Abstract
Os odontoideum is a rare condition. Nevertheless this condition was described by Giacomini in 1886. It is defined radiologicaly as an oval or round-shaped ossicle of variable size with smooth circumferential cortical margins representing the odontoid process that has no continuity with the body of C2. It is important to review this topic since the upper cervical spinal region is complex from anatomical point of view and has many vital structures passing in close relation to each other. If a person suffers from hyper mobile dens due to insufficiency of its ligamentous complex, it may cause translation of the atlas on the axis and may compress the cervical cord or vertebral arteries. There are cases where patients suffering from Os odontoideum became quadriplegic after a minor trauma. This lesion usually present in pediatric population and its cause is widely debatable today. In our paper we present a review of Os odontoideum in general and present a specific case of a young woman that was diagnosed with Os odontoideum together with the methods that were used to examine, stabilize and finally treat her.
Keywords: Spine, os odentoideum, trauma, harms technique
Introduction
Os odontoideum is a rare condition defined radiographically as an oval or round-shaped ossicle of variable size with smooth circumferential cortical margins representing the odontoid process that has no continuity with the body of C2 (Giacomini, 1886) [1,2]. This topic is prominent since when a person suffers from mobile or insufficient dens due to ineffective transverse atlantal ligament that functions at restraining atlantoaxial motion, it may cause translation of the atlas on the axis and may compress the cervical cord or vertebral arteries [3]. The exact etiology still remains obscure because those malformations mostly are incidentally detected in asymptomatic patients or are diagnosed only when patients become symptomatic. There are several reports of patients with Os odontoideum becoming quadriparetic after minor trauma [4,5]. Although Os odentoideum is a rare condition its exact frequency remains unknown since no large-scale screening studies have been performed. Nevertheless, in a study made by Perdikakis et al. they described the MR appearance of the odontoid process and calculated the prevalence of its morphological variants. They retrospectively reviewed 133 patients, age range between 19 and 81 years, which were examined within a period of 7 years. They found Os odontoideum in only one case (0.7%) [6]. This lesion usually presents clinically in pediatric population, moreover, most authors today believe it might represent an unrecognized fracture or damage to the epiphyseal plate during the first few years of life [[7], [8], [9]]. Some believe that it may represent a congenital anomaly instead of occult trauma [[10], [11], [12], [13], [14]]. The clinical presentation is a wide range starting from complete asymptomatic to devastating neurological injury. Some might express symptoms secondary to vertebral artery compression [[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]].
Case report
We present a case of a 28 years old female, generally healthy, who presented to the E.R. after obtaining a cervical trauma in a car accident when she was hit from behind. At site she was found outside the car that was hit by a truck, GCS was 11. Given the high energy obtained she was fitted with a hard cervical collar at site. She was not intubated and been taken to our hospital by ambulance.
History and Physical examination preformed in the trauma bay revealed an alert patient with normal vital signs complaining of diffuse pain including her neck among others. She had no wounds around the neck, palpation of the midline revealed no obvious step of and was diffusely tender, there was no obvious deformation and she was neurologically intact.
Since cervical x rays are not obtained routinely as the standard of care in the trauma bay, the cervical collar was not removed and she was taken to whole body CT study. This study revealed what was reported to be a positional asymmetry of C1–C2. Revision of the study revealed a true right unilateral C1–C2 lateral mass subluxation. This injury is highly uncommon in adults. We re-examined the patient after obtaining the CT and revealed after removing the hard collar that there was no torticollis, which would be expected in a case of rotatory subluxation. We also noticed a fare range of painless range of motion with a 20 degrees flexion and extension. The discrepancies between the physical examination and CT scan (Figs. 1–4) had lead us to obtain a flexion and extension x ray study which revealed an alarming distraction of the ADI to 16 mm, there was no rotation of C1 posterior arch on a lateral view and no rotation on AP view which lead us to believe that a bilateral dislocation occurs and severe instability (Figs. 5–8). One should also notice that extension reduced the dislocation completely to a normal limit of less than 2 mm.
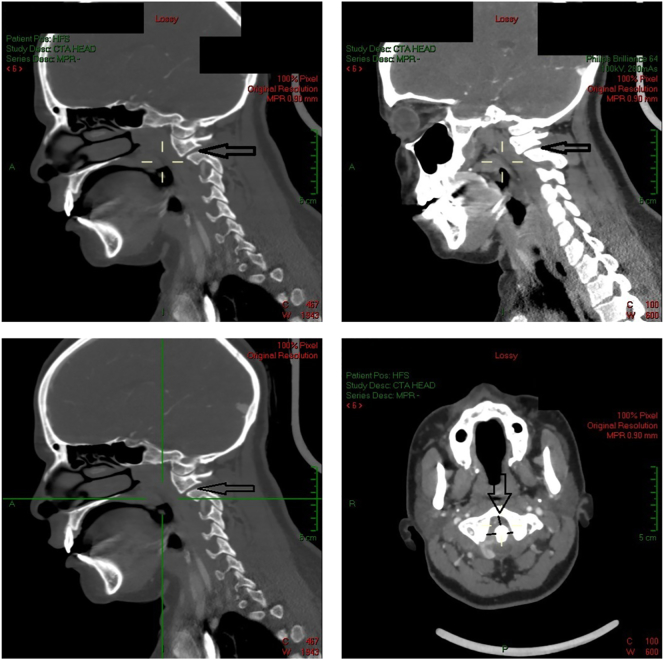
Figs. 1–4.
CT-study: Showing – C1–C2 subluxation with increased ADI distance and dystopic os odontoideum. Upper left – left sagittal, upper middle - right sagittal, upper right – axial, lower right – sagittal showing dens.
Figs. 5–8.
X-ray study. Upper left – flexion study, upper right – lateral study, lower left – extension study, lower right – odontoid open mouth view.
At this point we obtained an MRI study of the cervical spine including the occipitocervical junction. It should be mentioned that we do not routinely obtain MRIs in neither neurologically intact trauma patients nor in complete SCI patients. The MRI that was obtained has revealed that there is no evidence of acute bleeding; there was a small cephalic Os odentoideum that was missed on the CT and thinning of the spinal cord behind the odontoid without myellomalacia.
Since the patient was now symptomatic with pain and “clicking” of the neck when trying to move to more than 20 degrees of flexion or extension and a dynamic study that demonstrated severe instability, we decided to offer surgery.
Three weeks after the admission we preformed posterior C1–C2 fusion with separate instrumentation of C1 and C2 (harms technique). The technical challenge was to approach the C1 lateral mass with the C1–C2 reduced since complete reduction was obtained only at maximal extension. In order to solve this we attached the head to a hallo ring, for better grip of the cranium, which was in turn attached to a Jackson frame. We exposed the posterior elements with the head in flexion and inserted the C1 and C2 screws achieving reduction by extending and posterior translation of the head. We then locked the posterior bars (Figs. 9–10).
Figs. 9–10.
Intraoperative fluoroscopy showing alignment after posterior instrumentation.
The patient was left in a hard collar and dismissed at the first post-operative day. The follow up X-ray(Figs. 11–12) and CT (Figs. 13–16) scan has revelled stable reduction with a painless range of motion. She remained neurologically intact.
Fig. 11–12.
AP and lateral cervical radiographs a month after surgery. Showing that the instrumentation is in position and the reduction is stable.
Figs. 13–16.
CT-study a month after surgery: Showing – C1–C2 stable reduction with acceptable ADI distance and dystopic os odontoideum. Upper left – axial, upper right- left sagittal, Lower left – right sagittal, lower right – coronal showing dens.
Discussion
Os odentoideum is a rare occipitocervical lesion with varied clinical manifestation. The etiology of this rare lesion remains unknown. Most patients will present in childhood with neck pain or neurologic symptoms due to cord compression from posterior translation of the Os into the cord in extension or the odontoid into the cord in flexion. Increased motion at the C-1 to C-2 level can lead to vertebral artery occlusion, ischemia of the brainstem and posterior fossa structures, resulting in seizures, syncope, vertigo, visual disturbances and even sudden death [[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]].
C1–C2 instability without a fracture is highly uncommon in adults. Most cases are secondary to trauma with ligamentous injury, especially transverse ligament mid substance tear and odontoid fracture being the most common [[7], [8], [9]].
There are variable sizes of radiographic Os odontoideum, with some having a very small cephalic ossicle which may be hard to diagnose on plain X-rays or CT. High index of clinical suspicion and cervical MRI that includes the C1–C2 are mandatory in the diagnosis and treatment of this rare condition [1,[3], [4], [5], [6]].
Conclusion
In our case we might be describing either a case of an asymptomatic patient which was incidentally diagnosed in the routine evaluation of a cervical trauma or a case of fibrous union that was interrupted by the flexion extension injury. The absence of high signal in the FFE sequence MRI neither in the C1–C2 joints nor in the cord diminishes the chance of an acute injury, however, does not completely rule out an acute or chronic injury. Minor trauma in undiagnosed cervical instability might end in catastrophic neurological insult, hence is the importance of early diagnosis and treatment.
C1–C2 independent instrumentation and fusion (harms technique) is a safe and effective procedure and can be achieved even in cases in which a great deal of extension is needed in order to achieve the reduction.
It is advisable that in all cases of suspected C1–C2 instability including those without neurological deficiencies, MRI should be obtained. As in other ligamentous injuries dynamic imaging has an important role and shouldn't be excluded.
Contributor ship statement
-
•
Yuri Klassov: Author, guarantor of the paper, is responsible for the conception, design, analysis and interpretation of data together with drafting the article and revising its content and final approval of the version to be published.
-
•
Vadim Benkovich: Author, guarantor of the paper, is responsible for the conception, design, analysis and interpretation of data together with drafting the article and revising its content and final approval of the version to be published.
-
•
Moti Kramer M: Author, guarantor of the paper, is responsible for the conception, design, analysis and interpretation of data together with drafting the article and revising its content and final approval of the version to be published.
Data sharing statement
No additional data available.
Ethics
We received the permission by the ethics commission in our country stating that this article does not possess any ethical problem.
Funding
The article and all related issues were sponsored solely by the authors.
The authors have obtained the patient's informed written consent for print and electronic publication of the case report.
References
- 1.Fielding J.W., Hensinger R.N., Hawkins R.J. Os Odontoideum. J. Bone Joint Surg. Am. 1980;62:376–383. [PubMed] [Google Scholar]
- 2.Perrini P., Montemurro N., Iannelli A. The contribution of Carlo Giacomini (1840–1898): the limbus Giacomini and beyond. Neurosurgery. 2013 Mar.;72(3):475–481. doi: 10.1227/NEU.0b013e31827fcda3. (discussion 481–2) [DOI] [PubMed] [Google Scholar]
- 3.Klimo P., Jr., Kan P., Rao G., Apfelbaum R., Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J. Neurosurg. Spine. Oct 2008;9(4):332–342. doi: 10.3171/SPI.2008.9.10.332. [DOI] [PubMed] [Google Scholar]
- 4.Karmakar P.S., Karmakar P.S., Mitra R., Basu S., Ghosh A. Sudden onset quadriparesis after minor injury to neck in a male with OS odontoideum. J. Assoc. Physicians India. 2013 Feb.;61(2):138–139. [PubMed] [Google Scholar]
- 5.Graillon N., Rakotozanani P., Graillon T., Dufour H., Fuentes S. Acute decompensation of os odontoideum in the elderly. Case report. Neurochirurgie. 2013 Aug–Oct;59(4–5):195–197. doi: 10.1016/j.neuchi.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Perdikakis E., Skoulikaris N. The odontoid process: various configuration types in MR examinations. Eur. Spine J. 2014 May;23(5):1077–1083. doi: 10.1007/s00586-013-3135-4. [DOI] [PubMed] [Google Scholar]
- 7.Hukuda S., Ota H., Okabe N., Tazima K. Traumatic atlantoaxial dislocation causing os odontoideum in infants. Spine. May–Jun 1980;5(3):207–210. doi: 10.1097/00007632-198005000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Kuhns L.R., Loder R.T., Farley F.A., Hensinger R.N. Nuchal cord changes in children with os odontoideum: evidence for associated trauma. J. Pediatr. Orthop. Nov–Dec 1998;18(6):815–819. [PubMed] [Google Scholar]
- 9.Brecknell J.E., Malham G.M. Os odontoideum: report of three cases. J. Clin. Neurosci. Mar 2008;15(3):295–301. doi: 10.1016/j.jocn.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 10.Morgan M.K., Onofrio B.M., Bender C.E. Familial os odontoideum. Case report. J. Neurosurg. 1989;70:636–639. doi: 10.3171/jns.1989.70.4.0636. [DOI] [PubMed] [Google Scholar]
- 11.Currarino G. Segmentation defect in the midodontoid process and its possible relationship to the congenital type of os odontoideum. Pediatr. Radiol. 2002;32:34–40. doi: 10.1007/s00247-001-0579-1. [DOI] [PubMed] [Google Scholar]
- 12.Hadley M. Os odontoideum. Neurosurgery. 2002;50:S148–S155. doi: 10.1097/00006123-200203001-00023. [DOI] [PubMed] [Google Scholar]
- 13.Wada E., Matsuoka T., Kawai H. Os odontoideum as a consequece of a posttraumatic displaced ossiculum terminale. A case report. J. Bone Joint Surg. Am. 2009;91:1750–1754. doi: 10.2106/JBJS.H.01182. [DOI] [PubMed] [Google Scholar]
- 14.Arvin B., Fournier-Gosselin M.P., Fehlings M.G. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66:22–31. doi: 10.1227/01.NEU.0000366113.15248.07. [DOI] [PubMed] [Google Scholar]
- 15.Dai L., Yuan W., Ni B., Jia L. Os odontoideum: etiology, diagnosis and management. Surg. Neurol. 2000;53:106–109. doi: 10.1016/s0090-3019(99)00184-6. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki H., Itoh T., Takei H., Hayashi M. Os odontoideum with cerebellar infarction. Spine. 2000;25(9):1178–1181. doi: 10.1097/00007632-200005010-00020. [DOI] [PubMed] [Google Scholar]
- 17.Chang H., Park J., Kim K., Choi W. Retro-dental reactive lesions related to development of myelopathy in patients with atlantoaxial instability secondary to os odontoideum. Spine. 2000;25(21):2777–2783. doi: 10.1097/00007632-200011010-00010. [DOI] [PubMed] [Google Scholar]
- 18.Galli J., Tartaglione Calo L., Ottaviani F. Os odontoideum in a patient with cervical vertigo: a case report. Am. J. Otolaryngol. 2001;22(5):371–373. doi: 10.1053/ajot.2001.26503. [DOI] [PubMed] [Google Scholar]
- 19.Fukuda M., Aiba T., Akiyama K., Nishiyama K., Ozawa T. Cerebellar infarction secondary to os odontoideum. J. Clin. Neurosci. 2003;10(5):625–627. doi: 10.1016/s0967-5868(03)00131-0. [DOI] [PubMed] [Google Scholar]
- 20.Ramos L.S., Taylor J.A.M., Lackey G., Lindsay D. Topics In Diagnostic Radiology and Advanced Imaging. 3(1) 1996. Os odontoideum with sagittal and coronal plane instability: a report of three cases; pp. 5–12. [Google Scholar]
- 21.Clements W., Mezue W. Mathew Os odontoideum - congenital or acquired? – that's not the question. Injury. 1995;26(9):640–642. doi: 10.1016/0020-1383(95)00123-q. [DOI] [PubMed] [Google Scholar]
- 22.Takakuwa T., Hiroi S., Hasegawa H., Hurukawa K., Endo S., Shimamura T. Os odontoideum with vertebral artery occlusion. Spine. 1994;19(4):460–462. doi: 10.1097/00007632-199402001-00015. [DOI] [PubMed] [Google Scholar]
- 23.Watanabe M., Toyama Y., Fujimura Y. Atlantoaxial instability in os odontoideum with myelopathy. Spine. 1996;21(12):1435–1439. doi: 10.1097/00007632-199606150-00007. [DOI] [PubMed] [Google Scholar]
- 24.Hensinger R. Osseous anomalies of the craniovertebral junction. Spine. 1986;11(4):323–333. doi: 10.1097/00007632-198605000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Ebraheim N., Lu M., Yang H. The effect of translation of the C1–C2 on the spinal canal. Clin. Orthop. Relat. Res. 1998;351:222–229. [PubMed] [Google Scholar]
- 26.Thurlow R. Odontoid agenesis with atlanto-axial luxation. J. Can. Chiropr. Assoc. 1986;30(2):77–80. [Google Scholar]