Abstract
Objective:
To describe a new measure, the unintended pregnancy risk index (UPRI), which is based primarily on attitudinal and behavioral measures of women’s prospective pregnancy desire, and compare it to the unintended pregnancy rate, typically calculated retrospectively.
Study design:
We used three rounds of the National Survey of Family Growth to calculate trends in the UPRI and compare it to the retrospective rate. The UPRI estimates the annual risk of becoming unintentionally pregnant on a scale from 0 to 100. It is based on women’s prospective pregnancy desire as well as fecundity, sexual activity and contraceptive use patterns.
Results:
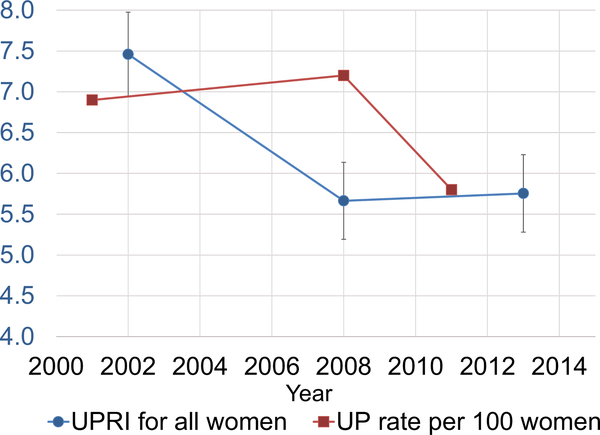
Among all women aged 15–34, the UPRI ranged from 7.4 in 2002 to 5.7 in 2013. The retrospective unintended pregnancy rate had similar levels and declines for the same overall period, although the UPRI declined earlier than the retrospective rate.
Conclusions:
Changes in the use of any contraceptive method, the methods used and the effectiveness of the methods used all contributed to the decline in the UPRI.
Implications:
The sufficiency of retrospective measures of pregnancy intention has been challenged, and data availability has constrained needed surveillance of the unintended pregnancy rate. The UPRI offers a new measure that can be calculated with existing national surveillance data or for any population for which data on prospective pregnancy desire, pregnancy risk and contraceptive use are available.
Keywords: Unintended pregnancy, Contraception, Sexual behavior, Prospective measurement
1. Introduction
The rate of unintended pregnancy in a population is a key reproductive health measure. Births that follow unintended conceptions have been found to be associated with increased risk of many negative health and social outcomes, independently or because of their association with women’s disadvantaged social and economic status [1–3]. The unintended pregnancy rate in the United States decreased substantially between 2008 and 2011 but is relatively high [4], and large disparities by income and race/ethnicity remain [4]. For these reasons, reducing the unintended pregnancy rate remains a national public health goal [5].
However, the limitations of and the potential for improvements to the measurement of unintended pregnancy have been the focus of extensive research and critical debate [2,6–9]. For one, traditional estimates of national unintended pregnancy rates combine information about births and miscarriages from the National Survey of Family Growth (NSFG), a nationally representative in-person survey of women and men aged 15–44, with data about abortions from other sources because abortions are underreported in the NSFG. This methodology has permitted consistent tracking of trends in the unintended pregnancy rate over time [4,10–12], but it is also data-intensive.
In the past, the NSFG was conducted periodically (about every 7 years), making it difficult to produce updated estimates of unintended pregnancy rates in a timely manner. In 2006, the NSFG switched to a continuous format, collecting data year-round in an uninterrupted fashion [13]. However, the surveys of abortion providers and patients are undertaken less frequently — once every 6 years — due to the substantial cost and effort necessary to field them [14,15]. Thus, despite the shift to more frequent NSFG data, the requirement for external data on induced abortion still limits frequent monitoring of unintended pregnancy rates. In addition, to measure intendedness, the NSFG asks each respondent to retrospectively recall whether she had wanted to have a baby right before she conceived each of the pregnancies she experienced [16,17]. The retrospective measure has been critiqued because of the potential for recall bias [18,19].
The limitations of the traditional measure highlight the need for measures that approach the concept of intendedness from new angles. A measure that looks at pregnancy desire prospectively — before the woman has become pregnant — and incorporates both behavioral and affective measures could provide a strong complement to existing retrospective measures. Moreover, since nonuse and sporadic use of contraception are major contributors to unintended pregnancy [20], we see value in situating these factors within the context of other factors that define the population at risk of unintended pregnancy, such as fecundity and pregnancy desire.
To respond to the need for more frequent surveillance of unintended pregnancy rates and improve our understanding of intendedness, we develop a methodology for estimating an alternate measure of unintended pregnancy based solely on NSFG data, which we term an unintended pregnancy risk index (UPRI). This measure is an extension of prior research developing and refining a pregnancy risk index (PRI), which combines the risk from sexual activity, protection from contraceptive method use and the method failure rate into one quantity. The PRI appears to be a valid measure for examining trends in pregnancy risk across multiple data sources and populations [21–25]. The UPRI incorporates information on women’s self-reported current contraceptive use (such women are assumed to be seeking to avoid pregnancy), the prospectively reported pregnancy intentions among those not using and the estimated effectiveness of their contraception. By relying on data solely from the NSFG, the UPRI is a simpler, quicker measure that can be produced soon after the NSFG is released, in contrast to the unintended pregnancy rate, which requires supplemental data and analyses.
This paper provides the first evaluation of the validity and usefulness of the UPRI as a surveillance and analytical tool. We contrast the trends and patterns of demographic subgroup differentials estimated with this new methodology against the retrospective methodology that uses the full complement of data sources and the retrospectively reported pregnancy intentions. Finally, we use statistical decomposition to attribute changes in the UPRI to changes in contraceptive use patterns and changes in contraceptive effectiveness.
2. Materials and methods
2.1. Data
The NSFG is a national probability survey of the noninstitutionalized population of men and women aged 15–44 in the United States [17,26]. The NSFG uses a multistage, stratified, clustered sampling frame. Interviews included in this analysis were conducted from January 2002 to March 2003 and then continuously from June 2006 to June 2010 and September 2011 to September 2015; we include data from each year within the data collection periods, but for simplicity, we refer to the midpoints in each of these period in our analyses of trends: 2002, 2008 and 2013, respectively. Methods of data collection and dissemination of the public-use dataset were reviewed by NCHS’s Institutional Review Board. All analyses were limited to women aged 15–34 at the time of the interview (N=22,047 over the three periods), as impaired fecundity and infertility are much higher after age 35 [27–29]. Earlier research suggests that unreported infecundity among women aged 35–44 incorrectly inflates the pregnancy risk index [24] and thus, presumably, the UPRI.
2.2. Measures
We calculated the UPRI for each period estimating the annual risk of becoming unintentionally pregnant on a scale from 0 to 100. We calculated the UPRI separately for all women overall and those at risk of unintended pregnancy (defined as being fecund,1 sexually active during the interview month, not surgically sterilized, neither currently pregnant nor postpartum, and not seeking pregnancy). Women using contraception were included in the latter group since they were considered conceptually to be “at risk” due to their efforts to prevent unintended pregnancy. In the overall estimate, individuals not included in these parenthetical groups were assigned a UPRI of zero, as they were not exposed to the risk of unintended pregnancy. Although there are other measures of sexual activity that are available, such as whether the respondent was sexually active in the past 3 months [30], we considered the 1-month measure to be most analogous to the contraceptive use measure, which focuses on the month of interview. We consider contraceptive use to be a behavioral indicator of the desire to avoid pregnancy; for women in this category, who comprise the majority of women, their specific UPRI was estimated as the contraceptive failure rate (CFR) for the contraceptive method used during the interview month [31]. Among women using more than one method, the UPRI score was calculated as the product of the two most effective methods’ CFRs, following an approach used by researchers previously [23]. Nonusers of contraception were asked, “Is the reason you are not using a method of birth control now because you, yourself, want to become pregnant as soon as possible?” Women reporting that they wanted to become pregnant were assigned a risk of zero in the UPRI for all women and were excluded from the analytic sample limited to at-risk women. Women who were sexually active and not using a method but not wanting to become pregnant were assigned a CFR of 85% based on published estimates of the risk of pregnancy from noncontraceptive use [32]; all of these pregnancies would be considered unintended and included in the UPRI. The overall UPRI was then estimated as the mean of all women’s individual scores, while the estimate for those at risk of unintended pregnancy was restricted to the scores from the subset of at-risk women.
This analysis used published typical-use first-year CFRs from 2002 and 2008, calculated from the 2002 NSFG and 2006–2010 NSFG, respectively [31,33]. Typical-use CFRs are the number of pregnancies occurring among 100 women using a specific contraceptive method within 12 months of initiating use. They reflect both the intrinsic efficacy of contraceptive methods as well as the challenges women experience using methods consistently and correctly. Given recent research that suggests significant variation in CFRs by race, we used race-specific CFRs that were available for three methods: pill, condom and withdrawal. Otherwise, overall CFRs were used (see Table 1).
Table 1.
| Method typee | 2002c |
2008d |
|---|---|---|
| % | ||
| Female sterilization | 0.5 | 0.5 |
| Male sterilization | 0.2 | 0.2 |
| IUD | 3.2 | 1.4 |
| Implant | 3.2 | 1.4 |
| Injectable | 6.7 | 4.0 |
| Pill | 8.7 | 7.2 |
| Non-Hispanic white | - | 6.1 |
| Non-Hispanic black | - | 13.1 |
| Hispanic | - | 9.5 |
| Patch | 8.7 | 7.2 |
| Ring | 8.7 | 7.2 |
| Rhythm | 25.3 | 13.0 |
| Condom | 17.4 | 12.6 |
| Non-Hispanic white | - | 8.7 |
| Non-Hispanic black | - | 20.7 |
| Hispanic | - | 19.3 |
| Diaphragm | 13.1 | 12.0 |
| Withdrawal | 18.4 | 19.9 |
| Non-Hispanic white | - | 21.4 |
| Non-Hispanic black | - | 18.3 |
| Hispanic | - | 21.9 |
| Spermicide | 28.1 | 28.0 |
| Nomethod | 85.0 | 85.0 |
Race-specific CFRs are provided where available. Unless otherwise specified, 2002 and 2008 data are from Kost et al., 2008, and Sundaram et al., 2017, respectively.
2008 CFRs are applied to the 2008 and 2013 NSFG data.
2002 CFRs for the IUD, implant, diaphragm and spermicide come from Ranjit et al., 2001.
2008 CFRs for female and male sterilization, diaphragm, spermicide and rhythm method come from Contraceptive Technology, 2011. Consistent with the earlier set of CFR estimates, the 2008 CFRs for patch and ring methods were set equal to the pill CFR estimate.
Most effective methods include female and male sterilization, IUD and implant. In addition to these methods, injectable, pill, patch and ring comprise more effective methods.
2.3. Analysis
Not all women are at risk of unintended pregnancy. To provide context, we examined each of the factors that contribute to unintended pregnancy risk (pregnancy status and pregnancy intention, fecundity and sexual activity) as well as the overall proportion of women aged 15–34 who were at risk for unintended pregnancy at each time point. We then limited our analysis to the group of women who were at risk, and because method use is a key factor driving unintended pregnancy risk for each woman, we calculated the percentage of sexually active women using each specific contraceptive method(s) at the time of the interview. We also focused on methods with lower CFRs (Table 1) to examine the percentage of sexually active women using more effective (i.e., IUD, implant, injectable, pill, patch and ring) and most effective (i.e., contraceptive sterilization and long-acting reversible contraception such as the IUD and implant) contraceptive methods. In order to understand what method-use changes might be driving changes in the UPRI, we used bivariate logistic regression to test for significant changes over time between adjacent periods (2002 vs. 2008 and 2008 vs. 2013) and across the whole time period (2002 vs. 2013).
We then took the method-specific CFR multiplied by the proportion of women using that method to calculate the mean UPRI among all women and among all women at risk of unintended pregnancy. The earlier failure rates were applied to the 2002 data, whereas 2008 CFRs wereused for 2008 and 2013. Among women at risk, we also calculated the UPRI by key demographics including age, race/ethnicity, marital status and income as a percentage of the federal poverty level. Paired t tests for the difference in means were used to test for significant changes over time. We also calculated the annualized percentage change over time using the formula ((UPRIt2/UPRIt1)(1/[t2−t1])) − 1.
To assess the extent to which the change in UPRI from 2002 to 2013 was due to changes in contraceptive failure rates or changes in contraceptive method mix, we used a standard demographic decomposition formula [34]. We calculated a standardized rate for both 2002 and 2013; the difference between the two is the amount we would expect the UPRI to change from 2002 to 2013 if only the failure rates had changed during that time. We then divided the change in standardized rate between the two time periods by the observed change in rate for the same time frame to estimate the proportion of the observed change in UPRI that was due to shifts in contraceptive failure rates. The expected proportion of change due to contraceptive method mix was calculated as the complement. We used sampling weights provided by the National Center for Health Statistics with the svy command prefix in Stata 14.1 to adjust for the complex survey design of the NSFG data [35].
Finally, to visually inspect the comparability of the trends in the UPRI to previously estimated trends in the unintended pregnancy rate, we graphed the mean UPRI among all women along with estimates of the retrospective unintended pregnancy rate among women aged 15–34 years [4,36].
3. Results
Table 2 presents the percentage of women aged 15–34 years by pregnancy intention, pregnancy status and sexual activity. Overall, there was little change in these measures. For all time periods, more than 95% of women were not seeking pregnancy at the time of interview, and the vast majority of women were not currently pregnant and did not report that they were infecund. Between 2002 and 2008, there were small but statistically significant declines in sexual activity in the last 3 months, in the last 4 weeks, and in the month of the interview, but these measures increased slightly or remained steady between 2008 and 2013. Over the full time period, there was a significant increase in the proportion of women fecund, neither currently pregnant nor postpartum, and not seeking pregnancy. Among these women, the percentage who were sexually active in the month of the interview declined significantly between 2002 and 2008 and then increased significantly between 2008 and 2013, with no resulting difference between 2002 and 2013.
Table 2.
Percentage of women aged 15–34 by pregnancy intention, pregnancy status and sexual activity across NSFG survey year, 2002–2013
| Characteristic | Survey year (midpoint) |
Comparison between survey years |
||||
|---|---|---|---|---|---|---|
| 2002a n=5164 |
2008b n=8795 |
2013c n=8088 |
2002 vs. 2008 |
2008 vs. 2013 | 2002 vs. 2013 | |
| % | p value | |||||
| Pregnancy intention | ||||||
| Not seeking pregnancy | 96 | 97 | 96 | .65 | .45 | .72 |
| Fecundity | ||||||
| Fecundd | 98 | 98 | 98 | .02 | .68 | .03 |
| Pregnancy status | ||||||
| Not pregnant | 94 | 94 | 95 | .93 | .52 | .58 |
| Currently pregnant | 6 | 6 | 5 | .93 | .52 | .58 |
| Postpartum | 1 | 1 | 1 | .26 | .27 | .93 |
| Sexual activity | ||||||
| Ever had sex | 82 | 80 | 82 | .14 | .20 | .79 |
| In last 12 months | 75 | 75 | 75 | .54 | .67 | .84 |
| In last 3 months | 71 | 68 | 69 | .01 | .51 | .02 |
| In last 4 weeks | 63 | 60 | 61 | .02 | .69 | .06 |
| In month of interview | 62 | 58 | 60 | <.01 | .15 | .10 |
| Not seeking pregnancy, fecund, not currently pregnant and not postpartum | 87 | 88 | 88 | .20 | .67 | .37 |
| Among such women, percentage sexually active in month of interviewe | 59 | 55 | 57 | <.01 | .11 | .20 |
Refers to data collected in 2002–2003.
Refers to data collected in 2006–2010.
Refers to data collected in 2011–2015.
Individuals who were surgically sterilized for contraceptive purposes were considered fecund.
This is the sample analyzed in Table 3.
Contraceptive use patterns over the three time periods indicate a significant increase in the use of any method by sexually active women at risk of unintended pregnancy, with a countervailing significant decline in the share of women using no method (Table 3). Additionally, there was a statistically significant increase from 2002 to 2013 in the share of women reporting multiple method use (two or more methods) in the month of the interview.
Table 3.
Selected contraceptive method use among women aged 15–34 who were at risk of unintended pregnancya by NSFG survey year, 2002–2013
| Method use | Survey year (midpoint) |
Comparison between survey years |
||||
|---|---|---|---|---|---|---|
| 2002b n=2672 |
2008c n=4191 |
2013d n=3827 |
2002 vs. 2008 |
2008 vs. 2013 | 2002 vs. 2013 | |
| % | p value | |||||
| Number of methods usede | ||||||
| No method | 8 | 7 | 7 | .03 | .82 | .05 |
| ≥1 | 92 | 93 | 93 | .03 | .82 | .05 |
| ≥2 | 17 | 20 | 23 | .05 | .02 | <.01 |
| Method type | ||||||
| Sterilization | 16 | 17 | 14 | .63 | .04 | .08 |
| Female sterilization | 12 | 13 | 12 | .79 | .40 | .54 |
| Male sterilization | 4 | 5 | 3 | .55 | <.01 | .01 |
| More effective methodsf | 47 | 46 | 49 | .80 | .16 | .22 |
| IUD and implant | 3 | 7 | 14 | <.01 | <.01 | <.01 |
| Injectable, pill, patch and ring | 43 | 40 | 34 | .04 | <.01 | <.01 |
| IUD | 3 | 6 | 12 | <.01 | <.01 | <.01 |
| Implant | .4 | .5 | 3 | .79 | <.01 | <.01 |
| Injectable | 7 | 4 | 5 | <.01 | .64 | <.01 |
| Pill | 36 | 32 | 27 | .01 | <.01 | <.01 |
| Patch | 1 | 1 | .4 | .86 | .04 | .09 |
| Ring | 0 | 3 | 3 | - | .65 | - |
| Rhythm | 2 | 2 | 4 | .32 | <.01 | .01 |
| Condom | 31 | 35 | 32 | .05 | .08 | .65 |
| Diaphragm | .3 | 0 | .1 | .01 | .60 | .08 |
| Withdrawal | 13 | 14 | 20 | .31 | <.01 | <.01 |
| Spermicide | 1 | .5 | .3 | .01 | .31 | <.01 |
Defined as being fecund, not currently pregnant, postpartum, or seeking pregnancy, and sexually active in the month of interview.
Refers to data collected in 2002–2003.
Refers to data collected in 2006–2010.
Refers to data collected in 2011–2015.
During month of interview.
Includes IUD, implant, injection, pill, patch and ring.
While the use of more-effective methods (IUD, implant, injectable, pill, patch and ring) as a group remained unchanged, there was a shift toward the most effective methods within this group. IUD use increased significantly between each time period and from 3% to 14% across the entire time frame. From 2002 to 2013, implant use significantly increased from 0.5% to 3%, whereas pill use declined significantly from 43% to 31%. Withdrawal increased significantly from 2008 to 2013 and overall from 2002 to 2013, while there was no significant change over time in condom use.
Table 4 presents the UPRI by key demographics and NSFG survey year. Among all women aged 15–34, the UPRI declined significantly from 2002 to 2013, with an annualized rate of change of −2.1% (Table 4). Among women at risk of unintended pregnancy, there was a significant decline in the UPRI of 4 points (from 17 to 13), which translated to an annualized decline of approximately −2.2% (Table 4). Among women at risk, the UPRI declined significantly for nearly all of the demographic subgroups examined. Among women aged 15–19, 20–24 and 25–29 years, the UPRI declined significantly from 2002 to 2013, with an annualized change of −3.2% (p<.01), −2.2% (p<.01) and −2.9% (p<.01), respectively. Across race/ethnicity, the UPRI significantly declined from 2002 to 2013 among white and Hispanic women, with annualized changes of −2.6% and −2.1%, respectively. Similarly, there were significant declines in UPRI in every marital status group from 2002 to 2013, with annualized declines of 2.8%, 1.6% and 2.6% among cohabiting, married and unmarried noncohabiting women, respectively. Women with household earnings less than 100% of the poverty level had the largest annualized change of any subgroup in this analysis (−3.4%, p<.01), followed by women with earnings 200% or more of the poverty level (annualized change of 2.3%, p<.01).
Table 4.
UPRI by key demographics and NSFG survey year, 2002–2013
| Demographic | Survey year (midpoint) |
Comparison between survey years |
Annualized change 2002–2013 | ||||
|---|---|---|---|---|---|---|---|
| 2002a |
2008b | 2013c | 2002 vs. 2008 |
2008 vs. 2013 | 2002 vs. 2013 | ||
| UPRI | p value | ||||||
| All women | 7 | 6 | 6 | <.01 | .79 | <.01 | −2.1 |
| 15–34 | |||||||
| Women 15–34 at riskd | 15 | 12 | 11 | <.01 | .71 | <.01 | −2.0 |
| Age (years) | |||||||
| 15–19 | 17 | 14 | 12 | .14 | .25 | .01 | −3.2 |
| 20–24 | 15 | 13 | 12 | .02 | .66 | <.01 | −2.1 |
| 25–29 | 15 | 12 | 11 | .01 | .42 | <.01 | −2.3 |
| 30–34 | 13 | 10 | 11 | .02 | .23 | .23 | −0.9 |
| Race/ethnicity | |||||||
| White | 13 | 9 | 10 | <.01 | .31 | <.01 | −2.4 |
| non-Hispanice | |||||||
| Black | 17 | 19 | 15 | .27 | .02 | .32 | −0.9 |
| non-Hispanic | |||||||
| Hispanic | 18 | 15 | 14 | .24 | .25 | .02 | −2.1 |
| Marital status | |||||||
| Cohabiting | 17 | 13 | 12 | .07 | .47 | .01 | −2.6 |
| Married | 13 | 10 | 11 | <.01 | .17 | .02 | −1.5 |
| Not married or cohabitingf | 15 | 13 | 11 | .05 | .08 | <.01 | −2.4 |
| Percent of poverty level | |||||||
| 0–99 | 18 | 15 | 13 | .09 | .05 | <.01 | −3.0 |
| 100 –199 | 15 | 11 | 12 | .01 | .47 | .15 | −1.3 |
| ≥200 | 13 | 11 | 10 | <.01 | .86 | <.01 | −2.1 |
Refers to data collected in 2002–2003.
Refers to data collected in 2006–2010.
Refers to data collected in 2011–2015.
Includes women who were fecund, not currently pregnant, postpartum, or seeking pregnancy, and sexually active in the month of their interview.
Includes respondents who identified as other.
Includes respondents who identified as widowed, divorced, separated for reasons of marital discord or never married.
The decomposition analysis (not shown) found that among women at risk, 47% of the change in UPRI from 2002 to 2013 was attributable to improvements in CFRs. The remaining 53% was due to changes in contraceptive method mix, including shifts in the percentage of women using any method as well as changes in the proportions of women using each method.
Fig. 1 compares the UPRI among all women at each time point with the retrospective unintended pregnancy rates per 100 women for women aged 15–34. The overall decline in the UPRI between 2002 and 2013 echoes the decline in the unintended pregnancy rate between 2002 and 2011, with annualized rates of decline of 2.1% and 1.7% respectively. However, we see a decline in the UPRI earlier in the period, while the decline in the retrospective unintended pregnancy rate occurs later in the period. The 2008 period was an unusual one in that adolescent pregnancy rates experienced an uptick in an otherwise longer downward progression, which may partially explain the larger difference between prospective and actual realized rates during this period.
Fig. 1.
UPRI and unintended pregnancy (UP) rate, women 15–34 years.
4. Discussion
Our goal was to develop and assess the value of a new measure of unintended pregnancy risk using data solely from the NSFG. Both the trends and differentials in our estimates of the UPRI parallel previous patterns seen in the retrospective unintended pregnancy rate [4].
By focusing on behavioral components of the UPRI, our decomposition analysis provides evidence that the decline in the UPRI among women at risk has been driven by changes in several factors, including the method mix — the proportion of women using any method and the proportion using each specific method, multiple methods and long-acting methods — as well as changes in how effectively women are using their method(s) of contraception.
Nonuse of contraception has been identified as a key behavioral determinant of unintended pregnancy, and reducing the size of this group can help to reduce unintended pregnancy risk; prior analyses indicated that the 14% of women at risk who do not use contraception account for 54% of all unintended pregnancies [20]. Given the high risk of pregnancy associated with method nonuse, an increase in the share of women using any contraceptive method decreases the UPRI, regardless of which specific method is used [37, 41]. Furthermore, the increase in use of two of more contraceptive methods and the concomitant increase in withdrawal highlight the involvement of men in couples’ contraceptive use.
This analysis documents increases in use of long-acting contraceptive methods (LARC) among women at risk of unintended pregnancy, corroborating findings in other studies [38–40]. We find that increases in LARC use occurred simultaneously with declines in the share of women using other effective methods, resulting in about half of women at risk of unintended pregnancy using an effective method in each time period. Still, within this category, women shifted to methods with a lower CFR, as LARCs have greater efficacy than other hormonal methods, lowering the UPRI.
These analyses incorporated new typical-use CFRs estimated from the 2006–2010 NSFG, which decreased compared to estimates derived from earlier rounds of the NSFG, indicating improvements in how couples use contraception [31]. Our decomposition found that these improvements accounted for half of the estimated decline in the UPRI, highlighting their importance. However, if contraceptive failure rates continued to improve (i.e., decline) after the 2006–2010 period, the true UPRI in later years may in fact be lower than our estimates. More research is needed to document and understand the reasons for the observed improvements in contraceptive efficacy, to continue to monitor future patterns and to identify interventions to support further improvements.
In addition to serving as a surveillance tool, the UPRI also has the potential to improve the provision and quality of family planning services. Recent clinical recommendations put forth by the U.S. Centers for Disease Control and Prevention and the Department of Health and Human Services [41] not only emphasize what and how family planning services should be provided in order to help people achieve their childbearing goals, they also highlight the importance of quality improvement in the context of family planning service provision [42, 43]. To this end, the UPRI, if calculated in clinical settings, could guide how clinicians provide contraceptive services based on women’s reproductive intentions and highlight particular subpopulations in which needs may not be met. Furthermore, the UPRI could be informed by clinical approaches such as the One Key Question initiative [44], which assesses women’s pregnancy intentions and, in turn, their contraceptive preferences; this information could be used to calculate the UPRI within health care settings and further improve the provision of contraceptive services.
Our analysis is subject to a few limitations. While women who were not using any contraceptive method were assigned a failure rate of 85%, this figure may be higher than what happens in practice [45], which would mean the UPRI is overestimated. To test the robustness of the estimate, we recalculated the UPRI using a no-method failure rate of 40%, 60% and 100%. As expected, the absolute level of the UPRI was higher when the no-method failure rate was higher, but trends over the study period were similar when using each of these no-method failure rates.
Many women reporting use of a method at the time of the NSFG survey interview may have been using the method continually and successfully for years so that their actual risk of failure is much lower than “typical use” failure rates, which are measured among women initiating use of a method (whether for first time or they are returning to use). These women are likely to have lower failure rates than the “typical use” estimates, which would mean the UPRI is actually lower than our estimates.
By using prospectively reported pregnancy intentions and behavioral indicators, the UPRI is responsive to calls for new approaches to conceptualizing and measuring pregnancy intentions. The UPRI prioritizes behavioral indicators: all pregnancies predicted among women using contraception are considered unintended because we assume that women are using contraception because they do not intend to get pregnant. However, other studies have found that some women retrospectively report that while their pregnancy was unintended according to the retrospective measure, they were happy about the pregnancy [46–49]. The UPRI does not identify these or other types of nuanced feelings toward a pregnancy. Further research could investigate the relationship between pregnancy wantedness and pregnancy intentions and how both relate to use of contraception.
In conclusion, the UPRI can serve as an additional tool that can complement surveillance of unintended pregnancy rates. It has the advantage of being calculable for any population for which data on prospective pregnancy desire, pregnancy risk and contraceptive use are available. With these data items being collected continuously in the NSFG and with data releases every 2 years, the UPRI allows for the production of new estimates immediately following availability of the NSFG. Moreover, a prospective measure can be calculated for the same time period when data were collected because women are reporting their intentions at time of interview. This is more contemporaneous than a retrospective measure, which must look back over several years of actual pregnancies to obtain a sufficient sample size. The UPRI can be calculated for women specifically at risk of unintended pregnancy, allowing for a focus on the effects of changes in contraceptive use. And if calculated consistently over time, it can be used to assess trends in risk.
Acknowledgments
The authors thank Kathryn Kost and Mia Zolna for reviewing and commenting on earlier versions of this manuscript.
Funding: This research was supported by a grant from an anonymous donor. The conclusions presented are those of the authors.
Footnotes
☆☆ Declaration of conflicting interests: The authors declare no conflicts of interest with respect to the authorship and publication of this article.
We used the NSFG’s recode variable of fecundity status, which describes the respondent’s ability to become pregnant and carry a pregnancy to term. The variable classifies women as surgically sterile (contraceptive and noncontraceptive), nonsurgically sterile, subfecund, infertile for 36+ months or fecund.
References
- [1].Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann 2008;39: 18–38. https://doi.org/10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- [2].Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography 2015;52:83–111. https://doi.org/10.1007/s13524-014-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Maddow-Zimet I, Lindberg L, Kost K, Lincoln A. Are pregnancy intentions associated with transitions into and out of marriage? Perspect Sex Reprod Health 2016;48: 35–43. https://doi.org/10.1363/48e8116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008– 2011. N Engl J Med 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].U.S. Department of Health and Human Services. 2020 Topics & objectives: family planning. HealthyPeopleGov; 2014. http://www.healthypeople.gov/2020/topicsobjectives/topic/family-planning/objectives, Accessed date: 24 February 2016.
- [6].Santelli JS, Lindberg LD, Orr MG, Finer LB, Speizer I. Toward a multidimensional measure of pregnancy intentions: evidence from the United States. Stud Fam Plann 2009;40:87–100. https://doi.org/10.1111/j.1728-4465.2009.00192.x. [DOI] [PubMed] [Google Scholar]
- [7].Bachrach CA, Morgan SP. A cognitive-social model of fertility intentions. Popul Dev Rev 2013;39:459–85. https://doi.org/10.1111/j.1728-4457.2013.00612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Aiken ARA, Westhoff CL, Trussell J, Castaño PM. Comparison of a timing-based measure of unintended pregnancy and the London measure of unplanned pregnancy. Perspect Sex Reprod Health 2016;48:139–46. https://doi.org/10.1363/48e11316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Aiken ARA, Borrero S, Callegari LS, Dehlendorf C. Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts? Perspect Sex Reprod Health 2016;48:147–51. https://doi.org/10.1363/48e10316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect 1998: 24–46. [PubMed] [Google Scholar]
- [11].Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health 2006;38:90–6. https://doi.org/10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- [12].Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011;84:478–85. https://doi.org/10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Groves RM, Mosher WD, Lepkowski JM, Kirgis NG. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat 1 2009:1–64. [PubMed] [Google Scholar]
- [14].Jones RK, Jerman J. Abortion incidence and service availability in the United States, 2014. Perspect Sex Reprod Health 2017;49:17–27. https://doi.org/10.1363/psrh.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jerman J, Jones RK, Onda T. Characteristics of US abortion patients in 2014 and changes since 2008. New York: Guttmacher Institute; 2016. [Google Scholar]
- [16].Mosher WD, Jones J, Abma JC. National health statistics reports. Natl Cent Health Stat n.d.:1982–2010. [Google Scholar]
- [17].Lepkowski JM, Mosher WD, Davis KE, Groves RM, Van Hoewyk J. The 2006–2010 National Survey of Family Growth: sample design and analysis of a continuous survey. Vital Health Stat 2 2010:1–36. [PubMed] [Google Scholar]
- [18].Joyce T, Kaestner R, Korenman S. On the validity of retrospective assessments of pregnancy intention. Demography 2002;39:199–213. https://doi.org/10.2307/3088371. [DOI] [PubMed] [Google Scholar]
- [19].Guzzo KB, Hayford SR. Revisiting retrospective reporting of first-birth intendedness. Matern Child Health J 2014;18:2141–7. https://doi.org/10.1007/s10995-014-1462-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Adam Sonfield, Kinsey Hasstedt, Gold Rachel Benson. Moving forward: family planning in the era of health reform. Guttmacher Inst; 2016. https://www.guttmacher.org/report/moving-forward-family-planning-era-health-reform, Accessed date: 7 July 2017. [Google Scholar]
- [21].Lindberg L, Santelli J, Desai S. Understanding the decline in adolescent fertility in the United States, 2007–2012. J Adolesc Health 2016;59:577–83. https://doi.org/10.1016/j.jadohealth.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Santelli JS, Abma J, Ventura S, Lindberg L, Morrow B, Anderson JE, et al. Can changes in sexual behaviors among high school students explain the decline in teen pregnancy rates in the 1990s? J Adolesc Health 2004;35:80–90. https://doi.org/10.1016/j.jadohealth.2004.05.001. [DOI] [PubMed] [Google Scholar]
- [23].Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: the contribution of abstinence and improved contraceptive use. Am J Public Health 2007;97:150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Santelli JS, Lindberg LD, Orr MG, Finer LB. The pregnancy risk index: a useful method to estimate risk of pregnancy using existing behavioral data. Columbia University; 2009. [Google Scholar]
- [25].Solomon M, Badolato GM, Chernick LS, Trent ME, Chamberlain JM, Goyal MK. Examining the role of the pediatric emergency department in reducing unintended adolescent pregnancy. J Pediatr 2017;189:196–200. https://doi.org/10.1016/j.jpeds.2017.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].U.S. Department of Health and Human Services. NSFG-2013–2015 NSFG-Public use data files, codebooks and documentation. https://www.cdc.gov/nchs/nsfg/nsfg_2013_2015_puf.htm; 2016, Accessed date: 7 July 2017.
- [27].Chandra A, Copen CE, Stephen EH. Infertility and impaired fecundity in the United States, 1982–2010: data from the National Survey of Family Growth. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- [28].Steiner AZ, Jukic AMZ. Impact of female age and nulligravidity on fecundity in an older reproductive age cohort. Fertil Steril 2016;105:1584–1588.e1. https://doi.org/10.1016/j.fertnstert.2016.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].White L, McQuillan J, Greil AL, Johnson DR. Infertility: testing a helpseeking model. Soc Sci Med 1982;2006(62):1031–41. https://doi.org/10.1016/j.socscimed.2005.11.012. [DOI] [PubMed] [Google Scholar]
- [30].Mosher W, Jones J, Abma J. Nonuse of contraception among women at risk of unintended pregnancy in the United States. Contraception 2015;92:170–6. https://doi.org/10.1016/j.contraception.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sundaram A, Vaughan B, Kost K, Bankole A, Finer L, Singh S, et al. Contraceptive failure in the United States: estimates from the 2006–2010 National Survey of family growth. Perspect Sex Reprod Health 2017;49:7–16. https://doi.org/10.1363/psrh.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hatcher RA. Contraceptive technology. 20th revised edition. New York, N.Y.: Bridging the Gap Communications; 2011 [Google Scholar]
- [33].Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception 2008;77:10–21. https://doi.org/10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Gupta PD. Standardization and decomposition of rates: a user’s manual. US Department of Commerce, Economics and Statistics Administration, Bureau of the Census; 1993. [Google Scholar]
- [35].StataCorp. Stata statistical software: release 14. College Station, TX: StataCorp LP; 2014. [Google Scholar]
- [36].Supplemental table: declines in unintended pregnancy in the United States, 2008– 2011. Guttmacher Inst; 2016. https://www.guttmacher.org/article/2016/03/supplemental-table-declines-unintended-pregnancy-united-states-2008-2011, Accessed date: 31 July 2017. [Google Scholar]
- [37].Thomas A, Karpilow Q. The intensive and extensive margins of contraceptive use: comparing the effects of method choice and method initiation. Contraception 2016;94:160–7. https://doi.org/10.1016/j.contraception.2016.03.014. [DOI] [PubMed] [Google Scholar]
- [38].Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among US women, 2009–2012. Obstet Gynecol 2015;126:917–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Kavanaugh ML, Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception 2018;97:14–21. https://doi.org/10.1016/j.contraception.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Karpilow QC, Thomas AT. Reassessing the importance of long-acting contraception. Am J Obstet Gynecol 2017;216:148.e1–148.e14. https://doi.org/10.1016/j.ajog.2016.10.012. [DOI] [PubMed] [Google Scholar]
- [41].Gavin L, Moskosky S, Carter M, Curtis K, Glass E, Godfrey E, et al. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm rep 2014;63:1–54. [PubMed] [Google Scholar]
- [42].Gavin L, Moskosky S. Improving the quality of family planning services: the role of new federal recommendations. J Womens Health 2014;23:636–41. https://doi.org/10.1089/jwh.2014.4865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Gavin L, Moskosky S. Developing new federal guidelines on family planning for the United States. Contraception 2014;90:207–10. https://doi.org/10.1016/j.contraception.2014.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Bellanca HK, Hunter MS. ONE KEY QUESTION®: preventive reproductive health is part of high quality primary care. Contraception 2013;88:3–6. https://doi.org/10.1016/j.contraception.2013.05.003. [DOI] [PubMed] [Google Scholar]
- [45].Darroch JE. Adding it up: investing in contraception and maternal and newborn health, 2017—estimation methodology. New York: Guttmacher Institute; 2018. [Google Scholar]
- [46].Hartnett CS. Are Hispanic women happier about unintended births? Popul Res Policy Rev 2012;31:683–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Trussell J, Vaughan B, Stanford J. Are all contraceptive failures unintended pregnancies? Evidence from the 1995 National Survey of Family Growth. Fam Plann Perspect 1999;31:246–7 [260]. [PubMed] [Google Scholar]
- [48].Aiken ARA, Dillaway C, Mevs-Korff N. A blessing I can’t afford: factors underlying the paradox of happiness about unintended pregnancy. Soc Sci Med 2015;132:149–55. https://doi.org/10.1016/j.socscimed.2015.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Sable MR, Libbus MK. Pregnancy intention and pregnancy happiness: are they different? Matern Child Health J 2000;4:191–6. https://doi.org/10.1023/A:009527631043. [DOI] [PubMed] [Google Scholar]