Abstract
Background:
Numerous studies indicate caesarean delivery is associated with childhood asthma. Sex-specific associations were reported in four of these studies, and in all four studies the estimated association between caesarean delivery and asthma was of greater magnitude among girls, although most report a lack of evidence of multiplicative interaction.
Methods:
We assessed potential effect modification by sex, on the additive and multiplicative scales, of the association between caesarean delivery and asthma by ages 2 through 6 in up to 17 075 racially-diverse children from a retrospective birth cohort, the Kaiser Air Pollution and Pediatric Asthma (KAPPA) Study. We also conducted a random effects meta-analysis, combining our sex-stratified results (using the odds ratio for compatibility with previous studies) with previously published results.
Results:
Adjusted risk differences for caesarean delivery and asthma in the KAPPA cohort were higher among girls than boys at every follow-up age. By age 5, caesarean delivery was associated with an absolute 3.8% (95% confidence interval [CI] 0.4%, 7.3%) higher asthma risk among girls and a 1.9% (95% CI −1.7, 5.4) higher risk among boys. The summary odds ratio from the meta-analysis for caesarean delivery and asthma among girls was 1.26 (95% CI 1.14, 1.39) and 1.08 (95% CI 0.98, 1.20) among boys (P=0.036).
Conclusions:
Higher, but imprecise, estimates for females across five studies should motivate investigators to estimate sex-specific associations for caesarean delivery and asthma and to explore biological mechanisms or sex-dependent biases that could explain this possible heterogeneity.
Keywords: caesarean delivery, asthma, effect modification, sex
Introduction
Over the past two decades numerous investigators have reported an association between caesarean delivery and asthma development. Proposed mechanisms for this association include differences by delivery mode in microbial colonization1, 2 and neonatal respiratory morbidity.3–6 Three separate meta-analyses have concluded that asthma risk is approximately 20% higher in children delivered by caesarean than those delivered vaginally.7–9 In the literature on the association between caesarean and asthma, to our knowledge, only four studies have reported sex-specific associations between caesarean and asthma or persistent wheezing, and all four reported higher point estimates among girls than boys.10–13 Only one12 of the four studies10–13 reported evidence of multiplicative interaction. The consistency of stronger associations among girls is noteworthy, particularly in light of the frequently limited power for tests of interaction,14 and known sex differences in the epidemiology and natural history of childhood asthma. For example, asthma prevalence is higher among boys until puberty when prevalence becomes higher among girls. Observed sex differences in airway size, lung growth, and immunology are thought to play a role in higher prevalence among young boys; sex hormones are thought to play a role in the increase among girls after puberty.15
We conceptualize three potential explanations for why the association between caesarean delivery and asthma appears stronger in girls than boys. First, estimates in one sex could be more biased than the other, for example due to differential sources or magnitude of confounding (e.g., if maternal asthma was a risk factor for childhood asthma only among female offspring). Second, the four studies to observe stronger associations among girls all used ratio measures of association. Given the known higher baseline risk of asthma among young boys than young girls, if the effect of caesarean on asthma is additive rather than multiplicative, ratio measures could make the associations appear stronger in girls. Third, caesarean may truly be a more frequent cause of asthma among girls than boys.
The provocative but limited evidence on sex differences in the association between caesarean delivery and asthma motivated us to test this hypothesis. We addressed whether observed differences by sex could be explained by sex differences in confounding by measured variables for caesarean and asthma (sex-dependent associations between covariates and caesarean or asthma); or the use of ratio measures of association instead of difference measures. We also conducted meta-analyses stratified by sex, combining results from our study with those published in the literature, to summarize the evidence on this association.
Methods
The Kaiser Air Pollution and Pediatric Asthma Study (KAPPA) is a retrospective birth cohort of 24,608 racially-diverse children insured by Kaiser Permanente Georgia (KPGA) Health Maintenance Organization (HMO) for at least the first year of life (allowing up to 90-day enrollment gaps) and born between 2000 and 2010. KPGA and Emory University institutional review boards approved this study. Children in the KAPPA cohort were followed from birth until KPGA enrollment ended, or until September 2013 if that occurred first. Mode of delivery was determined using Georgia birth certificates and dichotomized as vaginal or caesarean. Linkage to birth certificates was completed by KPGA through maternal information (i.e., name, date of delivery, address). There were 7533 children from the KAPPA study excluded from this analysis due to missing mode of delivery information. Mode of delivery was missing for three reasons: inability to link children to mothers in KPGA (n=2817), inability to link children to birth certificates on maternal information (n=3208), and missing data from birth certificates due primarily to an administrative issue involving a change in variable names (n=1508). eFigure 1 provides details on this linkage. Information from KPGA medical records was available for all children included in this analysis and their mothers.
We examined cumulative asthma incidence by ages 2 through 6, classifying a child as having asthma if after the first year of life they received at least one asthma diagnosis (ICD-9 493.XX) and one asthma-related medication dispensing (including steroid and non-steroid relievers and controllers). Once a child was classified as asthmatic, they were classified as such at every subsequent age. There is no one widely accepted case definition for early-life asthma due to the difficulty of diagnosing asthma in young children and the transience of childhood asthma. As a secondary outcome we examined persistent asthma at age 5, defined as a child with incident asthma by age 5 who also had at least 1 asthma diagnosis or 1 asthma-related medication dispensing between his or her 4th and 5th birthdays; for this analysis we excluded children who met the definition of incident asthma but had no evidence of asthma morbidity between age 4 and 5. Age 5 was selected because diagnoses of asthma become more reliable around age 5.
Statistical analysis
The association between caesarean and cumulative asthma incidence was assessed using binomial generalized linear regression. The risk difference (binomial model with an identity link function) and risk ratio (log binomial regression) were the primary and secondary measures of association of interest, respectively. We calculated both measures to investigate whether the measure used affected conclusions. Cumulative risk of asthma was assessed in successively longer time periods among children enrolled to each follow-up age: 1 to 2-year risk, 1 to 3-year risk, 1 to 4-year risk, 1 to 5-year risk, and 1 to 6-year risk. Models were estimated using generalized estimating equations with robust variance estimation to account for correlation between siblings.
Models were adjusted for sex (male, female), birth year (indicator variables for 2000–2010), maternal age (linear splines using tertile (29, 34) cut points), maternal education (<12th grade, high school/GED, some college or more, missing), race (white, black, other/unknown), ethnicity (Hispanic, non-Hispanic), maternal asthma (≥1 diagnosis of asthma (ICD-9 code 493.XX)), maternal atopy (≥1 diagnosis of allergic rhinitis (ICD-9 code 477.X) or atopic dermatitis (ICD-9 code 691.8)), and preterm birth (<37 weeks’ gestation determined from last menstrual period). Effect modification by sex was assessed in sex-stratified models and by the addition of a product term to models.
Meta-analyses
We conducted a literature search of papers published through February 2017 in PubMed and Web of Science with the search terms (cesarean section OR C-section OR mode of delivery) and (asthma OR wheeze). Abstracts were screened to identify studies that estimated the association between mode of delivery and asthma or wheeze among children. Only articles in English were included, and we confirmed that all studies included in meta-analyses on this topic7–9 were captured. We then reviewed the results sections of included articles on the association between caesarean and asthma to identify any reported sex-specific associations. To summarize the evidence for potential effect modification of the association between caesarean and asthma by sex, we performed random effects meta-analyses combining our sex-specific results with those from previous studies. We used the odds ratio as the measure of association for the meta-analyses because it was used by the majority of previous studies on this topic. This and another study did not use the odds ratio as a measure of association in their analysis: (i) for our study we re-calculated the age 5 adjusted analyses using logistic regression; (ii) for one previously published study we approximated odds ratios from risk ratios.16 Publication bias assessment was completed using funnel plots and Egger’s test.17 Analyses were completed in SAS 9.4 (SAS Institute Inc., Cary, NC) and R 3.1.
Results
Of the 17,075 children from the KAPPA study, 31.2% were delivered by caesarean. Preterm birth and maternal age of 40 or more were strongly associated with increased risk of caesarean. There was a trend of increasing proportion of deliveries by caesarean over time, from 23% among children born in 2000 to 34% among children born in 2010; no temporal trend was observed for asthma incidence. Boys were more likely to be delivered by caesarean than girls (33% versus 30%, Table 1), and also were more likely to have asthma at every age (eTable 1). Distributions of caesarean and asthma were similar between children lost to follow-up and children retained in the cohort. The strongest predictors of childhood asthma were male sex, maternal asthma, and preterm birth (eTable 2).
Table 1.
Overall cohort characteristics among 17,075 children from the KAPPA cohort and number and percent caesarean delivery among males (n=8,729) and females (n=8,346)
| KAPPA Cohort n |
Caesarean delivery among males n(%) |
Caesarean delivery among females n(%) |
|
|---|---|---|---|
| All | 17,075 | 2,858 (33) | 2,466 (30) |
| Race/Ethnicity | |||
| Black | 6,363 | 1,180 (36) | 1,025 (33) |
| White | 8,299 | 1,284 (30) | 1,096 (27) |
| Other1 | 2,370 | 392 (32) | 331 (29) |
| Unknown race | 43 | 2 (20) | 14 (42) |
| Hispanic ethnicity | 1,591 | 266 (33) | 223 (29) |
| Preterm Birth (birth at <37 weeks gestation) | |||
| Yes | 1,839 | 481 (49) | 402 (47) |
| No | 15,236 | 2,377 (31) | 2,064 (28) |
| Low Birthweight (birthweight <2500 grams) | |||
| Yes | 1,367 | 383 (58) | 363 (51) |
| No | 15,708 | 2,475 (31) | 2,103 (28) |
| Maternal Education | |||
| <12th grade | 290 | 38 (25) | 36 (26) |
| High school/GED | 2,605 | 439 (33) | 332 (26) |
| Some college or more | 13,143 | 2,194 (33) | 1,919 (30) |
| Missing | 1,037 | 187 (37) | 179 (34) |
| Maternal Asthma2 | |||
| Yes | 2,075 | 409 (38) | 296 (30) |
| No | 15,000 | 2449 (32) | 2,170 (29) |
| Maternal Atopy3 | |||
| Yes | 6,254 | 1,130 (35) | 961 (32) |
| No | 10,821 | 1,728 (31) | 1,505 (28) |
| Maternal Age at Delivery | |||
| <25 | 1,509 | 183 (23) | 114 (16) |
| 25 – <30 | 4,934 | 700 (27) | 590 (25) |
| 30 – <35 | 6,364 | 1,086 (33) | 928 (30) |
| 35 – <40 | 3,494 | 701 (41) | 651 (37) |
| ≥40 | 774 | 188 (49) | 183 (47) |
Includes Asian, American Indian, Alaska Native, Native Hawaiian or other Pacific Islander, and children identifying with more than one racial group
Maternal asthma defined as one or more diagnosis of asthma (ICD-9 code 493.XX).
Maternal atopy defined as one or more diagnosis of allergic rhinitis (ICD-9 code 477.X) or atopic dermatitis (ICD-9 code 691.8)
Overall risk differences for caesarean and asthma incidence were positive in both crude and adjusted models and increased with follow-up age (Table 2); associations combining the sexes are presented for comparison with previous studies. When adjusting for covariates, the overall association between caesarean and asthma ranged from an absolute 0.9% (95% CI −0.3, 2.1) increase in asthma risk by age 2 (i.e., 9 more asthma cases per 1,000 deliveries) to a 4.1% (1.1, 7.1) increase in asthma risk by age 6 (i.e., 41 more asthma cases per 1,000 deliveries).
Table 2.
Risk differences, risk ratios and 95% confidence intervals for asthma incidence by ages 2–6 and caesarean delivery; full cohort and stratified by sex
| RISK DIFFERENCE | |||
|---|---|---|---|
| Cohort | Both Sexes Crude RD (95% CI) |
Male Crude RD (95% CI) |
Female Crude RD (95% CI) |
| Age 2 | 1.7% (0.5, 2.9) | 1.6% (−0.2, 3.4) | 1.7% (0.1, 3.3) |
| Age 3 | 2.0% (0.3, 3.6) | 1.4% (−1.0, 3.7) | 2.4% (0.2, 4.7) |
| Age 4 | 3.1% (1.0, 5.1) | 2.7% (−0.3, 5.6) | 2.9% (0.1, 5.7) |
| Age 5 | 4.2% (1.7, 6.7) | 3.5% (−0.0, 7.1) | 4.2% (0.7, 7.6) |
| Age 6 | 5.5% (2.6, 8.5) | 4.9% (0.7, 9.0) | 5.2% (1.1, 9.4) |
| Cohort | Both Sexes Adjusted RD (95% CI) |
Male Adjusted RD (95% CI) |
Female Adjusted RD (95% CI) |
| Age 2 | 0.9% (−0.3, 2.1) | 0.6% (−1.1, 2.3) | 1.2% (−0.3, 2.7) |
| Age 3 | 1.3% (−0.4, 2.9) | 0.2% (−2.2, 2.5) | 2.2% (0.0, 4.4) |
| Age 4 | 2.3% (0.2, 4.4) | 1.5% (−1.4, 4.5) | 2.9% (0.1, 5.7) |
| Age 5 | 2.9% (0.4, 5.5) | 1.9% (−1.7, 5.4) | 3.8% (0.4, 7.3) |
| Age 6 | 4.1% (1.1, 7.1) | 3.2% (−0.9, 7.4) | 4.7% (0.5, 8.8) |
| RISK RATIO | |||
| Cohort | Both Sexes Crude RR (95% CI) |
Male Crude RR (95% CI) |
Female Crude RR (95% CI) |
| Age 2 | 1.17 (1.05, 1.29) | 1.13 (0.99, 1.28) | 1.21 (1.02, 1.43) |
| Age 3 | 1.11 (1.02, 1.21) | 1.06 (0.96, 1.18) | 1.17 (1.02, 1.34) |
| Age 4 | 1.13 (1.04, 1.23) | 1.10 (0.99, 1.22) | 1.15 (1.01, 1.32) |
| Age 5 | 1.16 (1.06, 1.26) | 1.11 (1.00, 1.24) | 1.18 (1.03, 1.35) |
| Age 6 | 1.18 (1.08, 1.29) | 1.14 (1.02, 1.28) | 1.20 (1.04, 1.38) |
| Cohort | Both Sexes Adjusted RR (95% CI) |
Male Adjusted RR (95% CI) |
Female Adjusted RR (95% CI) |
| Age 2 | 1.08 (0.97, 1.20) | 1.06 (0.93, 1.20) | 1.15 (0.97, 1.37) |
| Age 3 | 1.05 (0.97, 1.15) | 1.01 (0.91, 1.13) | 1.15 (1.00, 1.33) |
| Age 4 | 1.08 (0.99, 1.18) | 1.06 (0.95, 1.18) | 1.14 (1.00, 1.31) |
| Age 5 | 1.08 (1.00, 1.18) | 1.05 (0.94, 1.17) | 1.14 (1.00, 1.31) |
| Age 6 | 1.11 (1.02, 1.22) | 1.08 (0.97, 1.21) | 1.14 (0.99, 1.32) |
RD = risk difference. RR = risk ratio. Adjusted models control for sex (excluded from stratified models), race, ethnicity, year of birth, maternal asthma, maternal atopy, maternal education, maternal age, and preterm birth.
Stratifying by sex, crude risk differences were similar between sexes, but slightly larger among girls than boys. In adjusted results, differences by sex were more pronounced, with stronger evidence of an association between caesarean and asthma among girls than among boys at every follow-up age (Table 2). For example, among girls by age 5, caesarean was associated with a 3.8% (95% CI 0.4, 7.3) higher risk of asthma while among boys caesarean was associated with a 1.9% (95% CI −1.7, 5.4) higher risk. Sex-specific risk differences calculated using a cross-product term between caesarean and sex (eTable 3) were very similar to risk differences from stratified models (Table 2), as were models controlling for low birthweight instead of preterm birth. When using the risk ratio, effect estimates did not increase with follow-up age, but otherwise the pattern of results was similar to those observed using risk differences (Table 2). Tests for interaction were not statistically significant (P-values >0.2 for interaction in adjusted models). We examined the individual and joint effects of male sex and caesarean, each relative to the referent group of females born vaginally for both the risk difference and risk ratio for cumulative asthma incidence of asthma by age 5. For both additive and multiplicative measures, the interaction parameter male*caesarean was imprecise, but in the direction of sub-additive and sub-multiplicative (negative interaction) (eTable 4).
When we assessed the outcome of persistent asthma at age 5 (cases restricted to those with evidence of asthma morbidity between ages 4 and 5), results were similar to results for incident asthma. In adjusted models the RD for persistent asthma at age 5 was 3.4% (95% CI 0.2, 6.6) for girls and 0.8% (95% CI −2.5, 4.2) for boys.
Assessment of individual covariates and their impact on sex-specific results indicated that preterm birth and maternal asthma were confounders of the association between caesarean and asthma for both males and females; however, preterm birth was a stronger predictor of asthma for boys (risk increase of 12% for boys versus 5% for girls by age 5, eTable 2), therefore adjustment for preterm birth (which is also associated with caesarean, Table 1) reduced the estimates more for boys than girls. We defined full-term births as births ≥37 weeks gestation and observed similar results when restricting analyses to full-term births. Maternal asthma and atopy were similarly predictive of asthma incidence in males and females (risk differences from age 5 models in males: maternal asthma 13.4% (8.6, 18.2), maternal atopy 4.7% (1.4, 8.0); females: maternal asthma 14.0% (9.1, 18.8), maternal atopy 4.2% (1.1, 7.2)). However, maternal asthma increased the caesarean rate by 6% for boys, and only 1% for girls, relative to non-asthmatics (Table 1), so adjustment for maternal asthma had a greater impact on estimated associations for boys. These findings are consistent with our DAG (Figure 2) highlighting assumptions about relationships between key variables in our analysis.
Figure 2.
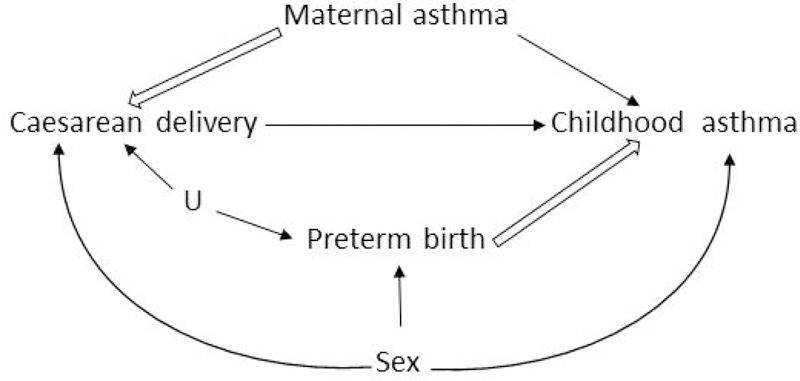
Simplified directed acyclic graph highlighting variables that were important in our analysis of sex heterogeneity [hollow arrows represent relationships that differed by sex, U represents obstetric factors that are indications for preterm birth via caesarean delivery].
We identified 60 studies that assessed the relationship between delivery mode and childhood asthma. Five of these studies indicated that they explored interaction by sex, and four reported separate estimates for males and females10–13 (Table 3). One study18 did not provide estimates, but indicated they observed no interaction by sex when assessed by a Wald test. In random effects meta-analyses combining stratified results from the KAPPA study with those from previous studies, the summary odds ratio for the association between caesarean and asthma among girls was 1.26 (95% CI 1.14, 1.39) and 1.08 (95% CI 0.98, 1.20) among boys. We observed no evidence of heterogeneity (Figure 1) or publication bias (eFigure 2) for either meta-analysis. The summary odds ratios for males and females were different (P=0.036).
Table 3.
Characteristics of results for the association between caesarean delivery and asthma stratified by sex from current and previous studies included in meta-analysis (results shown in Figure 1)
| First
author, year, country |
Study design | Analytic sample size |
Outcome, age at assessment |
Model covariates |
|---|---|---|---|---|
| Magnus, 2011, Norway |
prospective cohort study |
37,171 | maternal report of asthma, 36 months |
premature rupture of membranes,
gestational age, birthweight, breastfeeding, early day care attendance, pregnancy complications, maternal variables (parity, age, previous caesarean delivery, education, prepregnancy body mass index, smoking, chronic conditions, preference for caesarean delivery, atopy) |
| Menezes, 2011, Brazil |
prospective cohort study |
855 | maternal/child report of persistent wheezing, 4 and 11 yearsa |
birthweight, gestational age,
intrauterine growth restriction, skin color, birth order, maternal variables (age, education, smoking, wheezing), paternal smoking and wheezing, socioeconomic position |
| Pennington, 2018, USA |
retrospective cohort study |
6,478 | ≥1 asthma diagnosis and ≥1 asthma- related medication dispensing after the first year of life, 5 yearsb |
race, ethnicity, year of birth,
preterm birth, maternal variables (age, education, asthma, atopy) |
| Renz- Polster, 2005, USA |
Retrospective cohort study |
7,872 | ≥1 asthma
diagnosis, 6–10 years |
diagnosis age, birthweight, birth
order, antibiotics exposure, ethnicity, multiple gestation, maternal variables (age, education, marital status, smoking, asthma and/or hay fever medication use) |
| Werner, 2007, Denmark |
prospective cohort study |
7,119 | maternal report of child ever being diagnosed with asthma, 15 to 18 yearsc |
restricted to full-term births ≥2500
grams, Apgar score ≥7 (5 minutes), no model covariates indicated; however, adjustment for breast feeding, maternal age, smoking, education, previous deliveries, and sex did not meaningfully change overall caesarean estimate (sexes combined) |
Persistent wheezing results were also reported for ages 11 and 15. We included results for this age range in our meta-analysis because it is more consistent with early childhood.
Our study examined outcomes at ages 2–6, but results at age 5 were included in the meta-analysis.
While the age at outcome assessment was after childhood, participants were asked about their child ever being diagnosed with asthma. Since many of these diagnoses were likely during childhood we included this article.
Figure 1.
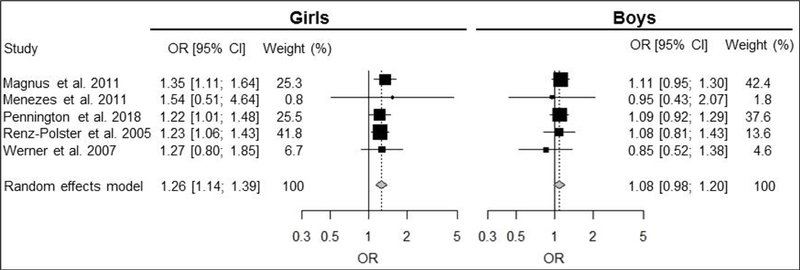
Meta-analysis for the association between caesarean delivery and childhood asthma, stratified by sex [Tests of heterogeneity results: Girls: I-squared=0%, tau-squared=0, Q=0.8, df=4, p=0.94. Boys: Isquared= 0%, tau-squared=0, Q=1.2, df=4, p=0.88. Z-test for comparison between sexes: 2.10, df = 1, Pvalue= 0.036].
Comment
Principal findings
This is the fifth study to report stronger estimated associations between caesarean delivery and asthma among girls than boys. Within our study and in three of the four previous studies, there was not strong evidence of sex differences, but the consistency of higher estimates among girls across the five studies that report sex-specific associations is noteworthy. The meta-analysis showed a 26% increase in odds of asthma for caesarean among girls compared to an 8% increase among boys, and it provided stronger evidence of a sex difference. Higher estimated associations among girls on both additive and multiplicative scales indicated that differences observed on the multiplicative scale are not due to the higher baseline asthma risk among young boys. In our study, adjusting for potential confounders led to larger differences between the sexes.
Interpretation
Differences by sex were first reported in 2005 among children enrolled in Kaiser Permanente Northwest Region with an odds ratio of 1.53 (95% CI 1.11, 2.10) in girls and 1.08 (95% CI 0.81, 1.43) in boys.12 When researchers restricted their exposure to repeat caesareans (used as a proxy for deliveries least likely to include transfer of vaginal flora, a proposed mechanism of effect1, 2) there was stronger evidence of multiplicative interaction between caesarean and sex. Two additional publications, on cohorts in Denmark and Brazil, presented stronger associations between caesarean and asthma or persistent wheezing among girls than boys, but with confidence intervals including the null for both sexes.11, 13 Finally, the Norwegian mother and child cohort study of 37,171 children reported risk ratios for caesarean and asthma of 1.32 (95% CI 1.09, 1.60) among girls and 1.09 (95% CI 0.93, 1.27) among boys (P=0.13 for interaction).10 In four out of five studies that assessed these sex-specific associations (including ours), statistical tests of interaction were not significant (i.e., P<0.05). However, tests of interaction frequently have low power to detect modest heterogeneity, as studies are typically powered only to detect the main effects of interest. The limited but consistent higher estimates reported among girls thus far on this topic should motivate future studies to report sex-specific estimates for caesarean and asthma regardless of whether the tested interaction is significant.
The well-documented sex differences in the natural history of asthma lend credence to the possibility that caesarean may be an asthma risk factor of differential importance for males and females. Biologic differences that contribute to differences in asthma susceptibility may start in utero, where lung development occurs more rapidly in females, and are evident in structural differences between male and female respiratory systems at birth.19, 20 In childhood, asthma prevalence is higher among males, but after puberty the prevalence is higher among females, potentially due to hormonal changes among other factors.15, 21 Moreover, there is some evidence of other risk factors for asthma and wheeze that differ by sex.22, 23 One proposed mechanism for an association between caesarean and asthma, relating to the hygiene hypothesis, is that children who are not delivered vaginally have altered microbial colonization which could influence immune system development and asthma susceptibility.1, 2 A second proposed mechanism is that neonatal respiratory morbidity, for which children delivered by caesarean are at an increased risk,3–5 may subsequently increase asthma risk.6 Although the underlying mechanisms that drive sex differences in asthma are poorly understood, it is possible that a greater proportion of girls are vulnerable to these hypothesized mechanisms for caesarean and asthma.
An alternative to true effect modification by sex is the possibility that the association for one sex is more affected by biases such as unmeasured confounding or misclassification. We were unable to adjust for maternal body mass index, birth order, and breastfeeding all of which may influence the association between caesarean and asthma.10, 12 To explain any observed heterogeneity by sex, unmeasured confounders would also have to be associated with sex (i.e., be a stronger confounder for one sex than the other). We note previous studies reporting sex-specific associations controlled for the factors listed above.10–12
We controlled for gestational age based on our DAG (Figure 2) assuming that preterm birth and caesarean share an unmeasured common cause (U) related to underlying fetal or maternal health. Preterm birth can alternatively be considered on the causal pathway between caesarean and asthma; under these latter conditions our results do not estimate the total effect of caesarean, but rather the effect of caesarean on asthma not mediated through preterm birth. This is consistent with previous studies which typically control for gestational age to focus on pathways between caesarean and asthma independent of gestational age.
We chose to conduct sex-stratified analyses to allow relationships between all variables to be modeled separately by sex and thus account for sex differences in confounding by measured covariates. As shown in a recent simulation by Buckley et al., when confounding is sex-dependent, the common approach of including a single product term between sex and exposure can yield biased estimates.24 Despite the apparent sex differences in magnitude of confounding, our sex-specific estimates from stratified models and our sex-specific estimates based on interaction models were ultimately very similar yielding the same conclusions.
One possible non-causal explanation for the association between caesarean delivery and asthma is uncontrolled confounding by treatment-seeking behavior (e.g. treatment-seeking behavior leads both to the decision to have a caesarean and a child asthma diagnosis). There is some evidence of differences in asthma severity and diagnosing by sex,15 and if treatment-seeking behavior was more common among parents of girls, this could lead to a stronger positive bias in the caesarean-asthma association among girls. Differences in disease misclassification by sex could also lead to apparent sex heterogeneity in this association. For example, greater disease misclassification among boys could lead to underestimation of the caesarean-asthma association for boys.
Strengths of the study
This study uses a mother-child linked cohort, estimates associations on both the additive and multiplicative scales, and uses medical records for asthma classification. Following the suggestion by Magnus and colleagues,10 we assessed the association between caesarean and asthma at several ages. Birth records were used to classify mode of delivery which is one of the more accurate birth record fields.25, 26 The meta-analysis of this study’s findings with those from the literature summarize the state of the knowledge on potential sex differences in the association between caesarean and asthma.
Limitations of the data
Due to missing mode of delivery data, 30.6% (n=7533) of the KAPPA cohort was excluded from this analysis. For the children whose data were missing because of the administrative management issue with the pulling of birth record data (n=1508, eFigure 1), we do not expect them to be systematically different than those retained on factors other than birth year.
Comparing children who were included and excluded from the analysis due to missing birth mode, asthma rates were similar, although this is insufficient evidence to rule out selection bias. Of children included in the analysis, there were minimal differences in caesarean proportion or earlier asthma diagnoses between children followed to age 6 and children who were not. Many of the children were not followed until the older ages due to censoring at the time of study completion (for example, children born in 2010 could be at most three years old when follow-up ended in 2013).
We could not determine whether caesarean deliveries were planned or emergency, which can be used to approximate whether caesareans occurred after labor or membrane rupture. If caesarean causes asthma due to the prevention of gut colonization by vaginal flora, one would expect to see a stronger association between caesarean and asthma in caesareans that do not involve membrane rupture. Future studies could assess how the type of caesarean impacts sex differences. Identifying children with asthma in early life is challenging and outcome measurement error is likely in our study.
The meta-analysis was limited to sex-specific results authors chose to report in their publications on caesarean and asthma. It is plausible that the sex-stratified results reported in the literature are not a random sample of sex-stratified results in all studies; some studies may have examined heterogeneity by sex but not reported such results if the estimates were similar between sexes. This potential for reporting bias could lead to the spurious appearance of effect modification by sex. Nonetheless, we believe it is unlikely that investigators who estimated sex-specific associations preferentially reported them only when estimates were higher for females.
Conclusions
Attempting to elucidate the potential link between caesarean delivery and asthma is an active area of research. Due to an emerging pattern of stronger associations among girls we encourage researchers to present results stratified by sex, regardless of their findings. Further study of sex differences in this association may advance our understanding of the nature of the association between caesarean delivery and asthma and shed light on sex differences in the etiology of asthma in early life.
Supplementary Material
Acknowledgements
The authors acknowledge funding from the National Institute of Allergy and Infectious Diseases (NIAID; R01AI122266) and thank Natalie Rosenquist for her assistance with the literature search for this manuscript.
References
- 1.Stokholm J, Thorsen J, Chawes BL, Schjorring S, Krogfelt KA, Bonnelykke K, et al. Cesarean section changes neonatal gut colonization. J Allergy Clin Immunol 2016; 138:881–889.e882. [DOI] [PubMed] [Google Scholar]
- 2.Björkstén B, Sepp E, Julge K, Voor T, Mikelsaar M. Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol 2001; 108:516–520. [DOI] [PubMed] [Google Scholar]
- 3.Zanardo V, Simbi AK, Franzoi M, Solda G, Salvadori A, Trevisanuto D. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr 2004; 93:643–647. [DOI] [PubMed] [Google Scholar]
- 4.Annibale DJ, Hulsey TC, Wagner CL, Southgate WM. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med 1995; 149:862–867. [DOI] [PubMed] [Google Scholar]
- 5.Ramachandrappa A, Jain L. Elective cesarean section: its impact on neonatal respiratory outcome. Clin Perinatol 2008; 35:373–393, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith GC, Wood AM, White IR, Pell JP, Cameron AD, Dobbie R. Neonatal respiratory morbidity at term and the risk of childhood asthma. Arch Dis Child 2004; 89:956–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disease: meta-analyses. Clin Exp Allergy 2008; 38:634–642. [DOI] [PubMed] [Google Scholar]
- 8.Thavagnanam S, Fleming J, Bromley A, Shields MD, Cardwell CR. A meta-analysis of the association between Caesarean section and childhood asthma. Clin Exp Allergy 2008; 38:629–633. [DOI] [PubMed] [Google Scholar]
- 9.Huang L, Chen Q, Zhao Y, Wang W, Fang F, Bao Y. Is elective cesarean section associated with a higher risk of asthma? A meta-analysis. J Asthma 2015; 52:16–25. [DOI] [PubMed] [Google Scholar]
- 10.Magnus MC, Haberg SE, Stigum H, Nafstad P, London SJ, Vangen S, et al. Delivery by Cesarean section and early childhood respiratory symptoms and disorders: the Norwegian mother and child cohort study. Am J Epidemiol 2011; 174:1275–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Menezes AM, Hallal PC, Matijasevich AM, Barros AJ, Horta BL, Araujo CL, et al. Caesarean sections and risk of wheezing in childhood and adolescence: data from two birth cohort studies in Brazil. Clin Exp Allergy 2011; 41:218–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Renz-Polster H, David MR, Buist AS, Vollmer WM, O’Connor EA, Frazier EA, et al. Caesarean section delivery and the risk of allergic disorders in childhood. Clin Exp Allergy 2005; 35:1466–1472. [DOI] [PubMed] [Google Scholar]
- 13.Werner A, Ramlau-Hansen CH, Jeppesen SK, Thulstrup AM, Olsen J. Caesarean delivery and risk of developing asthma in the offspring. Acta Paediatr 2007; 96:595–596. [DOI] [PubMed] [Google Scholar]
- 14.Fleiss JL. The Design and Analysis of Clinical Experiments NY: Wiley and Sons; 1986. [Google Scholar]
- 15.Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy 2008; 63:47–57. [DOI] [PubMed] [Google Scholar]
- 16.Shrier I, Steele R. Understanding the relationship between risks and odds ratios. Clin J Sport Med 2006; 16:107–110. [DOI] [PubMed] [Google Scholar]
- 17.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braback L, Ekeus C, Lowe AJ, Hjern A. Confounding with familial determinants affects the association between mode of delivery and childhood asthma medication - a national cohort study. Allergy Asthma Clin Immunol 2013; 9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Postma DS. Gender differences in asthma development and progression. Gend Med 2007; 4 Suppl B:S133–146. [DOI] [PubMed]
- 20.Carey MA, Card JW, Voltz JW, Arbes SJ Jr., Germolec DR, Korach KS, et al. It’s all about sex: gender, lung development and lung disease. Trends Endocrinol Metab 2007; 18:308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kynyk JA, Mastronarde JG, McCallister JW. Asthma, the sex difference. Curr Opin Pulm Med 2011; 17:6–11. [DOI] [PubMed] [Google Scholar]
- 22.Mandhane PJ, Greene JM, Cowan JO, Taylor DR, Sears MR. Sex differences in factors associated with childhood- and adolescent-onset wheeze. Am J Respir Crit Care Med 2005; 172:45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenblatt R, Mansour O, Zhao E, Ross M, Himes BE. Gender-specific determinants of asthma among U.S. adults. Asthma Res Pract 2017; 3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buckley JP, Doherty BT, Keil AP, Engel SM. Statistical approaches for estimating sex-specific effects in endocrine disruptors research. Environ Health Perspect 2017; 125:067013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE. Reliability of birth certificate data: a multi-hospital comparison to medical records information. Matern Child Health J 2002; 6:169–179. [DOI] [PubMed] [Google Scholar]
- 26.Zollinger TW, Przybylski MJ, Gamache RE. Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol 2006; 16:1–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


