Abstract
Background
Suboptimal health status (SHS) is an intermediate health status between health and illness, a syndrome characterised by the perception of health complaints, general weakness and low energy. This study aimed to investigate the prevalence of SHS and the correlation between SHS and psychological symptoms among Chinese college students and to identify the SHS-related risk factors from the perspective of predictive, preventive and personalised medicine (PPPM).
Methods
A cross-sectional study was conducted among 4119 college students who were enrolled from Taishan Medical University and Baoji Vocational and Technical College in the eastern and western areas of China. SHS levels of the participants were measured by an established self-reporting Suboptimal Health Status Questionnaire-25 (SHSQ-25). Psychosomatic conditions were estimated by the self-rating Symptom Checklist-90 (SCL-90) scale. Spearman correlation analysis was applied to analyse the relationship between SHSQ-25 scores and SCL-90 estimates. Logistic regression analysis was applied for multivariate analysis.
Results
The prevalence of SHS was 21.0% (864/4119), with 23.3% (701/3005) for female students and 14.6% (163/1114) for male students. The prevalence of general positive psychological symptom was 14.2% (586/4119), with 15.6% (470/3005) for female students and 10.4% (116/1114) for male students. A strong correlation was identified between SHS score and SCL-90 estimates, with the correlation coefficient (r) of 0.719. Logistic regression showed that variables significantly associated with SHS were somatisation (adjusted odds ratio (aOR) = 3.185, 95% confidence interval [CI] = 2.048–4.953), obsessive-compulsive (aOR = 3.518, 95% CI = 2.834–4.368), interpersonal sensitivity (aOR = 1.883, 95% CI = 1.439–2.463) and depression (aOR = 1.847, 95% CI = 1.335–2.554).
Conclusions
Our findings confirm that there is a high prevalence of SHS among college students and there is a strong association between SHS and psychological symptoms among Chinese college students. High susceptibility of SHS occurs particularly in vulnerable groups: female students, sophomore students, medical students and students from rural area. Identification of SHS and prompt application of personalised psychological health-supporting activities will promote college students’ health status.
Electronic supplementary material
The online version of this article (10.1007/s13167-018-0148-4) contains supplementary material, which is available to authorized users.
Keywords: Suboptimal health status, Psychological symptoms, Suboptimal Health Status Questionnaire-25, Symptom Checklist-90, College students, China
Background
Health, defined by the World Health Organization (WHO), is a condition of complete physical, mental and social well-being and not merely the absence of disease or infirmity [1]. Rapid changes in environment and lifestyles in China widely influence health conditions, exposing people to the increased risk of suboptimal health status (SHS) [2]. Likewise, SHS has been recognised as a major public health challenge globally [3–7]. The characteristics of SHS are described as the perception of health complaints, general weakness and low energy [8]. The Suboptimal Health Status Questionnaire-25 (SHSQ-25) has been established to measure SHS and has been validated among three major ethnic groups: Africans, Asians and Caucasians [9]. Published studies demonstrated that the perceptible symptoms of SHS include chronic fatigue, non-specific pain (e.g. foot pain, pelvic pain or back pain), headaches, dizziness, anxiety, depression, fibromyalgia and functional disorders [10–13]. Although SHS is regarded as a reversible stage of preclinical status, persons with SHS usually undergo impaired quality of life, frequent hospital visits and incur extra-medical expenses [14, 15]. An increasing number of studies have shown that SHS is associated with the development of diabetes mellitus, as well as coronary heart disease and stroke [3–5, 16–18]. Previous studies have reported that the prevalence of SHS was 55.9% among college students and 46.0% in a general adult population in China [11, 19]. A recent study showed that SHS prevalence was 51.2% among college freshmen from a Chinese university [20].
The underlying causes of SHS are not clearly documented yet. Lifestyles, such as poor dietary intake, cigarette smoking and physical inactivity, play important roles in its development [20]. Moreover, psychological factors are associated with SHS and are always measured within SHS assessment [14]. Generally, psychological problems are considered as either the cause or the outcome of SHS [21]. Mental health promotion is crucial for health management of college students who are experiencing an increasing prevalence of mental disorder [22, 23]. Although mental health counselling centres and mental health promotion programmes have been widely established in colleges, the mental health challenges among college students in China are often underestimated [24]. From the perspectives of predictive, preventive and personalised medicine (PPPM), baseline information on both physical and mental health for college students is urgently needed [25, 26].
We conducted this study to estimate the prevalence rates of SHS and mental health conditions among college students and to investigate whether SHS and mental health conditions were associated with gender, homeland location and disciplinary major of the college students. We also quantified the correlation between SHS and mental health-related symptoms.
Methods
Study participants
A cross-sectional study was carried out from February to March 2018. The study approach was approved by the Human Research Ethics Committee of Taishan Medical University (TSMU). For the sample selection, we chose two universities, TSMU in eastern China and Baoji Vocational and Technical College (BJVC) in western China using a convenience sampling approach. We randomly selected three schools from TSMU and three schools from BJVC using a cluster sampling approach. A total of 4300 undergraduates (1800 from TSMU, 2500 from BJVC) were recruited for this study. The geographic locations of TSMU and BJVC are shown in Fig. 1. The flowchart of enrollment of participants is shown in Fig. S1.
Fig. 1.
Location of the survey sites in China. TSMU, Taishan Medical University; BJVC, Baoji Vocational and Technical College
The inclusion criteria were (1) no somatic diseases, (2) no history of psychiatric abnormalities, (3) no psychiatric abnormalities currently, (4) full-time undergraduates and (5) no history of medication consumption in the previous 2 weeks. Participants were first asked about their health history, followed by a physical examination in the TSMU affiliated hospital and BJVC campus health clinic. Fifty-four students of TSMU and 46 students of BJVC who had a diagnosed disease or declined participation were excluded from this study. The self-administered questionnaires were implemented to measure SHS and psychological symptoms of 4200 students. Among them, 4119 completed the questionnaires, with a valid response rate of 98.07%. Each questionnaire was introduced by an interviewer and completed by each student within 30 min. Written informed consents were obtained from participants. The individual information for each participant was de-identified in the following analyses.
SHS evaluation
The condition of SHS was evaluated by the self-reporting questionnaire SHSQ-25 which includes 25 items on five dimensions: (1) fatigue, (2) cardiovascular health, (3) digestive tract, (4) immune system and (5) mental health [27]. Each item was displayed as a specific statement on a 5-point Likert-type scale based on how often they underwent uncomfortable symptoms in the preceding 3 months. The experiences of (1) never or almost never, (2) occasionally, (3) often, (4) very often and (5) always were rated as 0, 1, 2, 3 and 4, respectively [3]. The total score of SHSQ-25 of each student was obtained by summing the scores of the 25 items [27]. The health status of participants was stratified into two classifications: ideal health (with summed score < 35) and suboptimal health (with summed score ≥ 35).
Psychological state evaluation
The psychological conditions of participants were assessed by the Symptom Checklist-90 (SCL-90) instrument, a 90-item multidimensional symptom scale that measures psychopathological or somatic disturbances on a 5-point scale ranging from 0 (not at all) to 4 (extremely) over the past 7 days [28]. SCL-90 scale consists of nine factors assessing psychological symptoms and one factor assessing additional items. These 90 items are classified into the following 10 domains: somatisation symptom (12 items), obsessive-compulsive symptom (10 items), interpersonal sensitivity symptom (9 items), depression symptom (13 items), anxiety symptom (10 items), hostility symptom (6 items), phobic anxiety symptom (7 items), paranoid ideation symptom (6 items), psychoticism symptom (10 items) and others symptom (sleep and diet, 7 items). Students with a summed score ≥ 160 were considered as having a general positive symptom. The standardised mean score was obtained to measure the symptom in each dimension. A standardised subscale score ≥ 2 was suggestive of having the symptom in a specific dimension [29].
Statistical analysis
The statistical analysis was performed by SPSS (v 24.0, IBM, New York, USA). Quantitative data that were normally distributed were expressed as means and standard deviations while non-normally distributed data were expressed as medians and quartiles (P25~P75). A Mann-Whitney test or a Kruskal-Wallis test was used to compare the differences between groups. Qualitative data were presented as a rate or percentage. A Pearson chi-squared (χ2) test was used to compare the differences between groups. Spearman correlation analysis was then carried out to analyse the relationship between SHSQ-25 scores and SCL-90 estimates. Logistic regression analysis was applied for multivariate analysis, by which the adjusted odds ratio (aOR) and 95% confidence intervals (CI) were calculated. The p value < 0.05 was considered statistically significant.
Results
Characteristics of participants
The characteristics of the students enrolled in this study are presented in Table 1, with an average age of 19 years (quartile 18~19, range 17~22) and a gender ratio of 3005/1114 (female/male). Among the total 4119 students, 2466 (59.9%) were freshmen, 1114 (27.0%) were sophomores and 539 (13.1%) were junior students. In addition, 2851 (69.2%) students came from rural area, while 1268 (30.8%) came from urban area. In terms of university, 1552 (37.7%) students were from TSMU in eastern China and 2567 (62.3%) were from BJVC in western China. The participants were further classified into medical students (2460, 59.7%) and non-medical (1659, 40.3%) in accordance with their disciplinary majors.
Table 1.
Characteristics of participants
| Variables | n | Healthy (%) (n = 3255) |
SHS (%) (n = 864) |
χ2/Z | |
|---|---|---|---|---|---|
| Gender | Male | 1114 | 951 (85.4) | 163 (14.6) | 37.075* |
| Female | 3005 | 2304 (76.7) | 701 (23.3) | ||
| BMI categories | Thin | 970 | 780 (80.4) | 190 (19.6) | 14.184* |
| Normal | 2454 | 2023 (82.4) | 431 (17.6) | ||
| Overweight | 495 | 429 (86.7) | 66 (13.3) | ||
| Obese | 200 | 152 (76.0) | 48 (24.0) | ||
| Grade | Freshmen | 2466 | 2038 (82.6) | 428 (17.4) | 142.416* |
| Sophomore | 1114 | 745 (66.9) | 369 (33.1) | ||
| Junior | 539 | 472 (87.6) | 67 (12.4) | ||
| Area | Rural | 2851 | 2219 (77.8) | 632 (22.2) | 7.934* |
| Urban | 1268 | 1036 (81.7) | 232 (18.3) | ||
| Major | Medicine | 2460 | 1836 (74.6) | 624 (25.4) | 71.008* |
| Non-medicine | 1659 | 1419 (85.5) | 240 (14.5) | ||
| Geographic | East China | 1552 | 1155 (74.4) | 397 (25.6) | 31.844* |
| West China | 2567 | 2100 (81.8) | 467 (18.2) | ||
| Age | 4119 | 18.0 (18.0~19.0)a | 19.0 (18.0~19.0)a | 2.626* | |
| Vital capacity | 4119 | 3248.5 (2452.5~3975.5)a | 2978.0 (2270.0~3791.0)a | 1.451 | |
| SCL-90 | 4119 | 108 (98~126)a | 159 (135~190)a | 33.941* | |
BMI body mass index, SCL-90 Symptom Checklist-90 scale
aData of continuous variables were expressed as medians and quartiles (P25~P75)
*p < 0.01 for statistical tests
The prevalence of SHS
As shown in Table 1, the prevalence of SHS was 21.0% (864/4119). The prevalence was higher among female students (23.3%; 701/3005) than male students (14.6%; 163/1114). The respective prevalence rates were 17.4% (428/2466) in the freshmen, 33.1% (369/1114) in the sophomores and 12.4% (67/539) in the junior students. The prevalence of SHS was 18.3% (232/1268) in urban students and 22.2% (632/2851) in rural students. Students from TSMU in eastern China were more susceptible to SHS (25.6%; 397/1552) than students from BJVC in western China (18.2%; 467/2567). According to the discipline major of participants, medical students had a prevalence of 25.4% (624/2460), while non-medical students showed a lower prevalence of 14.5% (240/1659). By reference to the Chinese criteria of body mass index (BMI) [30], we classified the participants into four categories: thin (BMI < 18.5), normal (18.5 ≤ BMI < 24), overweight (24 ≤ BMI < 28) and obese students (BMI ≥ 28). The prevalence of SHS among obese students was the highest (24.0%, 48/200). Interestingly, SHS prevalence among overweight students was the lowest (13.3%, 66/495). With regard to age and vital capacity, there were no statistical differences between the healthy and SHS students.
As shown in Table S1, the scores in the domains of fatigue, cardiovascular health, digestive tract, immune system and mental health were 10.0 (quartile 7.0~14.0), 0.0 (quartile 0.0~3.0), 2.0 (quartile 0.0~4.0), 2.0 (quartile 1.0~4.0) and 7.0 (quartile 2.0~10.0), respectively. The medians and quartiles of the summed SHS scores were 20.0 (quartile 11.0~29.0) among male students and 24.0 (quartile 13.0~34.0) among female students, indicating that female students suffered more psychological problems than males. The score was 27.0 (quartile 18.0~38.0) among sophomore students, which was higher than that of freshmen 22.0 (quartile 13.0~31.0) and junior students 11.0 (5.0~24.0). The median SHS score was higher among medical students 25.0 (15.0~35.0) than non-medical students 19.0 (quartile 10.0~29.0). Moreover, according to BMI classifications, obese students had the highest SHS score of 19.00 (quartile 11.0~35.5), while overweight students had the lowest SHS score of 19.00 (quartile 9.5~32.0). Among students from rural area, the score was 23.0 (quartile 13.0~33.0), which was statistically higher than that of urban students 21.0 (quartile 11.0~31.0). In addition, the summed SHS score of students in the TSMU located in eastern China was 25.0 (quartile 15.0~35.0), higher than that of students from BJVC in western China who scored 21.0 (quartile 11.0~31.0).
Stratified analysis for students from different geographical locations was carried out. As shown in Table S2, the SHS score of students who came from rural area was statistically higher than that of students who came from urban area in BJVC, western China, whereas no statistically significant difference was observed between the students from rural and urban areas in TSMU located in eastern China.
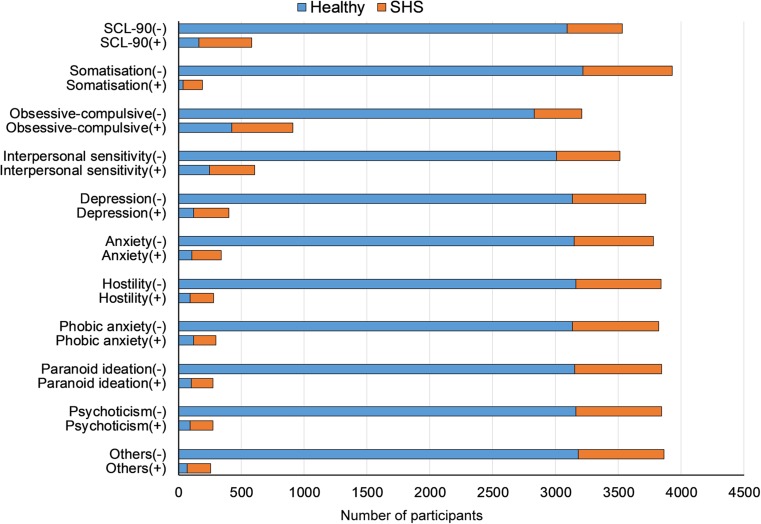
Psychological states of the participants
As shown in Fig. 2 and Table S3, the prevalence of general positive psychological symptoms was 14.2% (586/4119), with the prevalence rates of 4.6% for a positive somatisation symptom, 22.1% for an obsessive-compulsive symptom, 14.7% for interpersonal sensitivity symptom, 9.7% for depression symptom, 8.2% for anxiety symptom, 6.8% for hostility symptom, 7.3% for phobic anxiety symptom, 6.7% for paranoid ideation symptom, 6.7% for psychoticism symptom and 6.3% for the others (e.g. sleep and diet), respectively.
Fig. 2.
Frequencies of participants with psychological symptoms. SCL-90, Symptom Checklist-90 scale; +, positive for relevant symptom; −, negative for relevant symptom
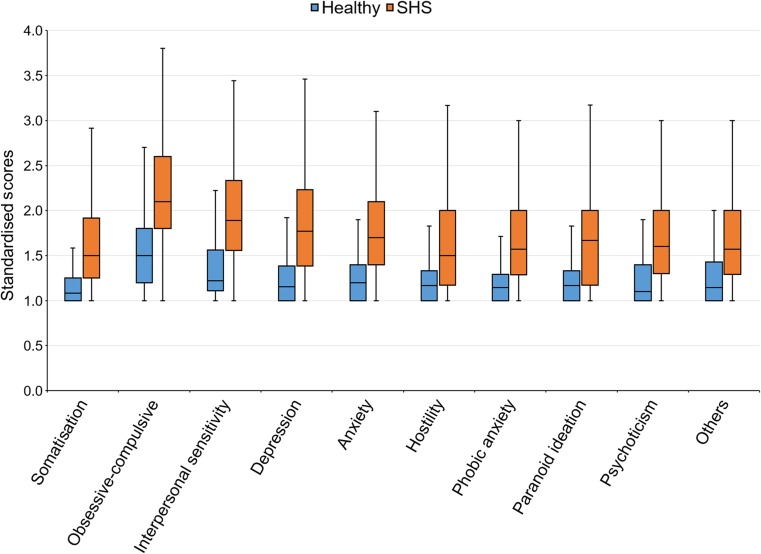
The sum of SCL-90 scores among SHS students was 159.0 (quartile 135.0~190.0), whereas the sum among healthy students was 108.0 (quartile 98.0~126.0), indicating that SHS students suffered more psychological problems than healthy students (Table 1). The standardised scores of 10 dimensions of SCL-90 were also calculated. As shown in Fig. 3, the score of somatisation, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, terror, stubborn, psychoticism and other symptoms in SHS students were statistically higher than that of the healthy group.
Fig. 3.
Box plot of SCL-90 scores of healthy and SHS participants. The data were expressed as minimum, P25, median, P75, and maximum; SCL-90, Symptom Checklist-90 scale; SHS, Suboptimal Health Status Questionnaire-25
As shown in Table S4, summed SCL-90 score among female students of 118.0 (quartile 101.0~145.0) was higher than that for male students of 111.0 (quartile 99.0~129.0), and the score of each dimension was higher among female students with statistical significance. For grade classifications, the SCL-90 score for sophomore students of 128.0 (quartile 109.0~166.0) was higher than those for freshmen who scored 115.0 (quartile 101.0~137.3) and junior students who scored 92.0 (quartile 90.0~107.0). The score of each dimension was higher among sophomore.
The SCL-90 score for students from rural area of 116.0 (quartile 100.0~143.0) was higher than that for students from urban area who scored 113.0 (quartile 99.0~135.0). In addition, the summed SCL-90 score of students from TSMU was 123.5 (quartile 105.0~151.0), statistically higher than that of students from BJVC (median 110.0, quartile 98.0~133.0). To further identify the difference between the students from urban and rural areas who were studying in the same university, a stratified analysis was applied and illustrated that the SCL-90 score of the students from rural area was statistically higher than that of students from urban area in BJVC, whereas no statistically significant difference was observed between the students from rural and urban areas in TSMU (Table S5).
With regard to the BMI classifications, the SCL-90 scores among thin, normal, overweight and obese students were 124.0 (quartile 107.8~151.0), 123.0 (quartile 106.0~147.5), 124.0 (quartile 101.5~144.0) and 124.0 (quartile 109.0~164.5), respectively, showing no statistical difference between the groups.
The summed score of SCL-90 among medical students was 121.0 (quartile 103.0~148.0), and the score among non-medical students was 107.0 (quartile 97.0~128.0), showing that the SCL-90 score for medical students was statistically higher than that for non-medical students, and the score for each dimension of SCL-90 was also higher among medical students (see Table S4).
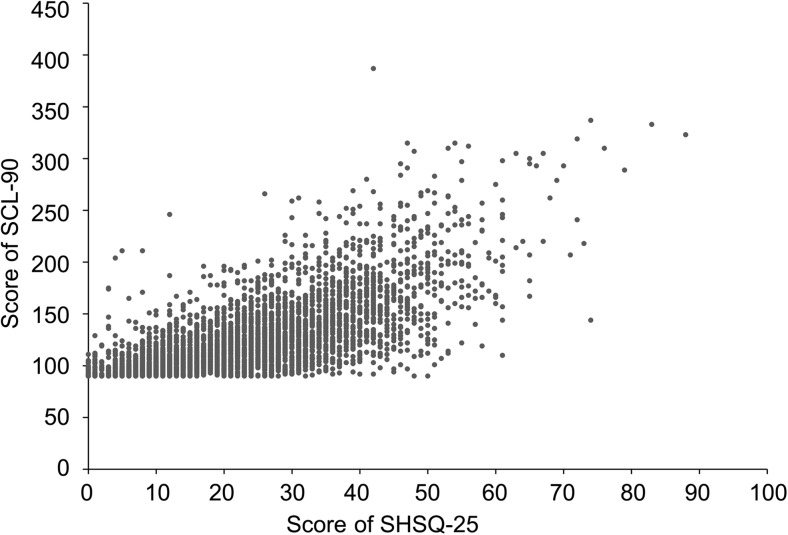
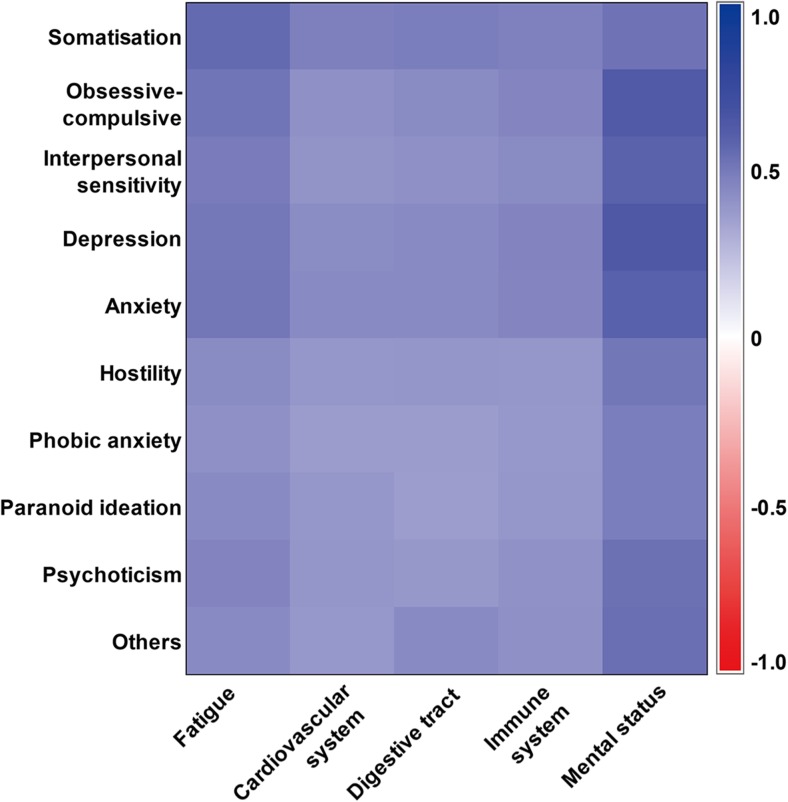
Correlation coefficients between SCL-90 and SHS scores
Bivariate correlation analysis between SCL-90 and SHS scores revealed a high correlation (Fig. 4), with the Spearman correlation coefficient (r) of 0.719. Moreover, the correlations between each dimension of SHS and each psychological subscale were analysed. The symptoms of somatisation, obsessive-compulsive, interpersonal sensitivity, depression and anxiety all had high positive correlations with each dimension of SHS (Fig. 5).
Fig. 4.
Scatter plot of SCL-90 score versus SHSQ-25 score. Correlation coefficient (r) is 0.719; SCL-90, Symptom Checklist-90 scale; SHSQ-25, Suboptimal Health Status Questionnaire-25
Fig. 5.
Correlation matrix heatmap of SCL-90 scores and SHSQ-25 scores. SCL-90, Symptom Checklist-90 scale; SHSQ-25, Suboptimal Health Status Questionnaire-25
Logistic regression analysis on SHS with psychological symptoms
The logistic regression analysis was performed to determine the major influences on SHS development. After adjusting for age, gender, grade, BMI, vital capacity, homeland, major and university location, we found that somatisation (aOR = 3.185, 95% CI = 2.048–4.953), obsessive-compulsive (aOR = 3.518, 95% CI = 2.834–4.368), interpersonal sensitivity (aOR = 1.883, 95% CI = 1.439–2.463), depression (aOR = 1.847, 95% CI = 1.335–2.554) and other symptoms of SCL-90 (sleep and diet, aOR = 2.064, 95% CI = 1.422–2.997) were positively associated with SHS (Table 2).
Table 2.
Multivariate logistic regression analysis for SHS
| Variables | B | SE | Wald | P | aOR | 95% CI |
|---|---|---|---|---|---|---|
| Somatisation | 1.158 | 0.225 | 26.434 | < 0.001 | 3.185 | 2.048~4.953 |
| Obsessive-compulsive | 1.258 | 0.110 | 129.939 | < 0.001 | 3.518 | 2.834~4.368 |
| Interpersonal sensitivity | 0.633 | 0.137 | 21.305 | < 0.001 | 1.883 | 1.439~2.463 |
| Depression | 0.613 | 0.166 | 13.723 | < 0.001 | 1.847 | 1.335~2.554 |
| Other symptom of SCL-90 | 0.725 | 0.190 | 14.510 | < 0.001 | 2.064 | 1.422~2.997 |
| Grade | 0.159 | 0.061 | 6.883 | 0.009 | 1.172 | 1.041–1.320 |
SE standard error, aOR adjusted odds ratio, CI confidence interval
Discussion
This study illustrated a SHS prevalence of 21.0% and a psychological symptom prevalence of 14.2% among Chinese college students. The median of the summed SCL-90 scores of SHS students was 159.0, while the median score in healthy students was 108.0, indicating that SHS students suffered from more severe psychological problems than healthy students. SHS was strongly correlated with psychological symptoms, with the Spearman correlation coefficient of 0.719. Moreover, the symptoms of somatisation, obsessive-compulsive, interpersonal sensitivity, depression, sleep and diet problems were the main factors positively associated with SHS.
Psychological factor plays a crucial role in the development of SHS, and a psychological complaint is always one of the key indicators of SHS occurrence. Therefore, we focused on the relationship between psychological factors and SHS prevalence in this study. We found that 14.2% of students showed a general positive symptom according to the SCL-90 scale, including symptoms such as somatisation, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism and others (e.g. sleep and diet). The prevalence rates of obsessive-compulsive and interpersonal sensitivity symptoms were 22.1 and 14.7%, respectively, which are more severe than other symptoms. Each dimension of SCL-90 was not only correlated with the summed SHS score but also with specified dimensions of SHS (i.e. fatigue, cardiovascular system, digestive tract, immune system, mental status). This finding identifies the impact of psychological factors on the health status of college students, since students with psychological stress tend to have low levels of participation in healthy life experiences or activities.
Somatisation, also known as somatic complaint, is considered to cause serious medical problems, including functional somatic disorders [31, 32]. We found that somatisation displays the highest correlation coefficient with four SHS dimensions (i.e. fatigue, cardiovascular system, digestive tract, immune system) when compared with the other SCL-90 dimensions. Obsessive-compulsive disorder is a psychiatric condition featured by recurrent, self-generating obsessions and compulsions, leading to significant distress or impairment [33]. Obsessive-compulsive disorder is commonly implicated in co-occurrence with neurological symptoms, such as chronic widespread pain, fatigue, cognitive dysfunction and sleep problems [34]. In addition to the high prevalence of clinical obsessive-compulsive disorder, many people sometimes suffer from a tendency for obsessive-compulsive behaviour without having the full syndrome [35]. In the present study, obsessive-compulsive symptoms had a close relationship with the SHS dimension of mental status, which is consistent with the above findings [34, 35]. A strong correlation was also noted between interpersonal sensitivity of SCL-90 and SHS. Some college students suffer from the symptom of interpersonal sensitivity that refers to the misunderstanding of personal perceptions of inadequacy and inferiority and lack of ability to estimate and recollect other students’ behaviours, feelings of and performances [36, 37]. Interpersonal sensitivity induces feeling discomfort in the presence of other people, which can lead to interpersonal avoidance and non-assertive behaviour [38]. Even though interpersonal sensitivity was relatively low across all symptoms of SCL-90 in the current study, medical students and sophomore students experienced higher tendencies for interpersonal sensitivity than the others. Furthermore, depression and anxiety were strongly correlated with each dimension of SHS in this current study. As is widely known, depression and anxiety are common among college students globally, which affect their academic performance and quality of life [39]. Both academic and non-academic factors lead to increased depression and anxiety tendency. These include but are not limited to high academic load, financial strains, colleague competiveness, poor sleep quality and social problems [40]. A systematic review documented that 7.7–65.5% of medical students suffer from anxiety in Europe [41]. We also found a high prevalence (10.3%) of anxiety symptom among medical students in China in the present study, particularly among the students from TSMU in the eastern part of China.
Unbalanced economic development between eastern and western areas of China has been a major challenge for decades [42]. Recent statistics displayed gross domestic product (GDP) per capita of US$ 9892 in Taian City where TSMU is located and US$ 7800 in Baoji City where BJVC is located [43]. Our study showed that students who came from rural area suffer more from SHS and psychological problems than students from urban area in BJVC, western China. For those from rural area, it is more difficulty to adapt to the college environment and academic pressure, resulting in higher incidences of SHS and psychological problems (e.g. anxiety and depression) [20]. Further evidence that supports this finding is that college students from urban area experience healthier behaviours (e.g. exercise, regular activities and nutrition) [44]. To relieve the pressure students from rural area faced in the college environment, which is very different to their homelands, personalised psychological health-promotion activities need to be introduced.
However, our stratified analysis on the results of TSMU did not show the same picture. The SHS and SCL-90 scores of students who came from rural area did not differ from students from urban area in TSMU, eastern China. Other than the fact that TSMU is a medical school, this might be also explained by the smaller rural-urban gap in the economically developed eastern area of China where rapid economic development and urbanisation continue.
Our results revealed a higher prevalence of SHS and SCL-90 symptoms among female students compared with male students, indicating that female students are more susceptible to developing SHS and mental problems. The differences in physiological and psychological profiles between genders may contribute to this phenomenon [18]. Furthermore, male and female students have different lifestyles and pursue physical activities relevant to their physical and psychological health state [45, 46]. This finding is consistent with previous studies, in which women are documented to be more prone to depression, anxiety and other neuropsychiatric disorders [19, 47].
This study has also indicated that the prevalence of SHS among sophomore students is about three times that of junior students and nearly two times that of freshmen. In particular, the prevalence of positive SCL-90 symptoms in sophomores is about three times that observed in freshmen and nearly five times that of juniors. This might indicate that because freshmen are newly exposed to university life, they have not yet feeled the academic pressure in universities, while junior students have already adapted well to academic and living environments during their 2 years of university life [20].
Significant differences of SHS prevalence as well as significant discrepancies of SCL-90 symptoms between medical and non-medical students were also observed in this study. It has been shown that, worldwide, academic stressors and competitive pressure in medical school, different to that faced by non-medical students, induce this outcome [48]. A comprehensive review of 183 original studies showed that the pooled prevalence rate of depression or depression symptoms among medical students is 27.2% [48]. Two representative studies evaluating depression symptoms among non-medical college students revealed the prevalence of depression ranged from 13.8 to 21.0%, lower than the levels of medical college students [49, 50]. Therefore, strategies for predictive, preventive and personalised health interventions for medical undergraduates need more attention.
Counterintuitively, SHS was relatively lower in the overweight students than in other groups in this study. Moreover, the summed SCL-90 score in the overweight students was slightly lower than that in the other three groups. Meanwhile, age and vital capacity level were not found to be different between SHS and healthy participants. This may result from the homogenous age range and physical features across the students in our study. Compared with Africans and Caucasians who were also measured by SHSQ-25, our study found a similar SHS level with Ghanaians and a higher level than Russians [4, 16].
The multivariate logistic regression analysis showed that grade, symptoms of somatisation, obsessive-compulsive, interpersonal sensitivity, depression and other problems such as sleep and diet are the main factors associated with SHS. Univariate analysis showed that rural students and medical students suffer more from SHS, while the results of the multivariate analysis suggested that the psychological problems among these students play a crucial role in the development of SHS. Students who had the same score of SHS may experience discrepancies in their psychological status, whereas students with the same SCL-90 score might differ in other SHS health conditions. In addition, gender, discipline major, grade, homeland and academic pressure are all aspects that have to be considered in terms of PPPM.
Limitations
This was a cross-sectional study, which did not allow us to measure accurate causality between psychological symptoms and SHS. Additionally, all data was collected by self-rating questionnaires, which might have led to information bias.
Conclusions
This study demonstrated that female students, sophomore students, medical students and students from rural area are at high risk of SHS and psychological symptoms. Psychological factors, such as somatisation, obsessive-compulsive, interpersonal sensitivity, depression and sleep and diet problems, are the key factors positively associated with SHS. From the perspectives of PPPM, strategies for early, personalised intervention at the SHS stage are urgently needed to promote student capacities for psychological adaptation and to improve their flexibility and resilience. More attention on relieving the academic stress experienced by medical students is needed.
Recommendations
With regard to synergetic strength of using a continuation of physical and mental tools for measuring health, a simple method for psychological and physical health assessments of college students is urgently needed from the perspectives of PPPM. The differences in health status between students, in terms of rural vs. urban, medical vs. non-medical discipline, male vs. female and economically developed region vs. under development region in China, suggest that a combination approach of using SHSQ-25 and SCL-90 is a cost-effective and time-efficient tool for health measurement at a population level, aligning with the PPPM strategy. Reliable prediction of SHS and mental health, and consequent solution through the early application of personalised psychological health-supporting activities, such as the application of SHS and SCL-90 in this current study, is of great benefit not only at an individual level but also at a societal level from the perspective of PPPM.
Electronic supplementary material
(DOCX 346 kb)
Acknowledgements
We acknowledge the participants from Taishan Medical University and Baoji Vocational and Technical College for their consent and support for this investigation. We also thank Amanda Harris for her English editing.
Abbreviations
- BMI
Body mass index
- CI
Confidence intervals
- OR
Odds ratio
- SCL-90
Symptom Checklist-90
- SHS
Suboptimal health status
- SHSQ-25
Suboptimal Health Status Questionnaire-25
- WHO
World Health Organization
Authors’ contributions
HH, DL and WW designed the study. XF, YL, GD, DG, FW, ZP and WZ carried out the participant recruitment and the survey. ZG and YZ conducted the statistical analyses. ZM, HH, WW and GD wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethical approval and consent to participate
The Human Research Ethics Committee of Taishan Medical University (TSMU) approved this study. All procedures performed in the study involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments. All participants were required to sign an informed consent form before being enrolled in this study.
Contributor Information
Haifeng Hou, Email: hfhou@163.com.
Xia Feng, Email: fengxia357@163.com.
Yuejin Li, Email: lyjtsmc@163.com.
Zixiu Meng, Email: zixiumeng@163.com.
Dongmei Guo, Email: 296546137@qq.com.
Fang Wang, Email: wangf@tsmc.edu.cn.
Zheng Guo, Email: hero3632@vip.qq.com.
Yulu Zheng, Email: 737821417@qq.com.
Zhiqi Peng, Email: 153676392@qq.com.
Wangxin Zhang, Email: zwxxwz0@163.com.
Dong Li, Email: tsmcdongli@163.com.
Guoyong Ding, Phone: +86-13205381630, Email: dgy153@126.com.
Wei Wang, Phone: +61-418469913, Email: wei.wang@ecu.edu.au.
References
- 1.WHO Terminology Information System [online glossary] http://www.who.int/health-systems-performance/docs/glossary.htm
- 2.Wang Y, Liu X, Qiu J, Wang H, Liu D, Zhao Z, Song M, Song Q, Wang X, Zhou Y, Wang W. Association between ideal cardiovascular health metrics and suboptimal health status in Chinese population. Sci Rep. 2017;7(1):14975. doi: 10.1038/s41598-017-15101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yan YX, Dong J, Liu YQ, Yang XH, Li M, Shia G, Wang W. Association of suboptimal health status and cardiovascular risk factors in urban Chinese workers. J Urban Health. 2012;89(2):329–338. doi: 10.1007/s11524-011-9636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adua E, Roberts P, Wang W. Incorporation of suboptimal health status as a potential risk assessment for type II diabetes mellitus: a case-control study in a Ghanaian population. EPMA J. 2017;8(4):345–355. doi: 10.1007/s13167-017-0119-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzain MA, Asweto CO, Zhang J, Fang H, Zhao Z, Guo X, Song M, Zhou Y, Chang N, Wang Y, Wang W. Telomere length and accelerated biological aging in the China suboptimal health cohort: a case-control study. OMICS. 2017;21(6):333–339. doi: 10.1089/omi.2017.0050. [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Ge S, Yan Y, Wang A, Zhao Z, Yu X, Qiu J, Alzain MA, Wang H, Fang H, Gao Q, Song M, Zhang J, Zhou Y, Wang W. China suboptimal health cohort study: rationale, design and baseline characteristics. J Transl Med. 2016;14(1):291. doi: 10.1186/s12967-016-1046-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yan Yu-Xiang, Wu Li-Juan, Xiao Huan-Bo, Wang Shuo, Dong Jing, Wang Wei. Latent class analysis to evaluate performance of plasma cortisol, plasma catecholamines, and SHSQ-25 for early recognition of suboptimal health status. EPMA Journal. 2018;9(3):299–305. doi: 10.1007/s13167-018-0144-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang W, Yan Y. Suboptimal health: a new health dimension for translational medicine. Clin Transl Med. 2012;1(1):28. doi: 10.1186/2001-1326-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang W, Russell A, Yan Y. Traditional Chinese medicine and new concepts of predictive, preventive and personalized medicine in diagnosis and treatment of suboptimal health. Global Health Epidemiology Reference Group (GHERG) EPMA J. 2014;5(1):4. doi: 10.1186/1878-5085-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joustra ML, Janssens KA, Bültmann U, Rosmalen JG. Functional limitations in functional somatic syndromes and well-defined medical diseases. Results from the general population cohort LifeLines. J Psychosom Res. 2015;79(2):94–99. doi: 10.1016/j.jpsychores.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Cheng J, Liu Y, Tang Y, Sun X, Wang T, Xiao Y, Li F, Xiang L, Jiang P, Wu S, Wu L, Luo R, Zhao X. Associations between breakfast eating habits and health-promoting lifestyle, suboptimal health status in Southern China: a population based, cross sectional study. J Transl Med. 2014;12:348. doi: 10.1186/s12967-014-0348-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tavel ME. Somatic symptom disorders without known physical causes: one disease with many names? Am J Med. 2015;128(10):1054–1058. doi: 10.1016/j.amjmed.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 13.Greco M. The classification and nomenclature of 'medically unexplained symptoms': conflict, performativity and critique. Soc Sci Med. 2012;75(12):2362–2369. doi: 10.1016/j.socscimed.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Liang YZ, Chu X, Meng SJ, Zhang J, Wu LJ, Yan YX. Relationship between stress-related psychosocial work factors and suboptimal health among Chinese medical staff: a cross-sectional study. BMJ Open. 2018;8(3):e018485. doi: 10.1136/bmjopen-2017-018485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henningsen P, Zipfel S, Sattel H, Creed F. Management of functional somatic syndromes and bodily distress. Psychother Psychosom. 2018;87(1):12–31. doi: 10.1159/000484413. [DOI] [PubMed] [Google Scholar]
- 16.Kupaev V, Borisov O, Marutina E, Yan YX, Wang W. Integration of suboptimal health status and endothelial dysfunction as a new aspect for risk evaluation of cardiovascular disease. EPMA J. 2016;7(1):19. doi: 10.1186/s13167-016-0068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neumann A, Schoffer O, Norström F, Norberg M, Klug SJ, Lindholm L. Health-related quality of life for pre-diabetic states and type 2 diabetes mellitus: a cross-sectional study in Västerbotten Sweden. Health Qual Life Outcomes. 2014;12:150. doi: 10.1186/s12955-014-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu SH, Chen DR, Cheng Y, Su TC. Association of psychosocial work hazards with depression and suboptimal health in executive employees. J Occup Environ Med. 2016;58(7):728–736. doi: 10.1097/JOM.0000000000000760. [DOI] [PubMed] [Google Scholar]
- 19.Bi J, Huang Y, Xiao Y, Cheng J, Li F, Wang T, Chen J, Wu L, Liu Y, Luo R, Zhao X. Association of lifestyle factors and suboptimal health status: a cross-sectional study of Chinese students. BMJ Open. 2014;4(6):e005156. doi: 10.1136/bmjopen-2014-005156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma C, Xu W, Zhou L, Ma S, Wang Y. Association between lifestyle factors and suboptimal health status among Chinese college freshmen: a cross-sectional study. BMC Public Health. 2018;18(1):105. doi: 10.1186/s12889-017-5002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yan YX, Dong J, Liu YQ, Zhang J, Song MS, He Y, Wang W. Association of suboptimal health status with psychosocial stress, plasma cortisol and mRNA expression of glucocorticoid receptor α/β in lymphocyte. Stress. 2015;18(1):29–34. doi: 10.3109/10253890.2014.999233. [DOI] [PubMed] [Google Scholar]
- 22.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K. Prevalence of mental disorders in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand. 2004;109:21–27. doi: 10.1111/j.1600-0047.2004.00325.x. [DOI] [PubMed] [Google Scholar]
- 23.Twenge JM, Gentile B, DeWall CN, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938-2007: a cross-temporal meta-analysis of the MMPI. Clin Psychol Rev. 2010;30:145–154. doi: 10.1016/j.cpr.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Liu F, Zhou N, Cao H, Fang X, Deng L, Chen W, Lin X, Liu L, Zhao H. Chinese college freshmen's mental health problems and their subsequent help-seeking behaviors: a cohort design (2005-2011) PLoS One. 2017;12(10):e0185531. doi: 10.1371/journal.pone.0185531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Velten J, Bieda A, Scholten S, Wannemüller A, Margraf J. Lifestyle choices and mental health: a longitudinal survey with German and Chinese students. BMC Public Health. 2018;18(1):632. doi: 10.1186/s12889-018-5526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation—EPMA position paper 2016. EPMA J. 2016;7:23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan YX, Liu YQ, Li M, Hu PF, Guo AM, Yang XH, Qiu JJ, Yang SS, Wang W. Development and evaluation of a questionnaire for measuring suboptimal health status in urban Chinese. J Epidemiol. 2009;19(6):333–341. doi: 10.2188/jea.JE20080086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derogatis LR, Cleary PA. Factorial invariance across gender for the primary symptom dimensions of the SCL-90. Br J Soc Clin Psychol. 1977;16(4):347–356. doi: 10.1111/j.2044-8260.1977.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 29.Liu J, Yi Z, Zhao Y, Qu B, Zhu Y. The psychological health and associated factors of men who have sex with men in China: a cross-sectional survey. PLoS One. 2018;13(5):e0197481. doi: 10.1371/journal.pone.0197481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Working Group on Obesity in China The guidelines for prevention and control of overweight and obesity in Chinese adults (in Chinese) Acta Nutrimenta Sinica. 2004;26(1):1–4. [Google Scholar]
- 31.Chakraborty K, Avasthi A, Kumar S, Grover S. Psychological and clinical correlates of functional somatic complaints in depression. Int J Soc Psychiatry. 2012;58(1):87–95. doi: 10.1177/0020764010387065. [DOI] [PubMed] [Google Scholar]
- 32.Fink P, Rosendal M, Olesen F. Classification of somatization and functional somatic symptoms in primary care. Aust N Z J Psychiatry. 2005;39(9):772–781. doi: 10.1080/j.1440-1614.2005.01682.x. [DOI] [PubMed] [Google Scholar]
- 33.Richter PMA, Ramos RT. Obsessive-compulsive disorder. Continuum (MinneapMinn) 2018;24:828–844. doi: 10.1212/CON.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 34.Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, Huppert JD, Kjernisted K, Rowan V, Schmidt AB, Simpson HB, Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- 35.Jaisoorya TS, Janardhan Reddy YC, Nair BS, Rani A, Menon PG, Revamma M, Jeevan CR, Radhakrishnan KS, Jose V. Prevalence and correlates of obsessive-compulsive disorder and subthreshold obsessive-compulsive disorder among college students in Kerala, India. Indian J Psychiatry. 2017;59(1):56–62. doi: 10.4103/0019-5545.204438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harb GC, Heimberg RG, Fresco DM, Schneier FR, Liebowitz MR. The psychometric properties of the interpersonal sensitivity measure in social anxiety disorder. Behav Res Ther. 2002;40(8):961–979. doi: 10.1016/S0005-7967(01)00125-5. [DOI] [PubMed] [Google Scholar]
- 37.Mohammadian Y, Mahaki B, Dehghani M, Vahid MA, Lavasani FF. Investigating the role of interpersonal sensitivity, anger, and perfectionism in social anxiety. Int J Prev Med. 2018;9:2. doi: 10.4103/ijpvm.IJPVM_364_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davidson J, Zisook S, Giller E, Helms M. Symptoms of interpersonal sensitivity in depression. Compr Psychiatry. 1989;30(5):357–368. doi: 10.1016/0010-440X(89)90001-1. [DOI] [PubMed] [Google Scholar]
- 39.January J, Madhombiro M, Chipamaunga S, Ray S, Chingono A, Abas M. Prevalence of depression and anxiety among undergraduate university students in low- and middle-income countries: a systematic review protocol. Syst Rev. 2018;7(1):57. doi: 10.1186/s13643-018-0723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Haidar SA, de Vries NK, Karavetian M, El-Rassi R. Stress, anxiety, and weight gain among university and college students: a systematic review. J Acad Nutr Diet. 2018;118(2):261–274. doi: 10.1016/j.jand.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 41.Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48(10):963–979. doi: 10.1111/medu.12512. [DOI] [PubMed] [Google Scholar]
- 42.Hou J, Xu M, Kolars JC, Dong Z, Wang W, Huang A, Ke Y. Career preferences of graduating medical students in China: a nationwide cross-sectional study. BMC Med Educ. 2016;16:136. doi: 10.1186/s12909-016-0658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Bureau of Statistics of China . China statistical yearbook 2017 (in Chinese) Beijing: China Statistics Press; 2017. [Google Scholar]
- 44.Wang D, Xing XH, Wu XB. Healthy lifestyles of university students in China and influential factors. Sci World J. 2013;2013:412950. doi: 10.1155/2013/412950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu J, Wei Y. Social support as a moderator of the relationship between anxiety and depression: an empirical study with adult survivors of Wenchuan earthquake. PLoS One. 2013;8(10):e79045. doi: 10.1371/journal.pone.0079045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adams TB, Moore MT, Dye J. The relationship between physical activity and mental health in a national sample of college females. Women Health. 2007;45(1):69–85. doi: 10.1300/J013v45n01_05. [DOI] [PubMed] [Google Scholar]
- 47.Romero-Acosta K, Canals J, Hernández-Martínez C, Penelo E, Zolog TC, Domènech-Llaberia E. Age and gender differences of somatic symptoms in children and adolescents. J Ment Health. 2013;22(1):33–41. doi: 10.3109/09638237.2012.734655. [DOI] [PubMed] [Google Scholar]
- 48.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am J Orthop. 2007;77(4):534–542. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- 50.Steptoe A, Tsuda A, Tanaka Y, Wardle J. Depressive symptoms, socio-economic background, sense of control, and cultural factors in university students from 23 countries. Int J Behav Med. 2007;14(2):97–107. doi: 10.1007/BF03004175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 346 kb)