Abstract
Background:
Virtual reality (VR) experiences (through games and virtual environments) are increasingly being used in physical, cognitive, and psychological interventions. However, the impact of VR as an approach to rehabilitation is not fully understood, and its advantages over traditional rehabilitation techniques are yet to be established.
Method:
We present a systematic review which was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). During February and March of 2018, we conducted searches on PubMed (Medline), Virtual Health Library Search Portal databases (BVS), Web of Science (WOS), and Embase for all VR-related publications in the past 4 years (2015, 2016, 2017, and 2018). The keywords used in the search were “neurorehabilitation” AND “Virtual Reality” AND “devices.”
Results:
We summarize the literature which highlights that a range of effective VR approaches are available. Studies identified were conducted with poststroke patients, patients with cerebral palsy, spinal cord injuries, and other pathologies. Healthy populations have been used in the development and testing of VR approaches meant to be used in the future by people with neurological disorders. A range of benefits were associated with VR interventions, including improvement in motor functions, greater community participation, and improved psychological and cognitive function.
Conclusions:
The results from this review provide support for the use of VR as part of a neurorehabilitation program in maximizing recovery.
Keywords: Devices, neurorehabilitation, virtual reality
Introduction
Neurological disorders (characterized by impaired function) affect a significant amount of people worldwide.1 Such disorders are typically associated with reduced daily function, and a negative impact on quality of life is common.2
A range of rehabilitation programs may be offered to individuals with such difficulties, to improve abilities in activities of daily living and increase social participation.3 Such programs are frequently delivered to patients with a range of conditions including patients recovering from stroke,4 living with cerebral palsy (CP),5 or spinal cord injury (SCI).6
It has been suggested that traditional therapy is not without limitations in aiding recovery, and that more radical approaches are much needed.7 Stasieńko and Sarzyńska-Długosz,8 for example, report that constant repetition of the same movements will result in the patient being less engaged and resistant to treatment, which will affect involvement in exercise and ultimately reduce effectiveness of the therapy. The success of many conventional therapy treatment plans requires both attendance at treatment sessions and adherence to exercises that are to be completed. The majority of activity required is unsupervised and in the individual’s own time. A paucity of studies has sought to establish how therapists can optimize on adherence to prescribed exercises and physical activity guidelines.9
It is reasonably well-established that the rehabilitation process can become unnecessarily prolonged if the patient loses interest and if there is a paucity of human and technological resources.3 In this context, combining traditional rehabilitation techniques with the use of new technologies (eg, robotics, brain-computer interfaces, noninvasive brain stimulators, neuroprostheses, and wearable devices for movement analysis) may positively impact on rehabilitation of cognitive and motor functions.3,10 However, there may be obvious barriers in terms of additional costs, access, and usability of such technology which means that rehabilitation teams may not ultimately adopt such approaches.
An intriguing (emerging) and novel possibility for rehabilitation of neurological disorders in individuals may lie in the use of virtual reality (VR).
Virtual reality is essentially a way for humans to visually connect with, manipulate, and interact with computers.11,12 Virtual reality can be seen as an advanced form of human-computer interaction that allows users to become immersed within synthetic computer-generated virtual environments.13 The creation of an engaged VR user experience can be accomplished using combinations of a wide variety of interaction devices, sensory display systems, and content presented in the virtual environment.
Virtual reality can be a totally immersive experience in computer-generated environments with 3-dimensional (3D) images or objects. In VR paradigms, participants can explore with a perception of reality.14 We therefore note that the demand characteristics of such VR settings can facilitate the activities required by rehabilitation programs, but as part of a more engaging experience.15 The VR-based experimental approaches have been found to offer advantages for individuals with severe motor impairment,16 and studies have demonstrated improved motivation.17
In considering the VR characteristics of current systems and how these systems may be useful in engaging patients, studies have indicated that VR provides the possibility of creating real 3D environments capable of eliciting realistic perceptions and reactions in the patient, whereas the observer may monitor and record the performance of the proposed task, allowing the progress of the patient to be tracked and further developed.3
A number of systematic reviews provide evidence of the positive benefits of such systems. Smith,18 for example, provides a summary of the positive effects on physical functioning and motivational aspects in older adults. Benefits have also been reported in reviews with patients poststroke, in terms of functional recovery of the upper extremities,19–21 and in increasing mobility and quality of life in individuals living with Parkinson disease (PD).22 However, the impact of VR-based approaches on recovery is not fully understood and its advantages compared with traditional neurorehabilitation methods have not yet been established.20,23
With the above literature in mind, our group conducted review studies using VR with focus on (1) which mechanism of injury, illness, or disease has been most commonly used/sampled in investigating VR treatment; (2) how VR has been applied; (3) potential benefits; and (4) limits of the procedures available in the use of VR in neurorehabilitation programs.
Methods
Search strategy
A systematic search was conducted in March 2018 of published articles available on PubMed (Medline), Virtual Health Library Search Portal databases (BVS), Web of Science (WOS), and Embase.
Virtual reality is a rapidly developing and novel field. To maintain focus on more recent studies, we limited searches to studies published in the past 4 years (2015, 2016, 2017, and 2018). The review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.24 The use of checklists of the kind offered in PRISMA improves the reporting quality of systematic reviews and provides substantial transparency in the article selection process.25–27 The search was undertaken using the keywords “neurorehabilitation” AND “Virtual Reality” AND “devices” (Table 1). Applicable articles were identified through screening reference lists of relevant articles.
Table 1.
Search methods for identification of studies in databases.
| Search syntax | No. of articles |
|---|---|
| PUBMED ((“neurological rehabilitation”[MeSH Terms] OR (“neurological”[All Fields] AND “rehabilitation”[All Fields]) OR “neurological rehabilitation”[All Fields] OR “neurorehabilitation”[All Fields]) AND (“virtual reality”[MeSH Terms] OR (“virtual”[All Fields] AND “reality”[All Fields]) OR “virtual reality”[All Fields])) AND (“instrumentation”[Subheading] OR “instrumentation”[All Fields] OR “devices”[All Fields] OR “equipment and supplies”[MeSH Terms] OR (“equipment”[All Fields] AND “supplies”[All Fields]) OR “equipment and supplies”[All Fields]) AND (“2013/02/17”[PDat]: “2018/02/15”[PDat]) |
50 |
| BVS (tw:(neurorehabilitation)) AND (tw:(virtual reality)) AND (tw:(devices)) AND (instance: “regional”) (tw:(neurorehabilitation)) AND (tw:(virtual reality)) AND (tw:(devices)) AND (instance: “regional”) AND (instance: “regional”) |
25 |
| EMBASE ((neurorehabilitation [Title/Abstract]) AND virtual reality [Title/Abstract]) AND devices [Title/Abstract] |
19 |
| WOS ((neurorehabilitation [Title/Abstract]) AND virtual reality [Title/Abstract]) AND devices [Title/Abstract] |
19 |
To select the articles, we used 3 steps. The first step was looking for articles in databases and reading the titles and abstracts. The second step was the exclusion of works using the title or abstract and inclusion criteria analysis. The third and final step was to analyze the full text of the eligible works.23,27,28
Inclusion criteria
Studies were eligible for inclusion if they were written in English. Only studies that included technology devices for evaluation or rehabilitation were accepted.
Exclusion criteria
Review articles, meta-analyses, and editorials were excluded, and published clinical trial protocols were also excluded as they do not provide data for analysis.
Study selection
Studies published in English were eligible if they met the following criteria: (1) analysis of VR devices and (2) discussion of/ evaluation of neurorehabilitation treatments. There were no restrictions regarding sample size. Articles were excluded if they (1) were not databased (eg, books, theoretical papers, or secondary reviews), (2) were not in the English language, (3) studies that did not explicitly identify neurorehabilitation, (4) did not emphasize VR devices as therapeutic intervention, or (5) the studies were not published in the past 4 years (2015, 2016, 2017, and 2018). We pooled statistical data from quantitative studies within meta-analyses.
After the removal of duplicates, 3 authors evaluated titles, abstracts, and the inclusion criteria independently. All identified studies were collected in EndNote Web (Thomson Reuters).
Results
The initial search strategy yielded 113 references (including duplicates) from the 4 electronic databases. After duplicates were removed, 79 references were assessed by 2 authors. Based on titles and abstracts, 41 manuscripts were considered relevant and the full texts were analyzed. The search results are shown in Figure 1.
Figure 1.
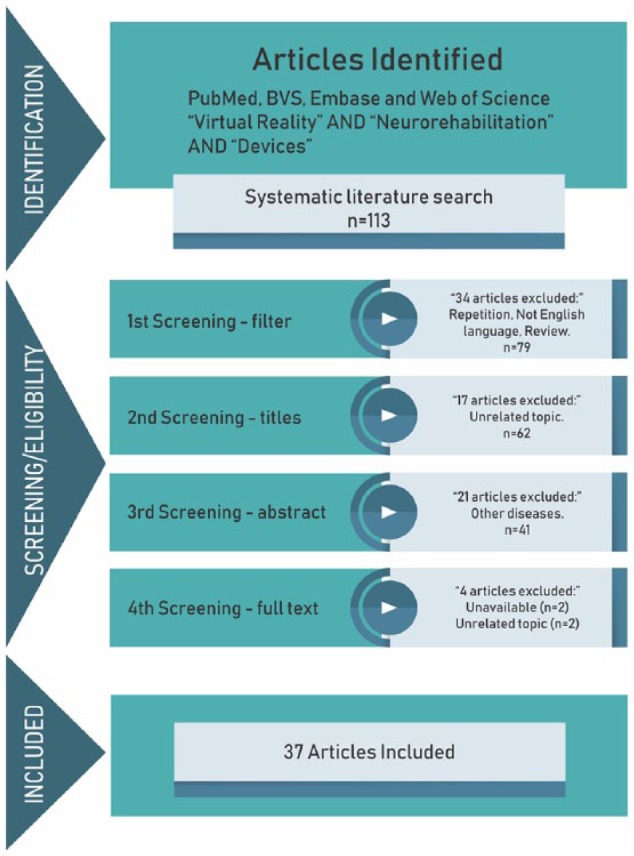
Procedures for determination of eligibility.
Adapted from Moher et al84.
A summary of characteristics of included studies is presented in Tables 2 and 3.
Table 2.
Characteristics of included studies ordered by pathology most investigated.
| Reference | Pathology involved (rehabilitation focus) | Devices (name) | VR environment | Main outcomes |
|---|---|---|---|---|
| Assis et al29 | Stroke (upper limbs) | Webcam love rojection screen (NeuroR system) |
Two visual tracking approaches for NeuroR system were developed. (1) Participants wore a glove on the injured arm and physical markers were adjusted to each participant’s shoulder. (2) The computer system identified the injured arm and tracked it without the glove (markerless tracking). In both cases, the participants are not facing the screen displaying the injured arm wearing the glove. Instead, they see a virtual 3-dimensional arm replacing the actual limb on the screen | NeuroR system provides a mental practice method combined with visual feedback for motor rehabilitation of chronic stroke patients, giving the illusion of injured upper-limb (UL) movements while the affected UL is resting. Its application is feasible and safe. This system can be used to improve UL rehabilitation, an additional treatment past the traditional period of the stroke patient hospitalization and rehabilitation |
| Calabro et al30 | Stroke (lower limbs) | Lokomat 42-in flat screen Dolby surround system (—) |
The 2D VR presented visual feedback showing a VR run game where the patient had to collect or avoid objects, to motivate himor her to walk actively The Lokomat device served as a multimodal feedback system: the human-machine interaction forces measured from the Lokomat device were used as an input device for the patient’s movements into the VR |
The robotic-based rehabilitation combined with VR in patients with chronic hemiparesis induced an improvement in gait and balance. EEG data suggest that the use of VR may entrain several brain areas (probably encompassing the mirror neuron system) involved in motor planning and learning, thus leading to an enhanced motor performance |
| Held et al31 | Stroke (posture rehabilitation) | Force plate 3D camera Kinect TV screen (REWIRE autonomous telerehabilitation platform) |
Exergames where the patient sees himself as an avatar moving and interacting in real time with the virtual game environment | Autonomous telerehabilitation for balance and gait training with the REWIRE system is safe, feasible and can help to intensive rehabilitative therapy at home |
| Mousavi Hondori et al32 | Stroke (cognitive and motor rehabilitation) | Small plastic cup with color marker Overhead camera LifeCam (—) |
A version of Fruit Ninja video game. A fruit target would then appear in 1 of the 4 corners of the tabletop and start moving around the desktop workspace. The subject was to use the stroke-affected hand to move the cursor onto the fruit (which would slice the fruit in half, make a noise, and score 1 point) before the fruit disappeared (which would score 0 points). Once the fruit was sliced, or disappeared, or unsliced, a new fruit target would appear in 1 of the 4 corners, the sequence of which was pseudo-randomized. Subjects were instructed to slice as many fruits as possible within the allotted time. The score was presented throughout each game. One round of each game was 90 seconds long. | The optimal choice of human-computer interface likely varies across individuals, over time, and according to specific goals. This study provides insights into how choice of human-computer interface affects motor performance and thus might influence stroke rehabilitation and motor recovery |
| House et al33 | Stroke (cognitive and bimanual upper extremity rehabilitation) | A low-friction symmetrical table that was wheelchair accessible and electrically lifted or lowered to accommodate different body types. (BrightArm Duo system) | BrightArm Duo simulations allow to adapt to each participant each day. The adaptation was based on arm reach and grasp strength baselines performed at the start of each rehabilitation session. Each of the custom games had some settings that required reach and grasp dual tasking | The results showed clinical benefits in the motor, emotive, and cognitive domains, as well as good technology acceptance by the participants. There was a large impact on attention/working memory following training on the BrightArm Duo system |
| Lin et al34 | Stroke (fine motor impairment in finger movement) | Vibration-assisted glove (—) |
The virtual environment consisted of 2 games. Gopher hitting game: 4 individual gopher-like cartoon characters correspond to the 4 fingers of a patient and randomly appear in a virtual environment. When a gopher appears on the computer screen, the vibration motor stimulates the assigned finger inducing the patient to use that particular finger to hit a designated click region on the table. Musical note hitting game: the musical note hitting game with balls in 4 regions. To enable patients who are familiar with musical instruments to play this game and receive effective therapeutic evaluation, a random and nonrepeating melody consisting of 7 fundamental notes is played through a computer speaker. A ball in a virtual environment is programmed to rise depending on simultaneous vibrotactile and acoustic stimulation. In each trial, the patient presses the tip of the corresponding finger on the correct click region | The preliminary test results of using healthy people elucidated the potential use and benefits of adding vibrotactile stimulation in practical haptic training. Design concerns related to the mechatronic design and clinical trials were presented to enable optimizing the performance of the proposed system. Future studies could apply this system on stroke patients and investigate the rehabilitation performance by following comparative clinical protocols |
| Lledo et al14 | Stroke (upper-limb neurorehabilitation) | Robot system (PUPArm) | The virtual task with the VR environment consists on a roulette formed by a central target and 8 peripheral targets. These targets were circles with a radius of 1 cm. The 8 peripheral targets were distributed uniformly on the circumference of the circle and placed 10 cm from the center target. The main purpose of this task was to reach 1 of the 8 peripheral targets from central target by controlling the robot end-effector attached to the subject’s hand | The hypothesis that consists of showing a visualization environment more natural (3D) increasing the immersion level did not provide many improvements regarding an environment simpler (2D). Using 2D environments in virtual therapy may be a more appropriate and comfortable way to perform tasks for upper limb rehabilitation of poststroke patients, in terms of accuracy to effectuate optimal kinematic trajectories |
| Mobini et al35 | Stroke (upper body joints) | Microsoft Kinect for Xbox 360 Microsoft Kinect’s skeleton tracking (—) |
In the program, they were instructed to move their hands to intercept and catch several approaching balls. All of the targets are on a plane parallel to the frontal plane but reaching them requires movements in the 3D space. The program also provided audio feedback to the patients based on their performance | The results are promising for the development of home-based rehabilitation systems, which can analyze patient’s movements using Kinect as an affordable motion capture sensor |
| da Silva et al36 | Stroke (sensorimotor function) | Nintendo Wii Multimedia projector (—) |
The Tennis and Hula hoop games were applied during the first session; the Soccer and Boxing games were applied during the second session | Virtual rehabilitation using the Nintendo Wii and conventional physical therapy both effectively treat poststroke hemiparetic patients by improving passive movement and pain scores, motor function of the upper limb, balance, physical functioning, vitality, and the physical and emotional aspects of role functioning |
| Saposnik et al37 | Stroke (motor recovery of upper extremity) | Nintendo Wii (—) |
Wii Sports and Game Party 3 | This study suggests that the type of task used in motor rehabilitation poststroke might be less relevant, as long as it is intensive enough and task specific. Simple, low-cost, and widely available recreational activities might be as effective as innovative nonimmersive VR technologies |
| Simkins et al38 | Stroke | Two-armed robot, 14-DOF exoskeleton termed the EXO-UL7 50-in flat screen monitor (—) |
The virtual games were controlled using the joint angles of the robot. Full-arm movements in flower, paint, reach, and handball were generated using a forward kinematic model of the avatar arms. The Pinball game was unique in that the paddles were simply actuated by wrist flexion and extension. The Pong and Circle games used a paddle that was constrained to a linear path | After 12 training sessions (90 minutes/session), the bilateral training group had the greatest intensity of movement training. They also had the greatest improvement in range of motion at the shoulder. The unilateral training group showed the greatest reduction in spasticity |
| Steinisch et al39 | Stroke (neuromotor rehabilitation of upper limbs) | Passive robotic device (Trackhold) 22-in LCD (—) |
The VR training applications (Sponge, Bug Hunt, Grab 2D, Grab 3D) simulate ADLs and/or reproduce simple visuomotor coordination tasks. Subjects interact online with the VR training applications by moving the Trackhold’s end-effector and observe the changes occurring in the virtual environments in real time | Results from kinematic and EEG data analysis are in line with knowledge from currently available literature and theoretical predictions and demonstrate the feasibility and potential usefulness of the proposed rehabilitation system to monitor neuro-motor recovery |
| Thielbar et al40 | Stroke (fine motor control) | Actuated glove PneuGlove (Actuated virtual keypad—AVK system) |
The AVK system combines a custom actuated glove, the PneuGlove, with a virtual scene consisting of a hand and 5 keys. The PneuGlove provides both independent measurement and actuation of each digit. Air pressure controlled through servovalves is used to extend (or prevent flexion of) a specified digit by inflating an air chamber located on the palmar side of the digit. Evacuation of the air chamber permits almost unrestricted movement of the digit | Actively assisted individuation therapy comprised nontask-specific modalities, such as can be achieved with virtual platforms like the AVK described here, may prove to be valuable clinical tools for increasing the effectiveness and efficiency of therapy following stroke. Stroke survivors with chronic impairment were able to successfully use the system to improve hand motor control. Thus, repetitive movement therapy for independent finger movements, such as with AVK system, may be beneficial and warrants further exploration |
| Trombetta et al41 | Stroke (upper limb motor and balance rehabilitation) | HMD Oculus Rift and HTC Vive Kinect for Windows SDK 2.0 Unity game engine to create the game interface Support for stereoscopic visualization Smart TV 3D (Motion Rehab AVE 3D) |
The game contemplates different exercises in a 3D space: flexion, abduction, shoulder adduction, horizontal shoulder adduction and abduction, elbow extension, wrist extension, knee flexion, and hip flexion and abduction. The aim is to simulate 6 activities in which the patient must move his or her hands, upper limbs, lower limbs, and trunk, to get the objects and score. All activities developed for the game contemplates exercises used in conventional physiotherapy sessions | Our evaluation showed that the game could be used as a useful tool to motivate the patients during rehabilitation sessions. All participants classified as an interesting and excellent experience for elderly age. We also suggested to use the game in sessions with poststroke patients, initially, with a most popular visualization device (Smart TV 3D), in third person as the participants felt little bit comfortable during the interaction process Next step is to evaluate its effectiveness for stroke patients, to verify whether the interface and game exercises contribute into the motor rehabilitation treatment progress |
| Verma et al42 | Stroke (lower limbs) | Nintendo Wii Balance board Sacral Belt holding an android phone (VR-based balance training—VBaT platform) |
A database of 30 unique combinations of VR-based environments and virtual objects related to tasks of daily living and entertainment. The task required participants to shift their weight in different directions from the central hold state in the VR environment to a predefined target position, with various target images (chosen randomly from a database) | Results indicate the potential of the VBaT system to cause improvement in overall average task performance over the course of training while using the VBaT. Thus, the VBaT system is proposed to be a step toward an effective balance training platform for people with balance disorder |
| Zoccolillo et al43 | Cerebral palsy (upper limbs) | Xbox with Kinect (—) |
Three games were included into the Kinect Adventures Package. In “Space pops,” the subject is asked to pop bubbles appearing in the virtual environment by touching them. Subject should flap arms for flying around the virtual environment and put arms back down for descending. In “20.000 Leaks,” the child is asked to stop the water from filling the tank by placing a hand, or a foot, or any other body parts over a leak opened on a wall of an underwater glass tank. In “Rally Ball,” balls will shoot down a lane toward the avatar, and the child must hit the balls back with a part of body and destroy targets at the end of the lane. Other 3 games were included into the Kinect Sports Package and were virtual simulation of 3 sports: boxe and volley mainly (but not only) involving bimanual movements, and bowling in which the child was asked to throw the virtual ball toward the pins with the paretic upper limb | Video game–based therapy resulted effective in improving the motor functions of upper limb extremities in children with cerebral palsy, conceivably for the increased quantity of limb movements, but failed in improving the manual abilities for performing activities of daily living which benefited more from conventional therapy |
| Bortone et al44 | Cerebral palsy and developmental dyspraxia (upper limbs) | HMD Oculus Rift DK2 Optical tracking systems Wearable haptic devices (Moneybox Game and Labyrinth Game) |
The Moneybox Game focuses on grasp and reaching tasks with pronation/supination of the hand. The player is asked to grasp a golden coin and to insert it in a floating piggy bank. In the Labyrinth Game, a sliding token has to be driven through a maze by dragging it with the fingertip |
All the subjects completed the rehabilitation session, including both the gaming scenarios, without interrupting the treatment due to fatigue or other reasons. Together with positive comments reported after the rehabilitation session, results are encouraging for application of the method in a prolonged rehabilitation treatment |
| Keller and Van Hedel45 | Cerebral palsy (motor learning) | Adaptable exoskeleton Position sensors (Armeo Spring) |
Moorhuhn (Crazy Chicken) is an exergame with the goal of hunting birds of various sizes (and thereby various points). It requires the player to move and position the arm and hand quickly and accurately in the virtual environment and timely grasp the joystick to shoot at a chicken | The results showed the successful acquisition, transfer, and retention of upper extremity skills. The motor learning occurred when children trained their more affected arm with weight support in a playful, virtual environment |
| Keller et al46 | Cerebral palsy, stroke, and traumatic brain injury (arm rehabilitation) | Arm robot (ChARMin robot) |
The ChARMin platform is characterized by a hardware that is safe and highly adjustable and a patient-cooperative controller that supports arm movements in game-like scenarios (Tornalino, Airplane, Diver, Whack-a-Mole, and Spaceship Game) with an integrated audiovisual interface | These preliminary tests suggest that the ChARMin setup can be used as an advanced exercise tool for arm neurorehabilitation that optimally challenges children and adolescents with severely to moderately affected arm motor functions |
| Shokur et al47 | Spinal cord injury (lower limb somatosensory feedback) | Tactile shirt HMD Oculus Rift (—) |
Missing haptic sensation from the lower limbs was replaced by rich tactile stimulation on the skin of SCI patients’ forearms. This feedback was integrated with an immersive VR environment where a 3D human avatar was simulated. The 3D human avatar projected in the HMD could stand and walk and as it performed these movements, tactile feedback, reproducing the touch of the avatar feet on the ground, was delivered on the skin of the patients’ forearm through the employment of a haptic display (eg, the tactile shirt: see Integration of the virtual body avatars with the tactile shirt) | The addition of tactile feedback to neuroprosthetic devices is essential to restore a full lower limb perceptual experience in spinal cord injury patients, and will ultimately lead to a higher rate of prosthetic acceptance/use and a better level of motor proficiency. Interestingly, patients were never instructed on what the tactile feedback displayed or represented. As totally naïve subjects, they acquired vivid tactile/proprioceptive sensations after exposure to 1 minute of synchronous visuo-tactile stimulation (patients observed the 3D human avatar walking and received the tactile stimulation on their forearm). This suggests that such tactile feedback became intuitive to the subjects rather quickly. As such, we propose that our haptic display paradigm was capable of inducing patients to experience a proprioceptive illusion that allowed them to deduce the position of the virtual avatar legs relying solely on the tactile feedback |
| Dimbwadyo-Terrer et al48 | Spinal cord injury Motion capture systems to train activities of daily living |
CyberTouch™ CyberGlove (—) |
The virtual scene consists of 1 room, 2 shelves and a trench. The user is able to see her or his virtual hand in the scene, as well as virtual objects. A set of virtual geometric elements was created and can be randomly presented in different parts of the upper shelving for each trial | The first findings showed the possibility to conduct a training based on functional reaching movements in a virtual environment in people with spinal cord injury using a data glove and to obtain objective data through 2 functional parameters |
| Kim et al49 | Parkinson disease (neurorehabilitation) | HMD Oculus Rift DK2 (—) |
The virtual environment consisted of a cityscape with buildings, animated avatars, and an 800-m straight sidewalk. The avatars were added to provide a dynamic element to the virtual environment, and they were the only animated features of the environment. Movements through the environment were constrained to the forward direction, but participants were able to freely look around the scene while walking. The environment did not include any turns, doorways, or crossing of thresholds. The velocity of the simulation was synchronized to the speed of the treadmill, and the orientation of the participants’ viewpoint was synchronized with head orientation using an inertial measurement unit embedded in the HMD | Older adults and individuals with PD were able to successfully use immersive VR during walking without adverse effects. This provides systematic evidence supporting the safety of immersive VR for gait training in these populations |
| (Rohani and Puthusserypady50 | Attention deficit hyperactivity disorder (attention) | Microsoft Kinect (—) |
The classroom includes 6 pupil desks each having 2 seats, projection screen, posters, a soccer ball, several hula hoops, a wall clock, book shelves, and a first aid kit. Two windows in the left side of the room are facing out onto a road. The ceiling of the classroom contains a fan, projector, and 6 fluorescent lights. Also is seen a female teacher, her desk, as well as a computer on the desk, and a blackboard behind her | This work has successfully demonstrated a nonintrusive, low-cost, and portable system targeting attention in a motivating and engaging environment. The authors found the low-cost system to be good enough in practice, as the major limitation of BCI feedback system were related to the reliability and minimization of false classifications by their P300 speller, which they solved by a better and faster machine learning classifier based on support vector machines (SVM) |
| Pedroli et al51 | Dyslexia (reading abilities) | Microsoft Kinect Audio system (—) |
The tasks took place in the same Virtual Classroom, where patients were sitting at a desk and looking at the blackboard. All the visual stimuli were shown on the blackboard and the tasks were explained by a voice. All the instructions were presented before the tasks and repeated until the child understood. To respond to a target, the children had to raise 1 extended arm laterally and stop when the hand reached shoulder height | The results do not demonstrate an immediate effect on reading performance, suggesting that a more prolonged protocol may be a future direction, the presence of a significant decrease in the time of reading low frequency longwords supports the possible validity of the proposed approach. The protocol is innovative because it uses VR to improve attentional skills in children with dyslexia. This technology is able to involve children in nonconventional tasks and allow them to work in a virtual environment similar to the real one |
| Peruzzi et al52 | Multiple sclerosis (dual-task walking) | HMD Emagin, Z800 LCD screen Two magneto-inertial measurement units (—) |
Participants walked on the treadmill while watching a VR environment representing a tree-lined trail. Subjects were required to pass obstacles (puddles and logs) appearing on the trail. The specific simulation was chosen to address specific gait problems, common in multiple sclerosis (ie, decreased foot clearance, obstacle avoidance, and problems with planning). Successful and unsuccessful passes, as determined by the inertial measurements, were rendered to the subject during the trial with visual and auditory feedbacks. A cognitive concurrent task was added by asking subject to memorize the route to follow, which was shown to them prior to the trial. Several dynamic distractors were also added to the virtual environment to challenge subject’s attention | VR-based treadmill training program is feasible and safe for multiple sclerosis subjects with moderate disabilities and may positively affect gait under complex conditions, such as dual tasking and obstacle negotiation |
| Gagnon et al53 | Autosomal-recessive spastic ataxia of Charlevoix-Saguenay (measures of upper limb coordination) | Haptic device equipped with a custom-made handle instrumented with 3 force sensors (Virtual Peg Insertion Test—VPIT) |
VR environment displaying a pegboard tasks. Pegs can be grasped in the virtual environment by precisely aligning a cursor representing the position of the handle of the haptic device with 1 of the 9 pegs (distal coordination) and grasping the handle over a force threshold of 2 N (prehension strength) | The results demonstrate the potential to evaluate upper limb impairment, in particular impaired coordination, and monitor its progression over time |
| Grewe et al54 | Focal epilepsy (cognitive neurorehabilitation) | 360° VR apparatus, OctaVis Throttle joystick LCD touchscreens (—) |
Virtual medium-sized supermarket, which had a structure comparable with that of a real supermarket | A novel 360° VR environment demands real-world–like visual-spatial and motor actions and thus allows for the training of the respective cognitive abilities |
Abbreviations: BCI, Brain Computer Interface, EEG, electroencephalography, PD, Parkinson disease; VR, virtual reality.
Table 3.
Characteristics of included studies that used the new virtual reality environment in healthy participants.
| Reference | Rehabilitation focus | Devices (name) | VR environment | Main outcomes |
|---|---|---|---|---|
| Borrego et al80 | Lower limbs | HMD Oculus Rift DK2 3D glasses Crystaleyes 3 CAVE system (—) |
The environment represented an aisle of a grocery store, defined by 2 shelves with different kind of sodas. Each shelf consisted of 6 racks with 72 different items. The price of each soda was indicated in the shelf | The marker-based solution provided accurate, robust, and fast head tracking to allow navigation in the VR system by walking without causing relevant sickness and promoting higher sense of presence than CAVE systems, thus enabling natural walking in full-scale environments, which can enhance the ecological validity of VR-based rehabilitation applications |
| Byagowi et al81 | Motion sickness | Joystick Wheelchair with a custom designed motion capture unit (VRNChair) |
VR navigational environment that is operated using a wheelchair experiment consisted of a first-person view, traversing a lawn of a 3-story building, entering the building, and approaching a specified target window on the second floor. The target window was shown to the participant from outside the building by rotating the entire building in VR. Then, the participant was instructed to go inside and find the target | The designed VRNChair technology successfully provides an input device to receive navigational commands, providing a more naturalistic input method for VR navigation experiments, reducing the kinetosis effect |
| Cappa et al79 | Dexterity in planning and generating the multijoint visuomotor tasks | Novint Falcon haptic device Video screen (—) |
The 2D scenario was the representation of New York City’s Bronx Zoo, where a predefined path The selection of a 2D scenario was motivated by future use of the system with clinical population with reduced visuo-spatial abilities |
Preliminary evidence that using educational content increases subjects’ satisfaction. Improving the level of interest through the inclusion of learning elements can increase the time spent performing rehabilitation tasks and promote learning in a new context |
| Dobkin55 | Directions for research | Wireless chargers for sensors Ankle accelerometers with Gyroscopes Android phone to monitor walking and cycling Force sensor Stretch band to monitor resistance exercises LEAP motion (RIoT—Rehabilitation-Internet-of-Things) |
Collect data from real life | The sensors are charged wirelessly overnight as the raw data for walking (the accelerations and decelerations of each gait cycle for each leg, including heel strike, foot flat, heel-off, toe-off, swing, and single- and double-limb stance duration) are sent to a server. All signal processing is performed automatically, providing a therapist with a record of every bout of walking with its time of day, duration, speed, distance, and aspects of quality. The coaching therapist and patient can use the feedback to lessen sedentary time, summated on an hourly basis, and to increase the number, duration, and speed of walking bouts |
| Fluet et al56 | Directions for research Arm and finger rehabilitation activities |
Haptic MASTER ROBOT CyberGlove CyberGrasp (—) |
Virtual environments with haptic guidance in 3D space provided by a robot: Performing hand simulations emphasizing hand opening and individual finger movement; arm simulations emphasizing 3D reaching, and forearm pronation with the arm elevated away from the trunk; simulated functional movements (hammering a peg, pressing piano keys, and placing cups on a shelf) and game-based activities (pong, piloting a space ship and blowing up targets) | The results demonstrated that improvements in motor function elicited by practicing simulated activities might transfer to real-world task performance as well as training in the real world |
| Luu et al82 | Human bipedal locomotion | Television Goniometers Accelerometers Electroencephalography Electrooculogram (—) |
A television monitor was placed in front of the treadmill, displaying an avatar of the subjects standing/walking in a virtual environment. The screen only showed movement of body parts below the waist of the avatar because this study focused on lower limb movements. The avatar followed the subject’s lower limb movements precisely in real time by matching the joint angles (hip, knee, and ankle) on both legs | Our results demonstrate the feasibility of using a closed-loop brain-computer interfaces to learn to control a walking avatar under normal and altered visuomotor perturbations, which involved cortical adaptations |
| Basso Moro et al77 | Maintenance of the postural balance | Force platform Projection screen 3D depth-sensing camera Middleware High-performance real-time 3D engine (—) |
The subject, standing on the force platform, observes his body model and the virtual swing board on the screen when performing a semi-immersive virtual reality incremental swing balance task in the forward and backward direction | The use of the depth-sensing camera for capturing the whole subject’s motion (which preserves the geometry of the movement with respect to the body and the environment) allowed an accurate mapping of the center of mass movements of the subject into a semi-immersive VR environment (the subject’s movements were not suggested by the system), which was confirmed using a standard force platform. Considering the adaptability of this virtual balance task to specific neurological disorders, the absence of motion sensing devices, and the motivating/safe semi-immersive VR environment, the incremental swing balance task adopted in this study could be considered valuable for diagnostic testing and for assessing the effectiveness of functional neurorehabilitation |
| Moro et al78 | Neurorehabilitation of the upper limb motor function | LEAP motion controller (visuomotor task—VMT) | Customized version of Marble Motion game. At the beginning of the task, the subjects had to guide the virtual sphere (VS) over the virtual path using 4 commands. The first command (flexion) allowed the VS to proceed forward; the second command (extension) allowed the VS to decrease the speed (up to stop the VS) and to proceed backward; the third and the fourth commands (rotations of the wrist, for a maximum of about 80°, in the clockwise and counter-clockwise direction, starting from pronation) moved the VS to the left or to the right side, respectively | This study has revealed a particular involvement of the ventrolateral prefrontal cortex in the execution of the novel proposed semi-immersive VMT adoptable in the neurorehabilitation field |
| Pacheco et al83 | Lower limb motor task | Wii Balance Board Portable EEG device Emotiv EPOC (—) |
The virtual game was “Basic Step,” which aims to make the avatar move up and down the Wii Balance Board in the antero-posterior and lateral direction, according to the auditory and visual feedback provided by the game | Theta, alpha, beta, and gamma activity during the execution of a motor task differs according to the environment that the individual is exposed—real or virtual—and may have varying size effects if brain area activation and frequency spectrum in each environment are taken into consideration |
| Vourvopoulos and Bermudez57 | Upper limbs | HMD Oculus Rift DK1 LEAP Motion Control (—) |
The motor execution task, a “virtual garage,” involved the rotation of a virtual lever through circular movements for opening a large garage door. The virtual environment included spatial sounds related to the movement of the door and the lever. The sounds generated by the chain mechanism and other mechanical sounds were activated through the rotation of a handle that controls the opening of a virtual garage door | Our data suggest that both VR and particularly MP can enhance the activation of brain patterns present during overt motor execution. Furthermore, we show changes in the interhemispheric EEG balance, which might play an important role in the promotion of neural activation and neuroplastic changes in stroke patients in a motor imagery neurofeedback paradigm |
Discussion
Rehabilitation programs are increasingly using VR environments to simulate natural events and social interactions. Bohil et al58 show that VR creates interactive, multimodal sensory stimuli that offer unique advantages over other approaches in research and clinical practice. Our results show that several studies have demonstrated the effectiveness of VR in therapeutic interventions even considering 8 studies that selected healthy participants to explore the efficacy of innovative devices to contribute toward the neurorehabilitation field. To understand how practices using VR are being implemented and their contributions to the neurorehabilitation field, we present our discussion focussed on in the available studies according to (1) which mechanism of injury, illness, or disease has been most commonly used/sampled in investigating VR treatment-(populations investigated); (2) how VR has been applied; (3) potential benefits; and (4) limits of the procedures available in the use of VR in neurorehabilitation programs.
Populations investigated
Studies have investigated populations with stroke, CP, and SCI, among other diseases. Most of the studies presented were performed with poststroke patients.14,29–36,38–42,46,56,57,59 We hypothesize that stroke has been predominantly investigated due to the high incidence of this disease in developed countries (affecting 1/500 individuals every year). Most of the studies which explore the use of VR evaluated its effectiveness in facilitating improvement of upper-limb function.
After stroke, CP was the most studied neurological disorder in VR rehabilitation. Four studies identified in our review have explored the effectiveness of VR in individuals with CP using immersive VR,44 nonimmersive VR,43 and dedicated devices, such as robotics.45,46 Similarly, to its use with stroke patients, VR was used only for upper limbs rehabilitation, demonstrating positive results for individuals with CP, promoting motor learning and improvement in performance for both immersive and nonimmersive environments. However, we note here the work of Zoccolillo et al43 who found that although the VR improved the quantity of movements of upper limbs, the quality of hands and finger movements improved more in the real environment, ie, using conventional rehabilitation.
de Mello Monteiro et al60 similarly report findings from a cross-sectional randomized study evaluating transfer of motor learning from virtual to natural environments in individuals with CP. The authors showed that these individuals improved performance in virtual and natural environments; however, there was no transfer of learning between environments and their performance was less accurate in an abstract task than in the more real task, thus a rehabilitation team should be careful in implementing virtual environments when attempting to enhance motor functioning of individuals with CP.
Not all studies align in these findings however. A recent meta-analysis61 showed that VR rehabilitation programs focused on motor control, balance, gait, and strength are, overall, more effective than traditional rehabilitation programs. The authors speculated that this may be due to the excitement, physical fidelity, and cognitive fidelity provided by the virtual environment. Moreover, another review and meta-analysis that assessed the effectiveness of VR in children with CP demonstrated that VR is a viable intervention in improving arm function, gait, and postural control. The authors also emphasize that the repetition of therapeutic exercises should be performed in the VR home environment to maximize the positive benefits of intervention.62
The third neurological disease most studied was SCI. Two studies have focused on this population. One of the studies demonstrated a new and interesting approach in reproducing lower-limb somatosensory feedback in paraplegics, in restoring a full lower-limb perceptual experience in patients with SCI. They provide feedback integrated with an immersive VR environment where a 3D human avatar was simulated. The authors reported some positive sensation from participants. The second study looked at the patient’s functional performance through the use of a glove, with a training based on functional range movements in a virtual environment.48 Training of people with SCI is demonstrated based on functional reaching movements in a virtual environment using a data glove.
Among the remaining studies of VR in neurorehabilitation, some pathologies are only recently being explored, probably due to the lower incidence of these pathologies and greater difficulty in recruiting populations given the heterogeneous nature of impairments these groups present with.
In relation to multiple sclerosis, the study we identified focused on the performance of this population walking in complex conditions. The participants walked on a treadmill while watching a VR environment representing a wooded trail. The subjects were encouraged to pass obstacles (puddles and trunks) appearing on the trail. The authors concluded that the treadmill training program is feasible and safe for training of gait with obstacles in individuals with multiple sclerosis.52
In PD, independence related to gait in individuals with PD was focused on and the authors demonstrated that the patients with PD were able to use the immersive VR during the walk successfully and without adverse effects.49
Participants with ataxia were evaluated with a VR tool developed for assessing impaired coordination and monitoring progression over time.53 In another study of coordination disorders, the participants performed rehabilitation sessions focused on grasping and reaching tasks with pronation/supination of the hand. The authors report positive results in a prolonged rehabilitation treatment, which usually is necessary in this population.44 Four further studies are addressed: autosomal recessive spastic ataxia of Charlevoix-Saguenay, focal epilepsy, attention deficit hyperactivity disorder (ADHD), and dyslexia. These studies focused on the cognitive aspects of neurorehabilitation and have indicated the effectiveness of devices used during the VR interventions for evaluating and monitoring upper limb impairment, in particular impaired coordination,53 for training cognitive abilities54 and for promoting attention in a motivating and engaging environment.50,51
How VR has been applied
From our review, we note that VR can be considered a computer technology that provides 3D artificial sensory feedback, whereby the user engages in experiences similar to real-life activities and events. Commercial games have some limitations, for example, the calibration of a game’s difficulty is conducted with healthy players and does not consider individuals with disabilities. In studies of the commercial games currently available, a rehabilitation team might often rely on adapted versions of the game to improve performance.63 In considering the work by Crocetta et al,63 we advocate that the development of platforms with tasks that are adapted to the needs of people with disabilities is the future of the use of VR in rehabilitation. It is certainly the case that research involving specific platforms for rehabilitation should be developed that would consider user experience (the kind of experience the games create for the individual who uses it how virtual experience then informs specific skill sets in the real world).64 Indeed, engagement with online communities, including a community of people with neurological diseases, would depend on the usability and adaptability of platforms for games (see the work by Crossley et al64). We therefore consider that the factors that can influence user experience should be carefully observed when designing games.
It is difficult to extrapolate directions that innovative hardware of the future may take for people with neurological disorders. Virtual reality is an emergent technology that is still being constructed and expanded on by science and research. However, this work has given an overview of how scientists and researchers are working toward development of new devices that address the needs of this population. Studies have pointed out relevant and strategic approaches that attest to how future advances may support the development of innovative devices that are more specifically effective for this population.
In considering the work by Pichierri et al,65 VR can result in an optimal solution for the rehabilitation of cognitive and motor functions and we note that VR interactive devices are precious tools in the process of inclusion and actual interfacing with people with some type of disability.
The potential benefits reported in the current literature are commonly noted in a context where VR devices have been customized for people with neurological disabilities. To this extent, we advocate that it would be important to increase accessibility to this technology through developing and maintaining low-cost products on the market. According to Crocetta et al,63 there are different VR devices that can be efficiently used to provide the user with greater control over the VR experience and associated actions through a remote input device, such as a keyboard or a mouse,32,63 or by more advanced VR devices such as a Kinect sensor, special gloves,66 and new hardware that may be adapted to provide a patient-compatible controller that supports arm movements in different game scenarios with an integrated audiovisual interface.46 It is important to emphasize that because each VR device has a potential function, a multidisciplinary evaluation of each person’s needs is important to provide a functional interaction and identify the best bespoke device.55
Potential benefits
Several benefits were widely reported in relation to motor function: upper limb and postacute treatment beyond the initial period of hospitalization and rehabilitation, improvement in balance and gait,31,42 neuromotor monitoring of recovery,39 improvement of strength fitness,67 skills,68 improvement in the range of movement of shoulder and reduction in spasticity,38 and also the improvement of the levels of participation in both domestic and community environments.38 Furthermore, there were psychological and cognitive benefits reported when the VR device is adapted to the patient, such as improvement in attention, or memory stimulation and decrease in depression symptomology in elderly participants. This was evident even several years after stroke.14,29,33,36 Therefore, VR devices could be used as effective tool to motivate patients during rehabilitation sessions,41 to improve spatial orientation and attention in daily life activities,59 and to improve pain relief scores and emotional aspects related to functionality.36
Additional benefits of using VR environments in neurological rehabilitation were also reported, such as safety/security, multitask possibilities, patient’s adherence, and lower cost. According to Lange et al,69 a real and safe VR training environment will provide subjects with task-specific training, accurate sensory and tactile feedback, and motivation. Furthermore, to develop an individualized rehabilitation program targeted to different dysfunctions, and to keep patient’s interests, an active participation can be achieved using telerehabilitation, which can be remotely controlled by the therapist and can cost significantly less compared with traditional face-to-face interventions.29,32,55
Moreover, Saposnik et al,37 comparing real intervention (simple recreational activities, eg, play cards and ball game) and nonimmersive VR intervention (Nintendo Wii gaming system) in a randomized, multicenter, single-blind, controlled trial with poststroke patients, reported that both interventions provide improvement and benefits to participants. However, they emphasized that combined therapy (real and VR) presented better outcomes. These results align with Aminov et al70 who also emphasized that the use of combined therapy is effective in patients with neurological disorders.
Regarding children, more research is clearly needed, and we are yet to understand whether VR holds any implications for brain development. Keller et al46 report that VR is an excellent way of offering optimal challenges to children and adolescents with severe-to-moderate arm motor function difficulties. Pulay71 demonstrate that eye-tracking and EMG-supported 3D VR combination devices worked well in terms of efficiency in children with spastic tetraparesis. Again, the accessible environment that is motivating will reportedly empower children with disabilities to take an active role in their rehabilitation.72 It is important to also highlight (as in Table 2) the use of eye trackers, which are expected to become popular in near future.47 The manufacturers are hoping to be able to create high-resolution, foveated (level-of-detail) rendering, thus increasing the realism of VR environments with less hardware power. This general trend is expected to increase utility in increasing medical applications with development of pervasive eye-tracking VR headsets, expanding the number of developers available who may be familiar with integrating eye tracking with VR.
It is also important to note how the use of VR applications in the future may benefit from larger pooled automated data and artificial intelligence. For example, if eye trackers become a standard feature of VR in every headset, this could generate data from healthy controls and individuals with disability. This may be to the effect that results may allow for equality of performance, where people with disabilities could interact competitively with people with typical development—we advocate that this should be further explored in future studies.
Limitations
Despite the increasing enthusiasm for VR, and evidence of its use in clinical applications, the recent literature has highlighted some limitations:
In the work by Lin et al,34 preliminary tests were conducted to assess the feasibility of the developed haptic rehabilitation system and they identified design concerns that should be considered regarding the practical use in future clinical testing.
In addition, the use of immersive and semi-immersive VR can and does cause unwanted effects, and typical symptoms such as sickness, dizziness, headache, nausea, and vomiting are frequently reported.73 From our own VR experience, we consider that it could be due to the visual perception of movement and motion while the person is still. The mixed messages on the brain can cause a “motion sickness” effect. This needs careful consideration where there may be vestibular effects of injury. We have found that computers with increased processing capacity that enable smoother visual experiences can minimize such motion sickness effects, but more research is needed here. This paired with the fact that some devices are already considered expensive and may need some specific training to use74 and can be considered as a technology or marked limitation.
There are many elements to be considered in discussing limiting factors that prevent mainstream VR applications being sufficient for neurorehabilitation purposes. The literature has highlighted that VR for neurorehabilitation can provide modern tools for increasing efficiency. However, despite the full potential of VR approaches, the technology is in early development and there is further development needed before this technology can be fully integrated into the routine rehabilitation.75 We consider that VR should be used only as a tool in the hands of neurorehabilitation teams or therapists in the framework of a rehabilitative program and not as a rehabilitative approach per se. Therefore, VR should be used to boost certain specific aspects of rehabilitation such us intensity, participation, engagement, and feedback, but here we recognize that we need more studies to establish generalizability of benefits.
New technological devices and some applications for computers and mobile phone (different start-ups created specific tasks) have been commercialized despite the lack of a clear proof of their effectiveness and/or a clear definition of user guidelines.76 Public policies that ensure scientific scrutiny of this new technology should be in place to protect the interests of individuals with disability. According to Morone et al,76 it is important to establish proof of the effectiveness of VR and to generate clearly defined user guidelines before new devices are made available commercially.
From a financial perspective, the high cost of new VR technology needs to be considered as a limitation. For this reason, video game–based therapy and nonimmersive VR systems are playing an important role in cost-effective rehabilitation. Cost-saving approaches include using commercial gaming systems and augmenting the involvement of patients’ attention and participation to the exercise/game.75
As a limitation of this review, it is important to acknowledge that our interpretation of the studies was directed at VR use in rehabilitation team settings, and so our specific interpretation focused on the development and technological engineering and software development that may be developed in future work.
Final considerations
The results from this review provide evidence that VR can and does have beneficial effects on rehabilitation of patients with neurological disorders. In our view, future developments in VR will lead to improved motor, psychological, and cognitive functions in this population and are likely to be an increasingly important option to complement traditional therapies. Based on our findings, we advocate for the relevance of innovative, functional, and interactive VR devices and the importance of availability and accessibility for individuals with neurological disorders. Moreover, we emphasize the need for studies that prove the effectiveness of existing technologies and greater scientific support for future proposals.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/ or publication of this article: This work was supported by the Brazilian agency CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) process number 442456/2016-6 and 8887.091039/2014-01.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: TM structured the script and directed the work; TM, TDS and TBC performed the data collection and organized the data; RG and BLF performed the data collection and organized the data; The PBL structured the method and data analysis; SW and JT structured the discussion and conclusion; TM and TDS performed the data analysis and assembled the results work; PBL and JT adapted the work to the English language; SW and TM helped build the discussion; The CBMM reviewed and organized the manuscript in general.
References
- 1. Shishov N, Melzer I, Bar-Haim S. Parameters and measures in assessment of motor learning in neurorehabilitation; a systematic review of the literature. Front Hum Neurosci. 2017;11:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cincotti F, Mattia D, Aloise F, et al. Non-invasive brain-computer interface system: towards its application as assistive technology. Brain Res Bull. 2008;75:796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tieri G, Morone G, Paolucci S, Iosa M. Virtual reality in cognitive and motor rehabilitation: facts, fiction and fallacies. Expert Rev Med Devices. 2018;15:107–117. [DOI] [PubMed] [Google Scholar]
- 4. Coleman ER, Moudgal R, Lang K, et al. Early rehabilitation after stroke: a narrative review. Curr Atheroscler Rep. 2017;19:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gagliardi C, Turconi AC, Biffi E, et al. Immersive virtual reality to improve walking abilities in cerebral palsy: a pilot study. Ann Biomed Eng. 2018;46:1376–1384. [DOI] [PubMed] [Google Scholar]
- 6. An CM, Park YH. The effects of semi-immersive virtual reality therapy on standing balance and upright mobility function in individuals with chronic incomplete spinal cord injury: a preliminary study. J Spinal Cord Med. 2018;41:223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liao YY, Yang YR, Cheng SJ, Wu YR, Fuh JL, Wang RY. Virtual reality-based training to improve obstacle-crossing performance and dynamic balance in patients with Parkinson’s disease. Neurorehabil Neural Repair. 2015;29:658–667. [DOI] [PubMed] [Google Scholar]
- 8. Stasieńko A, Sarzyńska-Długosz I. Virtual reality in neurorehabilitation. Adv Rehabil. 2016;30:67–75. [Google Scholar]
- 9. McGrane N, Galvin R, Cusack T, Stokes E. Addition of motivational interventions to exercise and traditional physiotherapy: a review and meta-analysis. Physiotherapy. 2015;101:1–12. [DOI] [PubMed] [Google Scholar]
- 10. Iosa M, Morone G, Fusco A, et al. Leap motion controlled videogame-based therapy for rehabilitation of elderly patients with subacute stroke: a feasibility pilot study. Top Stroke Rehabil. 2015;22:306–316. [DOI] [PubMed] [Google Scholar]
- 11. Aukstakalnis S, Blatner D. Silicon Mirage; the Art and Science of Virtual Reality. Berkeley, CA: Peachpit Press; 1992. [Google Scholar]
- 12. Massetti T, Favero FM, Menezes LDC, et al. Achievement of virtual and real objects using a short-term motor learning protocol in people with Duchenne muscular dystrophy: a crossover randomized controlled trial. Games Health J. 2018;7:107–115. [DOI] [PubMed] [Google Scholar]
- 13. Rizzo AS, Shilling R. Clinical virtual reality tools to advance the prevention, assessment, and treatment of PTSD. Eur J Psychotraumatol. 2017;8:1414560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lledo LD, Diez JA, Bertomeu-Motos A, et al. A comparative analysis of 2D and 3D tasks for virtual reality therapies based on robotic-assisted neurorehabilitation for post-stroke patients. Front Aging Neurosci. 2016;8:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fernani DCGL, Prado MTA, Fell RF, et al. Motor intervention on children with school learning difficulties. J Hum Growth Dev. 2013;23:209–214. [Google Scholar]
- 16. Ferreira Dos Santos L, Christ O, Mate K, Schmidt H, Krüger J, Dohle C. Movement visualisation in virtual reality rehabilitation of the lower limb: a systematic review. Biomed Eng Online. 2016;15:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Teo W-P, Muthalib M, Yamin S, et al. Does a combination of virtual reality, neuromodulation and neuroimaging provide a comprehensive platform for neurorehabilitation? a narrative review of the literature. Front Hum Neurosci. 2016;10:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smith JW. Immersive virtual environment technology to supplement environmental perception, preference and behavior research: a review with applications. Int J Environ Res Public Health. 2015;12:11486–11505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cameirao MS, Badia SB, Oller ED, Verschure PF. Neurorehabilitation using the virtual reality based Rehabilitation Gaming System: methodology, design, psychometrics, usability and validation. J Neuroeng Rehabil. 2010;7:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lucca LF. Virtual reality and motor rehabilitation of the upper limb after stroke: a generation of progress? J Rehabil Med. 2009;41:1003–1006. [DOI] [PubMed] [Google Scholar]
- 21. Viñas-Diz S, Sobrido-Prieto M. Realidad virtual con fines terapéuticos en pacientes con ictus: revisión sistemática. Neurología. 2016;31:255–277. [DOI] [PubMed] [Google Scholar]
- 22. Alves PDR, McClelland J, Morris M. Complementary physical therapies for movement disorders in Parkinson’s disease: a systematic review. Eur J Phys Rehabil Med 2015;51:693–704. [PubMed] [Google Scholar]
- 23. Massetti T, da Silva TD, Ribeiro DC, et al. Motor learning through virtual reality in cerebral palsy—a literature review. Med Exp. 2014;1:302–306. [Google Scholar]
- 24. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. [DOI] [PubMed] [Google Scholar]
- 25. Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. 2011;39:91–92. [DOI] [PubMed] [Google Scholar]
- 26. Panic N, Leoncini E, de Belvis G, Ricciardi W, Boccia S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS ONE. 2013;8:e83138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Massetti T, Trevizan IL, Arab C, Favero FM, Ribeiro-Papa DC, de Mello Monteiro CB. Virtual reality in multiple sclerosis—a systematic review. Mult Scler Relat Disord. 2016;8:107–112. [DOI] [PubMed] [Google Scholar]
- 28. Menezes LDC, Massetti T, Oliveira FR, et al. Motor learning and virtual reality in Down syndrome; a literature review. Int Arch Med. 2015;8:119. [Google Scholar]
- 29. Assis GA, Correa AG, Martins MB, Pedrozo WG, Lopes Rde D. An augmented reality system for upper-limb post-stroke motor rehabilitation: a feasibility study. Disabil Rehabil Assist Technol. 2016;11:521–528. [DOI] [PubMed] [Google Scholar]
- 30. Calabro RS, Naro A, Russo M, et al. The role of virtual reality in improving motor performance as revealed by EEG: a randomized clinical trial. J Neuroeng Rehabil. 2017;14:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Held JP, Ferrer B, Mainetti R, et al. Autonomous rehabilitation at stroke patients home for balance and gait: safety, usability and compliance of a virtual reality system. Eur J Phys Rehabil Med. 2018;54:545–553. [DOI] [PubMed] [Google Scholar]
- 32. Mousavi Hondori H, Khademi M, Dodakian L, McKenzie A, Lopes CV, Cramer SC. Choice of human-computer interaction mode in stroke rehabilitation. Neurorehabil Neural Repair. 2016;30:258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. House G, Burdea G, Polistico K, et al. Integrative rehabilitation of residents chronic post-stroke in skilled nursing facilities: the design and evaluation of the BrightArm Duo. Disabil Rehabil Assist Technol. 2016;11:683–694. [DOI] [PubMed] [Google Scholar]
- 34. Lin CY, Tsai CM, Shih PC, Wu HC. Development of a novel haptic glove for improving finger dexterity in poststroke rehabilitation. Technol Health Care. 2015;24:S97–S103. [DOI] [PubMed] [Google Scholar]
- 35. Mobini A, Behzadipour S, Saadat M. Test-retest reliability of Kinect’s measurements for the evaluation of upper body recovery of stroke patients. Biomed Eng Online. 2015;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. da Silva RNM, Ferraz DD, Pedreira E, et al. Virtual rehabilitation via Nintendo Wii® and conventional physical therapy effectively treat post-stroke hemiparetic patients. Top Stroke Rehabil. 2015;22:299–305. [DOI] [PubMed] [Google Scholar]
- 37. Saposnik G, Cohen LG, Mamdani M, et al. Efficacy and safety of non-immersive virtual reality exercising in stroke rehabilitation (EVREST): a randomised, multicentre, single-blind, controlled trial. Lancet Neurol. 2016;15:1019–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simkins M, Byl N, Kim H, Abrams G, Rosen J. Upper limb bilateral symmetric training with robotic assistance and clinical outcomes for stroke: a pilot study. Int J Intell Comput Cyber. 2016;9:83–104. [Google Scholar]
- 39. Steinisch M, Tana MG, Comani S. A post-stroke rehabilitation system integrating robotics, VR and high-resolution EEG imaging. IEEE T Neural Syst Rehabil Eng. 2013;21:849–859. [DOI] [PubMed] [Google Scholar]
- 40. Thielbar KO, Lord TJ, Fischer HC, et al. Training finger individuation with a mechatronic-virtual reality system leads to improved fine motor control post-stroke. J Neuroeng Rehabil. 2014;11:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Trombetta M, Bazzanello Henrique PP, Brum MR, Colussi EL, De Marchi ACB, Rieder R. Motion Rehab AVE 3D: a VR-based exergame for post-stroke rehabilitation. Comput Methods Programs Biomed. 2017;151:15–20. [DOI] [PubMed] [Google Scholar]
- 42. Verma S, Kumar D, Kumawat A, Dutta A, Lahiri U. A low-cost adaptive balance training platform for stroke patients: a usability study. IEEE T Neural Syst Rehabil Eng. 2017;25:935–944. [DOI] [PubMed] [Google Scholar]
- 43. Zoccolillo L, Morelli D, Cincotti F, et al. Video-game based therapy performed by children with cerebral palsy: a cross-over randomized controlled trial and a cross-sectional quantitative measure of physical activity. Eur J Phys Rehabil Med. 2015;51:669–676. [PubMed] [Google Scholar]
- 44. Bortone I, Leonardis D, Solazzi M, et al. Integration of serious games and wearable haptic interfaces for Neuro Rehabilitation of children with move-ment disorders: a feasibility study. IEEE Int Conf Rehabil Robot. 2017;2017:1094–1099. [DOI] [PubMed] [Google Scholar]
- 45. Keller JW, van Hedel HJA. Weight-supported training of the upper extremity in children with cerebral palsy: a motor learning study. J Neuroeng Rehabil. 2017;14:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Keller U, van Hedel HJ, Klamroth-Marganska V, Riener R. ChARMin: the first actuated exoskeleton robot for pediatric arm rehabilitation. IEEE/ASME T Mechatron. 2016;21:2201–2213. [Google Scholar]
- 47. Shokur S, Gallo S, Moioli RC, et al. Assimilation of virtual legs and perception of floor texture by complete paraplegic patients receiving artificial tactile feedback. Sci Rep. 2016;6:32293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dimbwadyo-Terrer I, Trincado-Alonso F, de Los Reyes-Guzman A, et al. Upper limb rehabilitation after spinal cord injury: a treatment based on a data glove and an immersive virtual reality environment. Disabil Rehabil Assist Technol. 2016;11:462–467. [DOI] [PubMed] [Google Scholar]
- 49. Kim A, Darakjian N, Finley JM. Walking in fully immersive virtual environments: an evaluation of potential adverse effects in older adults and individuals with Parkinson’s disease. J Neuroeng Rehabil. 2017;14:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rohani DA, Puthusserypady S. BCI inside a virtual reality classroom: a potential training tool for attention. EPJ Nonlin Biomed Phys. 2015;3:12. [Google Scholar]
- 51. Pedroli E, Padula P, Guala A, Meardi MT, Riva G, Albani G. A psychometric tool for a virtual reality rehabilitation approach for dyslexia. Comput Math Method M 2017;2017:7048676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Peruzzi A, Cereatti A, Della Croce U, Mirelman A. Effects of a virtual reality and treadmill training on gait of subjects with multiple sclerosis: a pilot study. Mult Scler Relat Disord. 2016;5:91–96. [DOI] [PubMed] [Google Scholar]
- 53. Gagnon C, Lavoie C, Lessard I, et al. The Virtual Peg Insertion Test as an assessment of upper limb coordination in ARSACS patients: a pilot study. J Neurol Sci. 2014;347:341–344. [DOI] [PubMed] [Google Scholar]
- 54. Grewe P, Kohsik A, Flentge D, et al. Learning real-life cognitive abilities in a novel 360-virtual reality supermarket: a neuropsychological study of healthy participants and patients with epilepsy. J Neuroeng Rehabil. 2013;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Dobkin BH. A rehabilitation-Internet-of-things in the home to augment motor skills and exercise training. Neurorehabil Neural Repair. 2017;31:217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fluet GG, Merians AS, Qiu Q, Rohafaza M, VanWingerden AM, Adamovich SV. Does training with traditionally presented and virtually simulated tasks elicit differing changes in object interaction kinematics in persons with upper extremity hemiparesis? Top Stroke Rehabil. 2015;22:176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Vourvopoulos A, Bermudez IBS. Motor priming in virtual reality can augment motor-imagery training efficacy in restorative brain-computer interaction: a within-subject analysis. J Neuroeng Rehabil. 2016;13:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bohil CJ, Alicea B, Biocca FA. Virtual reality in neuroscience research and therapy. Nat Rev Neurosci. 2011;12:752–762. [DOI] [PubMed] [Google Scholar]
- 59. Fordell H, Bodin K, Eklund A, Malm J. RehAtt—scanning training for neglect enhanced by multi-sensory stimulation in virtual reality. Top Stroke Rehabil. 2016;23:191–199. [DOI] [PubMed] [Google Scholar]
- 60. de Mello Monteiro CB, Massetti T, da Silva TD, et al. Transfer of motor learning from virtual to natural environments in individuals with cerebral palsy. Res Dev Disabil. 2014;35:2430–2437. [DOI] [PubMed] [Google Scholar]
- 61. Howard MC. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput Hum Behav 2017;70:317–327. [Google Scholar]
- 62. Chen Y, Fanchiang HD, Howard A. Effectiveness of virtual reality in children with cerebral palsy: a systematic review and meta-analysis of randomized controlled trials. Phys Ther. 2017;98:63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Crocetta TB, de Araújo LV, Guarnieri R, et al. Virtual reality software package for implementing motor learning and rehabilitation experiments. Virtual Real. 2018;22:199–209. [Google Scholar]
- 64. Crossley C, Fanfarelli JR, McDaniel R. User experience design considerations for healthcare games and applications. Paper presented at: IEEE International Conference on Serious Games and Applications for Health (SeGAH); May 11-13, 2016; Orlando, FL New York, NY: IEEE. [Google Scholar]
- 65. Pichierri G, Wolf P, Murer K, de Bruin ED. Cognitive and cognitive-motor interventions affecting physical functioning: a systematic review. BMC Geriatr. 2011;11:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yanovich E, Ronen O. The use of virtual reality in motor learning: a multiple pilot study review. Adv Phys Educ. 2015;5:188–193. [Google Scholar]
- 67. Lotan M, Yalon-Chamovitz S, Weiss PLT. Improving physical fitness of individuals with intellectual and developmental disability through a Virtual Reality Intervention Program. Res Dev Disabil. 2009;30:229–239. [DOI] [PubMed] [Google Scholar]
- 68. Monteiro CBD, da Silva TD, de Abreu LC, et al. Short-term motor learning through non-immersive virtual reality task in individuals with Down syndrome. BMC Neurol 2017;17:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lange BS, Requejo P, Flynn SM, et al. The potential of virtual reality and gaming to assist successful aging with disability. Phys Med Rehabil Clin N Am. 2010;21:339–356. [DOI] [PubMed] [Google Scholar]
- 70. Aminov A, Rogers JM, Middleton S, Caeyenberghs K, Wilson PH. What do randomized controlled trials say about virtual rehabilitation in stroke? a systematic literature review and meta-analysis of upper-limb and cognitive outcomes. J Neuroeng Rehabil. 2018;15:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Pulay MA. Eye-tracking and EMG supported 3D virtual reality—an integrated tool for perceptual and motor development of children with severe physical disabilities: a research concept. Stud Health Technol Inform. 2015;217:840–846. [PubMed] [Google Scholar]
- 72. Caroux L, Isbister K, Le Bigot L, Vibert N. Player-video game interaction: a systematic review of current concepts. Comput Hum Behav. 2015;48:366–381. [Google Scholar]
- 73. LaViola JJ., Jr. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000;32:47–56. [Google Scholar]
- 74. Gutierrez RO, Galan Del Rio F, Cano de la Cuerda R, Alguacil Diego IM, Gonzalez RA, Page JC. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. Neurorehabilitation. 2013;33:545–554. [DOI] [PubMed] [Google Scholar]
- 75. Morone G, Tramontano M, Iosa M, et al. The efficacy of balance training with video game-based therapy in subacute stroke patients: a randomized controlled trial. Biomed Res Int. 2014;2014:580861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Morone G, Paolucci S, Mattia D, Pichiorri F, Tramontano M, Iosa M. The 3Ts of the new millennium neurorehabilitation gym: therapy, technology, translationality. Expert Rev Med Devices. 2016;13:785–787. [DOI] [PubMed] [Google Scholar]
- 77. Basso Moro S, Bisconti S, Muthalib M, et al. A semi-immersive virtual reality incremental swing balance task activates prefrontal cortex: a functional near-infrared spectroscopy study. Neuroimage. 2014;85 Pt 1:451–460. [DOI] [PubMed] [Google Scholar]
- 78. Moro SB, Carrieri M, Avola D, et al. A novel semi-immersive virtual reality visuo-motor task activates ventrolateral prefrontal cortex: a functional near-infrared spectroscopy study. J Neural Eng. 2016;13(3):036002. [DOI] [PubMed] [Google Scholar]
- 79. Cappa P, Clerico A, Nov O, Porfiri M. Can force feedback and science learning enhance the effectiveness of neuro-rehabilitation? An experimental study on using a low-cost 3D joystick and a virtual visit to a zoo. PLoS One. 2013;8(12):e83945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Borrego A, Latorre J, Llorens R, Alcaniz M, Noe E. Feasibility of a walking virtual reality system for rehabilitation: objective and subjective parameters. J Neuroeng Rehabil. 2016;13(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Byagowi A, Mohaddes D, Moussavi Z. Design and Application of a Novel Virtual Reality Navigational Technology (VRNChair). J Exp Neurosci. 2014;8:7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Luu TP, He Y, Brown S, Nakagame S, Contreras-Vidal JL. Gait adaptation to visual kinematic perturbations using a real-time closed-loop brain-computer interface to a virtual reality avatar. J Neural Eng. 2016;13(3):036006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Pacheco TBF, Oliveira Rego IA, Campos TF, Cavalcanti F. Brain activity during a lower limb functional task in a real and virtual environment: A comparative study. NeuroRehabilitation. 2017;40(3):391-400. [DOI] [PubMed] [Google Scholar]
- 84. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]