Abstract
Background:
Use of more effective contraception may lead to less condom use and increased incidence of sexually transmitted infection.
Objective:
The objective of this study was to compare changes in condom use and incidence of sexually transmitted infection acquisition among new initiators of long-acting reversible contraceptives to those initiating non-long acting reversible contraceptive methods.
Study Design:
This is a secondary analysis of the Contraceptive CHOICE Project. We included two sample populations of 12-month continuous contraceptive users. The first included users with complete condom data (baseline, 3, 6, and 12 months) (long-acting reversible contraceptive users: n=2371; other methods: n=575). The second included users with 12-month sexually transmitted infection data (long-acting reversible contraceptive users: n=2102; other methods: n=592). Self-reported condom use was assessed at baseline and at 3, 6, and 12 months following enrollment. Changes in condom use and incident sexually transmitted infection rates were compared using chi-square tests. Risk factors for sexually transmitted infection acquisition were identified using multivariable logistic regression.
Results:
Few participants in either group reported consistent condom use across all survey time points and with all partners (long-acting reversible contraceptive users: 5.2%; other methods: 11.3%, P<0.001). There was no difference in change of condom use at 3, 6 and 12 months compared to baseline condom use regardless of method type (p=0.65). A total of 94 incident sexually transmitted infections were documented, with long-acting reversible contraceptive users accounting for a higher proportion (3.9% vs. 2.0%; P=0.03). Initiation of a long-acting reversible contraceptive method was associated with increased sexually transmitted infection incidence (OR 2.0, 95% CI: 1.07, 3.72).
Conclusions:
Long-acting reversible contraceptive initiators reported lower rates of consistent condom use, but did not demonstrate a change in condom use when compared to pre-initiation behaviors. Long-acting reversible contraceptive users were more likely to acquire a sexually transmitted infection in the 12 months following initiation.
Keywords: Sexually transmitted infection, long-acting reversible contraception, LARC
Summary
Changes in condom use behavior was not different between women initiating LARC and women initiating non-LARC methods; however, the risk of incident STI was increased.
Introduction
Long acting reversible contraceptives (LARCs) are the most effective reversible methods of pregnancy prevention (1), however they do not provide protection against sexually transmitted infections (STIs) (2–6). Barrier methods, such as condoms, are the most effective method for STI prevention (2, 7), but have a typical use contraceptive failure rate of 15–17% (8, 9). Clinicians have long recommended dual protection with an effective contraceptive method along with condom use. Poor adherence to these recommendations poses a challenge to reliable prevention of both STIs and pregnancy (5–7, 10, 11). Several studies have suggested that rates of dualmethod use among LARC users is lower than among users of other short acting reversible methods (10, 12–15). Available literature indicates that across women of all reproductive ages, there is low adherence to dual-method use (6, 10). Studies evaluating factors associated with higher rates of dual-method compliance have shown age (5), race, and number of sexual partners (15), but not necessarily contraceptive method to be associated (16) with dual use. Most studies, however, have not specifically compared LARC to non-LARC users.
Varying risk perception (5, 15), partner discordance in condom preference (15), intermittent or partner specific condom use (5, 6, 13), and potential social desirability and recall bias (2, 10, 12) make accurate assessment of condom use difficult. Additionally, few studies specifically evaluate the correlation between reported changes in condom use and acquisition of STIs.
The objective of this analysis was to examine the change in condom use in women initiating LARC methods versus those initiating non-LARC methods, as well as to evaluate rates of incident STI in women initiating LARC and non-LARC methods. We hypothesized that there would be no difference in condom use behavior or incident STIs in women initiated LARC or non-LARC methods.
Materials and Methods
This is a secondary analysis of the Contraceptive CHOICE Project, a prospective cohort study in which 9,256 women were offered the contraceptive method of their choice at no cost for two to three years. Full details of this study have been previously published (17). This analysis includes two distinct populations of participants that chose a method and continued using that method through 12-months (Figure 1). To evaluate changes in condom use behaviors, we included all participants who provided complete data (baseline, 3, 6 and 12 month surveys) on condom use (N=2946). Condom use behaviors were collected through a series of questions. Participants were first asked to identify their current number of sexual partners, and if they had multiple partners, they were asked each question as it related to the main partner as well as their additional partner(s). Specifically, participants were asked “Since the last time we spoke, when you had vaginal or anal sex with your main (other) partner, how often did you use condoms?” Response options included every time, almost every time, sometimes, almost never, and never. The reason for condom use was also assessed by asking participants if condom use was for pregnancy prevention and/or STI prevention.
Figure 1:
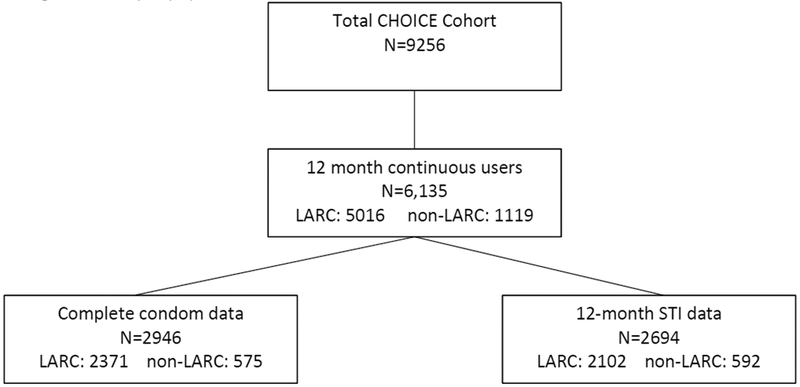
Analytic population
To assess the impact of method on incident acquisition, we included all participants for whom STI testing results were available during the 12-month reference period (N=2694). The CHOICE Project provided STI screening on an annual basis as well as any time a participant requested screening secondary to perceived exposure, or if they reported symptoms of infection. In addition to any testing that was completed at the research center, possible diagnosis and treatment at other facilities were captured at each survey point. STIs were identified using nucleic acid amplification testing from self-collected swabs sent to each participant annually or in clinic collection (self-collected or clinician collected). STI testing included Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomomonas vaginalis. Any reported or documented positive test was considered an incident infection.
The primary objective of this analysis is to evaluate the impact of method choice on condom use behaviors. Secondarily, we compare incident STI rates between LARC and non-LARC initiators over a 12-month period. Demographic characteristics of the two cohorts are presented as means and standard deviations, or frequencies and percentages based on the data type. Student t-test or chi-square tests were performed to examine the differences in subjects’ characteristics between LARC and non-LARC users. Frequency of incident STI was calculated for LARC and non-LARC and compared using chi-square test. Condom use behaviors with both main partner and additional partners were evaluated at baseline, 3, 6, and 12 months. If participants reported different frequency of condom use with main partner versus other partners, the least frequent response was used. Changes in condom use from baseline to follow-up time points were categorized as less frequent use, more frequent use, and no change in use. Multivariable logistic regression models were used to evaluate the association between contraceptive method (LARC vs. non-LARC) and STI acquisition. Known risks factors and other clinically relevant factors were evaluated for their association with STI acquisition and for potential confounding effect. A confounder was identified if a greater than 10% change in the effect size was noted when the covariate was added to the model. All statistical tests were performed using Stata 12. Significance levels were set at type I error less than 0.05.
Results
Of the 9,256 participants enrolled in the Contraceptive CHOICE Project, 6,135 (66%) were 12-month continuous users of the method they chose at baseline. LARC users comprised 82% of this cohort (LARC: N=5016; non-LARC: N=1119). Of those continuous users, 2,946 participants provided complete condom use behavior data (LARC: N=2371; non-LARC: N=575). The mean age was 26.1 years in the LARC group and 24.4 years in the non-LARC group. The cohort was racially diverse amongst both LARC and non-LARC initiators. Participants who chose to initiate a non-LARC method were more likely to be younger, uninsured, single, and nulliparous (Table 1). Among the 6,135 continuous users, 2694 participants contributed STI results. LARC users comprised 78% of this analytic cohort (LARC: N=2102; non-LARC: N=592). This cohort was similar to the condom cohort. However, more LARC users reported a history of STI (LARC: 42.6% (895/2102); non-LARC: 34.6% (205/592) p<0.01).
Table 1:
Demographic Characteristics 12-month continuous users with complete condom data
| ALL | Non-LARC | LARC | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | p- value | |
| Age | 25.8 | 5.7 | 24.4 | 5.0 | 26.1 | 5.9 | <0.01 |
| N | % | N | % | N | % | ||
| <0.01 | |||||||
| 14–24 | 1448 | 49.2 | 346 | 60.2 | 1102 | 46.5 | |
| 25+ | 1498 | 50.8 | 229 | 39.8 | 1269 | 53.5 | |
| Race | 0.07 | ||||||
| Black | 1247 | 42.3 | 264 | 45.9 | 983 | 41.5 | |
| White | 1442 | 48.9 | 271 | 47.1 | 1171 | 49.4 | |
| Others | 257 | 8.7 | 40 | 7.0 | 217 | 9.2 | |
| Marital Status | <0.01 | ||||||
| Single | 1446 | 49.1 | 338 | 58.8 | 1108 | 46.8 | |
| Married/Lliving with partner | 1318 | 44.8 | 221 | 38.4 | 1097 | 46.3 | |
| Separated/Divorced/Widowed | 181 | 6.1 | 16 | 2.8 | 165 | 7.0 | |
| Education | 0.01 | ||||||
| <=High School | 847 | 28.8 | 137 | 23.9 | 710 | 30.0 | |
| Some College | 1280 | 43.5 | 265 | 46.2 | 1015 | 42.8 | |
| College/Grad | 817 | 27.8 | 172 | 30.0 | 645 | 27.2 | |
| Insurance | <0.01 | ||||||
| None | 1222 | 41.7 | 265 | 46.8 | 957 | 40.4 | |
| Private | 1400 | 47.7 | 273 | 48.2 | 1127 | 47.6 | |
| Public | 311 | 10.6 | 28 | 4.9 | 283 | 12.0 | |
| Parity | <0.01 | ||||||
| 0 | 1369 | 46.5 | 381 | 66.3 | 988 | 41.7 | |
| 1 | 697 | 23.7 | 104 | 18.1 | 593 | 25.0 | |
| 2 | 552 | 18.7 | 54 | 9.4 | 498 | 21.0 | |
| 3+ | 328 | 11.1 | 36 | 6.3 | 292 | 12.3 | |
| History of STI | 0.03 | ||||||
| No | 1838 | 62.4 | 381 | 66.3 | 1457 | 61.5 | |
| Yes | 1108 | 37.6 | 194 | 33.7 | 914 | 38.5 | |
| Low SES | <0.01 | ||||||
| No | 1347 | 45.7 | 297 | 51.7 | 1050 | 44.3 | |
| Yes | 1598 | 54.3 | 277 | 48.3 | 1321 | 55.7 | |
| Got new partner | 0.09 | ||||||
| No | 2226 | 75.6 | 450 | 78.3 | 1776 | 74.9 | |
| Yes | 720 | 24.4 | 125 | 21.7 | 595 | 25.1 | |
| STD at enrollment | 0.10 | ||||||
| No | 2682 | 94.0 | 504 | 92.5 | 2178 | 94.3 | |
| Yes | 172 | 6.0 | 41 | 7.5 | 131 | 5.7 | |
Consistent condom use, defined as use every time across all time points with all partners, was low for all participants (6.4% or 187/2946); however, non-LARC initiators were significantly more likely to report always using condoms (11.3%) as compared to LARC initiators (5.2%, P<0.001). While there was overall less consistent condom use among LARC users, the changes in condom use patterns from time of initiation through the 12-month study period was not significantly different (Table 2). Approximately 70% of participants in both LARC and non-LARC groups reported no change in their condom use behaviors when compared to baseline.
Table 2:
Changes in condom use from baseline
| Baseline method | Change from baseline to 3 month among continuers all 12 month, with all partners | Change from baseline to 6 month among continuer all 12 month, with all partners | Change from baseline to 12 month among continuer by 12 month, with all partners | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| no change | More use | Less use | no change | More use | Less use | no change | More use | Less use | ||
| non-LARC | N | 426 | 31 | 118 | 415 | 33 | 127 | 409 | 30 | 136 |
| % | 74.09 | 5.39 | 20.52 | 72.17 | 5.74 | 22.09 | 71.13 | 5.22 | 23.65 | |
| LARC | N | 1,688 | 116 | 567 | 1,687 | 99 | 585 | 1,639 | 132 | 600 |
| % | 71.19 | 4.89 | 23.91 | 71.15 | 4.18 | 24.67 | 69.13 | 5.57 | 25.31 | |
| Total | N | 2,114 | 147 | 685 | 2,102 | 132 | 712 | 2,048 | 162 | 736 |
| % | 71.76 | 4.99 | 23.25 | 71.35 | 4.48 | 24.17 | 69.52 | 5.5 | 24.98 | |
| Chi-square test | p=0.22 | p=0.14 | p=0.65 | |||||||
The overall incidence of incident STI in the cohort was 3.5% (96/2694). There was a significant difference in STI incidence among LARC and non-LARC initiators (LARC: 3.9% (82/2102) versus non-LARC: 2.0% (12/5925), P=0.03).
After adjusting for potential confounding factors, use of LARC methods was associated with increased incidence of STIs (ORadj= 2.0; 95% CI 1.07, 3.72; Table 3). Several risk factors were found to be associated with increased risk for STI acquisition. Young women compared to women 25 years or older (ORadj=2.94; 95% CI 1.74, 4.97), black race (ORadj= 3.18; 95% CI 1.91, 5.31), separated, divorced, or widowed marital status compared to married or living with partner (ORadj= 3.17; 95% CI 1.21, 8.26), and women with a new sexual partner (ORadj= 2.16; 95% CI 1.40, 3.33) were at higher risk for STI acquisition (Table 3).
Table 3:
Risk factors associated with incident STI
| Crude | Adjusted | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| non-LARC | Reference | Reference | ||||
| LARC | 1.96 | 1.06 | 3.62 | 2.00 | 1.07 | 3.72 |
| age 14–24 | 3.09 | 1.90 | 5.01 | 2.94 | 1.74 | 4.97 |
| White | Reference | Reference | ||||
| Black | 3.33 | 2.01 | 5.51 | 3.18 | 1.91 | 5.31 |
| Other | 1.55 | 0.57 | 4.17 | 1.50 | 0.55 | 4.07 |
| Hx of STI | 1.60 | 1.06 | 2.42 | - | - | - |
| Married/Living with partner | Reference | Reference | ||||
| Single | 2.62 | 1.49 | 4.59 | 1.57 | 0.87 | 2.83 |
| Separated/Divorced/Widowed | 2.71 | 1.09 | 6.75 | 3.17 | 1.21 | 8.26 |
| Always using condom | 0.73 | 0.23 | 2.34 | - | - | - |
| got new partner | 2.54 | 1.68 | 3.85 | 2.16 | 1.40 | 3.33 |
| low SES | 1.39 | 0.91 | 2.12 | - | - | - |
Comments
As the uptake of LARC has increased, several hypothesized themes of concern have emerged. Clinicians have raised the possibility that increased LARC use may also increase sexual risk taking behavior, may have negative effects on condom use (13, 19), and may increase rates of STI (12, 20). A previous analysis of the Contraceptive CHOICE data demonstrated that there was no increase in risk taking behavior (18). The purpose of this analysis was to evaluate the impact LARC initiation had on condom use as well as rates of incident STIs. Our data, consistent with previously published studies, reaffirms that consistent condom use and dual contraceptive method use are low (5, 10, 11, 21) regardless of which additional contraceptive method is being used. Data from the 2006–2008 NSFG survey found 7.3% of women using any contraceptive method reported dual-method use at their most recent intercourse in the previous 12 months (10). Although we present data for consistent condom use over 12 months, as opposed to just the last act of intercourse, we too found a low incidence of consistent dual-method use (6.13%).
Increasing rates of LARC use in the U.S., most recently reported as 11.6% (22), have renewed concerns that use of LARC may elevate risks of STI by less frequent use of condoms. Recent studies have evaluated condom use in LARC users and have demonstrated that LARC use does not compromise condom use (19, 21). Conversely, one early study evaluating dualmethod use in users of the Norplant found an overall decrease in condom use among women who initiated this LARC method (20). However, it was the cohort of women reporting one sexual partner where the largest decline was noted (20% to 10%) (20). In the same cohort, women reporting more than one partner demonstrated an increase in reported condom use from 25% to 31% (20). El Ayadi et al. reported findings from their cluster randomized trial in which LARC access was assessed after a provider targeted intervention to increase LARC was implemented. The authors assessed the impact of their intervention on condom use and STI incidence and did not find a negative impact on either (21). Our findings continue to support that initiation of LARC does not change the condom use behavior of women.
The overall rate of incident STI in this analysis was 3.5%. Although we did demonstrate that LARC users were at increased risk (OR 2.0) of incident STI, the cohort maintained a low rate overall (3.9%). Regardless, this data highlights the importance of counseling contraceptive users on dual method protection.
The strengths of this study include its large sample size and inclusion of participants who were continuous method users, allowing for more thorough evaluation of the impact of method on behaviors. We also utilized a rigorous evaluation of reported condom use over time. The study collected information about condom use at baseline, 3 months, 6 months, and 12 months. Frequent contact with participants not only helped establish rapport but also likely helped to minimize recall bias. An additional strength of this study is the measure of both a behavioral outcome (condom use) and an important biological endpoint (STI incidence).
This study was not without limitations. Including only those who completed STI screening may have falsely underestimated our STI detection rate, especially if participants at highest STI risk are those who have not been included. However, we feel that because we maintained frequent contact with participants and offered both testing and treatment free of charge, the likelihood that we had differential participation is low. Frequent contact with participants, particularly when asking questions about sexual behavior and condom use, could have an effect in and of itself. Participants may have been more aware of the importance of condom use, or STI prevention influencing their behavior. As is true with all sensitive subjects, the potential for social desirability bias is unavoidable; however, we believe the relationship we had with our participants served to minimize this bias.
This study adds to the growing body of literature that provides reassurance that LARC use does not change condom use behavior. However, the slight increase in STI acquisition observed among LARC users highlights the importance of dual method education. Similar to previous reports, we noted that dual contraceptive method use is low, regardless of contraceptive method. Given the known benefits, healthcare providers should continue to encourage all at-risk patients to use dual-methods for STI and pregnancy prevention
Acknowledgments
Funding: This research was supported by an anonymous foundation, Washington University Institute of Clinical and Translational Sciences grant UL1 TR00048, and the National Institutes of Health (NIH) T32 research training grant number 19 5T32HD055172–03.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Jessica Klugman and Qiuhong Zhao report no conflicts of interest.
References
- 1.Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. N Engl J Med 2012. May 24;366(21):1998–2007. [DOI] [PubMed] [Google Scholar]
- 2.Gallo MF, Warner L, Jamieson DJ, Steiner MJ. Do women using long-acting reversible contraception reduce condom use? A novel study design incorporating semen biomarkers. Infect Dis Obstet Gynecol 2011;2011:107140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cates W Jr., Steiner MJ. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach? Sex Transm Dis 2002. March;29(3):168–74. [DOI] [PubMed] [Google Scholar]
- 4.Peipert JF, Redding CA, Blume JD, Allsworth JE, Matteson KA, Lozowski F, et al. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol 2008. June;198(6):630–e1–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tyler CP, Whiteman MK, Kraft JM, Zapata LB, Hillis SD, Curtis KM, et al. Dual use of condoms with other contraceptive methods among adolescents and young women in the United States. J Adolesc Health 2014. February;54(2):169–75. [DOI] [PubMed] [Google Scholar]
- 6.Pazol K, Kramer MR, Hogue CJ. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep 2010. Mar-Apr;125(2):208–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peipert BJ, Scott DM, Matteson KA, Clark MA, Zhao Q, Peipert JF. Sexual Behavior and Contraceptive Use at Brown University: 1975–2011. J Reprod Med 2016. Mar-Apr;61(3–4):101–8. [PubMed] [Google Scholar]
- 8.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception 2008. January;77(1):10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu H, Darroch JE, Haas T, Ranjit N. Contraceptive failure rates: new estimates from the 1995 National Survey of Family Growth. Fam Plann Perspect 1999. Mar-Apr;31(2):56–63. [PubMed] [Google Scholar]
- 10.Eisenberg DL, Allsworth JE, Zhao Q, Peipert JF. Correlates of dual-method contraceptive use: an analysis of the National Survey Of Family Growth (2006–2008). Infect Dis Obstet Gynecol 2012;2012:717163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peipert JF, Zhao Q, Meints L, Peipert BJ, Redding CA, Allsworth JE. Adherence to dualmethod contraceptive use. Contraception 2011. September;84(3):252–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darney PD, Callegari LS, Swift A, Atkinson ES, Robert AM. Condom practices of urban teens using Norplant contraceptive implants, oral contraceptives, and condoms for contraception. Am J Obstet Gynecol 1999. April;180(4):929–37. [DOI] [PubMed] [Google Scholar]
- 13.Steiner RJ, Liddon N, Swartzendruber AL, Rasberry CN, Sales JM. Long-Acting Reversible Contraception and Condom Use Among Female US High School Students: Implications for Sexually Transmitted Infection Prevention. JAMA Pediatr 2016. May 1;170(5):428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santelli JS, Davis M, Celentano DD, Crump AD, Burwell LG. Combined use of condoms with other contraceptive methods among inner-city Baltimore women. Fam Plann Perspect 1995. Mar-Apr;27(2):74–8. [PubMed] [Google Scholar]
- 15.Williams RL, Fortenberry JD. Dual use of long-acting reversible contraceptives and condoms among adolescents. J Adolesc Health 2013. April;52(4 Suppl):S29–34. [DOI] [PubMed] [Google Scholar]
- 16.Santelli JS, Warren CW, Lowry R, Sogolow E, Collins J, Kann L, et al. The use of condoms with other contraceptive methods among young men and women. Fam Plann Perspect 1997. Nov-Dec;29(6):261–7. [PubMed] [Google Scholar]
- 17.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol 2010. August;203(2):115–e1–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Secura GM, Adams T, Buckel CM, Zhao Q, Peipert JF. Change in sexual behavior with provision of no-cost contraception. Obstet Gynecol 2014. April;123(4):771–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rattray C, Wiener J, Legardy-Williams J, Costenbader E, Pazol K, Medley-Singh N, et al. Effects of initiating a contraceptive implant on subsequent condom use: A randomized controlled trial. Contraception 2015. December;92(6):560–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cushman LF, Romero D, Kalmuss D, Davidson AR, Heartwell S, Rulin M. Condom use among women choosing long-term hormonal contraception. Fam Plann Perspect 1998. Sep-Oct;30(5):240–3. [PubMed] [Google Scholar]
- 21.El Ayadi AM, Rocca CH, Kohn JE, Velazquez D, Blum M, Newmann SJ, et al. The impact of an IUD and implant intervention on dual method use among young women: Results from a cluster randomized trial. Prev Med 2017. January;94:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daniels K, Daugherty J, Jones J, William M. National Health Statistics Report: Current Contraceptive Use and Variation by Selected Characteristics Among Women Aged 15–44: United States, 2011–2013. Center for Disease Control; 2015. p. 1–15. [PubMed] [Google Scholar]


