84. [Google Scholar]
- 5.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Millbank Memorial Fund Q. 1973;51:95–124. [PubMed] [Google Scholar]
- 6.Brezzi M, Dijkstra L, Ruiz V. OECD Extended Regional Typology. The economic performance of remote rural regions Documento de Trabajo OECD Regional Devolement n° 2001/06. París: OECD Publishing, 2011. 10.1787/5kg6z83tw7f4-en. Accessed 28 March 2018. [DOI] [Google Scholar]
- 7.Ministerio de Sanidad, Servicios Sociales e Igualdad. Estudio n° 8815. Barómetro Sanitario 2015. Madrid: Dirección General de Salud Pública Calidad e Innovación Subdirección General de Información Sanitaria e Innovación. Ministerio de Sanidad, Servicios Sociales e Igualdad y Centro de Investigaciones Científicas, 2015. http://www.msc.es/estadEstudios/estadisticas/docs/BS_2015/Es8815mar.pdf. Accessed 28 March 2018.
- 8.Pedregal B, Torres FJ, Zoido F. Medición y desarrollo desigualdades territoriales. Aplicación al Territorio Andaluz. Scripta Nova. Revista Electrónica de Geografía y Ciencias Sociales, Vol. 10, n° 220 Barcelona. 2006. http://www.ub.edu/geocrit/sn/sn-220.htm. Accessed 18 April 2016. [Google Scholar]
- 9.Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica. 2009;25(1):728. [DOI] [PubMed] [Google Scholar]
- 10.Durand AC, Gentile S, Devictor B, et al. ED patients: how nonurgent are they? systematic review of the emergency medicine literature. Am J Emerg Med. 2011;29(3):333345. [DOI] [PubMed] [Google Scholar]
- 11.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency Department Visits for Nonurgent Conditions: Systematic Literature Review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 12.Cowling TE, Harris MJ, Watt HC, Gibbons DC, Majeed A. Access to general practice and visits to accident and emergency departments in England cross-sectional analysis of a national patient survey. Br J Gen Pract. 2014;e434–439. 10.3399/bjgp14X680533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowling TE, Cecil EV, Soljak MA, Lee JT, Millett C, et al. (2013) Access to Primary Care and Visits to Emergency Departments in England: A Cross-Sectional, Population-Based Study. PLoS ONE. 8(6):e66699 10.1371/journal.pone.0066699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young GP, Wagner MB, Kellermann AL, Ellis J, Bou- ley D. Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 Hours in the ED Study Group. JAMA. 1996;276:460–5. [DOI] [PubMed] [Google Scholar]
- 15.Moll van Charante EP, terRiet G, Bindels P. Self-referrals to the A&E department during out-of-hours: patients' motives and characteristics. Patient Educ Couns. 2008;70(2):256–65. 10.1016/j.pec.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 16.McKee CM, Gleadhill DN, Watson JD. Accident and emergency attendance rates: variation among patients from different general practices. Br J Gen Pract. 1990;40:150–3. [PMC free article] [PubMed] [Google Scholar]
- 17.Hull SA, Jones IR, Moser K. Factors influencing the attendance rate at accident and emergency departments in East London: the contributions of practice organization, population characteristics and distance. J Health Serv Res Policy. 1997;2:6–13. [DOI] [PubMed] [Google Scholar]
- 18.Márquez JJ, Domínguez B, Méndez J, Gómez B, Toronjo S, Del Río E, Caballero F. Diferencias en los motivos de consulta entre pacientes que acuden derivados y por iniciativa propia a un Servicio de Cuidados Críticos y Urgencias de un hospital general. Emergencias. 2007;19:70–6. [Google Scholar]
- 19.Grafstein E, Wilson D, Stenstrom R, Jones C, Tolson M, Poureslami I, et al. A Regional Survey to Determine Factors Influencing Patient Choices in Selecting a Particular Emergency Department for Care. Acad Emerg Med. 2013;20(1):63–70. 10.1111/acem.12063 [DOI] [PubMed] [Google Scholar]
- 20.Van der Linden MC, Lindeboom R, van der Linden N, van den Brand CL, Lam RC, Lucas C, et al. Self-referring patients at the emergency department: appropriateness of ED use and motives for self-referral. Int J Emerg Med. 2014;16(7):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sarría-Santamera A, Prado-Galbarroa J, Ramallo-Farinac Y, Quintana-Díaze M, Martínez-Virtoe A, Serrano-Aguilar P. Utilización de los servicios de urgencias en zonas rurales y urbanas. Semergen. 2015;41(2):63–9. 10.1016/j.semerg.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 22.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9:916–23. [DOI] [PubMed] [Google Scholar]
- 23.Oster A, Bindman A. Emergency department visits for ambulatory care sensitive conditions. Med Care. 2003;41:198–207. 10.1097/01.MLR.0000045021.70297.9F [DOI] [PubMed] [Google Scholar]
- 24.Espinel M, Romero L, Fernández L, Torres J, D’ Antonio S. Utilización por cuenta propia de los Servicios de Urgencias Hospitalarias: razones que dan las personas con problemas de salud de baja complejidad para utilizar estos servicios. Polit Soc (Madrid). 2011;48(2):329–52. [Google Scholar]
- 25.Sánchez JA, Alarcón D, Murillo F, Pérez I. Análisis de los factores socioeconómicos y sanitarios que influyen en el aumento progresivo de la frecuentación de las urgencias hospitalarias. Agencia de Evaluación de Tecnologías Sanitarias de Andalucía. Sevilla, 2011. Page 108. [Google Scholar]
- 26.Ojeda JJ, Freire JM, Gérvas J. La coordinación entre Atención Primaria y Especializada. Rev Adm Sanit. 2006;4(2):357–82. [Google Scholar]
- 27.Harris MJ, Patel B, Bowen S. Primary care access and its relationship with emergency department utilisation: an observational, cross-sectional, ecological study. Br J Gen Pract. 2011. 10.3399/bjgp11X613124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kraaijvanger N, van Leeuwen H, Rijpsma D, Edwards M. Motives for self-referral to the emergency department: a systematic review of the literature. BMC Health Serv Res 2016. December 9;16910:685 10.1186/s12913-016-1935-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information file.