Abstract
Background
With the complexity of calcaneal fracture (CF) increasing, its treatment has changed to include inserting the screw used to secure the facies articular posterior into the sustentaculum tail (ST). Some research progress has been made in this area, but there has been little in-depth research on the anatomical morphology of the sustentaculum tail, which is necessary for clinical surgery, and more information about Chinese anatomic characteristics and improved surgical techniques for CF are needed.
Material/Methods
This anatomical study, based on a three-dimensional (3D) computed tomographic (CT) reconstruction technique, included 287 dry calcaneus, consisting of 144 left and 143 right calcaneus. The images were reconstructed in 3D after CT scanning. Seven subjects were enrolled (L and R): (1) The vertical distance from inside the sustentaculum tail (IST) to inside the facies articularis talaris posterior; (2) The vertical distance from IST to the outside facies articularis talaris posterior; (3) The thickness of sulcus calcaneal nadir; (4) The distance from IST to processus medislis tuberis calcaneus; (5) The distance from IST to calcaneal posterosuperior tuber; (6) The angle of the prolate axial intersection between ST and calcaneus on the normal superior as ∠α; and (7) The angle of the prolate axial intersection between ST and calcaneus on the normal posterior as ∠β. All measurement results were analyzed by SPSS 22.0.
Results
Based on morphological classification, the average length of AB, AC, AE, and AF on left ST were 16.956±1.391 mm, 37.803±2.525 mm, 43.244±3.617 mm, and 51.113±4.455 mm, respectively. Among the others, ∠β was 81.227±6.317 mm on the left and 74.581±9.008 mm on the right (P<0.05).
Conclusions
These results suggest better ways to treat the special characteristics and to reduce the risk of CF surgery.
MeSH Keywords: Anatomy; Calcaneus; Imaging, Three-Dimensional
Background
For the past few years, the complexity of calcaneal fractures (CFs) has increased with the increasing incidence of high-energy injury. As a lower bone of the body, the calcaneus has the task of supporting the axial load from the weight of the body and can be fractured when people fall accidentally from a height [1]. Most calcaneal thrypsis can only be treated by plate-screw internal fixation. When performing the operation, the screw that is used to secure the facies articular posterior should be inserted into the sustentaculum tail (ST), because the ST is an optimal structure that can give the fractured articular surface a new support point, and it is best to insert the screw from inside to outside and just reach the ST. However, although there are many characteristics of ST, the surgeon can still encounter some classifications that differ from all of those, and it is difficult to make a proper screw or anything else to deal with the unknown characteristic that lead to an unsuccessful operation, such as broken bones and unsteadiness. Thus, the length and diameter of the screw and the angle and point of insertion and the structure around the ST have been studied.
In 1993, Sander divided CFs into 4 classifications by coronal calcaneus CT scanning, which was named the Sander type and became the standard, and all classifications relating to the ST and facies articularis calcaneus posterior become are 3D, which is an evident norm for surgery [2]. The anatomic structures of the ST require further study. The ST is surrounded by many stable joint capsules, ligaments, and muscle tendons, including ligamentum triangularity, tendinous sheath of flexor digitorum longus, and flexor pollicis longus muscle tendon. They are intersected by the tibial nerve, posterior tibial artery, and posterior tibial vein, making the anatomic structure of the calcaneus quite complicated, and the irregular geometrical shape of the calcaneus makes CF surgery challenging. Many studies have focused on CF and its treatment, but little is known about the anatomic details. Some researchers have used CT and 3D reconstruction techniques to locate and mark the ST and measure the angle and length of the specified point of the lateral wall of the calcaneus to the ST [1,3]. Harnroongroj et al. created a new anatomic characteristics system used by Glluzzo et al. to assist their work in CF management and a simple classification of displaced articular fracture of the calcaneus [4]. Defining the detailed anatomy of the ST forms can increase stability and security, reduce postoperative pain, and speed functional recovery in treating CF [5,6]. Fixation of the calcaneus aided by ST screwing has advantages of shorter operative time and fluoroscopy time, reduced incidence of complications, and better function recovery [7–9]. The points and angles of insertion and the screw length are particularly important for surgical success. Firstly, when screw insertion is performed, the wrong points and angles can injure blood vessels, neurons, and muscle tendons inside the ST. Secondly, it can cause broken bones if the screw is inserted into the subtalar articular surface in error. Lastly, if the screw is not inserted into the ST, the repair will not be firm enough [10]. Accordingly, the purpose of the present study is to reduce the operative risk.
We numerically assessed the STs on 287 dry calcaneus from Chinese patients to explore reliable ST anatomic forms to improve CF surgery to and define specific characteristics of Chinese patients with CF, so that proper screw fixation can be made and to reduce the risk of CF surgery.
Material and Methods
Ethics statement
All the procedures were approved by the Ethics Inspection Committee at Southwest Medical University (Luzhou, China), and the computed tomographic (CT) data of calcaneus were collected at the Radiology Department of the Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University (Luzhou, China).
Instruments
A spiral CT scanner (Somatom Emotion; Siemens AG, Munich, Germany) was used. The images were reconstructed in 3D after CT scanning and all 3D images were stored in the Picture Archiving Communication System (PACS; DJ HealthUnion Systems Corporation, Shanghai, China). The system not only can record radiographic images and store many images, but also allows access from any networked station. PACS the software (UniReport version 2.0) can also assist in accurate measuring (Figures 1, 2).
Figure 1.
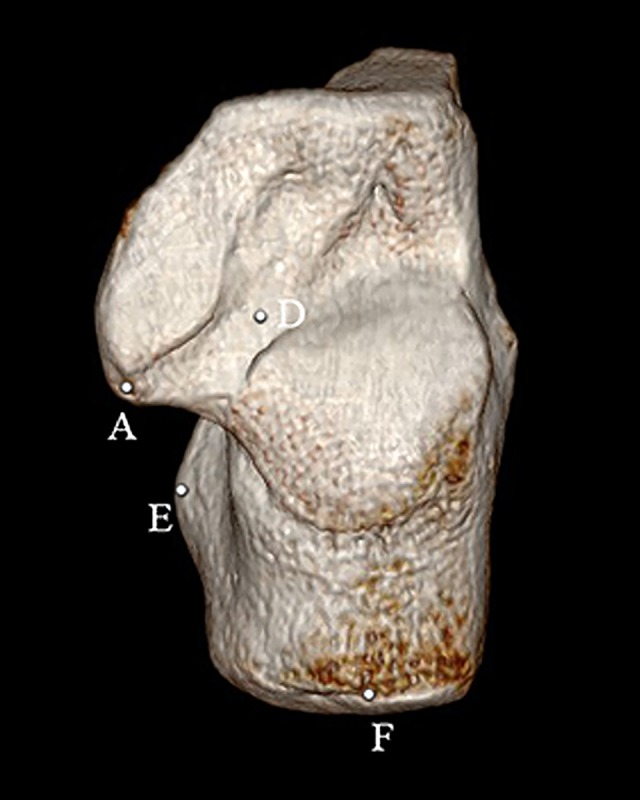
3D CT image of ST on normal superior. A 3D CT image from a Chinese patient. Point A: inside sustentaculum tail; Point B: inside facies articularis talaris posterior; Point C: outside facies articularis talaris posterior; Point E: processus medislis tuberis calcaneus; Point F: calcaneal posterosuperior tuber.
Figure 2.
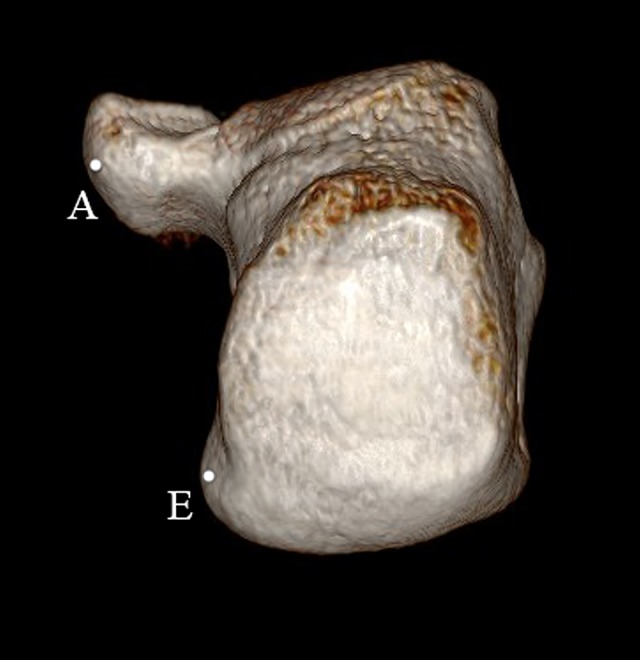
3D CT image of ST on norma posterior. A 3D CT image from a Chinese patient. Point A: inside sustentaculum tail; Point E: processus medislis tuberis calcaneus.
Study population
The demographic characteristics of the scanning group were age 20–60 years old and Chinese Han ethnicity. Inclusion criteria were: (1) Chinese Han ethnicity (both sexes); (2) Complete development of talus; and (3) Never had a calcaneus fracture. Exclusion criteria were: (1) The undeveloped complete calcaneus from patients under 20 years old and the osteoporosis calcaneus from patients over 60 years old; (2) Congenital foot malformation; and (3) Fracture.
Method of measurement
Point A, inside sustentaculum tail.
Point B, inside facies articularis talaris posterior.
Point C, outside facies articularis talaris posterior.
Point D, the thickness of sulcus calcaneal nadir.
Point E, processus medislis tuberis calcaneus.
Point F, calcaneal posterosuperior tuber.
AB, the vertical distance from A to B.
AC, the vertical distance from A to C.
AE, the distance from A to E.
AF, the distance from A to F.
∠α, the prolate axial intersection between ST and calcaneus on the normal superior (Figure 3).
∠β, the prolate axial intersection between ST and calcaneus on the normal posterior (Figure 4).
Figure 3.
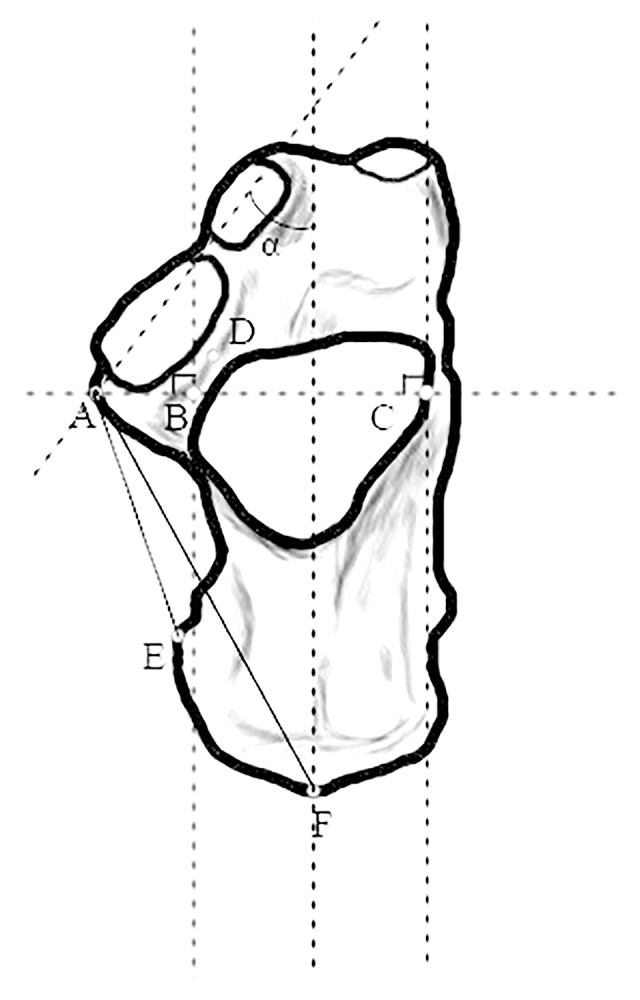
Morphometric measurements on normal superior. Measurement method for ST. Point D: the thickness of sulcus calcaneal nadir; AB: the vertical distance from inside sustentaculum tail to inside facies articularis talaris posterior; AC: the vertical distance from inside sustentaculum tail to outside facies articularis talaris posterior; AE: the distance from inside sustentaculum tail to processus medislis tuberis calcaneus; AF: the distance from inside sustentaculum tail to calcaneal posterosuperior tuber; Angle a: the prolate axial intersection between ST and calcaneus on the normal superior.
Figure 4.
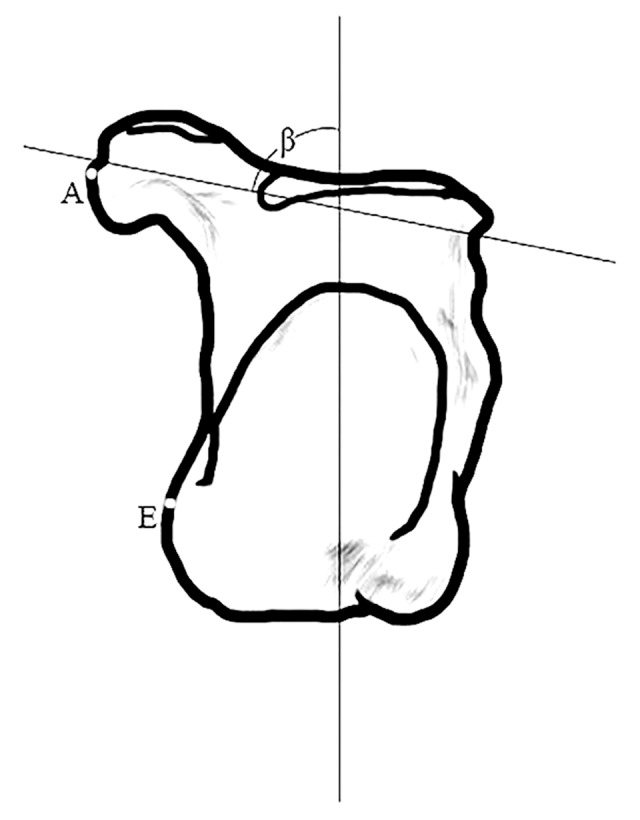
Morphometric measurements on normal posterior. Measurement method for ST. Point A: inside sustentaculum tail; Point E: processus medislis tuberis calcaneus; Angle b: the prolate axial intersection between ST and calcaneus on the normal posterior.
Point B and C: 2 tangent lines were made at inner and outer sides of facies articularis calcanea posterior, and a vertical line from Point A crossing the tangent line at 2 points marked as B and C.
Statistical analysis
All data are presented as the mean and standard deviation (SD). Statistical analysis was performed using SPSS, version 22.0 (IBM Corp., Armonk, NY, USA). The numbers of lefts and rights in each group were analyzed by the independent-samples t test. The parameters are expressed as the mean ± standard deviation. ∠β with a P-value <0.05 was regarded as statistically significant.
Results
Based on morphological classification, the average length of AB, AC, AE, and AF on total left ST were 17.208±1.640 mm, 38.250±2.757 mm, 43.570±3.621 mm, and 52.566±4.829 mm, respectively. The average length of AB, AC, AE, and AF on left ST were 16.956±1.391 mm, 37.803±2.525 mm, 43.244±3.617 mm, and 51.113±4.455 mm, respectively; the average length of AB, AC, AE, and AF on right ST were 17.466±1.843 mm, 38.708±2.934 mm, 43.903±3.637 mm, and 54.053±4.792 mm, respectively; Point D, the thickness sulcus calcaneal nadir, was 8.576±1.270 mm on left ST and 8.927±1.379 mm on right ST; ∠α was 40.772±5.247 mm on the left and 41.744±5.433 mm on the right; and ∠β was 81.227±6.317 mm on the left and 74.581±9.008 mm on the right (P<0.05). There were no statistically significant differences between left and right sides, except for ∠β. All data are listed in Table 1.
Table 1.
Height, length, and angle distribution and measurements of sustentaculum tail based on body side. ∠β in left side is bigger than right side. There was no significant difference between other indexes.
| Sample | Left | Right | Total |
|---|---|---|---|
| AB, mm | 16.956±1.391 | 17.466±1.843 | 17.208±1.640 |
| AC, mm | 37.803±2.525 | 38.708±2.934 | 38.250±2.757 |
| D, mm | 8.576±1.270 | 8.927±1.379 | 8.750±1.329 |
| ∠α,°* | 40.772±5.247 | 41.744±5.433 | 41.253±5.331 |
| ∠β,°** | 81.227±6.317 | 74.581±9.008 | 77.943±8.411 |
| AE, mm | 43.244±3.617 | 43.903±3.637 | 43.570±3.621 |
| AF, mm | 51.113±4.455 | 54.053±4.792 | 52.566±4.829 |
Measured on cross-section;
Measured on coronal section, P<0.05 vs. right.
Discussion
The literature on CF and ST includes many detailed anatomic studies on ST, and most of them used sensitive instruments for measurements, but they just prove that ST screw fixation is the best way to treat CF and it is important to revise surgery according to classification.
In the present study, 287 intact dry calcaneus anatomic data were collected by 3D CT technique and showed specific characteristics of Chinese patients. The information in this study has practical significance for CF surgery in China, such as improving the surgical success rate and reducing the incidence of complications. Our results demonstrated no significant differences between left and right sides, except that ∠β was 81.227±6.317 mm on the left and 74.581±9.008 mm on the right (P<0.05), which may be influenced by strained condition of body sides. According to [11] and ZongPing Luo et al. [12], subtalar stability is influenced by the surrounding ligaments, including the calcaneofibular, the cervical, and the interosseous talocalcaneal ligaments. Thus, a patient who supports the weight of the body heavier and more frequently on their left foot may be left-handed. Population statistics show that 6–13% of Chinese are left-handed, meaning there are at least 100 million left-handed Chinese, and the ratio of left-handed to right-handed people leads to the result that ∠β has a P-value <0.05.
This is an important finding in reducing intraoperative bleeding, and avoiding blood vessels and nerve injury, which can lead to poor functional recovery. For example, the blood supply of the heel fat pad from medial branch of posterior tibial artery and the blood supply of the lateral foot skin soft tissue consists of the perforating peroneal artery and the deep soft tissue supplies blood directly to the skin [13]. Thus, if the screw injures these blood vessels and nerves, a large area of soft tissue in the posterior foot is damaged. If there is a small gap or bone defect at the fracture end, stress will focus at the fracture and the internal fixation will bear most of it, which can lead to internal fixation failure and then lead to refracture and steel plate breakage [14,15].
The Sander type, which was created by Sander in 1993, has become the standard for classifying anatomic characteristics. However, the data used by Sander were from the USA, as were the data used by Harnroongroj et al. [4]. Though the Sander type includes most fracture conditions, it cannot account for special characteristics of Chinese patients. In the matter of instruments, CT scanning is faster and clearer, and 3D images can provide more vivid effects than conventional 2D images [1]. The combination of CT scanning and 3D technique can provide adequate and accurate data for creating 3D images.
Nevertheless, further research is needed. Firstly, although some distinctive characteristics were found here to improve surgery, the ST has a complex structure and some distinctive characteristics remain to be defined. Secondly, the samples in the present study were all from southwestern China and the sample size was small. Thirdly, the inferences about ST are limited.
Conclusions
Most calcaneal thrypsis can only be treated by plate-screw internal fixation, and ST is an optimal structure that can give fractured articular surface a new supporting point. These results suggest better approaches to treatment based on the special anatomic characteristics of Chinese patients to reduce the risk of CF surgery.
Footnotes
Source of support: Academician Workstation Construction Project of Luzhou, Sichuan Province, China (No. 20180101)
Conflict of interests
None.
References
- 1.De Boer AS, Van Lieshout EMM, et al. 2D and 3D assessment of sustentaculum tail screw fixation with or without screw targeting clamp. Injury. 2017;48(12):2864–71. doi: 10.1016/j.injury.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 2.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;(290):87–95. [PubMed] [Google Scholar]
- 3.Gras F, Marintschev I, Wilharm A, et al. Sustentaculum tali screw placement for calcaneus fractures – different navigation procedures compared to the conventional technique. Z Orthop Unfall. 2010;148(3):309–18. doi: 10.1055/s-0029-1240973. [DOI] [PubMed] [Google Scholar]
- 4.Harnroongroj T, Chuckpaiwong B, Angthong C. Displaced articular calcaneus fractures: Classification and fracture scores: A preliminary study. J Med Assoc Thai. 2012;95(3):366–77. [PubMed] [Google Scholar]
- 5.Bing W, Tao L, Yu-Cheng Z, et al. [Anterior part of calcaneus and sustentaculum tali: anatomic relationship and clinical significance]. Chinese Journal of Clinical Anatomy. 2012;30(2):131–35. [in Chinese] [Google Scholar]
- 6.Udupa JK, Hirsch BE, Hillstrom HJ, et al. Analysis of in vivo 3-D internal kinematics of the joints of the foot. IEEE Trans Biomed Eng. 1998;45(11):1387–96. doi: 10.1109/10.725335. [DOI] [PubMed] [Google Scholar]
- 7.Gu ZQ, Pang QJ, Yu X, et al. [Sustentaculum tali screw fixation for the treatment of Sanders type II and III calcaneal fractures]. Zhongguo Gu Shang. 2015;28(1):31–35. [in Chinese] [PubMed] [Google Scholar]
- 8.Wang Y, Liu BG, Pang QJ, et al. [Comparison of fixation of sustentaculum tali of calcaneus aided by director for sustentaculum tali screwing and ordinary screwing guide]. Zhongguo Gu Shang. 2016;29(12):1097–103. doi: 10.3969/j.issn.1003-0034.2016.12.007. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 9.Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1994;15(7):349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 10.Mei J, Yu G, Zhu H, et al. [Anatomic characteristics and clinical significance of the sustentaculum tali of calcaneus]. Chinese Journal of Clinical Anatomy. 2002;20(1):9–11. [in Chinese] [Google Scholar]
- 11.Keefe DT, Haddad SL. Subtalar instability. Etiology, diagnosis, and management. Foot Ankle Clin. 2002;7(3):577–609. doi: 10.1016/s1083-7515(02)00047-5. [DOI] [PubMed] [Google Scholar]
- 12.Luo ZP, Kitaoka HB, Hsu H-C. Physiological elongation of ligamentous complex surrounding the hindfoot joints: In vitro biomechanical study. Foot Ankle Int. 1997;18(5):277–83. doi: 10.1177/107110079701800506. [DOI] [PubMed] [Google Scholar]
- 13.Beynnon BD, Webb G, Huber BM, et al. Radiographic measurement of anterior talar translation in the ankle: determination of the most reliable method. Clin Biomech (Bristol, Avon) 2005;20(3):301–6. doi: 10.1016/j.clinbiomech.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Schepers T, van Lieshout EM, van Ginhoven TM, et al. Current concepts in the treatment of intra-articular calcaneal fractures: Results of a nationwide survey. Int Orthop. 2008;32(5):711–15. doi: 10.1007/s00264-007-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yun SJ, Jin W, Kim GY, et al. A different type of talocalcaneal coalition with os sustentaculum: The continued necessity of revision of classification. Am J Roentgenol. 2015;205(6):W612–18. doi: 10.2214/AJR.14.14082. [DOI] [PubMed] [Google Scholar]


