Abstract
Objectives:
The aim of this study was to describe the proportion of acute respiratory compromise events in hospitalized pediatric patients progressing to cardiopulmonary arrest, and the clinical factors associated with progression of acute respiratory compromise to cardiopulmonary arrest. We hypothesized that failure of invasive airway placement on the first attempt (defined as multiple attempts at tracheal intubation, and/or laryngeal mask airway placement, and/or the creation of a new tracheostomy or cricothyrotomy) is independently associated with progression of acute respiratory compromise to cardiopulmonary arrest.
Design:
Multicenter, international registry of pediatric in-hospital acute respiratory compromise.
Setting:
American Heart Association’s Get with the Guidelines-Resuscitation registry (2000–2014).
Patients:
Children younger than 18 years with an index (first) acute respiratory compromise event.
Interventions:
None.
Measurements and Main Results:
Of the 2,210 index acute respiratory compromise events, 64% required controlled ventilation, 26% had return of spontaneous ventilation, and 10% progressed to cardiopulmonary arrest. There were 762 acute respiratory compromise events (34%) that did not require an invasive airway, 1,185 acute respiratory compromise events (54%) with successful invasive airway placement on the first attempt, and 263 acute respiratory compromise events (12%) with failure of invasive airway placement on the first attempt. After adjusting for confounding variables, failure of invasive airway placement on the first attempt was independently associated with progression of acute respiratory compromise to cardiopulmonary arrest (adjusted odds ratio 1.8 [95% CIs, 1.2–2.6]).
Conclusions:
More than 1 in 10 hospitalized pediatric patients who experienced an acute respiratory compromise event progressed to cardiopulmonary arrest. Failure of invasive airway placement on the first attempt is independently associated with progression of acute respiratory compromise to cardiopulmonary arrest. (Pediatr Crit Care Med 2017; XX:00–00)
Keywords: acute respiratory compromise, cardiac arrest, children, delayed airway, pediatrics
In-hospital cardiac arrest (IHCA) is a major public health burden in children and is associated with significant morbidity and mortality. Each year more than 6,000 hospitalized children in the United States suffer a cardiopulmonary arrest (CPA) requiring cardiopulmonary resuscitation (1). Although survival in children who suffer IHCA has improved over the last two decades (from 19% in 2000 to 26% in 2016), outcomes following CPA remain poor (2–4). Earlier recognition of patients at high risk for CPA is a first step to prevent CPA and improve outcomes.
Most pediatric IHCAs are due to respiratory insufficiency and/or hemodynamic instability (5, 6). In-hospital acute respiratory compromise (ARC) events, defined as “absent, agonal, or inadequate respiration requiring emergency-assisted ventilation and eliciting a hospital-wide or unit-based emergency response” can be a manifestation of many serious medical conditions associated with acute respiratory illnesses, neurologic problems, and/or circulatory shock. These respiratory crises require emergency-assisted ventilation with bag-valve-mask ventilation and/or tracheal intubation in either critical care or noncritical care areas. In adult patients, ARC events requiring tracheal intubation are associated with an increased risk of progression to CPA (7–13). Similarly, children who require emergency tracheal intubation have a markedly increased risk of progression to CPA (14, 15).
A recent publication utilized a large, multicenter, prospective U.S. registry reporting the epidemiology of pediatric in-hospital ARC to describe the overall landscape of these events and their association with in-hospital mortality (16). Building on these results, we aimed to examine the impact of invasive airway placement on progression of ARC to CPA, with the specific hypothesis that failure of invasive airway placement on the first attempt is independently associated with progression of ARC to CPA.
MATERIALS AND METHODS
Study Design and Data Source
We conducted an observational study using prospectively collected data from the Get With The Guidelines-Resuscitation (GWTG-R) registry (17). The GWTG-R is a quality improvement initiative sponsored by the American Heart Association (AHA). Participating hospitals may choose to contribute data to modules regarding IHCA (CPA), medical emergency team responses, ARC events, and postcardiac arrest care for both pediatric and adult patients. Each module has a separate database with distinct data collection forms (data collection form available at http://www.heart.org/idc/groups/heart-public/@private/@wcm/@hcm/@gwtg/documents/downloadable/ucm_457479.pdf); the pediatric ARC module alone was used in this study. Trained personnel at each participating hospital collect data for entry in to the database. Certification of data entry personnel and the use of standardized software further improve data integrity (18–21). We identified study subjects with an ARC event from patients enrolled in the AHA GWTG-R registry. At the time of this analysis, 338 hospitals participated in GWTGR and 168 provided data on pediatric ARC events. The study was presented to the Institutional Review Board at the Children’s Hospital of Philadelphia and determined exempt.
Population and Outcomes
“Acute respiratory compromise” is defined by the GWTG-R registry as “absent, agonal, or inadequate respirations that requires emergency assisted ventilation and elicits a hospital-wide or unit-based emergency response.” Emergency-assisted ventilation may include noninvasive (e.g., mouth-to-mouth, mouth-to-barrier device, bag-valve-mask, continuous positive airway pressure [CPAP], or bilevel positive airway pressure [BiPAP]) and invasive (e.g., endotracheal or tracheostomy tube, laryngeal mask airway) positive pressure ventilation. Out-of-hospital events or elective intubations are not entered in to the database.
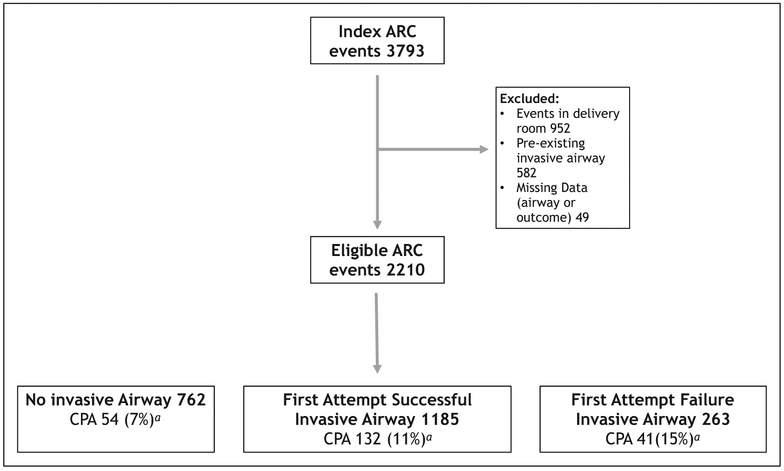
We identified index ARC events (i.e., the first ARC event during that hospitalization) in pediatric patients (age less than 18 years) enrolled in the registry from January 2000 to December 2014. We excluded events that took place in the delivery room, events in which the patient had a preexisting invasive airway, events in which we were unable to determine the respiratory support provided, and those that did not report an outcome (Fig. 1). The start of the ARC was defined by the date and time of the emergency response activation, and the end of the ARC was defined by a composite outcome of either 1) return of spontaneous ventilation (ROSV) sustained for more than 20 minutes; or 2) controlled ventilation (CV) with assisted ventilation sustained for more than 20 minutes; or 3) progression to CPA. CPA was defined as a state of pulselessness or a pulse with inadequate perfusion requiring chest compressions and/or defibrillation (in the case of ventricular fibrillation or pulseless ventricular tachycardia). Other than survival, details occurring after the ARC event ended and during the CPA event are not included in the ARC module and were not part of this analysis.
Figure 1.
Patient selection. aExcludes 11 total patients in whom acute respiratory compromise (ARC) interventions were terminated because of advanced directives (two in the No Invasive Airway group, five in the First Attempt Successful Invasive Airway Group, and four in the First Attempt Failure Invasive Airway Group). CPA = cardiopulmonary arrest.
For each ARC event, we identified patient characteristics (age, sex, race, and preexisting medical conditions), preceding clinical circumstances (interventions in place at the time of the event, location, breathing pattern, and cardiac rhythm), details of the resuscitation event (respiratory support, medications given, interventions provided), and outcome. Preexisting medical conditions are defined in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/PCC/A550). Location of the event was classified for analysis as the ICU, emergency department, general inpatient area, neonatal ICU, procedural area/operating room, and other.
Statistical Analysis
In order to assess the impact of invasive airway placement on ARC outcomes, we grouped the ARC events into three categories depending on differences in invasive airway placement. Those events that did not require invasive airway placement were classified in the “No invasive airway group” (None), those events in which an invasive airway was placed successfully on the first attempt were classified in the “First attempt successful invasive airway group” (First Success), and those events that required multiple attempts at tracheal intubation, and/or laryngeal mask airway placement, and/or the creation of a new tracheostomy or cricothyrotomy were classified in the “First attempt failure invasive airway group” (First Failure) (19). We defined our outcome groups as “ARC only” (ARC that did not progress to CPA) and “ARC to CPA” (ARC that progressed to CPA). Our primary outcome of interest was ARC progression to CPA across these three groups (None, First Success, and First Failure).
Statistical analysis was performed using SAS version 9.42 (SAS Institute, Cary, NC). We compared progression of ARC to CPA across the three groups by univariate analysis (Chi-square for categorical values or Wilcoxon rank sum for continuous variables). All factors associated with the primary outcome on univariate analysis (p < 0.1) were included in a multivariable logistic regression to analyze factors associated with ARC progression to CPA. Generalized estimating equation methods were used to account for clustering by sites. Any variable missing more than 10% of measured values was dropped from the model. Statistical significance was set at p = 0.05. Outcome, a Quintiles company, is the data collection coordination center for the AHA GWTG programs.
RESULTS
The initial data query yielded 3,793 index ARC events, of which 2,210 were analyzed after exclusion criteria were applied (Fig. 1). Ten percentage of ARC events progressed to CPA, 26% had ROSV, and 64% progressed to CV. Two-thirds of the cohort required invasive airway placement. Cardiac arrest occurred most frequently in the First Failure group. The median age of the overall cohort was 0.8 years (interquartile range, 0–5) and the majority of the patients were male (55%). Approximately one-third of ARC events occurred in the ICU, one-third in the general inpatient area, and one-sixth in the emergency department.
Supplemental Table 2 (Supplemental Digital Content 2, http://links.lww.com/PCC/A551) depicts the demographic characteristics of the subjects with an ARC event alone compared with subjects with an ARC event that progressed to CPA. Mortality was higher in those ARC patients who progressed to CPA compared with those who did not (41% vs. 13%; p < 0.0001). Hypotension preceding the ARC event as well as preexisting cardiac and noncardiac congenital malformations were more common among children with progression to CPA than those with ARC alone. Patients with ARC that progressed to CPA experienced more failure in first attempt invasive airway placement compared with those who had ARC alone (15% vs. 11%; p = 0.001).
Table 1 depicts the clinical characteristics among the three categories depending on the airway management provided: “No invasive airway group” (None), “First attempt successful invasive airway group” (First Success), and “First attempt failure invasive airway group” (First Failure). The First Failure group had 239 patients with more than one attempt at tracheal intubation, 15 patients who required laryngeal mask airway placement, and nine who underwent the creation of a new tracheostomy or cricothyrotomy during their ARC event. There were no significant differences in terms of age, gender, or race; however, there were several variables that were significantly different across the groups including an increased likelihood of no preexisting medical condition, increased events in the general inpatient area and procedural/operating area, increased apnea at the time of the ARC event, increased use of CPAP/BiPAP during the ARC event, and an increased use of a reversal agent (naloxone, flumazenil, neostigmine) during the ARC event. Hospital mortality was significantly higher among children who required invasive ventilation compared with those with no invasive airway inserted (19% First Success vs. 18% First Failure vs. 9% None; p < 0.0001).
TABLE 1.
Clinical Characteristics of the Three Airway Groupsa
| Characteristics | None (n = 762) | First Success (n = 1,185) | First Failure (n = 263) | p |
|---|---|---|---|---|
| Patient illness category, n (%) | < 0.0001 | |||
| Medical cardiac | 67 (9) | 110 (9) | 21 (8) | |
| Medical noncardiac | 451 (59) | 593 (50) | 143 (54) | |
| Surgical cardiac | 46 (6) | 101 (9) | 17 (6) | |
| Surgical noncardiac | 92 (12) | 120 (10) | 24 (9) | |
| Newborn | 94 (12) | 167 (14) | 43 (16) | |
| Obstetric | 1 (0) | 1 (0) | 1 (0) | |
| Trauma | 9 (1) | 87 (7) | 12 (5) | |
| Other or unknown | 2 (0) | 6 (1) | 2 (1) | |
| Preexisting medical conditions, n (%) | ||||
| None | 335 (49) | 356 (36) | 99 (41) | < 0.0001 |
| Acute central nervous system nonstroke event | 85 (12) | 147 (15) | 23 (9) | 0.071 |
| Acute stroke | 4 (1) | 7 (1) | 3 (1) | 0.69 |
| Acyanotic cardiac malformation | 36 (5) | 66 (7) | 16 (7) | 0.49 |
| Cyanotic cardiac malformation | 55 (8) | 90 (9) | 19 (8) | 0.71 |
| Noncardiac congenital malformation | 115 (17) | 108 (11) | 26 (11) | 0.0009 |
| Congestive heart failure | 22 (3) | 46 (5) | 9 (4) | 0.35 |
| Hypotension/hypoperfusion | 23 (3) | 97 (10) | 10 (4) | < 0.0001 |
| Major trauma | 7 (1) | 91 (9) | 12 (5) | < 0.0001 |
| Pneumonia | 50 (9) | 93 (9) | 31 (13) | 0.12 |
| Septicemia | 36 (5) | 100 (10) | 26 (11) | 0.0009 |
| Interventions already in place, n (%) | ||||
| Electrocardiogram | 479 (63) | 888 (75) | 198 (75) | < 0.0001 |
| Pulse oximeter | 566 (74) | 965 (81) | 219 (83) | 0.0002 |
| Supplemental oxygen | 326 (46) | 625 (59) | 138 (57) | < 0.0001 |
| Location of event, n (%) | <0.0001 | |||
| ICU | 90 (12) | 419 (35) | 79 (30) | |
| Emergency department | 45 (6) | 249 (21) | 63 (24) | |
| General inpatient area | 484 (64) | 317 (27) | 62 (24) | |
| Neonatal ICU | 30 (4) | 87 (7) | 36 (14) | |
| Procedural area/operating room | 79 (10) | 64 (5) | 12 (5) | |
| Other | 32 (4) | 47 (4) | 4 (2) | |
| Breathing at the time of event, n (%) | < 0.0001 | |||
| Yes | 378 (50) | 616 (52) | 156 (59) | |
| No | 236 (31) | 218 (18) | 44 (17) | |
| Agonal | 68 (9) | 137 (12) | 29 (11) | |
| Assisted noninvasive ventilation | 46 (6) | 137 (12) | 25 (10) | |
| Unknown | 34 (4) | 77 (6) | 9 (3) | |
| Hospital-wide response?, n (%) | ||||
| Yes | 539 (71) | 479 (40) | 106 (40) | < 0.0001 |
| Ventilation during event, n (%) | ||||
| Bag-valve-mask | 624 (82) | 1,050 (89) | 244 (93) | < 0.0001 |
| Continuous positive airway pressure/bilevel positive airway pressure | 250 (33) | 122 (10) | 21 (8) | < 0.0001 |
| Other noninvasive ventilation | 26 (3) | 17 (1) | 10 (4) | 0.0059 |
| Pharmacologic interventions, n (%) | ||||
| Bronchodilator | 57 (7) | 63 (5) | 19 (7) | 0.13 |
| Calcium | 9 (1) | 54 (5) | 5 (2) | < 0.0001 |
| Fluid bolus | 97 (13) | 272 (23) | 72 (27) | < 0.0001 |
| Neuromuscular blockade | 10 (1) | 580 (49) | 116 (44) | < 0.0001 |
| Reversal agent | 46 (6) | 29 (2) | 4 (2) | < 0.0001 |
| Sedative/induction agent | 61 (8) | 741 (63) | 171 (65) | < 0.0001 |
| Sodium bicarbonate | 14 (2) | 94 (8) | 15 (6) | < 0.0001 |
| Other | 122 (16) | 355 (30) | 88 (33) | < 0.0001 |
| Nonpharmacologic interventions, n (%) | ||||
| Central venous line | 6 (1) | 68 (6) | 14 (5) | < 0.0001 |
| Chest tube | 3 (0) | 17 (1) | 5 (2) | 0.049 |
| Event outcomeb, n (%) | < 0.0001 | |||
| Return of spontaneous ventilation | 531 (70) | 23 (2) | 10 (4) | |
| Controlled with assisted ventilation | 175 (23) | 1,025 (86) | 208 (79) | |
| Oardiopulmonary arrest, n (%) | 56 (7) | 137 (12) | 45 (17) | |
| Discharge disposition, n (%) | < 0.0001 | |||
| Survivor | 663 (88) | 926 (78) | 208 (80) | |
| Nonsurvivorc | 71 (9) | 230 (19) | 47 (18) |
”None” is no invasive airway required, “First Success” is successful first attempt intubation, and “First Failure” is any event that had > 1 attempt at tracheal intubation, a laryngeal mask airway placement, or the creation of a new tracheostomy or cricothyrotomy.
Excludes 11 patients with do-not-resuscitate orders.
Fifty-two patients listed as pending hospital discharge.
Table 2 depicts variables associated with progression of ARC to CPA after adjusting for confounding variables of age, race, and illness category. The model demonstrated an independent association of failure of first attempt invasive airway placement with progression of ARC to CPA (adjusted odds ratio, aOR, 1.8 [95% CIs, 1.2–2.6]). Other variables associated with increased risk for progression of ARC to CPA included female sex, location of event in the emergency department, presence of apnea and/or agonal breathing, use of assisted noninvasive ventilation prior to the start of the ARC event, lack of a hospital-wide response activation, administration of sodium bicarbonate, and central venous catheter placement. The use of CPAP/BiPAP during the ARC event, administration of a reversal agent, and location of the event on the general inpatient ward were independently associated with a decreased risk for progression of the ARC event to a CPA.
TABLE 2.
Multivariate Analysis of Variables Associated With Progression of Acute Respiratory Compromise to Cardiopulmonary Arresta
| Variables | Adjusted Odds Ratio (95% CI) | p |
|---|---|---|
| Gender | ||
| Female | 1.38 (1.03–1.85) | 0.033 |
| Event location (compared with ICU) | ||
| Emergency department | 1.67 (1.13–2.48) | 0.011 |
| General inpatient area | 0.42 (0.26–0.69) | 0.005 |
| Respiratory status at the start of event | ||
| Apnea | 2.10 (1.23–3.58) | 0.007 |
| Agonal | 1.89 (1.06–3.39) | 0.032 |
| Assisted noninvasive ventilation | 1.81 (1.27–2.58) | 0.0010 |
| Rapid response team | ||
| No hospital-wide activation | 1.83 (1.03–3.22) | 0.038 |
| Intervention during event | ||
| Continuous positive airway pressure/bilevel positive airway pressure | 0.55 (0.33–0.93) | 0.026 |
| Reversal agent | 0.30 (0.11–0.85) | 0.023 |
| Sodium bicarbonate | 2.77 (1.73–4.34) | < 0.0001 |
| Central venous line | 2.58 (1.44–4.63) | 0.0015 |
| Failure of invasive airway placement on first attempt | 1.76 (1.20–2.59) | 0.0039 |
Multivariable analysis adjusted for age, race, illness category with generalized estimating equations to account for clustering within sites.
DISCUSSION
This report describes risk factors associated with the progression of an ARC event to CPA for in-hospital pediatric patients from the AHA GWTG-R registry. More than 10% of these 2,210 children progressed from ARC to CPA during the ARC event. ARC events with failure of invasive airway placement on the first attempt were independently associated with higher risk for progression to CPA with an aOR of 1.8 (95% CI, 1.20–2.59). The use of noninvasive-assisted ventilation prior to the start of the ARC event also demonstrated an aOR of 1.8 (95% CI, 1.3–2.6) for progression to CPA.
A recent publication from the GWTG-R ARC dataset described the association of ARC with in-hospital mortality in 1,952 children who experienced an ARC event. Although the cohort had an overall mortality rate of 14.6%, the mortality rate increased to 18.6% in those patients requiring the placement of an invasive airway and to 46.2% in those patients whose ARC event progressed to CPA. After controlling for potentially confounding factors, having an unmonitored event, medical cardiac illness category, preexisting hypotension, and septicemia were all independently associated with mortality (16). However, this study did not specifically examine delay in invasive airway placement in progression of ARC to CPA.
This study adds to the growing body of literature highlighting the importance of rapidly and efficaciously securing an invasive airway for patients who experience an acute respiratory event and require definitive airway management. Numerous studies in adult patients have demonstrated that repeated attempts at tracheal intubation are associated with increased complication rates (10, 22). In a seminal study of nearly 3,000 adults, three or more attempts at tracheal intubation were associated with a 14-fold increased risk of desaturation below 70% and a seven-fold increased risk for cardiac arrest (10). Lee et al (22) examined over 3,000 pediatric tracheal intubations in PICUs using a multicenter database and observed that the risk of tracheal intubation–associated cardiac arrest increased with a greater number of intubation attempts. In our cohort, ARC events with failure of invasive airway placement on the first attempt (defined as ARC events that required more than a single attempt at endotracheal intubation, LMA placement, or tracheostomy or cricothyrotomy) were significantly associated with higher risk of progression to CPA.
In the present study, there were 173 CPA events among 1,448 ARC events in the two airway groups requiring invasive airway placement (First Success and First Failure), resulting in a cardiac arrest occurrence rate of 12%. In a prospective multicenter PICU study, tracheal intubation–associated CPA occurred in 1.7% of 5,232 tracheal intubation attempts (14). However, this prior study included stable patients intubated for elective procedures with optimal preparation, whereas the patients in our cohort were all emergently intubated for ARC, and likely represent a very different risk profile that could explain the discrepant rates of cardiac arrest.
The GWTG-R registry does not include information regarding the experience or expertise of the providers performing tracheal intubation. This is important because several pediatric studies have established the association between provider training and tracheal intubation success. Sanders et al (23) showed that both successful first attempts and overall success of tracheal intubation were lower for pediatric residents than fellows, and the incidence of adverse events associated with intubation were substantially higher among intubations by less experienced trainees. Another investigation demonstrated that only 23% of pediatric residents achieved competency in neonatal intubation, presumably because the median number of intubation opportunities for any one individual over his or her training period was three (24). Not surprisingly, the length of training time within a pediatric critical care fellowship is significantly associated with overall tracheal intubation success rate (25). These data regarding provider training and tracheal intubation success rate taken in conjunction with the increased cardiac arrest occurrence rate seen in our study as compared with previously published studies suggest that emergent tracheal intubation in the setting of an in-hospital ARC event should be regarded as a high-risk event.
Noninvasive-assisted ventilation is increasingly provided in pediatric critical care units (26, 27). In our cohort, there was an increased use of noninvasive-assisted ventilation at the start of the ARC event in patients who had progression of ARC to CPA compared with ARC alone. This also was noted in multivariable analysis, with an increased association of assisted noninvasive ventilation at the start of the ARC event (aOR, 1.8 [95% CI, 1.3–2.6]) in patients who progressed to CPA. However, CPAP and/or BiPAP was used less frequently as rescue therapy in ARC patients who progressed to CPA than in ARC patients who did not progress to CPA (10% vs. 19%; p = 0.0005). CPAP and/or BiPAP initiated “during” the ARC event was also independently associated with a lower odds ratio of progression to CPA in our multivariate regression. These retrospective associations preclude delineation of causality (i.e., whether noninvasive ventilation is protective or it is used in children with less severe respiratory distress), but represent an important area for future study.
In order for the event to meet criteria for an ARC event, patients had to require emergency-assisted ventilation and the event had to elicit a hospital-wide or unit-based emergency response. In our regression model, the lack of a hospital-wide emergency response was significantly associated with progression of ARC to CPA (aOR, 1.8 [95% CI, 1.0–3.2]). This likely represents patients who had their ARC event while in an ICU or emergency department and elicited a unit-based localized response rather than a hospital-wide response. Notably, ARC events in a general inpatient area had a lower odds ratio of progression to CPA (aOR, 0.4 [95% CI, 0.3–0.7]).
The findings of the current study should be interpreted in the context of its methodology and the limitations concerning the use of a large, multicenter database. For example, though we found that ARC events with failure of invasive airway placement on the first attempt were independently associated with higher risk for progression to CPA, most events did not include information regarding the number of attempts required to secure an airway. A dose-response effect, if present, could have provided stronger evidence to support the association. Though we have demonstrated the association between failure of invasive airway placement on the first attempt and progression to CPA, further study is needed to better understand this relationship. Limitations related to integrity and validity of data were minimized by use of standardized Utstein definitions, rigorous abstractor training, and uniform data collection. However, underreporting may exist. Selection bias may impact the data analysis performed. It is also important to note that participation in GWTG-R is voluntary and that there may be differences in care between those hospitals that choose to participate and those who do not.
CONCLUSION
More than 10% of 2,210 children with an in-hospital ARC event progressed to a cardiac arrest. Failure of invasive airway placement on the first attempt at tracheal intubation, defined as multiple attempts at tracheal intubation, and/or laryngeal mask airway placement, and/or the creation of a new tracheostomy or cricothyrotomy, is independently associated with progression of ARC to CPA.
Supplementary Material
ACKNOWLEDGMENTS
We thank the members of the pediatric Get with the Guidelines Resuscitation task force: Tia Raymond, MD, Medical City Dallas Hospital and Medical City Children’s Hospital; Alexis Topjian, MD, The Children’s Hospital of Philadelphia; Vinay Nadkarni, MD, The Children’s Hospital of Philadelphia; Amy Praestgaard, University of Pennsylvania Center for Clinical Epidemiology and Biostatistics; Emilie Allen, MSN, RN, CCRN, Parkland Health & Hospital System; Melanie Bembea, MD, MPH, Johns Hopkins University School of Medicine; Ericka Fink, MD, University of Pittsburgh School of Medicine; Elizabeth Foglia, MD, MA, The Children’s Hospital of Philadelphia; Michael Gaies, MD, MPH, University of Michigan; Anne-Marie Guerguerian, MD, PhD, The Hospital for Sick Children; Monica Kleinman, MD, Boston Children’s Hospital; Lynda Knight, RN, CCRN, CPN, Stanford Children’s Health Hospital; Peter Laussen, MBBS, Hospital for Sick Children, Toronto; Chris Parshuram, MCChB, DPhil, The Hospital for Sick Children; Taylor Sawyer, DO, MedEd, Seattle Children’s Hospital; Stephen Schexnayder, MD, Arkansas Children’s Hospital/University of Arkansas College of Medicine, Robert Sutton, MD, The Children’s Hospital of Philadelphia. We also thank Xuemei Zhang, MS, of Biostatistics & Data Management Core at The Children’s Hospital of Philadelphia for performing statistical analyses.
Supported by Russell Raphaely Endowed Chair in Critical Care Medicine, The Children’s Hospital of Philadelphia.
Footnotes
The work was completed at The Children’s Hospital of Philadelphia, Philadelphia, PA.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjournal).
Dr. Topjian’s institution received funding from the National Institutes of Health (NIH); she received support for article research from the NIH, and she received funding from expert testimony. Dr. Sutton’s institution received funding from the NIH/National Heart, Lung, and Blood Institute; he received funding from Zoll Medical Corporation and expert testimony/case reviews, and he disclosed being a member of the Pediatric Research Task Force of the American Heart Association (AHA)’s Get with the Guidelines-Resuscitation Registry. Dr. Nadkarni is a volunteer chair of AHA’s Get with the Guidelines-Resuscitation Registry, and his institution receives unrestricted research funding from Zoll Medical and Nihon Kohden. Dr. Berg is a volunteer for the AHA’s Get with the Guidelines-Resuscitation committee and has several NIH grants funding his institution for laboratory and clinical cardiopulmonary resuscitation studies, but did not receive funding for this study. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Berg RA, Nadkarni VM, Clark AE, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network: Incidence and outcomes of cardiopulmonary resuscitation in PICUs. Crit Care Med 2016; 44:798–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleinman ME, Chameides L, Schexnayder SM, et al. : Part 14: Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122:S876–S908 [DOI] [PubMed] [Google Scholar]
- 3.Girotra S, Spertus JA, Li Y, et al. ; American Heart Association Get With the Guidelines–Resuscitation Investigators: Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes 2013; 6:42–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jayaram N, Spertus JA, Nadkarni V, et al. ; American Heart Association’s Get with the Guidelines-Resuscitation Investigators: Hospital variation in survival after pediatric in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes 2014; 7:517–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tibballs J, Kinney S: A prospective study of outcome of in-patient paediatric cardiopulmonary arrest. Resuscitation 2006; 71:310–318 [DOI] [PubMed] [Google Scholar]
- 6.Nadkarni VM, Larkin GL, Peberdy MA, et al. ; National Registry of Cardiopulmonary Resuscitation Investigators: First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 2006; 295:50–57 [DOI] [PubMed] [Google Scholar]
- 7.Mort TC: The incidence and risk factors for cardiac arrest during emergency tracheal intubation: A justification for incorporating the ASA Guidelines in the remote location. J Clin Anesth 2004; 16:508–516 [DOI] [PubMed] [Google Scholar]
- 8.Schwartz DE, Matthay MA, Cohen NH: Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology 1995; 82:367–376 [DOI] [PubMed] [Google Scholar]
- 9.De Jong A, Molinari N, Terzi N, et al. ; AzuRéa Network for the Frida-Réa Study Group: Early identification of patients at risk for difficult intubation in the intensive care unit: Development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med 2013; 187:832–839 [DOI] [PubMed] [Google Scholar]
- 10.Mort TC: Emergency tracheal intubation: Complications associated with repeated laryngoscopic attempts. Anesth Analg 2004; 99:607–613, table of contents [DOI] [PubMed] [Google Scholar]
- 11.Heffner AC, Swords DS, Neale MN, et al. : Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation 2013; 84:1500–1504 [DOI] [PubMed] [Google Scholar]
- 12.Kim WY, Kwak MK, Ko BS, et al. : Factors associated with the occur-rence of cardiac arrest after emergency tracheal intubation in the emergency department. PLoS One 2014; 9:e112779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaber S, Amraoui J, Lefrant JY, et al. : Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit Care Med 2006; 34:2355–2361 [DOI] [PubMed] [Google Scholar]
- 14.Shiima Y, Berg RA, Bogner HR, et al. ; National Emergency Airway Registry for Children Investigators: Cardiac arrests associated with tracheal intubations in PICUs: A multicenter cohort study. Crit Care Med 2016; 44:1675–1682 [DOI] [PubMed] [Google Scholar]
- 15.Nishisaki A, Ferry S, Colborn S, et al. ; National Emergency Airway Registry (NEAR); National Emergency Airway Registry for kids (NEAR4KIDS) Investigators: Characterization of tracheal intubation process of care and safety outcomes in a tertiary pediatric intensive care unit. Pediatr Crit Care Med 2012; 13:e5–10 [DOI] [PubMed] [Google Scholar]
- 16.Andersen LW, Vognsen M, Topjian A, et al. Pediatric in-hospital acute respiratory compromise: A report from the American Heart Association’s Get With the Guidelines-Resuscitation Registry. Pediatr Crit Care Med 2017. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The American Heart Association: Get With The Guidelines Resuscitation web page, 2016. Available at: http://www.heart.org/idc/groups/heart-public/@private/@wcm/@hcm/@gwtg/documents/downloadable/ucm_457479.pdf. Accessed November 1, 2016
- 18.Peberdy MA, Kaye W, Ornato JP, et al. : Cardiopulmonary resuscitation of adults in the hospital: A report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2003; 58:297–308 [DOI] [PubMed] [Google Scholar]
- 19.Wang HE, Abella BS, Callaway CW; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators: Risk of cardiopulmonary arrest after acute respiratory compromise in hospitalized patients. Resuscitation 2008; 79:234–240 [DOI] [PubMed] [Google Scholar]
- 20.Zaritsky A, Nadkarni V, Hazinski MF, et al. : Recommended guidelines for uniform reporting of pediatric advanced life support: The Pediatric Utstein Style. A statement for healthcare professionals from a task force of the American Academy of Pediatrics, the American Heart Association, and the European Resuscitation Council. Resuscitation 1995; 30:95–115 [DOI] [PubMed] [Google Scholar]
- 21.Jacobs I, Nadkarni V, Bahr J, et al. ; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes: Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004; 110:3385–3397 [DOI] [PubMed] [Google Scholar]
- 22.Lee JH, Turner DA, Kamat P, et al. ; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI); National Emergency Airway Registry for Children (NEAR4KIDS): The number of tracheal intubation attempts matters! A prospective multi-institutional pediatric observational study. BMC Pediatr 2016; 16:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanders RC Jr, Giuliano JS Jr, Sullivan JE, et al. ; National Emergency Airway Registry for Children Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network: Level of trainee and tracheal intubation outcomes. Pediatrics 2013; 131:e821–e828 [DOI] [PubMed] [Google Scholar]
- 24.DeMeo SD, Katakam L, Goldberg RN, et al. : Predicting neonatal intubation competency in trainees. Pediatrics 2015; 135:e1229–e1236 [DOI] [PubMed] [Google Scholar]
- 25.Ishizuka M, Rangarajan V, Sawyer TL, et al. ; National Emergency Airway Registry for Children Investigators and Pediatric Acute Lung Injury and Sepsis Investigators Network: The development of tracheal intubation proficiency outside the operating suite during pediatric critical care medicine fellowship training: A retrospective cohort study using cumulative sum analysis. Pediatr Crit Care Med 2016; 17:e309–e316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marohn K, Panisello JM: Noninvasive ventilation in pediatric intensive care. Curr Opin Pediatr 2013; 25:290–296 [DOI] [PubMed] [Google Scholar]
- 27.Yaman A, Kendirli T, Ödek Ç, et al. : Efficacy of noninvasive mechanical ventilation in prevention of intubation and reintubation in the pediatric intensive care unit. J Crit Care 2016; 32:175–181 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.