An accurate understanding of a diagnosis is important for patients with advanced cancer so that the patient can make decisions that align with preferences and values. This study examined the understanding of prognosis and therapy goals in patients with newly diagnosed advanced lung cancer, as well as the understanding of the patients' caregivers.
Keywords: Prognostic perception, Advanced lung cancer, Family caregiver, Quality of life, Psychological distress, Illness understanding
Abstract
Background.
Prognostic understanding in advanced cancer patients and their caregivers may have an impact on the delivery of effective care. The aims of this study were to explore prognostic understanding at diagnosis in both patients with advanced lung cancer and their caregivers and to investigate correlates of their understanding.
Subjects, Materials, and Methods.
A total of 193 patients with newly diagnosed advanced lung cancer and their 167 caregivers were enrolled at 16 hospitals in Japan. We assessed their perceptions of prognosis and goals of therapy and examined their associations with their sociodemographic characteristics, clinical status, quality of life, mood symptoms, and the status of disclosure of information by their treating physicians.
Results.
One fifth of patients and caregivers (21.7% and 17.6%, respectively) mistakenly believed that the patients’ cancer was “completely curable.” Substantial proportions of them (16.9% and 10.3%, respectively) mistakenly believed that the primary goal of therapy was to remove all the cancer. Levels of anxiety and depression in both patients and caregivers were significantly higher among those who had accurate understanding of prognosis. In multivariate analyses, inaccurate perceptions of prognosis in patients were associated with sex, better emotional well‐being, and lower lung cancer‐specific symptom burden. Caregivers’ inaccurate perceptions of patients’ prognoses were associated with better performance status and better emotional well‐being of patients.
Conclusion.
Substantial proportions of advanced lung cancer patients and their caregivers misunderstood their prognosis. Interventions to improve their accurate prognostic understanding should be developed with careful attention paid to its associated factors.
Implications for Practice.
This study demonstrated that substantial proportions of patients with newly diagnosed advanced lung cancer and their caregivers had misunderstandings about their prognosis. Accurate perceptions of prognosis, which are indispensable in the delivery of effective care, were associated with elevated levels of anxiety and depression in both patients and caregivers, warranting psychosocial care and support for them immediately after diagnosis. Inaccurate perceptions of prognosis in patients were associated with better emotional well‐being and lower lung cancer‐specific symptom burden. Illness understanding in caregivers was associated with patients’ physical and mental status. Those findings provide insight into how they obtain accurate illness understanding.
摘要
背景。晚期肺癌患者及其照料者对预后的认知可能影响医疗的有效提供。本研究旨在探讨晚期肺癌患者及其照料者对诊断时的预后认知情况,并研究其相关性
受试者、材料和方法。日本16家医院共有193名近期被诊断为患有晚期肺癌的患者及其 167 名照料者参与本研究。我们评估了他们对预后和治疗目标的认知,并调查了他们与其社会人口学特征、临床状态、生活质量、情绪症状以及主治医师对病情披露情况之间的关系。
结果。五分之一的患者和照料者(分别为21.7%和17.6%)错误地认为,患者所患癌症“完全可以治愈”。他们中的大部分人(分别为16.9%和10.3%)错误地认为,治疗的主要目标是消除所有癌症。在准确了解预后的患者和照料者中,焦虑和忧郁程度显著提高。在多变量分析中,患者对预后的不准确认知与性别、情绪较为健康以及肺癌特异性症状负担较低有关。照料者对患者预后的不准确认知与患者体能状况较好及情绪较为健康有关。
结论。大部分晚期肺癌患者及其照料者对其预后存在误解。应特别留意其相关因素,制定干预措施,以加强他们对预后的准确认知了解。
实践意义
本研究表明,大部分近期被诊断为患有晚期肺癌的患者及其照料者对其预后存在误解。预后的准确认知对于提供有效医疗至关重要,它与患者和照料者的焦虑和沮丧程度提高有关,需要在诊断后能够立即为他们提供社会心理医疗和支持。患者对预后的不准确认知与情绪更为健康以及肺癌特异性症状负担较低有关。照料者对病情的了解与患者的身心状况有关。这些发现有利于他们对患者病情的准确了解程度。
Introduction
Accurate illness understanding is important for patients with advanced cancer, so that they can make decisions that align with their preferences and values [1]. Evidence has been accumulated that illness understanding has various impacts on advance care planning and end‐of‐life care [2], [3], [4], [5]. Patients’ willingness to accept chemotherapy for advanced lung cancer is influenced by their prognostic understanding [6]. Patients who overestimate their prognosis are more likely to receive aggressive care at the end of life, which could cause deterioration in their quality of life (QOL) during this time without significant improvement in survival [7]. However, past studies have consistently shown that many patients with advanced cancer have inaccurate prognostic understanding [4], [8], [9], [10], [11], [12]. Accurate prognostic understanding is difficult for patients even when accurate information is provided by their treating physicians [13], [14], [15]. To improve patients’ illness understanding, clinicians need to be aware of factors that could hamper patients’ accurate illness understanding.
Illness understanding among caregivers of patients with advanced cancer is also an important issue to be addressed. Caregivers can easily misunderstand patients’ illness conditions, and this can be a barrier to efficient support for and communication with the patients [12], [16], [17]. Discrepancies in illness understanding between patients and their caregivers can complicate their decision‐making processes [16]. However, influence of caregivers’ misunderstanding on both patients and caregivers has not been sufficiently explored. It is also unclear which factors are associated with caregivers’ accurate illness understanding.
Therefore, in this multicenter study, we aimed to examine understanding of patients with newly diagnosed advanced lung cancer and their caregivers on their prognosis and therapy goals. We also evaluated concordance rate of their understanding. Further, we explored the factors that were potentially associated with their prognostic understanding. We hypothesized that sociodemographic characteristics, including their family situation and employment status, clinical status, QOL, and mood symptoms, as well as the status of disclosure of information by their treating physicians, would be associated with their understanding. We also hypothesized that family caregivers’ understanding is influenced by both variables of the patients and the caregiver themselves.
Subjects, Materials, and Methods
Study Participants
The participants were recruited at the oncology clinics of 16 hospitals in Japan during the period between December 2013 and November 2015. Recruitment was conducted consecutively in the clinics of the physicians of each hospital who agreed to contribute to this study.
Patients were eligible if they were (a) newly diagnosed with clinical stage IIIB or IV lung cancer, (b) 20 years of age or older, and (c) able to write and comprehend Japanese. Exclusion criteria were the following: patients who (a) had significant cognitive impairment or (b) had already received anticancer treatments (chemotherapy, radiation, surgery, or immunotherapy).
Caregivers were eligible if they were (a) identified by the patients as their primary caregiver, (b) 20 years of age or older, and (c) able to write and comprehend Japanese. Caregivers were not eligible if they had significant cognitive impairment. The study was approved by the institutional review board of all the participating hospitals, and all participants submitted written informed consent.
Self‐Reported Outcomes
To assess the participants’ illness understanding, we used two self‐report questions that were adopted and modified from those used in the relevant past studies [4], [10], [18], [19], [20]. Participants were asked whether their cancer was completely curable (response options: “completely curable” or “complete cure is difficult”) [4], [10], [19]. They were also asked to choose the primary goal of therapy from among the following options: “to get rid of all of the cancer,” “to help them live longer,” and “to improve symptoms or to lessen distress” [4], [18], [19], [20]. The Japanese version of these questions used in this study are shown in supplemental online Appendix 1. Because advanced lung cancer is an incurable disease and complete response to anticancer therapy is exceptionally rare [21], [22], responses of “the cancer is completely curable” and “the goal of therapy is to get rid of all of the cancer” were regarded as misunderstandings of prognosis and of the goals of therapy, respectively.
The patients’ health‐related QOL was measured with the Functional Assessment of Cancer Therapy‐Lung scale (FACT‐L). This scale assesses multiple dimensions of QOL during the past week: physical well‐being, social well‐being, emotional well‐being (EWB), functional well‐being (FWB), and lung cancer symptom burden (lung cancer subscale: LCS) [23], [24]. Higher scores indicate better QOL and lower symptom burden.
Health‐related QOL of caregivers was measured with the Short‐Form 8‐Item Health Survey (SF‐8). This instrument assesses eight aspects of health‐related QOL. The physical component summary (PCS) and mental component summary are calculated by weighing each of the eight items [25], [26].
Mood symptoms of both patients and caregivers were measured with the Hospital Anxiety and Depression Scale (HADS), a 14‐item self‐report questionnaire that contains two subscales measuring anxiety (HADS‐A) and depression (HADS‐D) [27], [28]. Scores for each subscale range from 0 (no distress) to 21 (maximum distress). Scores of seven or greater indicate clinically significant psychological distress. The FACT‐L, SF‐8, and HADS have been validated in the Japanese population [24], [29], [30], [31].
Clinical Data
The patients’ clinical characteristics were collected through the reports from their treating physicians. While participants were asked to complete the questionnaires, their physicians were also asked to administer questionnaires that inquire whether they had explained the following issues to the patients and their caregivers: “complete cure is difficult”; “predictable life expectancy”; “time will come when they will need to discontinue anticancer treatments”; and “palliative care” (yes or no for each issue).
Procedure
The participants were recruited upon disclosure of their diagnosis of clinical stage IIIB or IV lung cancer, when physicians usually discussed the illness, treatment, and future perspectives. They were approached as soon as possible after their cancer diagnosis was discussed. However, specific timing of the approach (e.g., on the same day or on a different day of the discussion) was decided based on medical staffs’ judgement in consideration of the patients’ and their caregivers’ emotional states. After submitting written informed consents, the participants were asked to independently complete the questionnaires promptly (in principle within 2 weeks).
Statistical Analysis
With an estimation that 30%–70% of the participants misunderstand their prognosis, we calculated that 167 patients and 167 caregivers were required in order to allow at least five independent variables in binary logistic regression models. After descriptive analyses, bivariate analyses were conducted to investigate factors associated with illness understanding of patients and caregivers. Fisher's exact tests were used for categorical variables and Mann‐Whitney U tests for continuous and ordinal variables.
Because the proportions of misunderstanding were lower than expected, the authors decided to reduce the number of independent variables to be entered into the subsequent multivariate regression analyses. Based on the past studies that reported significant associations of prognostic understanding with sex [1], [32], [33], [34], and with QOL [19], [35], we selected the following variables out of the variables that were found significant in the bivariate analysis: sex, emotional well‐being (FACT‐EWB), physical symptom burden (FACT‐LCS), and functioning (FACT‐FWB).
For caregivers, because past relevant studies were limited, we selected three highly significant variables with the lowest p values, focusing on patients’ physical status (performance status) and emotional states (FACT‐EWB) and how the caregivers are informed of the patients' condition (physicians’ explanation to caregivers about future discontinuation of anticancer treatment).
All the analyses were two‐sided and p < .05 was considered statistically significant. Analyses were conducted using SPSS 22.0 software (IBM, Chicago, IL).
Results
Characteristics of the Participants
Of the 307 newly diagnosed lung cancer patients and their caregivers, 219 patients and their 211 caregivers were eligible and were approached. Of them, 204 patients and their 193 caregivers agreed to participate in this study (consent rates: 93.2% and 91.4%). Responses were obtained from 193 patients and 169 caregivers (response rates: 94.6% and 87.6%). The patients who participated in this study were more likely to receive anticancer therapies, compared with those who did not participate in this study. Responses from two caregivers had substantial missing values and were excluded, resulting in 167 caregiver responses entered into analyses. Participants’ characteristics are shown in Table 1. Most patients were over 60 years of age, male, smokers, and with Eastern Cooperative Oncology Group performance status of 1 or 2. Most patients (83.4%) had stage IV lung cancer. Chemotherapy was scheduled for most patients (85.3%). Only a few patients (3.2%) were scheduled solely to receive supportive care. Most caregivers were spouses who were over 50 years of age, female, and resided with the patient.
Table 1. Sociodemographic and clinical characteristics of patients and caregivers.
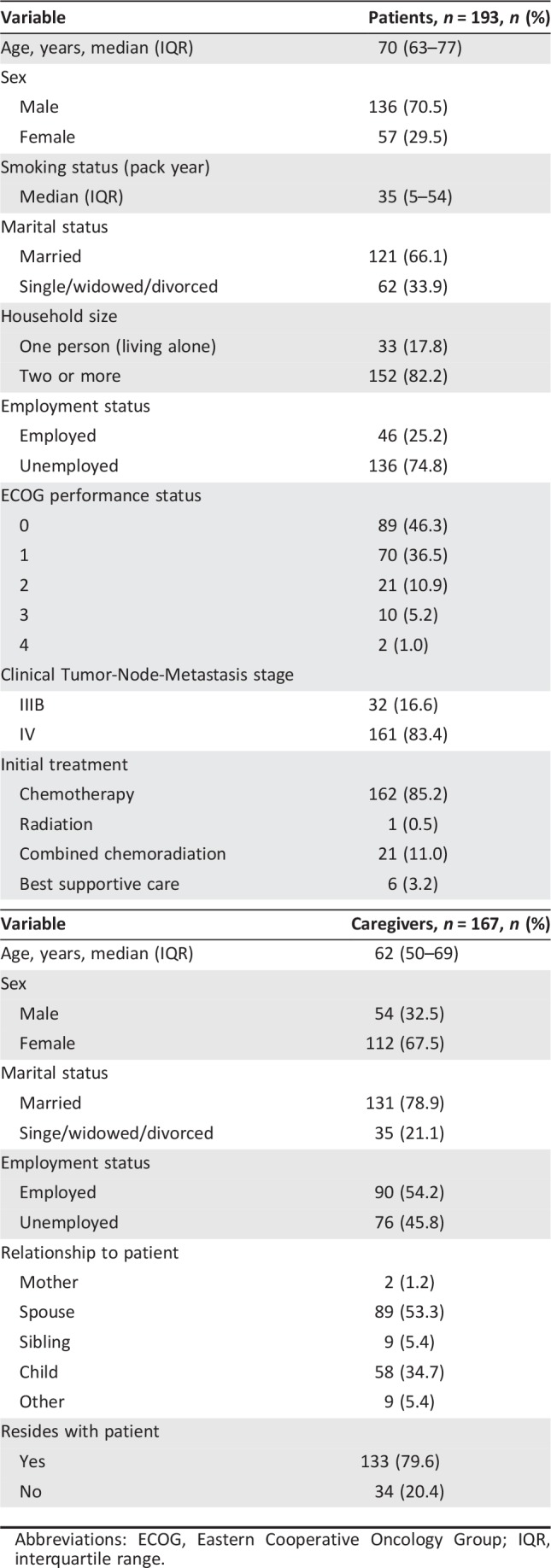
Abbreviations: ECOG, Eastern Cooperative Oncology Group; IQR, interquartile range.
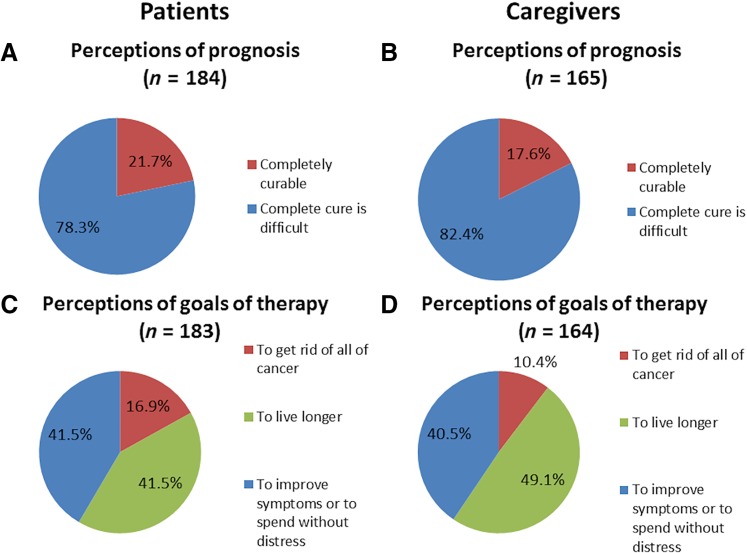
Illness Understanding at Diagnosis
As shown in Figure 1A, one fifth (21.7%) of patients mistakenly believed that their cancer was completely curable. A similar proportion of caregivers had the same misunderstanding (Fig. 1B). The goal of therapy was misunderstood as “to get rid of all of the cancer” by 16.9% of patients and 10.3% of caregivers (Fig. 1C, 1D). When we conducted subgroup analyses, enrolling only stage IV lung cancer patients, the results were generally consistent with the whole‐group analyses. However, slightly lower proportions of caregivers misunderstood the patient’ prognosis and the goals of therapy (14.7% and 7.5%, respectively) when the patients had more advanced illness (supplemental online Fig. 1B, 1D).
Figure 1.
Perceptions of prognosis and goals of therapy at diagnosis in advanced lung cancer patients and their caregivers. Perceptions of prognosis (“completely curable” or “complete cure is difficult”) in 184 patients (A) and in 165 caregivers (B). Perceptions of goals of therapy (“to get rid of all of the cancer,” “to live longer,” or “to improve symptoms or to live without distress”) in 183 patients (C) and in 164 caregivers (D).
In total, 20.1% of the patients and 15.4% of the caregivers had inconsistent perceptions between prognosis and goals of therapy (supplemental online Fig. 2), and 7.8% of the patients and 4.3% of the caregivers perceived the prognosis as “complete cure is difficult” yet misunderstood the goal of therapy as “to get rid of all of the cancer.”
Four fifths of dyads (80.8%) had concordant perceptions of prognosis (kappa = 0.37, 95% confidence interval 0.18–0.55), and 83.6% of dyads had concordant perceptions of goals of therapy (kappa = 0.27, 95% confidence interval 0.06–0.48; supplemental online Fig. 3). In 11.5% of the dyads, the patient misunderstood the prognosis whereas their caregiver accurately understood it. In 7.7% of the dyads, the patient accurately understood the prognosis whereas their caregiver misunderstood it. Discrepancies in perceptions of the goals of therapy were observed in 16.4% of the dyads. Patients misunderstood it in 11.1% of the dyads and the caregivers in 5.2%. Both the patient and their caregiver misunderstood the prognosis and goals of therapy in 9.0% and 4.6% of the dyads, respectively.
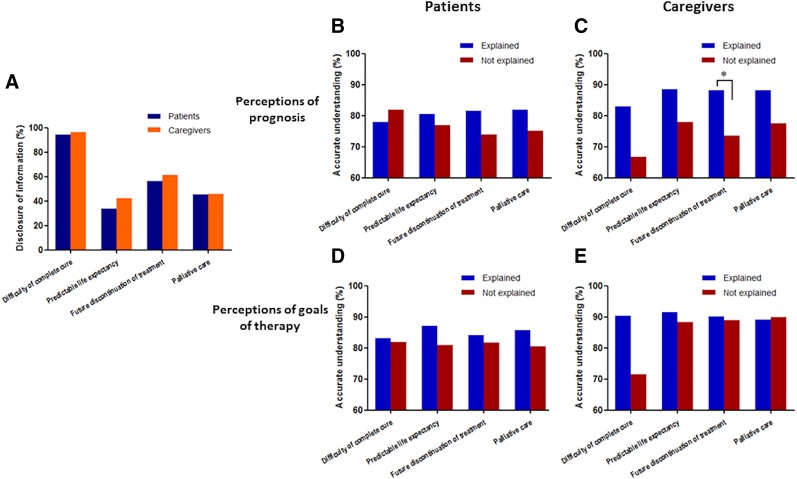
Physicians’ Explanations and Their Association with Illness Understanding of Patients and Caregivers
Figure 2A shows the status of disclosure of information by treating physicians of patients and caregivers, according to the physicians’ self‐report (Fig. 2A). In most cases, physicians explained to the patients and caregivers that complete cure is difficult (94.0% and 96.3%, respectively). Predictable life expectancy was explained to 33.9% of the patients and 42.1% of the caregivers. Less than two thirds of physicians explained to the patients and the caregivers that a time would come when they would have to discontinue anticancer treatment (56.3% and 61.0%, respectively). Physicians explained about palliative care at the time of diagnosis to 45.4% of the patients and 45.7% of the caregivers.
Figure 2.
(A): Physicians’ reports of disclosure of information to advanced lung cancer patients and caregivers. (B–E): Illness understanding in advanced lung cancer patients and their caregivers associated with physicians’ explanations. Proportions of participants with accurate understanding are shown in bar graphs. Perceptions of prognosis in 183 patients (B) and in 164 caregivers (C). Physicians’ explanations to caregivers about future discontinuation of anticancer treatment were correlated at a statistically significant level with caregivers’ accurate perceptions of prognosis (*; Fisher's exact test for comparison, p = .021). Perceptions of goals of therapy in 182 patients (D) and in 163 caregivers (E). There was no significant difference in physicians’ explanations concerning perceptions of goals of therapy for both patients and caregivers.
Associations between physicians’ explanations and illness understanding among patients and caregivers are shown in Figure 2B–2E. Patients who were provided with information on their predictable life expectancy, future discontinuation of anticancer treatment, and palliative care were more likely to have accurate perceptions of prognosis, although there was no statistically significant difference (Fig. 2B). A similar tendency was observed in caregivers (Fig. 2C). Caregivers who were given an explanation about future discontinuation of anticancer treatment were more likely to have accurate perceptions of prognosis compared with caregivers who were not given such an explanation (p = .021). There was no significant association between physicians’ explanations and perceptions of goals of therapy in either patients or caregivers (Fig. 2D, 2E).
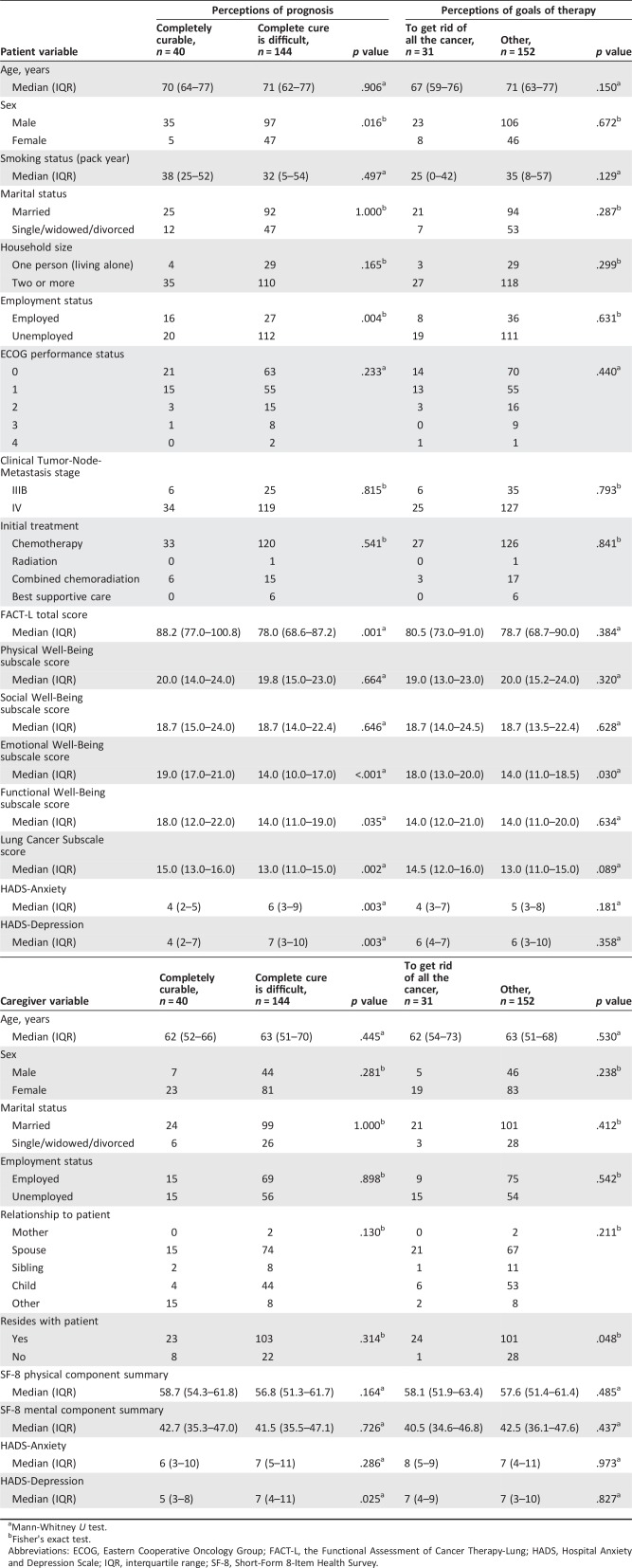
Associations Between Illness Understanding and Characteristics of Participants
As shown in Table 2, male patients and patients who are employed were more likely to misunderstand their prognosis. Patients’ overall health‐related QOL (FACT‐L total scores), FACT‐EWB, FACT‐FWB, and FACT‐LCS were significantly worse among patients who had accurate perceptions of prognosis. Anxiety and depression, measured by HADS‐A and HADS‐D scores, were significantly higher among patients who had accurate perceptions of prognosis. Performance status, clinical stage, and planned initial treatment were not associated with perceptions of prognosis in patients. Patients’ misunderstanding regarding the goals of therapy were associated only with lower FACT‐EWB.
Table 2. Associations between prognostic understanding in patients and variables.
Mann‐Whitney U test.
Fisher's exact test.
Abbreviations: ECOG, Eastern Cooperative Oncology Group; FACT‐L, the Functional Assessment of Cancer Therapy‐Lung; HADS, Hospital Anxiety and Depression Scale; IQR, interquartile range; SF‐8, Short‐Form 8‐Item Health Survey.
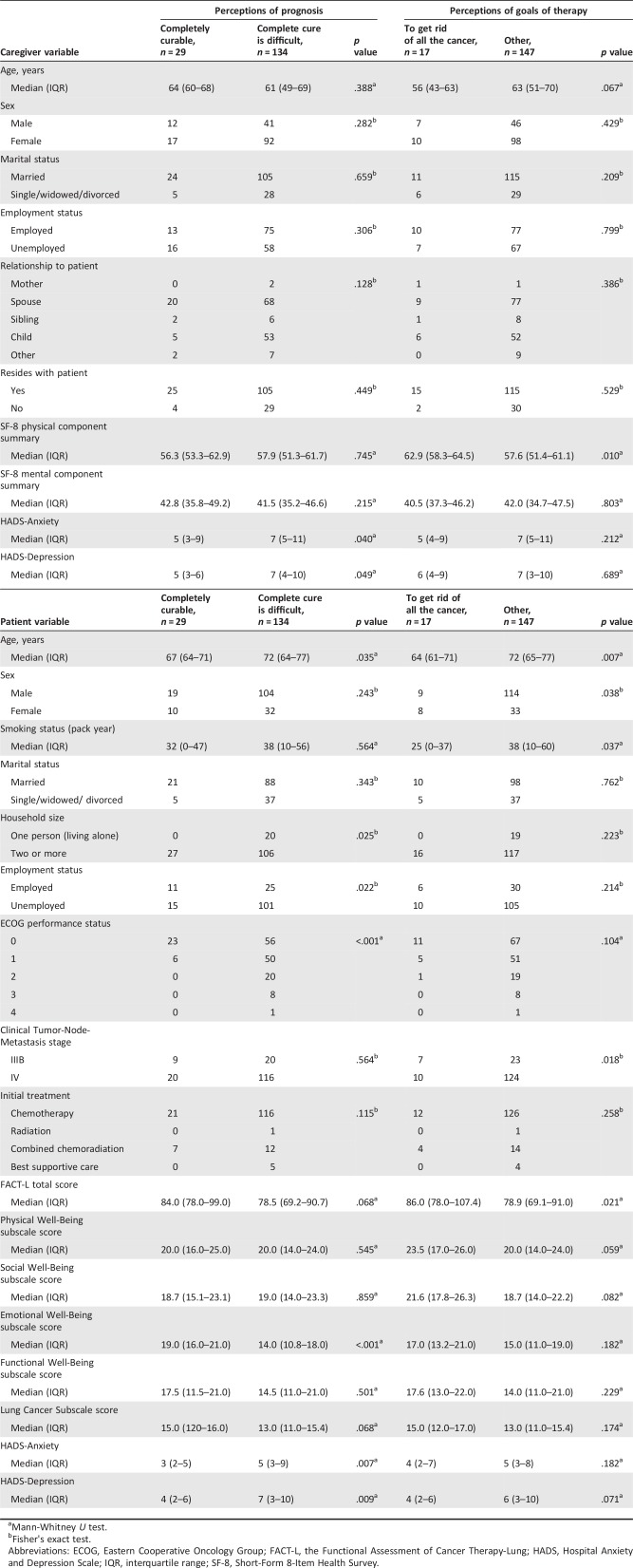
The caregivers were more likely to misunderstand the patient's prognosis if the patient was younger, cohabiting, employed, or with better performance status. The caregivers who had accurate understanding of the prognosis had significantly higher HADS‐A and HADS‐D (Table 3). The caregivers were more likely to misunderstand the goals of therapy when the patient was younger, female, with lighter smoking history, in clinical stage of IIIB (compared with stage IV), or with better global QOL (FACT‐L total score). The caregivers’ accurate understanding was associated with higher physical QOL of caregivers themselves (PCS scores of the SF‐8; Table 3).
Table 3. Associations between prognostic understanding in caregivers and variables.
Mann‐Whitney U test.
Fisher's exact test.
Abbreviations: ECOG, Eastern Cooperative Oncology Group; FACT‐L, the Functional Assessment of Cancer Therapy‐Lung; HADS, Hospital Anxiety and Depression Scale; IQR, interquartile range; SF‐8, Short‐Form 8‐Item Health Survey.
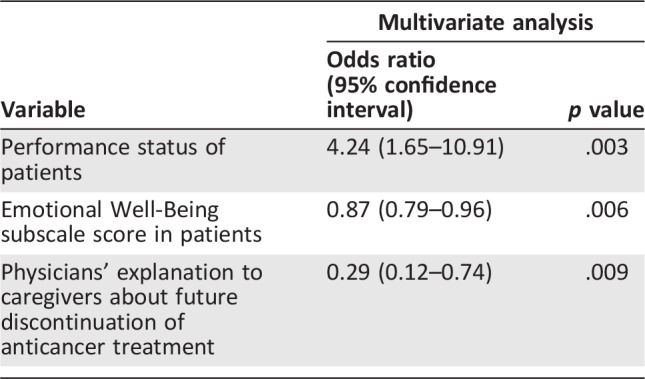
The subsequent binary logistic regression analysis (shown in Table 4) demonstrated that patients’ higher FACT‐EWB and lower FACT‐LCS were significant predictors of patient misunderstandings about prognosis (p < .001 and p = .043, respectively). In caregivers (shown in Table 5), misunderstandings about the patient's prognosis were associated with the patient's better performance status and with the patient's higher emotional well‐being (p < .001 and p = .004, respectively). Caregivers who received the explanations about future discontinuation of anticancer treatment were more likely to have accurate prognostic understanding (p = .034). No significant predictor was found for accurate understanding on goals of therapy in patients. Caregivers were more likely to misunderstand the goals of therapy when the patients were younger and had clinical stage IIIB disease (p = .005 and p = .005 respectively). The caregivers with higher physical QOL (PCS scores of SF‐8) are more likely to misunderstand the patient's goals of therapy (p = .046).
Table 4. Multivariate analysis of predictive factors of misunderstandings about prognosis in patients (binary logistic regression model).
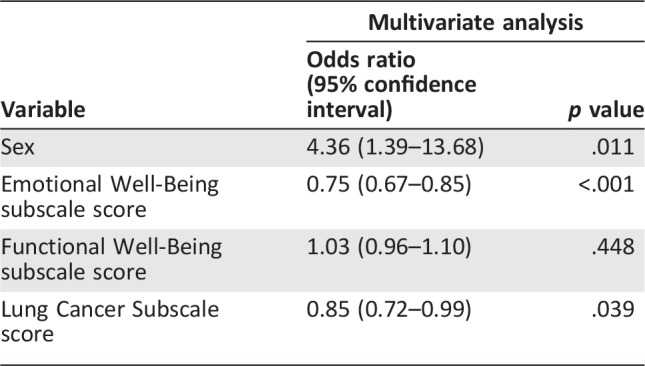
Table 5. Multivariate analysis of predictive factors of misunderstandings about prognosis in caregivers (binary logistic regression model).
Discussion
In this multicenter study, we demonstrated that substantial proportions of both patients with newly diagnosed advanced lung cancer and their caregivers had misunderstandings about their prognosis. To the best of the authors’ knowledge, this is the first study that evaluated prognostic understanding of advanced lung cancer patients and their caregivers simultaneously and investigated their associated factors, including self‐reported outcomes and the status of disclosure of information by their treating physicians. Also, of note, this is the first study in Japan that systematically evaluated advanced cancer patients’ understanding of their prognosis and the goal of therapy at the time of diagnosis.
A substantial proportion of the participants misunderstood their prognosis and goals of treatment, even though the proportion was relatively low compared with that of previous studies [1], [4], [5], [10], [11], [12], [16], [17]. Such misunderstandings can be crucial, because they could negatively affect decision‐making regarding choice of cancer treatments and supportive care [2], [3], [4], [5], [6], [7]. Discrepancies between a patient and their caregiver in understanding of the prognosis and goals of therapy were observed in a substantial proportion of patient‐caregiver dyads, as has been reported by Burns et al. [16]. Such discrepancies may negatively affect patients’ well‐being due to inappropriate support and communication. Provision of appropriate psychosocial care to cancer patients and their family caregivers from the time of cancer diagnosis has been promoted under the Basic Plan to Promote Cancer Control Program, which was launched in 2007 and revised in 2012 and 2017. A relatively high proportion of accurate illness understanding may be partly attributable to this health policy. However, it is evident that further promotion is necessary.
Contrary to our hypotheses, provision of information by the treating physician was not associated with accurate understanding of illness status or the goal of therapy in patients. A possible explanation is that physicians’ methods of providing information were too ambiguous or too complicated for patients to understand [14] or that patients were too emotionally overwhelmed to understand the physicians’ explanations, even though they had been provided.
Notably, explanations about future discontinuation of anticancer treatment were associated with accurate understanding of prognosis in caregivers. Caregivers may be more likely to accept physicians’ explanations in a more straightforward manner than patients, while patients may deny the seriousness of their situation. Additionally, we speculate that information on the possibility of future discontinuation of chemotherapy is less overwhelming and more acceptable to caregivers than other kinds of information, such as incurability and life expectancy. Moreover, for physicians, telling patients and caregivers about incurability, expected length of life, and palliative care may be more difficult than telling them about the probability of discontinuing chemotherapy [14], [36]. Although these findings need to be verified further, they provide some insight into what type of information is beneficial to facilitate accurate prognostic understanding among patients and caregivers.
Our study demonstrated a few key factors that are associated with accurate prognostic understanding. Clinical factors, such as performance status, stage of cancer, and types of planned treatment, were not associated with prognostic understanding; rather, patients’ subjective factors appear to play a greater role. Consistent with past studies, female patients are more likely to have accurate prognostic understanding [1], [32], [33], [34]. Our study highlighted that employed patients are more likely to misunderstand their prognosis. In combination with the findings that patients with higher emotional well‐being and lower lung cancer symptom burden are more likely to misunderstand their illness as “curable,” we speculate that people in relatively good conditions tend to deny their real clinical status. On the other hand, patients with greater symptom burden and worse QOL may be able to assess their illness more accurately. Because our study is cross‐sectional and causal relationship is unclear, we can interpret it the other way: It is possible that accurate understanding of prognosis disappointed the patients, which resulted in lower emotional well‐being. Consistent with our finding, one cross‐sectional study demonstrated that awareness of terminal illness was associated with heightened emotional struggle and lessened sense of peacefulness in patients with advanced cancer [37]. The process of developing prognostic understanding may parallel with emotional reactions to the illness.
Caregivers’ prognostic understanding was associated mostly with characteristics of the patients rather than those of the caregiver themselves. It seems that caregivers perceive patients’ illness status from the perspectives of the patient, rather than objective clinical status.
In both patients and caregivers, accurate perceptions of prognosis were associated with elevated levels of anxiety and depression. Even though we did not assess these associations in multivariate analyses, extra psychosocial support for both patients and caregivers is needed after the diagnosis of advanced cancer [19], [34], [38].
Our data suggest that patients and caregivers interpret physicians’ explanations differently, causing discrepancies in prognostic understanding between them. Interestingly, discordance in perceptions of prognosis was also associated with higher emotional well‐being of patients (p = .002; supplemental online Table 3).
Our study has a few limitations. First, the number of recruited patients was relatively small, and they may not fully represent the whole of lung cancer patients in Japan. Some sampling bias may exist because in the comparison of the patients who participated in the study and those who did not, the latter were more likely to receive best supportive care (BSC) as an initial treatment. Treating physicians might be hesitant to approach such patients. Comparison with the national cancer registry data revealed that the proportion of the patients who received BSC was much less in our registry cohort [39]. Besides, the physicians who cooperated in this study might focus more intensively on disclosing prognostic information to their patients and their caregivers than the physicians who did not participate. Second, assessment of illness understanding has not been validated. Although we used similar questions to those that had been employed in previously published studies, the questionnaire has not been validated in the Japanese cancer population. Further, clinical interview may have been more reliable than a self‐administered questionnaire. Some participants may have expressed their “wishes” rather than their actual understanding regarding their prognosis and goals of therapy. Third, the quality of information provided by the physicians was not verified. It is unclear whether physicians appropriately conveyed information to their patients and caregivers. Fourth, because this was a cross‐sectional study, causal relationships of the associated variables cannot be inferred. The nature of our study should be considered hypothesis generating rather than confirmatory. The factors associated with illness understanding in this study need further validation. Also, other possible explanatory factors that may affect illness understanding (race, culture, religion, beliefs, education, and economic status of the participants) were not examined in this study.
Despite these limitations, this study is noteworthy in that it is the first to evaluate illness understanding of patients with advanced lung cancer and their caregivers in Japan and to highlight clinically important associated factors.
Conclusion
Not only patients with advanced lung cancer but also their caregivers have difficulty attaining accurate prognostic understanding. It appears that patients tend to judge their illness status according to their subjective well‐being. In addition, caregivers seem to understand patients’ illness status from the patients’ perspectives. Better communication with physicians may have substantial benefits in terms of accurate understanding.
See http://www.TheOncologist.com for supplemental material available online.
Acknowledgments
We thank Naoto Minematsu (Department of Medicine, Hino Municipal Hospital, Tokyo, Japan), Akira Umeda (International University of Health and Welfare Shioya Hospital, Tochigi, Japan), Toru Shirahata (Saitama Medical Center, Saitama, Japan), Hidefumi Koh (Tachikawa Hospital, Tokyo, Japan), Hiroki Tateno (Saitama Municipal Hospital, Saitama, Japan), and Chiyomi Uemura for assisting in data collection. We also thank Jane Brill, Stephanie Tuminello, Maya Fridrikh, and Editage (www.editage.jp) for English‐language editing.
Author Contributions
Conception/design: Takashi Sato, Kenzo Soejima, Daisuke Arai, Katsuhiko Naoki
Provision of study material or patients: Takashi Sato, Kenzo Soejima, Katsuhiko Naoki, Ichiro Kawada, Hiroyuki Yasuda, Tomoko Betsuyaku
Collection and/or assembly of data: Takashi Sato, Ichiro Nakachi, Ichiro Kawada, Hiroyuki Yasuda, Kota Ishioka, Shigenari Nukaga, Katsunori Masaki, Takashi Inoue, Kota Hikima, Morio Nakamura, Keiko Ohgino, Yoshitaka Oyamada, Yohei Funatsu, Takeshi Terashima, Naoki Miyao, Koichi Sayama, Fumitake Saito, Fumio Sakamaki, Tomoko Betsuyaku
Data analysis and interpretation: Takashi Sato, Kenzo Soejima, Daisuke Fujisawa, Mari Takeuchi, Daisuke Arai, Katsuhiko Naoki, Ichiro Nakachi
Manuscript writing: Takashi Sato, Kenzo Soejima, Daisuke Fujisawa, Mari Takeuchi, Daisuke Arai, Ichiro Nakachi, Tomoko Betsuyaku
Final approval of manuscript: Takashi Sato, Kenzo Soejima, Daisuke Fujisawa, Mari Takeuchi, Ichiro Nakachi, Tomoko Betsuyaku
Disclosures
The authors indicated no financial relationships.
References
- 1. Baek SK, Kim SY, Heo DS et al. Effect of advanced cancer patients' awareness of disease status on treatment decisional conflicts and satisfaction during palliative chemotherapy: A Korean prospective cohort study. Support Care Cancer 2012;20:1309–1316. [DOI] [PubMed] [Google Scholar]
- 2. Hui D, Con A, Christie G et al. Goals of care and end‐of‐life decision making for hospitalized patients at a Canadian tertiary care cancer center. J Pain Symptom Manage 2009;38:871–881. [DOI] [PubMed] [Google Scholar]
- 3. Wright AA, Mack JW, Kritek PA et al. Influence of patients' preferences and treatment site on cancer patients' end‐of‐life care. Cancer 2010;116:4656–4663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Temel JS, Greer JA, Admane S et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non‐small‐cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319–2326. [DOI] [PubMed] [Google Scholar]
- 5. Yun YH, Lee MK, Kim SY et al. Impact of awareness of terminal illness and use of palliative care or intensive care unit on the survival of terminally ill patients with cancer: Prospective cohort study. J Clin Oncol 2011;29:2474–2480. [DOI] [PubMed] [Google Scholar]
- 6. Silvestri G, Pritchard R, Welch HG. Preferences for chemotherapy in patients with advanced non‐small cell lung cancer: Descriptive study based on scripted interviews. BMJ 1998;317:771–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weeks JC, Cook EF, O'Day SJ et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences. JAMA 1998;279:1709–1714. [DOI] [PubMed] [Google Scholar]
- 8. Craft PS, Burns CM, Smith WT et al. Knowledge of treatment intent among patients with advanced cancer: A longitudinal study. Eur J Cancer Care (Engl) 2005;14:417–425. [DOI] [PubMed] [Google Scholar]
- 9. Weeks JC, Catalano PJ, Cronin A et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tang ST, Liu TW, Chow JM et al. Associations between accurate prognostic understanding and end‐of‐life care preferences and its correlates among Taiwanese terminally ill cancer patients surveyed in 2011–2012. Psychooncology 2014;23:780–787. [DOI] [PubMed] [Google Scholar]
- 11. Corli O, Apolone G, Pizzuto M et al. Illness awareness in terminal cancer patients: An Italian study. Palliat Med 2009;23:354–359. [DOI] [PubMed] [Google Scholar]
- 12. Chan WC. Being aware of the prognosis: How does it relate to palliative care patients' anxiety and communication difficulty with family members in the Hong Kong Chinese context? J Palliat Med 2011;14:997–1003. [DOI] [PubMed] [Google Scholar]
- 13. Gattellari M, Voigt KJ, Butow PN et al. When the treatment goal is not cure: Are cancer patients equipped to make informed decisions? J Clin Oncol 2002;20:503–513. [DOI] [PubMed] [Google Scholar]
- 14. Enzinger AC, Zhang B, Schrag D et al. Outcomes of prognostic disclosure: Associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol 2015;33:3809–3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leighl NB, Shepherd FA, Zawisza D et al. Enhancing treatment decision‐making: Pilot study of a treatment decision aid in stage IV non‐small cell lung cancer. Br J Cancer 2008;98:1769–1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Burns CM, Broom DH, Smith WT et al. Fluctuating awareness of treatment goals among patients and their caregivers: A longitudinal study of a dynamic process. Support Care Cancer 2007;15:187–196. [DOI] [PubMed] [Google Scholar]
- 17. Silveira MJ, Given CW, Given B et al. Patient‐caregiver concordance in symptom assessment and improvement in outcomes for patients undergoing cancer chemotherapy. Chronic Illn 2010;6:46–56. [DOI] [PubMed] [Google Scholar]
- 18. Burns CM, Dixon T, Broom D et al. Family caregiver knowledge of treatment intent in a longitudinal study of patients with advanced cancer. Support Care Cancer 2003;11:629–637. [DOI] [PubMed] [Google Scholar]
- 19. El‐Jawahri A, Traeger L, Park ER et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 2014;120:278–285. [DOI] [PubMed] [Google Scholar]
- 20. Wolfe J, Klar N, Grier HE et al. Understanding of prognosis among parents of children who died of cancer: Impact on treatment goals and integration of palliative care. JAMA 2000;284:2469–2475. [DOI] [PubMed] [Google Scholar]
- 21. Sandler A, Gray R, Perry MC et al. Paclitaxel‐carboplatin alone or with bevacizumab for non‐small‐cell lung cancer. N Engl J Med 2006;355:2542–2550. [DOI] [PubMed] [Google Scholar]
- 22. Fukuoka M, Wu YL, Thongprasert S et al. Biomarker analyses and final overall survival results from a phase III, randomized, open‐label, first‐line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non‐small‐cell lung cancer in Asia (IPASS). J Clin Oncol 2011;29:2866–2874. [DOI] [PubMed] [Google Scholar]
- 23. Cella DF, Bonomi AE, Lloyd SR et al. Reliability and validity of the Functional Assessment of Cancer Therapy‐Lung (FACT‐L) quality of life instrument. Lung Cancer 1995;12:199–220. [DOI] [PubMed] [Google Scholar]
- 24. Saitoh E, Yokomizo Y, Chang CH et al. Cross‐cultural validation of the Japanese version of the lung cancer subscale on the functional assessment of cancer therapy‐lung. J Nippon Med Sch 2007;74:402–408. [DOI] [PubMed] [Google Scholar]
- 25. Ware JE, Kosinski M, Dewey JE et al. How to Score and Interpret Single‐Item Health Status Measures: A Manual for Users of the SF‐8 Health Survey. Lincoln, RI: QualityMetric, Inc, 2001. [Google Scholar]
- 26. Fukuhara S, Suzukamo Y. Manual of the SF‐8 Japanese Version. Kyoto, Japan: Institute for Health Outcomes and Process Evaluation Research, 2004. [Google Scholar]
- 27. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 28. Kitamura T. The Hospital Anxiety and Depression Scale [in Japanese]. Arch Psychiatr Diagn Clin Eval 1993;4:371–372. [Google Scholar]
- 29. Tokuda Y, Okubo T, Ohde S et al. Assessing items on the SF‐8 Japanese version for health‐related quality of life: A psychometric analysis based on the nominal categories model of item response theory. Value Health 2009;12:568–573. [DOI] [PubMed] [Google Scholar]
- 30. Higashi A, Yashiro H, Kiyota K et al. Validation of the hospital anxiety and depression scale in a gastro‐intestinal clinic [in Japanese]. Nihon Shokakibyo Gakkai Zasshi 1996;93:884–892. [PubMed] [Google Scholar]
- 31. Matsudaira T, Igarashi H, Kikuchi H et al. Factor structure of the Hospital Anxiety and Depression Scale in Japanese psychiatric outpatient and student populations. Health Qual Life Outcomes 2009;7:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Papadopoulos A, Vrettos I, Kamposioras K et al. Impact of cancer patients' disease awareness on their family members' health‐related quality of life: A cross‐sectional survey. Psychooncology 2011;20:294–301. [DOI] [PubMed] [Google Scholar]
- 33. Bracci R, Zanon E, Cellerino R et al. Information to cancer patients: A questionnaire survey in three different geographical areas in Italy. Support Care Cancer 2008;16:869–877. [DOI] [PubMed] [Google Scholar]
- 34. Hinton J. The progress of awareness and acceptance of dying assessed in cancer patients and their caring relatives. Palliat Med 1999;13:19–35. [DOI] [PubMed] [Google Scholar]
- 35. Greer JA, Pirl WF, Jackson VA et al. Perceptions of health status and survival in patients with metastatic lung cancer. J Pain Symptom Manage 2014;48:548–557. [DOI] [PubMed] [Google Scholar]
- 36. Sato RS, Beppu H, Iba N et al. The meaning of life prognosis disclosure for Japanese cancer patients: A qualitative study of patients' narratives. Chronic Illn 2012;8:225–236. [DOI] [PubMed] [Google Scholar]
- 37. Mack JW, Nilsson M, Balboni T et al. Peace, Equanimity, and Acceptance in the Cancer Experience (PEACE): Validation of a scale to assess acceptance and struggle with terminal illness. Cancer 2008;112:2509–2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fang F, Fall K, Mittleman MA et al. Suicide and cardiovascular death after a cancer diagnosis. N Engl J Med 2012;366:1310–1318. [DOI] [PubMed] [Google Scholar]
- 39.Division of Cancer Surveillance National Cancer Center Japan. Hospital‐based cancer registry. 2015 National Report [in Japanese]. Available at http://ganjoho.jp/data/reg_stat/statistics/brochure/2015_report.pdf. Accessed November 21, 2017. [Google Scholar]