Abstract
Background
Restoring normal femoral rotation is an important consideration when managing femur fractures. Femoral malrotation after fixation is common and several preventive techniques have been described. Use of the lesser trochanter profile is a simple method to prevent malrotation, because the profile changes with femoral rotation, but the accuracy of this method is unclear.
Questions/purposes
The purposes of this study were (1) to report the rotational profiles of uninjured femora in an adult population; and (2) to determine if the lesser trochanter profile was associated with variability in femoral rotation.
Methods
One hundred fifty-five consecutive patients (72% female and 28% male) with a mean age of 32 years (range, 12–56 years) with a CT scanogram were retrospectively evaluated. Patients were included if CT scanograms had adequate cuts of the proximal and distal femur. Patients were excluded if they had prior hip/femur surgery or anatomic abnormalities of the proximal femur. CT scanogram measurements of femoral rotation were compared with the lesser trochanter profile (distance from the tip of the lesser trochanter to the medial cortex of the femur) measured on weightbearing AP radiographs. These measurements were made by a single fellowship-trained orthopaedic surgeon and repeated for intraobserver reliability testing. Presence of rotational differences based on sex and laterality was assessed and correlation of the difference in lesser trochanter profile to the difference in femoral rotation was determined using a coefficient of determination (r2).
Results
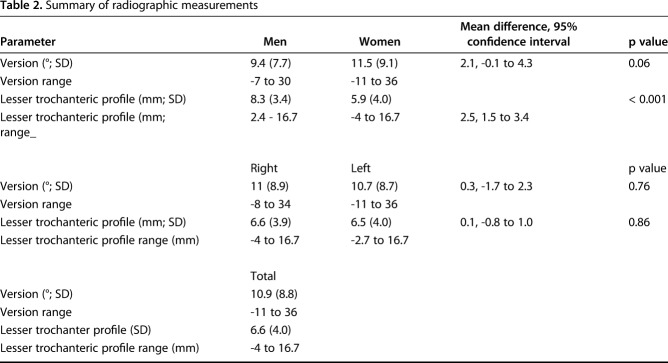
The mean femoral rotation was 10.9° (SD ± 8.8°) of anteversion. Mean right femoral rotation was 11.0° (SD ± 8.9°) and mean left femoral rotation was 10.7° (SD ± 8.7°) with a mean difference of 0.3° (95% confidence interval [CI], -1.7° to 2.3°; p = 0.76). Males had a mean rotation of 9.4°(SD ± 7.7°) and females had a mean rotation of 11.5° (SD ± 9.1°) with a mean difference of 2.1° (95% CI, -0.1° to 4.3°; p = 0.06). Mean lesser trochanter profile was 6.6 mm (SD ± 4.0 mm). Mean right lesser trochanter profile was 6.6 mm (SD ± 3.9 mm) and mean left lesser trochanter profile was 6.5 mm (SD ± 4.0 mm) with a mean difference of 0.1 mm (-0.8 mm to 1.0 mm, p = 0.86). The lesser trochanter profile varied between the sexes; males had a mean of 8.3 mm (SD ± 3.4), and females had a mean of 5.9 mm (SD ± 4.0). The mean difference between sexes was 2.5 mm (1.5-3.4 mm; p < 0.001). The magnitude of the lesser trochanter profile measurement and degree of femoral rotation were positively correlated such that increasing measures of the lesser trochanter profile were associated with increasing amounts of femoral anteversion. The lesser trochanter profile was associated with femoral version in a linear regression model (r2 = 0.64; p < 0.001). Thus, 64% of the difference in femoral rotation can be explained by the difference in the lesser trochanter profile. Intraobserver reliability for both the femoral version and lesser trochanter profile was noted to be excellent with intraclass correlation coefficients of 0.94 and 0.95, respectively.
Conclusions
This study helps define the normal femoral rotation profile among adults without femoral injury or bone deformity and demonstrated no rotational differences between sexes. The lesser trochanter profile was found to be positively associated with femoral rotation. Increasing and decreasing lesser trochanter profile measurements are associated with increasing and decreasing amounts of femoral rotation, respectively.
Clinical Relevance
The lesser trochanter profile can determine the position of the femur in both anteversion and retroversion, supporting its use as a method to restore preinjury femoral rotation after fracture fixation. Although some variability in the rotation between sides may exist, matching the lesser trochanter profile between injured and uninjured femora can help reestablish native rotation.
Introduction
The rotational profile of the femur is of clinical importance in many orthopaedic procedures and is a primary focus during fracture fixation [2, 6, 19, 21, 23, 25, 28, 30, 31]. Malrotation of the femur after fracture fixation is often underappreciated and is a difficult complication to detect both clinically and radiographically [19]. Several studies have demonstrated a high risk of malrotation after fracture fixation [3, 11, 13, 26, 29] and this remains a challenging aspect of femur fracture care [2, 6, 8, 25, 28, 30, 31]. Malrotation may negatively influence outcomes after surgery [12, 27] and may have detrimental long-term effects on knee function [10, 20]. Malrotation after femoral fracture surgery is associated with abnormal foot progression angles [12, 27], a posterior shift of the weightbearing axis of the knee [10], and higher peak patellofemoral contact pressure [20], which may lead to worse functional outcomes as measured by the Oxford-12 item and WOMAC surveys [12].
Femoral rotation, anteversion, and retroversion may be restored through indirect means such as assessment of cortical thickness and alignment on intraoperative imaging [19]. However, fractures at higher risk of malrotation such as those that are transverse, segmental, comminuted, or associated with bone loss may not be as amenable to indirect assessment [14]. Clinical assessment of rotation by radiographic and/or clinical comparison of the injured and unaffected extremity is another means of judging rotation but has proven to be inconsistent [13].
The challenges of assessing and restoring femoral anteversion during fracture fixation have led to the advent of several fluoroscopic measurements to address this problem [4, 7, 29]. Each technique uses fluoroscopic images of the uninjured extremity as a template to restore anatomy to the injured extremity. Deshmukh et al. [7] popularized using the fluoroscopic profile of the lesser trochanter to guide restoration of femoral rotation during fracture fixation. This method has become accepted as a simple, effective manner of preventing malrotation that does not unduly prolong operative time or require special instrumentation [7, 15, 16, 18]. The principle used by Deshmukh et al. [7] is that the image of the lesser trochanter becomes more pronounced in the coronal plane with increased external rotation angles. However, prior work has demonstrated large anatomic variability of the proximal femur, and it is unclear if this variation in anatomy is reflected through the lesser trochanter profile [15, 21] or whether the lesser trochanter profile is an accurate predictor of rotation. To our knowledge, no study has reported on rotational profiles of uninjured femora in a large patient cohort using modern measurement techniques and compared this with the lesser trochanter profile.
The goal of this study therefore was to (1) report on the rotational profiles of uninjured femora in an adult population as measured by CT scanogram; and (2) determine if variability in native femoral rotation was associated with the lesser trochanter profile.
Patients and Methods
Institutional review board approval was obtained using an umbrella protocol for retrospective studies at our institution. All skeletally mature patients treated at our tertiary referral center between January 2010 and June 2017 who had a CT scanogram were identified with the use of Current Procedural Terminology (CPT) coding. Patients with CPT code 77037 (bone length studies [orthoroentgenogram, scanogram]) were included in the data set. CT scanograms were reviewed to isolate the patients who had adequate imaging to measure the rotational profile of both femurs. Patient age, sex, and the radiographic measurements of interest were recorded. Patient chart review was used to determine if prior hip, femur, or knee surgery had been performed and make note of prior femur fracture.
All patients included in this study were skeletally mature and seen by a single fellowship-trained orthopaedic surgeon specializing in hip pathology (TGM). The indication for plain radiographic imaging was generalized hip pain, and CT scanograms were obtained when plain radiographs demonstrated no evidence of significant arthrosis as an advanced imaging evaluation for possible osseous pathomorphology. CT scanograms had to include adequate cuts of the proximal and distal femur to allow for an accurate assessment of femoral rotation. Patients were excluded from the study if they had prior trauma to the femur or previous surgical intervention involving the hip, femur, or knee. Patients with anatomic abnormalities of the lesser trochanter or proximal femur such as prior slipped capital femoral epiphysis (SCFE) or Legg-Calvé-Perthes disease were also excluded from the study.
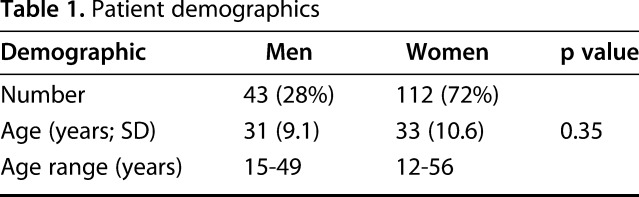
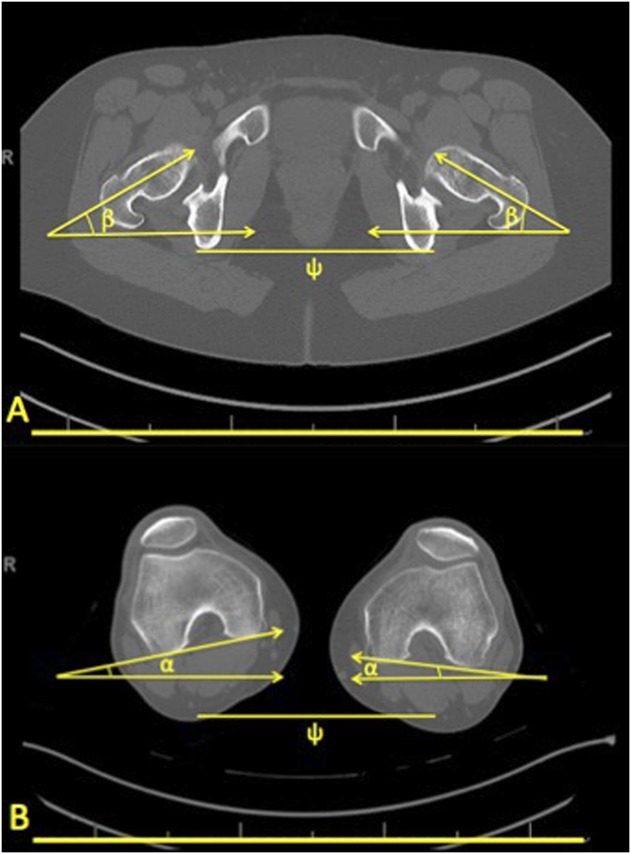
A total of 214 consecutive patient scanograms were reviewed initially. Of this cohort, 59 patients were excluded from the study for the following reasons: lack of bilateral imaging (53), abnormal appearance of the lesser trochanter (three), a prior diagnosis of SCFE (two), or a fracture of the lesser trochanter (one). The remaining 155 patients (310 femora) were included in the study (Fig. 1). Mean age of the cohort was 32 years (range, 12-56 years) with 112 (72%) female and 43 (28%) male (Table 1).
Fig. 1.
A flowchart displays those patients included and excluded from the study. SCFE, Perthes, and lesser trochanter (LT) fractures were excluded from the study.
Table 1.
Patient demographics
All CT scanograms were obtained by certified CT technicians at the university hospital or university orthopaedic center per a standard protocol. The images were obtained with the patient placed in a CT scanner in a supine position with both feet pointed up and the long axis of the femora parallel to the long axis of the scanner. Legs were positioned flat on the table with no cushion or wedges allowed. A full-length scout film was obtained to include the bilateral hips and ankles. Thereafter, 3-mm thick helical images taken in 3-mm intervals were obtained at the hips and knees. This included cuts from just above the femoral heads through the lesser trochanters and from just above the femoral physis through the top of the tibia.
Weightbearing AP pelvis radiographs were obtained by experienced technicians at the university orthopaedic center using a standard protocol. These images were acquired with patients in a standing position and with the lower extremities parallel. The lower extremities were aligned in a neutral position with knees and feet pointed directly forward. Patients were instructed to bear equal weight on the bilateral lower extremities. The x-ray beam was directed at a center position between the pubic symphysis and anterosuperior iliac spine. We accounted for magnification of the image by using a marker ball to standardize measurements.
As per radiology protocol, the supine CT is obtained with the feet pointed up, whereas standard weightbearing AP pelvis radiographs were obtained with the feet pointing forward. There is no way to confirm, however, that the rotational profile of the leg was the same with each imaging study.
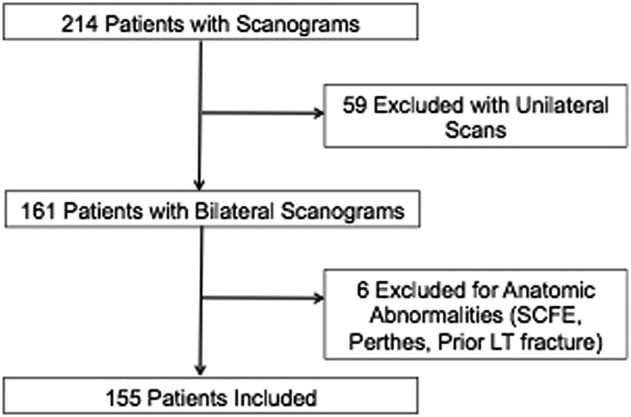
Femoral rotation was measured on the CT scanograms using a modified version of a technique initially described by Goldman and Freeman [9]. First, a line was drawn through the center of the femoral neck and an angle made relative to the horizontal plane in a single CT cut (β). Then a tangent line was drawn across the axis of the posterior femoral condyles and an angle made relative to the horizontal plane in that CT cut (α). The amount of femoral rotation was established by subtracting the condylar angle (α) from the neck angle (β) (Fig. 2). All rotational measurements were made by an attending, fellowship-trained orthopaedic surgeon (TGM). Intraobserver reliability for both the femoral rotation and lesser trochanter profile was determined using the intraclass correlation coefficient given that the data being analyzed were continuous. The single observer repeated measurements on 26 randomly selected hips from the data set. Measurements were made 3 months apart. The intraclass correlation coefficient determines reliability on a scale from 0 to 1, with 0 to 0.5 being poor, 0.51 to 0.75 being moderate, 0.76 to 0.9 being good, and 0.91 to 1 being excellent reliability. Convention was maintained throughout the study such that positive rotational values represent femoral anteversion and negative rotational values represent femoral retroversion.
Fig. 2A-B.
An example measurement of femoral rotation as determined on CT scanogram is shown. (A) An axial CT image of the pelvis was used to measure the rotation of the proximal femur (β). A line was drawn through the center of the femoral neck and an angle made relative to the horizontal plane (ψ) in a single CT cut (β = femoral neck rotation). (B) An axial CT image of the distal femur was used to measure the rotation of the distal femur (α). A tangent line was drawn across the axis of the posterior femoral condyles and an angle made relative to the horizontal plane (ψ) in that CT cut (α = distal femur rotation). The difference in these measurements is equal to femoral rotation (femoral rotation = β - α). β = Femoral neck rotation; α = distal femur rotation; ψ = horizontal plane.
The lesser trochanter profile was measured on the weightbearing AP radiograph. A vertical line was extended along the border of the medial femoral cortex proximally past the lesser trochanter. We then established a horizontal plane by using a transteardrop line. Parallel to the horizontal plane, the greatest distance from the apex of the lesser trochanter to the line extending along the medial femoral cortex was measured (Fig. 3). Convention was maintained throughout the study such that lesser trochanter profile measurements were positive if the tip of the lesser trochanter was medial to the vertical extension of the medial femoral cortex and negative if the tip of the lesser trochanter was lateral to the vertical extension of the medial femoral cortex.
Fig. 3.
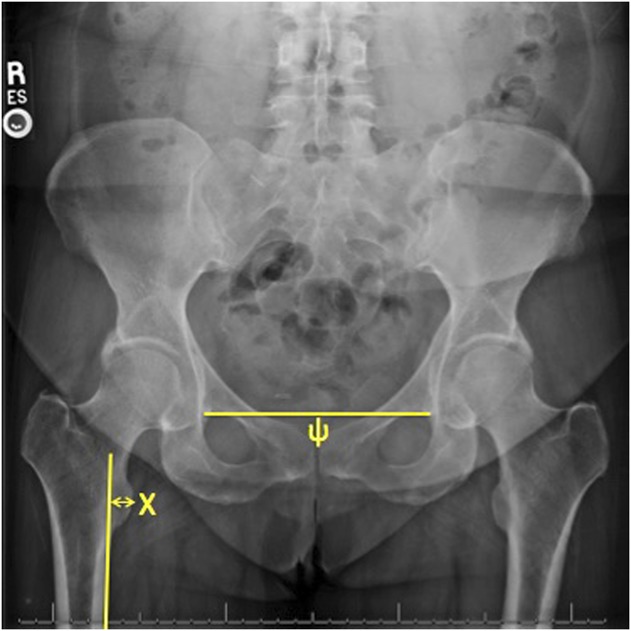
Example measurement of the lesser trochanter profile (X) as determined on a plain film radiograph. The lesser trochanter profile was measured from the apex of the lesser trochanter to the edge of a line drawn along the medial border of the femoral cortex. The horizontal plane (ψ) was established using a transteardrop horizontal line.
All measurements were made with a virtual ruler on magnified digital images on a university-licensed imaging system (Intellispace PACS Enterprise; Phillips, Foster City, CA, USA).
Statistical Analysis
For calculated differences in laterality, the measurement for the left hip was subtracted from the measurement of the right hip for all calculations. Statistical comparison of the mean age data was completed using a two-tailed Student’s t-test. Means for radiographic measurements were calculated and a two-tailed Student’s t-test was used to determine the presence of differences based on sex and laterality. Correlation of differences in the lesser trochanter profile to differences in femoral rotation was determined using a coefficient of determination (r2) for the entire cohort as well as by sex. As is standard for determining r2 values, outliers were removed from the data set. These outliers were as follows (femoral version difference, lesser trochanter profile difference): -6°, 2.4 mm; 8°, 6.9 mm; -4°, 3.4 mm; 5°, -4.2 mm; and -9°, 3.2 mm. Finally, a subgroup analysis of anteverted, normal, and retroverted femora was performed. An analysis of variance test was used to determine differences in the lesser trochanter profile based on femoral version. These groups were determined by the mean and SD of the entire cohort. Femora were considered anteverted if they had a version > 1 SD from the mean. Normal femora were determined to be within 1 SD of the mean. Finally, retroverted femora had versions < 1 SD from the mean. Significance was determined at a p value of < 0.05. All statistical analyses were performed using StatPlus 2 (AnalystSoft Inc, Walnut, CA, USA).
Results
Mean femoral rotation was noted to be 10.9° (SD ± 8.8°) across all femora. No difference was found in the mean femoral rotation between the right and left femora. Mean right femoral rotation was 11.0° (SD ± 8.9°) and mean left femoral rotation was 10.7° (SD ± 8.7°) with a mean difference of 0.3° (95% confidence interval [CI], -1.7° to 2.3°; p = 0.76) (Table 2). There was no difference in femoral rotation between the sexes; males had a mean rotation of 9.4° (SD ± 7.7°), and females had a mean rotation of 11.5° (SD ± 9.1°) (Table 2). The mean difference in rotation between sexes was 2.1° (95% CI, -0.1° to 4.3°; p = 0.06). The mean lesser trochanter profile was noted to be 6.6 mm (SD ± 4.0 mm) across all femora. No difference was found in the mean lesser trochanter profile between the right and left femora. The mean right lesser trochanter profile was 6.6 mm (SD ± 3.9 mm) and mean left lesser trochanter profile was 6.5 mm (SD ± 4.0 mm) with a mean difference of 0.1 mm (-0.8 to 1.0 mm, p = 0.86). The lesser trochanter profile varied between the sexes; males had a mean of 8.3 mm (SD ± 3.4), and females had a mean of 5.9 mm (SD ± 4.0) (Table 2). The mean difference between sexes was 2.5 mm (1.5-3.4 mm; p < 0.001).
Table 2.
Summary of radiographic measurements
The magnitude of the lesser trochanter profile measurement and degree of femoral rotation were positively correlated. Increasing measures of the lesser trochanter profile were associated with increasing amounts of femoral anteversion. Likewise, smaller measures of the lesser trochanter profile were associated with decreasing amounts of femoral anteversion (or more retroversion). For the entire cohort, the r2 value was 0.64 (p < 0.001) (Fig. 4). As such, 64% of the difference in femoral rotation can be explained by the difference in the lesser trochanter profile as noted on weightbearing radiographs. For males, the r2 value was 0.66 (p < 0.001). For females, the r2 value was 0.62 (p < 0.001).
Fig. 4.
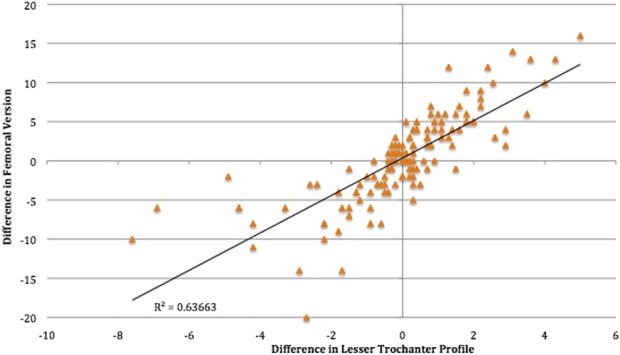
Linear regression demonstrates the correlation in difference in femoral version to the difference in lesser trochanter profile across the study cohort.
A subgroup analysis was completed to evaluate femoral rotation and lesser trochanter profile measurements in those patients 1 SD above and below the mean. We tested the association of femoral rotation to the lesser trochanter profile by comparing those patients with normal rotation with anteverted and retroverted patient groups. In the subgroup analysis, 56 femora (18%) were considered “anteverted” or > 1 SD from the mean rotation. Additionally, 203 (65%) femora were considered “normal” or within 1 SD of the mean rotation, and 51 (16%) femora were considered “retroverted” or < 1 SD from the mean rotation (Fig 5). Those hips that were considered normal had a mean lesser trochanter profile of 6.4 mm (SD ± 3.8), whereas those hips that were considered retroverted had a mean lesser trochanter profile of 4.9 mm (SD ± 3.9). When comparing normal rotation with those considered anteverted, there was a mean difference of 2.1 mm (0.9-3.3 mm, p < 0.001). When comparing normal rotation with those considered retroverted, there was a mean difference of 1.6 mm (0.3-2.8 mm, p = 0.006). The intraclass correlation coefficient was determined to be 0.94 for femoral version and 0.95 for lesser trochanter profile measurements. Both of these values are interpreted to mean excellent intraobserver reliability.
Fig. 5.
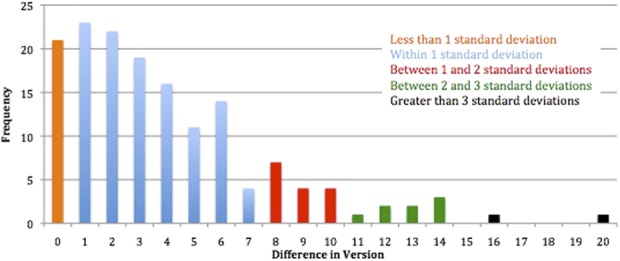
Total counts are noted as a distribution of femoral version differences across the study cohort.
Discussion
Restoration of femoral rotation after fracture has proven to be a difficult task and is done in a patient-specific manner with the goal of achieving an anatomic femur reconstruction. The fluoroscopic profile of the lesser trochanter is commonly used as a guide to the rotational alignment of the femur, but variations in proximal femoral anatomy may question the validity of this method. Our study measured the mean femoral rotation in a large cohort of adult, paired femora using modern methods of assessing femoral rotation (CT scanogram) and tested the correlation between CT scanogram measurements of femoral rotation and the lesser trochanter profile. The lesser trochanter profile was positively associated with femoral rotation. Importantly, the association of the lesser trochanter profile to femoral rotation did not change with greater differences in femoral rotation, and the lesser trochanter profile was associated with both anteverted and retroverted femoral rotation.
This study has several notable limitations. CT scanograms were obtained in patients with groin and hip pain without plain film radiographic evidence of arthrosis (Tönnis < 2) as an advanced three-dimensional evaluation of hip pathomorphology. Therefore, we can only conclude that the lesser trochanter profile is associated with femoral rotation in this patient population. The absence of arthrosis as a requisite criteria to obtain a CT scanogram in the inclusion patient population may bias the population to a younger age group and may not make these results generalizable to an arthritic population. To the authors’ knowledge, no study to date has suggested that hip arthritic change results in a morphologic change to femoral rotation or lesser trochanter anatomy. Having hip or groin pain as an indication for CT scanogram may preclude the generalizability of the current study data to the trauma population who may or may not have antecedent groin or hip pain. We compared supine CT scanograms with weightbearing AP pelvic radiographs and although the radiographs were obtained by the same three experienced radiology technicians, foot position and rotation of the lower extremities almost certainly varied among patients, which would have affected the lesser trochanter profile measurement. Although weightbearing and supine radiographs have been shown to affect pelvic and acetabular orientation, there should be very little effect on femoral orientation if foot position and lower extremity rotation are standardized [24]. Unfortunately, given the retrospective nature of the current study, there is no way to confirm that the rotational position of the lower extremities was the same during acquisition of the supine CT and weightbearing AP pelvis radiograph. Additionally, measuring the “magnitude” of the lesser trochanter has yet to be described, but the excellent intraobserver reliability noted in this study does provide support to the notion that these measurements can be reproducibly made. Prior studies [7, 15] have only referred to the general size of the lesser trochanter profile without providing any concrete measurement in this regard. Because a different amount of proximal femur was imaged with each weightbearing AP pelvis radiograph, it is difficult to standardize the vertical line extending along the medial cortex of the femur introducing some error to this measurement.
An additional limitation to consider is that the lesser trochanter profile on weightbearing AP pelvic radiographs may not directly extrapolate to the lesser trochanter profile in patients placed in the supine or lateral position during fracture fixation. One of the main challenges in the operating room is to obtain standardized fluoroscopic pictures of the hip and this challenge certainly remains. Moreover, standardized digital measurements of the lesser trochanteric profile are frequently not obtainable with many C-arm systems currently in use. Although the current study has demonstrated an association of the lesser trochanter profile and femoral rotation, the relationship between these two variables is not perfect and variation in leg rotation may exist even when the lesser trochanter profile is used to restore rotational anatomy after fracture fixation.
In our study, femoral rotation among skeletally mature patients without prior femur fracture or surgery was noted to be 10.9° of anteversion across all patients with a mean lesser trochanter profile of 6.6 mm. Several studies have attempted to evaluate and establish normal femoral rotation; however, these studies used methods for measuring rotation that cannot be implemented clinically. Kingsley and Olmsted [17] first reported on femoral rotation as measured with a protractor in 630 adult cadaveric femurs, including 45 paired femora. Mean femoral rotation was noted to be 8° of anteversion, slightly less than what was noted in the current study. Unfortunately, Kingsley and Olmsted [17] did not report the rotational difference between matched pairs, and the sex of the cadaveric specimen was not known but rather inferred from the size of the cadaver. More recently, Reikerås et al. [22] reported on the femoral rotation of 48 cadaveric femora pairs (24 males, 24 female pairs) as determined by the use of plain film radiography. Rotational measurements were made through the use of atypical radiographic projections and required the assistance of trigonometry to determine the overall femoral rotation. Similar to our study, Reikerås et al. [22] concluded that mean femoral anteversion was 10.4°. Other studies that have attempted to establish normal femoral rotation have used less reliable assessment methods such as ultrasound [1] or have measured femoral rotation only after fracture fixation [3, 5], thus making it difficult to determine the standard measurement. Despite these deficiencies, knowing mean femoral rotation is of paramount importance for surgeons treating femur fractures.
Our analysis revealed that the lesser trochanter profile was associated with femoral version in a linear regression model with an r2 value of 0.64 (p < 0.001) after removal of outliers. Although this association is not a perfect linear relationship, it does suggest that the lesser trochanter profile may be used as a means of determining and reestablishing femoral rotation during fracture fixation because 64% of femoral rotation can be ascribed to the lesser trochanter profile. Despite the current use of the lesser trochanter profile to aid in preventing femoral malrotation after traumatic reconstruction of the femur, only two previous studies have evaluated the efficacy of this technique. Desmukh et al. [7] initially popularized the lesser trochanter profile in a study comparing femoral malrotation after fracture fixation in two groups of five patients with unilateral femur fractures. Subsequent to this, Jaarsma et al. [15] tested the ability of five surgeons to detect malrotation using the lesser trochanter profile on 10 prepared cadaveric femora. Although both studies supported the use of the lesser trochanter profile for preventing femoral malrotation, the small numbers reported in each study limit the generalizability of their findings. Interestingly, there was no difference in rotation between male (9.4°) and female (11.5°) rotation in the current study, but the lesser trochanter profile was different between male (8.3 mm) and female (5.0 mm). The fact that males had a greater lesser trochanter profile is most likely attributed to the overall increased size in male femoral anatomy as compared with females.
Femoral rotation is clinically important and remains a key consideration when treating femur fractures because malrotation after fixation may often result [2, 19, 21, 23, 25, 28, 30, 31]. Techniques such as those described by Tornetta et al. [29], the neck horizontal angle [4], and the lesser trochanter profile [7, 15] have been established to help surgeons minimize malrotation after fixation of femur fractures. These techniques rely on the assumption that rotation is similar between injured and uninjured femora, highlighting the importance of our study that shows this to be true in most patients (Fig. 6). Among adults without femoral injury or bone deformity, average femoral rotation was 10.9° and did not differ between sides or sexes. The magnitude of the lesser trochanter profile measurement and degree of femoral rotation were positively correlated in the current study, meaning increasing measures of the lesser trochanter profile were associated with increasing amounts of femoral anteversion. This information may be used as an aid in restoring anatomic femoral rotation after fracture fixation because it substantiates prior work [7]. A perfect lateral of the distal femur and AP of the hip can be obtained on the uninjured femur. A perfect lateral of the distal femur is then obtained on the injured femur and the lesser trochanter profile is matched on the AP hip of the injured and uninjured femora. Although some variability in the rotation between sides may exist using this technique, the association of the lesser trochanter profile and femoral rotation noted in this study reinforces the utility of this approach. Future studies may seek to evaluate the utility of using the lesser trochanter profile as compared with other commonly used methods of restoring femoral rotation after fracture fixation such as the neck horizontal angle or true lateral techniques.
Fig. 6A-B.
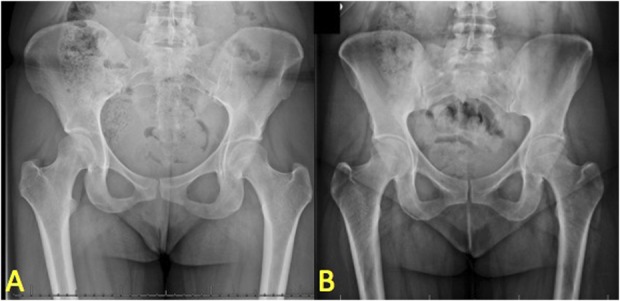
Examples demonstrate symmetric and asymmetric lesser trochanter profiles. (A) An asymmetric lesser trochanter profile correlates with the patient’s asymmetric CT scanogram rotational measurements. (B) A symmetric lesser trochanter profile correlates with the patient’s symmetric CT scanogram rotational measurements.
Acknowledgments
We thank Lindsay Kellam MS, for assistance with statistical analysis and review.
Footnotes
One of the authors certifies that he (TGM), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 2200 from Arthrex (Naples, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bråten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults. Ultrasound measurements in men and 50 women. Acta Orthop Scand. 1992;63:29–32. [DOI] [PubMed] [Google Scholar]
- 2.Bråten M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary nailing of femoral shaft fractures. Measurement of anteversion angles in 110 patients. J Bone Joint Surg Br. 1993;75:799–803. [DOI] [PubMed] [Google Scholar]
- 3.Bråten M, Terjesen T, Rossvoll I. Femoral shaft fractures treated by intramedullary nailing. A follow-up study focusing on problems related to the method. Injury. 1995;26:379–383. [DOI] [PubMed] [Google Scholar]
- 4.Bråten M, Tveit K, Junk S, Aamodt A, Anda S, Terjesen T. The role of fluoroscopy in avoiding rotational deformity of treated femoral shaft fractures: an anatomical and clinical study. Injury. 2000;31:311–315. [DOI] [PubMed] [Google Scholar]
- 5.Brouwer KJ, Molenaar JC, van Linge B. Rotational deformities after femoral shaft fractures in childhood. A retrospective study 27-32 years after the accident. Acta Orthop Scand. 1981;52:81–89. [DOI] [PubMed] [Google Scholar]
- 6.Buckley R, Mohanty K, Malish D. Lower limb malrotation following MIPO technique of distal femoral and proximal tibial fractures. Injury. 2011;42:194–199. [DOI] [PubMed] [Google Scholar]
- 7.Deshmukh RG, Lou KK, Neo CB, Yew KS, Rozman I, George J. A technique to obtain correct rotational alignment during closed locked intramedullary nailing of the femur. Injury. 1998;29:207–210. [DOI] [PubMed] [Google Scholar]
- 8.Espinoza C, Sathy AK, Moore DS, Starr AJ, Reinert CM. Use of inherent anteversion of an intramedullary nail to avoid malrotation in femur fractures. J Orthop Trauma. 2014;28:e34–38. [DOI] [PubMed] [Google Scholar]
- 9.Goldman MJ, Freeman LM. Computer tomography of neck, chest, spine, and limbs. In: Jeanmart L, Baert AL, Wackenheim A, eds. Atlas of Pathological Computer Tomography. Vol 3 Berlin, Germany: Springer-Verlag; 1984. [Google Scholar]
- 10.Gugenheim JJ, Probe RA, Brinker MR. The effects of femoral shaft malrotation on lower extremity anatomy. J Orthop Trauma. 2004;18:658–664. [DOI] [PubMed] [Google Scholar]
- 11.Hüfner T, Citak M, Suero EM, Miller B, Kendoff D, Krettek C, Citak M. Femoral malrotation after unreamed intramedullary nailing: an evaluation of influencing operative factors. J Orthop Trauma. 2011;25:224–227. [DOI] [PubMed] [Google Scholar]
- 12.Jaarsma RL, Ongkiehong BF, Grüneberg C, Verdonschot N, Duysens J, van Kampen A. Compensation for rotational malalignment after intramedullary nailing for femoral shaft fractures. An analysis by plantar pressure measurements during gait. Injury. 2004;35:1270–1278. [DOI] [PubMed] [Google Scholar]
- 13.Jaarsma RL, Pakvis DFM, Verdonschot N, Biert J, van Kampen A. Rotational malalignment after intramedullary nailing of femoral fractures. J Orthop Trauma. 2004;18:403–409. [DOI] [PubMed] [Google Scholar]
- 14.Jaarsma RL, van Kampen A. Rotational malalignment after fractures of the femur. J Bone Joint Surg Br. 2004;86:1100–1104. [DOI] [PubMed] [Google Scholar]
- 15.Jaarsma RL, Verdonschot N, van der Venne R, van Kampen A. Avoiding rotational malalignment after fractures of the femur by using the profile of the lesser trochanter: an in vitro study. Arch Orthop Trauma Surg. 2005;125:184–187. [DOI] [PubMed] [Google Scholar]
- 16.Kim JJ, Kim E, Kim KY. Predicting the rotationally neutral state of the femur by comparing the shape of the contralateral lesser trochanter. Orthopedics. 2001;24:1069–1070. [DOI] [PubMed] [Google Scholar]
- 17.Kingsley PC, Olmsted KL. A study to determine the angle of anteversion of the neck of the femur. J Bone Joint Surg Am. 1948;30:745–751. [PubMed] [Google Scholar]
- 18.Krettek C, Rudolf J, Schandelmaier P, Guy P, Könemann B, Tscherne H. Unreamed intramedullary nailing of femoral shaft fractures: operative technique and early clinical experience with the standard locking option. Injury. 1996;27:233–254. [DOI] [PubMed] [Google Scholar]
- 19.Langer JS, Gardner MJ, Ricci WM. The cortical step sign as a tool for assessing and correcting rotational deformity in femoral shaft fractures. J Orthop Trauma. 2010;24:82–88. [DOI] [PubMed] [Google Scholar]
- 20.Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994:69–74. [PubMed] [Google Scholar]
- 21.Lindsey JD, Krieg JC. Femoral malrotation following intramedullary nail fixation. J Am Acad Orthop Surg. 2011;19:17. [DOI] [PubMed] [Google Scholar]
- 22.Reikerås O, Høiseth A, Reigstad A, Fönstelien E. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand. 1982;53:775–779. [DOI] [PubMed] [Google Scholar]
- 23.Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R. Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:161–169. [DOI] [PubMed] [Google Scholar]
- 24.Ross JR, Tannenbaum EP, Nepple JJ, Kelly BT, Larson CM, Bedi A. Functional acetabular orientation varies between supine and standing radiographs: implications for treatment of femoroacetabular impingement. Clin Orthop Relat Res. 2015;473:1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salem KH, Maier D, Keppler P, Kinzl L, Gebhard F. Limb malalignment and functional outcome after antegrade versus retrograde intramedullary nailing in distal femoral fractures. J Trauma. 2006;61:375–381. [DOI] [PubMed] [Google Scholar]
- 26.Sathy A, Barnwell JC, Shahrestani SN, Moore D. Reliable method for avoiding malrotation deformity after intramedullary nailing of comminuted femur fractures: clinical validation of a previously described technique. J Orthop Trauma. 2017;31:e121–e126. [DOI] [PubMed] [Google Scholar]
- 27.Stahl J-P, Alt V, Kraus R, Hoerbelt R, Itoman M, Schnettler R. Derotation of post-traumatic femoral deformities by closed intramedullary sawing. Injury. 2006;37:145–151. [DOI] [PubMed] [Google Scholar]
- 28.Stephen DJG, Kreder HJ, Schemitsch EH, Conlan LB, Wild L, McKee MD. Femoral intramedullary nailing: comparison of fracture-table and manual traction. a prospective, randomized study. J Bone Joint Surg Am. 2002;84:1514–1521. [DOI] [PubMed] [Google Scholar]
- 29.Tornetta P, Ritz G, Kantor A. Femoral torsion after interlocked nailing of unstable femoral fractures. J Trauma. 1995;38:213–219. [DOI] [PubMed] [Google Scholar]
- 30.Winquist RA, Hansen ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–539. [PubMed] [Google Scholar]
- 31.Yang KH, Han DY, Jahng JS, Shin DE, Park JH. Prevention of malrotation deformity in femoral shaft fracture. J Orthop Trauma. 1998;12:558–562. [DOI] [PubMed] [Google Scholar]