Abstract
Background:
The accuracy of correction has been shown to be an important determinant in long-term outcomes of patients who were treated with a medial open-wedge high tibial osteotomy (HTO) who suffer from unicompartmental osteoarthritis (OA). Computer navigation systems have the potential to improve surgical precision. The purpose of this study was to compare radiographic outcomes between patients treated with a navigation system and those treated through conventional methods of assessing alignment intra-operatively. The null hypothesis was that the method of assessing the alignment intra-operatively would make no difference in the accuracy of correction.
Methods:
In this retrospective study, 107 patients with medial varus OA who were managed by open-wedge HTO were included. Of the 107 patients, 41 were treated using an intraoperative navigation system and 66 were treated using conventional methods. Pre-operative and postoperative single-leg, long-leg standing alignment films were used to determine the extent of pre-operative varus deformity and the post-surgical correction achieved compared to the predetermined target range.
Results:
The navigational system had eight instances of software malfunction (19.5%) intraoperatively and correction was determined using the cable method. These results were analyzed as part of the conventional group. Post-operative radiographic differences were significant between the two groups. In the navigation group, 75.8% of the patients were corrected within the target range compared to 66.2% in the conventional group. More patients were also under corrected (to the point of remaining in varus) using conventional methods compared to a navigation system. There was no statistically significant difference in the degree of correction in the sagittal plane between the two groups. Regardless of the method used for checking alignment intra-operatively, there was a statistically significant difference in post-operative weight-bearing measurements when the surgeon had intra-operative axial loading versus when they did not.
Conclusion:
For coronal plane corrections, the navigation system was shown to have greater success in achieving the desired correction value and in having fewer patients who were under corrected. Despite the measurement technique a surgeon chooses to assess the accuracy of correction, axial loading the extremity in order to simulate the weight-bearing film alignment postoperatively is important to maximize the accuracy of correction needed.
Keywords: Accuracy, computer-assisted surgery, navigation, orthopedic surgery, osteotomy
Introduction
Patients who present with varus deformity of the knee are subject to progressive degenerative changes and further angular deformity [1–3]. It is well documented that medial open-wedge high tibial osteotomy (HTO) is a successful treatment in correcting the malalignment and slowing down disease progression [4–9]. The goal of surgical treatment is to shift the weight-bearing line from the medial compartment to the lateral compartment. Noyes et al. demonstrated that the weight-bearing line should be between 50 and 75% of the medial to lateral edge of the tibial plateau – where the medial edge is designated as 0% and the lateral edge as 100% – with the ideal target at 62.5% (Figure 1) [10–12]. The mechanism in achieving satisfactory outcomes is largely mechanical, therefore, accurate pre-operative assessment and technical precision are essential to achieving surgical benefits [7,13,14].
Figure 1.
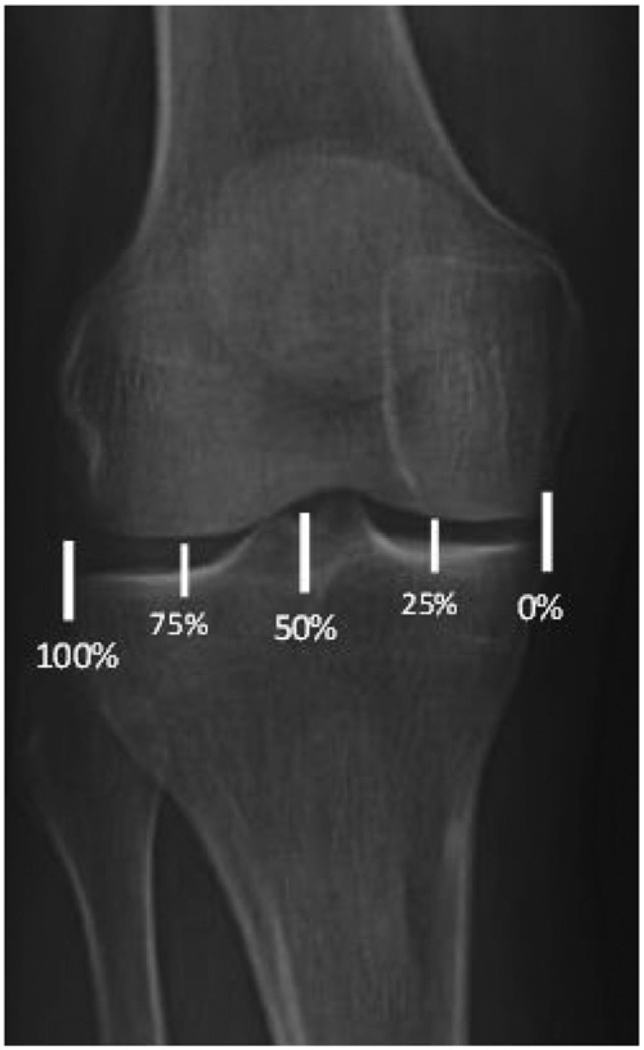
Weight-bearing alignment as described by Noyes et al. [10–12,25]. The medial edge is designated as 0% and the lateral edge as 100%. A line is drawn from the center of the femoral head to the center of the tibiotalar joint and is measured at the point where the line intersects the tibial plateau.
Conventional surgical treatments include pre-operative calculations based on long leg films and/or intra-operative fluoroscopic guidance by the cable method [10–12]. There are a number of limitations with these approaches that could lead to under- or over-correction. Suboptimal radiographs, inaccurate pre-operative calculation, and obesity can lead to intra-operative error calculating the mechanical axis.
Navigation systems are marketed to provide more precise analysis of limb alignment due to their capacity to make multi-plane measurements in real time [15–21]. The purpose of this study was to determine if a navigation system produced better post-operative long-leg weight-bearing radiographic hip to ankle alignment than conventional methods. The primary outcome parameter was the accuracy of correction on weight-bearing based single-leg, long-leg radiographic films. Secondary outcomes included radiographic tibial slope, surgery time, and the effect of end-loading the extremity intra-operatively on either measurement technique. Surgical complications including infections, delayed union, hardware removal, revision HTO, and subsequent arthroplasty within the follow-up window were noted.
Materials and methods
Subjects
This is a retrospective cohort study conducted at the University of Iowa Hospital and Clinics. A total of 153 patients underwent HTO between 2005 and 2013 and patients were included consecutively. Of which, 46 did not meet the inclusion criteria and were not included. The patients who had known clinical multi-compartmental OA, were over the age of 60 years at the time of surgery, and required concurrent surgeries such as ACL reconstruction or cartilage defect reconstruction were excluded. The patients who underwent multiple procedures were excluded because they were generally in a younger age group where concern for the longevity of the procedure requires different approaches; therefore, a neutral type of correction was usually the goal rather than the standard parameters used for the study group.
The patients were divided into two groups based on surgical procedures. There were three surgeons who exclusively used conventional methods and one surgeon who used both the methods. For the surgeon who used both methods, about half of the conventional surgeries done by the involved surgeon were done initially using conventional methods and was followed by using the navigational system. The navigational system was used not because of displeasure with using the conventional system, but intrigue by the possibility of improvement in outcomes from this difficult surgery. All surgeons were experienced in performing HTOs at the beginning of the study and surgical technique did not change throughout the study. In the navigated group, 41 patients were treated using OrthoPilot navigational system (3D HTO version 1.5, B. Braun Aesculap). In the conventional group, 66 patients were treated with conventional methods (Table 1).
Table 1.
Demographic characteristics of patients treated with medial open wedge HTOa.
| Variable | Conventional group | Navigated group |
|---|---|---|
| Subjects (n) | 74 | 33 |
| Male | 56 | 15 |
| Female | 18 | 18 |
| Age (years) | 43.3 ±8.4 | 43.5 ± 8.4 |
| BMI (kg/m2) | 33.2 ±8.0 | 33.4 ± 8.4 |
HTO: high-tibial osteotomy; BMI: body mass index.
Plus–minus values are means ± SD.
Pre-operative and post-operative assessments
Single-leg, long-leg films were obtained routinely to assess pre-operative varus deformity and the postoperative correction outcome. The patients were instructed to bear full weight on the affected leg. The weight-bearing line was expressed as a percentage previously described by Noyes et al. where the mechanical axis line from the center of the femoral head to the center of the tibiotalar joint intersects the tibial plateau [10]. Anterior-posterior and lateral views of the knee were also obtained to calculate the posterior tibial slope in the sagittal plane. The posterior tibial slope was measured as the angle between the line parallel to the anterior border of the tibia and tangent to the medial tibial plateau. Films were measured by four observers. Pre-operative and post-operative films were read sequentially and the observers were blinded to treatment group. The inter-observer and intra-observer reliability was determined with a randomized sample of 25 films. Each observer was asked to make measurements three times on the same film at different time intervals.
Operative procedures
Both the groups used the same approach and osteotomy technique for medial open wedge HTO. Intra-operative calculation of correction was different between the navigation group and the conventional group. The navigated group utilized OrthoPilot’s navigation system in determining the alignment of the weight-bearing line from hip to ankle, while the conventional group used the traditional cable method and pre-operative templates.
Regardless of the grouping of alignment method, there were two different steps utilized. First, pre-operative weight-bearing long leg films were obtained and the angles needed for correction to the target area of62.5%, but with an accepted range of 50% to 75% as described by Noyes, were calculated. Second, intraoperatively the alignment of the corrected osteotomy was determined by either a fluoroscopic visualization of an alignment rod or a cautery cord extended from the center of the hip down to the mid talar dome. The target of the anatomic landmark is a point just lateral to the tibial spine. Loading was applied with the leg in full extension while the surgeon puts approximately 15 pounds of axial load at the base of the patient’s foot. In the Orthopilot navigation system, position transmitters were placed in the femur, tibia, and foot in order to allow the surgeon to visualize the achievement of the target alignment on the computer.The navigation group utilized a navigation based protocol system to calculate the intra-operative alignment for the coronal and sagittal planes. Third, post-operatively weight-bearing long leg films were repeated once the patient was fully able to weight bear.
In this series, there was one surgeon who did not apply intra-operative axial loading (30 patients). However, weight-bearing simulation by axial loading the limb with the foot on the surgeon’s chest was performed on the majority of patients in this study regardless of the method used for assessing the adequacy of the osteotomy. For the surgeon who used the navigation system, there were also 29 patients who employed the conventional fluoroscopic method. This consisted of 29 patients who were chronologically assigned to the conventional method in this study until the surgeon began to institute use of the navigational system in the next 41 patients.
Statistical analyses
The pre-operative and follow-up data for two groups were compared. The statistical test used was paired t-test comparison, with an alpha level selected at 0.05 for significance. A sub-group analysis using t-test comparison was also performed for all the patients of the surgeon who used both methods. Linear regression and analysis of variance were calculated to determine if there was a relationship between post-operative weight bearing line and BMI. There were eight software malfunctions (19.5%) in the navigated group and the procedures were carried out by the cable method. Therefore, 31 cases were carried out using the navigational system and analyzed accordingly. The postoperative results of these patients were included in the analysis as part of the conventional group; intention-to-treat analysis was not done. Interobserver and intraobserver reliability was calculated using the IntraClass correlation formula [22]. Interobserver reliability was 0.65 and the intraobserver reliability was0.99 and may be interpreted as good and excellent, respectively [23].
Results
Radiograph results
Regarding the pre-operative weight-bearing measurements, there did not appear to be any selection bias between the two study groups. In the navigated group, the pre-operative weight bearing line passed through 24.1% ± 3% (range from 0 to 56%) coordinate at the tibial plateau (0% is consistent with the medial border and 100% is consistent with the lateral border). In the conventional group, the pre-operative weight-bearing alignment measurements passed through19.9% ± 1.7% (range from 0 to 58) and there was no statistical difference between groups (p = .23).
In the navigated group, the post-operative weight bearing line passed through 64.3% ± 12.3% (range from 41 to 100%). In the conventional group, the post-operative weight-bearing line passed through57.3% ± 15.4% (range from 12 to 86%). This resulted in a statistically significant difference (p = .011) with the navigation system yielding more accurate post-opera tive correction.
In the navigated group (Figure 2), 75.8% (25/33) of patients were corrected within the target range compared to 66.2% (49/74) in the conventional group (Figure 3). In this study, the target range was set between 50% and 75%. This meant that 18.9% (18/74) were under-corrected in the conventional group and12.1% (4/33) were under-corrected in the navigated group, remaining in unacceptable varus position (defined as the weight-bearing line falling under 50%). In the conventional group, 9.5% (7/74) of the patients were over-corrected compared to 12.1% (4/33) in the navigated group. The pre-operative posterior tibial slope was 11.7°± 0.7° (range from 5 to 22°) in the navigated group and 12.1°± 0.6° (range from 6 to 20°) in the conventional group and were not statistically different (p = .65). The post-operative posterior tibial slope was 12.2°± 0.8°(range from 2 to 28°) in the navigated group and 13.1°± 0.6°(range from 5 to 22°) in the conventional group and were not statistically significant (p = .34). Surgery duration was 172 min ±34.4 min (range from 113 to 511) in the navigation group and 115 min ±31.9 min (range from 52 min to 172 min) in the conventional group (Table 2).
Figure 2.
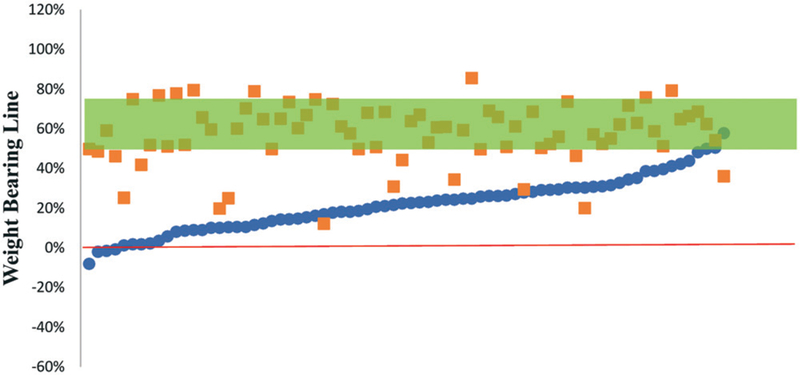
Pre- and post-operative weight-bearing line for the navigated group. Circles are pre-operative values and squares postoperative values. The bar represents the target for correction (50–75%).
Figure 3.
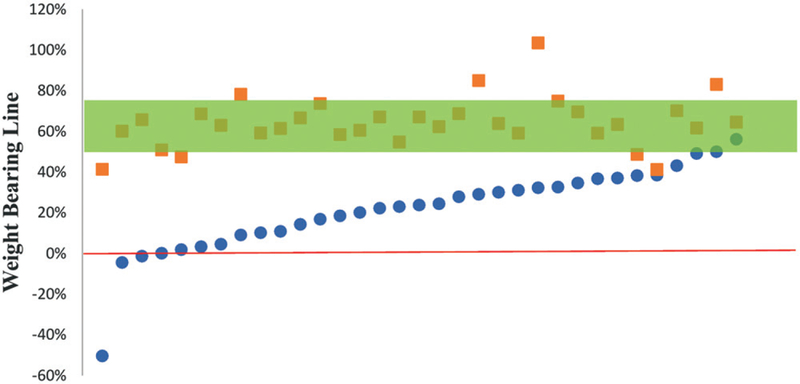
Pre- and post-operative weight-bearing line for the conventional group. Circles are pre-operative values and squares are post-operative values. The bar represents the target for correction (50–75%).
Table 2.
Post-operative radiographic and clinical results.
| Variable | Navigated group | Conventional group | p-value |
|---|---|---|---|
| Weight bearing line (%) | 64.3 ± 12.3 | 57.2 ± 15.4 | .011 |
| ΔTibial Slope (°) | 0.4 ±4.0 | 1.5 ± 4.0 | n.s. |
| Duration (min) | 172 ±34.4 | 115.6 ± 31.9 | .000 |
| Complications - no. (%) | |||
| Hardware Removal | 10 (23) | 9 (19) | |
| Surgical Site Infections | 3 (14) | 4 (10) | |
| Revisions | 2 (1) | 4 (10) | |
| Non-unions | 3 (14) | 3 (1) | |
It was obvious that the technique for axial loading during surgery did mislead the surgeon’s assessment of achieving the desired intra-operative alignment. To assess this factor, a separate analysis was carried out for intra-operative axial loading as an additional variable because it was not routinely used in all cases. Patients were divided into intra-operative axial loading versus non-loading. There were 70 patients in the loading group and 37 patients in the non-loading group. In the loading group, the average correction was 63.4% ± 12.7% (range from 25 to 103%). In the non-loading group, the average correction was50.9% ± 16.5% (range from 12 to 78%). There was a statistically significant difference between the two groups (p = .001).
To support the concept that the navigation system was superior in its ability to predict the post-operative weight-bearing film based measurements, a comparison of the surgeon who utilized both methods was performed. In the navigated group in this subset of patients, the average correction was 64.3 ± 12.3% (range from 41 to 100%). In the conventional group, the average correction was 59.2% ± 14.1% (range from 25 to 79%) and was statistically different from the navigated group (p =.041).
Using linear regression, there was no statistically significant correlation between post-operative weight bearing line and BMI. In the navigated group, there was a statistically significant correlation between BMI and surgery duration; one unit increase in BMI will result in 5.39 min longer (p < .05).
Complications
Complications at 1-year post-operation included hardware removal, surgical site infection, revision HTO, and non-union of graft. In the navigated group, there were 10 (24%) hardware removals, 3 (7%) surgical site infections, 2 (5%) revisions and 3 (7%) non-unions. Software malfunctions and the inability to use the navigation system occurred in 8 (19.5%) patients, requiring transition to conventional measurement techniques. In the conventional group, there were 9 (13%) hardware removals, 4 (6%) surgical site infections, 4 (6%) revisions and 3 (5%) non-unions.
Discussion
Medial open wedge high tibial osteotomy (HTO) is regarded as an accepted surgical option in treating patients suffering from varus deformity with medial compartment osteoarthritis. Good clinical outcomes are dependent on a variety of factors including optimal correction, age and BMI. Computer navigation systems offer a promising approach in improving correction precision when compared to conventional methods [18,24]. The majority of authors state that good correction is characterized by a post-operative weight-bearing line that intersects the knee joint line at 50–75%, with optimal correction at 62.5% [6,10]. Navigation systems offer the potential for multi-plane measurements and millimeter precision to improve accuracy and precision and decrease alignment error. These modalities provide surgeons with objective limb alignment data. Pre-operative planning is susceptible to poor pre-operative radiographs. The cable method allows intra-operative visualization of knee alignment, but it is susceptible to limb malrotation, cable tension and radiographic accuracy. The hip, knee and ankle joint centers are visualized on three separate radio-graphs intra-operatively. This makes the cable method vulnerable to positional shifts while adjusting the portable X-ray. Body habitus may also skew the correction when using the cable method.
In the present study, there is a statistically significant difference in post-operative radiographic measurements. The navigated group achieved a greater number of acceptable corrections and fewer patients were over corrected and under corrected. According to the Noyes criteria for success [11,25], almost 40% of the patients achieved suboptimal correction in the conventional group compared to just over 20% in the navigated group. Additionally, the navigated group had less variability of correction within the target zone. However, there were eight software malfunctions requiring transition to using the cable method for determining limb alignment. There was not a statistically significant change in tibial slope with either technique. With respect to posterior tibial slope, results vary among studies on the benefits of using navigational systems [15,19,26]. The navigational system used in the current study did not improve the surgeon’s ability to maintain the tibial slope. Frequently, the balls placed in the proximal tibial fragment were too loose and gave spurious results for determining the tibial slope. In these instances, fluoroscopy was used for final assessment of the tibial slope in the sagittal plane only. Conventional technique for avoiding increased tibial slope involved placing the stabilizing implants in the posterior part in all cases. Traditionally, a gap ratio of 2:1 posteromedial to anteromedial is felt to maintain native posterior tibial slope during HTO.
The navigated group had a significantly longer operation time compared to the conventional group, on average almost an hour longer. The longer operation time is likely due to the need to fasten position transmitters to the limb, technical difficulties associated with calibrating the system, and a relatively high-learning curve [27]. Experience in using the navigational system probably played a lesser role in operation time in the current study; there was little variability in operative duration when plotted over the study period (Figure 4). Obesity had a significant effect on operating time, with an increase in BMI resulted in5.4 minute longer duration. Obesity may have played a role in technical difficulties. There was difficulty placing the position markers in obese patients, especially when registering kinematic center of rotation. If the position markers were smudged during the operation, software calibration and registration were susceptible. This required frequent examination and cleaning of the markers during surgery.
Figure 4.
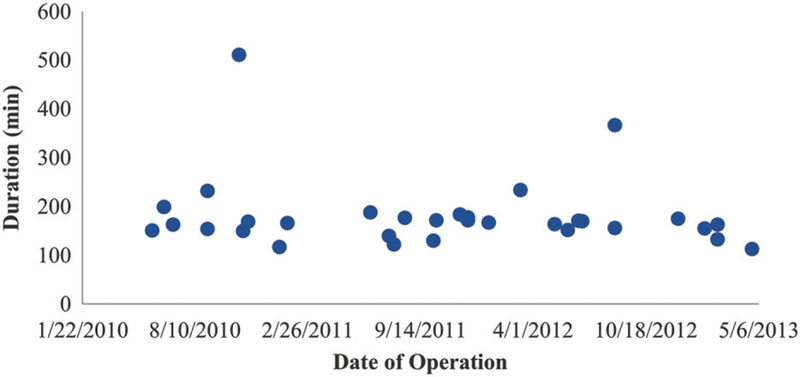
Duration of operation in the navigated group plotted over time. Each circle represents a single operation.
An additional finding revealed from this study was that intra-operative axial loading of the leg has a significant impact at the time of measurement regardless of the measurement technique (navigated versus non-navigated) used. The sub-group analysis demonstrated that the axial loading group achieved better postoperative measurements compared to the non-loading group. Ultimately, calculation of weight bearing axis was made on weight bearing X-ray. It is understandable that intra-operative axial load would increase radiographic accuracy and better represent post-operative functional joint loading [18,28].
There were four cases in the conventional group where the degree of post-operative correction was either the same or worse than pre-operative values.
In two cases, the patients suffered injury to the osteotomy site post-operatively and some correction was lost. The patients reported they were doing well prior to their injuries. The two other cases showed signs of non-union and genu varum recurred; the patients underwent revision HTO. However, the long-term clinical results of the patients corrected within the target range, is a subject of a follow-up study.
Limitations of the study
This study is a retrospective review of an institutional registry. A randomized control trial would further elucidate the relationship of navigation during HTO to radiographic outcomes. There is a possibility for operator bias in this study. Four surgeons performed this procedure using conventional methods, however only one surgeon performed the surgery using navigation. While, this surgeon performed the majority of the conventional operations as well, this may present a confounding element to the study. On the other hand, his results comparing the conventional group versus the navigation group were no different than the group results. Radiographs were examined sequentially, which may have contributed to observer bias. This was minimal because the inter- and intra-observer reliability was deemed good and excellent, respectively, and was determined from a randomized sample. There was also the potential for observers to identify drill holes on the films and identify the method used in determining alignment, but no comments were made by the observers.
Conclusion
In conclusion, computer navigation systems offer an improvement in the radiographic accuracy over the conventional fluoroscopic method in achieving targeted alignment in patients treated with medial open-wedge HTO. Also, simulation of axial loading of the extremity further improves assessment of alignment regardless of the method of intra-operative measurement. Using the navigation system resulted in fewer patients who were under-corrected as well as a larger percentage of patients corrected within the target range. However, sagittal navigational plane guidance was not effective.
Acknowledgements
We would like to thank Yubo Gao, PhD, for his contributions in statistical analysis.
Funding
No funding was provided for this project. The OrthoPilot navigational system (3D HTO version 1.5, B. Braun Aesculap) was available through a research grant from prior ACL surgery studies in cadavers. The receiver system was provided by the manufacturer. The same system with the HTO protocol was used in this study. During the course of this study, no external research support was provided
Footnotes
Disclosure statement
The authors have no conflict of interests to disclose.
References
- [1].Brouwer GM, van Tol AW, Bergink AP, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56: 1204–1211. [DOI] [PubMed] [Google Scholar]
- [2].Sharma L, Song J, Dunlop D, et al. Varus and valgus alignment and incident and progressive knee osteo-arthritis. Ann Rheum Dis 2010;69:1940–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tanamas S, Hanna FS, Cicuttini FM, et al. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61:459–467. [DOI] [PubMed] [Google Scholar]
- [4].Agneskirchner JD, Hurschler C, Wrann CD, et al. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852–861. [DOI] [PubMed] [Google Scholar]
- [5].Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010;34: 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hernigou P, Medevielle D, Debeyre J, et al. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–354. [PubMed] [Google Scholar]
- [7].Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am. 1984;66:1040–1048. [PubMed] [Google Scholar]
- [8].Mathews LS, Goldstein SA, Malvitz TA, et al. Proximal tibial osteotomy: factors that influence the duration of satisfactory function. Clin Orthop Relat Res 1988;229:193–200. [PubMed] [Google Scholar]
- [9].Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am. 2003;85-A:469–474. [PubMed] [Google Scholar]
- [10].Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofe-moral separation and tibiofemoral length. Clin Orthop Relat Res 1992;274:248–264. [PubMed] [Google Scholar]
- [11].Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282–296. [DOI] [PubMed] [Google Scholar]
- [12].Noyes FR, Mayfield W, Barber-Westin SD, et al. Opening wedge high tibial osteotomy: an operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med 2006;34:1262–1273. [DOI] [PubMed] [Google Scholar]
- [13].Amendola A, Panarella L. High tibial osteotomy for the treatment of unicompartmental arthritis of the knee. Orthop Clin North Am. 2005;36: 497–504. [DOI] [PubMed] [Google Scholar]
- [14].Franco V, Cipolla M, Gerullo G, et al. [Open wedge osteotomy of the distal femur in the valgus knee]. Orthopade. 2004;33:185–192. [DOI] [PubMed] [Google Scholar]
- [15].Akamatsu Y, Mitsugi N, Mochida Y, et al. Navigated opening wedge high tibial osteotomy improves intra-operative correction angle compared with conventional method. Knee Surg Sports Traumatol Arthrosc 2012;20:586–593. [DOI] [PubMed] [Google Scholar]
- [16].Gebhard F, Krettek C, Hufner T, et al. Reliability of computer-assisted surgery as an intraoperative ruler in navigated high tibial osteotomy. Arch Orthop Trauma Surg 2011;131:297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Heijens E, Kornherr P, Meister C. The role of navigation in high tibial osteotomy: a study of 50 patients. Orthopedics. 2009;32:40–43. [DOI] [PubMed] [Google Scholar]
- [18].Iorio R, Pagnottelli M, Vadala A, et al. Open-wedge high tibial osteotomy: comparison between manual and computer-assisted techniques. Knee Surg Sports Traumatol Arthrosc 2013;21:113–119. [DOI] [PubMed] [Google Scholar]
- [19].Kim SJ, Koh YG, Chun YM, et al. Medial opening wedge high-tibial osteotomy using a kinematic navigation system versus a conventional method: a 1-year retrospective, comparative study. Knee Surg Sports Traumatol Arthrosc 2009;17:128–134. [DOI] [PubMed] [Google Scholar]
- [20].Ribeiro CH, Severino NR, Fucs PM. Preoperative surgical planning versus navigation system in valgus tibial osteotomy: a cross-sectional study. Int Orthop (SICOT). 2013;37:1483–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Song EK, Seon JK, Park SJ, et al. Navigated open wedge high tibial osteotomy. Sports Med Arthrosc 2008;16:84–90. [DOI] [PubMed] [Google Scholar]
- [22].Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86: 420–428. [DOI] [PubMed] [Google Scholar]
- [23].Shoukri MMP, Cihon C. Statistical methods for health sciences. 2nd ed. Boca Raton (FL): CRC; 1998. [Google Scholar]
- [24].Reising K, Strohm PC, Hauschild O, et al. Computer-assisted navigation for the intraoperative assessment of lower limb alignment in high tibial osteotomy can avoid outliers compared with the conventional technique. Knee Surg Sports Traumatol Arthrosc 2013;21:181–188. [DOI] [PubMed] [Google Scholar]
- [25].Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 2005;33:378–387. [DOI] [PubMed] [Google Scholar]
- [26].Ribeiro CH, Severino NR, Moraes de Barros Fucs PM. Opening wedge high tibial osteotomy: navigation system compared to the conventional technique in a controlled clinical study. Int Orthop (SICOT). 2014;38:1627–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Picardo NE, Khan W, Johnstone D. Computer-assisted navigation in high tibial osteotomy: a systematic review of the literature. Open Orthop J 2012;6: 305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kyung BS, Kim JG, Jang KM, et al. Are navigation systems accurate enough to predict the correction angle during high tibial osteotomy? Comparison of navigation systems with 3-dimensional computed tomography and standing radiographs. Am J Sports Med 2013;41: 2368–2374. [DOI] [PubMed] [Google Scholar]


