Abstract
Anterior cruciate ligament (ACL) injuries are common among adolescent athletes and are rising with increased participation in higher level athletics at earlier ages. In these young patients, often with open physes, soft tissue grafts continue to be the primary graft choice for ACL reconstruction. Reinjury continues to be a concern in this high-risk age group, with failure rates 2 to 3 times higher than in adults. Recently, primary ACL reconstruction with suture tape augmentation/reinforcement has been described in both hamstring autografts and allografts. Purported advantages include protection of the graft during the revascularization and remodeling phase of incorporation. This Technical Note details a surgical technique of independent suture tape reinforcement during primary all soft tissue quadriceps tendon autograft ACL reconstruction using an all-inside technique.
Anterior cruciate ligament (ACL) injuries are common among adolescent athletes and are rising with increased participation in higher level athletics at earlier ages.1 Soft tissue grafts continue to be the primary graft choice for ACL reconstruction, especially in young patients with open physes.2, 3, 4 Reinjury continues to be a concern in this high-risk age group. Both the U.S.-based Multicenter Orthopaedic Outcomes Network and the Danish Knee Ligament Reconstruction Registry have reported graft failure rates 2 to 3 times higher in adolescents than in adults.4, 5, 6 The combined (ipsilateral or contralateral) risk of subsequent ACL injury in school-aged children returning to competitive sports is as high as 25% to 35%.7, 8, 9 Furthermore, early return to sport is predictive of second ACL tear.7
Orthopaedic surgeons must consider the biological and biomechanical aspects of graft healing for optimal results after ACL reconstruction. Recently, in an attempt to improve clinical outcomes, suture tape augmentation/reinforcement (InternalBrace; Arthrex, Naples, FL) has been described in both hamstring autografts and allografts.10, 11, 12, 13 The InternalBrace is composed of a FiberTape (Arthrex) suture, an ultrahigh-molecular-weight polyethylene/polyester tape that is collagen coated to increase tissue integration. Purported advantages include protection of the graft during the proliferation, maturation, and ligamentization phases of healing.
This Technical Note details a surgical technique of independent suture tape reinforcement during primary all soft tissue quadriceps tendon autograft ACL reconstruction using an all-inside technique. The collagen-coated suture tape is incorporated into the quadriceps autograft construct and is tensioned independently after the graft. This technique can be performed in adolescent and adult patients, including skeletally immature patients in the setting of an all-epiphyseal ACL reconstruction.
Surgical Technique
A demonstration of the technique in the right knee of an adolescent patient is provided in Video 1. The advantages and disadvantages of the procedure are presented in Table 1. The indications, pearls, and pitfalls are summarized in Table 2.
Table 1.
Advantages and Disadvantages of Suture Tape Reinforcement
| Advantages | Disadvantages |
|---|---|
|
|
Table 2.
Indications, Pearls, and Pitfalls of Suture Tape Reinforcement
| Indications | Pearls | Pitfalls |
|---|---|---|
| Isolated ACL tears and ACL tears in the setting of a multiligament injury | Use a PassPort cannula for suture management and avoiding a soft tissue bridge. | Overtensioning the FiberTape sutures |
| Adult, adolescent, and pediatric patients | Cycle the knee and tension the graft first with the knee in full extension. | Leaving the SwiveLock anchor proud, which may lead to hardware irritation |
| Tension the FiberTape sutures after the graft with the knee in full extension. | ||
| Place a hemostat under the free ends of the FiberTape to avoid overtensioning. |
ACL, anterior cruciate ligament.
Patient Positioning and Preparation
Preoperatively, the patient receives a single-shot sciatic nerve block and adductor canal nerve block with indwelling catheter. After the induction of general anesthesia, an examination under anesthesia is performed to assess knee stability and range of motion (ROM). The contralateral knee is examined for side-to-side comparison. A single dose of antibiotics is administered for infection prophylaxis. A nonsterile tourniquet is placed high on the leg and set at 225 to 250 mm Hg (the tourniquet is inflated only during the graft harvest portion of the procedure). The patient is then positioned supine with the surgical limb secured in an arthroscopic leg holder and the contralateral leg in a foam well-leg holder (Fig 1). The surgical area is prepped in standard fashion, and sterile drapes are applied.
Fig 1.
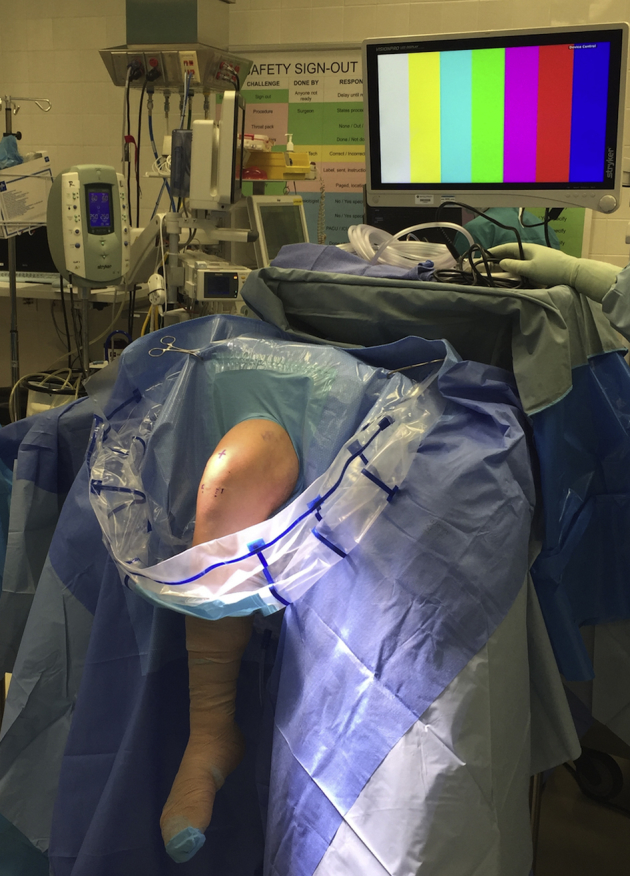
The patient is positioned supine with the surgical limb (right knee) secured in an arthroscopic leg holder and the contralateral leg in a foam well-leg holder.
Graft Harvest
Minimally invasive all soft tissue quadriceps tendon graft harvest is performed in similar fashion to the technique as described by Slone et al.14 The knee is flexed to 90° to place tension on the quadriceps and facilitate harvesting. A mixture of saline and epinephrine is injected into the skin and subcutaneous tissue to distend the tissue off the tendon. An approximately 2-cm-long vertical incision is made at the apex of the patella. Subcutaneous fat is dissected and removed proximally and distally from the incision for adequate visualization. Blunt dissection is performed to sweep tissue off of the quad tendon and anterior patella. A retractor is used to lift the skin, and the arthroscope is placed under the skin with the fluid off to visualize the width and course of the tendon (Fig 2). A mark is placed on the anterior thigh approximately 7 cm from the superior border of the patella. Next, an approximately 7-cm tendon-only graft is harvested in standard fashion using the Quad Tendon Graft Cutting Guide (Arthrex) and the Quad Tendon Stripper/Cutter (Arthrex; Fig 3). The tourniquet is let down, and bleeding is controlled with electrocautery.
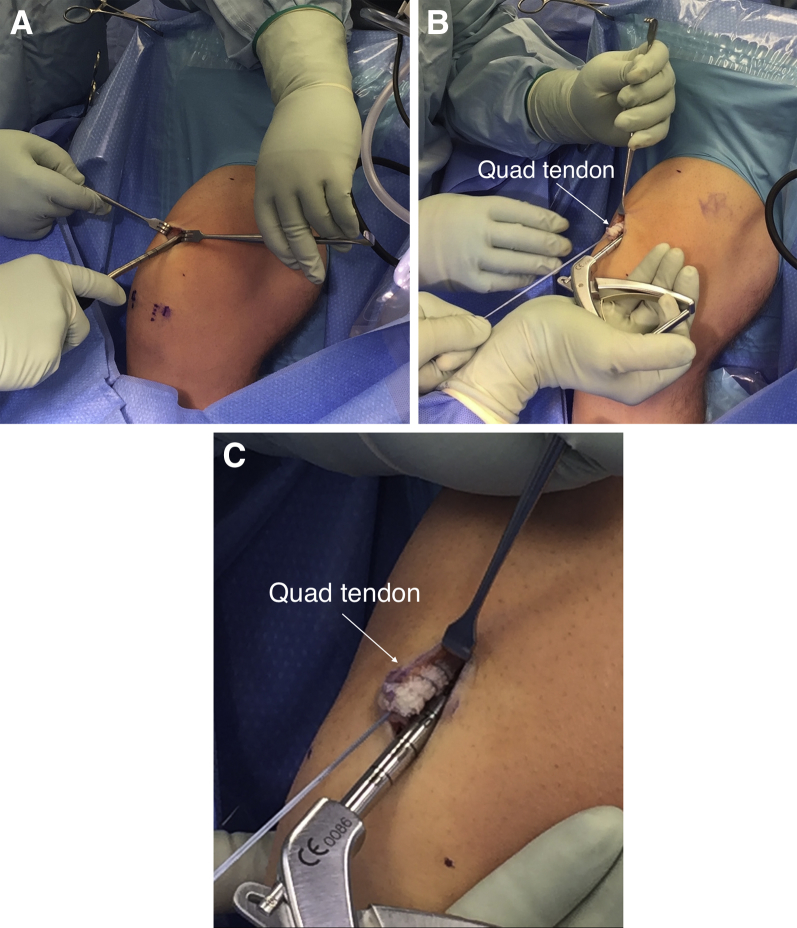
Fig 2.
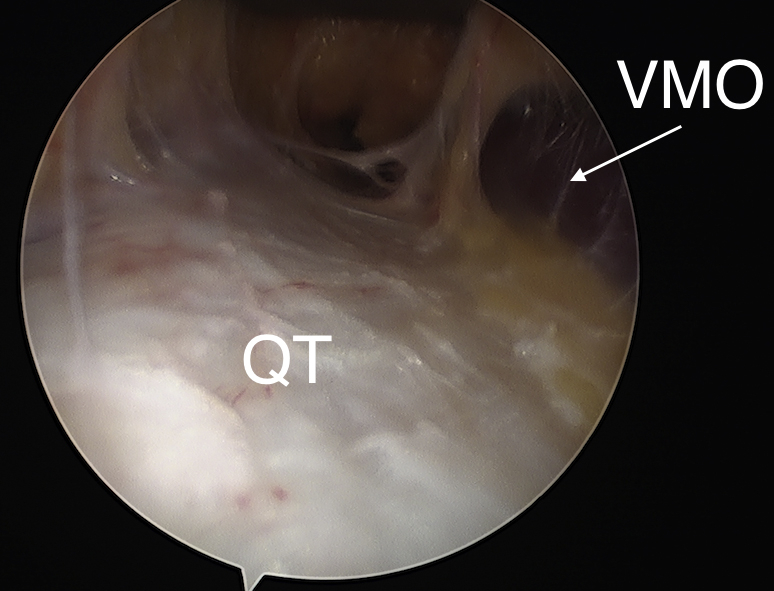
A retractor is used to lift the skin, and the arthroscope is placed under the skin with the fluid off to visualize the width and course of the quadriceps tendon (QT) (right knee). The vastus medialis oblique (VMO) is visualized medial to the tendon.
Fig 3.
An approximately 7-cm tendon-only graft is harvested in standard fashion using the Quad Tendon Graft Cutting Guide (A) and the Quad Tendon Stripper/Cutter (B and C).
Graft Preparation
The graft is taken to the back table, and the ends are prepared using a SpeedWhip ripstop technique with No. 2 FiberLoop with FiberTag Tape (Arthrex; Fig 4). A TightRope RT (Arthrex) is used on the femoral side, and a TightRope ABS (Arthrex) is used on the tibial side. The TightRope implants are secured by passing the FiberLoop suture through the loop of each implant. On the femoral side, the free FiberLoop sutures are cut and tied, and the knot is buried into the tissue. The 2 free No. 2 FiberLoop sutures on the tibial side are left in place for later backup fixation. A luggage tag–type suture with FiberWire (Arthrex) is temporarily placed at the base of the loop on the no button TightRope to protect the loop during passage.
Fig 4.
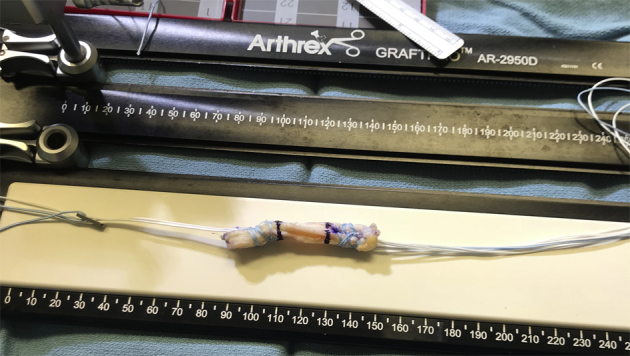
The graft is prepared using a SpeedWhip ripstop technique with No. 2 FiberLoop with FiberTag Tape. A TightRope RT is used on the femoral side, and a TightRope ABS is used on the tibial side. The TightRope implants are secured by passing the FiberLoop suture through the loop of each implant. On the femoral side, the free FiberLoop sutures are cut and tied, and the knot is buried into the tissue. The 2 free No. 2 FiberLoop sutures on the tibial side are left in place for later backup fixation.
Suture Tape Reinforcement
Reinforcement of the all-inside quadriceps graft construct is completed by using a free needle to loop a collagen-coated FiberTape suture through the button of the TightRope RT implant with the 2 free ends of the tape on the tibial side (Fig 5). The graft is pretensioned on the GraftPro (Arthrex) at 20 pounds until its use later in the procedure. It is soaked in a moist sponged soaked in vancomycin.
Fig 5.
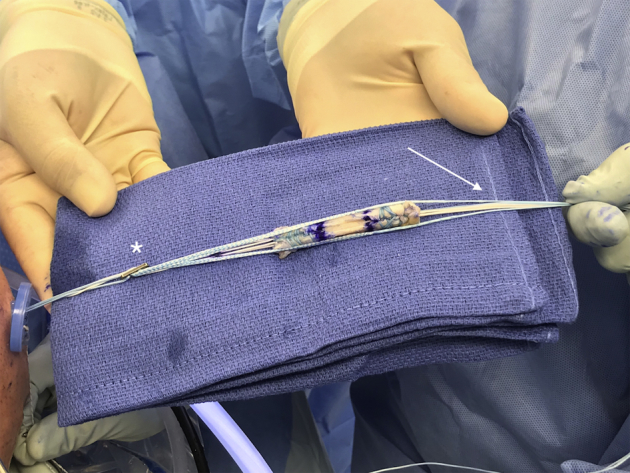
To create the ligament reinforcement construct, a FiberTape suture is looped through the button of the TightRope RT implant (asterisk) with the 2 free ends of the tape toward the tibial side of the graft (white arrow).
ACL Reconstruction
Diagnostic arthroscopy is routinely performed, and intra-articular findings are noted. Associated pathology such as meniscus tears and chondral injuries are treated. Next, the intercondylar notch is prepared. The tibial insertion site and the femoral origin of the native ACL are carefully inspected. Remnants of the native ACL on the tibia are left attached for reference. Having sized and prepared the graft on the back table, the corresponding size tunnels are drilled in the femur and tibia. The reconstruction is carried out using an arthroscopic all-inside technique with the RetroConstruction Drill Guide System (Arthrex). Using an outside-in technique and the right footprint femoral ACL guide set at 110°, a 25-mm femoral socket is created at the ACL insertion with the FlipCutter drill (Arthrex; Fig 6 A and B). Confirmation is made with the camera showing that the back wall is intact. A FiberStick (Arthrex) passing suture is passed and clamped outside the knee (Fig 6C). The same process is used for the preparation of a 30-mm tibial socket at the native ACL footprint with the tibial guide set at 60° (Fig 7). The tibia is prepared through a 2-cm vertical skin incision made over the anteromedial tibia. A PassPort (Arthrex) cannula is placed in the inferomedial portal, and the passing sutures are pulled out through the cannula to avoid a soft tissue bridge.
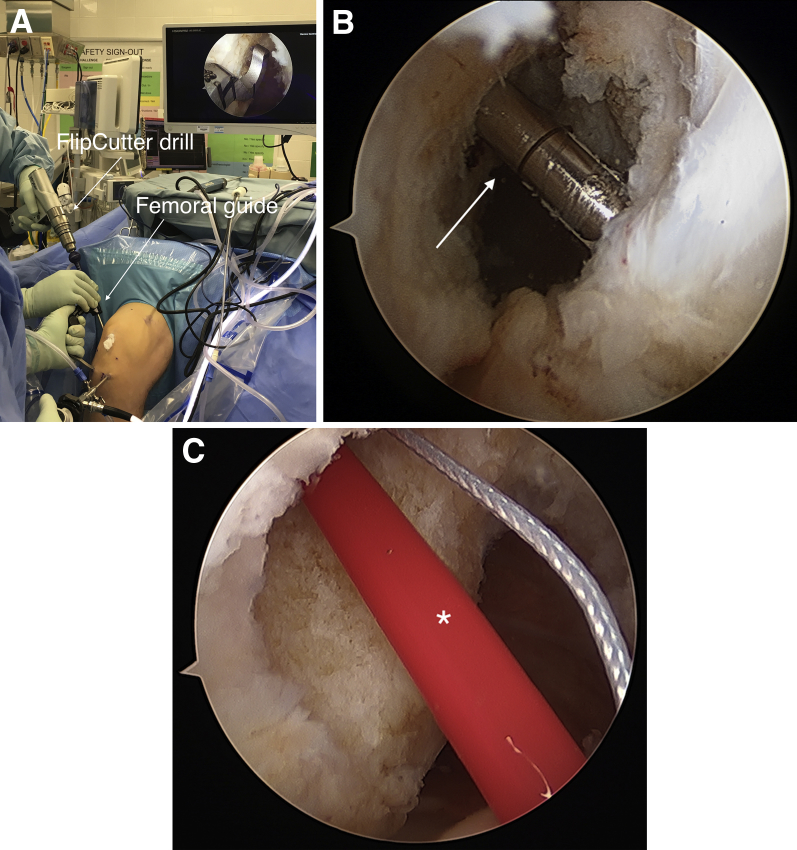
Fig 6.
(A) Using an outside-in technique and the femoral guide set at 110°, a 25-mm femoral socket is created within the native ACL footprint with the FlipCutter drill (right knee) (A). Right knee viewed from the inferomedial portal with a 30° arthroscope. The FlipCutter drill (white arrow) enters the knee within the native ACL footprint on the femur (B). A FiberStick passing suture (asterisk) is passed from outside-in through the femoral socket and clamped outside the knee (C).
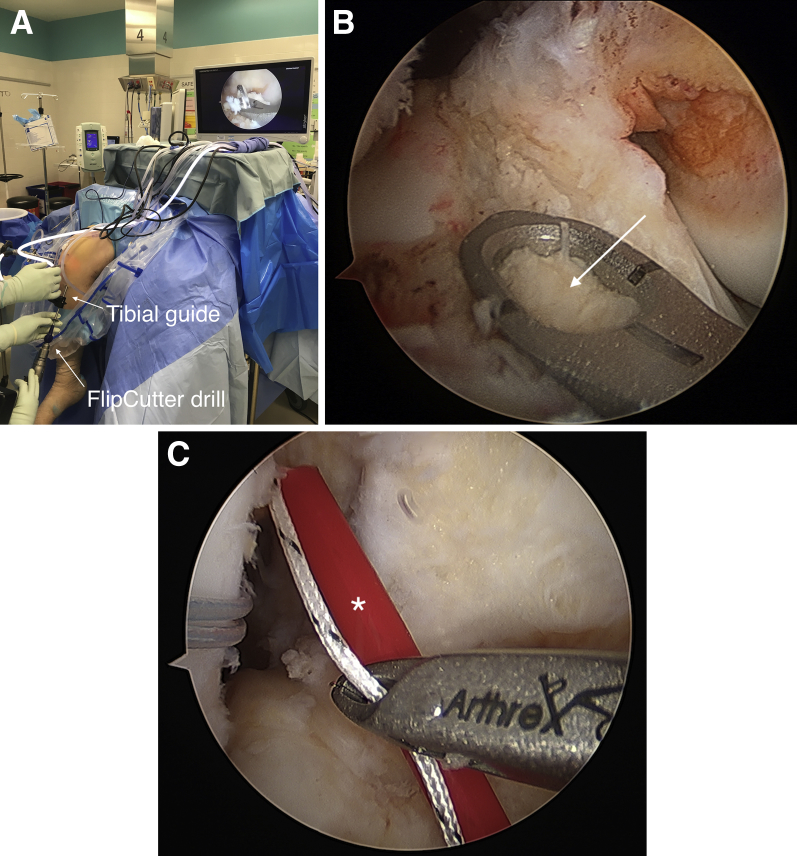
Fig 7.
Using an outside-in technique and the tibial guide set at 60°, a 30-mm tibial socket is created within the native anterior cruciate ligament footprint with the FlipCutter drill (right knee) (A). Right knee viewed from the inferomedial portal with a 30° arthroscope. The tibial guide (white arrow) is placed at the native anterior cruciate ligament footprint on the tibia (B). A TigerStick passing suture (asterisk) is passed from outside in through the tibial socket, pulled out through the PassPort cannula, and clamped outside the knee (C).
Graft Fixation
A goal of 20 mm of graft in each socket is desired. The graft is passed into the femoral socket using the TightRope RT shortening sutures, and the knee is cycled 20 times. The tibial side of the graft with the TightRope ABS, No. 2 FiberLoop sutures, and FiberTape is then advanced into the tibia. The knee is brought into full extension. An 11-mm concave ABS button (Arthrex) is applied to the TightRope ABS. The No. 2 FiberLoop backup sutures and FiberTape are also secured in the button with the FiberTape sutures situated peripherally (Fig 8). With an assistant applying a posterior drawer force, the shortening sutures from the TightRope ABS are secured to the ABS button for final fixation. The knee is cycled several times again for further tensioning, and all shortening sutures are retightened with the knee in full extension and posterior drawer force applied. The TightRope sutures on the femoral and tibial sides are tied to their respective buttons for backup fixation.15 The free No. 2 FiberLoop sutures on the tibial side are tied over the ABS button in similar fashion. The knee is examined to ensure there is a negative Lachman and negative pivot shift. The knee should easily be brought from full extension to full passive flexion, indicating no restriction from the graft. The arthroscope is then carefully placed back into the joint to inspect the graft to ensure excellent tension to probing and no impingement on the lateral wall or in full extension.
Fig 8.
With the knee in full extension, an 11-mm concave ABS button (white arrow) is applied to the TightRope ABS. The No. 2 FiberLoop backup sutures and FiberTape are also secured in the button with the FiberTape sutures situated peripherally (right knee).
Suture Tape Tensioning
Tensioning of the InternalBrace is performed independently after the graft as described by Smith and Bley.11 The ACL Backup Fixation System (Arthrex) is used to secure the FiberTape sutures on the tibia. Approximately 1.5 cm distal to the ABS button, the spade tip drill (Arthrex) is drilled into the tibia to the depth of the drill collar (20 mm). The hole is tapped twice with the 4.75-mm tap. The FiberTape sutures are passed through the eyelet of the 4.75-mm BioComposite SwiveLock (Arthrex). The anchor is pushed into the drill hole until the eyelet is fully seated. The knee is kept in full hyperextension to avoid limiting motion. To avoid stress shielding of the graft, a hemostat is placed underneath the 2 free ends of the FiberTape (Fig 9). With tension maintained on the sutures, the anchor is screwed into the tibia. The knee is checked to confirm full ROM. The arthroscope can be placed back into the joint to inspect the tension of the FiberTape sutures (Fig 10).
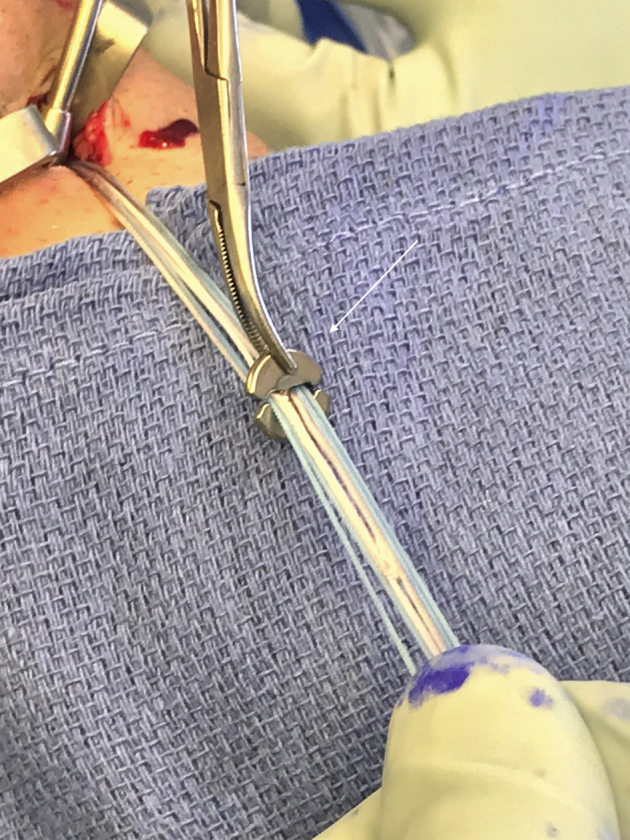
Fig 9.

Tensioning of the InternalBrace. The FiberTape sutures are passed through the eyelet of the 4.75-mm BioComposite SwiveLock. The anchor is pushed into the drill hole until the eyelet is fully seated. The knee is kept in full hyperextension to avoid limiting motion. To avoid stress shielding of the graft, a hemostat is placed underneath the 2 free ends of the FiberTape (white arrow). With tension maintained on the sutures, the anchor is screwed into the tibia.
Fig 10.
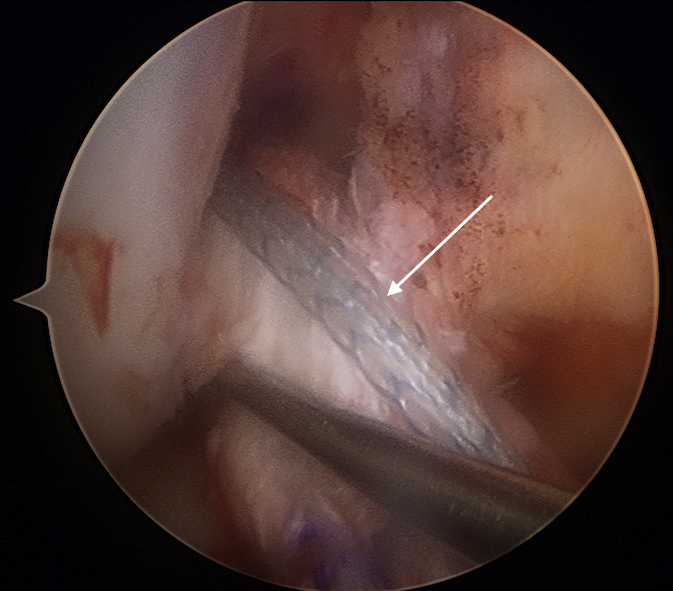
Right knee viewed from the inferomedial portal with a 30° arthroscope. The arthroscope is placed back into the joint to inspect the tension of the FiberTape sutures (white arrow). Overtensioning can lead to stiffness, loss of motion, and stress shielding of the graft, which can interfere with incorporation.
Closure
The wounds are irrigated copiously, and the knee is cleared of any loose debris. The subcutaneous layer and skin are closed in standard fashion. Sterile dressings are applied, and the leg is placed in a hinged knee brace locked in full extension.
Postoperative Protocol
Formal postoperative rehabilitation is initiated 3 to 4 days following surgery and consists of 6 separate phases. Weight bearing as tolerated is allowed immediately postoperatively in a hinged brace locked in full extension. The brace is worn during the first 6 weeks. It is kept locked in extension for the first 2 to 4 weeks. During the first week, ROM exercises are initiated and exercises to reestablish quadriceps control are begun. During phase 2, the patient works to gradually improve ROM (ideally 90° by week 4). Phase 3 goals include working to gradually restore full ROM, restoring muscular strength and balance, and enhancing neuromuscular control. Phases 4 and 5 focus on strength, power, and endurance, as well as the progression of functional activities. Track or treadmill running is not started before 4 months postop. For adolescent patients involved in pivoting sports, return to sport is allowed a minimum of 9 months after surgery on successful completion of a formal strength and functional assessment.
Discussion
This Technical Note detailed a surgical technique of suture tape reinforcement during primary quadriceps tendon autograft ACL reconstruction using an all-inside technique. An advantage of this technique is that it is a reproducible method of independent tensioning of the FiberTape sutures, thereby protecting the graft during the proliferation, maturation, and ligamentization phases of healing. It also can be used with existing all-inside ACL reconstruction techniques, including physeal-sparing reconstructions in pediatric patients. Furthermore, although described here with primary ACL reconstruction in the case of an isolated ACL injury, it can be used in the setting of multiligament knee injuries and the revision setting.
ACL injuries are common among adolescent athletes and are rising with increased participation in higher level athletics at earlier ages.1 In these young patients, often with open physes, soft tissue grafts continue to be the primary graft choice for ACL reconstruction.2, 3, 4 Re-injury continues to be a concern in this high-risk age group, with failure rates 2 to 3 times higher than in adults.4, 5, 6 Multiple factors seem to predispose the adolescent population to ACL reinjury. Morgan et al.1 showed that a third of patients younger than 19 years are at risk of further ACL graft ruptures to either knee after primary ACL reconstruction, especially in patients with a family history of ACL injury, young male patients, and those returning to cutting or pivoting sports.
Although good results after revision ACL surgery have been reported in this high-risk population, outcomes are inferior to primary reconstruction.16 Suture tape augmentation/reinforcement has been performed in an attempt to improve results after primary ACL reconstruction.10, 11, 12, 13 Interest in augmenting grafts during ACL reconstruction stems from the biomechanical and clinical success of suture augmentation in non-knee-related procedures such as Brostrom repairs17 and ulnar collateral ligament repairs in the elbow.18 Promising outcomes have also been seen in conjunction with medial knee injuries19, 20 and ACL repairs.21, 22 Recently, Bachmaier et al.23 investigated independent suture tape reinforcement of soft tissue grafts for ACL reconstruction. They biomechanically tested simulated tripled and quadrupled all-inside hamstring ACL graft constructs using bovine tendons. They found that the suture tape has synergistic load-sharing properties and functions as a protective “safety belt.” Their results showed that reinforcement with an independent suture tape led to a significant improvement in mechanical behavior of the ACL graft. The added suture tape significantly reduced elongation and higher ultimate failure load without stress shielding of the graft. Purported advantages of these findings include protection of the graft during the proliferation, maturation, and ligamentization phases of healing. Further, the suture tape reinforcement may assist in managing peak forces that occur during accelerated rehabilitation protocols or an accidental fall and reduce the risk of graft rupture.23
Some concerns with the procedure are worth noting. Nonanatomic femoral and tibial tunnel placement will result in inappropriate graft behavior during knee ROM and produce suboptimal outcomes. Although suture augmentation/reinforcement of Brostrom repairs,17 ulnar collateral ligament repairs in the elbow,18 medial knee injuries,19, 20 and ACL reconstructions23 have shown excellent biomechanical and/or clinical results, long-term clinical outcomes after ACL reconstruction are unknown. Another concern is potential overconstraint of the knee, which can occur if the FiberTape sutures are tensioned too tightly. This may result in kinematic limitations (stiffness and/or loss of motion) and cause graft or fixation failure.23 Furthermore, overtensioning may lead to stress shielding of the graft, which can interfere with incorporation. Although the suture reinforcement configuration used in this technique is similar to that of Bachmaier et al.,23 the exact biological and biomechanical consequences of suture reinforcement of human quadriceps graft ACL reconstructions are unknown.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This Technical Note details a surgical technique of independent suture tape reinforcement (InternalBrace) during primary quadriceps tendon autograft anterior cruciate ligament (ACL) reconstruction using an all-inside technique (right knee). Minimally invasive quadriceps tendon graft harvest is performed in similar fashion to the technique as described by Slone et al.14 The ends of the graft are prepared using a SpeedWhip ripstop technique with No. 2 FiberLoop with FiberTag Tape (Arthrex). A TightRope RT (Arthrex) is used on the femoral side, and a TightRope ABS (Arthrex) is used on the tibial side. To create the ACL InternalBrace construct, a FiberTape (Arthrex) suture is looped through the button of the TightRope RT implant with the 2 free ends of the tape toward the tibial side of the graft. Standard all-inside ACL reconstruction is carried out using an outside-in technique with FlipCutter drills (Arthrex). Tensioning of the FiberTape sutures is performed independently after the graft with the knee in full extension as described by Smith and Bley.11
References
- 1.Morgan M.D., Salmon L.J., Waller A., Roe J.P., Pinczewski L.A. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44:384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 2.Inacio M.C.S., Paxton E.W., Maletis G.B. Patient and surgeon characteristics associated with primary anterior cruciate ligament reconstruction graft selection. Am J Sports Med. 2012;40:339–345. doi: 10.1177/0363546511424130. [DOI] [PubMed] [Google Scholar]
- 3.Middleton K.K., Hamilton T., Irrgang J.J., Karlsson J., Harner C.D., Fu F.H. Anatomic anterior cruciate ligament (ACL) reconstruction: A global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467–1482. doi: 10.1007/s00167-014-2846-3. [DOI] [PubMed] [Google Scholar]
- 4.Fauno P., Rahr-Wagner L., Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: Results from the Danish registry of knee ligament reconstruction. Orthop J Sports Med. 2014;2(10) doi: 10.1177/2325967114552405. 2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., MOON Consortium. Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynch T.S., Parker R.D., Patel R.M. The impact of the Multicenter Orthopaedic Outcomes Network (MOON) research on anterior cruciate ligament reconstruction and orthopaedic practice. J Am Acad Orthop Surg. 2015;23:154–163. doi: 10.5435/JAAOS-D-14-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dekker T.J., Godin J.A., Dale K.M., Garrett W.E., Taylor D.C., Riboh J.C. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99:897–904. doi: 10.2106/JBJS.16.00758. [DOI] [PubMed] [Google Scholar]
- 8.Wiggins A.J., Grandhi R.K., Schneider D.K., Stanfield D., Webster K.E., Myer G.D. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webster K.E., Feller J.A., Whitehead T.S., Myer G.D., Merory P.B. Return to sport in the younger patient with anterior cruciate ligament reconstruction. Orthop J Sports Med. 2017;5(4) doi: 10.1177/2325967117703399. 2325967117703399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daggett M., Redler A., Witte K. Anterior cruciate ligament reconstruction with suture tape augmentation. Arthrosc Tech. 2018;7:e385–e389. doi: 10.1016/j.eats.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith P.A., Bley J.A. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. doi: 10.1016/j.eats.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aboalata M., Elazab A., Halawa A., Imhoff A.B., Bassiouny Y. Internal suture augmentation technique to protect the anterior cruciate ligament reconstruction graft. Arthrosc Tech. 2017;6:e1633–e1638. doi: 10.1016/j.eats.2017.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aboalata M., Elazab A., Halawa A., Ahmed M.S., Imhoff A.B., Bassiouny Y. The crossing internal suture augmentation technique to protect the all-inside anterior cruciate ligament reconstruction graft. Arthrosc Tech. 2017;6:e2235–e2240. doi: 10.1016/j.eats.2017.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slone H.S., Ashford W.B., Xerogeanes J.W. Minimally invasive quadriceps tendon harvest and graft preparation for all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1049–e1056. doi: 10.1016/j.eats.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noonan B.C., Dines J.S., Allen A.A., Altchek D.W., Bedi A. Biomechanical evaluation of an adjustable loop suspensory anterior cruciate ligament reconstruction fixation device: The value of retensioning and knot tying. Arthroscopy. 2016;32:2050–2059. doi: 10.1016/j.arthro.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Saper M., Pearce S., Shung J., Zondervan R., Ostrander R., Andrews J.R. Outcomes and return to sport after revision anterior cruciate ligament reconstruction in adolescent athletes. Orthop J Sports Med. 2018;6(4) doi: 10.1177/2325967118764884. 2325967118764884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoo J.-S., Yang E.-A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones C.M., Beason D.P., Dugas J.R. Ulnar collateral ligament reconstruction versus repair with internal bracing: Comparison of cyclic fatigue mechanics. Orthop J Sports Med. 2018;6(2) doi: 10.1177/2325967118755991. 2325967118755991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilmer B.B., Crall T., DeLong J., Kubo T., Mackay G., Jani S.S. Biomechanical analysis of internal bracing for treatment of medial knee injuries. Orthopedics. 2016;39:e532–537. doi: 10.3928/01477447-20160427-13. [DOI] [PubMed] [Google Scholar]
- 20.Lubowitz J.H., MacKay G., Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech. 2014;3:e505–508. doi: 10.1016/j.eats.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der List J.P., DiFelice G.S. Arthroscopic primary anterior cruciate ligament repair with suture augmentation. Arthrosc Tech. 2017;6:e1529–e1534. doi: 10.1016/j.eats.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tapasvi S.R., Shekhar A., Patil S.S. Primary anterior cruciate ligament repair with augmentation. Arthrosc Tech. 2018;7:e139–e145. doi: 10.1016/j.eats.2017.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bachmaier S., Smith P.A., Bley J., Wijdicks C.A. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthroscopy. 2018;34:490–499. doi: 10.1016/j.arthro.2017.10.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This Technical Note details a surgical technique of independent suture tape reinforcement (InternalBrace) during primary quadriceps tendon autograft anterior cruciate ligament (ACL) reconstruction using an all-inside technique (right knee). Minimally invasive quadriceps tendon graft harvest is performed in similar fashion to the technique as described by Slone et al.14 The ends of the graft are prepared using a SpeedWhip ripstop technique with No. 2 FiberLoop with FiberTag Tape (Arthrex). A TightRope RT (Arthrex) is used on the femoral side, and a TightRope ABS (Arthrex) is used on the tibial side. To create the ACL InternalBrace construct, a FiberTape (Arthrex) suture is looped through the button of the TightRope RT implant with the 2 free ends of the tape toward the tibial side of the graft. Standard all-inside ACL reconstruction is carried out using an outside-in technique with FlipCutter drills (Arthrex). Tensioning of the FiberTape sutures is performed independently after the graft with the knee in full extension as described by Smith and Bley.11