History
The classification of thoracolumbar injuries remains controversial, and no clear consensus has been reached despite various classification systems being used during the past several decades [9]. Although Böhler [2] introduced his sentinel scheme in 1929, the first published thoracolumbar injury classification in the English literature was by Watson-Jones in 1938 [23] . He identified three distinct fracture types: the simple wedge fracture, the comminuted fracture, and the fracture dislocation [16, 23]. In 1949, Nicoll [11] further classified these injuries as anterior wedge fractures, lateral wedge fractures, and isolated neural arch fractures and characterized two basic groups of injury: stable and unstable fractures. He asserted that the fracture gap caused by the comminution of the vertebral body and injury of the posterior ligamentous complex (PLC) could induce instability [11]. In 1970, Holdsworth [5] defined a burst fracture as any vertebral body compression fracture that disrupted the posterior vertebral wall and proposed the first classification based on mechanism of injury. He recognized the importance of the traumatic forces causing distinct fracture patterns, described as flexion, flexion and rotation, extension, and compression. Holdsworth also conceptualized the anterior column as resisting compressive loads and the PLC resisting tensile forces acting as a tension band [5]. Kelly and Whitesides [8] formally presented the two-column concept in 1968, whereby the entire vertebral body and intervertebral disc were considered as the anterior column, and the posterior column comprised the neural arch and PLC.
With the development of CT spine imaging, Denis [4] proposed the three-column theory of spinal stability in 1983. He introduced the concept of the middle column between the PLC and the anterior longitudinal ligament. This middle column comprised the posterior wall of the vertebral body, the posterior longitudinal ligament, and posterior annulus fibrosus [4]. Denis further classified major spinal injuries into four different categories: compression, burst, seatbelt-type injuries, and fracture-dislocations. In 1994, Magerl et al. [10] divided fractures into three types based on major external forces placed on the vertebral body (compression, distraction, and rotation). They reported the AO classification using the 3-3-3 principle that divides thoracolumbar injury into a total of 53 fracture groups [10]. In the 3-3-3 classification system each type is further subdivided into three additional groups, and these groups are each separated yet again into three more subgroups with specifications, or even further as required.
In 2005, Vaccaro et al. [21] introduced the Thoracolumbar Injury Severity Score (TLISS), a scoring system that focused on injury mechanism rather than morphologic features and is the predecessor of the Thoracolumbar Injury Classification and Severity Score (TLICS). The TLISS was based on three major injury components: the mechanism of injury, the integrity of the PLC, and the patient’s neurologic status [21]. This was the first classification to include the neurologic status of the patient. Poor reproducibility with respect to injury mechanism led to modification of the TLISS scoring system and resulted in a transition to the TLICS, in which the fracture mechanism was replaced by the morphologic injury description [3]. This modification removes the subjective determination of the dynamic injury mechanism that is often difficult to interpret on static posttraumatic images and that is largely based on subjective criteria, and incorporates more-objective findings from imaging studies for facilitating accurate diagnosis of these fracture patterns [17].
Purpose
The thoracolumbar spine is the most-common site of spinal fractures, accounting for more than half of all spinal injuries [22]. Most patients are young men involved in high-energy accidents, such as traffic accidents, followed by falls from greater than 6 feet, and low-energy falls [25]. These injuries can result in severe functional disability, deformity, and neurologic deficits. Classifying these injuries is important to guide treatment, provide prognosis, facilitate communication among treating physicians, and advance clinical research. A working classification scheme of thoracolumbar spine fractures should be comprehensive, easy to apply, widely recognized, reproducible, and prognostic with the ability to provide information regarding injury severity and to guide treatment strategy.
Description
The TLICS system was created to address the shortcomings of previous thoracolumbar trauma classifications, including issues with respect to the validity and reproducibility of those systems. Three principal injury characteristics were identified as crucial to guide clinical management and to determine the treatment algorithm in thoracolumbar trauma: (1) the fracture pattern or morphologic features of the injury; (2) integrity of the PLC; and (3) the neurologic status. Injuries are analyzed and point values are assigned to subgroups in each category to determine an injury score from 1 to 4 points (1 = least severe to 4 = most severe). The composite Injury Severity Score is calculated by summation of the individual scores and can be used to guide conservative or surgical treatment. Fractures with 3 points or less are considered for nonoperative management. Fractures with scores of 4 points can be considered either for nonoperative or surgical intervention. Fractures graded as 5 or higher often benefit from surgery, provided the patient is medically fit for the intervention [20] (Table 1).
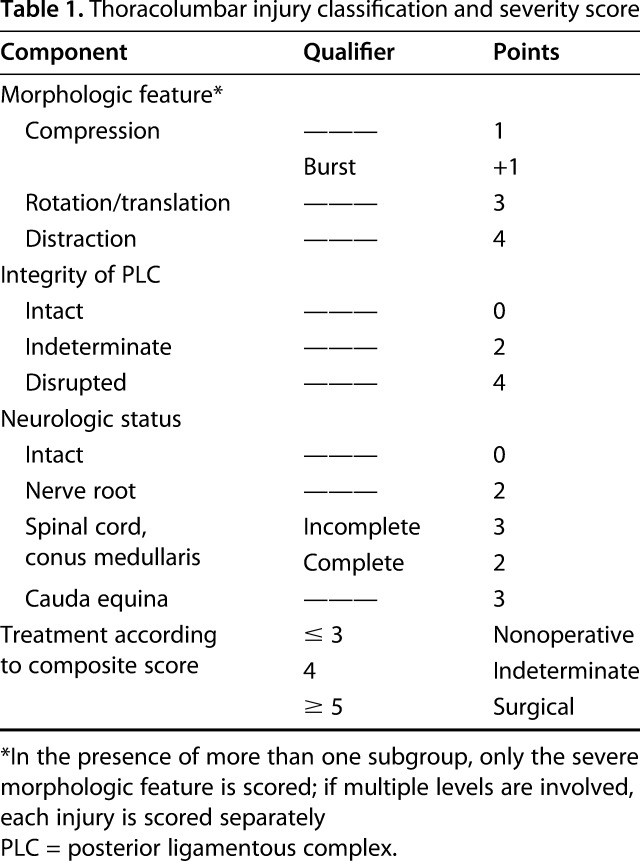
Table 1.
Thoracolumbar injury classification and severity score
Morphologic Features: Fracture Pattern
Fracture pattern can be summarized by one of three morphologic descriptors: (1) compression; (2) translation/rotation; and (3) distraction [20]. These are determined by a combination of plain films, CT, and MRI. The spinal level involvement should be included in the description. In a compression fracture, the vertebral body fails under axial loading. It can be represented by a simple compression fracture with buckling of the anterior wall of the vertebrae and accentuated with kyphosis [20] or, in its more severe form, as a burst fracture. Torsional and shear forces primarily are responsible for translation/rotational injuries. These injuries are characterized by horizontal separation of the spinous processes, altered alignment of the pedicles above and below the level of the injury, pars fracture, and facet fracture-dislocation. Finally, in the distraction morphologic features, the rostral spinal column becomes separated from the caudal segment owing to distraction forces, with an anatomic dissociation in the vertical axis. These often are very unstable injuries because, by definition, the spinal column is circumferentially disrupted.
Integrity of the PLC
The PLC serves as the posterior “tension band” of the spinal column and plays an important role in stability of the spine. The PLC is composed of the supraspinous ligament, interspinous ligament, ligamentum flavum, and the facet joint capsules. Once disrupted, this ligamentous complex generally benefits from surgical intervention since this can lead to progressive kyphosis and collapse owing to its poor healing ability [20]. Integrity of the PLC is classified as intact, indeterminate, or disrupted. Disruption is indicated by widening of the interspinous space, diastasis of the facet joints, avulsion fractures or transverse fracture of spinous processes or articular facet, and facet perch or subluxation and dislocation of the spine [20]. When the evidence of disruption is subtle, the integrity of the ligament is labeled indeterminate.
Neurologic Status
Evaluation of neurologic status is vital for clinical decision-making in thoracolumbar injuries. Acute neurologic deficits are sensitive indicators of the severity of the spinal column trauma. The neurologic function is described as: neurologically intact, nerve root injury, complete (motor and sensory) spinal cord injury, and incomplete (motor or sensory) spinal cord or cauda equina injury [20]. Treatment is based on maximizing neurologic recovery and preventing neurologic decline.
Case Examples
Case examples of TLICS stable, questionable TLICS, and TLICS unstable observed on CT imaging show the scoring process.
A patient was involved in a motor vehicle accident and sustained a compression fracture (1 point). The patient had a stable and intact PLC (0 points), and an intact neurologic examination (0 points). A clearly stable thoracolumbar fracture was observed on the CT images (Fig. 1), thus the patient had a TLICS score of 1 and was treated with bracing.
Fig. 1.
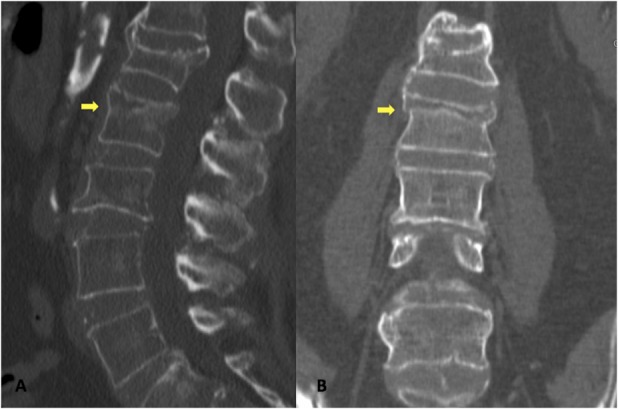
A-B (A) Sagittal and (B) coronal view CT scans show an acute L2 compression fracture (arrows) with previously healed L1 and L3 fractures.
CT images from another patient involved in a motor vehicle accident showed a burst fracture (2 points: 1 point for the compression fracture and +1 point for the burst modifier) with retropulsion, indeterminate but suspected PLC involvement (2 points). The patient had an intact neurologic examination (0 points). This patient had a TLICS score of 4 (Fig. 2); which is considered questionable or indeterminate. The patient was treated surgically with L2-L4 percutaneous instrumentation owing to concerns of instability, as the fracture might extend into the pedicle and facet.
Fig. 2.
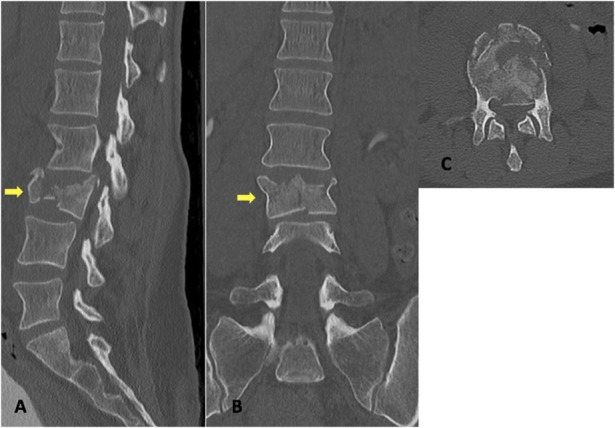
A-C (A) Sagittal, (B) coronal, and (C) axial view CT scans show an acute L3 burst fracture (arrows in Illustrations A and B) with retropulsion. There is loss of vertebral body height seen on the sagittal view with moderate narrowing of the spinal canal attributable to posterior fragment retropulsion as seen on the axial view.
In the third patient, CT images showed a burst fracture (2 points: 1 point for the compression fracture and +1 point for the burst modifier) with evidence of an injured PLC (the spinous process fracture and articular facet fracture are not shown) (3 points). Physical examination was concerning for an incomplete cord injury (American Spinal Injury Association Classification B) owing to decreased sensation, motor strength, absent rectal tone, and neurogenic bowel and bladder signs (3 points). This patient was clearly unstable with a TLICS score of 8 (Fig. 3). The patient was treated operatively with an L1 corpectomy with T12 to L2 fusion using a cage with autologous bone with anterior screw fixation from T12 to L2.
Fig. 3.
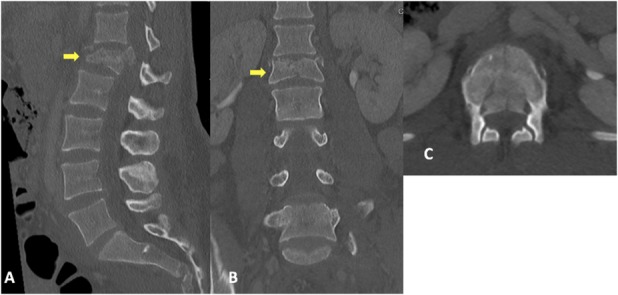
A-C (A) Sagittal, (B) coronal, and (C) axial view CT scans show an acute L1 burst fracture (arrows in Illustrations A and B) with retropulsion. There is loss of vertebral body height seen on the sagittal and coronal views with fragment retropulsion evident on the axial view.
Validation
The fundamental intent of the TLICS is to improve management of thoracolumbar injuries through a reproducible classification system that is easy to learn and is clinically applicable [12]. Intraobserver and interobserver reliability therefore are very important. The available research suggests that the reliability of the system is high, and initial studies showed good reliability and variability in terms of injury classification and treatment plans, although some of the studies were written by the developers of the TLICS system [6, 13, 14, 18]. Whang et al. [24] reported that the interrater kappa statistics of all subgroups (morphology, PLC, total score, predicted management) were within the range of moderate to substantial reproducibility (0.45-0.74); that study involved fellowship-trained spine surgeons, spine fellows, and senior and junior orthopaedic residents. Joaquim et al. [7] and Vaccaro et al. [18] reported that the retrospectively assigned TLICS, which would lead to a recommendation for surgical treatment (a TLICS score of 4 or higher), accurately matched the clinical decision of the surgeon to proceed with surgery in 47 of 49 patients (96%). In another study, Joaquim et al. [6] retrospectively evaluated the validity of TLICS in 458 patients treated over a decade at a tertiary medical center and reported the TLICS score they assigned (TLICS ≤ 4) accurately matched the nonsurgical treatment provided in 99% of the patients. However, in the group of patients who underwent surgery, 46.6% matched the TLICS score recommendation and 53.4% underwent surgical intervention for stable burst fractures (TLICS = 2). A study from North America and western Europe by Raja Rampersaud et al. [14] showed consistency of recommendations between fellowship-trained orthopaedic and neurosurgical spine surgeons, all of whom were academic members of an international spine trauma study group. The between-specialty interrater reliability of the management recommendation was moderate (74% agreement, kappa = 0.532) with orthopaedic surgeons and neurosurgeons agreeing with the management recommendation 91.4% and 94.4% of the time, respectively.
In a similar study at a Korean academic institution, Koh et al. [9] evaluated intrarater and interrater statistics of the TLICS in a series of 114 patients evaluated by two spine surgeons and one senior orthopaedic surgery resident. They reported intrarater kappa coefficients of 0.75, 0.81, 0.96, and 0.72 and interrater kappa coefficients of 0.60, 0.64, 0.91, and 0.57 for morphology, PLC involvement, neurologic status, and total severity score, respectively [9]. Furthermore, the TLICS also has been validated in the pediatric population. Savage et al. [15] reported moderate to substantial interrater and intrarater reliability for all categories and composite score (κ = 0.74-1.0 and κ = 0.52-0.95, respectively). Their study involved 20 spine surgeons in an academic setting with differing levels of experience, including 12 attending spine surgeons, four spine fellows, and four orthopaedic surgery residents. They reported acceptable indices for validity with 0.84 sensitivity, 0.78 specificity, 0.68 positive predictive value, and 0.90 negative predictive value. The differences in kappa values may be explained by geographic variation in surgical treatment decisions in the patient population with trauma, and the level of training and experience of the evaluators [1].
Limitations
There are exceptions to every rule and algorithm, and the TLICS is no different. The complete patient picture needs to be taken into account. Clinical situations and individual patient factors may supersede the TLICS score, regardless of where the score falls with respect to the surgical threshold. Vaccaro et al. [21] described various scenarios that might influence surgical management such as kyphosis or vertebral collapse, open fractures, and the inability to brace. Other issues such as multisystem trauma, limb amputation, rheumatoid arthritis, ankylosing spondylitis, general bone health, and overall health also may affect the decision to operate.
There have been concerns with application of the TLICS to burst fractures [6]. Joaquim et al. [6] described an L1 fracture with morphologic features of a compression and burst fracture injury (1 and 1 points), an intact PLC (0 points), and an intact neurologic status (0 points). At a TLICS of 2, the patient was below the operative threshold. There was 20% loss of height with kyphotic angulation of 19°. Nonoperative care with a thoracolumbar brace was instituted. At 1 month followup, pain was improved and radiographs showed a minimal increase of kyphosis to 21° with no major loss of height. Bracing was to be continued with followup radiographs in 3 months, but the patient was lost to followup for 1 year. The patient returned with worsening kyphotic deformity and bony fragment protrusion into the spinal canal, prompting surgical fixation at that time [23]. In certain unique situations, the surgeon’s preference and clinical judgment may overrule the TLICS algorithm; one group reported operating on a patient with a burst fracture without PLC injury or neurologic symptoms who had a TLICS of 2, yet there was bony retropulsion compromising 50% of the canal diameter [1]. A randomized trial from 2015 with a mean 18-year followup concluded that nonoperative treatment is the preferred management for TL burst fractures without neurologic deficit [26] .
However, considerable debate still exists with respect to the treatment of burst fractures. A randomized controlled trial found that patients treated surgically for thoracolumbar burst fractures without neurologic deficits had more complications compared with the nonoperative braced group [22]. There were no statistical differences in that study with pain or return to work issues between the braced and surgically treated groups. In contrast, a multicenter randomized study found those who underwent surgery for thoracolumbar burst fractures without neurologic deficits had significant increases in functional scores compared with the bracing group [19].
Another limitation of the classification may be related to imaging. A Swiss study used MR images combined with CT for the TLICS scoring system [27]. When compared with CT alone, the TLICS value changed from below to above the surgical threshold in 24% of 100 cases. With better observation of the PLC, the integrity of the PLC was felt to be intact in 80% with CT alone, whereas it was noted to be intact in only 55% when MRI was added [27].
Conclusions
The TLICS classification system provides an important treatment algorithm and has been shown to be reproducible with good reliability by the original authors and other groups. It is comprehensive and easy to apply in the clinical setting. It is the first system for thoracolumbar injuries to describe neurologic status in addition to morphologic features of fractures and PLC integrity. Because there are clinical concerns beyond those three metrics, including progression to late neurologic impairment, kyphosis, and issues of acute fracture comminution and canal involvement in the patient who is neurologically intact and whose TLICS score suggests nonoperative management, the algorithm is not a substitute for surgical experience and sound clinical judgment. The TLICS provides a rational guide for surgical decision-making; however, this decision must be individualized to each patient with a view toward the potential benefits, risks, and complications of all available treatment options.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Kentucky, Lexington, KY, USA.
References
- 1.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382:1121–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohler L. Mechanism of fracture and dislocation of the spine. The Treatment of Fractures. New York, NY: Grune and Stratton; 1956:300–329. [Google Scholar]
- 3.Chhabra HS, Kaul R, Kanagaraju V. Do we have an ideal classification system for thoracolumbar and subaxial cervical spine injuries: what is the expert's perspective? Spinal Cord. 2015;53:42–48. [DOI] [PubMed] [Google Scholar]
- 4.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817–831. [DOI] [PubMed] [Google Scholar]
- 5.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534–1551. [PubMed] [Google Scholar]
- 6.Joaquim AF, Daubs MD, Lawrence BD, Brodke DS, Cendes F, Tedeschi H, Patel AA. Retrospective evaluation of the validity of the Thoracolumbar Injury Classification System in 458 consecutively treated patients. Spine J. 2013;13:1760–1765. [DOI] [PubMed] [Google Scholar]
- 7.Joaquim AF, Fernandes YB, Cavalcante RA, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Phila Pa 1976). 2011;36:33–36. [DOI] [PubMed] [Google Scholar]
- 8.Kelly RP, Whitesides TE., Jr Treatment of lumbodorsal fracture-dislocations. Ann Surg. 1968;167:705–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koh YD, Kim DJ, Koh YW. Reliability and validity of Thoracolumbar Injury Classification and Severity Score (TLICS). Asian Spine J. 2010;4:109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. [DOI] [PubMed] [Google Scholar]
- 11.Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949;31:376–394. [PubMed] [Google Scholar]
- 12.Patel AA, Vaccaro AR. Thoracolumbar spine trauma classification. J Am Acad Orthop Surg. 2010;18:63–71. [DOI] [PubMed] [Google Scholar]
- 13.Patel AA, Vaccaro AR, Albert TJ, Hilibrand AS, Harrop JS, Anderson DG, Sharan A, Whang PG, Poelstra KA, Arnold P, Dimar J, Madrazo I, Hegde S. The adoption of a new classification system: time-dependent variation in interobserver reliability of the thoracolumbar injury severity score classification system. Spine (Phila Pa 1976). 2007;32:E105–110. [DOI] [PubMed] [Google Scholar]
- 14.Raja Rampersaud Y, Fisher C, Wilsey J, Arnold P, Anand N, Bono CM, Dailey AT, Dvorak M, Fehlings MG, Harrop JS, Oner FC, Vaccaro AR. Agreement between orthopedic surgeons and neurosurgeons regarding a new algorithm for the treatment of thoracolumbar injuries: a multicenter reliability study. J Spinal Disord Tech. 2006;19:477–482. [DOI] [PubMed] [Google Scholar]
- 15.Savage JW, Moore TA, Arnold PM, Thakur N, Hsu WK, Patel AA, McCarthy K, Schroeder GD, Vaccaro AR, Dimar JR, Anderson PA. The reliability and validity of the Thoracolumbar Injury Classification System in pediatric spine trauma. Spine (Phila Pa 1976). 2015;40:E1014–1018. [DOI] [PubMed] [Google Scholar]
- 16.Schroeder GD, Harrop JS, Vaccaro AR. Thoracolumbar trauma classification. Neurosurg Clin N Am. 2017;28:23–29. [DOI] [PubMed] [Google Scholar]
- 17.Schweitzer KM, Jr, Vaccaro AR, Lee JY, Grauer JN; Spine Trauma Study Group. Confusion regarding mechanisms of injury in the setting of thoracolumbar spinal trauma: a survey of The Spine Trauma Study Group (STSG). J Spinal Disord Tech. 2006;19:528–530. [DOI] [PubMed] [Google Scholar]
- 18.Vaccaro AR, Baron EM, Sanfilippo J, Jacoby S, Steuve J, Grossman E, DiPaola M, Ranier P, Austin L, Ropiak R, Ciminello M, Okafor C, Eichenbaum M, Rapuri V, Smith E, Orozco F, Ugolini P, Fletcher M, Minnich J, Goldberg G, Wilsey J, Lee JY, Lim MR, Burns A, Marino R, DiPaola C, Zeiller L, Zeiler SC, Harrop J, Anderson DG, Albert TJ, Hilibrand AS. Reliability of a novel classification system for thoracolumbar injuries: the Thoracolumbar Injury Severity Score. Spine (Phila Pa 1976). 2006;31(11 suppl):S62–69; discussion S104. [DOI] [PubMed] [Google Scholar]
- 19.Vaccaro AR, Lee JY, Schweitzer KM, Jr, Lim MR, Baron EM, Oner FC, Hulbert RJ, Hedlund R, Fehlings MG, Arnold P, Harrop J, Bono CM, Anderson PA, Anderson DG, Harris MB; Spine Trauma Study Group. Assessment of injury to the posterior ligamentous complex in thoracolumbar spine trauma. Spine J. 2006;6:524–528. [DOI] [PubMed] [Google Scholar]
- 20.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30:2325–2333. [DOI] [PubMed] [Google Scholar]
- 21.Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Lehman RA, Jr, Anderson DG, Bono CM, Kuklo T, Oner FC. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209–215. [PubMed] [Google Scholar]
- 22.Wang H, Zhang Y, Xiang Q, Wang X, Li C, Xiong H, Zhou Y. Epidemiology of traumatic spinal fractures: experience from medical university-affiliated hospitals in Chongqing, China, 2001-2010. J Neurosurg Spine. 2012;17:459–468. [DOI] [PubMed] [Google Scholar]
- 23.Watson-Jones R. The results of postural reduction of fractures of the spine. J Bone Joint Surg Am 1938;20:567–586. [Google Scholar]
- 24.Whang PG, Vaccaro AR, Poelstra KA, Patel AA, Anderson DG, Albert TJ, Hilibrand AS, Harrop JS, Sharan AD, Ratliff JK, Hurlbert RJ, Anderson P, Aarabi B, Sekhon LH, Gahr R, Carrino JA. The influence of fracture mechanism and morphology on the reliability and validity of two novel thoracolumbar injury classification systems. Spine (Phila Pa 1976).2007;32:791–795. [DOI] [PubMed] [Google Scholar]
- 25.Williams SK. Thoracic and lumbar spinal injuries. In: Herkowitz H, Garfin S, Eismont F, Bell G, Balderston R. Rothman-Simeone The Spine. 6th Ed. Philadelphia, PA: Elsevier Saunders; 2011:1363–1389. [Google Scholar]
- 26.Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, Bono CM, Harris MB. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Joint Surg Am. 2015;97:3–9. [DOI] [PubMed] [Google Scholar]
- 27.Wu HT, Morrison WB, Schweitzer ME. Edematous Schmorl's nodes on thoracolumbar MR imaging: characteristic patterns and changes over time. Skeletal Radiol. 2006;35:212–219. [DOI] [PubMed] [Google Scholar]


