The federal Care and Prevention in the United States (CAPUS) Demonstration Project (hereinafter, CAPUS), which is featured in this supplemental issue of Public Health Reports, highlighted how addressing social determinants of health (SDHs) could reduce morbidity and mortality from HIV infection and AIDS.1 In this commentary, we explore the rationale behind CAPUS and discuss how sustained efforts such as CAPUS could help reduce and ultimately eliminate racial/ethnic disparities in HIV/AIDS. We review growing scientific evidence documenting that interventions that address social and living conditions can be effective in reducing risks of HIV infection. We conclude that, to enhance our success in reducing morbidity and mortality from HIV/AIDS, we must understand the SDHs of HIV/AIDS, invest in efforts to dismantle the social conditions that lead to HIV/AIDS–related disparities, and strengthen the scientific evaluation of these efforts.
Disparities in HIV/AIDS
Although rates of HIV infection and AIDS and mortality of people with HIV infection declined from 2010 to 2014 in the United States, racial/ethnic disparities persist. HIV/AIDS is heavily concentrated among African American and Latino populations; African American people have higher rates of HIV/AIDS than do people of other racial/ethnic groups.2 Data from the Centers for Disease Control and Prevention revealed that, although African American people represented 12% of the US population in 2015, they accounted for 42% of all people living with HIV in 2014, 44% of all deaths from HIV/AIDS in 2014, and 43% of new HIV diagnoses in 2015. Likewise, Latino people represented 18% of the US population in 2015 but accounted for 24% of new HIV diagnoses in 2015. In 2015, 22% of all people newly diagnosed with HIV infection were aged 13-24, and African American and Latino gay and bisexual males were overrepresented in this age group. African American men who have sex with men (MSM) have the highest incidence of HIV in the United States; they accounted for 26% (10 223 of 39 782) of new HIV diagnoses in 2016.3 Racial/ethnic minority women account for a disproportionate share of diagnoses of HIV infection among women. In 2015, 61% of women newly diagnosed with HIV were African American, 19% were white, and 15% were Latino.4 Racial/ethnic health disparities exist at every step in the HIV care continuum, from HIV testing to mortality. Compared with white people, African American and Latino people are less likely to be aware of their HIV status, to begin treatment, to be retained in care, and to have their viral load suppressed.5
Social Determinants of Health
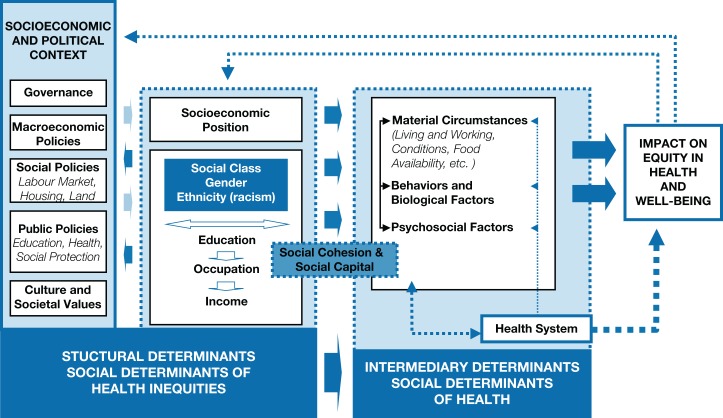
In this commentary, we use the terms health disparities and health inequities interchangeably. Although US researchers and policy makers have historically used the term disparities, the term inequities has increasingly been used to emphasize a focus on health differences that are avoidable and unjust.6 Contextual factors for disease, known generally in many disciplines as SDHs, have been conceptualized as the drivers of health for decades by many public health experts. Indeed, SDHs embody the history of public health, which has focused on improving social conditions for all.7 The SDH framework encompasses social, economic, and political systems and structural mechanisms that shape individual health-related risk behaviors (Figure).8 For example, SDHs may include access to adequate housing, access to health care and/or health insurance, access to child care and education, employment status, gender equality, and income.9 These upstream determinants help explain why race/ethnicity is associated with differential risks for disease and health outcomes.10 They also create social stratification by income, education, class, gender, and race/ethnicity, including those associated with HIV/AIDS.9
Figure.
A conceptual framework for action on the social determinants of health, 2010. Data source: World Health Organization.6 Used with permission. In this framework, structural determinants of health, including socioeconomic and political context and the person’s socioeconomic position, are considered upstream factors that influence the equity in health and well-being. Intermediary determinants of health, such as material circumstances, behaviors, and psychosocial factors, are considered downstream factors.
Although behavior, especially high-risk sexual behavior, is the final pathway to HIV/AIDS, it is closely linked to various SDHs.11-22 For example, one study found that young African American women from economically disadvantaged neighborhoods who reported a lack of food at home, homelessness, and low perceived education and employment prospects had 2.2 to 4.7 times higher odds than those without these risk factors for reporting multiple sex partners, risky sex partners (including older men and partners involved in gangs), substance use before sex, and exchange sex (ie, trading sex for goods and services).23 Other evidence indicates that poverty and other structural factors create a risk environment that is conducive to HIV transmission and suboptimal engagement in HIV care among low-income African American people living with HIV.24-30 Research also suggests that improving education and affordable housing can reduce incidence rates of HIV and AIDS because low levels of education and unstable housing have been found to decrease social stability and increase HIV risk behaviors (eg, risky sex and drug use).31-34
Most studies addressing SDHs for HIV have focused on women35,36 because of the vulnerability of many women to discriminatory social, economic, and political practices based on their sex. These studies reveal that interventions that strengthen women’s income, housing stability, and gender empowerment are associated with improved psychological well-being, economic productivity, and reduced HIV risk.36,37 Interventions that address SDHs also have improved HIV outcomes for men. For example, an intervention with MSM, the Mpowerment Project, recognized that because young gay or bisexual men engage in unsafe sex for various reasons, focusing solely on one level of risk factors (eg, individual-level factors) would omit men who engage in unsafe sex for other reasons. By using a multilevel approach, the Mpowerment Project developed community-level and individual-level capacity building and empowerment to reduce HIV-related risk behaviors in multiple communities in the United States in the 1990s.38,39 Similarly, interventions that address social and economic barriers may also lead to improvements in health. For example, for homeless and unstably housed people living with HIV, a randomized controlled trial conducted from 2004 to 2007 found that the receipt of stable housing reduced risk behavior, improved access to care, and increased adherence to medication regimens among people who received the intervention, compared with those who did not.40
Improving access to care and enhancing the quality of care can also contribute to reducing disparities in the incidence of HIV. Racial/ethnic stereotypes are deeply embedded in American culture and, whether consciously or not, can adversely affect the care that providers give to their patients.41 Interventions that address implicit bias and the cultural gaps between providers and patients can improve the quality of care and reduce racial/ethnic disparities in HIV outcomes. A 2007 study found no racial/ethnic disparities in the receipt of antiretroviral therapy, patient self-efficacy, and viral suppression when providers scored high on a novel measure of cultural competence.42 Other evidence indicates that interventions can reduce implicit and explicit bias among providers and others.43,44 The scarcity of health care providers from underrepresented racial/ethnic minority groups may also affect care. In 2012, only 3.8% of all practicing physicians were African American and 5.2% were Latino.45
Social Determinants, HIV/AIDS, and CAPUS
An emerging body of scientific evidence suggests that addressing SDHs must be an essential part of a comprehensive response to HIV/AIDS.36,46-51 Public health experts recognize that shifting the focus from one that emphasizes only behavioral change to one that emphasizes SDHs could address key structural drivers of HIV/AIDS vulnerability.36,51 A focus on SDHs could be the game changer needed to reframe the HIV/AIDS response at the national level and at last eradicate HIV/AIDS inequities. The premise of CAPUS was that all health-related behavior, including risk behaviors for HIV/AIDS, must be understood as a function of individuals within their environments, which either promote or decrease exposure to risk factors for infection.1 The higher rates of morbidity and mortality for HIV/AIDS observed among racial/ethnic minority populations are, in part, a product of social and physical conditions that underlie patterns of behavior.11-31 CAPUS focused on the idea that HIV interventions that focus narrowly on individual behavior change and/or pharmaceutical interventions cannot effectively address the magnitude and complexity of disparities in HIV.36,51 Accordingly, whenever feasible, SDHs need to be incorporated into behavioral and biomedical strategies to increase their likelihood of success, and a new generation of HIV interventions focused on the fundamental SDHs should be the centerpiece of efforts to address HIV-related disparities.
The premise of CAPUS was supported by scientific evidence indicating that policies across multiple sectors shape social conditions, which influence risk behaviors and, thus, increase vulnerability to HIV and affect population health and health equity.19,52 It is therefore important to integrate the Health in All Policies approach to have the widest impact on SDHs and population health. This approach recognizes that every aspect of government and the economy has the potential to affect health and health equity, including finance, education, housing, employment, transportation, and health.53,54
Economic studies also support the premise of CAPUS. Most interventions focused on SDHs that have been rigorously evaluated have been shown to be cost effective and to save society money in the long run.55 For example, the Mpowerment Project resulted in savings of $700 000 to $900 000 during a 5-year period. It showed that the cost of HIV prevention using a comprehensive SDH approach to HIV was much lower than the cost of lifetime medical treatment of HIV.38
Recommendations for Future Research
We recommend several priorities for future research. One recommendation is to better understand the dynamic nature of stigma and how stigmas linked to race/ethnicity (HIV itself, sexual orientation, transgender identity or expression, illicit drug use, sex work, incarceration, and immigration) can vary for the same individual across contexts and can interact with one another to affect racial/ethnic HIV-related disparities. Research also is needed to better understand how to build resilience and resistance in individuals and communities to protect them from the negative effects of these stigmas.56
A second recommendation is to better understand the extent to which SDHs can contribute to reducing the racial/ethnic inequities in initiation, uptake, and adherence to preexposure prophylaxis (PrEP) against HIV/AIDS.57-59 In one study, medical students rated black MSM patients as more likely than white MSM patients to engage in increased unprotected sex if prescribed PrEP, which, in turn, was associated with medical students’ reduced willingness to prescribe PrEP to black MSM patients.57 Future research could help identify how interventions that address SDHs can contribute to reducing racial/ethnic disparities in PrEP awareness, access, affordability, use, and provider bias.
A third recommendation is to maximize the impact of SDH interventions.60 For example, research suggests that improving housing and neighborhood quality can reduce HIV risk,36,40 but it is not clear which aspects of housing and neighborhood quality improvements lead to these reductions and the extent to which key components of comprehensive SDH interventions can be modified to achieve greater impact. Similarly, a firm empirical base is currently unavailable to determine which SDH strategies designed to reduce HIV/AIDS–related disparities are likely to have the greatest impact, which domains should be tackled first, and the extent to which features of interventions (eg, intensity and timing) can lead to differential effects. Future research should identify the relative costs and benefits of promising SDH interventions so that policy makers can fund those that are likely to have the greatest impact on HIV/AIDS.
A final recommendation, given the high risk of HIV/AIDS among MSM, is to develop and evaluate more SDH interventions for men and boys. A 2017 study of the biggest concerns of young adults (aged 18-24) in racial/ethnic minority groups who are at risk for HIV, including MSM, revealed that concerns about aggressive policing, high levels of community violence, and unstable housing led them to live with constant threat and fear, high levels of hopelessness, low perceived economic opportunity, and a desire to live in the moment given the uncertainty of the future.61 Thus, interventions are needed to develop self-esteem, job readiness, and service-learning opportunities among members of this sociodemographic group.
Public Health Implications
Addressing the SDHs of HIV has the potential to reduce the risk of other major diseases in the United States. A 2017 report from the National Academies of Sciences, Engineering, and Medicine called for multiple strategies to create sustainable financial models to promote improved population health through a focus on SDHs. These strategies included raising awareness among the public and policy makers of the magnitude of the health challenge, the availability of an evidence base, and the shared benefits that would accrue to multiple sectors of society from such investments.62
The growing recognition that health policy involves all sectors of society that have health consequences means that the health sector can work collaboratively with other sectors of society.53,54 An emerging body of evidence suggests that tackling SDHs holds great promise for making strides in reducing HIV/AIDS–related disparities.55,63 Implementing the Health in All Policies approach requires the involvement and coordination of several policy sectors to ensure policy coherence and achieve the overall objective of reducing health inequities through tackling SDHs.63 This policymaking process by various stakeholders requires representation of the perspectives and contexts of those most affected by health inequities. Thus, the engagement of civil society and affected communities in particular is necessary. The SDH framework provides direction to tackle health inequities by promoting equitable social, economic, and environmental conditions to achieve optimal health and well-being for all. With political will, this “culture of health,” where everyone has the opportunity to make choices that lead to a healthy lifestyle, is achievable.64
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Centers for Disease Control and Prevention. The Care and Prevention in the United States (CAPUS) Demonstration Project. 2016. http://www.cdc.gov/hiv/research/demonstration/capus/index.html. Accessed October 17, 2016.
- 2. Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveill Rep. 2015;27:1–114. [Google Scholar]
- 3. Centers for Disease Control and Prevention. HIV among African American gay and bisexual men. 2018. https://www.cdc.gov/hiv/group/msm/bmsm.html. Accessed June 12, 2018.
- 4. Centers for Disease Control and Prevention. HIV/AIDS, HIV by group. 2018. https://www.cdc.gov/hiv/group/index.html. Accessed July 20, 2017.
- 5. Grossman CI, Purcell DW, Rotheram-Borus MJ, Veniegas R. Opportunities for HIV combination prevention to reduce racial and ethnic health disparities. Am Psychol. 2013;68(4):237–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(suppl 1):S149–S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Irwin A, Scali E. Action on the social determinants of health: a historical perspective. Glob Public Health. 2007;2(3):235–256. [DOI] [PubMed] [Google Scholar]
- 8. Solar O, Irwin A. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2: Policy and Practice. Geneva: World Health Organization; 2010. [Google Scholar]
- 9. World Health Organization, Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. [Google Scholar]
- 10. Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1186:69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Riley ED, Neilands TB, Moore K, Cohen J, Bangsberg DR, Havlir D. Social, structural and behavioral determinants of overall health status in a cohort of homeless and unstably housed HIV-infected men. PLoS One. 2012;7(4):e35207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Milloy MJ, Marshall BD, Montaner J, Wood E. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Weiser SD, Fernandes KA, Brandson EK, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Walley AY, Cheng DM, Libman H, et al. Recent drug use, homelessness and increased short-term mortality in HIV-infected persons with alcohol problems. AIDS. 2008;22(3):415–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schwarcz SK, Hsu LC, Vittinghoff E, Vu A, Bamberger JD, Katz MH. Impact of housing on the survival of persons with AIDS. BMC Public Health. 2009;9:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lieb S, Brooks RG, Hopkins RS, et al. Predicting death from HIV/AIDS: a case-control study from Florida public HIV/AIDS clinics. J Acquir Immune Defic Syndr. 2002;30(3):351–358. [DOI] [PubMed] [Google Scholar]
- 18. Monette LE, Rourke SB, Gibson K, et al. Inequalities in determinants of health among Aboriginal and Caucasian persons living with HIV/AIDS in Ontario: results from the Positive Spaces Healthy Places study. Can J Public Health. 2011;102(3):215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galeucia M, Hirsch JS. State and local policies as a structural and modifiable determinant of HIV vulnerability among Latino migrants in the United States. Am J Public Health. 2016;106(5):800–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med. 2014;103:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Palazzolo SL, Yamanis TJ, De Jesus M, Maguire-Marshall M, Barker SL. Documentation status as a contextual determinant of HIV risk among young transgender Latinas. LGBT Health. 2016;3(2):132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Raiford JL, Herbst JH, Carry M, Browne FA, Doherty I, Wechsberg WM. Low prospects and high risk: structural determinants of health associated with sexual risk among young African American women residing in resource-poor communities in the South. Am J Community Psychol. 2014;54(3-4):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Friedman SR, Cooper HL, Osborne AH. Structural and social contexts of HIV risk among African Americans. Am J Public Health. 2009;99(6):1002–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thomas JC, Torrone E. Incarceration as forced migration: effects on selected community health outcomes. Am J Public Health. 2008;98(suppl 9):S181–S184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Walcott M, Kempf MC, Merlin JS, Turan JM. Structural community factors and sub-optimal engagement in HIV care among low-income women in the Deep South of the USA. Cult Health Sex. 2015;18(6):682–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Abbott LS, Williams CL. Influences of social determinants of health on African Americans living with HIV in the rural Southeast: a qualitative meta-synthesis. J Assoc Nurses AIDS Care. 2015;26(4):340–356. [DOI] [PubMed] [Google Scholar]
- 28. Brawner BM. A multilevel understanding of HIV/AIDS disease burden among African American women. J Obstet Gynecol Neonatal Nurs. 2014;43(5):633–643; quiz E49-E50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Davis SK, Tucker-Brown A. The effects of social determinants on black women’s HIV risk: HIV is bigger than biology. J Black Stud. 2013;44(3):273–289. [Google Scholar]
- 30. Buot ML, Docena JP, Ratemo BK, et al. Beyond race and place: distal sociological determinants of HIV disparities. PLoS One. 2014;9(4):e91711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zeglin RJ, Stein JP. Social determinants of health predict state incidence of HIV and AIDS: a short report. AIDS Care. 2014;27(2):255–259. [DOI] [PubMed] [Google Scholar]
- 32. Aidala AA, Wilson MG, Shubert V, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106(1):e1–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. German D, Latkin CA. Social stability and HIV risk behavior: evaluating the role of accumulated vulnerability. AIDS Behav. 2012;16(1):168–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: a social ecological approach to prevention and care. Am Psychol. 2013;68(4):210–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gibbs A, Willan S, Misselhorn A, Mangoma J. Combined structural interventions for gender equality and livelihood security: a critical review of the evidence from southern and eastern Africa and the implications for young people. J Int AIDS Soc. 2012;15(suppl 1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Prado G, Lightfoot M, Brown CH. Macro-level approaches to HIV prevention among ethnic minority youth: state of the science, opportunities, and challenges. Am Psychol. 2013;68(4):286–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sherman SG, German D, Cheng Y, Marks M, Bailey-Kloche M. The evaluation of the JEWEL project: an innovative economic enhancement and HIV prevention intervention study targeting drug-using women involved in prostitution. AIDS Care. 2006;18(1):1–11. [DOI] [PubMed] [Google Scholar]
- 38. Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. Am J Public Health. 1996;86(8):1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hays RB, Rebchook GM, Kegeles SM. The Mpowerment Project: community-building with young gay and bisexual men to prevent HIV1. Am J Community Psychol. 2003;31(3-4):301–312. [DOI] [PubMed] [Google Scholar]
- 40. Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503. [DOI] [PubMed] [Google Scholar]
- 41. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 42. Saha S, Korthuis PT, Cohn JA, Sharp VL, Moore RD, Beach MC. Primary care provider cultural competence and racial disparities in HIV care and outcomes. J Gen Intern Med. 2013;28(5):622–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: a prejudice habit-breaking intervention. J Exp Soc Psychol. 2012;48(6):1267–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Deville C, Hwang WT, Burgos R, Chapman CH, Both S, Thomas CR., Jr Diversity in graduate medical education in the United States by race, ethnicity, and sex, 2012. JAMA Intern Med. 2015;175(10):1706–1708. [DOI] [PubMed] [Google Scholar]
- 46. Gant Z, Lomotey M, Hall HI, Hu X, Guo X, Song R. A county-level examination of the relationship between HIV and social determinants of health: 40 states, 2006-2008. Open AIDS J. 2012;6:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cianelli R, Villegas N. Social determinants of health for HIV among Hispanic women. Hisp Health Care Int. 2016;14(1):4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(suppl 2):S132–S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–775. [DOI] [PubMed] [Google Scholar]
- 50. Ogden J, Gupta GR, Fisher WF, Warnerd A. Looking back, moving forward: towards a game-changing response to AIDS. Glob Public Health. 2011;6(suppl 3):S285–S292. [DOI] [PubMed] [Google Scholar]
- 51. Auerbach J. Transforming social structures and environments to help in HIV prevention. Health Aff (Millwood). 2009;28(6):1655–1665. [DOI] [PubMed] [Google Scholar]
- 52. Harrison KM, Dean HD. Use of data systems to address social determinants of health: a need to do more. Public Health Rep. 2011;126(suppl 3):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rudolph L, Caplan J, Ben-Moshe K, Dillon L. Health in All Policies: A Guide for State and Local Governments. Washington, DC, and Oakland, CA: American Public Health Association and Public Health Institute; 2013. [Google Scholar]
- 54. Clavier C. Implementing health in all policies—time and ideas matter too! Comment on “Understanding the role of public administration in implementing action on the social determinants of health and health inequities.” Int J Health Policy Manag. 2016;5(10):609–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Thornton RL, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff (Millwood). 2016;35(8):1416–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rucinski KB, Mensah NP, Sepkowitz KA, Cutler BH, Sweeney MM, Myers JE. Knowledge and use of pre-exposure prophylaxis among an online sample of young men who have sex with men in New York City. AIDS Behav. 2013;17(6):2180–2184. [DOI] [PubMed] [Google Scholar]
- 59. Strauss BB, Greene GJ, Phillips G, II, et al. Exploring patterns of awareness and use of HIV pre-exposure prophylaxis among young men who have sex with men. AIDS Behav. 2017;21(5):1288–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Williams DR, Purdie-Vaughns V. Social and behavioral interventions to improve health and reduce disparities in health. In: Kaplan RM, Spittel ML, David DH, eds. Population Health: Behavioral and Social Science Insights. AHRQ Publication No. 15-0002 Rockville, MD: Agency for Healthcare Research and Quality and Office of Behavioral and Social Science Research, National Institutes of Health; 2015:51–66. [Google Scholar]
- 61. Edwards LV, Lindong I, Brown L, et al. None of us will get out of here alive: the intersection of perceived risk for HIV, risk behaviors and survival expectations among African American emerging adults. J Health Care Poor Underserved. 2017;28(2S):48–68. [DOI] [PubMed] [Google Scholar]
- 62. National Academies of Sciences, Engineering, and Medicine. Building Sustainable Financial Structures for Population Health: Insights From Non-Health Sectors: Proceedings of a Workshop. Washington, DC: National Academies Press; 2017. [PubMed] [Google Scholar]
- 63. Osypuk TL, Joshi P, Geronimo K, Acevedo-Garcia D. Do social and economic policies influence health? A review. Curr Epidemiol Rep. 2014;1(3):149–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Williams DR, McClellan MB, Rivlin AM. Beyond the Affordable Care Act: achieving real improvements in Americans’ health. Health Aff (Millwood). 2010;29(8):1481–1488. [DOI] [PubMed] [Google Scholar]