Abstract
Knee flexion contracture is a clinically important complication that can be observed after trauma, after knee surgery, or as a result of osteoarthritis. When it is left untreated, knee shearing forces increase not only in the affected joint but also in the contralateral knee, leading to mechanical overload in both limbs. Conservative management is a first-line treatment option for extension deficits, but when it fails, surgical treatment is necessary. Open as well as arthroscopic techniques focus mainly on an anterior arthrolysis and a posterior capsular release. Until now, posterior capsulotomy involved either a medial posterior capsular release or medial and lateral posterior capsular releases. Our aim is to present the technique of arthroscopic complete posterior capsulotomy for knee flexion contractures.
Trauma, surgery, or osteoarthritis can lead to a limitation in knee motion. Whereas a small flexion deficit is tolerated well, an extension deficit is a clinically important issue because of relative shortening of the affected leg with the consequences of hip joint disorders and scoliosis formation. It is also worth noting that extension deficits cause mechanical overloads not only in the affected joint but also in the contralateral knee.1 Conservative management, which is a first-line treatment option for flexion contracture, can be ineffective owing to progressive thickening of the posterior knee capsule and changes in its histologic characterization over time.2 Then, surgical treatment is necessary. Open techniques with a posterior approach carry an increased risk of complications, such as a popliteal artery injury. Improvement in knowledge of the posterior knee anatomy, the development of arthroscopic surgery, and the creation of portals for posterior-compartment visualization are the reasons arthroscopic surgery has become the preferred treatment option for knee extension deficits.3, 4, 5, 6 Until now, an isolated medial posterior capsular release or medial and lateral posterior capsular releases have been described in the literature.7, 8 We present a safe and effective technique for arthroscopic complete posterior capsulotomy.
Surgical Technique
Indications
The indications for the described procedure are clinically significant asymmetrical extension deficits that persist after conservative management, manipulation under anesthesia, and anterior arthrolysis.
Patient Positioning
The operation is performed with the patient under general or regional anesthesia and positioned supine. Range of motion is evaluated with a goniometer for both knees. The operative leg with a nonsterile thigh tourniquet is placed in a leg holder and then prepared and draped in a sterile fashion.
Arthroscopic Complete Posterior Capsulotomy
The procedure is performed with the knee in 90° of flexion through standard anterolateral and anteromedial arthroscopic portals. After thorough inspection of the knee joint, through an anterolateral viewing portal, a 30° arthroscope (Arthrex, Naples, FL) is directed between the posterior cruciate ligament and medial femoral condyle, medially to the posterior cruciate ligament, and positioned in the posteromedial compartment. Under arthroscopic visualization, a posteromedial arthroscopic portal is created in the soft spot between the posterior oblique ligament and the medial edge of the medial head of the gastrocnemius muscle using a spinal needle and No. 11 surgical blade (Fig 1, Video 1). Metzenbaum scissors (Praxisdienst Medical Supplies, Longuich, Germany) are introduced through the posteromedial portal. Next, the closed Metzenbaum scissors are inserted behind the posteromedial joint capsule and directed anteriorly and laterally (Video 1). The instrument is then opened to spread open the tissue planes and is pulled out without closing medially until it reaches the posteromedial portal. In this way, a free space behind the posteromedial joint capsule is created. Then, the tight posteromedial capsule is placed between the scissor blades, and the posterior blade is directed anteriorly to avert it from the popliteal neurovascular bundle (Video 1). The capsule is sectioned from medial to lateral until the midline posterior septum is reached (Fig 2, Video 1). Then, a switching stick (ConMed, Largo, FL) is introduced through the posteromedial portal and used to insert the arthroscope. An additional anteromedial parapatellar portal is now made and used to introduce a radiofrequency (RF) probe (Smith & Nephew, London, England) into the posteromedial compartment. The aforementioned instrument is used to extend the sectioning of the posteromedial capsule laterally and partially remove the posterior septum (Fig 3, Video 1). A 4.5-mm shaver (ConMed) is used to remove the remainder of the posterior septum.
Fig 1.

Arthroscopic view from anterolateral viewing portal in posteromedial compartment of left knee joint. The posteromedial portal is created with a No. 11 blade in the soft spot between the posterior oblique ligament (POL) and medial edge of the medial head of the gastrocnemius. (MFC, medial femoral condyle; MM, medial meniscus.)
Fig 2.
(A) Arthroscopic view from anteromedial portal to posteromedial compartment in left knee joint. The posteromedial capsule is sectioned with scissors from the medial side to the posterior septum. (B) Arthroscopic view from posteromedial portal showing capsulotomy. (MFC, medial femoral condyle; PCL, posterior cruciate ligament.)
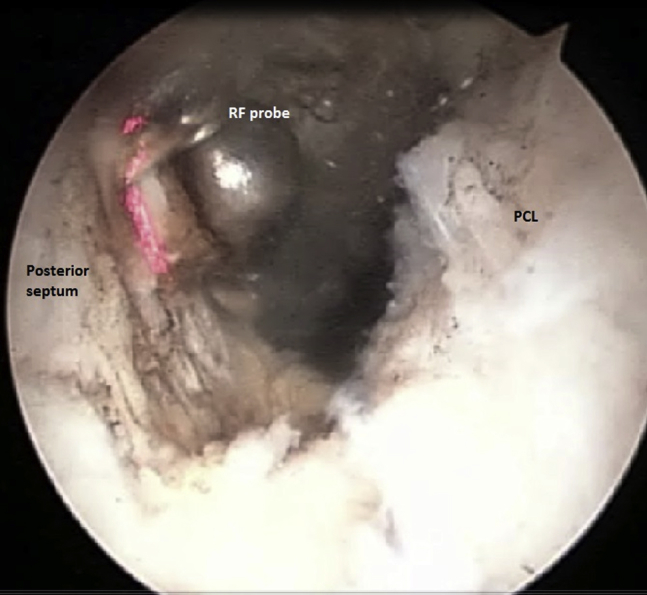
Fig 3.

Arthroscopic view from posteromedial portal in left knee joint. The radiofrequency (RF) probe, introduced through an additional anteromedial parapatellar portal, is used to extend the sectioning of the posteromedial capsule laterally and partially remove the posterior septum. (MFC, medial femoral condyle; PCL, posterior cruciate ligament.)
The arthroscope, introduced through the anteromedial viewing portal, is now inserted between the posterolateral bundle of the anterior cruciate ligament and lateral femoral condyle, as well as above the lateral meniscus root, to enter the posterolateral compartment. A posterolateral arthroscopic portal is created in the soft spot between the fibular collateral ligament and lateral edge of the lateral head of the gastrocnemius muscle (Fig 4, Video 1). As previously performed in the posteromedial compartment, Metzenbaum scissors are used to create a free space behind the posterolateral capsule and to perform a capsulotomy (Fig 5, Video 1). Because the posterolateral capsule is thicker than the posteromedial capsule, the superficial layer is sectioned first; then, the deep layer is sectioned in a stepwise fashion (Video 1). The deepest longitudinal fibers of the posterolateral capsule are sectioned with the RF probe until the connective tissue of the popliteal fossa becomes visible (Fig 6, Video 1). Then, the switching stick is introduced through the posterolateral portal and used to insert the arthroscope. Through the anteromedial parapatellar portal, the RF probe and shaver are introduced sequentially to remove the remaining lateral part of the posterior septum. The technique is a mirror image of the technique performed on the medial side. Now, both posterior recesses of the knee are visible.
Fig 4.

Arthroscopic view from anteromedial viewing portal in posterolateral compartment of left knee joint. The posterolateral portal is created in the soft spot between the fibular collateral ligament (FCL) and lateral edge of the lateral head of the gastrocnemius. (LFC, lateral femoral condyle; LM, lateral meniscus.)
Fig 5.

Arthroscopic view from anteromedial viewing portal in posterolateral compartment of left knee joint. Closed scissors, introduced behind the posterolateral capsule, are used to create free space for safe maneuvering. After that, the scissors are used to perform posterolateral capsulotomy. (LFC, lateral femoral condyle; LM, lateral meniscus.)
Fig 6.

Arthroscopic view from anteromedial viewing portal in posterolateral compartment of left knee joint. The radiofrequency (RF) probe, introduced through the posterolateral portal, is used to extend the sectioning of the posterolateral capsule and lateral part of the posterior septum. (LM, lateral meniscus.)
Viewing through the posteromedial portal, the surgeon introduces the RF probe through the posterolateral portal and uses it to remove the rest of the posterior septum (Fig 7, Video 1). The Metzenbaum scissors are introduced through the trans-septal portal, placed under visual control behind the remainder of the central posterior capsule, and used to push the capsule away from the popliteal fossa and separate it from the popliteal connective tissue (Video 1). The RF probe is then directed anteriorly and used to complete the cut of the longitudinal fibers of the posterior capsule (Fig 8, Video 1). In this way a complete posterior capsulotomy is performed. Now, a careful manipulation into hyperextension is performed until the symmetrical hyperextension of the knee joint is attained (Video 1).
Fig 7.
Arthroscopic view from posteromedial portal in left knee joint. The radiofrequency (RF) probe, introduced through the posterolateral portal, is used to remove the rest of the posterior septum. (PCL, posterior cruciate ligament.)
Fig 8.

Arthroscopic view from posteromedial portal in left knee joint. The radiofrequency probe, introduced through the posterolateral portal, is placed between the central posterior capsule and popliteal fossa connective tissue and used to remove the rest of the posterior capsule. The radiofrequency probe must be directed anteriorly.
Rehabilitation
After surgery, the patient performs gravitational hyperextension by keeping the heel of the operated leg on a pillow for 5 minutes each hour. Cold compresses and pain control are applied. Three weeks after surgery, the patient starts rehabilitation under the control of physiotherapist twice a week for 6 weeks. The patient walks using crutches for 2 to 6 weeks depending on the postoperative knee condition and the patient's tolerance.
Discussion
Limitation in knee motion remains one of the worst consequences of trauma or knee surgery. Extension deficits resistant to initial treatment usually are associated with posterior capsule contracture. Arthroscopic complete posterior capsulotomy, in comparison with open techniques, allows most complications of an open posterior approach to be avoided and the postoperative recovery time to be reduced. Using posteromedial, posterolateral, and trans-septal portals described in the literature for posterior knee arthroscopy enables one to precisely visualize the posterior knee compartments.4, 5, 6 It also minimizes the risk of improper identification of anatomic structures and landmarks, which can occur during open techniques, leading to intra-articular structure injuries and hematomas.9 Respecting the safe zones and relations between the popliteal neurovascular bundle and other structures allows the safe placement and use of instruments with the risk of popliteal artery injury reduced to a minimum.3 All the aforementioned facts made it possible for us to obtain access to the central part of the posterior knee capsule and to perform complete posterior knee capsulotomy, which is the most important advantage of our technique.
An incomplete posterior capsular release may result in surgical failure.9 In comparison with isolated posteromedial capsulotomy, the advantages of applying our technique are symmetry and complete release of contracted structures.7 Moreover, the posterolateral capsule is thicker than the posteromedial capsule, and releasing only the medial part may not be sufficient to restore full knee extension. This is why combined medial and lateral capsulotomy techniques were developed.8 Our technique, in comparison with the technique presented by Mariani,8 does not require cutting the gastrocnemius tendons. Thereby, the potential impairment of calf function with all further consequences can be omitted.
Arthroscopic complete posterior capsulotomy is an effective, safe, and reproducible technique to treat a knee flexion contracture. When performed with adequate anatomic knowledge and thoroughness, the risk of popliteal bundle injury is minimal. The presented technique allows not only for a combined medial and lateral posterior capsular release but also for a central capsulotomy. It provides a quick and permanent return of full knee extension and is well tolerated by patients. The recurrence of flexion contracture has not been observed.
Even if the risk of popliteal artery injury is minimal, it still exists. It can potentially occur when our technique is performed by an inexperienced surgeon. Moreover, the distance between the posterior capsule and popliteal neurovascular bundle is the highest in a knee with 90° of knee flexion. When 90° of flexion cannot be achieved, the technique should not be applied because of the higher risk of popliteal artery injury. Knowledge about creating posterior and trans-septal portals is also required. In addition, a preoperative magnetic resonance imaging scan should be obtained to exclude anatomic variations in the course of the popliteal vessels. Advanced degenerative changes, such as large osteophytes in the intercondylar fossa or on the tibial plateau, can make proper visualization of the posterior knee compartments complicated. In these cases the presented technique is much more difficult. All advantages and disadvantages of applying arthroscopic complete posterior capsulotomy are summarized in Table 1.
Table 1.
Advantages and Disadvantages of Arthroscopic Complete Posterior Capsulotomy
| Advantages | Disadvantages |
|---|---|
| Minimal invasiveness | Requirement for advanced arthroscopic skills |
| Adequate visualization of sectioned structures | Requirement for thorough knowledge of posterior knee anatomy |
| Symmetry and complete release of contracted structures | Necessity of experience in posterior knee compartment arthroscopy |
| Quick return of full knee extension | Risk of popliteal bundle injury |
| Good results of surgery independent of rehabilitation protocol | Application of technique hindered by advanced degenerative changes |
| High patient satisfaction | 90° of knee flexion crucial to perform procedure |
| Inexpensive and reproducible technique |
Footnotes
The authors report the following conflicts of interest or sources of funding: K.M. is a consultant for Zimmer Biomet and a board member for PTArtro. R.F.L. is a consultant for and receives royalties from Arthrex, Ossur, and Smith & Nephew, and is a member of the editorial boards for AJSM, JEO, and KSSTA. M.E.D. is a board member for PTArtro. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic complete posterior capsulotomy for left knee flexion contracture. During the procedure, 5 arthroscopic portals are used: posterolateral, anterolateral, additional anteromedial parapatellar, anteromedial, and posteromedial. At the beginning, the posteromedial portal is created under visual control. The scissors and radiofrequency (RF) probe are introduced through the posteromedial portal and used to section the posteromedial capsule from medial to lateral. The viewing portal is changed to posteromedial. The RF probe is introduced through an additional anteromedial parapatellar portal to the posteromedial compartment and is used to extend the posteromedial capsulotomy and remove the medial part of the posterior septum. Then, the instruments are moved to the posterolateral compartment. The technique on the lateral side is a mirror image of the technique performed previously in the posteromedial compartment. The capsule here is thicker, so it has to be sectioned sequentially—the superficial layer first, followed by the deep layer. When the lateral capsule is released, the arthroscope is introduced through the posteromedial portal. The RF probe, inserted through the posterolateral portal, is used to remove the rest of the posterior septum. At the end of the procedure, scissors introduced through the posterolateral portal are used to create free space between the central posterior capsule and popliteal fossa connective tissue. The RF probe directed anteriorly is introduced behind the central posterior capsule and used to section the rest of the posterior capsule. Now, a careful manipulation into hyperextension is performed until symmetrical hyperextension of the knee joint is attained.
References
- 1.Harato K., Nagura T., Matsumoto H., Otani T., Toyama Y., Suda Y. Knee flexion contracture will lead to mechanical overload in both limbs: A simulation study using gait analysis. Knee. 2008;15:467–472. doi: 10.1016/j.knee.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Campbell T.M., Trudel G., Laneuville O. Knee flexion contractures in patients with osteoarthritis: Clinical features and histologic characterization of the posterior capsule. PM R. 2015;7:466–473. doi: 10.1016/j.pmrj.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Pace J.L., Wahl C.J. Arthroscopy of the posterior knee compartments: Neurovascular anatomic relationships during arthroscopic transverse capsulotomy. Arthroscopy. 2010;26:637–642. doi: 10.1016/j.arthro.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Hamula M., Sewick A.E., Kelly J.D. Arthroscopic trans-septal portal to treat extension deficits from arthrofibrosis. Univ Penn Orthop J. 2012;22:21–25. [Google Scholar]
- 5.Ahn J.H., Ha C.W. Posterior trans-septal portal for arthroscopic surgery of the knee joint. Arthroscopy. 2000;16:774–779. doi: 10.1053/jars.2000.7681. [DOI] [PubMed] [Google Scholar]
- 6.Louisia S., Charrois O., Beaufils P. Posterior "back and forth" approach in arthroscopic surgery on the posterior knee compartments. Arthroscopy. 2003;19:321–325. doi: 10.1053/jars.2003.50082. [DOI] [PubMed] [Google Scholar]
- 7.Dean C.S., Chahla J., Mikula J.D., Mitchell J.J., LaPrade R.F. Arthroscopic posteromedial capsular release. Arthrosc Tech. 2016;5:e495–e500. doi: 10.1016/j.eats.2016.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mariani P.P. Arthroscopic release of the posterior compartments in the treatment of extension deficit of knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:736–741. doi: 10.1007/s00167-009-0920-z. [DOI] [PubMed] [Google Scholar]
- 9.Gomes J.L.E., Leie M.A., de Freitas Soares A., Ferrari M.B., Sánchez G. Posterior capsulotomy of the knee: Treatment of minimal knee extension deficit. Arthrosc Tech. 2017;6:e1535–e1539. doi: 10.1016/j.eats.2017.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic complete posterior capsulotomy for left knee flexion contracture. During the procedure, 5 arthroscopic portals are used: posterolateral, anterolateral, additional anteromedial parapatellar, anteromedial, and posteromedial. At the beginning, the posteromedial portal is created under visual control. The scissors and radiofrequency (RF) probe are introduced through the posteromedial portal and used to section the posteromedial capsule from medial to lateral. The viewing portal is changed to posteromedial. The RF probe is introduced through an additional anteromedial parapatellar portal to the posteromedial compartment and is used to extend the posteromedial capsulotomy and remove the medial part of the posterior septum. Then, the instruments are moved to the posterolateral compartment. The technique on the lateral side is a mirror image of the technique performed previously in the posteromedial compartment. The capsule here is thicker, so it has to be sectioned sequentially—the superficial layer first, followed by the deep layer. When the lateral capsule is released, the arthroscope is introduced through the posteromedial portal. The RF probe, inserted through the posterolateral portal, is used to remove the rest of the posterior septum. At the end of the procedure, scissors introduced through the posterolateral portal are used to create free space between the central posterior capsule and popliteal fossa connective tissue. The RF probe directed anteriorly is introduced behind the central posterior capsule and used to section the rest of the posterior capsule. Now, a careful manipulation into hyperextension is performed until symmetrical hyperextension of the knee joint is attained.



