Abstract
A snapping biceps tendon is an infrequently seen and commonly misdiagnosed pathology, leaving patients with persistent symptoms that can be debilitating. Patients will present with a visible, audible, and/or painful snap over the lateral aspect of their knee when performing squats, sitting in low seats, or participating in activities with deep knee flexion. A thorough knowledge of the anatomy is essential for surgical treatment of this pathology, which is caused by a detachment of the direct arms of the long and short heads of the biceps femoris off the fibular styloid. This Technical Note provides a diagnostic approach, postoperative management, and details of a surgical technique to treat a snapping biceps tendon with an anatomic repair of the long and short head attachments of the biceps femoris to the posterolateral fibular styloid.
Although snapping biceps femoris syndrome constitutes an uncommon cause of lateral knee pain or discomfort, it can be a debilitating and vexing condition. There is a limited body of literature regarding its anatomy, genesis, and potential treatment algorithm. This makes it a challenging condition to address, with several reported techniques including anatomic repair and reconstruction, with sometimes unpredictable results.1, 2, 3, 4, 5, 6, 7
The main components of the long head of the biceps muscle include a direct arm, a reflected arm, an anterior arm, and a lateral and anterior aponeurosis. The main components of the short head of the biceps femoris muscle are a proximal attachment to the long head's tendon, a capsular arm, a confluence of the biceps and the capsulo-osseous layer of the iliotibial tract, a direct arm, an anterior arm, and a lateral aponeurosis.7 This may explain the important role of the biceps femoris tendon in adding dynamic stability to the posterolateral corner by means of its numerous attachment sites.4, 5, 7, 8 The purpose of this Technical Note is to describe and show our indications, diagnosis, and preferred technique for the treatment of snapping biceps syndrome, highlighting important pearls and pitfalls to avoid complications and achieve successful results.
Objective Diagnosis and Indications for Surgery
When providing their history, patients with a snapping biceps will typically report a visible, audible, and/or painful snap over the lateral aspect of their knee when performing squats, sitting in low seats, or participating in activities that involve deep knee flexion that similarly presents when rising from a deep knee-flexed position. Patients will often report no specific history of knee trauma.
On examination, a thorough lower-extremity assessment is performed including palpation, range of motion, stability testing, patellofemoral examination, strength and neurovascular assessment, and gait evaluation. Patients with snapping biceps may present with pain to palpation over the fibular collateral ligament–biceps bursa,9 as well as the lateral aspect of the fibular styloid, or dysesthesia of the common peroneal nerve (CPN). When the patient is asked to perform a deep squat, the common biceps femoris tendon will visibly subluxate over the lateral aspect of the fibular head. Typically, when the common biceps tendon is held reduced by applying manual pressure where it crosses the fibular head, subluxation of the tendon—and the pain associated with the subluxation—can be minimized or prevented, which helps to verify the diagnosis.
In addition to a thorough history and examination, standard weight-bearing radiographs and an magnetic resonance imaging (MRI) scan are obtained. Plain radiographs usually show normal findings, and this pathology has not been reported to occur with other posterolateral knee injuries, so varus stress radiographs are usually not indicated. MRI is indicated to evaluate other possible concurrent knee pathology to explain a patient's symptoms, with particular attention paid to the posterolateral knee structures. In the setting of a snapping biceps, the MRI scan will often show thickening of the long head of the biceps femoris tendon with concurrent detachments or tears of the direct arms of the long and short heads of the biceps femoris off their fibular styloid attachments. However, it is also possible that the MRI scan will yield minimal information and the diagnosis will be made based on only the history and physical examination findings. An open anatomic repair of the biceps femoris long and short head attachments to the fibular styloid is indicated in patients in whom conservative measures have failed and who have persistent symptoms that limit their activities and quality of life.
Surgical Technique
Patient Positioning
The patient is positioned supine on the operating table, and an examination under anesthesia is performed to confirm the diagnosis. The surgical limb is then placed in a leg holder (Mizuho OSI, Union City, CA), and the nonsurgical limb is placed in an abduction stirrup (Birkova Products, Gothenburg, NE). A well-padded tourniquet is placed on the upper thigh of the operative leg, which is then prepared and draped in a standard fashion (Video 1).
Surgical Approach
A surgical approach to the biceps femoris is performed first. A lateral hockey-stick skin incision is made along the iliotibial band and extended distally, halfway between the fibular head and Gerdy tubercle (Fig 1). The subcutaneous tissue is dissected, and a posteriorly based skin flap is developed to preserve the vascular support to the superficial tissues.
Fig 1.

Lateral view of surgical positioning for a left knee placed in a leg holder (Mizuho OSI) with standard surgical draping. The posterolateral corner approach is begun with a lateral hockey-stick incision.
The long and short heads of the biceps femoris are exposed. CPN neurolysis is then performed. The nerve is typically located posteromedially to the long head of the biceps femoris and should be dissected up to 6 cm proximally (Fig 2). Distally, 5 to 7 mm of peroneus longus fascia is incised over the CPN to prevent nerve irritation or a foot drop due to postoperative swelling. The biceps femoris attachment on the fibular styloid is then exposed by elevating posteriorly under the biceps attachment on the fibular styloid. There is usually a bursa at this location, which forms owing to the subluxation of the biceps tendon over time. It has previously been reported that the long and short heads of the biceps femoris are torn from their fibular attachments in all cases of snapping biceps.10 In addition, the tension of the common biceps tendon and its ability to subluxate over the posterolateral fibular styloid and fibular head are evaluated intraoperatively.
Fig 2.
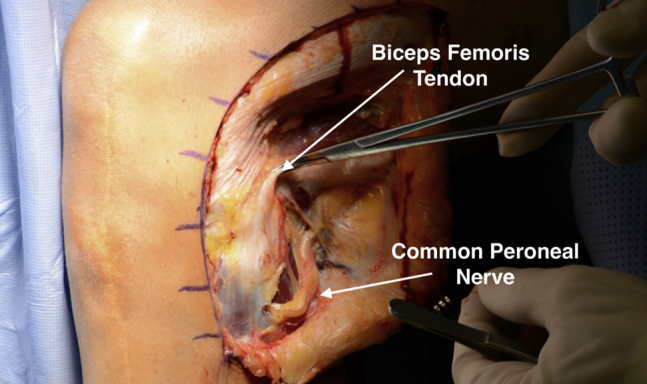
The common peroneal nerve is directly visualized and isolated from the tissue of the biceps femoris tendon, typically located posteromedially to the long head of the biceps femoris (lateral view, left knee). To prevent nerve irritation or a foot drop due to postoperative swelling, Common peroneal nerve neurolysis with a length of 5 to 7 mm, including the peroneus longus fascia, is performed.
The normal anatomic sites for insertion of the direct arms of the short and long heads of the biceps are identified and cleared of soft tissue in preparation for tendon reattachment. From the apex of the posterolateral fibular styloid down to the lateral aspect of the fibular head, a small rongeur is used to expose the subcortical bone (Fig 3). Two to three (depending on the need for further restoration of the anatomic attachment site) Mitek Super anchors (DePuy Synthes, West Chester, PA) are then placed onto the posterolateral aspect of the fibular styloid (Fig 4), and the short and long heads of the biceps are each repaired back separately to the posterolateral aspect of the fibular styloid (Fig 5). After completion of arthroscopy, the snapping biceps repair sutures are tied with the knee in full extension. The biceps femoris should then be assessed for proper restoration of its anatomic position.
Fig 3.
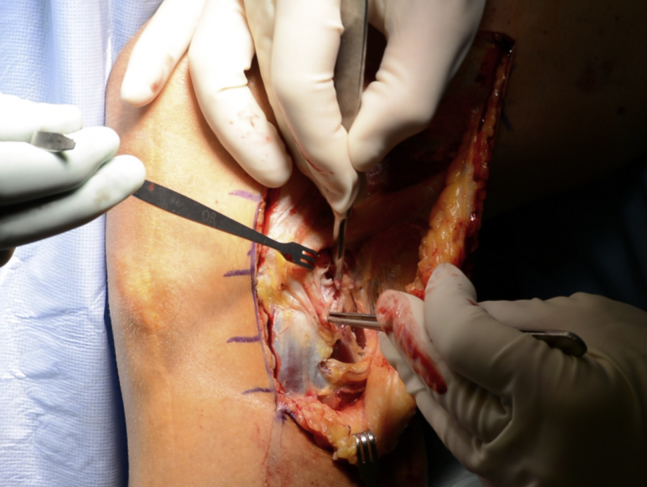
As shown on the lateral view of a left knee, from the apex of the posterolateral fibular styloid down to the lateral aspect of the fibular head, a small rongeur and scalpel are used to expose the anatomic attachment sites for insertion of the direct arms of the long and short heads of the biceps femoris tendon in preparation for drilling the suture anchors.
Fig 4.
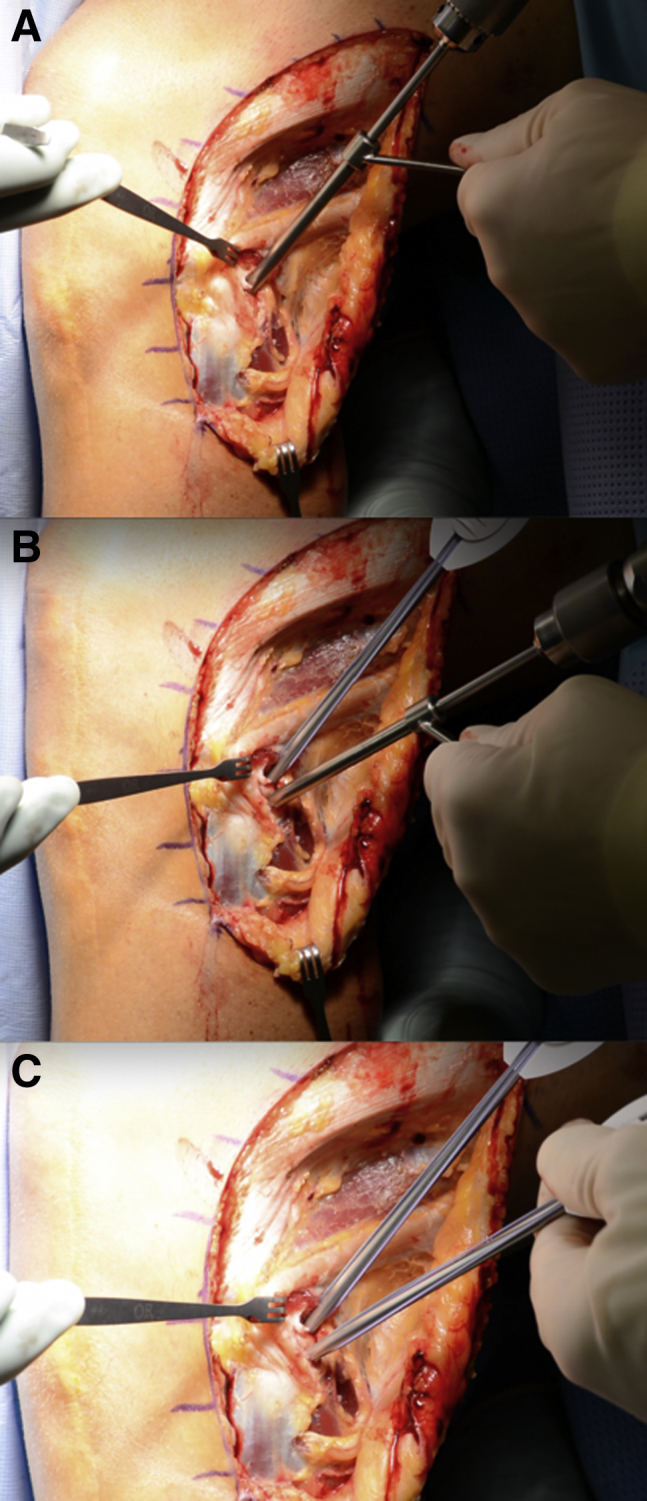
(A, B) As shown on the lateral view of a left knee, the direct arm attachments of the long and short heads of the biceps femoris tendon are positioned onto the posterolateral aspect of the fibular styloid, and 2 bone sockets are drilled with a 2.7-mm-diameter drill. (C) Two Mitek Super anchors are placed into the bone sockets; an additional anchor may be used if stabilization is not sufficient after repair of the biceps down to the fibular styloid.
Fig 5.
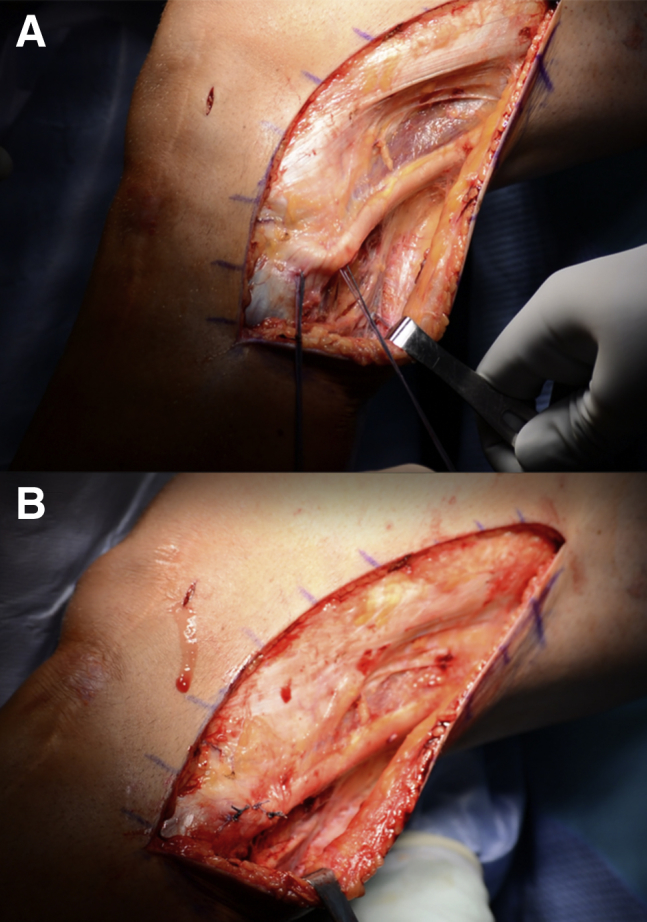
(A) As shown on the lateral view of a left knee, the sutures placed into the posterolateral aspect of the fibular styloid are passed into their respective portions of the long and short heads of the biceps femoris tendon. (B) The short and long heads of the biceps are each repaired back separately to the posterolateral aspect of the fibular styloid, with the sutures tied with the knee in full extension, and the repair is reinforced with a No. 0 Vicryl suture.
After irrigation of the tissues, the repair can be reinforced with a No. 0 Vicryl suture (Ethicon, Somerville, NJ). The superficial layers are closed in a regular fashion using interrupted subcutaneous skin sutures in the deep dermal layer using No. 2 Vicryl (Ethicon). The skin is closed with No. 4-0 Monocryl (Ethicon) in a running subcuticular stitch. The pearls and pitfalls of this technique are summarized in Table 1, and the advantages and disadvantages are reported in Table 2.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Identify the common peroneal nerve first and perform neurolysis. | Injury to the common peroneal nerve can occur owing to scarring and displacement of the nerve. |
| Tension the repair with the knee in full extension to replicate the normal anatomic and biomechanical characteristics of the biceps femoris muscle. | Over-tensioning of the biceps femoris repair can occur by tying the repair sutures with the knee flexed. |
| Ensure that the suture anchors are angled correctly into the fibular styloid to achieve the best pullout strength. | Potential misplacement of the suture anchors can occur owing to the lack of surface area of the fibular head. |
| Instruct the patient to avoid isolated hamstring curls and resistive exercises for 4 mo. | Failure to protect the repair can occur with an inappropriate rehabilitation protocol. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Technically straightforward surgical procedure | Nonanatomic repair may lead to failed surgery |
| Versatility with amount of tension during repair fixation of biceps femoris | Concurrent peroneal nerve neurolysis is required for exposure |
| No prominent hardware | |
| Ability to directly visualize common peroneal nerve |
Rehabilitation Protocol
The operative lower extremity is placed in a knee immobilizer in full extension. Patients are limited to no weight bearing for 6 weeks with no active knee flexion during this time. Passive knee range of motion is limited to 0° to 90° of flexion for the first 2 weeks; then, the patient is allowed to progress his or her motion as tolerated. Crutch weaning begins at 6 weeks postoperatively, and crutch use may be discontinued once the patient can ambulate without a limp. At 6 weeks, the patient can begin using a stationary bike, and no brace is required at this time. Isolated hamstring curls and resistive hamstring exercises are avoided for the first 4 months postoperatively to prevent the biceps femoris from avulsing off the fibular head. A return to full activities and sports is allowed after completion of a functional sports test around 5 to 6 months postoperatively.
Discussion
Because of the rarity of snapping biceps syndrome, this condition can commonly be missed or confused for other, more common lateral knee pathology. A thorough patient history and physical examination focusing on the location of the pain and a visible and/or audible snapping over the lateral knee, especially during deep flexion activities, are important to making the diagnosis. Snapping biceps femoris tendons may be present bilaterally, but surgical treatment should focus on the most symptomatic knee.
Causes of snapping biceps femoris syndrome have been reported to include idiopathic, abnormal biceps femoris tendon insertions; abnormal fibular head morphology; or direct trauma to the biceps femoris tendon insertion sites.11, 12, 13, 14, 15 Authors have reported favorable results with surgical treatment of snapping biceps syndrome, although these studies are limited to case reports with short-term follow-up. Published surgical treatment options for snapping biceps syndrome include partial fibular head excision,16, 17, 18 partial release of the biceps femoris tendon,11 or relocation of the long head of the biceps femoris insertion.13
The biceps femoris is a fusiform muscle that contains 2 heads, long and short, with multiple attachment points on the posterolateral aspect of the knee. It functions to flex the knee and to laterally rotate the knee in flexion.19 Most commonly, the snapping tendon occurs when the fibular head is brought to a more anterolateral position with internal rotation of the tibia.17 When nonoperative management fails to relieve the patient's symptoms, we perform our preferred surgical technique for anatomic restoration of the long and short head attachments of the biceps femoris to the posterolateral fibular styloid. We have previously reported 1-year outcomes in 3 patients treated for snapping biceps syndrome with this technique, all with resolution of their symptoms and no reported complications.10
In conclusion, we recommend an open repair of the biceps femoris tendon to the posterolateral aspect of the fibular styloid in patients with snapping biceps femoris syndrome by use of the reproducible technique described in this article. We have described our physical examination pearls, operative technique, and postoperative rehabilitation protocol for comprehensive management of patients with snapping biceps syndrome. Although promising results have been reported using this technique, further research is needed on the long-term outcomes of surgical treatment of snapping biceps femoris syndrome.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. receives royalties from Ossur, Smith & Nephew, and Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned supine on the operating table. The surgical limb (left knee) is then placed in a leg holder. The surgical approach to the biceps femoris is performed first. A lateral hockey-stick skin incision is made along the posterior aspect of the iliotibial band and extended distally, halfway between the fibular head and Gerdy tubercle. The subcutaneous tissue is dissected, and a posteriorly based skin flap is developed to preserve the vascular support to the superficial tissues. The long and short heads of the biceps femoris at the knee are exposed. Common peroneal nerve neurolysis is then performed. The nerve is typically located posteromedially to the long head of the biceps femoris and should be dissected up to 6 cm proximally. Distally, 5 to 7 mm of the thicker portion of the peroneus longus fascia is incised over the common peroneal nerve to prevent nerve irritation or a foot drop due to postoperative swelling. The biceps femoris attachment on the fibular styloid is then exposed by elevating posteriorly under the biceps attachment on the fibular styloid. The normal anatomic sites for the insertion of the direct arms of the short and long heads of the biceps are identified and cleared of soft tissue in preparation for the biceps tendon reattachment. From the apex of the posterolateral fibular styloid down to the lateral aspect of the fibular head, a small rongeur is used to expose the subcortical bone. Two to three suture anchors are then placed into the posterolateral aspect of the fibular styloid, and the short and long heads of the biceps are each repaired back separately to the posterolateral aspect of the fibular styloid. This anatomic repair is performed with the sutures tied with the knee in full extension. After the sutures are tied, the biceps femoris should be checked for proper restoration of its anatomic position.
References
- 1.Date H., Hayakawa K., Nakagawa K., Yamada H. Snapping knee due to the biceps femoris tendon treated with repositioning of the anomalous tibial insertion. Knee Surg Sports Traumatol Arthrosc. 2012;20:1581–1583. doi: 10.1007/s00167-011-1778-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fritsch B.A., Mhaskar V. Anomalous biceps femoris tendon insertion leading to a snapping knee in a young male. Knee Surg Relat Res. 2017;29:144–149. doi: 10.5792/ksrr.15.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guillin R., Mendoza-Ruiz J.J., Moser T., Ropars M., Duvauferrier R., Cardinal E. Snapping biceps femoris tendon: A dynamic real-time sonographic evaluation. J Clin Ultrasound. 2010;38:435–437. doi: 10.1002/jcu.20728. [DOI] [PubMed] [Google Scholar]
- 4.Kissenberth M.J., Wilckens J.H. The snapping biceps femoris tendon. Am J Knee Surg. 2000;13:25–28. [PubMed] [Google Scholar]
- 5.Matar H.E., Farrar N.G. Snapping biceps femoris: Clinical demonstration and operative technique. Ann R Coll Surg Engl. 2018;100:e59–e61. doi: 10.1308/rcsann.2018.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saltzman B.M., Collins M.J., Arns T.A., Forsythe B. Unilateral snapping biceps femoris tendon with an anomalous insertion treated with anatomic repositioning and lengthening with a single suture anchor: A report of two cases. JBJS Case Connect. 2018;8:e13. doi: 10.2106/JBJS.CC.16.00251. [DOI] [PubMed] [Google Scholar]
- 7.Terry G.C., LaPrade R.F. The biceps femoris muscle complex at the knee. Its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med. 1996;24:2–8. doi: 10.1177/036354659602400102. [DOI] [PubMed] [Google Scholar]
- 8.Terry G.C., LaPrade R.F. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996;24:732–739. doi: 10.1177/036354659602400606. [DOI] [PubMed] [Google Scholar]
- 9.LaPrade R.F., Hamilton C.D. The fibular collateral ligament-biceps femoris bursa. An anatomic study. Am J Sports Med. 1997;25:439–443. doi: 10.1177/036354659702500404. [DOI] [PubMed] [Google Scholar]
- 10.Bernhardson A.S., LaPrade R.F. Snapping biceps femoris tendon treated with an anatomic repair. Knee Surg Sports Traumatol Arthrosc. 2010;18:1110–1112. doi: 10.1007/s00167-009-1018-3. [DOI] [PubMed] [Google Scholar]
- 11.Crow S.A., Quach T., McAllister D.R. Partial tendon release for treatment of a symptomatic snapping biceps femoris tendon: A case report. Sports Health. 2009;1:435–437. doi: 10.1177/1941738109338360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lokiec F., Velkes S., Schindler A., Pritsch M. The snapping biceps femoris syndrome. Clin Orthop Relat Res. 1992:205–206. [PubMed] [Google Scholar]
- 13.Hernandez J.A., Rius M., Noonan K.J. Snapping knee from anomalous biceps femoris tendon insertion: A case report. Iowa Orthop J. 1996;16:161–163. [PMC free article] [PubMed] [Google Scholar]
- 14.Bansal R., Taylor C., Pimpalnerkar A.L. Snapping knee: An unusual biceps femoris tendon injury. Knee. 2005;12:458–460. doi: 10.1016/j.knee.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Fung D.A., Frey S., Markbreiter L. Bilateral symptomatic snapping biceps femoris tendon due to fibular exostosis. J Knee Surg. 2008;21:55–57. doi: 10.1055/s-0030-1247793. [DOI] [PubMed] [Google Scholar]
- 16.Bagchi K., Grelsamer R.P. Partial fibular head resection for bilateral snapping biceps femoris tendon. Orthopedics. 2003;26:1147–1149. doi: 10.3928/0147-7447-20031101-17. [DOI] [PubMed] [Google Scholar]
- 17.Bach B.R., Jr., Minihane K. Subluxating biceps femoris tendon: An unusual case of lateral knee pain in a soccer athlete. A case report. Am J Sports Med. 2001;29:93–95. doi: 10.1177/03635465010290012101. [DOI] [PubMed] [Google Scholar]
- 18.Kristensen G., Nielsen K., Blyme P.J. Snapping knee from biceps femoris tendon. A case report. Acta Orthop Scand. 1989;60:621. doi: 10.3109/17453678909150135. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez A.R., II, Sugalski M.T., LaPrade R.F. Anatomy and biomechanics of the lateral side of the knee. Sports Med Arthrosc Rev. 2006;14:2–11. doi: 10.1097/00132585-200603000-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned supine on the operating table. The surgical limb (left knee) is then placed in a leg holder. The surgical approach to the biceps femoris is performed first. A lateral hockey-stick skin incision is made along the posterior aspect of the iliotibial band and extended distally, halfway between the fibular head and Gerdy tubercle. The subcutaneous tissue is dissected, and a posteriorly based skin flap is developed to preserve the vascular support to the superficial tissues. The long and short heads of the biceps femoris at the knee are exposed. Common peroneal nerve neurolysis is then performed. The nerve is typically located posteromedially to the long head of the biceps femoris and should be dissected up to 6 cm proximally. Distally, 5 to 7 mm of the thicker portion of the peroneus longus fascia is incised over the common peroneal nerve to prevent nerve irritation or a foot drop due to postoperative swelling. The biceps femoris attachment on the fibular styloid is then exposed by elevating posteriorly under the biceps attachment on the fibular styloid. The normal anatomic sites for the insertion of the direct arms of the short and long heads of the biceps are identified and cleared of soft tissue in preparation for the biceps tendon reattachment. From the apex of the posterolateral fibular styloid down to the lateral aspect of the fibular head, a small rongeur is used to expose the subcortical bone. Two to three suture anchors are then placed into the posterolateral aspect of the fibular styloid, and the short and long heads of the biceps are each repaired back separately to the posterolateral aspect of the fibular styloid. This anatomic repair is performed with the sutures tied with the knee in full extension. After the sutures are tied, the biceps femoris should be checked for proper restoration of its anatomic position.


