Abstract
The erector spinae plane (ESP) block is a novel plane block first reported for thoracic analgesia. It affects the dorsal and ventral rami of the thoracic nerves. Owing to the ease of the technique and decreased risk of complication of the ESP block under ultrasound guidance, it can be a preferable procedure compared with other invasive techniques, such as neuraxial and nerve blocks. In this case report, we presented three patients who had thoracic surgery under general anesthesia. The ESP block and catheter placement was applied to the patients before operation. The catheter was inserted deep into the erector spinae muscle and was used successfully for postoperative pain management.
Keywords: Anaesthesiology, rerioperative and adult anesthesiology, pain medicine
Introduction
Regional anesthesia under ultrasound guidance (USG) is the most common technique for patients [1]. Radiological and anatomical cadaveric studies have been uncovering new block techniques. The most recently described plane block under USG is the erector spinae plane (ESP) block. This new block is performed at the level of the T5 spinous process under USG in the longitudinal probe orientation by using a linear probe and a sensory block spanning T3 to T9; the technique is done while the patient is in a sitting position [2].
We present three cases of the ESP block using a continuous technique for intraoperative and postoperative analgesia. Written informed consent was obtained from all of the patients included in this case report. The continuous ESP catheters were inserted in the patients in either the operating room or the regional anesthesia room. The level of the block was at T5 with a 30 mL local anesthesia (LA) mixture (10 mL of 0.5% bupivacaine, 10 mL of 2% lidocaine, and 10 mL of 0.9% saline) in all three cases. On postoperative day 3, the catheter was removed. All three cases were operated under general anesthesia with the same procedure for all of the patients.
Case Presentations
Case 1
A 37-year-old woman weighing 65 kg at a height of 162 cm and with American Society of Anesthesiologists (ASA) physical status I underwent surgery for esophageal leiomyoma under general anesthesia. The patient was placed in a prone position, and a linear US probe was used for ESP block catheter placement at the T5 spinous process approximately 3 cm laterally [2]. The LA solution (a 1:1:1 mixture of 30 mL of 0.5% bupivacaine, 2% lidocaine, and 0.9% saline) was injected deep into the erector spinae muscle. After LA injection, an epidural catheter (Perifix® Complete Set, B-Braun, Germany) was inserted and fixed to the skin. An evaluation of the sensory block was performed 20 min after the administration of the ESP block by pinprick and cold sensation tests. An esophageal leiomyoma was resected thoracoscopically. The patient’s neurologic rating scale (NRS) score was 2/10 in the postoperative care unit (PACU) in the first 12 h, and no rescue analgesia was needed. When the patient started to feel pain again, a second dose of LA mixture (15 mL of 0.5% bupivacaine and 15 mL of 0.9% saline) was injected through the catheter. The patient reported that her pain was relieved within 10 min.
Case 2
A 56-year-old man weighing 83 kg at a height of 175 cm and with ASA physical status I was diagnosed with lung cancer and was scheduled for an operation under general anesthesia. A US guided ESP block was performed before starting general anesthesia. A linear US probe was used for the block, which was placed at the T5 vertebral level. Pinprick and cold sensation tests were used to evaluate the sensory block and showed a loss of sensation after 30 min. The patient underwent a left-lower lobectomy. After surgical procedure, the patient was extubated and transferred to the PACU. The patient’s NRS score was 0/10 in the PACU in the first hour, and the sensory block was between the levels of the T3 and T10 dermatomes. The patient’s pain scores were assessed every hour, and he did not need rescue analgesia for the first 14 h. When the patient’s NRS score was >3, a second dose of LA mixture (15 mL of 0.5% bupivacaine and 15 mL of 0.9% saline) was administered through the catheter. During the operation, 200 μg of fentanyl was administered.
Case 3
A 48-year-old man with ASA status I who had been diagnosed with a right-side pulmonary hamartoma was scheduled for a thoracoscopic pulmonary wedge resection under general anesthesia. The patient was placed in a prone position, and a right-side ESP block was performed. An epidural catheter was inserted under the erector spinae muscle in the operating room (Figure 1). We aimed to put the catheter under the ESP muscle, and the catheter position was evaluated using air (Figure 2). Cold sensation and pinprick tests were used to evaluate the sensory block. A loss of the sensory block was determined within 30 min after the ESP block. A thoracoscopic pulmonary wedge resection was performed. The intraoperative process was uneventful, and general anesthesia was continued without any addition of opioids apart from 100 μg of fentanyl used at the induction. The patient’s NRS score was 1/10 in the first hour after the operation, and he did not need any analgesia for 13 h. A 30 ml mixture (15 mL of 0.5% bupivacaine and 15 mL of 0.9% saline) was injected through the catheter a second time.
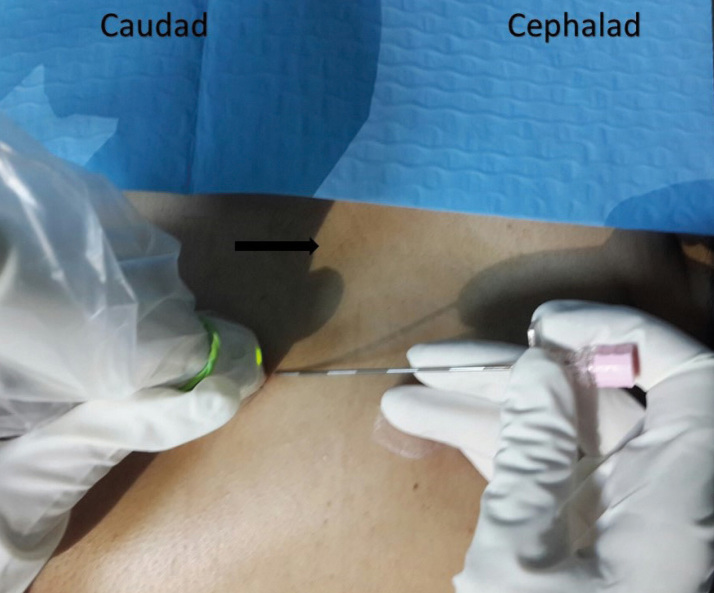
Figure 1.
Position of patient, needle, and ultrasound probe. Black arrow shows the midline.
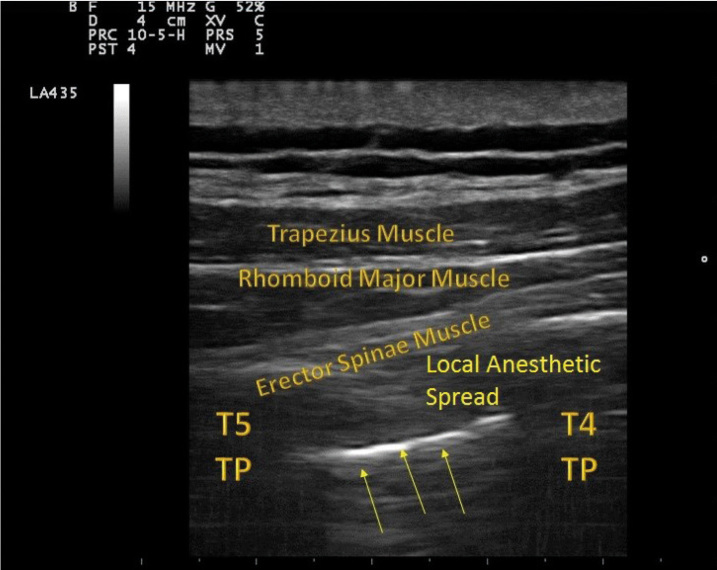
Figure 2.
Ultrasound-guided erector spinae plane block. Yellow arrows show the catheter placed under the erector spinae muscle. After 3 ml of air was injected through the catheter, it appeared hyperechoic under ultrasound imaging. TP: transverse process.
Discussion
The three case reports present successful pain management after thoracic surgery using an ESP block catheter. Some US guided plane blocks have been described for chest wall surgery [3, 4]. The ESP block has recently been described for analgesia after thoracic surgery and chronic thoracic neuropathic pain [2]. Since the introduction of the ESP block, it has been used for different surgical procedures, including hip surgery and cesarean section surgery at different vertebral levels [5, 6]. In the three cases reported here, we inserted a catheter deep into the ESP muscle and evaluated the effectiveness of the ESP block intraoperatively and through continuous analgesia management via catheter. The patients did not need any additional analgesia medication during their surgeries, and their NRS scores showed that the patients did not feel pain after surgery for approximately 12 h. In addition, pain management was achieved successfully by placing a catheter deep into the ESP block.
We performed the ESP block in a prone position. We believe that this position is more comfortable than a sitting or lateral position, especially for patients whom inserted catheter is more comfortable than others owing to the duration of the procedure. In addition, we used a 30 ml volume of LA, and we believe that plane blocks, such as ESP, need more volume, and that these blocks are volume dependent. Further studies are required to compare the effects of different volumes of LA.
On the other hand, the ESP block is a simple block. The block is technically easy to perform, and serious side effects are rare under USG compared with neuraxial and nerve blocks [7]. Furthermore, to our knowledge, no study has compared neuraxial and nerve blocks with ESP blocks.
Thoracic surgery is a very painful surgical procedure, and thoracic epidural analgesia and serratus anterior plane blocks have been used successfully [8, 9]. We performed US guided ESP blocks in these three cases owing to its safety and ease of use. Further additional controlled and randomized studies of the ESP block are required to demonstrate its safety, ease, and effectiveness.
Footnotes
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – I.I.; Design – I.I.; Supervision - Y.A.; Resources – M.A.; Materials – S.Z.; Data Collection and/or Processing – S.Z.; Analysis and/or Interpretation – I.I.; Literature Search – A.B.U.; Writing Manuscript – I.I.; Critical Review – O.O.
Conflict of Interest: Authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Ince I, Aksoy M, Celik M. Can We Perform Distal Nerve Block Instead of Brachial Plexus Nerve Block Under Ultrasound Guidance for Hand Surgery? Eurasian J Med. 2016;48:167–71. doi: 10.5152/eurasianjmed.2016.0256. https://doi.org/10.5152/eurasianjmed.2016.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. https://doi.org/10.1097/AAP.0000000000000451 [DOI] [PubMed] [Google Scholar]
- 3.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13. doi: 10.1111/anae.12344. https://doi.org/10.1111/anae.12344 [DOI] [PubMed] [Google Scholar]
- 4.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. https://doi.org/10.1016/j.redar.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 5.Tulgar S, Senturk O. Ultrasound guided Erector Spinae Plane block at L-4 transverse process level provides effective postoperative analgesia for total hip arthroplasty. J Clin Anesth. 2018;44:68. doi: 10.1016/j.jclinane.2017.11.006. https://doi.org/10.1016/j.jclinane.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 6.Yamak Altinpulluk E, García Simón D, Fajardo-Pérez M. Erector spinae plane block for analgesia after lower segment caesarean section: Case report. Rev Esp Anestesiol Reanim. 2018;65:284–6. doi: 10.1016/j.redar.2017.11.006. https://doi.org/10.1016/j.redar.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 7.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118:474–5. doi: 10.1093/bja/aex013. https://doi.org/10.1093/bja/aex013 [DOI] [PubMed] [Google Scholar]
- 8.De la Cuadra-Fontaine JC, Concha M, Vuletin F, Arancibia H. Continuous Erector Spinae Plane block for thoracic surgery in a pediatric patient. Paediatr Anaesth. 2018;28:74–5. doi: 10.1111/pan.13277. https://doi.org/10.1111/pan.13277 [DOI] [PubMed] [Google Scholar]
- 9.Khalil AE, Abdallah NM, Bashandy GM, Kaddah TA. Ultrasound-Guided Serratus Anterior Plane Block Versus Thoracic Epidural Analgesia for Thoracotomy Pain. J Cardiothorac Vasc Anesth. 2017;31:152–8. doi: 10.1053/j.jvca.2016.08.023. https://doi.org/10.1053/j.jvca.2016.08.023 [DOI] [PubMed] [Google Scholar]