Introduction
Prescription drug misuse (PDM) has increased steadily over the past two decades (McCabe, West, & Wechsler, 2007; Substance Abuse and Mental Health Services Administration [SAMHSA], 2007). Approximately 15 million people reported past year PDM (SAMHSA, 2015a). PDM is the non-medical use of prescription drugs including using drugs in other ways than intended or to get high. Classes of prescription drugs commonly abused include opioids, depressants, and stimulants (SAMHSA, 2013). Prescribed medications have a lower perceived risk of harm and stigma (Fleary, Heffer, & McKyer, 2013; Quintero, Peterson, & Young, 2006), but their misuse can be even more dangerous than some illicit drugs. The dangers of PDM include addiction, overdose, and increased risky sexual and risk-taking behaviors (National Institute on Drug Abuse [NIDA], 2015; Paulozzi, Kilbourne, & Desai, 2011).
The stigma of PDM is low due to the perceived safety and availability (Fleary, Heffer, McKyer, 2013; SAMHSA, 2014a). Prescription drugs are perceived as legal or quasi-legal and easily accessible in comparison to street drugs (Garnier, Arria, Caldeira, Vincent, O’Grady, & Wish, 2010). The overprescribing practices of some doctors also increase the accessibility of prescriptions (Paulozzi, Mack, & Hockenberry, 2014). Through diversion, or transferring legally prescribed controlled substances to illegal markets, people attain prescriptions through theft, forgery, doctor shopping and mail-order pharmacies (Inciardi, Surratt, Cicero, Kurtz, Martin, & Parrino, 2009). These practices may continue to fuel the PDM epidemic.
Pharmaceutical companies spend $5.2 billion annually on drug advertising (Picchi, 2016). To counteract their efforts, state, federal, and targeted interventions have been initiated to curb the PDM epidemic including health professional education, prescription drug monitoring programs, the development of prescription opioids with abuse-deterrent qualities, and media campaigns (Cicero, Ellis, & Surratt, 2012; Department of Health and Human Services, 2013; National Governor’s Association, 2012; Office of National Drug Control Policy Executive, 2011; SAMHSA, 2017). However, media prevention efforts are sparse and many are untested (SAMHSA, 2017). Despite limitations, the evidence suggests that opioid prescribing practices steadied between 2010 and 2012 (Levy, Paulozzi, Mack, & Jones, 2012). The rate of overdose deaths also declined during that time from 16,652 in 2010 to 16,007 in 2012, but rallied in 2014 with 18,893 deaths (Centers for Disease Control and Prevention, 2015). This highlights the need to consider alternative approaches.
Substance abuse interventions are not always equally effective across populations (Becker, Stein, Curry, & Hersh, 2012; Calsyn, Burlew, Hatch-Maillette, Wilson, Beadnell, & Wright, 2012) and those developed for abusable prescriptions may not have considered cultural differences. For example, many racial/ethnic groups have a collectivist culture whereby sharing is commonplace (Brewer & Chen, 2007). Existing interventions may not target prescription sharing among family and friends, but rather focus on locking up drugs or other strategies (SAMHSA, 2017). Further, there is a high rate of glamorization of prescription pills in urban pop culture and black market infiltration of prescriptions into urban communities (International Narcotics Board, 2015; Rehab International, 2017) yet these problems have not been the target of any identified research inquiry. Media ads also have a history of racial profiling such as the recent smoking campaigns targeted urban communities (Kirchner et al., 2015). These patterns suggest that more evidence of the impact of PDM in racial/ethnic minorities is warranted.
Golub, Johnson, and Dunlap (2005) postulated the theory of subcultural evolution, which conceptualizes the development of drug eras or epidemics especially among inner-city populations. The theory highlights the cultural processes that underlie the development of drug abuse subcultures. Substance abuse is thought to result from the convergence of individual identity development and the predominant culture in that both emerge from availability, symbolic significance, and the social effects of use or non-use. The four phases within a drug era include: (1) incubation, drug abuse begins within a select subgroup; (2) expansion, new drugs are introduced to the larger population; (3) plateau, those most at risk have or will initiate use with the new drug (e.g., substance abusers, youth) and; 4) decline, the drug loses popularity and is seen as outdated. Based on this theory, PDM likely falls within phase two or three and suggests that more research on subcultures is required.
The literature on PDM is sparse and primarily correlation; however, the varied motivations for use have been described. Rigg and colleagues (2010) identified motives for PDM that differed by race/ethnicity. Latinos were mostly likely to be motivated to engage in PDM to relieve anxiety or stress (OR = 3.59 [2.31, 5.56]) or to get high (OR = 1.46 [.91, 2.34]) than African Americans and Whites. African Americans reported seeking to mitigate the effects of other drugs more than Whites (OR = 2.06 [1.42, 3.01]). These findings suggest that subgroups of people of color, including those experiencing stress and engaging in polysubstance abuse, may have an increased risk for PDM that has been understudied in the literature.
According to the NIDA Research Report Series (2011), the patterns of use, correlates, and consequences are different for each class of drugs. For example, the report found that opioid pain relievers are the most commonly diverted prescription drugs. They have a large addiction potential and can result in respiratory depression and death. Central nervous system (CNS) depressants such as sedatives, tranquilizers, benzodiazepines, and non-benzodiazepines (sleep medications) inhibit brain activity. Each has the prospect of leading to abuse and death if used in conjunction with other substances particularly opioids (NIDA, 2011). Stimulants mimic neurotransmitters in the brain and cause euphoric sensations when taken recreationally. Despite the addiction potential, stimulants, such as Adderall, are commonly abused by academic professionals, students, athletes, and older adults (NIDA, 2011). In addition to prescriptions, over-the-counter drugs such as cold medicine and cough syrup are also commonly abused (NIDA, 2011). One study highlighted in the NIDA report found that in 2010, 6.6% of high schoolers reported having ingested cough syrup to get intoxicated. The report indicated that certain groups may be at an increased risk for PDM including girls (ages 12–17), young adults, and the elderly (NIDA, 2011). However, these findings overlook a critical, growing, and vulnerable segment of society, racial/ethnic minorities (Mechanic & Tanner, 2007; U.S. Census Bureau, 2015).
Racial/ethnic minorities exist in each of the aforementioned risk groups (females, young adults, and the elderly) yet limited research on PDM includes diverse samples. However, drawing on the extant literature, several known sociodemographic links to PDM may be particularly salient for racial/ethnic minorities. For example, racial/ethnic minorities are enrolling in college at high rates (Krogstad & Fry, 2014) and college students are known to have high rates of PDM (Johnston et al., 2011). Socioeconomic status and unemployment are also associated with PDM (Beyene, Sheridan, & Aspden, 2014) and people of color are overrepresented among the lower social strata and have higher unemployment rates (Bureau of Labor Statistics, 2016; Institute for Research on Poverty, 2016). Race/ethnicity is a social construct and may be a proxy for other differences such as economic, systemic, and life experiences. For example, “pharmacy deserts” or regions with limited access to pharmacies, are prevalent in urban communities (Qato et al., 2014), which have higher concentrations of racial/ethnic minorities (Institute for Research on Poverty, 2016). These access barriers may not be race/ethnicity-related, but could exacerbate PDM. Though diversion is most common between family and friends, recent data from the International Narcotics Control Board (2015) suggests that prescription drugs are increasingly prevalent in urban areas and the second most popular substance in the drug trade market.
Despite the extensive concern about PDM within the research community (Volkow, 2008), little is known about the incidence, prevalence, and correlates of PDM among racial/ethnic minorities. Over a third of the U.S. population identifies as a racial/ethnic minority and that number is expected to grow exponentially (U.S. Census Bureau, 2015). The existing literature finds that racial/ethnic minorities tend to engage in PDM less often than Whites (Arkes & Iguchi, 2008; Cicero, Kurtz, Surratt, Ibañez, Ellis et al., 2011; McCabe, West, Teter, & Boyd, 2014). Race/ethnicity has been identified as a protective factor in several studies (Schepis & Krishnan-Sarin, 2008; Young, Glover, & Havens, 2012). Also, Harrell and Broman (2009) found that among African Americans, religious attendance was a protective factor against PDM. However, there are disparate consequences for people of color that abuse illicit drugs (Feldstein Ewing, Venner, Mead, & Bryan, 2011). For example, African Americans and Latinos face more drug-related health disparities such as limited access to drug treatment and disparate quality of care (Wells, Klap, Koike, & Sherbourne, 2001), drug-related morbidity and mortality, and educational attrition (NIDA, 2003). They are more likely to receive longer jail sentences for drug-related crimes and are less likely to be sentenced to drug treatment (Demuth & Steffensmeier, 2004). In spite of these disparities, racial/ethnic minorities are underrepresented in substance abuse research and interventions (Shaya, Gbarayor, Yang, Agyeman-Duah, & Saunders, 2007; Waheed, Hughes-Morley, Woodham, & Bower, 2015). This gap also holds true in PDM research and the present review seeks to illuminate the prevalence and predictors in this population.
Identifying the Gaps
The utility of a systematic review on PDM in racial/ethnic minorities is multifaceted. Other reviews of PDM have focused on adolescents and have delineated the risk and protective factors (Nargiso, Ballard, & Skeer, 2015; SAMHSA, 2015b; Young, Glover, & Havens, 2012). No identified studies have systematically reviewed these factors in racial/ethnic minorities. These problems have been well-illuminated in the health disparities literature concerning other drugs and may also be reflected in the PDM epidemic. Examining these factors in racial/ethnic minorities can inform targeted interventions for health disparate populations. Two main objectives informed this review:
Identify the prevalence rates of PDM within racial/ethnic minority populations in the U.S.
Explore the correlates of PDM in racial/ethnic minority populations.
Method
Ethics Statement
The affiliated university Institutional Review Board deemed this study exempt since it did not directly involve human subjects. After exemption, the author conducted a systematic review of the empirical literature on PDM in racial/ethnic minorities.
Eligibility Criteria
The target populations included the five major racial/ethnic minority categories of the U.S. and included African Americans/Blacks, Latino/Hispanics, Asian Americans, American Indians/Alaska Natives, and Pacific Islanders (Pollard & O’Hare, 1999). However, no studies were identified that included Pacific Islanders, thus four groups remained. Studies using White comparison samples and race-specific studies were both included in this review. PDM was operationalized as any non-medically sanctioned use of prescription medication including using drugs in ways other than prescribed and using prescription drugs to get high. The prescription drugs of interest included: analgesics, anxiolytics, amphetamines, benzodiazepines, opioids, sedatives, stimulants, and tranquilizers. Due to the exploratory nature of this review, drugs that are not traditionally considered in PDM research were retained (e.g., sleep aids, diet pills).
Information Sources
Two of the top 10 academic research index directories were used to conduct this search (University of Cincinnati Libraries, n.d.; University of Wisconsin-Madison Libraries, n.d.). EBSCOhost was used to simultaneously search three databases including: Academic Search Complete, MEDLINE/PubMed and PsychINFO (EBSCOhost Online Research Databases, n.d.). Public Affairs Information Service (PAIS; ProQuest, n.d.) has 31 databases and was searched separately. The researcher indices were searched on three occasions between May of 2016 and September of 2017.
Search Strategy
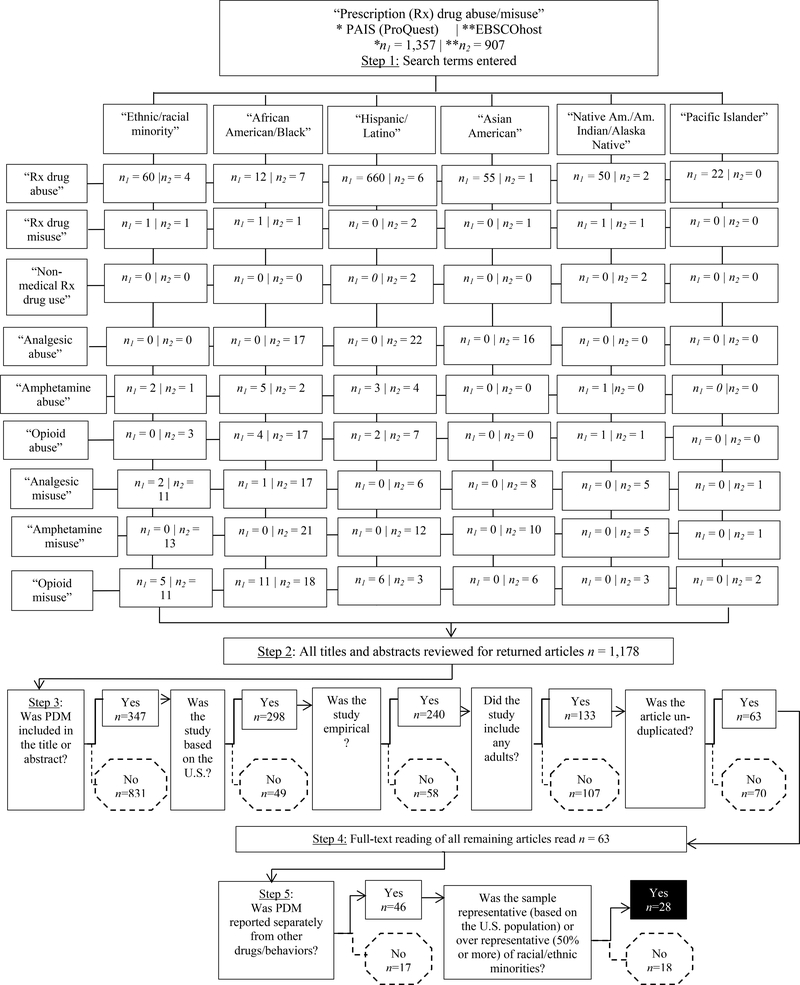
In Step 1, the author inputted 114 search combinations resulting in 1,507 articles (see Figure 1 for details). The initial search terms entered were “prescription drug abuse”, “prescription drug misuse”, and “nonmedical prescription drug use.” To enhance the thoroughness of the results, each drug of interest (analgesics, anxiolytics, amphetamines, benzodiazepines, opioids, sedatives, sleep drugs, stimulants, tranquilizers, and diet pills) was queried with both “abuse” and “misuse.” These main root terms with Boolean operators were searched in titles and abstracts. Each term was linked by the “AND” operator in conjunction with the following: “racial OR ethnic minority ”, “African American OR Black”, “Hispanic OR Latino”, “Asian American”, “Native American OR American Indian”, and “Pacific Islander.”
Limiters.
The following limiters were placed on the initial search combinations (see Figure 1 for a flowchart of the identification process): full-text, scholarly journals, English language, and human subjects. Limits were also set to identify peer-reviewed articles published between 2000 and 2017. No results were returned for the following drugs searches: anxiolytics, benzodiazepines, sedatives, sleep aids, stimulants, tranquilizers, or diet pills.
Abstract and Title Review
In Steps 2 and 3, the titles and abstracts of 1,178 articles were screened (see Figure 1 for article triage). Articles were omitted that did not include prescription drug abuse/misuse in either of those locations. Articles that did not include samples of U.S. populations were removed. Non-empirical articles such as conference abstracts/ presentations, epidemiological articles, commentaries, theses/dissertations, and unpublished reports were also excluded. Studies that did not include at least some adults ages 18 and older were eliminated. It is noteworthy that the scholarship of prolific PDM researchers (e.g., Boyd, C.; Harrell, Z.) focused among adolescents and is beyond the scope of this review. Lastly, about 6% of the returned results were duplicates identified in prior search combinations. At the completion of these two steps, 40 studies remained.
Full-text Review and Study Selection
In Step 4, the author read the full-text of each of the remaining articles (n = 40) and made further exclusions. A few studies purported to include PDM, but the results were combined with other illicit drugs (see Step 5 of Figure 1). Due to the exploratory nature of this review, prescription drugs that are uncommonly abused were retained (e.g., diet pills, antibiotics). Other studies were omitted that solely described factors associated with PDM such as physician prescribing practices, access, interventions, and diversion since they were beyond the confines of this inquiry. However, these studies were retained if prevalence or correlates of PDM were included (i.e., Goldsworthy et al., 2008; Ibañez et al., 2013; Kecojevic et al., 2015). Lastly, the author closely examined the demographic breakdown of the study samples. Studies with 50% or more racial/ethnic minorities were retained. Studies with representative samples that generally reflected the U.S. population were also included. These steps helped to ensure that the details about the prevalence or implications of PDM in racial/ethnic minorities could be extracted. A total of 28 articles were retained in the final stage.
The majority of the articles were available in full-text from the selected databases. For one article (Momper, Delva, & Reed, 2011), the lead author was contacted by email and provided the paper. One additional “recommended article” was suggested in ProQuest when downloading one of the selected articles. In addition, the author read the reference pages of all of the resulting articles and found one other study that met the inclusion criteria.
Data Extraction
Quantitative, qualitative, mixed-method, and case studies were all retained, which precluded conducting a meta-analysis of the study results. Moreover, the research design, sampling strategies, participant characteristics, measures, and procedures varied across the studies. In this review, the analysis consisted of reviewing the objectives, methods, and results of the identified studies and reporting findings corresponding to the objectives of the present study. The author followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISM; 2009) guidelines. Modified and reordered PICOS (participants, interventions, comparisons, outcomes, and study design) headings were used to sort the results (see Tables 1.1–1.4). Interventions were not the target of this review and the category omitted.
Table 1.1.
Summary of prescription (Rx) drug abuse articles including racial/ethnic minority adults (n = 14)
| Study | *Design and sample size | **Rx drugs | Primary measures | Key findings |
|---|---|---|---|---|
| [1] Arkes et al. (2008) | Secondary analysis; n = 164,87 U.S. representative sample; demographic breakdown for race/ethnicity likely reflects U.S. population | AN, ST | Nat’l Survey on Drug Use and Health | Racial/ethnic minority adults were less likely to abuse painkillers and stimulants compared to Whites. |
| [2] Bali et al. (2013) | Secondary analysis; n = 15,509,703; 25% African American, Latino, and Other racial/ethnic minorities | AN, T, ST, SE | Nat’l Survey on Drug Use and Health | Higher rates of Rx drugs among Latinos with health insurance versus the uninsured. |
| [3] Cicero et al. (2011) | Secondary analysis; n = 1,983 diagnosed opioid substance abusers; 5.2% African American, 4.2% Latino, 8.1% Other/Unknown | O | Survey of Key Informants Patient's (SKIP) | Immediate release oxycodone was the primary opioid abused. Racial/ethnic minorities were less likely to be opioid abusers than Whites. |
| [4] Goldsworthy et al. (2008) | Qualitative; n = 700 adults across the U.S.; 24.3% African American, 24.1% Hispanic, and 1% Asian | Interviews | 23.5% of African Americans, 23.1% of Latinos, and 30.4% of others reported taking prescriptions that belong to someone else. | |
| [5] Ibañez et al. (2013) | Non-experimental; n = 1,207; 23% African American, 23% Latino, and 5% Other racial/ethnic minority | B | Global Appraisal of Individual Needs | African Americans and Latinos had lower rates of benzodiazepine use compared to Whites. |
| [6] Martins et al. (2015) | Secondary analysis; n = 36,781 young adults nationwide; demographic breakdown for race/ethnicity likely reflects U.S. population | O, ST | Nat’l Survey on Drug Use and Health | African Americans, Asians, and Latinos were less likely to misuse Rx opiates/stimulants compared to Whites. For Latinos, the risk of Rx misuse of opioids was minimal across education levels. The relationship between educational attainment and risk of Rx misuse was pronounced among Native Americans/Pacific Islanders and Asian Americans though not dissimilar from Whites. |
| [7] McCabe (2005b) | Secondary analysis; n = 10,904 college students; 7.7% Latino, 7.2% African American, 7.6% Asian American, and 8.6% Other | B, AX | Harvard School of Public Health College Alcohol Study survey | 3.6% of African Americans, 3.6% of Asian Americans, 3.9% of Latinos, and 6.6% of others reported lifetime use of Rx benzodiazepine anxiolytics. Past year use ranged from 2.2% to 4.1% among racial/ethnic minorities. |
| [8] McCabe et al. (2007a) | Secondary analysis; n = 54,567 college students; 2% at HBCUs | AM, O, SE, T | College Alcohol Study | Students at historically Black colleges (HBCU's) had a significant increase in non-medical Rx drug use between 1993 and 2001. |
| [9] McCabe et al. (2007b) | Secondary analysis; n = 43,093 general population; 12% Latino, 11.5% African American, 4% Asian, and 2% Native American/Other | T, SE, ST, O, | Nat’l Epidemiologic Survey on Alcohol and Related Conditions | The odds of lifetime Rx abuse and dependence is lower for African Americans and Asian Americans and is slightly higher for Latinos and Native Americans compared to Whites. |
| [10] McCabe et al. (2014) | Secondary analysis; n = 21,771 undergraduates; 13% Asian American, 6% African American, 4% Latino, and 10% Other race/ethnic | SL, SE, ST, O, and other | College Student Life Survey | No significant changes in Rx drug abuse among racial/ethnic minorities including Asian Americans, African Americans, Latinos, or Others between 2003 and 2013. |
| [11] Varga et al. (2015) | Cross-sectional; n = 1,015 graduate students; .7% American Indian, 11% Asian, 5% African American, and 2% Latino | ST | Online survey developed from Monitoring the Future | The majority of illicit users were White (91%) followed by two African American participants, one Asian, four American Indians, and two Hispanics. |
| [12] Wang et al. (2013) | Secondary analysis; n = 75,964 rural U.S. residents; 11% African American, 14.1% Latino, and 6.6% Other race/ethnicity | O | Nat’l Survey on Drug Use and Health | Urban residents who were African American and Latino were less likely to abuse Rx opioids |
| [13] Wu et al. (2010) | Secondary analysis; n = 43,093 general population; 12% Latino, 11.5% African American, 4% Asian, and 2% Native American/Other | O | Nat’l Epidemiologic Survey on Alcohol and Related Conditions | Nonmedical opioid use was lower among African Americans, Asian Americans, and Latinos, but higher among Native Indian/Alaska Natives in comparison to Whites. |
| [14] Vietri et al. (2014) | Quantitative; n = 1,242 opioid abusers, 58.4% women | O | Work Productivity and Activity Impairment questionnaire | Ethnic/racial minorities had significantly more prescription opioid abuse in the past 3 months than Whites. |
Note:
The sample characteristics and findings highlight data for racial/ethnic minorities in the sample and may not include primary findings of the study.
Rx abbreviations are as follows; AN=analgesics, AX= anxiolytics, AM=amphetamines, B=benzodiazepines, O=opioids, SE=sedatives, SL=sleep, ST=stimulants, T=tranquilizers
Table 1.4.
Summary prescription (Rx) drug abuse articles with Asian American and American Indians/Alaska Native participants (n = 3)
| Study | *Sample characteristics | **Rx drugs | Primary measures | Key findings |
|---|---|---|---|---|
| Asian Americans | ||||
| [26] Bardhi et al. (2007) | Case study; n = 12 prescription pill using women; One Asian American | Unspecified | Qualitative data | One case described a 30-yr-old, 2nd generation Chinese woman who reported that her misuse was in rebellion against strict parents. She initiated use during pharmacy school and dropped out to become an artist. |
| [27] Gee et al. (2007) | Cross-sectional; n = 2,217 Filipino Americans | AN, SE, T, ST | Filipino American Community Epidemiological Study | 10% of the sample had misused analgesics, 5% stimulants, 3.6% sedatives, and 2.1% tranquilizers. Prescription drug abusers reported more frequent daily experiences of unfair treatment compared to non-users. |
| American Indian/Alaska Native | ||||
| [28] Momper et al. (2011) | Qualitative; n = 49 American Indian youth and adults | O | Emergent design with tribal leader feedback | During the talking circles, or focus groups, tribal members reported increased use of OxyContin. Prescription drug misuse was perceived as having a negative effect on individuals, families, and the community, or tribe. |
Note:
The sample characteristics and findings highlight data for racial/ethnic minorities in the sample and may not include primary findings of the study.
Rx abbreviations are as follows; AN=analgesics, AX= anxiolytics, AM=amphetamines, B=benzodiazepines, O=opioids, SE=sedatives, SL=sleep, ST=stimulants, T=tranquilizers
The findings for each of the remaining studies (n = 28) were sorted by racial/ethnic group and alphabetized (see Table 1.1–1.4). Studies including racial/ethnic minorities in equivalent or population-based proportions were classified as general, whereas those with an overrepresentation from one racial/ethnic group received a race-specific classification. Articles with special details on a particular racial/ethnic group were also classified as race/ethnic-specific regardless of percent of the representation. This review reports key findings that are inclusive of racial/ethnic minorities and not necessarily the general findings of the studies. The author then summarized the correlates of PDM across studies alphabetically (see Table 2).
Table 2.
PDM correlates among U.S. racial/ethnic minorities in national representative and targeted studies published between 2000–2017 (alphabetical)
| Correlates of PDM |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Author(s) | Minority status | Age | Gender | Other SA | No H.S. | Unwed | Uninsured | Unemployed | Low income | Health/ well-being | Other correlates |
| [1] | Arkes et al | α | 26–39 | ns | α | α | α | α | α | - | - | |
| [2] | Bali et al | ns | Y | M | α | α | α | α | α | α | - | |
| [26] | Bardhi et al | - | - | - | - | - | - | - | - | - | - | |
| [15] | Barry et al | α | 40–44 | - | α | α | ns | - | - | α | α | |
| [18] | Buttram et al | - | - | - | - | - | - | - | - | - | - | Demographics predicted for alt. routes of admin |
| [3] | Cicero et al | W | - | - | - | - | - | - | - | - | - | |
| [19] | Coffman et al | - | - | - | - | - | - | - | - | - | Healthcare barriers, cultural norms, and self-care | |
| [20] | Cohen et al | - | ns | - | - | - | α | - | - | - | ||
| [21] | Ford et al | α | 18–25 | M | α | - | - | α | - | α | α | |
| [27] | Gee et al | - | ns | ns | - | - | - | - | - | - | α | Nativity; ethnic identity |
| [4] | Goldsworthy et al | - | ns | ns | - | - | - | - | - | - | - | English speakers; high health literacy |
| [5] | Ibañez et al | W | - | - | - | - | - | - | - | - | - | |
| [16] | Kecojevic et al | ns | 18–29 | - | - | - | - | - | - | - | α | Bisexuals; survivors of childhood abuse |
| [22] | Kurtz et al | ns | ns | M | α | ns | - | - | ns | - | α | Ever arrested; same sex attraction; early onset of SA; prior drug treatment |
| [23] | Kurtz et al | - | Y | ns | α | ns | - | - | - | - | α | |
| [24] | Larson et al | - | - | - | - | ns | - | α | - | α | - | Contextual factors lead to self-prescription |
| [6] | Martins et al | ns | - | M | - | α | - | - | - | - | α | |
| [7] | McCabe | W | 24+ | - | - | - | - | - | - | - | - | Additional correlates exist for college students |
| [8] | McCabe et al | - | - | - | α | - | - | - | - | - | - | Additional correlates exist for college students |
| [9] | McCabe et al | ns | Y | M | α | - | ns | - | - | - | - | Early initiators; family history of alcoholism |
| [10] | McCabe et al | W | - | M | - | - | - | - | - | - | - | Additional correlates exist for college students |
| [28] | Momper et al | - | - | - | - | - | - | - | α | - | α | |
| [25] | Muñoz-Laboy et al | - | - | - | - | - | - | - | - | - | α | |
| [17] | Peters et al | - | Y | ns | α | α | ns | - | ns | ns | - | |
| [11] | Varga et al | W | 23–29 | F | α | - | - | - | - | α | α | Additional correlates exist for graduate students |
| [14] | Vietri et al | α | Y | M | α | - | - | - | ↔ | ↔ | α | |
| [12] | Wang et al | W | Y | M | α | α | α | α | α | α | α | |
| [13] | Wu et al | W | 18–29 | M | α | ns | α | - | - | α | - | History of SA treatment |
Note: PDM = prescription drug misuse; W = White; Y = younger; F = female; M = male; SA = substance abuse; H.S. = high school; α= statistical significance; ns = not significant; ↔ = inverse; - = not measured.
Data Analysis
Quantifiable data was calculated using SPSS version 23. The percentages, measures of central tendency, and standard deviations were computed to describe and summarize the numerical data. Qualitative data was processed in three ways: (1) pre-specified, data was categorized under pre-determined categories (e.g., race/ethnicity); (2) open, emergent categories were created as the data was inspected (e.g., categories for correlates of PDM) and; (3) patterned, reoccurring emergent themes were identified.
Results
In this section, three types of results are described. First, a descriptive analysis of the article type, region, and prescription drugs of interest are provided. The prevalence of PDM by general and then race/ethnicity-specific studies are then summarized. Last, the findings on the correlates of PDM are presented.
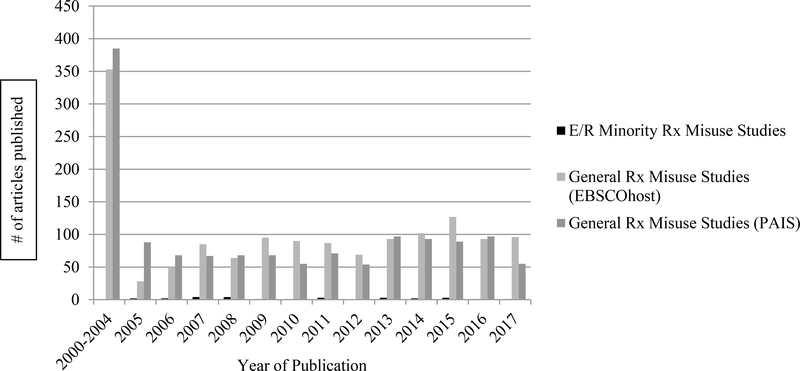
Article Descriptives
Of the 2,264 full-text, peer-reviewed articles returned on PDM between 2000 and 2017, a total of 1,178 (52%) purported to include racial/ethnic minorities. At the conclusion of the screening process, 28 (2.4%) of the articles described prevalence and correlates of PDM within these populations. Figure 2 depicts a graphical comparison of the identified studies on racial/ethnic minority PDM in comparison to a general search of “prescription drug misuse” on EBSCOhost and PAIS. Research on racial/ethnic minority prescription drug abusers was completely absent from the literature between 2000 and 2005. Based on the first author affiliations, the majority of the studies were conducted in the North/Northeast (32.1%; e.g., New York) and South (32.1%; e.g., Florida). The Midwest had eight studies and only two studies were conducted in the West. Over half (53.6%) of the studies investigated multiple prescription drugs. Analgesics and opioids were studied in 50% (n = 14) studies. Stimulants were examined in 42.8% of the investigations, followed by sedatives (35.7%), and tranquilizers (21.4%; see Table 3 for details).
Table 3.
Study descriptives
| Variable | N (%) |
|---|---|
| Study Location* | |
| West | 3 (7.1) |
| Midwest | 8 (28.6) |
| South | 9 (32.1) |
| North/Northeast | 9 (32.1) |
| Study Drugs** | |
| Analgesics (AN)/Opioids (O) | 14 (50) |
| Amphetamines (AM) | 1 (3.6) |
| Anxiolytics (AX) | 1 (3.6) |
| Benzodiazepines (B) | 3 (10.7) |
| Sedatives (SE) | 10 (35.7) |
| Sleep aids (SL) | 1 (3.6) |
| Stimulants (ST) | 12 (42.8) |
| Tranquilizers (T) | 6 (21.4) |
| Other/Unspecified | 5 (17.9) |
Note.
Location determined by author affiliation provided in manuscripts or search engine
Categories are not mutually exclusive and do not total 100%.
Prevalence of PDM by Racial/Ethnic Group
General studies.
Fourteen studies included outcome data on racial/ethnic groups with representative samples. The samples ranged in size from 700 to 15,509,703 (Median = 19,129; SD = 4,138,862.19) participants. Four (28.6%) articles used samples from various years of the National Survey on Drug Use and Health ([NSDUH]; see Table 1.1–1.4 for article numbering; 1, 2, 6, 12, 5]. Two (14.3%) used data from the National Epidemiological Survey on Alcohol and Related Conditions [9, 13]. The remaining studies used national, adapted, and researcher developed surveys. The overwhelming majority of studies (n = 10; 71.4%) were secondary data analyses. The general studies also had predominately White samples, with one study reporting representation at 51% [5]. One study (Ibañez, Levi-Minzi, Rigg, & Moss, 2013) had equal representation of African Americans and Latinos (23%). The outcomes focused on diversion, but it is noteworthy that participants reported obtaining an average of 51 to 672 pills in the past 90 days. One qualitative study (Goldsworthy, Schwartz, & Mayhorn, 2008) also had high representation of racial/ethnic minorities (49.4%) and reported elevated rates of participants taking medication other than prescribed with allergy medicine most common (25.3%), followed by pain medicine (21.9%), and antibiotics (20.6%). Three studies omitted sample demographic breakdowns [1, 6, 14], but either used nationally representative surveys or reported outcomes by race/ethnicity.
African Americans and PDM.
Three studies were identified that included predominately African American participants [15–17]. The sample sizes totaled 4,795 (M = 1,599) and ranged from 51% [58] to 100% [56] African American. The populations were very diverse and included veterans, crack users, and bisexual and heterosexual adults. The measures used in the studies included a mix of author-generated and standardized instruments. Opioid abuse was examined in all three studies with the addition of stimulants and tranquilizers in one study [16].
Barry and colleagues (2011) found that 13% of the sample reported engaging in the non-medical use of prescription opioids. Users also had significantly higher rates of HIV infection than non-users (60% vs. 52%; p < .05). Kecojevic, Wong, Corliss, and Lankenau (2015) studied young men who have sex with men (MSM) and also abused prescriptions. The researchers found that psychosocial risks such as childhood abuse, perceived stress, and homophobia/racism were associated with higher rates of PDM. Lastly, Peters and colleagues (2007) found that among crack users, polysubstance codeine misusers were less likely to have a main sexual partner and had higher rates of marijuana use (p = .05). Overall, the key findings revealed higher rates of prescription PDM among the samples with larger representation of African Americans than general samples.
Latino/as and PDM.
The eight studies on Latino/Hispanic populations had representation ranging from 17.5% [21] to 100% [19, 20, 24, 25]. The study on the lower end of the spectrum of representation included separate analyses for Latinos and was thus included in this category. There were a total of 38,602 participants (M = 4,825) across studies. Three studies specifically investigated opioid/analgesics, stimulants, and sedatives [18, 21, 25]. Other less commonly abused drugs were also studied including prescription diet pills [20], club drugs [22], and antibiotics [24]. The measures included a mix of researcher-generated surveys and standardized instruments (e.g., Global Appraisal of Individual Needs [GAIN], NSDUH).
Several studies provided evidence of health disparities as factors contributing to PDM in this population including prescription cost, lack of insurance, lower quality of care, and immigration status (Coffman, Shobe, & O'Connell, 2008; Larson, Dilone, Garcia, & Smolowitz 2006). Despite large representation of Latinos, language considerations were only investigated in one study [21]. Language may influence study measurement or serve as a proxy for acculturation (i.e., adapting to the dominate culture). Lastly, drugs that were barred in the U.S. remained accessible to a sample of Brazilian immigrants [20].
Asian Americans and American Indians and PDM.
Due to the small number of studies, the research on Asian Americans and American Indians and PDM were described together in Table 1.4. Representation ranged from one individual in a case study [26] to 100% Filipino American and American Indian [27, 28]. Two studies included Asian Americans (n = 2,229; M = 1,114.5), whereas the study on American Indians had a sample size of 49.
Gee, Delva, and Takeuchi’s (2007) research on Filipino Americans revealed that 10% of the sample endorsed analgesic abuse followed by stimulants (5%), sedatives (3.6%), and tranquilizers (2.1%). The study further suggested that psychosocial factors, such as unfair treatment, may lead to coping mechanisms such as PDM (b = .14, SE = .07). In the case study [26], the other 11 women in the study were White and thus the “predominate” ethnic group was the sole Chinese American in the study. The subject reported early exposure to PDM but experienced a delayed onset of problematic use. Only one identified study focused on PDM in indigenous population [28]. No specific data on the prevalence of PDM was reported, but data collected from the “talking circles” indicated an increase in OxyContin abuse.
Correlates of PDM in Racial/Ethnic Minority Populations
Racial/ethnic minority status.
All of the identified studies included race/ethnicity as a predictor or the primary study population. Varied groupings by ethnicity (e.g., “White” and “Other” vs. “White”, “Black”, Hispanic, Asian/Pacific Islander, “Native American/Alaskan”, and “Other”) and prescription drug of interest made comparisons difficult. Seven of the studies reported that Whites abuse prescription drugs at higher rates than people of color [3, 5, 7, 10–13]. Four studies found that one or more classes of drugs were abused at higher rates by racial/ethnic minorities than Whites [1, 14,15, 21] and five studies found no significant differences [2, 6, 9,1 6, 22]. All of the studies that found that Whites had higher rates of PDM were general rather than race/ethnicity specific.
Age.
All studies in this review included adult populations, with a few including adolescents. The age of adults ranged from 18–50 and was measured both categorically and continuously. To facilitate comparisons in the present review, younger was operationalized as 18–29 years of age. Eleven studies, that included age as a correlate, found that younger participants had higher rates of PDM [2, 7, 9, 11–14, 16, 17, 21, 23]. Four studies found no significant differences in PDM by age [4, 20, 22, 27]. Age was more often measured in the general rather than race/ethnic specific studies. Longitudinal and lifespan studies of PDM were wholly absent.
Gender.
Of the 15 of the identified studies that examined gender differences in PDM, over half (n = 9) reported that males were more likely to engage in PDM [2, 6, 9, 10, 12–14, 21, 22]. Gender was not a significant predictor in five studies [1, 4, 17, 23, 27]. One study found that female graduate students (57%) were more likely to abuse stimulants than males (41%; [11]).
Other substance abuse.
Polysubstance abuse is a common and confounding problem in substance abuse research. Half of the studies (n = 14) examined other substances as a correlated of PDM and all of them found a statistically significant relationship [1, 2, 8, 9, 11–15, 17, 21–23]. Abuse of other drugs included other prescriptions, marijuana, alcohol, crack and others.
Education.
Ten studies measured education as a correlate of PDM. A lack of a high school education predicted PDM in six studies [1, 2, 6, 7, 12, 15] and was not significant in four [17, 22–24]. Sean McCabe and colleagues found unique risks for PDM among college students including sorority/fraternity membership, school type (i.e., predominately White institutions [PWI] vs. historically Black colleges and universities [HBCUs]), and commuter status [7, 8, 10]. One study found that graduate students abused prescription drugs nearly twice the rate of undergraduates in other studies at 15% vs. 8.1% respectively [11]. School region or differences by gender composition were not assessed in any of the investigations.
Marital status.
Five studies found that unwed adults were more likely to engage in PDM [1, 2, 12, 13, 20]. Three studies found no significant differences by marital status [9, 15, 17]. Marriage types such as common law, partnered, cohabitation or the health of marriages were not evaluated.
Insurance coverage.
All of the studies that reported insurance status found that the uninsured had significantly higher rates of PDM [1, 2, 12, 21, 24]. One study found that the uninsured were more likely to acquire prescription drugs from non-healthcare sources [5]. The amount of coverage, plan type (e.g., HMO, high-deductible), and prescription coverage was not differentiated in any of the studies. However, Bali, Raisch, Noffett, and Khan (2013) compared public versus private insurance and found interaction effects. Specifically, Hispanics with private insurance were more likely to engage in PDM than those with public insurance (OR = 1.24, p = .001).
Employment status.
Unemployment was associated with PDM in four studies [1, 2, 12, 28] and was inversely related in one study [14]. Two studies found no significant differences between employed and unemployed participants [7, 22]. Across studies, employment status was conceptualized very narrowly and did not differentiate students, housewives, those laid off, or those unable to work in many cases.
Income.
Comparisons on income status were problematic given that it was measured both continuously and categorically. To facilitate comparisons, low income was herein defined as below $30,000, not adjusting for household size. Seven studies in this review found that lower income predicted PDM [2, 11–13, 15, 21, 24]. Conversely, Vietri, Joshi, Barsdorf, and Mardekian (2014) found that higher income was associated with PDM. One study found no significant differences in PDM by income [17].
Health and emotional issues.
A variety of health and emotional conditions were found to predict PDM including physical pain, mental illness (e.g., depression), and stress. All of the studies that included health and emotional predictors (n = 12) found that they significantly predicted PDM [6, 11, 12, 14, 15, 21–23, 25, 27, 28]. McCabe and colleagues (2007b) also found that family history of alcoholism predicted PDM. Two studies found that a history of substance abuse treatment was also a predictor of PDM [13, 22].
Other correlates.
Two studies explored cultural factors that predicted PDM such as nativity and racial/ethnic identity [19, 25]. Another study compared English-speakers to non-English speakers and found higher rates of PDM among the former [4]. Early initiation of substance abuse was identified as a correlate of PDM in two studies [9, 22]. Lastly, two studies found that same sex attraction and bisexuality predicted PDM [16, 24].
Discussion
The objective of this review was to investigate the prevalence and correlates of PDM among racial/ethnic minorities. The findings yielded 28 studies that provided a closer examination of the evidence.
The Prevalence of PDM in Racial/Ethnic Minorities
The first aim of this review was to identify the prevalence of PDM in understudied populations. The findings indicated that racial/ethnic minorities are represented in a fraction of the PDM literature. This is particularly significant since racial/ethnic minorities make up over a third of the U.S. population (U.S. Census Bureau, 2015). Based on the data in Figure 2, research on racial/ethnic minorities was completely absent at the dawn of the epidemic between 2000 and 2005 (Volkow, 2014). Many of the studies were secondary data analyses of large, nationally representative samples. The use of secondary data has several limitations: (1) the research questions tend to be data-driven, (2) the samples may not be reflective of high-risk groups, and; 3) confounding variables may be excluded (Cheng & Phillips, 2014). The nationally representative studies showed low rates of PDM in racial/ethnic populations yet target studies showed much higher rates of problematic use in subgroups. This suggests that there were limitations in the secondary data. The studies may also be regionally unrepresentative. For example, the affiliated institutes of the first authors were primarily located in the Midwest, South, and North/Northeast yet there are large Latino populations in the West (Pew Research Center, 2014a). These gaps suggest that the existing research may not be exhaustive or representative of the full scope of the prescription drug epidemic.
Generally, the findings were consistent with other reviews that report that Whites engage in more PDM (Young, Glover, & Haves, 2012); however, the findings may minimize the intricacy of the problem. The studies with larger samples of racial/ethnic minorities alluded to high-risk subpopulations such as veterans, college students, and bisexual and gay young adults. Veterans have higher rates of PDM (11%) than civilians (NIDA, 2013) and racial/ethnic minorities make up 40% of active-duty military (Pew Research Center, 2017). PDM is a well-established problem among college students (SAMHSA, 2007) and racial/ethnic minorities are enrolling in universities at high rates (Pew Research Center, 2014b). Lesbian, gay, and bisexual young adults have an earlier initiation into PDM than heterosexuals (Kecojevic, Wong, Schrager, Silva, Jackson Bloom, Iverson et al., 2012) and the additional layer of race/ethnicity may add complexities such as perceived homophobia and racism and contribute to drug use. The findings within these subgroups supports the notion that the PDM epidemic may be in the expansion phase of the theory of subcultural evolution (Golub, Johnson, & Dunlap, 2005) and that subpopulations of racial/ethnic minorities require more in-depth analysis.
The outcomes also suggest that cultural factors should be considered in research and interventions on PDM. Health disparities such as differential accessibility and perceived lower quality of care may drive racial/ethnic minorities towards prescription sharing and underground markets (e.g. street dealers, mail-order). Language barriers were only considered in one study (Cohen McCormick, Casey, Dawson, & Hacker, 2009) and should be measured along with other factors such as immigration status and acculturation level when investigating racial/ethnic/minorities. Hall and colleagues (2016) also make the case for the necessity of cultural adaptation in designing intervention.
The Correlates of PDM in Racial/Ethnic Minorities
In the second aim, the author sought to examine the correlates of PDM. The results provided some evidence of sociodemographic and psychosocial risks among racial/ethnic minorities. Though the age of study participants was truncated (18–50), the findings suggested that PDM is more prevalent among young adults. This should be interpreted with caution in light of research that suggests that the elderly also engage in PDM at high rates (Simoni-Wastila & Yang, 2006; West, Severtson, Green, & Dart, 2015). The studies predominately suggested that men have higher rates of PDM. Men tend to abuse illicit drugs more than women (SAMHSA, 2014b); however, drug dependence occurs at similar rates and women may be more likely to experience cravings and relapse, which contribute to the cycle of addiction (Anthony, Warner, & Kessler, 1994; Hitschfeld et al., 2015; Kippin et al., 2005). Gender is also salient given the challenges young males of color face in present society such as sentencing disparities in the criminal justice system (Demuth & Steffensmeier, 2004; Shaya, Gbarayor, Yang, Agyeman-Duah, & Saunders, 2007; Wells, Klap, Koike, & Sherbourne, 2001). According to Kaufman (1976) and others, drug users have historically engaged in polysubstance abuse (Kalyanam, Katsuki, Lanckriet, & Mackey, 2017; Kelly, Wells, Pawson, LeClair, & Parsons, 2014). All of the identified studies investigating abuse of other substances found that it was a significant predictor of PDM. More research is needed to disentangle the cause and consequences of PDM.
The other identified correlates including education, marital status, insurance coverage, employment, and income mirror risk factors for other illicit drug use (SAMHSA, 2014b). Racial/ethnic minorities are disproportionately represented among the undereducated, unmarried, uninsured, and unemployed (Bureau of Labor Statistics, 2013; Bureau of Labor Statistics, 2016; Kaiser Family Foundation, 2016; National Center for Education Statistics [NCES], 2010; NCES, 2016), providing additional evidence that PDM in these populations should be a significant concern. In 2011, 51% of adults over the age of 18 were married and the average age of marriage was 27 for women and 29 for men (Pew Research Center, 2011). Marriage rates are lower for subgroups of racial/ethnic minorities (Raley, Sweeney, & Wondra, 2015). Married people had lower rates of PDM in five studies and should be investigated further. Much of the research and data reported on insurance in the identified studies preceded the 2010 Affordable Care Act (ACA). The resulting changes in access to prescriptions and treatment may influence the future trajectory of PDM. Comorbidity with physical or psychological problems was a consistent correlate of PDM. These findings aligned with the evidence of health and mental health disparities among racial/ethnic minorities (Healthy People, 2017) and suggested a high risk demographic. Summed, the volume of risk factors suggests that future investigations and interventions would be remiss in excluding racial/ethnic minorities.
Limitations of the Studies
Methodological and cultural limitations were noted in the reviewed studies. Half of the studies were secondary data analyses and many used the same datasets. The upswing of PDM since 2000 suggests that more current data is needed. Secondary data can also inhibit more complex research questions. Research on prescription drug abuse is inherently limited by the fact that many people abuse multiple drugs. Sorting out the effects of PDM alone can be difficult. All of the studies in this review used self-report measures and the findings should be interpreted with caution. Problems with memory, underreporting, and social desirability are always an important consideration in drug abuse research. None of the studies used other methods to validate the veracity of participant responses, such as biological specimens. Many people mistakenly believe that PDM is less risky than other illicit drug use and it is not viewed as problematic (SAMHSA, 2014a), which may increase underreporting of misuse.
Underreporting may also intersect with cultural values. For example, ‘sharing’ is a value of collectivist cultures to which many racial/ethnic minorities ascribe (Brewer & Chen, 2007). People of color are also overrepresented among the economically disenfranchised (Institute for Research on Poverty, 2016), which may also influence sharing practices. Ultimately, sharing medication may be seen as less problematic in racial/ethnic minority populations. More data is needed to examine these connections.
Most of the general studies primarily described findings on African Americans and Latinos in comparison to White samples. Several concerns have been raised with regard to race-comparison studies including disregarding important cultural nuances (e.g., language, immigration status), meaningful group differences (e.g., urban vs. rural; African American vs. Caribbean American; biracial individuals), and intersectionality (e.g., race/ethnicity as a proxy for socioeconomic status; National Research Council, 2004). “Other” sometimes includes individuals of mixed race or participants who decline to answer questions of race/ethnicity and the results should be interpreted with caution. While collapsing groups may be statistically necessary, it depletes the richness of the data. Generalization or grouping of races makes it difficult to examine risk and protective factors and to create effective and perhaps culturally tailored PDM prevention and intervention programs. There are appropriate research questions that warrant race-comparison designs such as examining racial/ethnic differences to inform social policies or to explain the role of culture in group similarities and dissimilarities (Azibo, 1988; Joireman & Van Lange, 2015). None of the identified PDM race/ethnicity-comparison studies examined cultural influences.
The race/ethnicity-specific studies are useful, but it is challenging to draw conclusions since there were a wide range of prescription drugs of interest, target outcomes, and methodology. However, the studies provided a closer view of prevalence rates, drugs of choice, at-risk populations, and cultural considerations that can inform future directions in PDM research.
Limitations of the Review
As with any review, there are limitations. The search may not have been exhaustive and using alternative terminology and research databases may have resulted in divergent findings. “Gray literature”, such as dissertations, articles without full text, and unpublished studies were not included. Limiting the years for inclusion to 17 years may have also excluded relevant works. Finally, the authors may introduce bias into the inclusion and exclusion of studies; however, the process is described in full detail to permit replication.
Implications and Future Research
More evidence is needed on the prevalence, risk and protective factors, and evidence-based prevention and interventions associated with PDM. Future research should work towards inclusivity and oversample for underrepresented groups. Targeted studies are also needed on specific subgroups and should add cultural considerations such as perceived discrimination and immigration status. Existing PDM interventions appear to primarily focus on prescribing practices, monitoring programs, and abuse-deterrent drug formulations (Cicero et al., 2012; Department of Health and Human Services, 2013; National Governor’s Association, 2012; Office of National Drug Control Policy Executive, 2011); however, evidence based group interventions that consider culture at the outset may be warranted. High-risk groups also need more screening and effective education about the dangers of PDM to counteract the positive pop culture references (Rehab International, 2017). The risks of PDM in racial/ethnic minority populations can no longer be minimized in the field of substance abuse.
Conclusions
The low rates of PDM in general samples with racial/ethnic minorities may make the problem seem insignificant, while a closer look at targeted studies indicates that the problem is complex. First, racial/ethnic minority populations are growing exponentially (U.S. Census Bureau, 2015). The international increase in prescription pill trafficking and urban pop culture references to pill use also suggests that the profile of prescription drug users may be shifting (International Narcotics Control Board, 2015; Rehab International, 2017). Moreover, while present rates of PDM are low among racial/ethnic minorities, like other drugs, the outcomes may be more detrimental. For example, there are mixed findings on the prevalence of problematic drinking among racial/ethnic minorities (SAMHSA, 2008) yet African Americans and Latinos have higher rates of recurrent and persistent alcohol dependence and inequities in treatment use (Chartier & Caetano, 2010). Racial/ethnic minorities also have higher rates of drug-related mortality and sentencing for drug crimes (Demuth & Steffensmeier, 2004; NIDA, 2003) In addition, African Americans, Latinos, and American Indians experience profound negative outcomes of alcohol, which is complicated by cultural factors such as immigration status, perceived discrimination, neighborhood disenfranchisement, and alcohol-metabolizing genes (Chartier & Caetano, 2010). Given the prevalence of PDM in subgroups of racial/ethnic minorities coupled with these persistent substance abuse health disparities, the evidence suggests that research and interventions should move towards more inclusive, broader, and detailed investigations of PDM in racial/ethnic minority populations.
Figure 1.
Flow diagram of systematic selection of published research on Rx drug abuse in racial/ethnic minorities.
Note: *n1=ProQuest. **n2=EBSCOhost.
Figure 2.
Summary of prescription drug misuse research published by year on ethnic/racial (E/R) minorities versus general studies returned in searches. Groups are not mutually exclusive.
Table 1.2.
Summary prescription (Rx) drug abuse articles with African American participants (n = 3)
| Study | *Sample characteristics | **Rx drugs | Primary measures | Key findings |
|---|---|---|---|---|
| [15] Barry et al. (2011) | Secondary analysis; n = 4,122 veterans; Of the nonmedical users (n = 525), 69.9% were African American, 12.9% Latino, and 1.6% Other | AN | Veterans Aging Cohort Study | Veterans who abused prescription drugs were less likely to be African American than Latino. |
| [16] Kecojevic et al. (2015) | Chain-referral; n = 191 gay (57%) and bisexual/heterosexual (42.9%) Rx drug misusers; 37.2% African American, 18.3% Multiracial, 8.9% Latino/Other, and 1% Asian/Pacific Islander, 1% Native American | O, T, ST | Drug use outcomes survey including amount and purpose of use | The most popular drug of choice in this sample was tranquilizers followed by opioids, and stimulants. Bisexuals/heterosexuals reported higher Rx drug misuse. |
| [17] Peters et al. (2007) | Secondary analysis; n = 482 crack using adults; 100% African American | O | Peer Outreach Questionnaire | 8% of the sample used codeine. Younger and less educated participants used codeine. Codeine users were less like to have a main sex partner for money. |
Note:
The sample characteristics and findings highlight data for racial/ethnic minorities in the sample and may not include primary findings of the study.
Rx abbreviations are as follows; AN=analgesics, AX= anxiolytics, AM=amphetamines, B=benzodiazepines, O=opioids, SE=sedatives, SL=sleep, ST=stimulants, T=tranquilizers
Table 1.3.
Summary prescription (Rx) drug misuse articles with Latino participants (n = 8)
| Study | *Sample characteristics | **Rx drugs | Primary measures | Key findings |
|---|---|---|---|---|
| [18] Buttram et al. (2016) | Cross-sectional; n = 446 young adult opioid misusers; 64% Hispanic, 21.7% African American | SE, ST, Other | Global Appraisal of Individual Needs (GAIN) | Sedatives were the most commonly abused Rx (93.5%) followed by stimulants (49.8%). |
| [19] Coffman et al. (2008) | Exploratory; n = 19 Latino non-English speaking immigrants | Unspecified | 16-question moderator's guide | Participants self-medicated due to cost, access, and lack of quality care. |
| [20] Cohen et al. (2009) | Cross-sectional; n = 200 Brazilian women immigrants | Illegal diet pills | 23-item health habits survey | Compound diet pills that have been banned by the FDA are commonly used in this Brazilian immigrant community. |
| [21] Ford et al. (2008) | Secondary analysis; n = 37,154 youth and young adults; 17.5% Latino, 14.4% African American, 4.4% Asian, and 2.3% Other racial/ethnic minority | O, T, ST, SE | National Survey on Drug Use and Health (2005) | Patterns for Rx drug use for other racial/ethnic groups in this dataset remained consistent. Separate analyses for the Latinos revealed that younger vs older, healthy vs. unhealthy, and those who took the survey in Spanish were less likely to abuse Rx drugs. |
| [22] Kurtz et al. (2005) | Cross-sectional; n = 143 youth and adult ecstasy; 50.3% Latino, 3.5% African American, and 11.9% Other racial/ethnic minority | ST, SE, O and Club drugs | Washington University Risk Behavior Assessment | 82% of ecstasy users reported Rx drug misuse. Rx drug abusers had significantly lower age of first ecstasy use and used twice as many categories of drug use than non-Rx abusers. |
| [23] Kurtz et al. (2017) | Cross-sectional; n = 356 young adult benzo misusers; 71.1% Hispanic, 15.8% African American | B | Global Appraisal of Individual Needs (GAIN) | Alprazolam was the most frequently abused benzo and 12.6% of the sample met diagnostic criteria for benzo dependence. |
| [24] Larson et al. (2006) | Exploratory, qualitative; n = 25 Latino adults | Antibiotics | Antibiotic knowledge & attitudes questionnaires | Self-prescription of antibiotics was ascribed to lack of insurance, finances, immigration status. |
| [25] Muñoz-Laboy et al. (2014) | Mixed methods; n = 259 formerly incarcerated Latino men | AN, ST, SE | Data-driven measures | Nearly a third (26.9%) met criteria for depression. Depressive symptoms were correlated with higher lifetime and current use of ketamine and Rx stimulants. |
Note:
The sample characteristics and findings highlight data for racial/ethnic minorities in the sample and may not include primary findings of the study.
Rx abbreviations are as follows; AN=analgesics, AX= anxiolytics, AM=amphetamines, B=benzodiazepines, O=opioids, SE=sedatives, SL=sleep, ST=stimulants, T=tranquilizers
References
- Anthony JC, Warner LA, & Kessler RC (1994). Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology, 2, 244–268. [Google Scholar]
- Arkes J, & Iguchi MY (2008). How predictors of prescription drug abuse vary by age. Journal of Drug Issues, 38, 1027–1043. [Google Scholar]
- Azibo D (1988). Understanding the proper and improper usage of the comparative research framework. Journal of Black Psychology, 15, 81–91. doi: 10.1177/00957984880151010 [DOI] [Google Scholar]
- Bali V, Raisch D, Noffett M, & Khan N (2013). Determinants of nonmedical use, abuse or dependence on prescription drugs, and use of substance abuse treatment. Research in Social and Administrative Pharmacy, 9, 276–287. [DOI] [PubMed] [Google Scholar]
- Bardhi F, Sifaneck S, Johnson B, & Dunlap E (2007). Pills, thrills, and bellyaches: Case studies of prescription pill use and misuse among marijuana/blunt smoking middle class young women. Contemporary Drug Problems, 34, 53–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry DT, Goulet JL, Kerns RK, Becker WC, Gordon AJ, Justice AC, & Fiellin DA (2011). Non-medical use of prescription opioids and pain in veterans with and without HIV. Pain, 152, 1133–1138. 10.1016/j.pain.2011.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, Stein GL, Curry JF, & Hersh J (2012). Ethnic differences among substance-abusing adolescents in a treatment dissemination project. Journal of Substance Abuse Treatment, 42, 328–336. 10.1016/j.jsat.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Beyene KA, Sheridan J, & Aspden T (2014). Prescription medication sharing: A systematic review of the literature. American Journal of Public Health, 104, e15–e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer MB, & Chen YR (2007). Where (who) are collectives in collectivism? Toward conceptual clarification of individualism and collectivism. Psychological Review, 114, 133–151. doi: 10.1037/0033-295X.114.1.133. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (2013). Marriage and divorce: Patterns by gender, race, and educational attainment. Retrieved from https://www.bls.gov/opub/mlr/2013/article/marriage-and-divorce-patterns-by-gender-race-and-educational-attainment.htm
- Bureau of Labor Statistics (2016). Labor force statistics from the current population survey. Retrieved from http://www.bls.gov/web/empsit/cpsee_e16.htm
- Calsyn DA, Burlew A, Hatch-Maillette MA, Wilson J, Beadnell B, & Wright L(2012). Real men are safe-culturally adapted: Utilizing the Delphi process to revise Real Men Are Safe for an ethnically diverse group of men in substance abuse treatment. AIDS Education and Prevention, 24, 117–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng HG, & Phillips MR (2014). Secondary analysis of existing data: Opportunities and implementation. Shanghai Archives of Psychiatry, 26, 371–375. 10.11919/j.issn.1002-0829.214171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Kurtz SP, Surratt HL, Ibañez GE, Ellis MS, Levi-Minzi MA, & Inciardi JA (2011). Multiple determinants of specific modes of prescription opioid diversion. Journal of Drug Issues, 41, 283–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, & Surratt HL (2012). Effect of abuse-deterrent formulation of OxyContin. New England Journal of Medicine, 367, 187–189. [DOI] [PubMed] [Google Scholar]
- Coffman MJ, Shobe MA, & O'Connell B (2008). Self-prescription practices in recent Latino immigrants. Public Health Nursing, 25, 203–211. [DOI] [PubMed] [Google Scholar]
- Cohen PA, McCormick D, Casey C, Dawson GF, & Hacker KA (2009). Imported compounded diet pill use among Brazilian women immigrants in the United States. Journal of Immigrant and Minority Health, 11, 229–36. doi: 10.1007/s10903-007-9099-x [DOI] [PubMed] [Google Scholar]
- Demuth S, & Steffensmeier D (2004). Ethnicity effects on sentence outcomes in large urban courts: Comparisons among White, Black, and Hispanic defendants. Social Sciences Quarterly, 85, 994–1011. doi: 10.1111/j.0038-4941.2004.00255.x [DOI] [Google Scholar]
- Department of Health and Human Services, Behavioral Health Coordinating Committee Prescription Drug Abuse Subcommittee (2013). Addressing prescription drug abuse in the United States: Current activities and future opportunities. Washington, D.C.: Retrieved from http://www.cdc.gov/drugoverdose/pdf/hhs_prescription_drug_abuse_report_09.2013.pdf [Google Scholar]
- EBSCOhost Online Research Databases. (n.d.). Retrieved from https://www.ebscohost.com/
- Feldstein Ewing SW, Venner KL, Mead HK, & Bryan AD (2011). Exploring racial/ethnic differences in substance use: A preliminary theory-based investigation with juvenile justice-involved youth. BMC Pediatrics, 11, 71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleary S, Heffer R, & McKyer ELJ (2013). Understanding nonprescription and prescription drug misuse in late adolescence/young adulthood. Journal of Addiction, Article ID 709207. doi: 10.1155/2013/709207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JA, & Rivera FI (2008). Nonmedical prescription drug use among Hispanics. Journal of Drug Issues, 38, 285–310. [Google Scholar]
- Garnier LM, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, & Wish ED (2010). Sharing and selling of prescription medications in a college student sample. The Journal of Clinical Psychiatry, 71, 262–269. 10.4088/JCP.09m05189ecr [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Delva J, & Takeuchi DT (2007). Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. American Journal of Public Health, 98, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsworthy R, Schwartz N, & Mayhorn C (2008). Beyond abuse and exposure: Framing the impact of prescription-medication sharing. American Journal of Public Health, 98, 1115–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub A, Johnson BD, & Dunlap E (2005). Subcultural evolution and illicit drug use. Addiction Research & Theory, 13, 217–229. 10.1080/16066350500053497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy. 10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Harrell ZA, & Broman CL (2009). Racial/ethnic differences in correlates of prescription drug misuse among young adults. Drug and Alcohol Dependence, 104, 268–271 [DOI] [PubMed] [Google Scholar]
- Healthy People 2020. (2017). Disparities. Retrieved from https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
- Hitschfeld MJ, Schneekloth TD, Ebbert JO, Hall-Flavin DK, Karpyak VM, Abulseoud OA, ... Frye MA (2015). Female smokers have the highest alcohol craving in a residential alcoholism treatment cohort. Drug and Alcohol Dependence, 150, 179–182. doi: 10.1016/j.drugalcdep.2015.02.016 [DOI] [PubMed] [Google Scholar]
- Ibañez GE, Levi-Minzi MA, Rigg KK, & Mooss AD (2013). Diversion of benzodiazepines through healthcare sources. Journal of Psychoactive Drugs, 45, 48–56. doi: 10.1080/02791072.2013.764232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Kurtz SP, & Cicero TJ (2007). Mechanisms of prescription drug diversion among drug-involved club- and street-based populations. Pain Medicine (Malden, Mass.), 8, 171–183. 10.1111/j.1526-4637.2006.00255.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Cicero TJ, Kurtz SP, Martin SS, & Parrino MW (2009). The “Black Box” of prescription drug diversion. Journal of Addictive Diseases, 28, 332–347. 10.1080/10550880903182986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Research on Poverty. (2016). Who is poor? Retrieved from http://www.irp.wisc.edu/faqs/faq3.htm
- International Narcotics Control Board. (2015). Report of the International Narcotics Control Board. Retrieved from https://www.incb.org/documents/Publications/AnnualReports/AR2015/English/AR_2015_E.pdf
- Joireman J, & Van Lange P (2015). How to publish high-quality research. Washington D.C.: American Psychological Association. [Google Scholar]
- Kaiser Family Foundation. (2016). Key factors about the uninsured population. Retrieved from http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/#endnote_link_198942-14
- Kalyanam J, Katsuki T, Lanckriet G, & Mackey TK (2017). Exploring trends of nonmedical use of prescription drugs and polydrug abuse in the Twittersphere using unsupervised machine learning. Addictive Behavior, 65, 289–295. [DOI] [PubMed] [Google Scholar]
- Kaufman E (1976). The abuse of multiple drugs. Definition, classification, and extent of problem. American Journal of Drug and Alcohol Abuse, 3, 279–292. [DOI] [PubMed] [Google Scholar]
- Kecojevic A, Wong C, Corliss H, & Lankenau S (2015). Risk factors for high levels of prescription drug misuse and illicit drug use among substance-using young men who have sex with men (YMSM). Drug and Alcohol Dependence, 150, 156–163. doi: 10.1016/j.drugalcdep.2015.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly BC, Welles BA, Pawson M LeClair A, & Parsons JT (2014). Combinations of prescription drug misuse and illicit drugs among young adults. Addictive Behaviors, 39, 941–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kippin TE, Fuchs RA, Mehta RH, Case JM, Parker MP, Bimonte-Nelson HA, & See RE (2005). Potentiation of cocaine-primed reinstatement of drug seeking in female rats during estrus. Psychopharmacology (Berl), 182, 245–252. [DOI] [PubMed] [Google Scholar]
- Kirchner TR, Villanti AC, Cantrell J, Anesetti-Rothermel1 A, Ganz O, Conway KP,…….. Abrams DB (2015).Tobacco retail outlet advertising practices and proximity to schools, parks and public housing affect Synar underage sales violations in Washington, D.C. Tobacco Control, 24, e52–e58. [DOI] [PubMed] [Google Scholar]
- Kurtz SP, Inciardi JA, Surratt HL, & Cottler L (2005). Prescription drug abuse among ecstasy users in Miami. Journal of Addictive Diseases, 24, 1–16. [DOI] [PubMed] [Google Scholar]
- Larson EL, Dilone J, Garcia M, & Smolowitz J (2006). Factors which influence Latino community members to self-prescribe antibiotics. Nursing Research, 55, 94–102. [DOI] [PubMed] [Google Scholar]
- Martins SS, Kim JH, Chen L, Levin D, Keyes KM, & Cerdá M, & Storr, C. L. (2015). Nonmedical prescription drug use among U.S. young adults by educational attainment. Social Psychiatry and Psychiatric Epidemiology, 50, 713–724. doi: 10.1007/s00127-014-0980-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE (2005). Correlates of nonmedical use of prescription benzodiazepine anxiolytics: Results from a national survey of U.S. college students. Drug and Alcohol Dependence, 79, 53–62. doi: 10.1016/j.drugalcdep.2004.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West B, & Wechsler H (2007a). Trends and college-level characteristics associated with the non-medical use of prescription drugs among U.S. college students from 1993 to 2001. Addiction, 102, 455–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Morales M, Cranford JA, Delva J, McPherson MD, & Boyd CJ (2007b). Race/ethnicity and gender differences in drug use and abuse among college students. Journal of Ethnicity in Substance Abuse, 6, 75–95. 10.1300/J233v06n02_06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, & Boyd CJ (2014). Trends in medical use, Diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addictive Behavior, 39, 1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic D & Tanner J (2007). Vulnerable people, groups, and populations: Societal view. Health Affairs, 26, 1220–30. [DOI] [PubMed] [Google Scholar]
- Momper SL, Delva J, & Reed BG (2011). OxyContin misuse on a reservation: Qualitative reports by American Indians in talking circles. Substance Use & Misuse, 46, 1372–1379. doi: 10.3109/10826084.2011.592430 [DOI] [PubMed] [Google Scholar]
- Muñoz-Laboy M, Worthington N, Perry A, Guilamo-Ramos V, Cabassa L, Lee J, & Severson N (2014). Socio-environmental risks for untreated depression among formerly incarcerated Latino men. Journal of Immigrant and Minority Health, 16, 1183–92. doi: 10.1007/s10903-013-9814-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nargiso J, Ballard E, & Skeer M (2015). A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the United States: A social ecological perspective. Journal of Studies on Alcohol and Drugs, 76, 5–20. [PubMed] [Google Scholar]
- National Center for Education Statistics (NCES). (2010). Status and trends in the education of racial and ethnic groups. Retrieved from http://nces.ed.gov/pubs2010/2010015.pdf
- National Center for Education Statistics (NCES). (2016). Public high school graduation rates. Retrieved from http://nces.ed.gov/programs/coe/indicator_coi.asp
- National Governors Association. (2012). Six strategies for reducing prescription drug abuse. Retrieved from http://www.nga.org/files/live/sites/NGA/files/pdf/1209ReducingRxDrugsBrief.pdf
- National Institute on Drug Abuse (NIDA). (2003). Drug use among racial/ethnic minorities, revised. Retrieved from http://archives.drugabuse.gov/pdf/minorities03.pdf
- National Institute on Drug Abuse (NIDA) Research Report Series. (2011). Prescription drugs: Abuse and addiction. Retrieved from https://www.drugabuse.gov/sites/default/files/rrprescription.pdf
- National Institute on Drug Abuse (NIDA). (2013). Substance abuse in the military. Retrieved from https://www.drugabuse.gov/publications/drugfacts/substance-abuse-in-military
- National Institute on Drug Abuse (NIDA). (2015). DrugFacts: Prescription and over-the-counter medications. Retrieved from https://www.drugabuse.gov/publications/drugfacts/prescription-over-counter-medications
- National Research Council. (2004). Chapter 3: Measuring race, ethnicity, socioeconomic position, and acculturation In Ver Ploeg Michele and Perrin Edward (Eds.), Eliminating Health disparities: Measurement and data needs. Washington, D.C.: The National Academies Press; Retrieved from http://www.nap.edu/read/10979/chapter/5 [PubMed] [Google Scholar]
- Office of National Drug Control Policy Executive, Office of the President of the United States. (2011). Epidemic: Responding to America’s prescription drug abuse crisis. Washington, D.C. Retrieved from http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf
- Paulozzi LJ, Kilbourne EM, & Desai HA (2011). Prescription drug monitoring programs and death rates from drug overdose. Pain Medicine, 12, 747–754. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Mack KA, & Hockenberry JM (2014). Vital signs: Variation among states in prescribing of opioid pain relievers and benzodiazepines — United States, 2012. Morbidity and Mortality Weekly Report, 63, 563–568. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6326a2.htm?s_cid=mm6326a2_w [PMC free article] [PubMed] [Google Scholar]
- Peters RJ, Williams M, Ross MW, Atkinson J, & Yacoubian GS Jr. (2007). Codeine cough syrup use among African-American crack cocaine users. Journal of Psychoactive Drugs, 39, 97–102. doi: 10.1080/02791072.2007.10399868 [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2011). Barely half of U.S. adults are married – A record lowRetri eved from http://www.pewsocialtrends.org/2011/12/14/barely-half-of-u-s-adults-are-married-a-record-low/
- Pew Research Center. (2014a). In 2014, Latinos will surpass whites as largest racial/ethnic group in California. Retrieved from http://www.pewresearch.org/fact-tank/2014/01/24/in-2014-latinos-will-surpass-whites-as-largest-racialethnic-group-in-california/
- Pew Research Center. (2014b). More Hispanics,Blacks enrolling in college, but lag in bachelor’s degrees. Retrieved from http://www.pewresearch.org/fact-tank/2014/04/24/more-hispanics-blacks-enrolling-in-college-but-lag-in-bachelors-degrees/
- Pew Research Center. (2017). 6 facts about the U.S. military and its changing demographics. Retrieved from http://www.pewresearch.org/fact-tank/2017/04/13/6-facts-about-the-u-s-military-and-its-changing-demographics/
- Picchi A (2016). Drug ads: $5.2 billion annually and rising. MoneyWatch. Retrieved from https://www.cbsnews.com/news/drug-ads-5-2-billion-annually-and-rising/
- Pollard K, & O’Hare W (1999). America’s racial and ethnic minorities. Population Bulletin, 54, 1–52. Retrieved from http://www.prb.org/Source/54.3AmerRacialEthnicMinor.pdf [Google Scholar]
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). (2009). PRISMA 2009 Checklist. Retrieved from https://docs.google.com/viewer?url=http%3A%2F%2Fwww.prisma-statement.org%2Fdocuments%2FPRISMA%25202009%2520checklist.doc
- ProQuest. (n.d.). Retrieved from http://www.proquest.com/
- Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, & Lambert B (2014). ‘Pharmacy deserts’ are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Affairs, 33, 1958–1965. doi: 10.1377/hlthaff.2013.1397 [DOI] [PubMed] [Google Scholar]
- Quintero G, Peterson J, & Young B (2006). An exploratory study of socio-cultural factors contributing to prescription drug misuse among college students. Journal of Drug Issues, 36, 903–931. [Google Scholar]
- Raley RK, Sweeney MM, & Wondra D (2015). The growing racial and ethnic divide in U.S. marriage patterns. Future Child, 25, 89–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehab International. (2017). Drug use in pop culture infographic. Retrieved from https://rehab-international.org/blog/drug-use-in-pop-culture
- Rigg KK, & Ibañez GE (2010). Motivations for non-medical prescription drug use: A mixed methods analysis. Journal of Substance Abuse Treatment, 39, 236–247. doi: 10.1016/j.jsat.2010.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepis TS, & Krishnan-Sarin S (2009). Sources of prescriptions for misuse by adolescents: Differences in sex, ethnicity, and severity of misuse in a population-based study. Journal of the American Academy of Child Adolescent Psychiatry, 48, 828–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaya F, Gbarayor C, Yang H, Agyeman-Duah M, & Saunders E (2007) A perspective on African American participation in clinical trials. Contemporary Clinical Trials, 28, 213–217. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, & Yang HK (2006). Psychoactive drug abuse in older adults. American Journal of Geriatric Pharmocotherapy, 4, 380–394. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2007a). Results from the 2006 National Survey on Drug Use and Health: Detailed tables. Office of Applied Studies. Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2013/NSDUH-DetTabs2013.htm
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2007b). National Survey on Drug Use and Health, detailed tables, tobacco product and alcohol use, table 2.46B. Retrieved from http://oas.samhsa.gov/NSDUH/2k7NSDUH/tabs/Sect2peTabs43to84.htm#Tab2.46B
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2008). Results from the 2007 National Survey on Drug Use and Health: National Findings NSDUH Series H-34 DHHS Publication. Office of Applied Studies.
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2013). Results from the 2012 National Survey on Drug Use and Health: Detailed tables. Rockville, MD. Retrieved from http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/DetTabs/NSDUH-DetTabsTOC2012.htm
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2014a). Rise in prescription drug misuse and abuse impacting teens. Retrieved from http://www.samhsa.gov/homelessness-programs-resources/hpr-resources/teen-prescription-drug-misuse-abuse
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2014b). Results from the 2013 National Survey on Drug Use and Health: Summary of national findings. NSDUH Series H-48, HHS Publication No. (SMA) 14–4863. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf [PubMed]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2015a). Prescription drug misuse and abuse. Retrieved from http://www.samhsa.gov/prescription-drug-misuse-abuse
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2015b). Risk and protective factors associated with the non-medical use of prescription drugs: Using prevention research to guide prevention practice. Retrieved from http://www.drugs.indiana.edu/spf/docs/Risk%20and%20Protective%20Factors%20Associated%20with%20the%20Non-Medical%20Use%20of%20Prescription%20Drugs.pdf
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2017). Media campaigns to prevent prescription drug and opioid misuse. Retrieved from https://www.samhsa.gov/capt/tools-capt-learning-resources/media-campaigns-prevent-rx-drugs-opioid-misuse
- University of Cincinnati Libraries. (n.d.). Top ten UC databases for general research. Retrieved from http://guides.libraries.uc.edu/c.php?g=222600
- University of Wisconsin-Madison Libraries. (n.d.). Top 10 databases Retrieved from https://www.library.wisc.edu/find/top-10-databases/
- U.S. Census Bureau. (2015). Quickfacts. Retrieved from http://www.census.gov/quickfacts/table/PST045215/00
- Varga M, & Varga M (2015). Prescription stimulant use by graduate students. College Student Affairs Journal, 33, 124–145. [Google Scholar]
- Vietri J, Joshi A, Barsdorf A, & Mardekian J (2014). Prescription opioid abuse and tampering in the United States: Results of a self-report survey. Pain Medicine, 15, 2064–2074. [DOI] [PubMed] [Google Scholar]
- Volkow N (2008). Scientific research on prescription drug abuse. Testimony before the Subcommittee on Crime and Drugs, Committee on the Judiciary and the Caucus on International Narcotics Control United States Senate. Retrieved from https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2008/03/scientific-research-prescription-drug-abuse
- Volkow N (2014). America’s addiction to opioids: Heroin and prescription drug abuse. Senate Caucus on International Narcotics Control. Retrieved from https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse
- Waheed W, Hughes-Morley A, Woodham A, Allen G, & Bower P (2015). Overcoming barriers to recruiting ethnic minorities to mental health research: A typology of recruitment strategies. BMC Psychiatry, 15, 101–112. doi: 10.1186/s12888-015-0484-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang KH, Becker WC, & Fiellin DA (2013). Prevalence and correlates for nonmedical use of prescription opioids among urban and rural residents. Drug and Alcohol Dependence, 127, 156–162. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A & Sherbourne C (2001). Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry, 158, 2027–2032. [DOI] [PubMed] [Google Scholar]
- Wu L-T, Woody GE, Yang C, Pan J, & Blazer DG (2010). Subtypes of nonmedical opioid users: Results from the national epidemiologic survey on alcohol and related conditions. Drug and Alcohol Dependence, 112, 69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A, Glover N, & Havens J (2012). Nonmedical use of prescription drugs among adolescents in the United States: A systematic review. Journal of Adolescent Health, 15, 6–17. [DOI] [PubMed] [Google Scholar]