Abstract
Background
Vitamin K antagonist (VKA) to prevent thromboembolism in non-valvular atrial fibrillation (NVAF) patients has limitations such as drug interaction. This study investigated the clinical characteristics of Korean patients treated with VKA for stroke prevention and assessed quality of VKA therapy and treatment satisfaction.
Methods
We conducted a multicenter, prospective, non-interventional study. Patients with CHADS2 ≥ 1 and treated with VKA (started within the last 3 months) were enrolled from April 2013 to March 2014. Demographic and clinical features including risk factors of stroke and VKA treatment information was collected at baseline. Treatment patterns and international normalized ratio (INR) level were evaluated during follow-up. Time in therapeutic range (TTR) > 60% indicated well-controlled INR. Treatment satisfaction on the VKA use was measured by Treatment Satisfaction Questionnaire for Medication (TSQM) after 3 months of follow-up.
Results
A total of 877 patients (age, 67; male, 60%) were enrolled and followed up for one year. More than half of patients (56%) had CHADS2 ≥ 2 and 83.6% had CHA2DS2-VASc ≥ 2. A total of 852 patients had one or more INR measurement during their follow-up period. Among those patients, 25.5% discontinued VKA treatment during follow-up. Of all patients, 626 patients (73%) had poor-controlled INR (TTR < 60%) measure. Patients' treatment satisfaction measured with TSQM was 55.6 in global satisfaction domain.
Conclusion
INR was poorly controlled in Korean NVAF patients treated with VKA. VKA users also showed low treatment satisfaction.
Keywords: Atrial Fibrillation, Anticoagulation, Vitamin K Antagonist, INR Control, Satisfaction
Graphical Abstract
INTRODUCTION
The prevalence of atrial fibrillation (AF), the most common sustained arrhythmia, was 0.7% in adults 40 years of age or older and 2.1% in adults 65 years or older in Korea.1 As reported in several precedent studies, an increase in age is a risk factor in patients with AF,2 thus as the population is aging, the incidence rate of AF is likely to increase and hospital utilization rate and the mortality rate are expected to increase as well. In addition, AF is a disease that becomes a risk factor for stroke and systemic embolism.3 In particular, strokes accompanied by AF showed a higher mortality rate and hospitalization costs than strokes not accompanied by AF.4,5,6 According to the results of a study of the ratio of patients immobilized due to stroke, patients with strokes accompanied by AF showed a higher invalidity rate than patients with strokes not accompanied by AF (41.2% vs. 23.7%, P < 0.0005).5 Likewise, various studies showed that the prognosis is much worse when accompanied by AF than when not accompanied by AF.
The 2014 American Heart Association (AHA)/American College of Cardiology (ACC)/Heart Rhythm Society (HRS) guidelines recommend medicines for preventive treatment according to the risk of a stroke for a patient with AF.7 However, many study results showed that patients are receiving treatment that does not correspond to the treatment guidelines or have even received no treatment at all in real-world clinical scenes. According to a systematic literature review of 54 studies reported from 1998 to 2008,8 less than 70% of patients were treated with an anticoagulant even after they were determined to be in a high-risk group by the CHADS2 score used to determine the stroke risk level, and 2/3 of the studies reported that less than 60% of the patient group with a history of stroke or transient ischemic attack was treated.
Vitamin K antagonist (VKA), which is considered to be a standard of care among the anticoagulant medicines to prevent strokes in patients with AF, has a very narrow therapeutic range, thus regular monitoring is required to avoid potential adverse events.9 However, according to the results of the Korean Patients with Atrial Fibrillation (KORAF) study conducted on AF patients in Korea, the international normalized ratio (INR) was adequately controlled in only about 40% of patients treated with VKA.10 A comparative study on severe adverse events (SAE) such as death, occurrence of thrombosis related to an anticoagulant, and additional administration of heparin between a patient group that had a poorly controlled INR value and a patient group that had a well-controlled INR value revealed that the SAE incidence rate of the patient group that had a poorly controlled INR was higher than that of the patient group that had a well-controlled INR.11 Thus, INR control is important when using a VKA.
The purpose of this study is to investigate the clinical and demographic characteristics of Korean patients with non-valvular AF treated with VKA for stroke prevention and determine the ratio of patients who have a well-controlled INR, and also evaluate the difference between the group that has a well-controlled INR and the group that has a poorly controlled INR. In addition, we tried to identify the patients' satisfaction with VKA treatment, continuation rate, and reasons for discontinuation of treatment.
METHODS
Study subjects
This is a Korean Atrial Fibrillation Investigation II (KORAFII) study with a multicenter, prospective, non-interventional design. The patients were enrolled at 20 cardiology clinics nationwide from April 2013 to March 2014. The study subjects were selected according to the following inclusion criteria: 1) Patients who are 20 years of age or over and diagnosed with non-valvular AF, 2) Patients who newly start VKA treatment (Daehwa Warfarin 2 mg or 5 mg Tab, Daehwa Pharmaceutical, Hoengseong-eup, Korea; Jeil Warfarin 5 mg Tab, Jeil Pharmaceutical Co., Seoul, Korea; Kufarin 2 mg or 5 mg Tab, Hana Pharm Co., Seoul, Korea) to prevent a stroke and systemic embolism or have started VKA treatment within the last 3 months, 3) Patients with CHADS2 ≥ 1, 4) Patients for whom regular INR monitoring is considered possible by the researchers, 5) Patients for whom one-year follow-up is possible, and 6) Patients who can understand the description of the written consent and the consent form and submit the consent form.
Calculation of number of subjects
According to the related literature, about 50%12 of the patients treated with VKA discontinued VKA administration within 1 year, and thus received inappropriate care. Among the remaining 50% of patients who continued to receive VKA administration, about 60%1 (i.e., 30% of total patients) also received inappropriate care because their INR level failed to reach level 2–3. In other words, the adequate control ratio of INR for patients treated with VKA was about 20% at the maximum, and the number of final target cases calculated at 95% confidence level with a margin of error of ± 2.5% using the PASS 2008 program (NCSS, Kaysville, UT, USA)13 was approximately 1,000.14,15 In this study, a final 877 patients were enrolled according to their voluntary consent to participate and the selection criteria from among patients treated with VKA in all participating medical institutions.
Study data and follow-up
In this study, the characteristics of patients and VKA usage patterns were identified by following up for 12 months after the patient enrollment date, and the data collected to investigate the INR control, VKA treatment satisfaction and so on were largely classified into investigation variables at the baseline and at the follow-up point. The following variables were investigated as the baseline characteristics of patients: 1) Demographic/clinical characteristics (sex, age, body mass index [BMI], date diagnosed with non-valvular AF/AF type) and 2) stroke and hemorrhage risk factors (components of CHA2DS2-VASc and HAS-BLED scores). In addition, demographic variables that could not be gathered by the medical record review (smoking, drinking, underlying diseases, occupation and education) were collected with a patient questionnaire. The VKA treatment patterns (date/values of INR measurement, continuation of VKA prescription, etc.) were collected by the medical record review during the follow-up period, and treatment satisfaction was investigated with two types of questionnaires (a simple questionnaire and the Treatment Satisfaction Questionnaire for Medication, or TSQM).
Degree of INR control
The degree of INR control (well controlled or poorly controlled) was identified by 12-month follow-up and assessed by the proportion of tests in a range method. Time in therapeutic range (TTR) was defined as the ratio of the days showed the optimal INR level (2.0–3.0) to total visit days during 12 months. And the well-controlled INR group was defined as patients who showed TTR in equal to or more than 60%. The poor-controlled INR group was defined as patients other than well-controlled INR. The cut-off value, 60%, was defined by the investigators using insight based on extensive clinical experience. The INR values used in the analysis were from the patients whose INR was measured at least once during the 12-month follow-up.
VKA treatment satisfaction
The treatment satisfaction of patients was assessed by two types of self-completed treatment satisfaction surveys of all patients. A simple questionnaire simply asked if the patient was satisfied with the treatment and investigated the cause and presented the results in a percentage if the patient was not satisfied. The TSQM, which was composed of four domains (effectiveness, side effects, convenience, and global) was conducted as another survey tool. The score, which is from 0 to 100, is graded by domain, and a higher score means greater satisfaction. Multiple linear regressions were conducted to find the variables that affected satisfaction for each TSQM domain.
Definition of time to reach optimal dose
The time to reach the optimal dose was defined as the time from the baseline point to the initial point (day) at which the INR values were “consecutively” maintained within 2–3 scores twice or more. The subjects whose INR values were not consecutively maintained within 2–3 scores twice or more at each point of value measurement were processed as censored, and the time from the baseline to the final INR measurement date was considered to be the censored observation time. The Kaplan-Meier survival function was used to assess the time when they reached the optimal dose.
Statistical analysis
Baseline characteristics of study subjects
Continuous data was displayed by means, standard deviations or medians and was analyzed using Student's t-test or analysis of variance to compare the characteristics by group. Categorical data was displayed by absolute frequency and rate and was analyzed using a χ2 test or Fisher's exact test to compare the characteristics by group.
Ethics Statement
This study was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital (IRB No. AN12250-001). All patients provided their informed consent prior to their enrollment in the study.
RESULTS
Baseline characteristics
A total of 877 patients with NVAF (mean age, 67.7; males, 60.1%) were enrolled in this study. The mean CHADS2 scores of the patients was 1.85, and the ratio of high-risk group patients with scores of 2 or higher was more than half (56.0%). The mean CHA2DS2-VASc score was 2.9, and the ratio of high-risk group patients with scores of 2 or higher was considerable (83.6%). The mean HAS-BLED score was 1.5, and the ratio of high-risk group patients with scores of 3 or higher was 7.7% (Table 1).
Table 1. Baseline characteristics.
| Characteristics | Value (n = 877) | |
|---|---|---|
| Sex, male | 527 (60.1) | |
| Age, yr | 67.68 (10.1) | |
| BMI | 24.80 (3.3) | |
| NVAF duration,a mon | 18.17 (33.9) | |
| Type of NVAF | ||
| First diagnosed | 94 (10.7) | |
| Paroxysmal | 271 (30.9) | |
| Persistent | 346 (39.5) | |
| Long-standing persistent | 43 (4.9) | |
| Permanent | 82 (9.4) | |
| Unknown | 41 (4.7) | |
| Mental comorbid conditions, yes | 41 (4.7) | |
| Employment, yes | 316 (36.2) | |
| Alcohol use | ||
| Non-drinker | 382 (43.6) | |
| Past drinker | 218 (24.9) | |
| Current drinker | 277 (31.6) | |
| Smoking | ||
| Non-smoker | 516 (58.8) | |
| Past smoker | 281 (32.0) | |
| Current smoker | 80 (9.1) | |
| Education | ||
| No education | 67 (7.7) | |
| ≤ Elementary school | 216 (24.9) | |
| ≤ Middle school | 133 (15.3) | |
| ≤ High school | 243 (28.0) | |
| ≤ University | 172 (19.8) | |
| ≥ Post-graduation school | 38 (4.4) | |
| CHADS2 score | 1.85 (0.9) | |
| CHADS2 score ≥ 2 | 491 (56.0) | |
| CHA2DS2-VASc score | 2.94 (1.4) | |
| CHA2DS2-VASc score ≥ 2 | 733 (83.6) | |
| HAS-BLED score | 1.48 (0.7) | |
| HAS-BLED score ≥ 3 | 54 (7.7) | |
Data are presented as mean (standard deviation) or number (%).
BMI = body mass index, NVAF = non-valvular atrial fibrillation.
aUnknown: 149 cases.
Anticoagulation quality
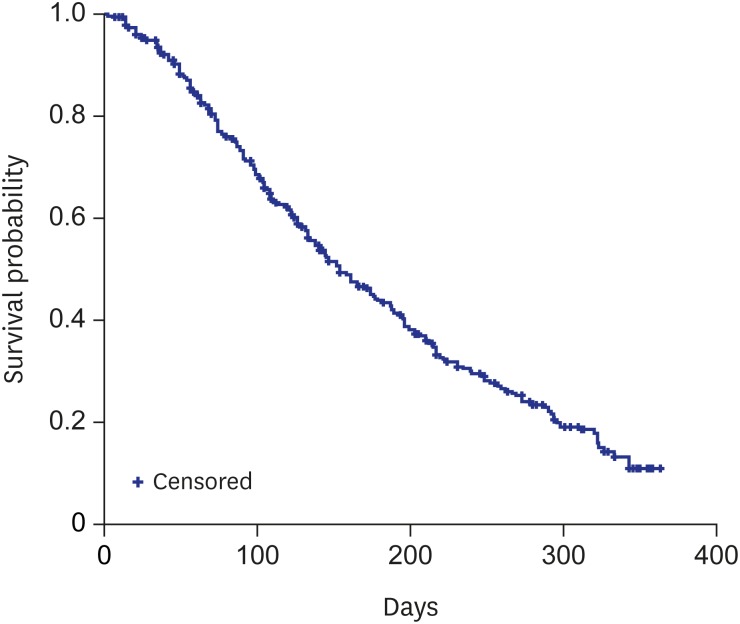
During the follow-up period, among 852 patients whose INR was measured more than once, the cases in which VKA was discontinued accounted for 18.5%. Among the patients to which VKA was discontinued, 60.1% were changed to antiplatelets, and the medicine was changed to non-vitamin K antagonist oral anticoagulants (NOAC) in 37.3% among them. The number of patients who had a well-controlled INR were 226 (26.5%) (Table 2). Also, 335 patients newly started taking VKA and 215 among them maintained the optimal dose twice in a row during the follow-up period. The median time to reach the optimal dose twice consecutively was 154 days (95% confidence interval [CI], 133–179 days) (Fig. 1).
Table 2. VKA treatment and INR level of the patients who had INR measurement ≥ 1 during their follow up period.
| Treatment/level | Value (n = 852) | |
|---|---|---|
| VKA treatment | ||
| Continuation | 635 (74.5) | |
| Switching to other drugs | 158 (18.5) | |
| Switching to aspirin | 59 (37.3) | |
| Switching to clopidogrel | 21 (13.3) | |
| Switching to aspirin + clopidogrel | 15 (9.5) | |
| Switching to NOAC | 59 (37.3) | |
| Switching to others | 4 (2.5) | |
| No switching | 59 (6.9) | |
| INR level, at baseline | 1.89 ± 0.96 | |
| INR level, during follow-up | 1.97 ± 0.64 | |
| No. of INR measurements during follow-up | 5.98 ± 3.29 | |
| Patients with TTR ≥ 60 | 226 (26.5) | |
Data are presented as mean (standard deviation) or number (%).
VKA = vitamin K antagonist, INR = international normalized ratio, NOAC = non-vitamin K antagonist oral anticoagulants, TTR = time in therapeutic range.
Fig. 1. Kaplan-Meier curve of time to optimal dose for VKA treatment with two-consecutive dose maintaining.
VKA = vitamin K antagonist, CI = confidence interval.
The CHA2DS2-VASc score was higher in the group that had a well-controlled INR than in the group that had a poorly controlled INR (3.2 vs. 2.9, P < 0.001). Patients in the group that had a poorly controlled INR were younger than the group that had a well-controlled INR (66 vs. 72 years, P < 0.001) and had a higher HAS-BLED score (1.5 vs. 1.4, P = 0.03) (Table 3).
Table 3. Factors related with INR control (n = 852).
| Characteristics | WC | PC | P value | |
|---|---|---|---|---|
| Sex, male | 131 (58.0) | 381 (60.9) | 0.4457a | |
| Age, yr | 71.77 (7.78) | 66.20 (10.42) | < 0.0001b | |
| BMI | 24.69 (3.32) | 24.87 (3.29) | 0.5242b | |
| NVAF duration, mon | 21.03 (40.42) | 17.44 (31.59) | 0.8384c | |
| Type of NVAF | 0.8887a | |||
| First diagnosed | 27 (12.0) | 65 (10.4) | ||
| Paroxysmal | 68 (30.1) | 195 (31.2) | ||
| Persistent | 85 (37.6) | 250 (39.9) | ||
| Long-standing persistent | 13 (5.8) | 30 (4.8) | ||
| Permanent | 24 (10.6) | 56 (9.0) | ||
| Unknown | 9 (4.0) | 30 (4.8) | ||
| Mental co-morbid conditions, yes | 14 (6.2) | 25 (4.0) | 0.1747a | |
| Employment, yes | 56 (24.9) | 247 (39.7) | < 0.0001a | |
| Alcohol use | 0.0775a | |||
| Non-drinker | 111 (49.1) | 256 (40.9) | ||
| Past drinker | 55 (24.3) | 162 (25.9) | ||
| Current drinker | 60 (26.6) | 208 (33.2) | ||
| Smoking | 0.0577a | |||
| Non-smoker | 140 (62.0) | 356 (56.9) | ||
| Past smoker | 74 (32.7) | 204 (32.6) | ||
| Current smoker | 12 (5.3) | 66 (10.5) | ||
| Education | 0.9384a | |||
| No education | 18 (8.0) | 48 (7.8) | ||
| ≤ Elementary school | 52 (23.1) | 157 (25.4) | ||
| ≤ Middle school | 34 (15.1) | 94 (15.2) | ||
| ≤ High school | 62 (27.6) | 173 (28.0) | ||
| ≤ University | 47 (20.9) | 123 (19.9) | ||
| ≥ Post-graduation school | 12 (5.3) | 24 (3.9) | ||
| CHADS2 score | 1.92 (0.89) | 1.83 (0.97) | 0.0637c | |
| CHA2DS2-VASc score | 3.21 (1.21) | 2.85 (1.43) | 0.0002b | |
| HAS-BLED score | 1.41 (0.63) | 1.52 (0.66) | 0.0292c | |
| VKA dosage, mg/day | 19.51 (7.61) | 19.36 (9.84) | 0.8190b | |
| VKA treatment | 0.0003a | |||
| Continue | 189 (83.6) | 446 (71.3) | ||
| Discontinued & switching | 22 (9.7) | 446 (71.3) | ||
| Discontinued & no switching | 15 (6.6) | 44 (7.0) | ||
Data are presented as mean (standard deviation) or number (%).
INR = international normalized ratio, WC = well-controlled, PC = poor-controlled, BMI = body mass index, NVAF = non-valvular atrial fibrillation, VKA = vitamin K antagonist.
aP value calculated by χ2 test; bP value calculated by Student's t-test; cP value calculated by Mann-Whitney's U test.
Treatment satisfaction
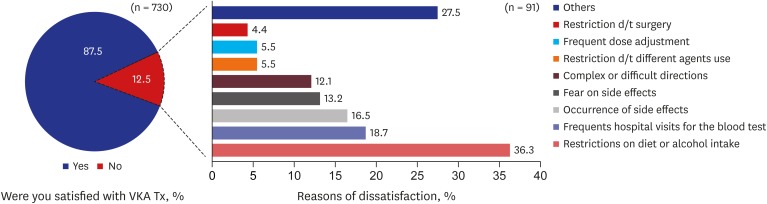
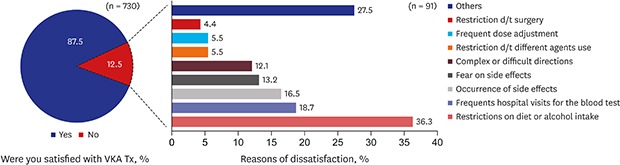
The patients' satisfaction with VKA treatment was investigated with a total of 730 patients (mean age, 67.9 years; males, 59.0%), and the mean of each domain of the TSQM was as follows: effectiveness (57.9 ± 12.0), side effects (96.3 ± 11.6), convenience (64.0 ± 13.5), and global satisfaction (55.6 ± 14.5) (Table 4). According to the simple questionnaire on treatment satisfaction, 91 patients (12.5%) replied that they were not satisfied with VKA treatment. The main reasons for dissatisfaction were restrictions on diet or alcohol intake (36.3%), frequent hospital visits for blood tests (18.7%), and side effects such as bleeding or bruising (16.5%) (Fig. 2).
Table 4. TSQM subscale scores (n = 730).
| TSQM score | Effectiveness | Side effects | Convenience | Global satisfaction |
|---|---|---|---|---|
| Mean (SD) | 57.9 (12.0) | 96.3 (11.6) | 64.0 (13.5) | 55.6 (14.5) |
| Median (Min, Max) | 55.6 (16.7, 100) | 100 (0, 100) | 66.7 (16.7, 100) | 57.1 (7.1, 100) |
TSQM = treatment satisfaction questionnaire for medication, SD = standard deviation.
Fig. 2. Dissatisfaction with the VKA use.
VKA = vitamin K antagonist.
In multivariable linear regression analysis based on the univariate results and clinically selected variables, the associations with lower effectiveness score and global satisfaction score were shown in long standing persistent AF compared to that of first diagnosed AF (β = −5.6, P < 0.05; β = −6.8, P < 0.05). In addition, the presence of a comorbid mental condition compared to none was associated with lower effectiveness score (β = −4.5, P < 0.05). The higher convenience score was related to the higher VKAs dose (β = 1.7, P < 0.01), and high level education of at least post-graduation school compared to no education (β = 7.4, P < 0.05). Side-effect score was not related to any of the factors (Table 5).
Table 5. Multivariable linear regression analysis for TSQM scoresa.
| Characteristics | Effectiveness | Side effects | Convenience | Global satisfaction | |||||
|---|---|---|---|---|---|---|---|---|---|
| β | Pb | β | Pb | β | Pb | β | Pb | ||
| Sex, male | 0.07 | 0.95 | −0.48 | 0.69 | 0.93 | 0.62 | 0.08 | 0.95 | |
| Age, yr | 0.03 | 0.60 | −0.01 | 0.85 | 0.09 | 0.31 | 0.02 | 0.79 | |
| BMI | −0.09 | 0.65 | |||||||
| Type of NVAF | |||||||||
| Paroxysmal | 1.72 | 0.29 | 2.21 | 0.16 | −0.24 | 0.90 | |||
| Persistent | 0.69 | 0.66 | 2.83 | 0.06 | 1.65 | 0.38 | |||
| Long-standing persistent | −5.56 | 0.02 | −0.72 | 0.76 | −6.77 | 0.02 | |||
| Permanent | 2.00 | 0.32 | 0.262 | 0.90 | 1.43 | 0.56 | |||
| Unknown | −2.29 | 0.36 | −2.19 | 0.36 | −3.88 | 0.20 | |||
| Mental co-morbid conditions, yes | −4.48 | 0.04 | |||||||
| Alcohol use | |||||||||
| Past drinker | −0.80 | 0.50 | |||||||
| Current drinker | 2.15 | 0.06 | |||||||
| Smoking | |||||||||
| Past smoker | 2.92 | 0.08 | |||||||
| Current smoker | 1.46 | 0.57 | |||||||
| Education | |||||||||
| ≤ Elementary school | −2.48 | 0.16 | 1.68 | 0.32 | 0.09 | 0.97 | −0.22 | 0.92 | |
| ≤ Middle school | 0.16 | 0.94 | 1.18 | 0.53 | 3.02 | 0.24 | 1.96 | 0.41 | |
| ≤ High school | −0.71 | 0.70 | 3.29 | 0.07 | −1.35 | 0.57 | −1.56 | 0.49 | |
| ≤ University | −1.86 | 0.36 | −1.04 | 0.59 | 1.39 | 0.59 | −3.06 | 0.21 | |
| ≥ Post-graduation school | 0.95 | 0.73 | 3.71 | 0.16 | 7.45 | 0.04 | 1.37 | 0.68 | |
| CHA2DS2-VASc Score | 0.11 | 0.81 | 0.07 | 0.87 | 0.13 | 0.84 | 0.01 | 0.99 | |
| HAS-BLED Score | 1.58 | 0.12 | |||||||
| VKA dosage, mg/day | 1.71 | < 0.01 | |||||||
| Well controlled INR | −0.66 | 0.63 | |||||||
| VKA Tx. | |||||||||
| Continue | 1.50 | 0.46 | 2.66 | 0.30 | |||||
| Discontinue & switching to other antithrombotics | −2.55 | 0.26 | 0.20 | 0.94 | |||||
TSQM = treatment satisfaction questionnaire for medication, BMI = body mass index, NVAF = non-valvular atrial fibrillation, VKA = vitamin K antagonist, INR = international normalized ratio.
aAdjusted variables were selected from univariate results (P < 0.1) and other clinically selected variables by physicians; bP value calculated by multiple linear regression analysis. Reference category: sex (female), type of NVAF (first diagnosed), mental co-morbid conditions (No), alcohol use (non-drinker), smoking (non-smoker), education (no education), VKA treatment (discontinue & no switching to other antithrombotics), INR (poor controlled).
DISCUSSION
The results of this study showed that the elderly and males comprised high proportions of non-valvular AF patients, the same as the study previously conducted on Korean patients with AF.1 The ratio of high-risk patients with a mean CHA2DS2-VASc score of 2 or higher was 83.6%, which was comparable to the fraction (85.4%) in the pre-direct oral anticoagulant period (January 2011 to July 2013) in the previous study.16 On the other hand, the percentage of high-risk patients with a HAS-BLED score of 3 or higher was 7.7%, which was somewhat lower than the percentage (32.3%) in the previous study.16
During the follow-up observation period, the percentage of patients that had well-controlled INR was 26.5%, which was within the 16.7% (Asia)–49.4% (Europe) range in the GARFIELD-AF study,17 a worldwide observational prospective study. The INR was especially poorly controlled in Asia compared to other regions, which is interpreted as being due to the characteristics of AF patients in Asia who have lower INR values than patients in other regions.18
The reason why the CHA2DS2-VASc score was higher in the group where the INR was more well-controlled than the group that was not might be because the doctors paid more attention to INR control for the people to whom a stroke could cause more harm.19 The group where the INR was well-controlled had a higher HAS-BLED score, but the difference was not clinically significant. In addition, the reason why INR is better controlled in the elderly is perhaps because the doctors prescribed medicine more carefully, since the elderly group was reported to be the group with a high risk of having a stroke.1
Patients' satisfaction with VKA treatment was low overall in all domains except for side effects. In particular, comparing the global satisfaction score to the score of patients with other diseases (hypertension [72.1],20 epilepsy [68.4],21 and coronary heart disease [69.2]22) measured by TSQM, the measurement tool like ours, it showed a much lower satisfaction level. The reasons why the patients who replied to the simple question of satisfaction with the treatment that they were not satisfied were restrictions on diet or alcohol intake,23,24,25,26,27 frequent hospital visits for blood tests28,29 and occurrence of bleeding,30,31,32 which were the same as those reported in previous studies.
The long duration of AF was a variable related to the low effectiveness of VKA treatment and overall satisfaction, and patients with co-morbid mental conditions showed low effectiveness of treatment. The higher the education level was and the higher the VKA prescription dosage was, the higher the convenience of VKA administration became. According to A PREFER in the AF Registry sub-study,33 the patients who switched to NOAC from VKA showed lower incidence rates of hypertension and heart valve dysfunction, fewer cases of combined therapy with antiplatelet/anti-inflammatory agents, and lower CHA2DS2-VASc scores. As shown in these results, it is likely that patients who had AF for a long time and were taking VKA had a more sensitive response to the effectiveness of treatment because the treatment effectiveness of VKA was lower than that of NOAC. In addition, there were many cases in which patients who had low anxiety/depressive traits expressed dissatisfaction with VKA and switched to another medicine.33
The limitations of this study are as follows: First, the participants in this study were patients who took part in it voluntarily, and the data was gathered at the time of their visit to the hospital as outpatients during the one-year follow-up period. Thus, the time of visit was different for each patient during the follow-up period. Second, unmeasured variables in this study were not considered as the potential confounders.
In spite of these limitations, in the real-world practice of Korea, INR was poorly controlled in patients. The principal reasons for dissatisfaction about VKA therapy were dietary restrictions, and regular monitoring etc. The global satisfaction score was lower among VKA users with NVAF than those of previous studies on treatment satisfaction in other diseases. Alternative oral anticoagulant therapy should be considered for patients with NVAF for enhancing treatment satisfaction and doing INR control well.
ACKNOWLEDGMENTS
This study was sponsored by BMS/Pfizer Pharmaceuticals Korea Ltd. This funding was provided from 2013 to 2016. The Authors, Seo BJ, Kim YJ, and Kang SS, who are employees of Pfizer contributed in the study design, data analysis, decision to publish, or preparation of the manuscript.
Footnotes
Funding: This research was sponsored by BMS/Pfizer Pharmaceuticals Korea Ltd.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Kim YJ, Kang SS, Kim YH.
- Data curation: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Kim YH.
- Formal analysis: Lee J.
- Investigation: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Seo BJ, Kim YJ, Kang SS, Kim YH.
- Methodology: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Seo BJ, Kim YJ, Kang SS, Lee J, Kim YH.
- Project administration: Seo BJ.
- Software: Lee J.
- Supervision: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Seo BJ, Kim YJ, Kang SS, Kim YH.
- Validation: Oh S, Kim JS, Oh YS, Shin DG, Park HN, Hwang GS, Choi KJ, Kim JB, Lee MY, Park HW, Kim DK, Jin ES, Park J, Oh IY, Shin DH, Park HS, Kim JH, Kim NH, Ahn MS, Seo BJ, Kim YJ, Kang SS, Lee J, Kim YH.
- Visualization: Lee J.
- Writing - original draft: Oh S, Seo BJ.
- Writing - review & editing: Oh S, Seo BJ, Kim YJ, Kang SS, Lee J, Kim YH.
References
- 1.Jeong JH. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J Korean Med Sci. 2005;20(1):26–30. doi: 10.3346/jkms.2005.20.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marinigh R, Lip GY, Fiotti N, Giansante C, Lane DA. Age as a risk factor for stroke in atrial fibrillation patients: implications for thromboprophylaxis. J Am Coll Cardiol. 2010;56(11):827–837. doi: 10.1016/j.jacc.2010.05.028. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 4.Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, Hsu CY, et al. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999;30(4):724–728. doi: 10.1161/01.str.30.4.724. [DOI] [PubMed] [Google Scholar]
- 5.Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology. 2003;22(2):118–123. doi: 10.1159/000068743. [DOI] [PubMed] [Google Scholar]
- 6.Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P, et al. Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ. 2008;336(7640):376–379. doi: 10.1136/bmj.39456.688333.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 8.Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010;123(7):638–645.e4. doi: 10.1016/j.amjmed.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 9.Lip GY, Agnelli G, Thach AA, Knight E, Rost D, Tangelder MJ. Oral anticoagulation in atrial fibrillation: A pan-European patient survey. Eur J Intern Med. 2007;18(3):202–208. doi: 10.1016/j.ejim.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Shin HW, Kim YN, Bae HJ, Lee HM, Cho HO, Cho YK, et al. Trends in oral anticoagulation therapy among Korean patients with atrial fibrillation: the Korean atrial fibrillation investigation. Korean Circ J. 2012;42(2):113–117. doi: 10.4070/kcj.2012.42.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witt DM, Delate T, Clark NP, Martell C, Tran T, Crowther MA, et al. Outcomes and predictors of very stable INR control during chronic anticoagulation therapy. Blood. 2009;114(5):952–956. doi: 10.1182/blood-2009-02-207928. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds MR, Shah J, Essebag V, Olshansky B, Friedman PA, Hadjis T, et al. Patterns and predictors of warfarin use in patients with new-onset atrial fibrillation from the FRACTAL Registry. Am J Cardiol. 2006;97(4):538–543. doi: 10.1016/j.amjcard.2005.09.086. [DOI] [PubMed] [Google Scholar]
- 13.NCSS. 2008. NCSS, LLC; [Updated 2012]. [Accessed December 10, 2012]. https://www.ncss.com/ [Google Scholar]
- 14.Fleiss JL, Levin B, Paik MC. An introduction to applied probability. In: Shewart WA, Wilks SS, editors. Statistical Methods for Rates and Proportions. Hoboken, NJ: John Wiley & Sons, Inc.; 2004. pp. 17–49. [Google Scholar]
- 15.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17(8):857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 16.Admassie E, Chalmers L, Bereznicki LR. Changes in oral anticoagulant prescribing for stroke prevention in patients with atrial fibrillation. Am J Cardiol. 2017;120(7):1133–1138. doi: 10.1016/j.amjcard.2017.06.055. [DOI] [PubMed] [Google Scholar]
- 17.Haas S, Ten Cate H, Accetta G, Angchaisuksiri P, Bassand JP, Camm AJ, et al. Quality of vitamin K antagonist control and 1-year outcomes in patients with atrial fibrillation: a global perspective from the GARFIELD-AF registry. PLoS One. 2016;11(10):e0164076. doi: 10.1371/journal.pone.0164076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh S, Goto S, Accetta G, Angchaisuksiri P, Camm AJ, Cools F, et al. Vitamin K antagonist control in patients with atrial fibrillation in Asia compared with other regions of the world: real-world data from the GARFIELD-AF registry. Int J Cardiol. 2016;223:543–547. doi: 10.1016/j.ijcard.2016.08.236. [DOI] [PubMed] [Google Scholar]
- 19.Kim TH, Yang PS, Kim D, Yu HT, Uhm JS, Kim JY, et al. CHA2DS2-VASc score for identifying truly low-risk atrial fibrillation for stroke: a Korean nationwide cohort study. Stroke. 2017;48(11):2984–2990. doi: 10.1161/STROKEAHA.117.018551. [DOI] [PubMed] [Google Scholar]
- 20.Al-Jabi SW, Zyoud SH, Sweileh WM, Wildali AH, Saleem HM, Aysa HA, et al. Relationship of treatment satisfaction to health-related quality of life: findings from a cross-sectional survey among hypertensive patients in Palestine. Health Expect. 2015;18(6):3336–3348. doi: 10.1111/hex.12324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sweileh WM, Ihbesheh MS, Jarar IS, Taha AS, Sawalha AF, Zyoud SH, et al. Self-reported medication adherence and treatment satisfaction in patients with epilepsy. Epilepsy Behav. 2011;21(3):301–305. doi: 10.1016/j.yebeh.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Liberato AC, Rodrigues RC, São-João TM, Alexandre NM, Gallani MC. Satisfaction with medication in coronary disease treatment: psychometrics of the treatment satisfaction questionnaire for medication. Rev Lat Am Enfermagem. 2016;24:e2705. doi: 10.1590/1518-8345.0745.2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kakkar AK, Mueller I, Bassand JP, Fitzmaurice DA, Goldhaber SZ, Goto S, et al. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS One. 2013;8(5):e63479. doi: 10.1371/journal.pone.0063479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tulner LR, Van Campen JP, Kuper IM, Gijsen GJ, Koks CH, Mac Gillavry MR, et al. Reasons for undertreatment with oral anticoagulants in frail geriatric outpatients with atrial fibrillation: a prospective, descriptive study. Drugs Aging. 2010;27(1):39–50. doi: 10.2165/11319540-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000;160(1):41–46. doi: 10.1001/archinte.160.1.41. [DOI] [PubMed] [Google Scholar]
- 26.Sudlow M, Thomson R, Thwaites B, Rodgers H, Kenny RA. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet. 1998;352(9135):1167–1171. doi: 10.1016/S0140-6736(98)01401-9. [DOI] [PubMed] [Google Scholar]
- 27.Lip GY, Golding DJ, Nazir M, Beevers DG, Child DL, Fletcher RI. A survey of atrial fibrillation in general practice: the West Birmingham Atrial Fibrillation Project. Br J Gen Pract. 1997;47(418):285–289. [PMC free article] [PubMed] [Google Scholar]
- 28.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–2962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 29.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071–2104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 30.Bajorek BV, Ogle SJ, Duguid MJ, Shenfield GM, Krass I. Balancing risk versus benefit: the elderly patient's perspective on warfarin therapy. Pharm Pract (Granada) 2009;7(2):113–123. doi: 10.4321/s1886-36552009000200008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wild D, Murray M, Donatti C. Patient perspectives on taking vitamin K antagonists: a qualitative study in the UK, USA and Spain. Expert Rev Pharmacoecon Outcomes Res. 2009;9(5):467–474. doi: 10.1586/erp.09.48. [DOI] [PubMed] [Google Scholar]
- 32.Dantas GC, Thompson BV, Manson JA, Tracy CS, Upshur RE. Patients' perspectives on taking warfarin: qualitative study in family practice. BMC Fam Pract. 2004;5(1):15. doi: 10.1186/1471-2296-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Caterina R, Bruggenjurgen B, Darius H, Kohler S, Lucerna M, Pecen L, et al. Quality of life and patient satisfaction in patients with atrial fibrillation on stable vitamin K antagonist treatment or switched to a non-vitamin K antagonist oral anticoagulant during a 1-year follow-up: a PREFER in AF registry substudy. Arch Cardiovasc Dis. 2018;111(2):74–84. doi: 10.1016/j.acvd.2017.04.007. [DOI] [PubMed] [Google Scholar]