Abstract
Although calls for intervention designs are numerous within the organizational literature and increasing efforts are being made to conduct rigorous randomized controlled trials, existing studies have rarely evaluated the long-term sustainability of workplace health intervention outcomes, or mechanisms of this process. This is especially the case with regard to objective and subjective sleep outcomes. We hypothesized that a work-family intervention would increase both self-report and objective actigraphic measures of sleep quantity and sleep quality at 6-months and 18-months post-baseline in a sample of information technology workers from a US Fortune 500 company. Significant intervention effects were found on objective actigraphic total sleep time and self-reported sleep insufficiency at the 6-month and 18-month follow-up, with no significant decay occurring over time. However, no significant intervention effects were found for objective actigraphic wake after sleep onset or self-reported insomnia symptoms. A significant indirect effect was found for the effect of the intervention on objective actigraphic total sleep time through the proximal intervention target of 6-month control over work schedule and subsequent more distal 12-month family time adequacy. These results highlight the value of long-term occupational health intervention research, while also highlighting the utility of this work-family intervention with respect to some aspects of sleep.
Keywords: intervention sustainability, sleep, conservation of resources theory, control over work schedule, family time adequacy
The topic of sleep has received increased interest in organizational and management sciences (e.g., Barnes, 2012; Barnes, Miller, & Bostock, 2017). This energetic area of research has resulted in the development of new sleep theories (Barnes, 2012; Barnes, Jiang, & Lepak, 2016; Mullins, Cortina, Drake, & Dalal, 2014) and an improved understanding of associations among sleep and work-related constructs (e.g., Crain et al., 2014; Wagner, Barnes, Lim, & Ferris, 2012; Welsh, Ellis, Christian, & Mai, 2014). Notably, a number of recent studies have found relations between work-family experiences and sleep outcomes (e.g., Allen & Kiburz, 2011; Crain et al., 2014; Barnes, Wagner, & Ghumman, 2012), suggesting that work-family experiences are an important target for future intervention studies.
Recently, the Work, Family, & Health Study (Bray et al., 2013; King et al., 2012) tested a work-family intervention within a randomized controlled trial design. Employee control over work schedule and family-supportive supervisor behaviors (FSSB) were both included as primary intervention targets. Kossek, Hammer, Kelly, and Moen (2014) describe the intervention design in detail. Results indicate that the intervention improves control over work time, FSSB, work-family conflict, subjective well-being, and family time adequacy (Kelly et al., 2014; Moen et al, 2016), while also increasing daily shared time by parents and children (Davis et al., 2015), and sleep of employees’ children (McHale et al., 2015). This intervention also protected against decreases in safety compliance and organizational citizenship behaviors (Hammer et al., 2016). Kossek et al. (in press) also find that the same intervention implemented in a healthcare setting improved psychological health for employees who were also caring for an aging relative, had child care responsibilities, or who were “sandwiched” and caring for both children and aging relatives, although these results varied across 6-, 12-, and 18-month follow-ups. Other work has found that this intervention results in a significant, positive return on investment (Barbosa et al., 2015). Of special relevance to the current work, a study conducted by Olson et al. (2015) evaluated the intervention effects at the 12-month time point on self-reported and objective sleep within a sample of information technology workers. They found that the intervention improved employee objectively-measured total sleep time and self-reported sleep insufficiency. Furthermore, the intervention affected sleep insufficiency at 12-months partially via increases in 6-month control over work schedule and associated reductions in work-to-family conflict (WTFC).
We argue that Olson et al.’s (2015) work can be further expanded upon to better inform future intervention research by evaluating the sustainability and mechanisms of the intervention effects at two additional time points. August, Bloomquist, Lee, Realmuto, and Hektner (2006) suggest that “sustainability is a multifaceted concept that encompasses diverse perspectives on a program’s long-term viability” (p. 151). In the current investigation, we focus on the sustainability of intervention effects following implementation.
We note three specific contributions of this work. First, although Olson et al. (2015) found significant intervention effects, it is not known whether sustainability is present before or after the 12-month follow-up. Providing evidence of long-term sustainability is critical for persuading organizational decision-makers to adopt such an intervention and informing future research that aims to further refine this promising intervention. Second, we evaluate new mediators, as Olson et al. (2015) found evidence of only partial mediation through control over work schedule and WTFC at 6 months, suggesting that other constructs may be contributing intervention effects on sleep outcomes. Lastly, while it was a strength of Olson et al.’s (2015) study that proximal mediators (i.e., immediate intervention effects) and distal mediators (i.e., subsequent intervention effects) were conceptualized and tested (i.e., control over work hours and WTFC, respectively), both variables were analyzed simultaneously at the 6-month time point. Although mediation analysis can be conducted with cross-sectional as well as longitudinal data, mediation analyses based on longitudinal data are superior, given concerns around common method bias (e.g., Maxwell & Cole, 2007).
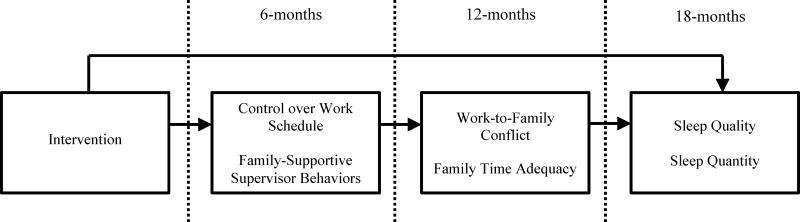
The current study evaluates intervention effects on objective and self-reported sleep outcomes at the 6-month, 12-month, and 18-month follow-ups, while a test of intervention effect sustainability from 6 to 18 months and 12 to 18 months is also conducted. We also examine how proximal intervention targets at the 6-month time point (schedule control and FSSB) and more distal work-family factors at 12-months (WTFC and family time adequacy) relate to sustained improvements in sleep outcomes at 18 months. The proposed theoretical model can be seen in Figure 1.
Figure 1.
Theoretical model.
In line with recommendations from Allen and Martin (2017), Barnes (2012), and Crain, Brossoit, and Fisher (in press), we include objective and subjective aspects of both sleep quantity and sleep quality in our study. Sleep quantity refers to the duration of time spent sleeping (i.e., objective total sleep time). Sleep quality, on the other hand, is multi-faceted as it consists of time spent awake during the sleeping period (i.e., objective wake after sleep onset [WASO]), an overall evaluation of the sufficiency of one’s sleep (i.e., self-report sleep insufficiency), and difficulty initiating or maintaining sleep throughout the night (i.e., self-report insomnia symptoms). As described by a number of sleep scholars (e.g., Barnes, 2012; Crain, Brossoit, and Fisher, in press), there is a need to include both measures of sleep quality and sleep quantity; although related, they are empirically and theoretically distinct constructs that may relate differentially to antecedents. Interestingly, both actigraphically-measured “objective” and subjective reports of sleep also often do not correspond for a variety of measurement reasons (e.g., Matthews et al., 2018; Sadeh, 2011), however, they are both important. This is especially true since most clinical interactions and workplace intervention implementations are based on subjective reports for reasons related to cost, absence of technical actigraphy knowledge, and feasibility within study design, and thus objective actigraphy provides measures less affected by common method bias and low-resolution categorical measures. However, some aspects of sleep quality, like sleep insufficiency, cannot be measured through objective means; the focus of such measures is on how the participant feels and whether they perceive their sleep to be adequate. As such, we include both objective and self-report measures because a) objective measurement of sleep acts as a validity check against more commonly used self-report scales, and b) so that multiple sleep quantity and quality constructs can be assessed, providing a more holistic understanding of how the intervention impacts sleep.
Increasing and Sustaining Work-Family Resources
Conservation of Resources Theory
The present study utilizes conservation of resources (COR; Hobfoll, 1989) theory. Hobfoll’s (1989) COR framework generally posits that strain results from investing resources, the threat of losing resources, or a lack of resource replenishment after resource investment. Halbesleben, Neveu, Pastian-Underdahl, and Westman (2014) have more recently proposed that resources are “anything perceived by the individual to help attain his or her goals” (p. 1338). Hobfoll and Shirom (2000) have suggested that work-family stressors, specifically, deplete resources. We focus specifically on the resources of control over work schedule and FSSB.
Sleep as a sustained health outcome of the intervention
A growing literature has established relations between resources, like job control and social support, in relation to sleep (e.g., De Lange et al., 2009; Magnusson Hanson et al., 2011). However, only a few studies to date have explicitly examined associations among control over work hours, FSSB, and sleep. For example, Crain et al. (2014) found that FSSB, work-to-family conflict, and family-to-work conflict, when examined as a block of predictors, are significantly related to objective sleep duration and self-reported sleep quality (e.g., insomnia symptoms). Individuals with more control over work hours and control over days off also report fewer insomnia symptoms, especially for men and daytime workers versus women and shiftworkers, respectively (Takahashi, Iwasaki, Saseki, Kubo, Mori, & Otsuka, 2011).
Regarding previous workplace intervention research aiming to improve employee sleep, a number of approaches have been taken. Some studies have adopted an individual-level approach whereby employees are trained on cognitive behavioral therapy for insomnia (CBT-I; Barnes et al., 2017; Thiart et al., 2016), or aspects of CBT-I plus recovery from work-related techniques (e.g., Ebert et al., 2015; Thiart, Ebert, Berking, & Riper, 2015). Mindfulness training has also been targeted in the workplace in order to improve sleep (Crain, Schonert-Reichl, & Roeser, 2017; Hulsheger, Feinholdt, & Nubold, 2015). Other recent intervention work has involved providing soldiers with individualized feedback on their sleep history, as measured objectively by actigraphy (Adler, Gunia, Bliese, Kim, & LoPresti, 2017).
In contrast to these intervention studies targeting employee behaviors, other sleep intervention work focuses on aspects of the work environment that can be changed, similar to the current study’s intervention. Van Laethem et al.’s (2013) review of organizational-level interventions highlights a number of studies that have sought to address work characteristics in an attempt to improve sleep, although the majority of these studies were not rigorous in nature. No intervention effects were found for two other studies not captured by Van Laethem and colleagues (2013). First, Garde, Nabe-Nielsen, and Aust (2011) did not find effects of an intervention designed to increase control over work time on self-reported sleep quality in a sample of healthcare workers, but the study authors note that the intervention was not implemented well across all employees. Second, Eriksen and Kecklund (2007) also did not find effects of an intervention designed to allow police officers to choose their work shifts on sleep quality, although police officers in the intervention group did experience longer sleep durations after morning and evening shifts. Just one of the intervention studies included in the review, however, specifically targeted work-family strain as a key lever for improving sleep (i.e., Moen, Kelly, Tranby, & Huang, 2011) in a natural experiment. The authors found that by increasing employees’ control over their working time, employees reported almost an extra hour of sleep on nights before work, 6 months after an intervention targeting control over work time was implemented.
Drawing on Hobfoll’s (1989) framework and prior empirical work, we argue that by targeting control over work schedule and FSSB as resources, the present intervention is likely to improve both objective and subjective measures of sleep quantity and sleep quality facets. These intervention resources should allow employees to obtain adequate sleep duration, while also decreasing employee strain that impacts sleep quality.
Hypothesis 1: The intervention will improve sleep quantity (i.e., increase objective total sleep time) and sleep quality (i.e., reduce objective WASO, subjective sleep insufficiency, and subjective insomnia symptoms) at the 6-month and 18-month follow-up data collections relative to baseline.
We expect that no decay in these intervention effects should occur, given that the intervention in question targeted the organizational-level and was focused on permanently improving supervisor behavior while also redesigning work in such a way that control over schedules would be lasting. As the COR framework proposes (Halbesleben et al., 2014; Hobfoll, 1989), individuals with access to resources are more likely to gain additional resources over time and maintain levels of heightened functioning and an ability to manage work and family boundaries, thereby leading to improved and sustained sleep over time.
COR Theory (Hobfoll, 1989) also generally suggests that individuals with resources are likely to acquire more resources over time, leading to gain spirals (e.g., Hobfoll, 1989). Thus, with the addition of resources provided by the WFHS intervention, we might expect increases in sleep quantity and quality 6 months beyond the previously evaluated 12-month time point. However, meta-analytic evidence suggests that lagged effects of stressors on physical strains do not tend to increase over time, in contrast to lagged effects of stressors on psychological strain, which tend to increase over time, peak, and then decrease (Ford, Matthews, Wooldridge, Mishra, Kakar, & Strahan, 2014). Although COR theory would suggest that sleep quantity and quality might improve over an additional 6 months in our intervention study, this empirical work on physical strains suggests that the intervention effects may be sustained over time, given that these effects tend to be small and difficult to detect. As we are interested in the effect of increasing workplace resources and decreasing workplace stressors on the physical outcome of sleep rather than a psychological outcome, we draw on Ford et al.’s (2014) findings and propose that sleep quantity and quality will be sustained over time, rather than being furthered improved within our given time frame. However, inferential statistical tests do not provide evidence for the null hypothesis, and thus hypothesizing no change in sleep outcomes between the 6-month and 18-month and the 12-month and 18-month time point would be inappropriate. As such, we offer the following as a research question, with the intention of investigating the intervention’s long term effects on sleep outcomes:
Research Question 1: Will the intervention’s effect on sleep be maintained between the 6- to 18-month follow-up time points and the 12- to the 18-month follow-up time points?
Additional mediators of intervention effects on sleep outcomes
King et al. (2012) proposed a theoretical model suggesting that a work-family intervention seeking to provide employees with the additional resources of control over work schedule and FSSB (i.e., proximal mediators), should decrease WTFC and family time adequacy (i.e., distal mediators) and ultimately improve sleep.
Control over work schedule and FSSB as proximal mediators
In line with Kelly and Moen (2007), our conceptualization of control over work schedule is specifically concerning one’s control over when and where they conduct their work. Broader reviews of the worktime control literature suggest that while there is evidence for worktime control being correlated with work-family variables, findings are generally inconsistent with regard to health and well-being outcomes (Nijp, Beckers, Geurts, Tucker, & Kompier, 2012). Control over work schedule is likely to act as a resource that subsequently improves sleep by providing employees with more flexibility to determine when and where they work. With increased control over work schedule, employees are more likely to find enough time to attend to family demands, thereby leaving more time for sleep and less motivation to borrow time from sleep in order to meet family demands. Indeed, a recent study indicated that individuals who experienced a greater mismatch between their needs for worktime control and their experienced worktime control were more likely to also experience WTFC and fatigue (Nijp, Beckers, Kompier, van den Bossche & Guerts, 2015). Other work indicates a beneficial impact on depressive symptoms (Kossek et al., 2006). Additionally, with greater control over how one allocates time over the day and week, employees will perceive the environment to be less threatening, experience less strain, and consequently experience better sleep quality.
Family-supportive supervisors empathize with an employee’s efforts to seek balance between work and family domains and similarly understand their desire to adequately fulfill both sets of roles (Hammer, Kossek, Yragui, Bodner, & Hanson, 2009; Thomas & Ganster, 1995). Previous research offers evidence for the direct effect of supportive supervisors on employee sleep (e.g., Berkman et al., 2010; Sorenson et al., 2011). Supervisors who are supportive provide resources necessary to manage both work and family demands. This in turn should allow employees who are able to manage work and family demands to be more likely to find adequate amounts of time to obtain sufficient sleep duration. Additionally, employees should experience better sleep quality because the environment is less pressured.
WTFC and family time adequacy distal mediators
WTFC has been defined as a form of inter-role tension where the demands of the work role are incompatible with the demands of the non-work role (Greenhaus & Beutell, 1985). We focus on the work-to-family direction of this construct, given our theoretical model examines how work-related resources can positively influence family and personal experiences. Previous studies have found a cross-sectional relationship between work-family conflict and sleep-related outcomes, including aspects of quantity (Crain et al., 2014) and sleep quality (Crain et al., 2014; Lallukka et al., 2010; Nylen, Melin, & Laflamme, 2007; Sekine et al., 2006). Other longitudinal studies indicate that decreases in WTFC are associated with increases in perceptions of adequate time for healthy sleep (Moen, Fan, & Kelly, 2013). Moreover, reductions in WTFC have resulted in longer sleep durations for individuals within intervention contexts (Moen et al., 2011).
According to Van Horn, Bellis, and Snyder (2001), family time adequacy refers to an individual’s evaluation of their available time resources that can be allotted to family members, including children, parents, and spouses. Previous research has found a positive association between FSSB and family time adequacy (Hammer, Kossek, Bodner, & Crain, 2013). To our knowledge, there are no studies that have linked family time adequacy with sleep outcomes. We propose that with greater perceived time resources for family, employees will experience improved sleep quantity and quality. Importantly, with increased family time adequacy, employees are less likely to need to borrow time from sleep in order care for family members.
Hypothesis 2: The intervention will improve 18-month sleep quantity (i.e., increase objective total sleep time) and sleep quality (i.e., reduce objective WASO, reduce subjective sleep insufficiency, and reduce subjective insomnia symptoms) relative to baseline through increased 6-month control over work schedule and FSSB that decreases subsequent 12-month WTFC and increases family time adequacy.
Methods
Participants and Procedures
The present investigation uses baseline, 6-month, 12-month, and 18-month data from a sample of employees located in teams within the information technology division of a large Fortune 500 information technology firm labeled with the pseudonym TOMO. To be eligible for the study, individuals had to be non-contract employees and located in one of the two cities where data collection took place. Table 1 shows the means and standard deviations of key participant characteristics across both conditions.
Table 1.
Mean (SD) and Percentage of Demographic Characteristics by Condition (N = 823)
| Usual Practice
|
Intervention
|
|
|---|---|---|
| Female | 37.9% | 42.3% |
| Age | 46.6 (8.4) | 46.9 (8.8) |
| Race/Ethnicity | ||
| White, Non-Hispanic | 72.1% | 70.7% |
| Black or African American, Non-Hispanic | 1.3% | 2.4% |
| Asian Indian | 13.8% | 11.8% |
| Other Asian | 4.2% | 4.9% |
| Other Pacific Islander | 0.8% | 1.2% |
| Hispanic | 6.7% | 8.1% |
| More Than One Race | 1.3% | 0.1% |
| Married or Living with Partner | 79.2% | 80.1% |
| Number of children | 1.0 (1.2) | 1.0 (.95) |
| Elder Care | 25.8% | 24.4% |
| Education | ||
| High School Graduate | 2.5% | 2.8% |
| Some College or Technical School | 17.9% | 22.4% |
| College Graduate | 79.6% | 78.4% |
| Hours worked per week Shift | 45.5 (6.0) | 45.6 (5.4) |
| Variable Schedule | 21.3% | 21.1% |
| Regular Daytime | 77.9% | 78.0% |
| Rotating | 0.4% | 0.8% |
| Split Shift | 0.4% | 0.0% |
Following baseline data collection, the intervention was implemented, being rolled out as a company-sponsored pilot program. In collaboration with company representatives, the researchers identified 56 study groups, each comprised either of individuals who reported to the same manager or multiple teams of individuals who worked collaboratively on common projects. An adaptive random assignment approach (Frane, 1998) was then used to assign study groups to either the usual practice or intervention condition (see Bray et al., 2013 for a detailed description of this methodology). The usual practice and intervention conditions were balanced on job function, the vice president study groups reported to, and number of employees in each of the two geographic regions home to the worksites.
Overview of the Intervention
The intervention designed and tested in this study, was comprised of two components: 1) facilitated training sessions with supervisors and employees that were participatory in nature aimed at identifying new work practices and processes that would increase employees’ control over work schedule, thereby shifting the performance focus to results rather than face time (adapted from Kelly et al., 2011; Moen et al., 2011; 2013), and 2) supervisor training and behavior tracking aimed at increasing supervisor support for employees’ family and non-work lives (adapted from Hammer et al., 2011). These two intervention components were adapted and customized for the information technology industry and this particular study through formative research. Data were collected using job shadowing, interviews with managers, and employee focus groups. Researchers also drew on notes from meetings with community partners to inform the customization. Based on this formative data collection, the final integrated intervention was tested in two industries, long-term healthcare and information technology. For the purposes of this paper, we focus solely on the information technology sample across four waves of data collection.
One part of the intervention involved employees and managers attending a series of facilitated participatory training sessions. Two different types of sessions were held: those for supervisors only and those for supervisors and employees jointly. In both sets of sessions, facilitators from an organizational development company, delivered face-to-face sessions. In the supervisor only sessions, the facilitators introduced leaders to the intervention, provided guidance on how to help transition employees to having full control over their work time, and created opportunities for managers to discuss their support for employees’ family demands. Within the supervisor and employee sessions, facilitators provided background on the intervention, led discussions around current workplace practices and policies, in addition to discussions around novel ways of working that could increase employee control over work schedule and support for others’ work performance and personal lives.
Managers within the intervention condition attended a two-hour long facilitated training session, which introduced them to the intervention. This was followed by a self-guided, hour-long computer-based training using cTRAIN software (Northwest Education Training and Assessment, Lake Oswego, OR; http://www.nweta.com; Anger, Rohlman, Kirkpatrick, Reed, Lundeen, & Eckerman, 2001). The training provided managers with information on the importance of decreasing employees’ work-family conflict and increasing supervisor support for non-work life, in addition to explaining why such efforts would be beneficial for both employees and the organization. Specific examples of how managers could engage in such support were also included in the training. Managers were then asked to set goals for exhibiting support to employees and were asked to carry an iPod Touch device over the next two weeks to log their supportive behaviors using an Enterprise Application (HabiTrack, OHSU, Portland, OR). Daily alarms on the devices reminded managers to self-monitor their supportive behaviors, and after the experience, each person was provided with personalized feedback on their behaviors relative to their individual goals and group averages. Supervisors completed two two-week bouts of behaviors tracking during the intervention period. Lastly, managers participated in a facilitated training session at the end of the initiative that allowed them to share their successes and to ask questions of the facilitators and other managers. Additional information on the intervention and all downloadable intervention materials can be found online (www.WorkFamilyHealthNetwork.org).
Data Collection
Data collections took place within the workplace on paid company time. At each of the four waves of data collection, trained field interviewers administered face-to-face computer-assisted personal interviews (CAPI) with employees, obtaining demographic, workplace, family, and health information, including self-report sleep data. These interviews lasted 60 minutes at the worksite and all employees were compensated with a $20 incentive per wave.
Immediately following the CAPI, interviewers introduced the actigraphy data collection process in order to collect objective sleep data. Participation resulted in an additional $20 incentive per wave. If the participant agreed, the interviewer provided them with and instructed them to wear a sleep monitor (Spectrum, Respironics-Philips, Murrysville, PA) on their non-dominant wrist at all times for the next week except in situations where the watch could be damaged (e.g., excessive impact, extreme temperatures).
Measures
In the following sections, we describe the organizational, family, and sleep measures used in the current study. Mean imputation of missing scores was utilized for all scales with four or more items when at least 75% of the data were present. Otherwise, listwise deletion was employed to construct scale scores. There was very little missing data across the items within a scale for the sample, ranging from 1-8%. Although all variables were collected at each of the four waves, control over work schedule and FSSB were assessed at baseline and 6 months, while WTFC and family time adequacy were assessed at baseline and 12 months to evaluate hypothesis 2. Self-report and objective sleep variables were also assessed at all waves. Selection of proximal and distal mediators at certain time points was based on our theoretical rationale; FSSB and schedule control between baseline and 6 months was assessed in order to evaluate immediate perceptions of intervention change effects since the intervention was delivered between baseline and 6 months, followed by the assessment of work-family conflict and time adequacy between baseline and 12 months to show the lagged effects on perceptions of work-family stress.
Control over work schedule
Control over work schedule assessed the degree to which employees perceive they have control over their work time using an eight-item scale based on Thomas and Ganster’s (1995) measure. A sample question is “How much choice do you have over when you begin and end each workday?” with responses ranging from 1 (Very little) to 5 (Very much) (α = .80–.83).
Family-supportive supervisor behavior (FSSB)
FSSB was assessed as employee perceptions of supervisors’ behavioral support for family and personal life. We used Hammer and colleagues’ (2013) four-item short form measure. Responses range from 1 (Strongly disagree) to 5 (Strongly agree), and a sample item is “Your supervisor works effectively with employees to creatively solve conflicts between work and non-work” (α = .88–.92).
Work-to-family conflict (WTFC)
WTFC, reflecting the degree to which work role responsibilities are incompatible with family role responsibilities, was assessed using a five item scale developed and validated by Netemeyer, Boles, and McMurrian (1996). A sample item is “Due to your work-related duties, you have to make changes to your plans for family or personal activities.” Item responses ranged from 1 (Strongly disagree) to 5 (Strongly agree) (α = .91–.92).
Family time adequacy
Family time adequacy assessed employees’ perceptions of available time resources for family members, including children, spouses, and parents (Van Horn et al., 2001) with a two item scale. A sample item is “To what extent is there enough time to be with your children?” and response options ranged from 1 (Never) to 5 (All of the Time), with higher values representing more time resources for family (α = .37–.57).
Objective sleep quantity and quality
Actigraphy represents a reliable and valid objective measure of sleep not used for the diagnosis of sleep disorders (Ancoli-Israel et al., 2003; Marino et al., 2013). Sleep monitor actigraphs are wrist-watch size devices that contain an accelerometer, continuously measuring movement as a proxy for waking activity (Ancoli-Israel et al., 2003; Barnes, 2012). In line with Crain et al. (2014) and Olson et al. (2015), we used Philips-Respironics’ Actiwatch Spectrum devices and procedures for double-scoring with experienced actigraphy scorers using Respironics Actiware sleep scoring program version 5.61. A recording was scored as invalid if there was a device malfunction and constant false activity was seen in the recording or if the actigraphy data could not be retrieved from the device. Specific days within the recording could also be labeled as invalid if a watch error occurred, such as a failing battery, or if the participant did not comply with the study’s actigraphic procedures (i.e., greater than four hours of actiwatch off-wrist time throughout the day, or an off-wrist period greater than 60 min within 10 min of the determined beginning or end of the main time in bed period for that day). Participants’ actigraphy records were only included in the analysis if they had three or more valid days of actigraphy data, suggested by Olson et al. (2015) to be a reliable number of days. For more detailed accounts of our validated actigraphy scoring procedure, please see Marino et al. (2013).
Actigraphic total sleep time
Actigraphic total sleep time, or objectively-measured quantity, can be derived from actigraphic periods of less frequent movement, indicating sleep, throughout a 24-hour period. Marino et al. (2013) found that a particular strength of actigraphy is that it has high sensitivity, in terms of an ability to correctly assign epochs of sleep time.
In the current study, the initial total sleep time measurement was the total number of epochs determined to be sleep multiplied by the set epoch length (30 seconds). These initial values for total sleep time were further modified to account for the total number of valid days. Actigraphic total sleep time was computed as the average amount of sleep attained per day in minutes (including naps). Thus, the total amount of time scored as sleep over the course of the study was divided by the total number of valid days.
Actigraphic wake after sleep onset (WASO)
Actigraphic WASO refers to the average amount of time spent awake per sleeping period, as evidenced by actigraphically-measured wrist movement patterns. Previous research validating actigraphy against polysomnography, the gold standard of sleep measurement involving surface electrodes, indicates that actigraphy estimates have high accuracy (Marino et al., 2013). However, although WASO estimates are unbiased when wake time is less than 30 minutes during the night, this same validation study also showed that actigraphy tends to overestimate WASO if true wake time during the night is greater than 30 minutes. We note this limitation of actigraphy here, as it is specific to the measurement of WASO.
In this study, the initial WASO measurement was the total number of epochs determined to be wake multiplied by the set epoch length (30 seconds). The initial value for WASO was further modified to account for the total number of valid days, in order to obtain a more accurate WASO value. Thus, WASO was computed as the average amount of time spent waking during nightly sleep in minutes, with the total amount of time scored as wake time being divided by the total number of valid days.
Self-reported sleep quality
In addition to objective measures of sleep, two measures of sleep quality were assessed: sleep insufficiency and insomnia symptoms.
Self-reported sleep insufficiency
Sleep insufficiency, a measure of poor sleep quality, was measured using one item (Buxton et al., 2009; Buxton et al., 2012; Centers for Disease Control, 2011). As a measure of sleep insufficiency, participants were asked, “How often during the past four weeks did you get enough sleep to feel rested upon waking up?” Items were rated on a scale from 1 (never) to 5 (very often). After reverse scoring, higher scores indicated greater sleep insufficiency.
Self-reported insomnia symptoms
Insomnia symptoms, another measure of poor sleep quality, were captured using two items from the PSQI (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). Participants were asked, “During the past four weeks, how often could you not get to sleep within 30 minutes?” and “During the past four weeks, how often did you wake up in the middle of the night or early morning?” Items were rated on a scale from 1 (never) to 4 (three or more times a week), with higher scores indicating more frequent insomnia symptoms. The two scores were then averaged for an overall insomnia symptoms score.
Analytic Strategy
Intervention effect analyses with sleep outcomes were conducted in SAS Proc Mixed (Version 9.3) with restricted maximum likelihood estimation, using a three-level general linear mixed model approach for cluster-randomized designs (Donner & Klar, 2004; Murray, Varnell, & Blitstein, 2004; Varnell, Murray, Janega, & Blitstein, 2004). All analyses were conducted within an intent-to-treat framework. Within these three-level models, time waves (Baseline, 6-month follow-up, 12-month follow-up, 18-month follow-up) were nested within participants and participants were nested within workgroups. ICCs at the workgroup level ranged from 0 to .05, while ICCs at the individual level ranged from .54-.67, depending on the outcome. The statistical model used (as seen in Table 4) is analogous to a general linear mixed model parameterization of a 2 by 4 ANOVA with workgroup-level random effects. In this conceptualization, condition (i.e., intervention versus usual practice) is crossed with time (i.e., baseline, 6-months, 12-months, 18-months). Thus, the eight condition by time means can be derived from the fixed effect model parameters that are shown in Table 2. The model’s parameterization included treating time wave as a categorical variable, such that the 6-month follow-up was contrasted with baseline, the 12-month follow-up was contrasted with baseline, and the 18-month follow-up was contrasted with baseline. The outcomes (total sleep time, WASO, sleep insufficiency, and insomnia symptoms) were regressed on the treatment indicator, the follow-up wave indicators, and the treatment-by-wave interaction terms. In these models, the primary parameters of interest are the interactions between follow-up time waves and the treatment indicator (see e.g., Bodner & Bliese, 2017), which represent the differential mean change in an outcome across time and intervention conditions (i.e., the treatment effect). A statistically significant treatment-by-wave interaction for each of the four sleep outcomes would confirm hypothesis 1, or that sleep quantity and quality would be improved at the 18-month time point.
Table 2.
Means by Condition Over Time
| Condition | Baseline | 6-months | 12-months | 18-months | |
|---|---|---|---|---|---|
| Mediator | |||||
|
| |||||
| Control Over Work Hours (1-5 rating) |
Usual Practice | 3.64 | 3.68 | 3.70 | 3.69 |
| Intervention | 3.56 | 3.83 | 3.80 | 3.80 | |
|
|
|||||
| FSSB (1-5 rating) |
Usual Practice | 3.84 | 3.93 | 3.79 | 3.77 |
| Intervention | 3.90 | 3.95 | 3.94 | 3.98 | |
|
|
|||||
| Work-to-Family Conflict (1-5 rating) |
Usual Practice | 2.99 | 2.89 | 2.87 | 2.84 |
| Intervention | 3.14 | 2.92 | 2.91 | 2.84 | |
|
|
|||||
| Family Time Adequacy (1-5 rating) |
Usual Practice | 3.40 | 3.50 | 3.39 | 3.37 |
| Intervention | 3.32 | 3.42 | 3.44 | 3.45 | |
|
| |||||
| Sleep Outcome | |||||
|
| |||||
| Actigraphic Total Sleep Time (mins) |
Usual Practice | 440.06 | 449.18 | 441.87 | 440.58 |
| Intervention | 429.55 | 440.49 | 434.44 | 443.39 | |
|
|
|||||
| Actigraphic WASO (mins) |
Usual Practice | 43.70 | 44.85 | 45.86 | 45.76 |
| Intervention | 44.14 | 47.45 | 43.27 | 47.45 | |
|
|
|||||
| Sleep Insufficiency (1-5 rating) |
Usual Practice | 2.81 | 2.64 | 2.80 | 2.71 |
| Intervention | 2.86 | 2.69 | 2.62 | 2.57 | |
|
|
|||||
| Insomnia Symptoms (1-4 rating) |
Usual Practice | 2.71 | 2.77 | 2.65 | 2.65 |
| Intervention | 2.69 | 2.70 | 2.63 | 2.70 | |
Notes: Adjusted means derived from general linear mixed model analysis results.
To test research question 1, we utilized this same analytical framework but selected only first for 6-month and 18-month data and then only for 12-month and 18-month data, in order to determine if the intervention effect was sustained. The primary parameter of interest is still the treatment-by-wave interaction term, which now represents the differential mean change in sleep from 6-months to 18-months and 12-months to 18-months, ignoring baseline data, across intervention conditions. As we expand upon in more detail in the results section, we evaluate whether no significant change (i.e., sustainability) is evidenced by determining if a criterion threshold value in the unstandardized mean difference effect size metric is contained within the confidence interval for each treatment-by-wave interaction term. If the confidence interval did contain this value, then we concluded that there is no substantial relevant change in effects over time.
To test hypothesis 2 that the intervention would improve 18-month sleep quantity and quality through 6-month change in control over work schedule and FSSB and subsequent 12-month change in WTFC and family time adequacy, difference scores were first computed for 6- and 12-month mediators (i.e., 6-month minus baseline scores, 12-month minus baseline scores). Next, multilevel structural equation modeling techniques were then employed using Mplus (Version 6.0) in order to evaluate the intervention’s effect on 18-month outcome difference scores through 6 and 12-month mediator difference scores (for a description of difference score use, see MacKinnon, 2008, Chapter 8). A fully-saturated model was specified with all study variables included. Hypothesis 2 would be confirmed if significant conditional indirect effects were found for the pathway from intervention to sleep outcomes through the 6- and 12-month mediators.
All analyses conducted for testing both intervention and mediation effects controlled for the number of employees used for randomization and the core function, a variable identifying groups where most individuals were involved with software development versus groups dominated by other information technology jobs. Additionally, the organization experienced a merger during the course of the study. Whether the merger was announced before or after baseline data collection was also controlled.
Results
Self-report data were collected at baseline (n = 823), 6-months (n = 701), 12-months (n = 701), and 18-months (n = 651). At baseline, 618 of these individuals provided a minimum of three valid days of actigraphy data (intervention = 313, usual practice = 305), while 557 provided a minimum of three valid days of actigraphy data at 6 months (270 = intervention, usual practice = 287). At 12 months, 474 individuals provided three or more days of valid actigraphy data (intervention = 234, usual practice = 240). At 18-months, 397 individuals provided three or more valid days of actigraphy data (intervention = 193, usual practice = 204). Analyses excluded 16 individuals who were part of a workgroup that was randomized to the intervention but never invited to intervention activities by error. Additionally, eight individuals were excluded from the analyses because they did not have valid randomization variables, including the number of employees used for randomization and the core function. In order to ensure that both objective and self-report samples are equivalent, we restrict our self-report analyses to the same sample of individuals who also provide valid actigraphy data. The final sample size used in the analyses was 791, which captures all individuals who did not have missing data on the predictors and control variables at baseline.
The model-based means for each time point across intervention and usual practice conditions can be found in Table 2. Descriptive statistics and bivariate correlations for all study variables are presented in Table 3.
Table 3.
Descriptives and Correlations of Study Variables
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Treatment | 0.51 | 0.50 | – | |||||||||||||||||||
| 2. 6m Control over work schedule | 3.76 | 0.67 | 0.09* | – | ||||||||||||||||||
| 3. 6m Family-Supportive Supervisor Behaviors | 3.86 | 0.77 | 0.06 | 0.40* | – | |||||||||||||||||
| 4. 12m Work-to-Family Conflict | 2.93 | 0.91 | −0.04 | −0.43* | −0.28* | – | ||||||||||||||||
| 5. 12m Family Time Adequacy | 3.43 | 0.68 | 0.00 | 0.31* | 0.19* | −0.46* | – | |||||||||||||||
| 6. Baseline Actigraphic Total Sleep Time | 435.10 | 53.39 | −0.08* | 0.01 | 0.00 | −0.04 | 0.02 | – | ||||||||||||||
| 7. 6m Actigraphic Total Sleep Time | 442.31 | 53.12 | 0.02 | 0.06 | 0.03 | −0.14* | 0.08 | 0.68* | – | |||||||||||||
| 8. 12m Actigraphic Total Sleep Time | 437.89 | 52.13 | 0.02 | 0.00 | −0.04 | −0.03 | 0.06 | 0.66* | 0.67* | – | ||||||||||||
| 9. 18m Actigraphic Total Sleep Time | 443.97 | 55.32 | 0.03 | 0.05 | 0.03 | −0.15* | 0.11* | 0.64* | 0.72 | 0.74* | – | |||||||||||
| 10. Baseline Actigraphic WASO | 43.93 | 16.26 | 0.01 | −0.01 | −0.07 | 0.01 | 0.04 | 0.11* | −0.04 | 0.01 | −0.01 | – | ||||||||||
| 11. 6m Actigraphic WASO | 46.70 | 19.30 | −0.02 | −0.02 | −0.11* | −0.01 | 0.02 | −0.04 | 0.12* | 0.02 | −0.02 | 0.68 | – | |||||||||
| 12. 12m Actigraphic WASO | 41.45 | 14.75 | 0.05 | 0.00 | −0.09 | 0.00 | 0.02 | −0.02 | −0.06 | 0.13* | −0.03 | 0.70* | 0.67* | – | ||||||||
| 13. 18m Actigraphic WASO | 46.08 | 16.18 | 0.06 | 0.05 | −0.07 | −0.06 | 0.03 | −0.02 | 0.01 | 0.04 | 0.14* | 0.61* | 0.63* | 0.66 | – | |||||||
| 14. Baseline Insufficiency | 2.85 | 0.87 | 0.06 | −0.15* | −0.13* | 0.24* | −0.18* | −0.09* | −0.06 | −0.01 | −0.05 | −0.03 | −0.02 | −0.03 | 0.02 | – | ||||||
| 15. 6m Insufficiency | 2.73 | 0.95 | −0.02 | −0.16* | 0.13* | −0.24* | −0.19* | −0.04 | −0.04 | 0.03 | −0.07 | −0.01 | −0.02 | 0.02 | 0.00 | 0.55* | – | |||||
| 16. 12m Insufficiency | 2.72 | 0.92 | −0.10* | −0.16* | −0.12* | 0.30* | −0.23* | 0.05 | 0.02 | 0.04 | −0.08 | −0.01 | 0.02 | −0.02 | 0.00 | 0.53* | 0.56* | – | ||||
| 17. 18m Insufficiency | 2.65 | 0.92 | −0.07 | −0.21* | −0.25* | 0.28* | −0.20* | 0.01 | −0.05 | −0.03 | −0.11* | 0.02 | −0.06 | 0.00 | 0.02 | 0.56* | 0.51* | 0.59* | – | |||
| 18. Baseline Insomnia | 2.70 | 0.78 | 0.02 | −0.05 | −0.11* | 0.08 | −0.06 | 0.13* | 0.11 | 0.15* | 0.09 | 0.12* | 0.15* | 0.14* | 0.13* | 0.25* | 0.26* | 0.24* | 0.22* | – | ||
| 19. 6m Insomnia | 2.68 | 0.77 | 0.04 | −0.03 | −0.12* | 0.03 | −0.06 | 0.14* | 0.16* | 0.13* | 0.09 | 0.19* | 0.21* | 0.15* | 0.15* | 0.16* | 0.22* | 0.28* | 0.22* | 0.57* | – | |
| 20. 12m Insomnia | 2.68 | 0.76 | −0.04 | −0.06 | −0.11* | 0.09 | −0.04 | 0.15* | 0.19 | 0.17* | 0.15* | 0.06 | 0.10* | 0.06 | 0.06 | 0.16* | 0.25* | 0.32* | 0.28* | 0.55* | 0.65* | – |
| 21. 18m Insomnia | 2.70 | 0.72 | 0.06 | −0.01 | −0.15* | 0.10 | −0.09 | 0.16* | 0.12 | 0.10 | 0.12* | 0.08 | 0.07 | 0.04 | 0.07 | 0.17* | 0.18* | 0.23* | 0.30* | 0.48* | 0.59* | 0.61* |
Note. N = 396-618. 6m = 6-months; 12m = 12-months; 18m = 18-months; WASO = wake after sleep onset.
Treatment: 1 = intervention, 0 = usual practice.
p < .05.
Intervention Effects
Hypothesis 1 stated that sleep quantity and quality at 6-months and 18-months would improve as a result of the intervention. Olson et al. (2015) previously found significant intervention effects on actigraphic total sleep time and self-reported sleep insufficiency at the 12-month follow-up. We include these 12-month data in our models for comparison. As seen in Table 3, we extend Olson et al.’s findings and show that such effects are again seen at the 6-month and 18-month follow-ups.
Specifically, a significant intervention by wave interaction is found for 6-month actigraphic total sleep time (γ = 9.13, t = 2.44, p = .02), indicating that individuals in the treatment group experienced approximately 9 minutes of sleep more per night at the 6-month follow-up, relative to individuals in the usual practice group. The magnitude of this effect is considered small (d = .37; Cohen, 1988).1 Additionally, a significant intervention by wave interaction is found for 18-month actigraphic total sleep time (γ = 13.32, t = 3.29, p < .001), indicating that individuals in the treatment group experienced approximately 13 minutes of sleep more per night at the 18-month follow-up, relative to individuals in the usual practice group. The magnitude of this effect is considered small (d = .27; Cohen, 1988). Figure 2 depicts this differential change across the treatment arms from baseline to 6-months, baseline to 12-months, and baseline to 18-months. Actigraphic total sleep time increased in the usual practice group and intervention group from baseline to 6-months, although the increase was greater in the intervention group. Relative to baseline, total sleep time then decreased in the usual practice group, while slightly decreasing in the intervention group at 12-months before increasing again at the 18-month time point.
Figure 2.
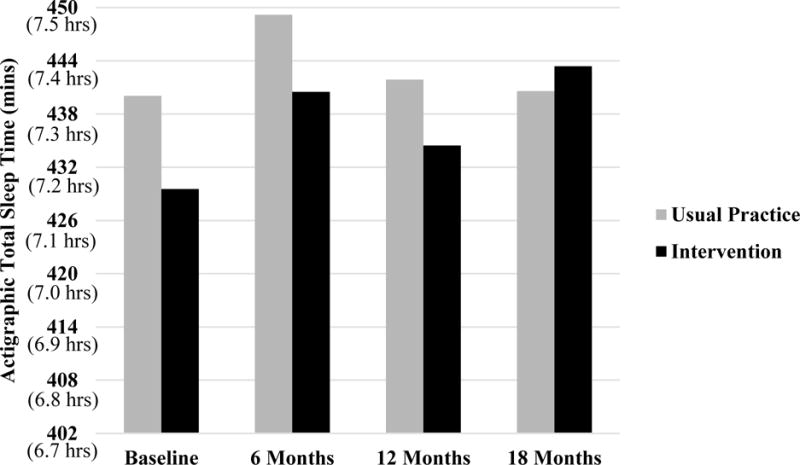
Graph of intervention effect on total daily sleep time.
In addition, a significant intervention effect was found on sleep insufficiency at 6-months (γ = −.25, t = −3.26, p < .001). The magnitude of this effect is also considered small (d = .36; Cohen, 1988). A significant intervention effect was found on sleep insufficiency at 18-months (γ = −.20, t = −2.14, p = .03). The magnitude of this effect is also considered small (d = .43; Cohen, 1988). As seen in figure 3, differential change across the treatment arms over time is evidenced by the intervention group experiencing decreased sleep insufficiency at the 6-month, 12-month, and 18-month follow-ups, whereas sleep insufficiency in the usual practice group decreases to a lesser degree at the 6-month follow up before increasing again at the 12-month follow-up and decreasing slightly at the 18-month follow-up. No significant intervention effects were found at 6-months (γ = 1.15, t = 1.00, p = .32, d = .27) or 18-months (γ = 1.25, t = 1.01, p = .17, d = .33) for either actigraphic WASO or at 6-months (γ = .06, t = 1.02, p = .31, d = .09) or 18-months (γ = .06, t = .89, p = .37, d = .06) for self-report insomnia symptoms.
Figure 3.
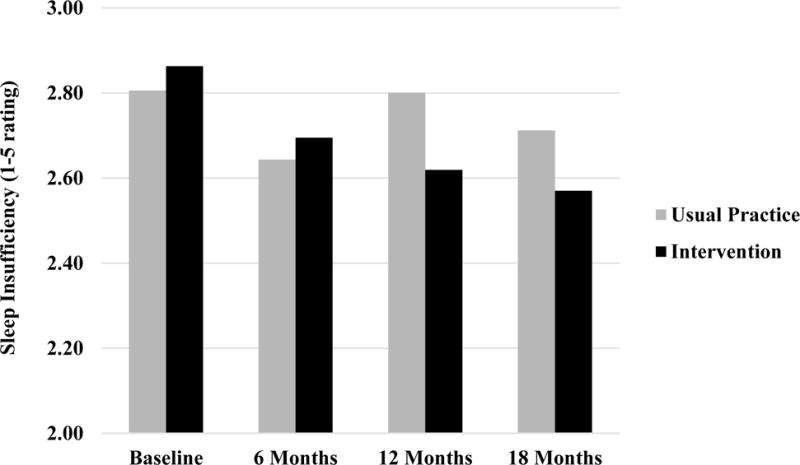
Graph of intervention effect on sleep insufficiency.
The results from these change-on-change models partially confirm hypothesis 1. Specifically, significant intervention effects are found for 6-month and 18-month actigraphic total sleep time and sleep insufficiency. This indicates that there was differential change from baseline to 6-months and baseline to 18-months on these two sleep outcomes depending on whether a participant resided in the control or treatment group. Although these effects are small, the findings indicate that total sleep time was lengthened over time as a result of the intervention, while sleep insufficiency decreased over time as a result of the intervention.
Sustainability Effects
Research question 1 considered whether the intervention effects on sleep quantity and quality would be sustained from the 6-month time point to 18-month time point and from the 12-month time point to the 18-month time point. We test whether changes occurred in sleep between each of the two time points for all four sleep outcomes (i.e., total sleep time, WASO, sleep insufficiency, insomnia) for the sake of completeness. Results from these analyses can be seen in Tables 5 and 6.
Table 5.
Sustainability of Intervention Effects from 6 to 18 Months
| Predictor | Sleep Outcomes
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Act. Total Sleep Time
|
Act. WASO
|
Insufficiency
|
Insomnia
|
|||||
| γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | |
| Fixed Effects | ||||||||
| Intercept | 445.67* | (430.76, 460.58) | 47.16* | (42.94, 51.39) | 2.55* | (2.33, 2.78) | 2.58* | (2.39, 2.76) |
| Core Functiona | −0.09 | (−10.95, 10.77) | −1.36 | (−4.33, 1.62) | −0.10 | (−0.26, 0.05) | −0.05 | (−0.18, 0.07) |
| #of Emps for Rmz | −0.00 | (−0.44, 0.42) | −0.05 | (−0.17, 0.06) | 0.01* | (0.00, 0.01) | 0.00 | (0.00, 0.00) |
| Merger | −5.18 | (−17.10, 6.73) | 0.54 | (−2.79, 3.87) | 0.13 | (−0.05, 0.31) | −0.03 | (−0.18, 0.11) |
| Intervention | 0.11 | (−11.07, 11.30) | 1.68 | (−1.48, 4.83) | −0.09 | (−0.27, 0.08) | 0.03 | (−0.10, 0.17) |
| Wave | −0.19 | (−5.98, 5.61) | 0.19 | (−1.83, 2.21) | −0.05 | (−0.18, 0.08) | 0.02 | (−0.08, 0.11) |
| Intervention* Wave | 1.56 | (−6.69, 9.82) | −0.55 | (−3.42, 2.33) | −0.07 | (−0.25, 0.18) | 0.00 | (−0.13, 0.14) |
| Random Effects | ||||||||
| CS Diagonal Offset | 821.85* | 101.37* | 0.42* | 0.23* | ||||
| CS Covariance | 2002.75* | 167.74* | 0.46* | 0.33* | ||||
| Intercept | 128.06 | 3.64 | N/A | N/A | ||||
Note. CI, confidence interval. # of Emps for Rmz, number of employees for randomization.
The core function identifies groups where most individuals were involved in software development; groups dominated by other IT jobs are the reference group. N/A, not available because covariance parameter is redundant and thus the confidence interval could not be computed.
p < .05.
Table 6.
Sustainability of Intervention Effects from 12 to 18 Months
| Predictor | Sleep Outcomes
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Act. Total Sleep Time
|
Act. WASO
|
Insufficiency
|
Insomnia
|
|||||
| γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | |
| Fixed Effects | ||||||||
| Intercept | 434.87* | (419.72, 450.03) | 42.07* | (38.09, 46.05) | 2.55* | (2.31, 2.80) | 2.59* | (2.40, 2.78) |
| Core Functiona | −0.68 | (−11.44, 10.08) | −1.40 | (−4.10, 1.31) | −0.07 | (−0.24, 0.10) | −0.11 | (−0.24, 0.02) |
| #of Emps for Rmz | 0.03 | (−0.41, 0.46) | −0.05 | (−0.16, 0.05) | 0.01* | (0.00, 0.01) | 0.01* | (0.00, 0.01) |
| Merger | 3.60 | (−8.39, 15.60) | 1.05 | (−2.06, 4.16) | 0.19 | (−0.00, 0.38) | 0.03 | (−0.12, 0.18) |
| Intervention | 1.85 | (−9.25, 12.95) | 2.33 | (−0.55, 5.20) | −0.23* | (−0.41, −0.05) | −0.11 | (−0.25, 0.03) |
| Wave | 4.45 | (−1.02, 9.93) | 4.33* | (2.57, 6.10) | −0.09 | (−0.20, 0.03) | −0.05 | (−0.15, 0.04) |
| Intervention* Wave | 5.13 | (−2.72, 12.97) | −0.02 | (−2.55, 2.50) | 0.03 | (−0.13, 0.20) | 0.13* | (0.00, 0.26) |
| Random Effects | ||||||||
| CS Diagonal Offset | 755.05* | 79.69* | 0.35* | 0.21* | ||||
| CS Covariance | 2040.28* | 158.20* | 0.46* | 0.34* | ||||
| Intercept | 104.79 | N/A | 0.02 | N/A | ||||
Note. CI, confidence interval. # of Emps for Rmz, number of employees for randomization.
The core function identifies groups where most individuals were involved in software development; groups dominated by other IT jobs are the reference group. N/A, not available because covariance parameter is redundant and thus the confidence interval could not be computed.
p < .05.
To evaluate the practical magnitude of the unstandardized effects discussed below and included in Tables 5 and 6, we provide a threshold value in the unstandardized mean difference effect size metric to be evaluated against the confidence intervals included in Tables 5 and 6. First, we defined a small threshold value for d and chose d = .10 on the grounds that a d = .20 is considered small by some in the social and behavioral sciences (Cohen, 1988) and that others argue that small effects can be theoretically and practically important (Prentice & Miller, 1992); thus, d = .10 represents a “smaller than small” change across time between the intervention and usual practice conditions, after the intervention. Next, we then multiplied this value of d = .10 by each baseline standard deviation of the sleep variable in question to yield a threshold value in the unstandardized mean difference effect size metric. These equaled threshold values of 5.33, 1.63, 0.09, and 0.08 for total sleep time, WASO, sleep insufficiency, and insomnia symptoms, respectively. Lastly, using the confidence intervals for unstandardized effects in Tables 5 and 6, we evaluated whether the confidence intervals contained the criterion threshold values. If the confidence interval did contain this value, then we concluded that there is no substantial relevant change in effects over time (i.e., sustainability of effects).
A non-significant intervention by wave interaction was found for actigraphic total sleep time (γ = 1.56, t = .38, p = .71), indicating that there is no significant change from 6 months to 18 months across the intervention and usual practice groups. Although no initial intervention effect was found for actigraphic WASO at 6 months, we tested whether any significant change occurred more so in the intervention than control condition from 6 to 18 months. The intervention by wave interaction was non-significant (γ = −0.55, t = −0.38, p = .71), indicating that there is no significant change over the additional 6 months. We found no evidence that the intervention effect on sleep insufficiency decayed more so in the intervention than control condition from 6 to 18 months, with a non-significant intervention by wave interaction (γ = −0.07, t = −.71, p = .48). Lastly, we tested whether any changes in insomnia symptoms occurred more so in the intervention than control condition from 6 to 18 months, despite initial intervention effects not being found, and did not find a significant intervention-by-wave interaction (γ = 0.00, t = .06, p = .95). For all four models, we then evaluated whether the confidence intervals in Table 5 contained the criterion threshold values, which would indicate sustainability. For example, the 5.33 criterion threshold value computed for total sleep time was contained within the treatment-by-wave interaction’s confidence interval shown in Table 5 (-6.69, 9.82). Each of the criterion threshold values were contained by the associated confidence intervals, and thus, all effects were sustained from 6 to 18 months.
We next tested the sustainability of intervention effects from 12 to 18 months. A non-significant intervention by wave interaction is found for actigraphic total sleep time (γ = 5.13, t = 1.30, p = .20), indicating that there is no significant change from 12 months to 18 months across the intervention and usual practice groups. Although no initial intervention effect was found for actigraphic WASO at 12 months, we tested whether any significant change occurred from 12 to 18 months. The intervention by wave interaction was non-significant (γ = −0.02, t = −0.02, p = .98), indicating that there is not a significant change over the additional 6 months. We found no evidence that sleep insufficiency decayed from 12 to 18 months, with a non-significant intervention-by-wave interaction (γ = 0.03, t = .39, p = .70). Lastly, we tested whether any changes in insomnia symptoms occurred more so in the intervention than control condition from 12 to 18 months, despite initial intervention effects not being found. Interestingly, we found a significant intervention by wave interaction (γ = 0.13, t = 2.02, p = .046), indicating that insomnia symptoms increased from 12 to 18 months. We then evaluated whether the confidence intervals in Table 6 contained the previously-computed criterion threshold values. For example, the 5.33 criterion threshold value computed for total sleep time was contained within the treatment-by-wave interaction’s confidence interval shown in Table 6 (-2.72, 12.97). Each of the criterion threshold values were contained by the associated confidence intervals, and thus, all effects were sustained from 12 to 18 months.
Indirect Effects
Using path modeling, we next tested hypothesis 2 as to whether intervention effects were mediated by changes in control over work schedule and FSSB at 6-months and subsequent changes in WTFC and family time adequacy at 12-months2. See figure 4 for the model that was tested. Results indicate a significant conditional indirect effect, controlling for all other variables in the model, of the intervention on 18-month total sleep time through increases in 6-month control over work schedule and 12-month family time adequacy (indirect effect = .73, p = .03)3. A significant direct effect of the intervention on total sleep time was also found with the path model, indicating partial mediation. This finding suggests that participation in the intervention group led to increases in employees’ control over work schedules. This in turn resulted in employees experiencing more adequate time with family and more distally, a greater ability to obtain longer sleep durations over time. However, evidence of partial mediation suggests that the intervention may have influenced other unmeasured mediators that had an impact on total sleep time, as well. Thus, hypothesis 2 was partially confirmed.
Figure 4.
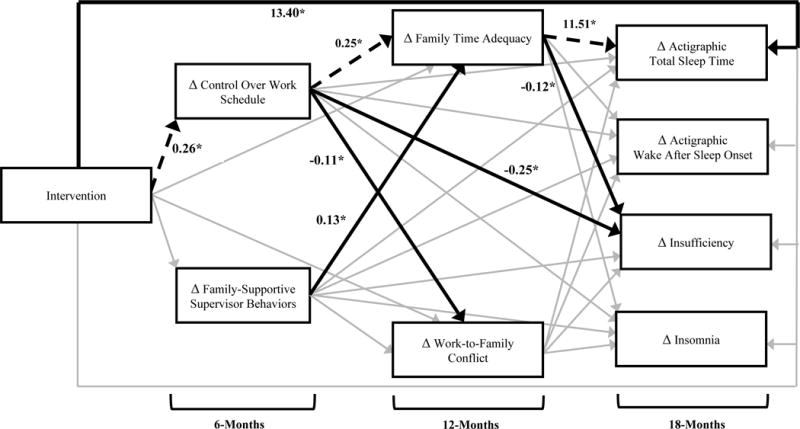
Empirical results of the intervention on 18-month sleep outcomes process model. Control variables (i.e., core function, number of employees for randomization, merger announcement) and covariances (i.e., between control over work schedule and family-supportive supervisor behaviors, family time adequacy and work-to-family conflict, and among sleep outcomes) not shown for parsimony. Bold arrows depict significant direct effects, bold dashed arrows depict significant indirect effects, and grey arrows depict non-significant direct effects. * p < .05
Discussion
Workplace interventions are difficult to sustain, and workplaces have invested relatively little effort into understanding how to improve the organization of work in order to benefit health and well-being. The results of this study indicate that a work-family intervention’s effect on certain aspects of sleep is not only maintained at 18-months, but also occurs through a longitudinal mediation with intended intervention targets at both 6- and 12-months. These effects are further bolstered by the adjusted means presented in Table 2, indicating that the hypothesized intervention targets improved over time. Moreover, both aspects of sleep quantity (i.e., actigraphic total sleep time) and sleep quality (i.e., sleep insufficiency) are improved a year and half after the intervention’s implementation and no significant decay is seen from 12 to 18 months post-baseline. These findings demonstrate the sustainability of the intervention in question for two of the four sleep outcomes evaluated.
Furthermore, we find that increases in 6-month control over work schedule and 12-month family time adequacy act as mediators of the intervention’s effect on 18-month actigraphic total sleep time. As such, we provide some support for COR theory and Hobfoll’s (1989) propositions that resources can help prevent strain outcomes. Our findings might suggest individuals did not have the same need to borrow time from sleep in order to accommodate family or work demands, and thus, were able to allocate more hours to sleep on average, even when sleep was measured at a distal time point 18 months after the intervention. Through evaluating additional mediators, we add to Olson et al.’s (2015) work by providing a comprehensive theoretical understanding of how the intervention improved sleep outcomes. This also points to the reality that, at least in this sample, control over work schedule was a critical resource for improving sleep outcomes, when compared to FSSB. These findings are consistent with those of Basner, Spaeth, and Dinges (2014), in that they identified challenges in the time domain as key determinants of sleep adequacy.
Our results indicate that intervention effects on total sleep time and sleep insufficiency present at the 12-month follow-up are maintained through the 18-month follow-up. As seen in Table 4, the treatment group experienced an approximate 9-minute per day increase in total sleep time relative to the usual practice group at 6 months compared to baseline, and an approximate 9-minute per day average increase in total sleep time relative to the usual practice group at 12 months compared to baseline. Furthermore, an approximate 13-minute increase in total sleep time per day was experienced by the intervention group relative to the usual practice group at 18 months compared to baseline. Thus, no decay and actually an increase in total sleep time is seen over an additional 6 months to the 18-month time point, although the effect is not significant. The intervention effects correspond to about one extra hour of sleep per week.
Table 4.
Effect of Intervention on 6-, 12- and 18-month Sleep Outcomes
| Predictor | Sleep Outcomes
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Act. Total Sleep Time
|
Act. WASO
|
Insufficiency
|
Insomnia
|
|||||
| γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | γ | (95% CI) | |
| Fixed Effects | ||||||||
| Intercept | 436.10* | (424.43, 447.77) | 46.50* | (42.89, 50.12) | 2.59* | (2.40, 2.78) | 2.59* | (2.48, 2.74) |
| Core Functiona | −4.35 | (−12.80, 4.11) | −1.32 | (−3.96, 1.32) | −0.07 | (−0.20, 0.06) | −0.10 | (−0.21, 0.01) |
| # of Emps for Rmz | 0.14 | (−0.18, 0.47) | −0.08 | (−0.19, 0.02) | 0.01* | (0.00, 0.01) | 0.01* | (0.00, 0.01) |
| Merger | 4.10 | (−5.15, 13.35) | 0.17 | (−2.70, 3.04) | 0.13 | (−0.01, 0.28) | 0.02 | (−0.11, 0.14) |
| Intervention | −10.51* | (−19.57, −1.45) | 0.44 | (−2.38, 3.26) | 0.06 | (−0.09, 0.21) | −0.01 | (−0.14, 0.11) |
| 6 m. Wave | 1.82 | (−3.41, 7.04) | 2.16* | (0.55, 3.76) | −0.01 | (−.11, .10) | −0.06 | (−0.15, 0.03) |
| 12 m. Wave | −3.75 | (−9.00, 1.50) | −2.27* | (−3.88, −0.66) | 0.01 | (−0.10, 0.11) | −0.01 | (−0.10, 0.08) |
| 18 m. Wave | 0.52 | (−5.04, 6.09) | 2.16* | (0.35, 3.77) | −0.09 | (−0.20, 0.02) | −0.06 | (−0.14, 0.04) |
| Intervention* 6 m. Wave | 9.13* | (1.77, 16.48) | 1.15 | (−1.11, 3.41) | −0.16* | (−0.31, −0.01) | 0.06 | (−0.06, 0.18) |
| Intervention* 12 m. Wave | 8.65* | (1.89, 16.12) | 1.40 | (−0.89, 3.69) | −0.25* | (−0.40, −0.10) | −0.05 | (−0.17, 0.07) |
| Intervention* 18 m. Wave | 13.32* | (5.36, 21.28) | 1.25 | (−1.19, 3.69) | −0.20* | (−0.36, −0.04) | 0.06 | (−0.07, 0.19) |
| Random Effects | ||||||||
| CS Diagonal Offset | 901.97* | 81.16* | 0.38* | 0.25 | ||||
| CS Covariance | 1966.11* | 170.94* | 0.45* | 0.33 | ||||
| Intercept | 11.65 | 2.86 | N/A | N/A | ||||
Note. CI, confidence interval. # of Emps for Rmz, number of employees for randomization.
The core function identifies groups where most individuals were involved in software development; groups dominated by other IT jobs are the reference group. N/A, not available because covariance parameter is redundant and thus the confidence interval could not be computed.
p < .05.
We had posed our predictions around the sustainability of the intervention effect as a research question rather than a hypothesis, given current uncertainty in the existing literature. Specifically, COR theory (Hobfoll, 1989) leads us to the conclusion that, with the addition of resources provided by the WFHS intervention, we would expect increases in sleep quantity and quality 6 months beyond the 12-month time point (i.e., gain spirals). In contrast, Ford et al.’s (2014) meta-analytic findings suggest that sleep effects may be sustained over time, given that lagged effects of stressors on physical strains tend to be small and difficult to detect. As a non-significant, albeit trending, increase in total sleep time from 12 to 18 months was found in our study, we conclude that our results best support Ford et al.’s (2014) work rather than COR theory. It is important to note, however, that Ford et al.’s (2014) work is not specific to interventions, but rather stressor-strain relationships more generally.
Regardless, given our trending increase in total sleep time, we believe that future interventions may in fact find sleep to further increase with successive time points beyond the 18-month mark and/or the addition of other resources (e.g., booster trainings, an individual-level sleep intervention component). It may also be the case that other physical health outcomes would respond more sensitively to the intervention, thereby representing the gain spiral processes Hobfoll (1989) hypothesizes. With increasing intervention research that aims to improve workplace resources, scholars should closely evaluate the process by which the implementation of new resources leads to additional resources in a gain spiral framework, while also collecting data at frequent successive time points in order to more accurately model any complex trajectories in outcomes over time. Lastly, as Ford et al. (2014) suggest, large sample sizes are needed to detect even small lagged effects. However, if small lagged effects are found, these are likely to have important clinical implications.
The public health relevance of the intervention is important given the goals of Healthy People 2020 (US Department of Health and Human Services, 2010) and other initiatives to improve sleep health at the population level. Of note, the intervention effect sizes found are small, but the intervention also did not directly engage sleep behavior modification at the individual level. Rather, this intervention focused on improving structural workplace factors that limit the employee’s ability to obtain adequate sleep. These findings provide valuable evidence supporting the initiatives of the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health to better understand the role of work in sleep health (Jacobsen et al., 2014) including interventions already developed for health care workers (NIOSH, Caruso, Geiger-Brown, Takahashi, Trinkoff, & Nakata, 2015). These results can be used in persuading organizational decision-makers to adopt such an intervention, while also informing future research that aims to further refine this promising intervention and evaluate whether stronger effects are found and whether effects are seen beyond 18 months. Health care providers may find value in evaluating work-related issues in patients exhibiting signs of deleterious health consequences of inadequate sleep.
We do not find support for the intervention’s effect on either actigraphic WASO or insomnia symptoms at the 6-month or 18-month follow-up. Although some research has found a relationship between work-family stress and difficulty initiating or maintaining self-report sleep (e.g., Crain et al., 2014; Lallukka et al., 2010), we are unaware of any intervention studies that have included such variables. These results are surprising given that the resources supplied by the intervention should have resulted in decreased strain that can result in difficulty falling asleep. These results are not in line with COR theory (Hobfoll, 1989), and it may be that these are aspects of sleep quality that are less likely to be improved through the provision of organizational resources, such as control over work schedule and FSSB. In fact, we find that insomnia symptoms actually worsen from 12 to 18 months.
When an individual is clinically diagnosed with insomnia, individual-level behavioral and/or pharmaceutical treatments are often administered (e.g., Drake, Roehrs, & Roth, 2003). Although we do not address insomnia as a disorder in this study, we do evaluate the lower-grade manifestations of insomnia symptoms and WASO. Given the focus on behavioral treatments for insomnia disorder in both literature and practice, it’s likely that individual behavior change is necessary for insomnia symptom and WASO improvement, as well. For example, Bootzin and Epstein (2013) explain that poor sleep habits, such as irregular sleep-wake schedules, dysfunctional cognitions such as worry, and physiological, emotional, and cognitive arousal are the primary factors targeted within insomnia treatments. While the intervention was designed and found to decrease work-family stressors, it did not address individuals’ sleep habits, ability to control unwanted cognitions during the day or before bed, or ability to engage in de-arousal strategies. As we explain in more detail below, future organizational interventions may be more efficacious in improving insomnia symptoms and WASO if combined with individual training targeting these behaviors (e.g., Barnes et al., 2017; Thiart et al., 2016). More generally, there is a need for future research to test this intervention in other industries to determine if effects are present and consistent in lower-wage samples, for instance, and whether moderating effects are present for workers with different types of family demands as has been shown in other recent work (e.g., Kossek et al., in press).
Future Directions and Limitations
Findings from the current study provide a foundation for future intervention research targeting sleep as a health outcome. Such studies should continue to use longitudinal designs, with follow-up data collections extending past the 18-month mark. Given intervention effects were found on sleep at both the 12- and 18-month follow-up, it’s likely that such effects were sustained and maybe even improved after this time.
A limitation of this study concerns our inability to speak to which aspects of control over work schedule were utilized by employees which in turn resulted in reports of more adequate time with family and consequently longer sleep durations. To this end, other sleep researchers (e.g., Basner et al., 2014) have proposed commute time as a target for future interventions, as commute time is reciprocally related to sleep. Thus, employees in this study may have been teleworking more and commuting less, allowing for more sufficient time with family. Alternatively, employees may have been choosing different times during the day to work, allowing them to be available for family during more critical periods of the day (e.g., family member doctor visits, dinner time), as opposed to being available for just more time during the day.
In addition, alternative proximal and distal mediators should be examined, given our results indicating a partial mediation through control over work schedule and family time adequacy. For example, other time-based measures may be incorporated, such as commute time or work-related technology use in the home domain. Alternatively, strain-based measures may also play mediator roles, such as rumination or worry.
It should also be noted that while a strength of this study is that we have measures of both objective and subjective sleep, which the literature has shown are related to unique antecedents, this study is part of interdisciplinary intervention work on linkages between sleep, health, and work-family conflict. As a result, we had to be parsimonious in how we measured sleep. Thus, we focused on capturing theoretically meaningful objective and subjective measures of sleep quantity and quality that were relevant for the current study. Although actigraphic software often provides a number of variables in addition to total sleep time and WASO (e.g., sleep efficiency or the ratio of total sleep time to time in bed, onset latency or the amount of time it takes to fall asleep, number of awakenings during the night), we chose those variables with high clinical utility and those that have been well-validated against polysomnography, the gold standard for measuring sleep (e.g., Marino et al., 2013; Winkelman et al., 2008). Furthermore, rather than relying solely on the standard algorithmic output from the actigraphy software, we used a rigorous scoring procedure outlined by Marino et al. (2013), allowing for the computation of total sleep time and WASO. In line with our discussion of actigraphy limitations in the method section, it is important to point out that actigraphy tends to have high sensitivity (i.e., actigraphic sleep closely matches polysomnographic sleep), but specificity tends to be lower (i.e., actigraphic wake time does not always closely match polysomnographic wake time) (Marino et al., 2013). As a result, actigraphic measures that are derived from wake time (e.g., WASO, sleep efficiency) can be less valid if individuals experience high amounts of time awake during sleep. Aside from objective measures of sleep, researchers should consider using additional self-report measures of sleep in future studies that are well-validated with modern psychometric techniques (e.g., Yu et al., 2011).
The intervention utilized in the current work was aimed primarily at improving the organizational factors of control over work schedule and FSSB, representing an approach to health protection. However, effects on sleep may have been stronger and more numerous had this intervention also incorporated training aimed at individual sleep hygiene behaviors combined with increasing control over work and FSSB. As such, Hammer and Sauter (2013) suggest that these integrated Total Worker Health® (TWH) interventions, with both health protection and health promotion aspects, are ideal for affecting work-family outcomes and subsequently health. As described in further detail below, potential health promotion aspects could include sleep education and sleep hygiene training, mindfulness training, cognitive-behavioral training, and/or strategies for de-arousal both during the day and prior to bed. In many ways, this is a protection-oriented intervention that may proactively help improve sleep quality as a health pathway where individual-level sleep training would be more of health promotion targeting individual change. On the other hand, teaching supervisors how to be more supportive of sleep health in their employees, which could include support for control over work as a way to further support increasing sleep hygiene, may be considered a health protection approach (similar to FSSB training), as it would address how the structure and culture of the organization of work affects employee sleep and health. Integrating individual-level training with the current health protection intervention would represent an integrated intervention such as those suggested in the TWH approach.
The first of these suggested components, sleep education and sleep hygiene training at the individual employee-level, may be particularly useful in changing behaviors that are related to the timing and duration of sleep, in addition to the consistency of sleep schedules. Such schedules may involve providing individuals with information around the function of sleep, sleep needs, circadian rhythms, and developmental changes in sleep over the lifespan. Sleep hygiene training with employees could provide information on those behaviors that will lead to improved sleep, such as the avoidance of caffeine, nicotine, alcohol, the reduction of bedroom noise, techniques for stress management, and the importance of regular exercise (Irish, Kline, Gunn, Buysse, & Hall, 2015). As mentioned above, this type of individual-level intervention could be further enhanced with a supervisor training component that encourages support for employee sleep hygiene behaviors.
Future interventions may make use of cognitive behavioral training and/or training focused on strategies for de-arousal. Although we suggest some specific intervention strategies above that represent a viable avenue for future research, we also acknowledge that these tactics may be less effective for individuals who are older or who have other comorbid medical psychiatric, sleep, or substance use disorders, given that these are risk factors for clinical insomnia disorder (Schutte-Rodin, Broch, Buysse, Dorsey, & Sateia, 2008). Recommended psychological and behavioral therapies for insomnia disorder include cognitive behavioral therapy and/or relaxation therapy, while insufficient evidence exists suggesting that sleep hygiene is an effective treatment in and of itself (Schutte-Rodin et al., 2008). Thus, elements of cognitive behavioral and relaxation training should be used when designing future interventions that are intended to be efficacious for a variety of individuals.
Practical Implications
As rigorous evidenced-based workplace interventions become more common, policy-makers, organizations, and employees must be reassured of a program’s effectiveness in both the short-term and long-term time period following the intervention. Given the well-established literature indicating that tired workers are more likely to experience accidents (e.g., Uehli et al., 2014), lowered performance (e.g., Philibert, 2005), and eventual chronic illness (e.g., Buxton & Marcelli, 2010), organizations should consider the efficacy of both organizational and individual interventions targeting employee sleep. Current consensus recommendations for sleep include the recommendation to obtain at least seven hours per night on a habitual basis, and modifying work practices to protect time for sleep is an important step towards this goal of reducing the population-level burden of sleep deficiency (Watson et al., 2015). Our mediation findings suggest that employee control over work schedule is a key factor for employees’ time with family and time for sleep. Organizations that may not have the resources to undergo a large-scale intervention as described here, may choose to focus on improving employees’ ability to determine when and where they work.
Conclusion
Organizations and individuals are more likely to invest in and adopt a program, despite scarce resources, if the research can provide evidence of sustained benefits. There is also a need to illuminate the time frames within which intervention effects are sustained so that interventions can be tailored, adjusted, and augmented in future studies for more robust and lasting effects. Interventions should not be labeled as good or bad, but rather should bring to light aspects of the program that can be revised in future iterations (Goldstein & Ford, 2002). With its focus on sustainability of intervention effects, the current study contributes to a new area within the organizational and implementation science fields. These results provide a foundation for future intervention research that targets a range of variables in an effort to improve sleep over time, a critical factor for long term health and well-being that is quickly becoming a national priority.
Acknowledgments
This research was conducted as part of the Work, Family and Health Network (www.WorkFamilyHealthNetwork.org), which is funded by a cooperative agreement through the National Institutes of Health and the Centers for Disease Control and Prevention: Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant # U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (Grant # U01AG027669), Office of Behavioral and Science Sciences Research, and National Institute for Occupational Safety and Health (Grant # U01OH008788, U01HD059773). Grants from the National Heart, Lung and Blood Institute (R01HL107240), the William T. Grant Foundation, Alfred P Sloan Foundation, and the Administration for Children and Families have provided additional funding. This publication was also supported by the Mountains and Plains Education and Research Center, Grant T42OH009229, funded by the Centers for Disease Control and Prevention. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices. Special acknowledgement goes to Extramural Staff Science Collaborator, Rosalind Berkowitz King, Ph.D. and Lynne Casper, Ph.D. for design of the original Workplace, Family, Health and Well-Being Network Initiative.
Outside of the submitted work, Orfeu M. Buxton reports investigator-initiated research grant support from Sepracor (now Sunovion) and Cephalon (now Teva); personal fees from Takeda Pharmaceuticals North America (consulting, speaking), Dinsmore LLC (expert witness tes− timony and consulting), Matsutani America (scientific advisory board), and Chevron (speaking fee).
Footnotes
OHSU has a significant financial interest in NwETA, a company that has a commercial interest in the results of this research and technology. This potential conflict was reviewed and managed by OHSU Conflict of Interest in Research Committee.
From Table 4, the effect size d equals the estimated difference in mean change over time from baseline to that time point across intervention conditions divided by the square root of the sum of the random effects for that model (Feingold, 2009).
Change-on-change analyses revealed significant and positive intervention effects on control over work hours at 6, 12, and 18 months post-intervention. A significant and positive intervention effect was found for FSSB and family time adequacy at 18 months post-intervention, while a significant and negative intervention effect was found for work-to-family conflict at 18 months post-intervention. We have omitted the details of these results from the paper’s text and tables for the sake of brevity.
Subsets of mediational paths from this larger model with all study variables included were also tested in a series of separate fully-saturated models to determine whether suppression effects were present in the larger model. If suppression effects were present, some significant conditional indirect effects might not be seen in the larger model, but would be seen in the smaller models evaluating individual mediations. In line with results from the larger model, a significant indirect effect was found from the intervention to 18−month total sleep time through 6−month control over work schedule and subsequently 12−month family time adequacy. No other significant indirect effects were found with the other smaller models, which evaluated the intervention’s effect on 18−month sleep outcomes through 6−month control over work schedule and FSSB, and subsequently 12−month family time adequacy and work-to-family conflict in all possible combinations. Thus, we conclude that no suppression effects were present in the larger model.
Contributor Information
Tori L. Crain, Department of Psychology, Colorado State University
Leslie B. Hammer, Oregon Institute of Occupational Health Sciences, Oregon Health & Science University (OHSU), Department of Psychology, Portland State University (PSU)
Todd Bodner, Department of Psychology, Portland State University.
Ryan Olson, Oregon Institute of Occupational Health Sciences, Oregon Health & Science University (OHSU), Department of Psychology, Portland State University, OHSU-PSU School of Public Health.
Ellen Ernst Kossek, Krannert School of Management and Butler Center for Research Excellence, Purdue University.
Phyllis Moen, Department of Sociology, University of Minnesota.
Orfeu M. Buxton, Department of Biobehavioral Health, Pennsylvania State University, Department of Medicine, Harvard Medical School, Division of Sleep Medicine, Harvard T.H. Chan School of Public Health, and Brigham and Women’s Hospital, Boston, Massachusetts
References
- Adler AB, Gunia BC, Bliese PD, Kim PY, LoPresti ML. Using actigraphy feedback to improve sleep in soldiers: an exploratory trial. Sleep Health. 2017;3(2):126–131. doi: 10.1016/j.sleh.2017.01.001. [DOI] [PubMed] [Google Scholar]
- Allen TD, Kiburz KM. Trait mindfulness and work–family balance among working parents: The mediating effects of vitality and sleep quality. Journal of Vocational Behavior. 2012;80:372–379. doi: 10.1016/j.jvb.2011.09.002. [DOI] [Google Scholar]
- Allen TD, Martin A. The work-family interface: A retrospective look at 20 years of research in JOHP. Journal of Occupational Health Psychology. 2017;22:259–272. doi: 10.1037/ocp0000065. [DOI] [PubMed] [Google Scholar]
- Anger WK, Rohlman DS, Kirkpatrick J, Reed RR, Lundeen CA, Eckerman DA. cTRAIN: A computer-aided training system developed in SuperCard for teaching skills using behavioral education principles. Behavior Research Methods, Instruments, & Computers. 2001;33:277–281. doi: 10.3758/bf03195377. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcraft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. SLEEP. 2003;26:342–392. doi: 10.1093/sleep/26.3.342. Retrieved from http://www.journalsleep.org/ [DOI] [PubMed] [Google Scholar]
- August GJ, Bloomquist ML, Lee SS, Realmuto GM, Hektner JM. Can evidence-based prevention programs be sustained in community practice settings? The early risers’ advanced-stage effectiveness trial. Prevention Science. 2006;7:151–165. doi: 10.1007/s11121-005-0024-z. [DOI] [PubMed] [Google Scholar]
- Barbosa C, Bray JW, Dowd WN, Mills MJ, Moen P, Wipfli B, Kelly EL. Return on investment of a work–family intervention: Evidence from the Work, Family, & Health Network. Journal of Occupational and Environmental Medicine. 2015;57:943–951. doi: 10.1097/jom.0000000000000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes CM. Working in our sleep: Sleep and self-regulation in organizations. Organizational Psychology Review. 2012;2:234–257. doi: 10.1177/2041386612450181. [DOI] [Google Scholar]
- Barnes CM, Jiang K, Lepak DP. Sabotaging the benefits of our own human capital: Work unit characteristics and sleep. Journal of Applied Psychology. 2016;101(2):209–221. doi: 10.1037/apl0000042. [DOI] [PubMed] [Google Scholar]
- Barnes CM, Miller JA, Bostock S. Helping employees sleep well: Effects of cognitive behavioral therapy for insomnia on work outcomes. Journal of Applied Psychology. 2017;102(1):104–113. doi: 10.1037/apl0000154. [DOI] [PubMed] [Google Scholar]
- Barnes CM, Wagner DT, Ghumman S. Borrowing from sleep to pay work and family: Expanding time-based conflict to the broader nonwork domain. Personnel Psychology. 2012;65:789–819. doi: 10.1111/peps.12002. [DOI] [Google Scholar]
- Basner M, Spaeth AM, Dinges DF. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. SLEEP. 2014;37:1889–1906L. doi: 10.5665/sleep.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Buxton O, Ertel K, Okechukwu C. Managers’ practices related to work–family balance predict employee cardiovascular risk and sleep duration in extended care settings. Journal of Occupational Health Psychology. 2010;15:316–329. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner T, Bliese P. Detecting and differentiating the direction of change and intervention effects in randomized trials. Journal of Applied Psychology. 2017 doi: 10.1037/apl0000251. Advance online publication . [DOI] [PubMed]
- Bootzin RR, Epstein DR. Understanding and treating insomnia. Annual Review of Clinical Psychology. 2011;7:435–458. doi: 10.1146/annurev.clinpsy.3.022806.091516. [DOI] [PubMed] [Google Scholar]
- Bray JW, Kelly EL, Hammer LB, Almeida DM, Dearing JW, King RB, Buxton OM. An integrative, multilevel, and transdisciplinary research approach to challenges of work, family, and health. Research Triangle Park, NC: RTI Press; 2013. (RTI Press publication No MR-0024-1302). [DOI] [PubMed] [Google Scholar]
- Buxton OM, Hopcia K, Sembajwe G, Porter JH, Dennerlin JT, Kenwood C, Sorenson G. Relationship of sleep deficiency to perceived pain and physical disability in hospital patient care workers. Journal of Occupational and Environmental Medicine. 2012;54:851–858. doi: 10.1097/JOM.0b013e31824e6913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social Science & Medicine. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Quintiliani LM, Yang MH, Ebbeling CB, Stoddard AM, Pereira LK, Sorensen G. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. American Journal of Public Health. 2009;99(S3):S636. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Unhealthy sleep-related behaviors – 12 states, 2009. Morbidity and Mortality Weekly Report. 2011;60:233–266. Retrieved from http://www.cdc.gov/mmwr/ [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. San Diego, CA: Academic Press; 1988. [Google Scholar]
- Crain TL, Brossoit RM, Fisher GG. Work, nonwork, and sleep (WNS): A review and conceptual framework. Journal of Business and Psychology. doi: 10.1007/s10869-017-9521-x. (in press) [DOI] [Google Scholar]
- Crain TL, Hammer LB, Bodner T, Kossek EE, Moen P, Lilienthal R, Buxton OM. Work–family conflict, family-supportive supervisor behaviors (FSSB), and sleep outcomes. Journal of Occupational Health Psychology. 2014;19:155–167. doi: 10.1037/a0036010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crain TL, Schonert-Reichl KA, Roeser RW. Cultivating teacher mindfulness: Effects of a randomized controlled trial on work, home, and sleep outcomes. Journal of Occupational Health Psychology. 2017;22:138–152. doi: 10.1037/ocp0000043. [DOI] [PubMed] [Google Scholar]
- Davis KD, Lawson KM, Almeida DM, Kelly EL, King RB, Hammer LB, McHale SM. Parents’ daily time with their children: A workplace intervention. Pediatrics. 2015;135:875–882. doi: 10.1542/peds.2014-2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Lange AH, Kompier MAJ, Taris TW, Geurts SAE, Beckers DGJ, Houtman ILD, Bongers PM. A hard day’s night: A longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. Journal of Sleep Research. 2009;18(3):374–383. doi: 10.1111/j.1365-2869.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- Donner A, Klar N. Pitfalls of and controversies in cluster randomization trials. American Journal of Public Health. 2004;94:416–422. doi: 10.2105/ajph.94.3.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CL, Roehrs T, Roth T. Insomnia causes, consequences, and therapeutics: An overview. Depression and Anxiety. 2003;18:163–176. doi: 10.1002/da.10151. [DOI] [PubMed] [Google Scholar]
- Ebert DD, Berking M, Thiart H, Riper H, Laferton JAC, Cuijpers P, Lehr D. Restoring depleted resources: Efficacy and mechanisms of change of an internet-based unguided recovery training for better sleep and psychological detachment from work. Health Psychology. 2015;34(Suppl):1240–1251. doi: 10.1037/hea0000277. [DOI] [PubMed] [Google Scholar]
- Eriksen CA, Kecklund G. Sleep, sleepiness and health complaints in police officers: The effects of a flexible shift system. Industrial Health. 2007;45(2):279–288. doi: 10.2486/indhealth.45.279. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford MT, Matthews RA, Wooldridge JD, Mishra V, Kakar UM, Strahan SR. How do occupational stressor-strain effects vary with time? A review and meta-analysis of the relevance of time lags in longitudinal studies. Work & Stress. 2014;28(1):9–30. doi: 10.1080/02678373.2013.877096. [DOI] [Google Scholar]
- Frane JW. A method of biased coin randomization, its implementation, and its validation. Therapeutic Innovation & Regulatory Science. 1998;32:423–432. doi: 10.1177/009286159803200213. [DOI] [Google Scholar]
- Garde AH, Nabe-Nielsen K, Aust B. Influence on working hours among shift workers and effects on sleep quality – An intervention study. Applied Ergonomics. 2011;42(2):238–243. doi: 10.1016/j.apergo.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein IL, Ford JK. Training in organizations. 4th. Belmont, CA: Wadsworth; 2002. [Google Scholar]
- Greenhaus JH, Beutell NJ. Sources of conflict between work and family roles. Academy of Management Review. 1985;10:76–88. Retrieved from http://aom.org/amr/ [Google Scholar]
- Halbesleben JRB, Neveu J-P, Paustian-Underdahl SC, Westman M. Getting to the “COR”: Understanding the role of resources in Conservation of Resources Theory. Journal of Management. 2014;40:1334–1364. doi: 10.1177/0149206314527130. [DOI] [Google Scholar]
- Hammer LB, Johnson RC, Crain TL, Bodner T, Kossek EE, Davis KD, Berkman L. Intervention effects on safety compliance and citizenship behaviors: Evidence from the Work, Family, and Health Study. Journal of Applied Psychology. 2016 doi: 10.1037/apl0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer LB, Kossek EE, Anger WK, Bodner T, Zimmerman KL. Clarifying work–family intervention processes: The roles of work–family conflict and family-supportive supervisor behaviors. Journal of Applied Psychology. 2011;96:134–150. doi: 10.1037/a0020927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer LB, Kossek EE, Bodner T, Crain T. Measurement development and validation of the Family Supportive Supervisor Behavior Short-Form (FSSB-SF) Journal of Occupational Health Psychology. 2013;18:285–296. doi: 10.1037/a0032612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer LB, Kossek EE, Yragui NL, Bodner TE, Hanson GC. Development and validation of a multidimensional measure of family supportive supervisor behaviors (FSSB) Journal of Management. 2009;35:837–856. doi: 10.1177/0149206308328510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer LB, Sauter S. Total worker health and work–life stress. Journal of Occupational and Environmental Medicine. 2013;55:S25–S29. doi: 10.1097/jom.0000000000000043. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037/0003-066X.44.3.513. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Shirom A. Conservation of resources theory: Applications to stress and management in the workplace. In: Golembiewski RT, editor. Handbook of organizational behavior. 2nd. New York: Dekker; 2000. pp. 57–81. [Google Scholar]
- Howell AJ, Digdon NL, Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Personality and Individual Differences. 2010;48:419–424. doi: 10.1016/j.paid.2009.11.009. [DOI] [Google Scholar]
- Hülsheger UR, Feinholdt A, Nübold A. A low-dose mindfulness intervention and recovery from work: Effects on psychological detachment, sleep quality, and sleep duration. Journal of Occupational and Organizational Psychology. 2015;88(3):464–489. doi: 10.1111/joop.12115. [DOI] [Google Scholar]
- Hülsheger UR, Lang JWB, Depenbrock F, Fehrmann C, Zijlstra FRH, Alberts HJEM. The power of presence: The role of mindfulness at work for daily levels and change trajectories of psychological detachment and sleep quality. Journal of Applied Psychology. 2014;99:1113–1128. doi: 10.1037/a0037702. [DOI] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews. 2015;22:23–36. doi: 10.1016/j.smrv.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen HB, Reme SE, Sembajwe G, Hopcia K, Stoddard AM, Kenwood C, Buxton OM. Work–family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health & Safety. 2014;62:282–291. doi: 10.3928/21650799-20140617-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Moen P. Rethinking the clock work of work: Why control over work schedule may pay off at work and at home. Advances in Developing Human Resources. 2007;9:487–506. doi: 10.1177/1523422307305489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Moen P, Tranby E. Changing workplaces to reduce work-family conflict: Schedule control in a white-collar organization. American Sociological Review. 2011;76:265–290. doi: 10.1177/0003122411400056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Moen P, Oakes JM, Fan W, Okechukwu C, Davis KD, Casper LM. Changing work and work-family conflict: Evidence from the work, family, and health network. American Sociological Review. 2014:1–32. doi: 10.1177/0003122414531435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King RB, Karuntzos G, Casper L, Moen P, Davis K, Berkman L, Kossek E. Work-family balance issues and work-leave policies. In: Gatchel RJ, Schultz IZ, editors. Handbook of occupational health and wellness. New York: Springer; 2012. pp. 323–339. [Google Scholar]
- Kossek EE, Hammer LB, Kelly EL, Moen P. Designing work, family & health organizational change initiatives. Organizational Dynamics. 2014;43:53–63. doi: 10.1016/j.orgdyn.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek E, Lautsch B, Eaton S. Telecommuting, control, and boundary management: correlates of policy use and practice, job control, and work-family effectiveness. Journal of Vocational Behavior. 2006;68:347–367. [Google Scholar]
- Kossek EE, Thompson RJ, Lawson KM, Bodner T, Perrigino MB, Hammer LB, Bray JW. Caring for the elderly at work and home: Can a randomized organizational intervention improve psychological health? Journal of Occupational Health Psychology. doi: 10.1037/ocp0000104. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lallukka T, Rahkonen O, Lahelma E, Arber S. Sleep complaints in middle-aged women and men: The contribution of working conditions and work-family conflicts. Journal of Sleep Research. 2010;19:466–477. doi: 10.1111/j.1365-2869.2010.00821.x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to mediation analysis. New York, NY: Taylor & Francis; 2008. [Google Scholar]
- Magnusson Hanson LL, Åkerstedt T, Näswall K, Leineweber C, Theorell T, Westerlund H. Cross-lagged relationships between workplace demands, control, support, and sleep problems. Sleep. 2011;34(10):1403–1410. doi: 10.5665/sleep.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Buxton OM. Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. SLEEP. 2013;36:1747–1755. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, Hall MH. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4:96–103. doi: 10.1016/j.sleh.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McHale SM, Lawson KM, Davis KD, Casper L, Kelly EL, Buxton O. Effects of a workplace intervention on sleep in employees’ children. Journal of Adolescent Health. 2015;56:672–677. doi: 10.1016/j.jadohealth.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen P, Fan W, Kelly EL. Team-level flexibility, work-home spillover, and health behavior. Social Science & Medicine. 2013;84:69–79. doi: 10.1016/j.jvb.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen P, Kelly EL, Tranby E, Huang Q. Changing work, changing health: Can real work-time flexibility promote health behaviors and well-being? Journal of Health and Social Behavior. 2011;52:404–429. doi: 10.1177/0022146511418979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen P, Kelly EL, Fan W, Lee S-R, Almeida D, Kossek EE, Buxton O. Does a flexibility/support organizational initiative improve high tech employee’s well being? Evidence from the Work, Family and Health Network. American Sociological Review. 2016;81(1):134–164. doi: 10.1177/0003122415622391. [DOI] [Google Scholar]
- Mullins HM, Cortina JM, Drake CL, Dalal RS. Sleepiness at work: A review and framework of how the physiology of sleepiness impacts the workplace. Journal of Applied Psychology. 2014;99:1096–1112. doi: 10.1037/a0037885. [DOI] [PubMed] [Google Scholar]
- Murray DM, Varnell SP, Blitstein JL. Design and analysis of group randomized trials: A review of recent methodological developments. American Journal of Public Health. 2004;94:423–432. doi: 10.2105/ajph.94.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center on Sleep Disorders Research. (NIH Publication No 11-7820).National Institutes of Health Sleep Disorders Research Plan. 2011 Retrieved from: http://www.med.umich.edu/umsleepscience/images/2011%20National%20Institutes%20of%20Health%20Sleep%20Disorders%20Research%20Plan.pdf.
- Netemeyer RG, Boles JS, McMurrian R. Development and validation of work-family conflict and family-work conflict scales. Journal of Applied Psychology. 1996;81:400–410. doi: 10.1037/0021-9010.81.4.400. [DOI] [Google Scholar]
- Nijp HH, Beckers DG, Geurts SA, Tucker P, Kompier MA. Systematic review on the association between employee worktime control and work–non-work balance, health and well-being, and job-related outcomes. Scandinavian Journal of Work, Environment & Health. 2012;38(4):299–313. doi: 10.5271/sjweh.3307. [DOI] [PubMed] [Google Scholar]
- Nijp HH, Beckers DG, Kompier MA, van den Bossche SN, Geurts SA. Worktime control access, need and use in relation to work-home interference, fatigue, and job motivation. Scandinavian Journal of Work, Environment & Health. 2015;41(4):347–355. doi: 10.5271/sjweh.3504. [DOI] [PubMed] [Google Scholar]
- NIOSH. Caruso CC, Geiger-Brown J, Takahashi M, Trinkoff A, Nakata A. NIOSH training for nurses on shift work and long work hours. 2015 May; Retrieved from www.cdc.gov/niosh/docs/2015-115/
- Nylen L, Melin B, Laflamme L. Interference between work and outside-work demands relative to health: Unwinding possibilities among full-time and part-time employees. International Journal of Behavioral Medicine. 2007;14:229–236. doi: 10.1007/BF03002997. [DOI] [PubMed] [Google Scholar]
- Olson R, Crain TL, Bodner TE, King R, Hammer LB, Klein LC, Buxton OM. A workplace intervention improves sleep: Results from the randomized controlled Work, Family, and Health Study. Sleep Health. 2015;1:55–65. doi: 10.1016/j.sleh.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philibert I. Sleep loss and performance in residents and nonphysicians: A meta-analytic investigation. SLEEP. 2005;28:1392–1402. doi: 10.1016/s8756-3452(08)70481-x. [DOI] [PubMed] [Google Scholar]
- Prentice DA, Miller DT. When small effects are impressive. Psychological Bulletin. 1992;112(1):160–164. doi: 10.1037/0033-2909.112.1.160. [DOI] [Google Scholar]
- Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 2011;15:259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine. 2008;4:487–504. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2576317/ [PMC free article] [PubMed] [Google Scholar]
- Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. SLEEP. 2006;29:206–216. doi: 10.1093/sleep/29.2.206. Retrieved from http://www.journalsleep.org/ [DOI] [PubMed] [Google Scholar]
- Semmer NK. Job stress interventions and organization of work. In: Quick JC, Tetrick LE, editors. Handbook of occupational health psychology. Washington, DC: American Psychological Association; 2011. pp. 299–318. [Google Scholar]
- Shediac-Rizkallah MC, Bone LR. Planning for the sustainability of community-based health programs: Conceptual frameworks and future directions for research, practice and policy. Health Education Research. 1998;13:87–108. doi: 10.1093/her/13.1.87. [DOI] [PubMed] [Google Scholar]
- Smith CS, Folkard S, Tucker P, Evans MS. Work schedules, health, and safety. In: Quick JC, Tetrick LE, editors. Handbook of occupational health and safety. Washington, DC: American Psychological Association; 2011. pp. 185–204. [Google Scholar]
- Sorensen G, Stoddard AM, Stoffel S, Buxton O, Sembajwe G, Hashimoto D, Hopcia K. The role of the work context in multiple wellness outcomes for hospital patient care workers. Journal of Occupational and Environmental Medicine. 2011;53:899–910. doi: 10.1097/jom.0b013e318226a74a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi M, Iwasaki K, Sasaki T, Kubo T, Mori I, Otsuka Y. Worktime control-dependent reductions in fatigue, sleep problems, and depression. Applied Ergonomics. 2011;42(2):244–250. doi: 10.1016/j.apergo.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Thiart H, Lehr D, Ebert DD, Berking M, Riper H. Log in and breathe out: internet-based recovery training for sleepless employees with work-related strain – results of a randomized controlled trial. Scandinavian Journal of Work, Environment & Health. 2015;41(2):164–174. doi: 10.5271/sjweh.3478. [DOI] [PubMed] [Google Scholar]
- Thiart H, Ebert DD, Lehr D, Nobis S, Buntrock C, Berking M, Riper H. Internet-based cognitive behavioral therapy for insomnia: A health economic evaluation. Sleep. 2016;39(10):1769–1778. doi: 10.5665/sleep.6152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas LT, Ganster DC. Impact of family-supportive work variables on work-family conflict and strain: A control perspective. Journal of Applied Psychology. 1995;80:6–15. doi: 10.1037/0021-9010.80.1.6. [DOI] [Google Scholar]
- Uehli K, Mehta AJ, Miedinger D, Hug K, Schindler C, Holsboer-Trachsler E, Künzli N. Sleep problems and work injuries: A systematic review and meta-analysis. Sleep Medicine Reviews. 2014;18:61–73. doi: 10.1016/j.smrv.2013.01.004. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy People 2020 Objective Topic Areas and Page Numbers. 2010 [updated 2011/01/04/; 300-1]. Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/default.aspx.
- Van Horn ML, Bellis JM, Snyder SW. Family resource scale-revised: Psychometrics and validation of a measure of family resources in a sample of low-income families. Journal of Psychoeducational Assessment. 2001;19:54–68. doi: 10.1177/073428290101900104. [DOI] [Google Scholar]
- Van Laethem M, Beckers DG, Kompier MA, Dijksterhuis A, Geurts SA. Psychosocial work characteristics and sleep quality: A systematic review of longitudinal and intervention research. Scandinavian Journal of Work, Environment & Health. 2013;39:535–549. doi: 10.5271/sjweh.3376. [DOI] [PubMed] [Google Scholar]
- Varnell SP, Murray DM, Janega JB, Blitstein JL. Design and analysis of group-randomized trials: A review of recent practices. American Journal of Public Health. 2004;94:393–399. doi: 10.2105/ajph.94.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner DT, Barnes CM, Lim VKG, Ferris DL. Lost sleep and cyberloafing: Evidence from the laboratory and a daylight saving time quasi-experiment. Journal of Applied Psychology. 2012;97:1068–1076. doi: 10.1037/a0027557. [DOI] [PubMed] [Google Scholar]
- Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Tasali E. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of s for a healthy adult: Methodology and discussion. Journal of Clinical Sleep Medicine. 2015;11:931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh DT, Ellis APJ, Christian MS, Mai KM. Building a self-regulatory model of sleep deprivation and deception: The role of caffeine and social influence. Journal of Applied Psychology. 2014;99:1268–1277. doi: 10.1037/a0036202. [DOI] [PubMed] [Google Scholar]
- Winkelman JW, Buxton OM, Jensen JE, Benson KL, O’Connor SP, Wang W, Renshaw PF. Reduced brain GABA in primary insomnia: Preliminary data from 4T Proton Magnetic Resonance Spectroscopy (1H-MRS) Sleep. 2008;31(11):1499–1506. doi: 10.1093/sleep/31.11.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, Baime M. Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. Journal of Occupational Health Psychology. 2012;17:246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, Pilkonis PA. Development of short forms from the PROMIS™ Sleep Disturbance and Sleep-Related Impairment Item Banks. Behavioral Sleep Medicine. 2012;10(1):6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]