Abstract
Introduction:
Sleep is essential for both physical and mental well-being. This study investigated sociodemographic, lifestyle/behavioural, environmental, psychosocial and health factors associated with sleep duration among Canadians at different life stages.
Methods:
We analyzed nationally representative data from 12 174 Canadians aged 3–79 years in the Canadian Health Measures Survey (2009–2013). Respondents were grouped into five life stages by age in years: preschoolers (3–4), children (5–13), youth (14–17), adults (18–64) and older adults (65–79). Sleep duration was classified into three categories (recommended, short and long) according to established guidelines. Logistic regression models were used to identify life stage–specific correlates of short and long sleep.
Results:
The proportion of Canadians getting the recommended amount of sleep decreased with age, from 81% of preschoolers to 53% of older adults. Statistically significant factors associated with short sleep included being non-White and having low household income among preschoolers; being non-White and living in a lone-parent household among children; and second-hand smoke exposure among youth. Boys with a learning disability or an attention-deficit/hyperactivity disorder and sedentary male youth had significantly higher odds of short sleep. Among adults and older adults, both chronic stress and arthritis were associated with short sleep. Conversely, mood disorder and poor/fair self-perceived general health in adults and weak sense of community belonging in adults and older men were associated with long sleep.
Conclusion:
Our population-based study identified a wide range of factors associated with short and long sleep at different life stages. This may have implications for interventions aimed at promoting healthy sleep duration.
Keywords: sleep, life stages, preschoolers, children, youth, adults, older adults
Highlights
A large proportion of Canadians across all life stages do not get the recommended amount of sleep.
This population-based study identified a wide range of factors associated with sleep duration at different life stages.
Sociodemographic factors, such as non-White ethnicity, low household income and living in a lone-parent household, are associated with short sleep in younger children.
Second-hand smoke exposure is associated with short sleep in youth.
Psychosocial and health-related factors, such as arthritis, chronic stress, self-perceived health, mood disorder, and sense of community belonging, are associated with short and/or long sleep in adults and older adults.
Introduction
Sleep is essential for the promotion and maintenance of health across all stages of life.1 However, sleep deprivation has become highly prevalent in modern societies. 1,2 For example, recent national surveys in Canada showed that approximately 20–30% of children and adolescents 3,4and one-third of adults and older adults 5 sleep less than the recommended amount for their age.
Insufficient sleep has been linked to a number of adverse physical and mental health outcomes, including obesity, diabetes, cardiovascular disease, injuries, anxiety, depression, neurological disorders and allcause mortality.2 In addition, sleep loss and related disorders contribute to substantial societal and economic burdens resulting from productivity losses and health care costs.6,7 There is some evidence suggesting a U-shaped relationship between sleep duration and health outcomes, where both short and long sleep, especially among adults, are associated with increased risk of chronic diseases.8-10A 2016 systematic review found that shorter sleep in children and youth was associated with excess adiposity, lower quality of life/well-being, and poorer emotional regulation and academic achievement.11
Despite the growing evidence on the health consequences of short (and long) sleep, public health research and education has paid relatively little attention to sleep compared to other health-related behaviours (e.g., diet, physical activity).1 To better identify targets for interventions aimed at improving sleep, an understanding of factors associated with sleep duration is warranted.
In addition to genetic and physiological factors, sleep duration is likely affected by a combination of behavioural, psychological, social, cultural and environmental factors.12 Studies in various countries have explored potential correlates of sleep duration among children,13-18 adolescents18-21and adults.22-26 For example, sociodemographic factors, such as ethnicity, parental education and household income,17-19 as well as lifestyle factors, especially screen time (e.g., television, computer),15-17,20,21have been identified as important correlates of sleep duration among children and adolescents. In adults, additional sociodemographic correlates, including employment and marital status, as well as various factors related to lifestyle (e.g., physical activity, smoking) and physical and mental health (e.g., self-rated general health, depression, chronic conditions) were found to affect sleep duration.22-26
To the best of our knowledge, there has not been a detailed assessment of factors associated with sleep duration in the general Canadian population. Given crosscultural differences in sleep duration and its correlates,26-28 identifying determinants of sleep duration in the Canadian context may have important implications for informing the development of future intervention strategies aimed at improving sleep. Furthermore, despite age-related differences in sleep needs and patterns,2 previous studies have not comprehensively examined life stage–specific associations between potential correlates and sleep duration within a single population. Hence, the objective of this study was to investigate sociodemographic, lifestyle/ behavioural, environmental, psychosocial and health factors associated with short and long duration of sleep among Canadians at different life stages.
Methods
Data source and study population
This study utilized data from the Canadian Health Measures Survey (CHMS), cycles 2 (2009–2011) and 3 (2012–2013). Details of the CHMS have been described elsewhere. 29,30 Briefly, the CHMS is an ongoing cross-sectional survey that uses a multistage stratified sampling design to collect nationally representative data from the Canadian household population 3–79 years of age. Residents of the three territories, people living on reserves or other Aboriginal settlements, full-time members of the Canadian Forces and residents of institutions and certain remote regions were excluded from the sampling frame. The sample for each cycle represented approximately 96% of the Canadian population in the target age range. The combined (household- and person-level) response rates were 55.5% and 51.7% for cycles 2 and 3, respectively.
The CHMS consists of an in-home household interview that collects information on various sociodemographic, lifestyle and health characteristics, followed by a visit to a mobile examination centre to take direct physical measures (e.g., height, weight). Written informed consent was obtained from respondents aged 14 years and older or from parents/guardians of those younger than 14 years who gave permission to participate. All processes of the CHMS were reviewed and approved by Health Canada and the Public Health Agency of Canada Research Ethics Board.
Analyses for this study were based on all respondents within the target age range (3–79 years) of the CHMS (cycle 2: n = 6395; cycle 3: n = 5785). Data from two survey cycles were pooled to increase sample size and precision of estimates. To keep consistency of the age groupings, cycle 1 (which covered 6–79 year-olds only) was not included in our analysis. Respondents with missing data on sleep duration (n = 6) were excluded, yielding a sample size of 12 174 respondents. To examine sleep duration and its correlates separately by life stage, respondents were grouped into five age categories, including preschoolers (3–4 years), children (5–13 years), youth (14–17 years), adults (18–64 years) and older adults (65–79 years), consistent with existing sleep duration recommendations. 31-33
Sleep duration
During the household interview, respondents (or parents/guardians for those aged less than 12 years) were asked to report the number of hours (to the nearest half hour) in a 24-hour period they usually spend sleeping, excluding time spent resting. Respondents were classified into three sleep duration categories (recommended, short or long) according to the Canadian 24-Hour Movement Guidelines for the Early Years (preschoolers),31 the Canadian 24-Hour Movement Guidelines for Children and Youth (children and youth),32 and the United States National Sleep Foundation’s sleep time duration recommendations (adults and older adults).33 The recommended hours of daily sleep were 10–13 hours/day for preschoolers, 9–11 hours/day for children, 8–10 hours/day for youth, 7–9 hours/day for adults and 7–8 hours/day for older adults.31-33 Respondents with sleep durations shorter or longer than the recommended range were classified as “short sleepers” or “long sleepers,” respectively.
Correlates
Potential correlates of sleep duration were identified from the existing literature13-26as applicable to each age group.
Sociodemographic factors included age (years); sex (male or female); ethnicity (White or non-White); highest level of education (less than secondary school degree, secondary school degree or postsecondary school degree) attained in the household for preschoolers, children and youth or by the respondent for adults and older adults; household type (no children < 18 years of age, couple with children < 18 years or lone-parent with children < 18 years); and household income adequacy. Based on total annual household income and number of people living in the household, household income adequacy was categorized as low (< $30 000 for 1–2 people, < $40 000 for 3–4 people, < $60 000 for ≥5 people); middle ($30 000–$ 59 999 for 1–2 people, $40 000–$79 999 for 3–4 people, $60 000–$79 999 for ≥ 5 people); or high (≥ $60 000 for 1–2 people, ≥ $80 000 for ≥ 3 people).34 We also examined marital status (married/common- law, divorced/separated, widowed or single/never married) and employment status (full-time [≥30 hours/week], parttime [<30 hours/week] or unemployed) among adults and older adults.
Lifestyle/behavioural and environmental factors included physical activity, screen time–based sedentary behaviour, active and/or passive smoking and alcohol consumption.
For consistency with sleep duration, we assessed physical activity and sedentary behaviour based on adherence to current Canadian guidelines.31,32,35 Physical activity was objectively measured using an activity monitor (Actical accelerometer) worn by respondents for 7 days following the mobile examination centre visit. Only respondents with 4 or more valid days of accelerometer data (i.e., wear time of ≥ 10 hours [≥ 5 hours for 3–5 year-olds] each day)30 (~75%) were assessed for guideline adherence; those with less than 4 valid days were included as a separate “missing” category for the logistic regression analysis. Preschoolers who accumulated 180 or more minutes of physical activity (any intensity) per day,31 children and youth who accumulated 60 or more minutes of moderate-to-vigorous physical activity per day,32 and adults and older adults who accumulated 150 or more minutes of moderate-to-vigorous physical activity (in bouts ≥10 minutes) per week35 were considered to have met the guidelines. Sedentary behaviour was assessed based on parent/guardian- or self-reported recreational screen time (i.e., watching television, playing video games and/or using a computer during leisure-time), with adherence defined as 1 hour/day or less for preschoolers31 and 2 hours/day or less for all other age groups.32,35
Passive smoking among preschoolers, children and youth was defined as regular (i.e., every day or almost every day) exposure to second-hand smoke at home. Smoking status (never, former or current) and alcohol consumption (non-drinker, less than once per week, 1–6 times per week or daily) were examined in youth, adults and older adults.
We assessed psychosocial factors, including self-perceived mental health (excellent/ very good, good or poor/fair) and sense of belonging to the local community (strong or weak) among youth, adults and older adults. We also examined self-perceived chronic stress (yes [extremely or quite a bit stressful in life] or no [a bit, not very or not at all stressful in life]) in adults and older adults.
Health factors included self- or parent/ guardian-perceived general health (excellent/ very good, good or poor/fair); body mass index, derived from directly measured weight and height and categorized according to standard World Health Organization cut-offs appropriate for each age group;36-38 and presence of each of the following self-reported, health professional–diagnosed chronic conditions: mood disorder, asthma, chronic obstructive pulmonary disease, arthritis, osteoporosis, diabetes, hypertension, heart disease, stroke, cancer, thyroid condition, kidney disease and liver/gall bladder disease. Due to the low prevalence of most chronic conditions among preschoolers, children and youth, we only examined asthma in these age groups and mood disorder in youth. We also examined learning disability or attention- deficit/hyperactivity disorder (ADHD) among preschoolers, children and youth.
Statistical analysis
To account for the complex sampling design of the CHMS, sampling weights were used in all of our analyses, and variance estimates were obtained using the bootstrap method.31,32 All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
First, we conducted descriptive analyses to examine the distribution of all variables of interest in the study population and to estimate the proportion of the population in each of the three sleep duration categories, by age group. Next, we used univariable logistic regression to estimate unadjusted associations between potential correlates and short (vs. recommended) sleep duration in each age group, as well as long (vs. recommended) sleep duration in adults and older adults. Because of the small numbers of long sleepers among preschoolers (n < 10; < 1%), children (n = 91; 2%) and youth (n = 29; 3%), we did not model long sleep as an outcome in these age groups. Variables that were statistically significant at p < .20 in the univariable analyses were selected as candidates for inclusion in multivariable models and were retained if they remained significant at p < .20, or if removing them resulted in greater than 10% change in the odds ratio (OR) for any of the other variables. 39,40 Age and sex were retained in all multivariable models regardless of statistical significance. We also evaluated potential interactions with sex by including product terms (sex × correlate), which were retained in the final model if statistically significant at p < .05, in which case effect estimates were reported separately for males and females. Respondents with missing data on any of the variables (< 5%) were excluded from the logistic regression analysis to ensure equal samples used for model building.
Results
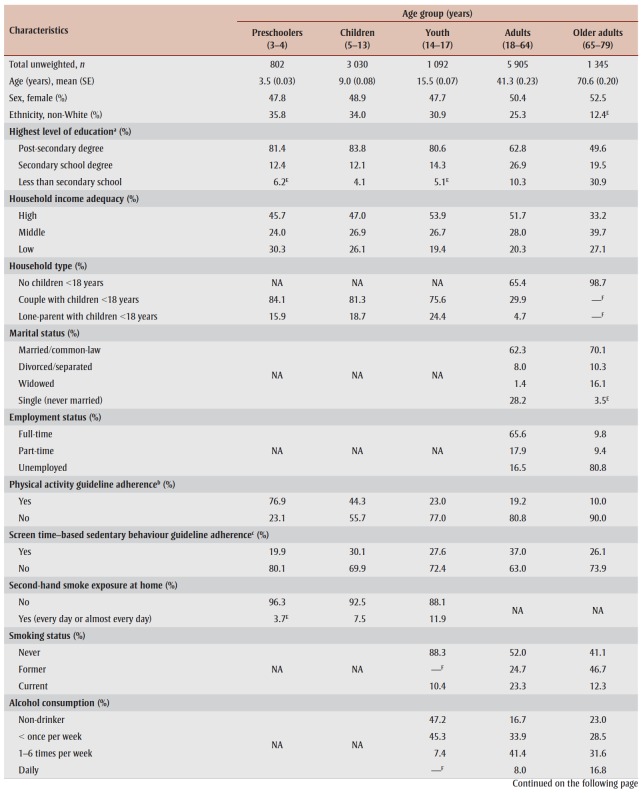
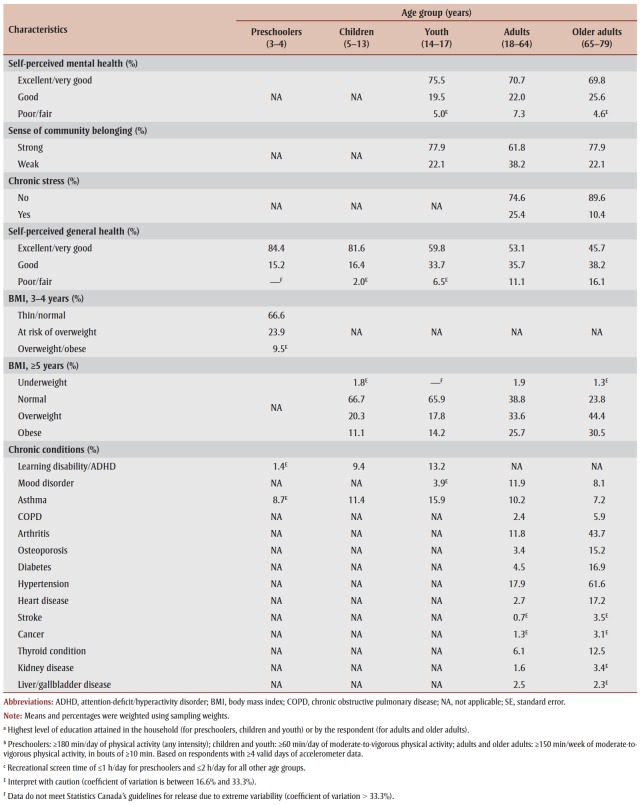
Characteristics of participants in each age group are shown in Table 1. The study sample (n = 12 174) represented approximately 31.6 million Canadians aged 3–79 years. The proportion of Canadians who slept for the recommended amount of time decreased across life stages (p-trend < .001), from 81% of preschoolers and 77% of children to 68%, 63% and 53% of youth, adults and older adults, respectively (Figure 1). The prevalence of short sleep duration increased from approximately 20% in preschoolers and children to 29% in youth and 34% in adults and 32% in older adults. Less than 5% of Canadians in each age group reported sleeping longer than the recommended range, with the exception of older adults (15%).
Table 1. Characteristics of the study population, by age group, 2009–2013, Canadian Health Measures Survey.
Figure 1. Proportion of the population in different sleep duration categories, by age group, 2009–2013, Canadian Health Measures Survey.
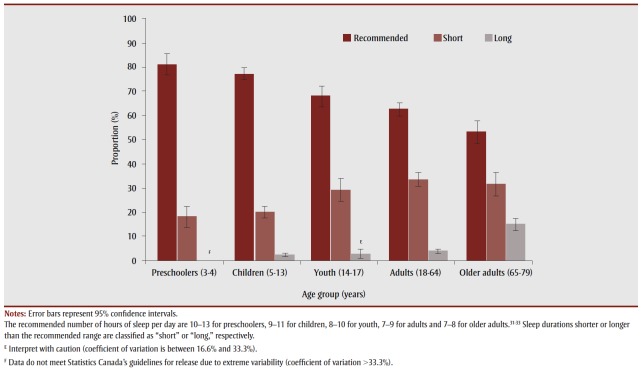
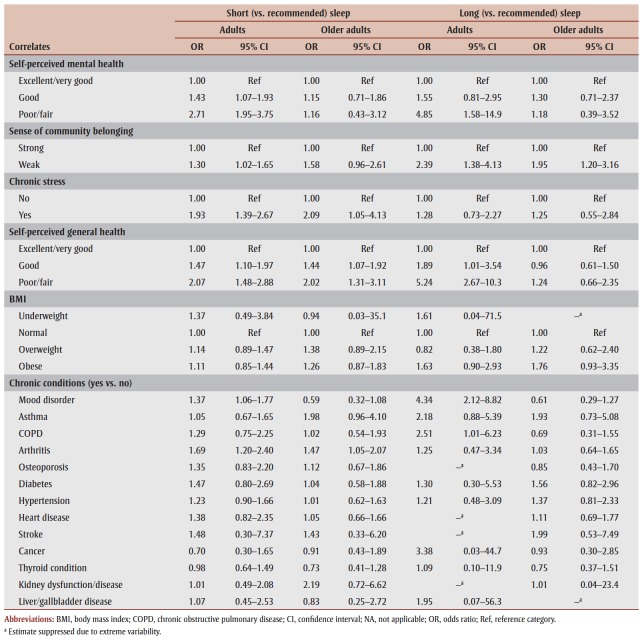
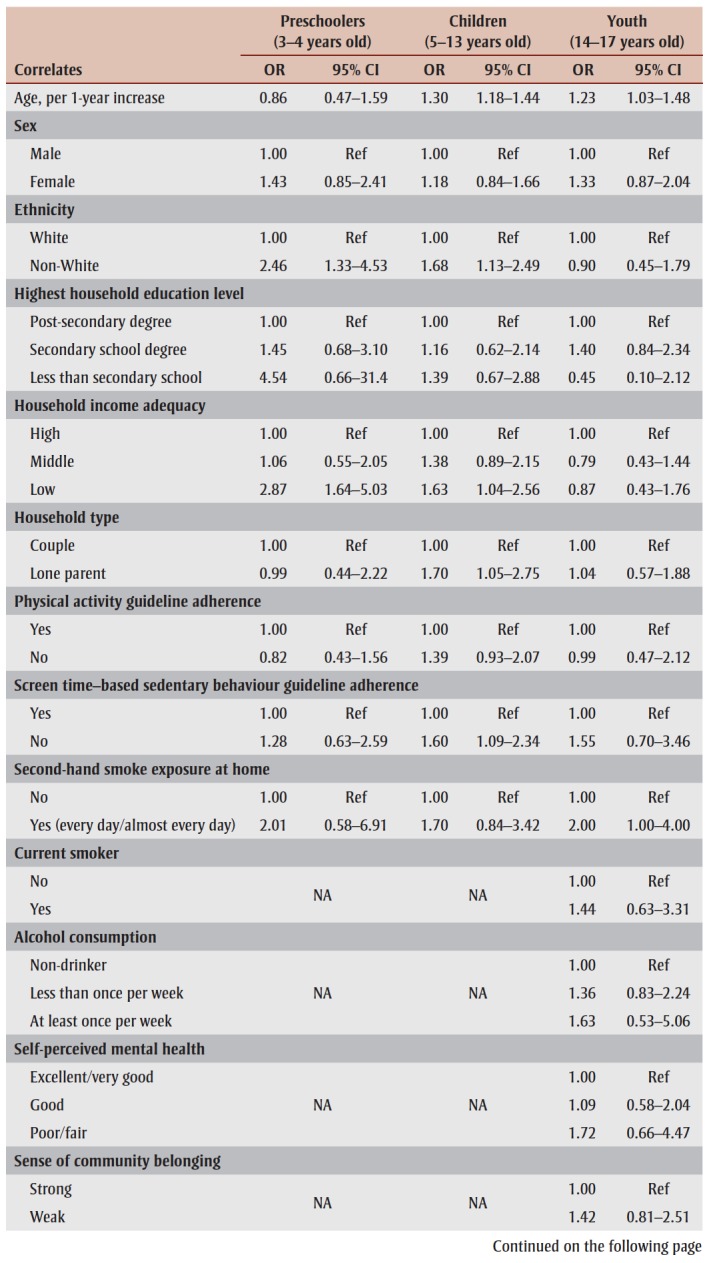
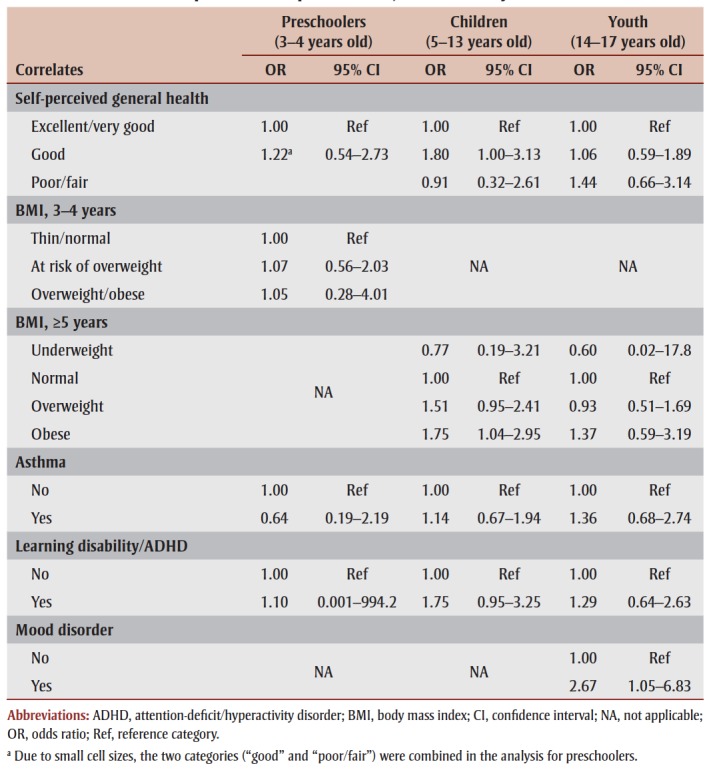
Unadjusted associations between potential correlates and short and long sleep are shown in Tables 2 and 3.
Table 2. Crude (unadjusted) logistic regression models for correlates of short (vs. recommended) sleep duration in preschoolers, children and youth.
|
Table 3. Crude (unadjusted) logistic regression models for correlates of short and long sleep duration in adults (18–64 years) and older adults (65–79 years).
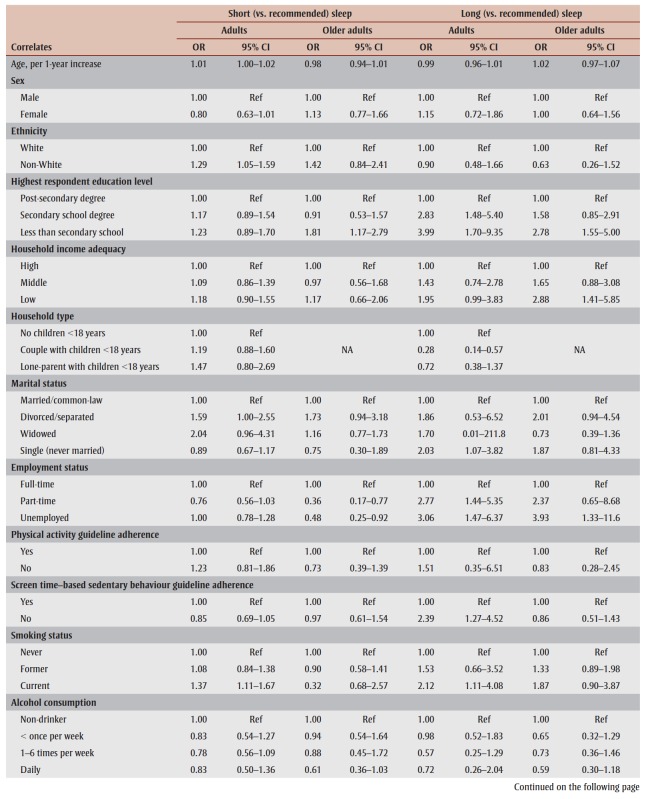
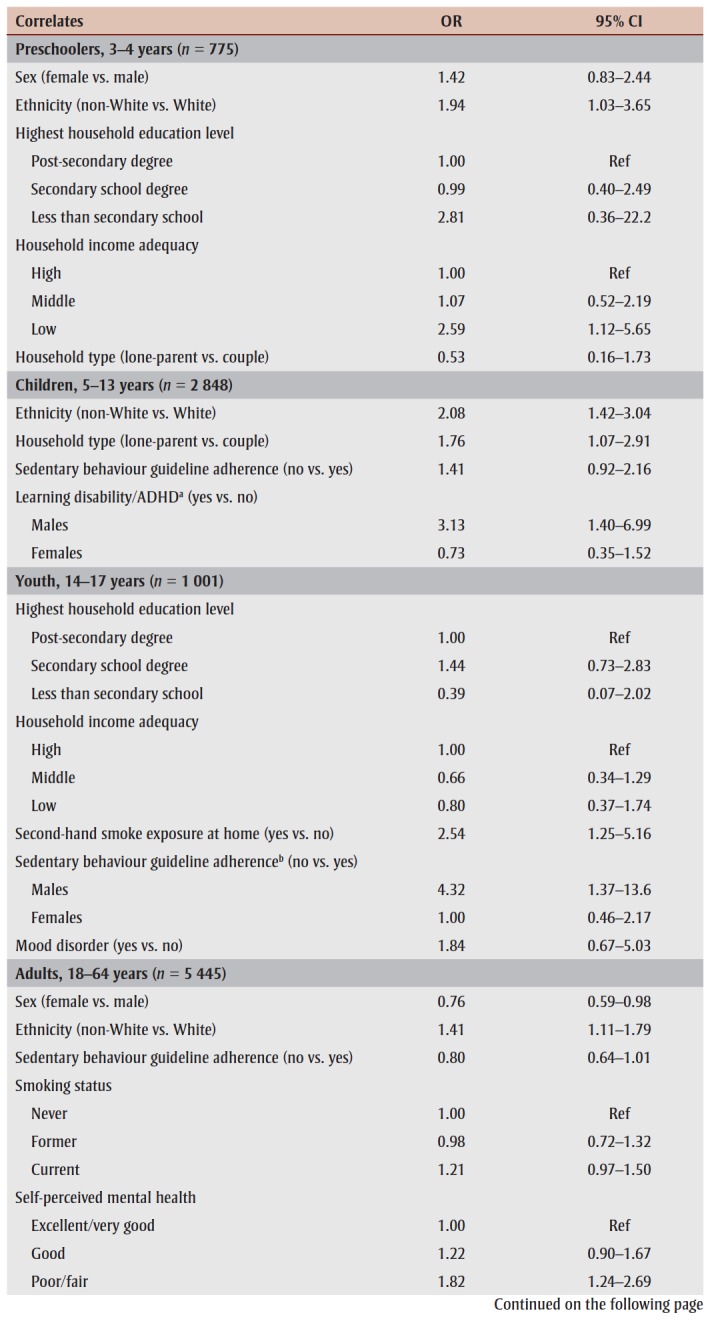
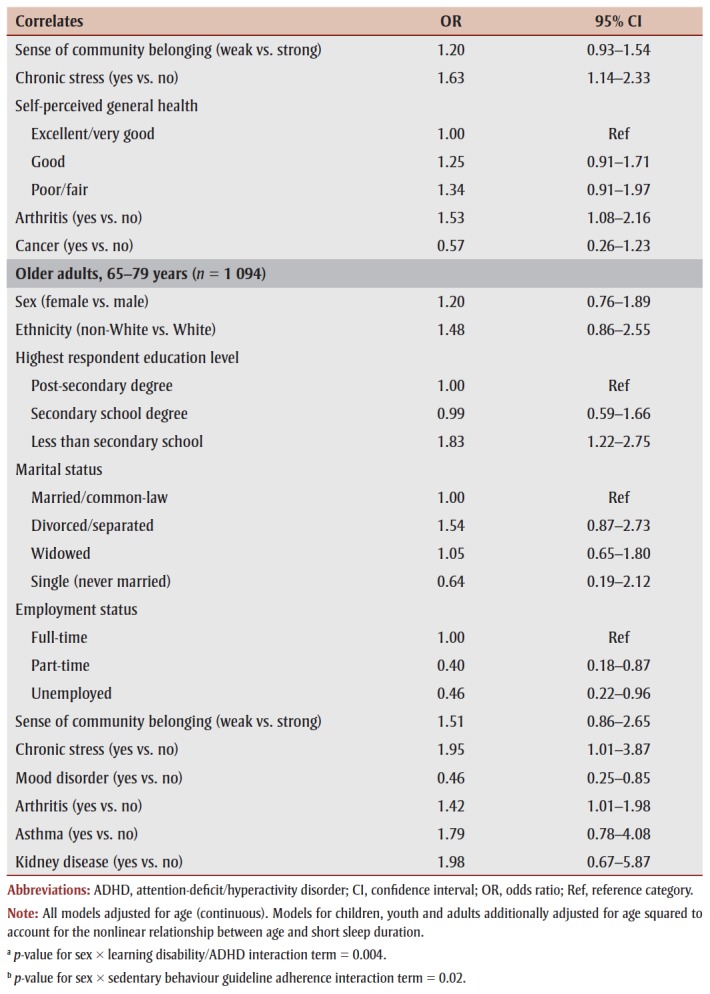
Table 4 presents life stage–specific multivariable models for correlates of short sleep. Among preschoolers, ethnicity (non-White vs. White; OR = 1.94, 95% confidence interval [CI]: 1.03–3.65) and household income adequacy (low vs. high; OR = 2.59, 95% CI: 1.12–5.65) were significantly associated with short sleep. Children who were non-White (OR = 2.08, 95% CI: 1.42–3.04) or living in a lone-parent household (OR = 1.76, 95% CI: 1.07–2.91), as well as youth regularly exposed to second-hand smoke at home (OR = 2.54, 95% CI: 1.25–5.16), had significantly higher odds of short sleep. In addition, interactions with sex (p < .05) were noted for learning disability/ ADHD in children and screen time– based sedentary behaviour in youth, with significant associations observed among boys only. Chronic stress in both adults (OR = 1.63, 95% CI: 1.14–2.33) and older adults (OR = 1.95, 95% CI: 1.01–3.87); arthritis in both adults (OR = 1.53, 95% CI: 1.08–2.16) and older adults (OR = 1.42, 95% CI: 1.01–1.98); being non-White (OR = 1.41, 95% CI: 1.11–1.79) and having poor/fair self-perceived mental health (OR = 1.82, 95% CI: 1.24–2.69) in adults; and less than secondary school education (OR = 1.83, 95% CI: 1.22–2.75) in older adults were all significantly associated with short sleep (Table 4). Conversely, female (vs. male) adults (OR = 0.76, 95% CI: 0.59–0.98) and older adults who were unemployed (OR = 0.46, 95% CI: 0.22– 0.96) or employed part-time (OR = 0.40, 95% CI: 0.18–0.87) and those with a mood disorder (OR = 0.46, 95% CI: 0.25– 0.85) were less likely to have short sleep.
Table 4. Multivariable logistic regression models for correlates of short (vs. recommended) sleep duration in preschoolers, children, youth, adults and older adults.
|
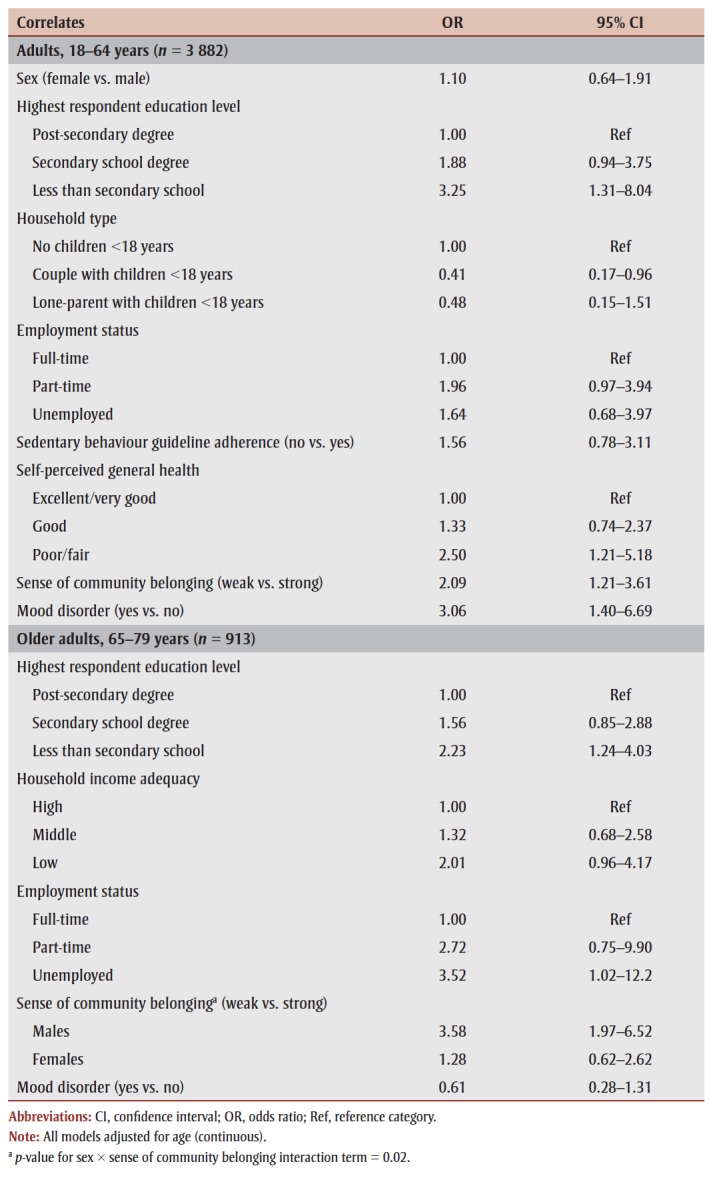
Table 5 presents multivariable models for correlates of long sleep among adults and older adults. In both age groups, less than secondary school education (vs. post-secondary degree) was significantly associated with long sleep. Adults living as a couple with children younger than 18 years (vs. no children) were less likely (OR = 0.41, 95% CI: 0.17–0.96) to have longer sleep than the recommended duration, while unemployed (vs. employed) older adults were more likely (OR = 3.52, 95% CI: 1.02–12.2) to sleep longer than the recommended duration. A weak sense of community belonging (OR = 2.09, 95% CI: 1.21–3.61), poor/fair self-perceived general health (OR = 2.50, 95% CI: 1.21– 5.18) and mood disorder (OR = 3.06, 95% CI: 1.40–6.69) in adults, as well as a weak sense of community belonging in older men (OR = 3.58, 95% CI: 1.97–6.52) were also associated with long sleep.
Table 5. Multivariable logistic regression models for correlates of long (vs. recommended) sleep duration in adults and older adults.
 |
Discussion
Even at a young age, a large proportion of Canadians do not get the recommended amount of sleep, with a prevalence of short sleep duration ranging from approximately one-fifth of preschoolers and children to one-third of youth, adults and older adults. In contrast, long sleep duration is relatively uncommon except in older adults.
Our analysis of a large-scale populationbased survey identified a wide range of factors associated with short and long sleep at different stages of life. Notably, sociodemographic factors (e.g., ethnicity, household income, lone-parent household) appeared to play a stronger role in determining sleep duration in preschoolers and children, whereas environmental and lifestyle factors (e.g., second-hand smoke exposure, screen time–based sedentary behaviour) may be more important in youth. In addition to sociodemographic factors (e.g., education, employment status), several psychosocial and healthrelated factors, including arthritis, chronic stress, mood disorder, self-perceived general or mental health and sense of community belonging, were found to be associated with short and/or long sleep among adults and older adults.
The prevalence estimates of short sleep duration in our study are similar to those reported previously in Canada4,5,41 and the USA,18,42 although differences in age groupings and methods of assessing sleep duration may have contributed to some inconsistencies. For example, based on child-reported sleep duration averaged across all days of the week, a 2016 Canadian study found that short sleepers were more common among children aged 10–13 years (31%) than among those aged 14–17 years (26%),3 whereas short sleepers were more common among youth aged 14–17 years (29%) than among children aged 5–13 years (20%) in our study.
Our results for the associations between sociodemographic factors and short sleep duration in the younger age groups are in line with previous research.17,43 For example, a recent United States birth cohort study showed that low maternal education, low household income and ethnicity (Black, Hispanic and Asian vs. White children) were associated with chronic sleep curtailment from infancy to mid-childhood. 17 The influence of sociocontextual factors on sleep at a young age may be related to variations in bedtime routines or behaviours (e.g., regular bedtime, parent– child interactive routines) across families of different structures (e.g., lone-parent vs. couple), cultures and socioeconomic status,44,45 as well as factors such as family stress and the living/bedroom environment (e.g., noise, crowding).17,18 Furthermore, our findings support existing evidence on the links between learning disability/ADHD and sleep deprivation or disturbances in children, possibly relating to shared neurobiological pathways and effects of ADHD medications.46,47 In particular, the significant association noted in boys alone is consistent with studies reporting a higher prevalence of sleep problems in boys (vs. girls) with ADHD.48,49However, a more detailed examination of sleep in relation to specific subtypes of learning disability/ADHD in boys and girls is warranted to further understand the moderating role of gender.49
While active smoking has been previously linked to short sleep duration and sleep problems among adolescents,50,51 our study is one of the very few demonstrating an association between second-hand smoke exposure and short sleep duration in this age group. These results are similar to a recent British Columbia study that assessed overall second-hand smoke exposure rather than exposure in the home environment.52 Possible mechanisms through which second-hand smoke exposure may interfere with sleep include nicotine-stimulating effect, nicotine withdrawal at night and disruption of pulmonary function.52,53 Future studies, including those with objective measures of secondhand smoke, are warranted to confirm these findings.
Despite evidence suggesting that screen time is inversely associated with sleep duration in children and adolescents,54 we only found a significant association among male youth. Sex has also been noted as an effect modifier in several other studies where male adolescents were more likely to show an association between television watching and short sleep compared to female adolescents.54,55 These age and gender differences may be related to the type and timing (e.g., bedtime) of screen time exposure.
In addition to sociodemographic characteristics, psychosocial and mental health– related factors appeared to play an important role in sleep duration among adults and older adults in our study. These findings are consistent with previous research,23-26 although it should be noted that the relationship between mental health and sleep is bidirectional and likely involves a complex interplay between biological and behavioural factors.56 Notably, in contrast to studies reporting associations between lifestyle/ behavioural factors and sleep duration in adults,22-24 these factors were not significant in our study, although unadjusted models suggested a possible link between current smoking and both short and long sleep in adults (Table 3).
Our results also highlight the importance of examining specific determinants of both short and long sleep durations. For example, while a high level of self-perceived lifetime stress (possibly a marker of coping ability) was associated with short sleep, having been diagnosed with a mood disorder (e.g., depression) was associated with long sleep, suggesting different measures or domains of mental health may affect sleep differently. Moreover, the association between arthritis and short sleep observed in both adults and older adults is likely mediated through pain-related sleep problems.57 Finally, our finding of an association between sense of community belonging and long sleep is novel and warrants additional research with regard to the role of community-level factors (e.g., social support) contributing to healthy sleep durations, including potential sex differences.
Strengths and limitations
Strengths of our study included the population- based design, large sample size, use of evidence-informed recommendations to define sleep duration categories,31-33 detailed assessment of a wide range of factors associated with both short and long sleep, and investigation of the associations, including potential sex differences, by life stage.
Our study had several limitations. First, sleep duration was assessed based on selfor parent/guardian-reported information, which has generally been shown to overestimate actual sleep duration and potentially bias the observed relationships between sleep duration and related factors or health outcomes.58,59 Including objective measurements of sleep, such as actigraphy- assessed sleep duration, may help reduce bias associated with measurement errors in future studies.58 Similarly, with the exceptions of body mass index and physical activity, all other factors were assessed by self- or parent/guardianreports, which were subject to social desirability and recall bias.
Second, given the cross-sectional nature of the CHMS, the temporality of associations could not be established. For example, while chronic stress may have contributed to short sleep duration among adults and older adults, it is also possible that inadequate sleep resulted in chronic stress.
Third, due to insufficient sample size, young adults (aged 18–24 years) were not examined as a separate life stage in our analyses; this age group may have distinct sleep patterns and correlates of sleep duration that warrant further research.
Fourth, the sleep questionnaire in the CHMS did not include details such as time spent napping and sleep duration on weekdays compared to weekends, which may provide additional insights into the role of different factors in determining sleep duration. Finally, despite the broad range of potential correlates evaluated, the CHMS lacked information on other factors that may affect sleep duration, such as shift work, caffeine intake and the bedroom environment.
Conclusion
Short sleep duration is highly prevalent among Canadians across all stages of life. The present study provides the first detailed examination of correlates of sleep duration in a nationally representative sample of Canadians. Although more research is needed to disentangle the complex interrelations between various factors and sleep, surveillance efforts should continue to monitor sleep and related factors to inform public policies aimed at promoting healthy sleep duration across life stages.
Acknowledgements
The CHMS was conducted by Statistics Canada in partnership with Health Canada and the Public Health Agency of Canada with funding from the Canadian federal government. No external funding was obtained for this study.
Conflicts of interest
The authors declare no conflicts of interest.
Authors’ contributions and statement
VC and MD conceptualized the study. VC conducted the data analyses, interpreted the results and drafted the manuscript. JC, KR, GJ and MD contributed to the interpretation of results and critically reviewed and revised the manuscript. All authors approved the final version submitted.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Grandner MA, et al. Sleep duration across the lifespan: implications for health. Sleep Med Rev. 2012 doi: 10.1016/j.smrv.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colten HR, Altevogt BM, et al. Colten HR, Altevogt BM, editors. Institute of Medicine Committee on Sleep Medicine and Research. 2006 [Google Scholar]
- Chaput JP, Janssen I, et al. Sleep duration estimates of Canadian children and adolescents. J Sleep Res. 2016 doi: 10.1111/jsr.12410. [DOI] [PubMed] [Google Scholar]
- Michaud I, Chaput JP, et al. Are Canadian children and adolescents sleep deprived. Public Health. 2016:126–9. doi: 10.1016/j.puhe.2016.09.009. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Wong SL, Michaud I, et al. Duration and quality of sleep among Canadians aged 18 to 79. Duration and quality of sleep among Canadians aged 18 to 79. Health Rep. 2017 [PubMed] [Google Scholar]
- Hafner M, Stepanek M, Taylor J, Troxel WM, Stolk C, Health Q, et al. Why sleep matters – the economic costs of insuf¬ficient sleep: a cross-country compa¬rative analysis. Rand Health Q. 2017 [PMC free article] [PubMed] [Google Scholar]
- Hillman DR, Lack LC, et al. Public health implications of sleep loss: the com¬munity burden. Med J Aust. 2013 doi: 10.5694/mja13.10620. [DOI] [PubMed] [Google Scholar]
- Knutson KL, Turek FW, et al. The U-shaped association between sleep and health: the 2 peaks do not mean the same thing. Sleep. 2006 doi: 10.1093/sleep/29.7.878. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA, Heart J, et al. Sleep dura¬tion predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011 doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- Shan Z, Ma H, Xie M, et al, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015 doi: 10.2337/dc14-2073. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Gray CE, Poitras VJ, et al, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016 doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- Watson NF, Badr MS, Belenky G, et al, et al. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and dis¬cussion. Sleep. 2015 doi: 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon GM, Thompson JM, Han DY, et al, et al. Short sleep duration in middle childhood: risk factors and conse¬quences. Sleep. 2008 doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hense S, Barba G, Pohlabeln H, et al, et al. Factors that influence weekday sleep duration in European children. Sleep. 2011 doi: 10.1093/sleep/34.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Zhu S, Jin X, et al, et al. Risk factors associated with short sleep duration among Chinese school-aged children. Sleep Med. 2010 doi: 10.1016/j.sleep.2010.03.018. [DOI] [PubMed] [Google Scholar]
- Marinelli M, Sunyer J, Pedrerol M, et al, et al. Hours of television viewing and sleep duration in child¬ren: a multicenter birth cohort study. JAMA Pediatr. 2014 doi: 10.1001/jamapediatrics.2013.3861. [DOI] [PubMed] [Google Scholar]
- a MM, Rifas-Shiman SL, Gillman MW, Redline S, Taveras EM, et al. Racial/ ethnic and socio-contextual correlates of chronic sleep curtailment in child¬hood. Sleep. 2016 doi: 10.5665/sleep.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smaldone A, Honig JC, Byrne MW, et al. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics. 2007 doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S, et al. Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related cha¬racteristics. Sleep Med. 2011 doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T, Wu Z, Shen Z, Zhang J, Shen X, Li S, et al. Sleep duration in Chinese ado¬lescents: biological, environmental, and behavioral predictors. Sleep Med. 2014 doi: 10.1016/j.sleep.2014.05.018. [DOI] [PubMed] [Google Scholar]
- Bauducco SV, Flink IK, jmark M, Linton SJ, et al. Sleep duration and patterns in adolescents: correlates and the role of daily stressors. Sleep Health. 2016 doi: 10.1016/j.sleh.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Ohida T, Kamal AM, Uchiyama M, et al, et al. The influence of lifestyle and health status factors on sleep loss among the Japanese general popula¬tion. Sleep. 2001 doi: 10.1093/sleep/24.3.333. [DOI] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM, et al. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009 doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon HS, Yang JJ, Song M, et al, et al. Correlates of self-reported sleep dura¬tion in middle-aged and elderly Koreans: from the Health Examinees Study. PLoS One. 2015 doi: 10.1371/journal.pone.0123510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Sotres-Alvarez D, eda SF, et al, et al. Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015 doi: 10.5665/sleep.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stranges S, Dorn JM, Shipley MJ, et al, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008 doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MA, Gradisar M, Lack LC, et al, et al. A cross-cultural comparison of sleep duration between U.S. Health Educ Behav. 2013 doi: 10.1177/1090198112451266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Katzmarzyk PT, LeBlanc AG, et al, et al. Associations between sleep patterns and lifestyle behaviors in children: an international compari¬son. Int J Obes Suppl. 2015 doi: 10.1038/ijosup.2015.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Health Measures Survey [CHMS] data user guide: cycle 2. Statistics Canada. 2013 [Google Scholar]
- Canadian Health Measures Survey [CHMS] data user guide: cycle 3. Statistics Canada. 2015 [Google Scholar]
- Tremblay MS, Chaput JP, Adamo KB, et al, et al. Canadian 24-Hour Movement Guidelines for the Early Years [0–4 years]: an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017 doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay MS, Carson V, Chaput JP, et al, et al. Canadian 24-Hour Movement Guidelines for Children and Youth: an integration of physical activity, seden¬tary behaviour, and sleep. Appl Physiol Nutr Metab. :41[6 Suppl 3]:S311–27. doi: 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, et al, et al. National Sleep Foundation’s sleep time duration recommenda¬tions: methodology and results sum¬mary. Sleep Health. 2015 doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Canadian Health Measures Survey [CHMS] derived variable [DV] specifications: cycle 2. Statistics Canada. 2012 [Google Scholar]
- Canadian Physical Activity and Sedentary Behaviour Guidelines. Canadian Society for Exercise Physiology. 2012 [Google Scholar]
- WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J, et al. Development of a WHO growth refe¬rence for school-aged children and adolescents. Bull World Health Organ. 2007 doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obesity: preventing and managing the global epidemic: report of a WHO consulta¬tion. World Health Organization. 2000 [PubMed] [Google Scholar]
- Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE, nd ed, et al. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. 2012 [Google Scholar]
- Maldonado G, Greenland S, et al. Simulation study of confounder-selection strate¬gies. Am J Epidemiol. 1993 doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Colley RC, Aubert S, et al, et al. Proportion of preschool-aged children meeting the Canadian 24-Hour Movement Guidelines and associa¬tions with adiposity: results from the Canadian Health Measures Survey. BMC Public Health. 2017 doi: 10.1186/s12889-017-4854-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB, et al. Prevalence of healthy sleep duration among adults—United States, 2014. Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. 2016 doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- Barazzetta M, Ghislandi S, et al. Family income and material deprivation: do they matter for sleep quality and quantity in early life. Sleep. 2017 doi: 10.1093/sleep/zsw066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J, et al. Social and demogra¬phic predictors of preschoolers’ bed¬time routines. J Dev Behav Pediatr. 2009 doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CH, Ball H, et al. Exploring socioeco¬nomic differences in bedtime beha¬viours and sleep duration in English preschool children. Infant Child Dev. 2014 doi: 10.1002/icd.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk J, et al. Sleep disorders in children and adolescents with learning disabi¬lities and their management. Adv Ment Health Learn Disabil. 2010 [Google Scholar]
- Tsai MH, Hsu JF, Huang YS, et al. Sleep problems in children with attention deficit/hyperactivity disorder: current status of knowledge and appropriate management. Curr Psychiatry Rep. 2016 doi: 10.1007/s11920-016-0711-4. [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ, Shrout PE, vez L, et al, et al. ADHD and gender: are risks and sequela of ADHD the same for boys and girls. J Child Psychol Psychiatry. 2007 doi: 10.1111/j.1469-7610.2007.01750.x. [DOI] [PubMed] [Google Scholar]
- Fisher BC, Garges DM, Yoon SY, Maguire K, Zipay D, Gambino M, et al. Sex differences and the interaction of age and sleep issues in neuropsychologi¬cal testing performance across the lifespan in an ADD/ADHD sample from the years 1989 to 2009. Fisher BC, Garges DM, Yoon SY, Maguire K, Zipay D, Gambino M. 2014 doi: 10.2466/15.10.PR0.114k23w0. [DOI] [PubMed] [Google Scholar]
- Patten CA, Choi WS, Gillin JC, Pierce JP, et al. Depressive symptoms and ciga¬rette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000 doi: 10.1542/peds.106.2.e23. [DOI] [PubMed] [Google Scholar]
- McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS, et al. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011 doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- Schwartz J, Bottorff JL, Richardson CG, et al. Secondhand smoke exposure, restless sleep, and sleep duration in adolescents. Sleep Disord. 2014:374732–85. doi: 10.1155/2014/374732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabanayagam C, Shankar A, et al. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011 doi: 10.1016/j.sleep.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Guan S, et al. Screen time and sleep among school-aged children and adolescents: a systematic litera¬ture review. Sleep Med Rev. 2015:50–8. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega FB, n P, Ruiz JR, et al, et al. Sleep patterns in Spanish adoles¬cents: associations with TV watching and leisure-time physical activity. Eur J Appl Physiol. 2010 doi: 10.1007/s00421-010-1536-1. [DOI] [PubMed] [Google Scholar]
- Kahn M, Sheppes G, Sadeh A, et al. Sleep and emotions: bidirectional links and underlying mechanisms. Int J Psychophysiol. 2013 doi: 10.1016/j.ijpsycho.2013.05.010. [DOI] [PubMed] [Google Scholar]
- Parmelee PA, Tighe CA, Dautovich ND, et al. Sleep disturbance in osteoarthri¬tis: linkages with pain, disability, and depressive symptoms. Arthritis Care Res [Hoboken] 2015 doi: 10.1002/acr.22459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ, et al. Sleep duration: how well do self-reports reflect objec¬tive measures. Epidemiology. 2008 doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayyat EA, Spruyt K, Molfese DL, Gozal D, et al. Sleep estimates in children: parental versus actigraphic assess¬ments. Nat Sci Sleep. 2011 doi: 10.2147/NSS.S25676. [DOI] [PMC free article] [PubMed] [Google Scholar]