Abstract
Background:
Chemical, physical and psychological stressors due to the 2010 Deepwater Horizon oil spill may impact coronary heart disease (CHD) among exposed populations. Using longitudinal information from two interviews in the Gulf Long Term Follow-up (GuLF) STUDY, we assessed CHD among oil spill workers and community members.
Objective:
To assess the associations between duration of oil spill clean-up work, residential proximity to the oil spill, and incidence of self-reported myocardial infarction or fatal CHD.
Methods:
Among respondents with two GuLF STUDY interviews (n=21,256), there were 395 first incident heart disease events (self-reported myocardial infarction or fatal CHD) across 5 years. We estimated hazard ratios (HR) and 95% confidence intervals (95%CI) for associations with duration of oil spill clean-up work and residential proximity to the oil spill. To assess potential impacts of non-response, we compared covariate distributions for those who did (n=21,256) and did not (n=10,353) complete the second interview and used inverse probability (IP) of censoring weights to correct for potential non-response bias.
Results:
Living in proximity to the oil spill (vs. living further away) was associated with heart disease, with [HR(95%CI)=1.30(1.01–1.67)] and without [1.29(1.00–1.65)] censoring weights. For work duration, hazard of heart disease appeared to be higher for those who worked >180 days (vs. 1–30 days), with and without censoring weights [1.43(0.91–2.25) and 1.36(0.88–2.11), respectively]. Associations persisted throughout the 5-year follow-up.
Conclusions:
Residential proximity to the spill and duration of clean-up work were associated with a suggested 29–43% higher hazard of heart disease events. Associations were robust to censoring.
Keywords: Deepwater Horizon, petroleum pollution, coronary disease, myocardial infarction, occupational exposure
1. Introduction
The 2010 Deepwater Horizon oil disaster was the largest marine oil spill in history. The spill began April 20th, 2010 when the Deepwater Horizon drilling rig exploded and sunk. Over 200 million gallons of crude oil were released into the Gulf of Mexico in the following months. The oil spill response and clean-up, which involved more than 100,000 workers, began at the start of the oil spill and continued through the end of 2010 (Kwok et al. 2017a).
During the oil spill response and clean-up, workers may have faced physical stress as well as chemical exposures from hydrocarbons volatilizing from fresh oil, combustion products from burning crude oil and flaring of natural gas, emissions from the equipment and machinery used during the clean-up, and chemical dispersants (Kwok et al. 2017a; Middlebrook et al. 2012; Stewart et al. 2018). Exposures to some of these pollutants, including particulate matter and volatile organic chemicals, have shown associations with risk of coronary heart disease (CHD) in environmental and occupational exposure studies (Bahadar et al. 2014; Brook et al. 2010; Peters 2005; Stewart et al. 2018). Airborne particulate levels during the oil spill were elevated in coastal communities and around clean-up sites compared to typical ambient levels in these regions (Nance et al. 2016).
Apart from chemical exposures related to the spill, Gulf Coast communities faced economic burdens and increases in psychosocial stress in the wake of the oil spill (Gould et al. 2015; Peres et al. 2016). Local industries including fishing and tourism were disrupted for months following the spill (Shultz et al. 2015), and loss of income may have contributed to psychosocial stress in these communities. Psychosocial stress can impact risk of cardiovascular diseases by accelerating progression of atherosclerotic plaques (Rozanski et al. 1999). Thus, the physical and emotional stress caused by the oil spill may have contributed to an increased risk of CHD.
It is unknown whether exposures to pollutants or physical stressors during the oil spill may affect risk of heart disease over time. Short-term increases in ambient particulate matter concentrations increase risk of cardiovascular events and overall mortality acutely, but the persistence of these associations remains unexplored (Brook and Rajagopalan 2010; Brook et al. 2010). A study of the Prestige oil spill found that respiratory symptoms among clean-up workers persisted up to 5 years after the spill (Zock et al. 2012). Studies of Hebei Spirit oil spill workers (Gwack et al. 2012) and United States Coast Guard deployed to work on the Deepwater Horizon spill (Alexander et al. 2018) have shown that longer durations of oil spill work were associated with increased respiratory symptoms. Despite the reported associations between oil spill work and persistent respiratory effects, no research has assessed incidence of cardiovascular diseases or other chronic health outcomes among oil-exposed populations.
The Gulf Long Term Follow-up (GuLF) STUDY is the largest study of the health impact of oil spills (Kwok et al. 2017a) and is the first study to assess heart disease among individuals exposed to oil spills. We have used longitudinal information from the GuLF STUDY to assess associations between duration of clean-up work, living in proximity to the oil spill, and self-reported myocardial infarction and fatal coronary heart disease up to 5 years after the oil spill. We also assessed predictors of non-response to the GuLF STUDY second interview and accounted for this attrition in our analyses.
2. Methods
2.1. Study population
The GuLF STUDY is a prospective cohort study of individuals who worked on, or had trained to work on, clean-up of the 2010 Deepwater Horizon oil spill (Kwok et al. 2017a). Participants in the study include individuals aged ≥21 years who completed mandatory oil spill safety training in order to take part in the oil spill response and clean-up as well as government workers and oil industry professionals who were living in the United States at the time of enrollment.
Recruitment began approximately 11 months after the start of the oil spill, in March 2011, and continued until May 2013. From a list of 62,803 presumably unique names with sufficient contact information, a total of 32,608 participants were enrolled and completed the first study interview. Of the enrolled participants, we excluded from the present analyses 999 individuals who completed a Vietnamese language abbreviated version of the questionnaire that did not collect complete information on oil spill clean-up jobs. Of the 31,609 participants who enrolled in the study and completed the full interview, 21,256 (67%) completed a second telephone interview in 2014–2016, two to three years after their first interview.
2.2. Exposure and outcome measures
All oil spill-related exposures and clean-up tasks were assessed during the first interview. Health outcomes were assessed during the first and second interviews. The exposures of interest in this report are duration of participation in oil spill clean-up work and home residence in an area proximal to the oil spill. Dates of initiating and ending clean-up work were self-reported by participants, as was their county or parish of residence at the time of enrollment. Work duration was defined categorically, based on the distribution of duration of oil spill work, as 1–30 days, 31–90 days, 91–180 days and >180 days. Analyses of work duration included clean-up workers only, whereas analyses of residential proximity to the oil spill included both workers and nonworkers. Residential proximity to the oil spill was defined as “direct or indirect” for participants living in or adjacent to a county that had coastline oiled from the spill and “away from the spill” for participants living elsewhere in the Gulf region or in another part of the US. We grouped coastal and adjacent counties because these areas were likely to have been similarly impacted by loss of income and community stress due to the oil spill, and living in or adjacent to a county affected by the oil spill was associated with mental health symptoms following the spill (Kwok et al. 2017b).
The outcome of interest is the incident occurrence of a first heart disease event, defined as a self-reported myocardial infarction (MI), or a fatal CHD event ascertained from death certificates. During the first and second interviews, participants were asked if they had ever received a diagnosis of a heart attack or MI and, if so, the month and year of their first MI diagnosis. Participants who reported an MI occurring before clean-up work (n=610) were excluded from the analyses.
Deaths due to CHD were ascertained from the National Death Index (NDI) for the entire enrolled cohort through December 31st, 2014, the latest date for which complete NDI data were available. International Classification of Diseases, 10th Edition (ICD-10) codes indicating ischemic heart disease as a cause of death (I20-I25) were counted as fatal CHD cases.
2.3. Risk period for heart disease events
The time at risk for a heart disease event was based on calendar time and was determined differently for analyses including all study participants and for analyses among clean-up workers only. For analyses of residential proximity to the spill and heart disease, participants were at risk for a self-reported first MI from the date that the oil spill began (April 20th, 2010); for analyses of work duration and heart disease, the risk period began at initiation of oil spill clean-up work, which was between April and July 2010 for most participants. For all analyses, the risk period for a self-reported MI ended at the earlier of the date of diagnosis of a first MI or the last GuLF STUDY interview that the participant completed. The risk period for a fatal CHD event began at the time of the enrollment interview, as participants had to be living to enroll in the study, and continued until December 31st, 2014. Only a participant’s first reported MI diagnosis or CHD event was counted in this study.
2.4. Statistical methods
2.4.1. Censoring and predictors of loss to follow-up
Nonfatal MIs were censored if a participant who was at risk for a first MI, i.e. did not report an MI at the first interview, did not complete the second interview. We compared distributions of a broad range of factors plausibly related to the outcome and non-response, between those who did and did not complete the second interview. The factors that we assessed, determined by literature review and dependent on availability of data, included demographic (age; gender; ethnicity), lifestyle (cigarette smoking; alcohol consumption) and socioeconomic (income; education; employment status) covariates, as well as factors related to health at enrollment (prevalent myocardial infarction; prevalent hypertension; perceived health), and oil spill clean-up work characteristics (working on clean-up; duration of clean-up work; clean-up job type; exposure to burning oil; exposure to total hydrocarbons; and residential proximity to the oil spill.) We compared crude proportions of censoring across levels of each predictor variable. The magnitude and precision of these estimates were considered in order to assess the ability of each variable to predict non-response.
To describe the major predictors of non-response in our study, we fit a logistic regression model combined with a Least Absolute Shrinkage and Selection Operator (LASSO) approach (Tibshirani 1996). Briefly, LASSO is a penalized regression method that is often used for variable selection. The level of penalization was selected using Akaike’s Information Criterion (AIC) (Akaike 1992) using the SAS procedure HPGENSELECT (Yuan and Lin 2006). We began with a full model that included the following covariates: gender (male; female), age (20–29, 30–39, 40–49, 50–59, 60–64, ≥65 years), ethnicity (white; black; Asian; other/multi-racial), income (≤$20,000; $20,001-$50,000; >$50,000), highest education attainment (less than high school; high school diploma/GED; some college/2-year degree; 4+ year college graduate), current alcohol intake (yes; no), cigarette smoking (current; former; never), heavy cigarette smoking (currently smokes ≥1 pack per day; smokes <1 pack per day or non-smoker), self-reported physician diagnosis of hypertension (yes; no), residential proximity to the oil spill (direct/indirect; away from the spill), maximum total hydrocarbon exposure during clean-up work (<0.30 ppm; 0.30–0.99 ppm; 1.00–2.99 ppm; >3.00 ppm), duration of clean-up work (1–30 days; 31–90 days; 91–180 days; >180 days), employment status at the time of enrollment (working; temporarily laid off, sick leave or maternity leave; looking for work or unemployed; retired; disabled; keeping house; student; other), previous work on clean-up of another oil spill (yes; no), and ever being enlisted in the military (yes, now on active duty; yes, on active duty during the last 12 months, but not now; yes, on active duty in the past, but not during the last 12 months; no, training for Reserves or National Guard only; no, never served in the military). We then fit a logistic regression model with non-response as the dependent variable, conditional on the variables selected by the LASSO procedure. We used this logistic model to estimate the concordance statistic, which quantifies the predictive accuracy of the model (Austin and Steyerberg 2012).
2.4.2. Estimating hazard ratios
We assessed the associations between work duration, residential proximity to the oil spill and heart disease in a time-to-event analysis (Cox 1992). We used inverse probability (IP) of censoring weights to weight the population that completed the second interview with respect to predictors of censoring, in order to estimate associations that would be observed in the absence of censoring (Cole and Hernan 2008). Each individuals’ probability of censoring for the IP weights was estimated using a logistic model with censoring as the dependent variable and predictors of censoring as the independent variables. We used a causal diagram (Greenland et al. 1999) to determine the minimally sufficient set of predictors to be included in the IP censoring weights model (Howe et al. 2016): age, education, residential proximity to the oil spill, duration of clean-up work, smoking, and maximum total hydrocarbon exposure during clean-up work (which was determined from a job exposure matrix described by Stewart and colleagues (Stewart et al. 2018)). The probabilities output from the weights model served as the basis for the denominator for the IP censoring weights, and for stabilized weights, the numerator was the probability of being observed at follow-up (Cole and Hernan 2008).
We controlled for confounders using two separate methods: (1) by conditioning on the covariates in the regression model; and (2) by applying IP exposure weights. An adjustment set of confounders was determined using a directed acyclic graph (DAG) (Greenland et al. 1999). For the analyses of work duration and heart disease, we adjusted for: gender (male; female), age (20–29; 30–39; 40–49; 50–59; 60–64; ≥65 years), maximum education attainment (less than high school; high school diploma/GED; some college/2-year degree; 4+ year college graduate), residential proximity to the oil spill (direct/indirect; away from the spill) and cigarette smoking (current; former; never). For the residential proximity to the spill analyses, we adjusted for gender, age, smoking, and maximum education attainment. We were unable to control for finer categories of smoking because of a substantial amount of missing data for pack-years of smoking among former smokers. Body mass index and self-reported prevalent hypertension were determined to not be confounders, and we did not adjust for these in any of the models; in addition, adjusting for these variables did not meaningfully change results (<10% change in beta estimates).
The IP exposure weights were obtained by fitting a logistic regression model (for the categorical work duration variable, we used a multinomial logistic regression model) for the exposure with confounders as independent variables. We used stabilized weights, where the numerator was the probability of exposure, and the denominator was the probability output from the model (Cole and Hernan 2008).
Cox proportional hazards models (Cox 1992) with a robust variance estimator were fit to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) (Williamson et al. 2014). We assessed whether each covariate met the proportional hazards assumption by modeling an interaction term between the natural log of time and each covariate in the model. We fit Cox models conditional on confounders, with and without IP censoring weights, as well as marginal Cox models, which controlled for confounders using IP exposure weights, with and without IP censoring weights.
To account for the fact that NDI data were censored before some participants had their second study interviews, we performed a sensitivity analysis where we administratively censored all participants on December 31st, 2014 (the date of last available NDI data); this analysis excluded 47 participants with an incident MI who gave their second interview on or after January 1st 2015. We also performed a sensitivity analysis to assess associations with non-fatal MI only, in order to create a more uniform follow-up period. This analysis included 355 incident non-fatal myocardial infarction that were reported during the first or second study interviews, excluding fatal events (n=48). Separate sensitivity analyses were restricted to fatal CHD events only (n=40).
2.4.3. Cumulative incidence of heart disease
We generated IP exposure-and censoring-weighted cumulative risk plots to illustrate changes in the risk of heart disease over the study period, for the exposures of interest (Cole and Hernán 2004). The time scale for the risk curves was months since initiation of clean-up work for the work duration analyses, and months since April 20th, 2010 for the proximity to the spill analyses. To assess whether associations with heart disease changed across the study period, we estimated risks and risk differences of heart disease at 12 months, 24 months, 36 months and 48 months of follow-up. The risks were defined as the proportion of cumulative cases at the given month, divided by the total number at risk for heart disease at that time. Risks were determined from proportional hazards regression using the complement of the Nelson-Aalen estimate of survival, with IP exposure and censoring weights to account for confounders and predictors of censoring (Cole and Hernán 2004).
3. Results
There were 31,609 participants who entered the cohort by completing the enrollment interview, including 24,375 clean-up workers. A total of 21,256 participants, including 16,814 clean-up workers, completed the second interview. Among the 21,256 participants who completed the second interview, 12,699 (59.7%) reported, at enrollment, that they lived in a county that we defined as proximal to the oil spill. Among the 16,814 clean-up workers who completed the second interview, 2,063 (12.3%) worked for 1–30 days, 5,293 (31.5%) worked for 31–90 days, 5,735 (34.1%) worked for 91–180 days, and 3,723 (22.1%) worked >180 days.
Those who completed the second interview were more likely to be older, white, have a 2010 household income >$50,000, and were more likely to have completed 4 years of college (table 1). There were no differences in perceived health between those who did and did not complete the second interview, however those who completed the interview were slightly more likely to have reported a diagnosis of hypertension, to have reported a diagnosis of MI, to be a current drinker, and were less likely to be current smokers (table 2). Those who completed the second interview were also more likely to have worked on oil spill clean-up and were slightly more likely to have low total hydrocarbon exposure during clean-up, but there were no differences with respect to clean-up work tasks or job characteristics (table 3). Participants who had served on active duty in the military were also slightly more likely to have completed the second interview. Neither duration of clean-up work nor exposure to burning oil was associated with participation.
Table 1.
Participant demographic characteristics for the enrollment cohort (N=31,609) and follow-up cohort (N=21,256). GuLF STUDY 2010–2016
| Interview #1 (N=31,609) |
Interview #2 (N=21,256) |
Did not complete interview #2 (N=10,353) |
Risk difference for non- response |
|||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | RD (95%CI) | |||
| Gender | ||||||
| Male | 25502 (80.7) | 17031 (80.1) | 8471 (81.8) | ref | ||
| Female | 6105 (19.3) | 4224 (19.9) | 1881 (18.2) | 0.0241 (0.0111, 0.037) | ||
| Missing | 2 (0.0) | 1 (0.0) | 1 (0.0) | |||
| Age category (years) | ||||||
| 20–29 | 6226 (19.8) | 3529 (16.6) | 2697 (26.2) | −0.0529 (−0.0695, −0.0364) | ||
| 30–39 | 7340 (23.3) | 4549 (21.5) | 2791 (27.1) | ref | ||
| 40–49 | 7709 (24.5) | 5302 (25.0) | 2407 (23.4) | 0.068 (0.0528, 0.0832) | ||
| 50–59 | 7019 (22.3) | 5294 (25.0) | 1725 (16.7) | 0.1345 (0.1195, 0.1495) | ||
| 60–64 | 1849 (5.9) | 1442 (6.8) | 407 (4.0) | 0.1601 (0.1382, 0.182) | ||
| ≥65 | 1364 (4.3) | 1085 (5.1) | 279 (2.7) | 0.1757 (0.1516, 0.1998) | ||
| Missing | 102 (0.3) | 55 (0.3) | 47 (0.5) | |||
| Ethnicity | ||||||
| White | 20688 (65.8) | 14134 (66.9) | 6554 (63.7) | ref | ||
| Black | 7425 (23.6) | 4836 (22.9) | 2589 (25.2) | −0.0319 (−0.0444, −0.0193) | ||
| Asian | 326 (1.0) | 186 (0.9) | 140 (1.4) | −0.1126 (−0.1668, −0.0585) | ||
| Other/multi-racial | 2990 (9.5) | 1985 (9.4) | 1005 (9.7) | −0.0193 (−0.0374, −0.0012) | ||
| Missing | 180 (0.6) | 115 (0.5) | 65 (0.6) | |||
| Hispanic | ||||||
| Yes | 2115 (6.7) | 1357 (6.4) | 758 (7.4) | −0.0332 (−0.0543, −0.0121) | ||
| No | 29400 (93.3) | 19840 (93.6) | 9560 (92.7) | ref | ||
| Missing | 94 (0.3) | 59 (0.3) | 35 (0.3) | |||
| Education completed | ||||||
| Less than high school | 5099 (16.2) | 3161 (14.9) | 1938 (18.8) | −0.014 (−0.0305, 0.0025) | ||
| High school | ||||||
| diploma/GED | 9436 (30.0) | 5982 (28.2) | 3454 (33.5) | ref | ||
| Some college/2-year | ||||||
| degree | 9382 (29.8) | 6339 (29.9) | 3043 (29.5) | 0.0417 (0.0281, 0.0553) | ||
| 4+ year college | ||||||
| graduate | 7584 (24.1) | 5709 (26.9) | 1875 (18.2) | 0.1188 (0.1051, 0.1326) | ||
| Missing | 108 (0.3) | 65 (0.3) | 43 (0.4) | |||
| Income | ||||||
| ≤ $20,000 | 8260 (29.2) | 5187 (27.0) | 3073 (33.6) | −0.0331 (−0.0473, −0.0188) | ||
| $20,001-$50,000 | 9060 (32.0) | 5989 (31.2) | 3071 (33.6) | ref | ||
| >$50,000 | 11001 (38.8) | 8007 (41.7) | 2994 (32.8) | 0.0668 (0.054, 0.0796) | ||
| Missing | 3288 (10.4) | 2073 (9.8) | 1215 (11.7) | |||
| Proximity to the spill | ||||||
| Direct/indirect | 19354 (61.2) | 12699 (59.7) | 6655 (64.3) | −0.0421 (−0.0526, −0.0316) | ||
| Away from spill | 12255 (38.8) | 8557 (40.3) | 3698 (35.7) | ref | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
Proximity to the oil spill is defined as living in, or adjacent to, a county or parish with coastline oiled during the spill.
Table 2.
Health and lifestyle characteristics among participants who completed the first (N=31,609) and second (N=21,256) study interviews. GuLF STUDY 2010–2016
| Interview #1 (N=31,609) |
Interview #2 (N=21,256) |
Did not Complete interview #2 (N=10,353) |
Risk difference for non- response |
|||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | RD (95%CI) | |||
| Report of ever having had a nonfatal | ||||||
| MI | ||||||
| Yes | 724 (2.3) | 548 (2.6) | 176 (1.7) | 0.0863 (0.0546, 0.118) | ||
| No | 30783 (97.7) | 20643 (97.4) | 10140 (98.3) | ref | ||
| Missing | 102 (0.3) | 65 (0.3) | 37 (0.4) | |||
| First incident nonfatal MI/fatal CHD since the oil | ||||||
| spill/study enrollment | ||||||
| Yes | 395 (1.9) | 314 (1.5) | 81 (0.8) | −0.2051 (−0.2472, −0.1629) | ||
| No | 20299 (98.1) | 20299 (98.5) | 10112 (99.2) | ref | ||
| Missing | 10915 (34.5) | 643 (3.0) | 160 (1.5) | |||
| Report of ever having had a diagnosis of hypertension | ||||||
| Yes | 8573 (27.2) | 6135 (29.0) | 2438 (23.6) | 0.0591 (0.0477, 0.0705) | ||
| No | 22927 (72.8) | 15052 (71.0) | 7875 (76.4) | ref | ||
| Missing | 109 (0.3) | 69 (0.3) | 40 (0.4) | |||
| Perceived health | ||||||
| Excellent | 5353 (17.0) | 3526 (16.7) | 1827 (17.8) | −0.0104 (−0.0261, 0.0053) | ||
| Very good | 10102 (32.1) | 6857 (32.4) | 3245 (31.5) | 0.0096 (−0.0033, 0.0226) | ||
| Good | 10010 (31.8) | 6698 (31.7) | 3312 (32.2) | ref | ||
| Fair | 4510 (14.3) | 3061 (14.5) | 1449 (14.1) | 0.0096 (−0.0069, 0.026) | ||
| Poor | 1478 (4.7) | 1017 (4.8) | 461 (4.5) | 0.019 (−0.0064, 0.0443) | ||
| Missing | 156 (0.5) | 97 (0.5) | 59 (0.6) | |||
| Health compared to several years ago | ||||||
| Better | 2664 (8.5) | 1787 (8.5) | 877 (8.5) | 0.0035 (−0.0156, 0.0225) | ||
| Worse | 9432 (30.1) | 6455 (30.6) | 2977 (29.0) | 0.017 (0.0055, 0.0285) | ||
| About the Same | 19269 (61.4) | 12859 (60.9) | 6410 (62.5) | ref | ||
| Missing | 244 (0.8) | 155 (0.7) | 89 (0.9) | |||
| Cigarette smoking | ||||||
| Current | 9449 (30.1) | 5884 (27.9) | 3565 (34.8) | −0.0676 (−0.0798, −0.0554) | ||
| Former | 6777 (21.6) | 4785 (22.7) | 1992 (19.4) | 0.0158 (0.0026, 0.0289) | ||
| Never | 15144 (48.3) | 10454 (49.5) | 4690 (45.8) | ref | ||
| Missing | 239 (0.8) | 133 (0.6) | 106 (1.0) | |||
| Heavy smoker (>1 pack per day) | ||||||
| Yes | 3178 (10.2) | 1979 (9.4) | 1199 (11.8) | −0.0569 (−0.0746, −0.0392) | ||
| No | 27966 (89.8) | 19006 (90.6) | 8960 (88.2) | ref | ||
| Missing | 465 (1.5) | 271 (1.3) | 194 (1.9) | |||
| Current drinker | ||||||
| Yes | 23774 (75.8) | 16098 (76.2) | 7676 (74.9) | 0.0159 (0.0037, 0.0281) | ||
| No | 7593 (24.2) | 5021 (23.8) | 2572 (25.1) | ref | ||
| Missing | 242 (0.8) | 137 (0.6) | 105 (1.0) | |||
Table 3.
Clean-up work and employment characteristics among participants who completed the first (N=31,609) and second (N=21,256) study interviews. GuLF STUDY 2010–2016
| Interview #1 (N=31,609) |
Interview #2 (N=21,256) |
Did not Complete interview #2 (N=10,353) |
Risk difference for non- response |
|||
|---|---|---|---|---|---|---|
| Worked on clean-up | n (%) |
n (%) |
n (%) |
RD (95% CI) |
||
| Yes | 24375 (77.1) | 16814 (79.1) | 7561 (73.0) | 0.0758 (0.0631, 0.0884) | ||
| No | 7234 (22.9) | 4442 (20.9) | 2792 (27.0) | ref | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Work duration | ||||||
| 1–30 days | 2998 (12.3) | 2063 (12.3) | 935 (12.4) | ref | ||
| 31–90 | 7669 (31.5) | 5293 (31.5) | 2376 (31.4) | 0.0021 (−0.0175, 0.0216) | ||
| 91–180 | 8363 (34.3) | 5735 (34.1) | 2628 (34.8) | −0.0024 (−0.0217, 0.017) | ||
| >180 | 5345 (21.9) | 3723 (22.1) | 1622 (21.5) | 0.0084 (−0.0122, 0.0291) | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Worked before the oil well was capped | ||||||
| Yes | 20950 (85.9) | 14362 (85.4) | 6588 (87.1) | −0.0304 (−0.0467, −0.014) | ||
| No | 3425 (14.1) | 2452 (14.6) | 973 (12.9) | ref | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Clean-up job type | ||||||
| Response work | 4462 (18.3) | 3048 (18.1) | 1414 (18.7) | −0.0252 (−0.0442, −0.0062) | ||
| Operations work | 4371 (17.9) | 2946 (17.5) | 1425 (18.9) | −0.0343 (−0.0535, −0.0152) | ||
| Water cleanup | 3803 (15.6) | 2620 (15.6) | 1183 (15.7) | −0.0194 (−0.0392, 0.0004) | ||
| Decontamination | 3555 (14.6) | 2455 (14.6) | 1100 (14.6) | −0.0177 (−0.0379, 0.0024) | ||
| Land cleanup | 3631 (14.9) | 2520 (15.0) | 1111 (14.7) | −0.0143 (−0.0343, 0.0057) | ||
| Support work | 4553 (18.7) | 3225 (19.2) | 1328 (17.6) | ref | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Potential exposure to burning/flaring | ||||||
| Unknown | 505 (2.1) | 356 (2.1) | 149 (2.0) | 0.0143 (−0.0259, 0.0546) | ||
| No | 21734 (89.2) | 15010 (89.3) | 6724 (88.9) | ref | ||
| Yes | 2136 (8.8) | 1448 (8.6) | 688 (9.1) | −0.0127 (−0.0335, 0.008) | ||
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Maximum total Hydrocarbon exposure (ppm) |
||||||
| None | ||||||
| (nonworkers) | 7234 (22.9) | 4442 (20.9) | 2792 (27.0) | −0.0959 (−0.1123, −0.0794) | ||
| <0.30 | 5443 (17.2) | 3864 (18.2) | 1579 (15.3) | ref | ||
| 0.30–0.99 | 7984 (25.3) | 5519 (26.0) | 2465 (23.8) | −0.0186 (−0.0344, −0.0029) | ||
| 1.00–2.99 | 7476 (23.7) | 5094 (24.0) | 2382 (23.0) | −0.0285 (−0.0446, −0.0125) | ||
| ≥3.00 | 3445 (10.9) | 2313 (10.9) | 1132 (10.9) | −0.0385 (−0.0583, −0.0187) | ||
| Missing | 27 (0.1) | 24 (0.1) | 3 (0.0) | |||
| Employment status | ||||||
| Working Now | 20758 (66.0) | 13994 (66.1) | 6764 (65.8) | ref | ||
| Temporarily | ||||||
| Laid Off, Sick Leave | ||||||
| Or Maternity Leave | 586 (1.9) | 391 (1.9) | 195 (1.9) | −0.0069 (−0.0456, 0.0318) | ||
| Looking For | ||||||
| Work Or | ||||||
| Unemployed | 5865 (18.7) | 3764 (17.8) | 2101 (20.4) | −0.0324 (−0.0462, −0.0185) | ||
| Retired | 1511 (4.8) | 1198 (5.7) | 313 (3.0) | 0.1187 (0.0973, 0.1401) | ||
| Disabled, | ||||||
| Permanently Or | ||||||
| Temporarily | 1016 (3.2) | 689 (3.3) | 327 (3.2) | 0.004 (−0.0254, 0.0334) | ||
| Keeping House | 284 (0.9) | 192 (0.9) | 92 (0.9) | 0.0019 (−0.0529, 0.0567) | ||
| Student | 652 (2.1) | 390 (1.8) | 262 (2.6) | −0.076 (−0.1142, −0.0378) | ||
| Other | 784 (2.5) | 550 (2.6) | 234 (2.3) | 0.0274 (−0.0053, 0.06) | ||
| Missing | 153 (0.5) | 88 (0.4) | 65 (0.6) | |||
| Other oil spill work | ||||||
| Yes | 3578 (11.3) | 2594 (12.2) | 984 (9.5) | 0.0591 (0.0435, 0.0747) | ||
| No | 27934 (88.4) | 18601 (87.5) | 9333 (90.2) | ref | ||
| Don’t Know | 51 (0.2) | 35 (0.2) | 16 (0.2) | 0.0204 (−0.1071, 0.1478) | ||
| Refused | 30 (0.1) | 18 (0.1) | 12 (0.1) | −0.0659 (−0.2413, 0.1095) | ||
| Missing | 16 (0.1) | 8 (0.0) | 8 (0.1) | |||
| Served on active duty | ||||||
| Yes, Now On | ||||||
| Active Duty | 2563 (8.1) | 1735 (8.2) | 828 (8.0) | 0.0216 (0.0025, 0.0407) | ||
| Yes, On Active | ||||||
| Duty During The Last 12 Months, But Not Now | ||||||
| 567 (1.8) | 424 (2.0) | 143 (1.4) | 0.0924 (0.0562, 0.1287) | |||
| Yes, On Active | ||||||
| Duty In The Past, But Not During The Last | ||||||
| 12 Months | 4553 (14.4) | 3400 (16.0) | 1153 (11.2) | 0.0914 (0.0774, 0.1054) | ||
| No, Training For Reserves Or National | ||||||
| Guard Only | 271 (0.9) | 192 (0.9) | 79 (0.8) | 0.0531 (−0.0013, 0.1076) | ||
| No, Never | ||||||
| Served In The | ||||||
| Military | 23565 (74.6) | 15444 (72.7) | 8121 (78.5) | ref | ||
| Don’t Know | 29 (0.1) | 23 (0.1) | 6 (0.1) | 0.1377 (−0.0098, 0.2853) | ||
| Refused | 44 (0.1) | 29 (0.1) | 15 (0.1) | 0.0037 (−0.1365, 0.1439) | ||
| Missing | 17 (0.1) | 9 (0.0) | 8 (0.1) | |||
The LASSO selection method determined a final model that included covariates for age, completing 4+ years of college, and former smoking. The concordance statistic was 0.621, indicating moderate ability for this model to predict non-response.
3.1. IP censoring and exposure weights
For the work duration analyses (clean-up workers only), the mean and range of the stabilized IP censoring weights was 1.00, 0.62–2.85 with standard deviation 0.22. For the residential proximity to the spill analyses (workers and non-workers), the mean of the stabilized IP censoring weights was 1.00 and the range was 0.55–2.61, with a standard deviation of 0.22.
The stabilized IP exposure weights for work duration had a mean of 1.00 and a range of 0.48 to 2.72 with standard deviation 0.16. The stabilized IP exposure weights for residential proximity to the spill had a mean of 1.00 and a range of 0.54 to 5.67, with a standard deviation of 0.39.
3.2. Heart disease outcomes
Among 31,609 study participants, 355 reported incident first MI diagnoses that occurred after the participant began clean-up work (or after the start of the oil spill, for non-workers). Among clean-up workers who worked >30 days, 9 reported an incident nonfatal MI within the first 30 days of clean-up work. In a sensitivity analysis, excluding these 9 cases from the analyses did not meaningfully impact results.
There were 347 deaths among the cohort during the study period. Of the total deaths, 316 were among participants who had not already reported a first nonfatal MI; 40 of these deaths were due to CHD. This analysis included a total of 395 first heart disease events, 355 of which were nonfatal and 40 which were fatal.
3.3. Time-to-event analysis
Hazard ratios for the associations of residential proximity to the spill, work duration and heart disease are presented in table 4. We observed a positive association between residential proximity to the oil spill and heart disease [marginal HR= 1.29 (95% CI: 1.00, 1.65)]. This association remained after accounting for censoring with IP weights [1.30 (1.01, 1.67)]. There were suggestive positive associations between work duration >180 days (vs 1–30 days) and heart disease [1.36 (0.88, 2.11)], and these associations also did not meaningfully change after applying censoring weights [1.43 (0.91, 2.25)]. Adjusting for having had to stop clean-up work due to heat did not meaningfully change the observed associations. The Wald test for a product term between time in study and each covariate showed no significant departures from proportional hazards (p>0.10, results not shown).
Table 4.
The associations of residential proximity to the oil spill, work duration, and self-reported MI/fatal CHD: conditional and marginal hazard ratios (HR). GuLF STUDY 2010–2016
| Conditional model* |
Marginal Model |
||
|---|---|---|---|
| Cases / total N** |
HR (95% CI) | HR (95% CI) | |
| Exposure: Residential proximity to the spill |
Among workers and nonworkers |
||
| No censoring weights | |||
| Away from spill | 100/11872 | ref | ref |
| Direct/indirect proximity | 292/18590 | 1.37 (1.09, 1.74) | 1.29 (1.00, 1.65) |
| IP censoring weighted | |||
| Away from spill | 99/11859 | ref | ref |
| Direct/indirect proximity |
291/18577 |
1.39 (1.09 1.78) |
1.30 (1.01, 1.67) |
| Exposure: Work duration |
Among clean-up workers only |
||
| No censoring weights | |||
| 1–30 days | 29/2877 | ref | ref |
| 31–90 days | 86/7385 | 1.23 (0.81, 1.88) | 1.27 (0.83, 1.94) |
| 91–180 days | 121/8091 | 1.48 (0.99, 2.22) | 1.43 (0.95, 2.15) |
| >180 days | 73/5193 | 1.43 (0.93, 2.21) | 1.36 (0.88, 2.11) |
| IP censoring weighted | |||
| 1–30 days | 29/2873 | ref | ref |
| 31–90 days | 85/7374 | 1.20 (0.78, 1.84) | 1.23 (0.79, 1.90) |
| 91–180 days | 121/8086 | 1.44 (0.95, 2.17) | 1.38 (0.91, 2.10) |
| >180 days | 72/5187 | 1.51 (0.96 2.35) | 1.43 (0.91, 2.25) |
HR= Hazard Ratio; 95% CI= 95% Confidence Interval Proximity to the oil spill is defined as living in, or adjacent to, a county or parish with coastline oiled during the spill.
Adjusts for gender, age, smoking, and education. Work duration models also adjusted for residential proximity to the spill.
Total N for non-censoring-weighted models is where all confounders (gender, age, smoking, education) are nonmissing. Total N for IP censoring-weighted-models is where all confounders and predictors of censoring (gender, age, smoking, education, maximum total hydrocarbon exposure, and work duration) are nonmissing.
Cumulative risk curves for work duration and heart disease showed that risk was similar across the categories of work duration, especially during the earlier months of follow-up (figure 1). The work duration categories 31–90 days, 91–180 days and >180 days did not diverge substantially over time, but those who worked 1–30 days consistently had the lowest risk of heart disease across the study period. The risk difference for >180 days of work (vs 1–30 days) ranged from 2 cases per 1,000 workers at 12 months to 6 cases per 1,000 workers at 48 months (table 5). When examining risk of heart disease by residential proximity to the spill, risks appeared to be higher in the group living in proximity to the spill (figure 2). The risk difference for living in proximity to the oil spill (vs living farther away) and heart disease was 1 case per 1,000 workers at 12 months, and 5 cases per 1,000 workers at 48 months (table 5).
Figure 1.
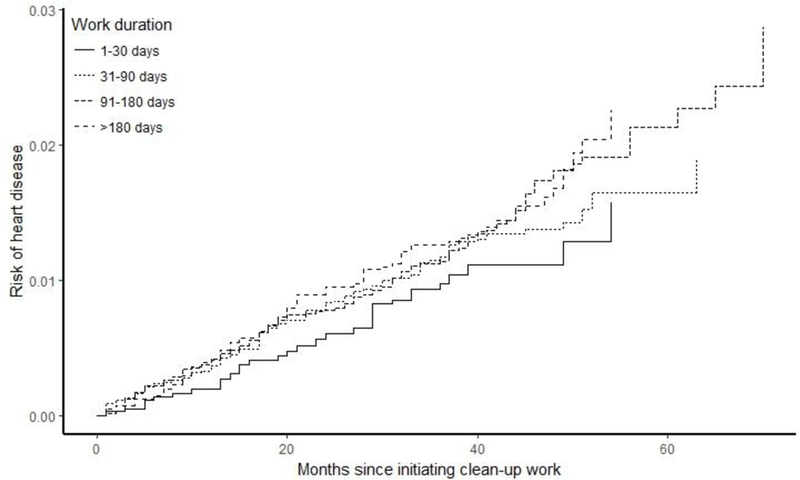
Cumulative risk curves for duration of clean-up work and self-reported MI/ fatal CHD with inverse probability of exposure and censoring weights to account for gender, age, smoking, education, maximum total hydrocarbon exposure, and residential proximity to the oil spill.
Table 5.
Risk of self-reported MI/fatal CHD by residential proximity to the spill and work duration. GuLF STUDY, 2010–2016
| Duration of follow-up: |
12 months |
24 months |
36 months |
48 months |
||||
|---|---|---|---|---|---|---|---|---|
| Risk* | RD | Risk* | RD | Risk* | RD | Risk* | RD | |
| Residential proximity to the spill |
Among the full study cohort (N=31,609) |
|||||||
| Away from the spill | 0.003 | ref | 0.007 | ref | 0.009 | ref | 0.012 | ref |
| Direct/indirect | 0.004 |
0.001 |
0.009 |
0.001 |
0.013 |
0.003 |
0.018 |
0.005 |
| Work duration | Among clean-up workers only (n=24,375) |
|||||||
| 1–30 days | 0.002 | ref | 0.006 | ref | 0.010 | ref | 0.011 | ref |
| 31–90 days | 0.004 | 0.002 | 0.008 | 0.002 | 0.012 | 0.002 | 0.014 | 0.003 |
| 91–180 days | 0.004 | 0.002 | 0.008 | 0.002 | 0.011 | 0.001 | 0.018 | 0.007 |
| >180 days | 0.004 | 0.002 | 0.010 | 0.003 | 0.013 | 0.003 | 0.017 | 0.006 |
Risks are equal to the proportion of the number of cumulative cases at the indicated point in time divided by the total number of study participants at risk at that time.
Proximity to the oil spill is defined as living in, or adjacent to, a county or parish with coastline oiled during the spill.
The risks are weighted to account for confounders and predictors of censoring.
Figure 2.
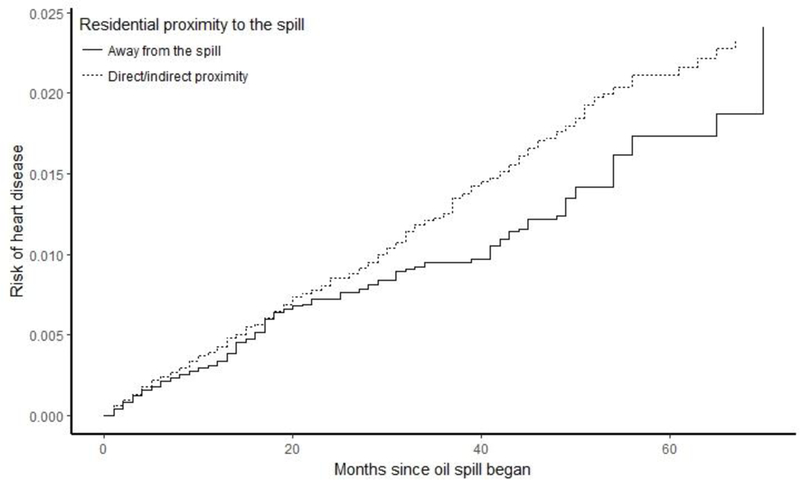
Cumulative risk curves for residential proximity to the oil spill and self-reported MI/ fatal CHD, with inverse probability of exposure and censoring weights to account for gender, age, smoking, education, maximum total hydrocarbon exposure, and work duration.
Sensitivity analyses where we censored the cohort after December 31st, 2014 showed no meaningful change in associations for work duration and heart disease [marginal HR for >180 days of work (vs 1–30 days): 1.45 (0.90–2.34)], or for residential proximity to the spill and heart disease [marginal HR: 1.39 (1.06–1.83)] (supplemental table S1), compared to the main results in table 4. Risk differences for work duration and heart disease, and proximity to the oil spill and heart disease were also unchanged (supplemental table S2). Analyses that excluded fatal CHD outcomes also did not show any meaningful changes in the observed associations for work duration [marginal HR for >180 days of work (vs 1–30 days): 1.47 (0.91–2.36)], or for residential proximity to the spill [marginal HR for direct/indirect proximity to the spill (vs away from spill): 1.28 (0.98–1.67)] (supplemental table S3). Analyses restricted to fatal CHD and excluding self-reported MI showed comparable results, though with wider confidence intervals due to the relatively low number of fatal CHD events (supplemental table S4).
In a sensitivity analysis, we removed US Coast Guard and other federal employees who worked on the oil spill clean-up from the analyses, as these workers may be more physically fit or have more access to health care services compared to non-federally-employed workers. After first excluding the 2,653 US Coast Guard, and then the total 4,640 federally employed workers from the cohort, we did not see any meaningful changes in the HR estimates for work duration and heart disease [marginal HR for >180 days (vs 1–30 days): 1.43 (0.91–2.24) excluding Coast Guard; 1.48 (0.92–2.40) excluding all federal employees]. We similarly did not see changes in the associations between residential proximity to the spill and heart disease [marginal HR for direct/indirect proximity to the spill (vs away from spill): 1.27 (0.99–1.64) excluding Coast Guard; 1.22 (0.95–1.58) excluding all federal employees], though the confidence intervals were wider compared to the analyses that included all participants (supplemental tables S5 and S6).
4. Discussion
This study, conducted among a cohort of trained workers in the response and clean-up of the Deepwater Horizon oil spill, along with others who had registered for training but did not ultimately work on the clean-up, showed suggestively higher hazards of heart disease of 29% to 43% among those living in proximity to the oil spill or who worked on clean-up >180 days. Risk differences for these associations ranged from 1 to 6 excess cases per 1,000 workers over the 5-year study period. We assessed predictors of non-response to the second interview for the GuLF STUDY and used IP weights to account for these factors in our models. Those who completed the second interview were more likely to be white, older age, nonsmokers, to have completed at least some college, have income >$50,000, and to have worked on oil spill clean-up compared to participants who did not complete the second interview. However, there were no particularly strong predictors of non-response, and hazard ratios appeared to be robust to censoring. Though applying IP censoring weights did not meaningfully change the results, weighting the cohort to resemble the full enrollment cohort addressed potential bias due to informative censoring.
This study showed a positive association between living in proximity to the spill and heart disease. This association may be driven by psychosocial stress caused by the oil spill, pollutant exposures, or other spill-related environmental factors. Other studies have shown that living in proximity to the Gulf oil spill is associated with acute health symptoms, and that affected communities faced economic and social hardships following the spill (Gould et al. 2015). A study of women living in Southeast Louisiana who were physically, environmentally or economically exposed to the oil spill showed elevations in acute symptoms including wheezing and nausea, compared to unexposed women (Peres et al. 2016). Living in or adjacent to a county oiled during the Deepwater Horizon oil spill was also shown to be associated with mental health symptoms (Kwok et al. 2017b). Increased stress, anxiety, or other health symptoms may increase risk of an acute or future heart disease manifestation (Steptoe and Kivimaki 2012). There were also some health differences among those living in proximity to vs. away from the spill. At the enrollment interview, participants living in proximity to the spill reported a higher prevalence of hypertension compared to those living further away (18.7% vs 14.9%), which may contribute to the higher hazard of heart disease observed in this group.
Work duration showed a suggestive positive association with heart disease, however there was no clear exposure-response relationship. Oil spill clean-up work was often highly physically demanding, and workers endured hot temperatures and strenuous conditions. Workers who were, perhaps, less physically capable of this work or who had health limitations may have been more likely to work a short duration, or not at all. This could lead to differences in underlying health between those with shorter work duration compared to those with longer work duration. Similarly, those who worked for longer may be healthier and less predisposed to CHD than those who worked shorter durations. If this were to be the case, the associations with heart disease observed in our study for workers in the longer duration categories would be attenuated due to healthy worker survivor bias (Arrighi and Hertz-Picciotto 1994; Buckley et al. 2015).
Despite ~33% non-response to the second telephone interview for the GuLF STUDY and differences between cohort members who did and did not complete the interview, we observed negligible impact of these differences on the estimated associations for duration of clean-up work and residential proximity to the oil spill in relation to heart disease. This is in accordance with what we anticipated, based on the fact that the associations between each predictor and loss to follow-up were generally weak (tables 1–3). The censoring weights would be expected to have more influence on effect estimates in the presence of stronger predictors of loss to follow-up (Howe et al. 2011). For the conditional hazard ratios, censoring weights may also not affect the estimates if the strong predictors of censoring are already adjusted for in the proportional hazards model. The robustness of our results to potential bias due to nonresponse increases our confidence in the generalizability of our results to the full GuLF STUDY cohort.
There are limitations of the IP censoring weights approach to address bias due to censoring, and we acknowledge that our results are specific to our chosen approach and the required modeling assumptions. One important assumption of our approach was that missing outcome data occurred at random within strata of the predictors included in the censoring weights models. Other unmeasured factors that we did not account for may have been associated with non-response. However, if non-response were random with respect to unmeasured factors within strata of the adjustment set for our censoring weights model, failure to account for unmeasured predictors would not bias our estimates (Westreich 2012). Overall, we believe it is unlikely that unmeasured factors would contribute substantial bias. Despite the fact that results were generally robust to censoring, use of IP censoring weights has been recommended as a means to interpret results as representative of the full cohort in the presence of non-random censoring of outcomes, a benefit of IP weighting that has been demonstrated in other work (Buchanan et al. 2014).
This study relied on self-reported information on nonfatal MI, which is subject to errors in recall. Previous research in other populations has shown that recall of an MI diagnosis may be poorer among individuals >75 years old, or those with less education (Yasaitis et al. 2015), however the majority of the GuLF STUDY cohort was <60 years old at enrollment, and more than half attended at least 2 years of college. Though agreement varies by study and by population, self-report of MI has shown moderate agreement with hospital discharge data (kappa=0.64) (Heckbert et al. 2004). Recall is also dependent on the time period for which disease is being ascertained, however this study focuses on a relatively short period (~5 years) during which a new diagnosis can occur. Misreport of MI diagnoses would be expected to be non-differential with respect to the exposures of interest and would bias results toward the null.
This study used National Death Index death certificate data to determine total mortality and CHD-related mortality in the cohort. Previous studies that have validated CHD-related cause of death in death certificates have found that sensitivity compared to cause-of-death determined by medical records varies between communities but is generally relatively high [81% (95% CI: 79%−83%)]. However, there was a 28% false-positive rate of classification of CHD mortality by death certificate cause-of-death among participants in the ARIC cohort (Coady et al. 2001). Misclassification of CHD-related deaths may impact results from this study, however we do not expect that misclassification would be differential with respect to the exposures of interest for this analysis, and therefore would most likely attenuate results.
Deaths prior to the start of follow-up were excluded. Thus, our results are conditional on surviving to enroll in the study. If deaths occurred more often among those with longer work duration or among those who lived closer to the spill, individuals in the higher exposure groups would have been less likely to have survived to be included in our study. This may have resulted in a lower observed risk of heart disease than what would be seen in the underlying target population of all Deepwater Horizon response and clean-up workers.
During the study there were 276 participants who were at risk for a first MI and died of non-CHD causes. At the time of death, these participants had been followed by the study for a period of 10–58 months, and 60 had completed the follow-up interview for the study and reported to have not received a diagnosis of an MI. The 216 who did not complete the follow-up interview were censored either due to death or our inability to reach them for an interview. We assessed crude risk differences of non-CHD deaths by duration of clean-up work and residential proximity to the spill. While work duration was not associated with non-CHD death, living in proximity to the oil spill had a small positive association with non-CHD death. Previous work has demonstrated that unmeasured confounders of the competing risk-exposure relationship can bias the unconditional risk difference estimates but not the conditional hazard ratio and conditional risk differences (Lesko and Lau 2017). Therefore, we do not think that bias related to non-CHD death has impacted our estimates, which are based on conditional hazard ratios and conditional risk differences. This feature is a relative advantage of our approach, versus estimating unconditional risk differences.
The GuLF STUDY is the largest prospective study of health effects related to oil spills and is the first to assess heart disease among oil spill-exposed populations. This study showed positive associations between duration of clean-up work, residential proximity to the oil spill and heart disease up to 5 years after the Deepwater Horizon oil spill. These associations persisted across the follow-up period and were also robust to censoring. Future research should investigate whether specific exposures, such as stress or individual chemical exposures, may drive the observed associations.
Supplementary Material
Highlights.
This is the first longitudinal study of oil spill exposure and heart disease.
Living near the spill was associated with 30% higher hazard of heart disease.
Elevated risks of heart disease persisted across the 5-year study period.
Censoring due to non-response to second interview did not impact results.
Acknowledgments:
The authors would like to acknowledge the study team at Social & Scientific Systems for their assistance in collecting and processing the data used for this analysis.
Funding: The GuLF STUDY is supported by the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences (NIEHS Z01-ES102945). While working on this research, Jean Strelitz was funded by a National Institute of Environmental Health Sciences T32 training grant (ES07018).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
REFERENCES
- Akaike H 1992. Information theory and an extension of the maximum likelihood principle. In: Breakthroughs in statistics:Springer, 610–624. [Google Scholar]
- Alexander M, Engel LS, Olaiya N, Wang L, Barrett J, Weems L, et al. 2018. The deepwater horizon oil spill coast guard cohort study: A cross-sectional study of acute respiratory health symptoms. Environmental research 162:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrighi HM, Hertz-Picciotto I. 1994. The evolving concept of the healthy worker survivor effect. Epidemiology 5:189–196. [DOI] [PubMed] [Google Scholar]
- Austin PC, Steyerberg EW. 2012. Interpreting the concordance statistic of a logistic regression model: Relation to the variance and odds ratio of a continuous explanatory variable. BMC medical research methodology 12:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahadar H, Mostafalou S, Abdollahi M. 2014. Current understandings and perspectives on non-cancer health effects of benzene: A global concern. Toxicology and applied pharmacology 276:83–94. [DOI] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S. 2010. Particulate matter air pollution and atherosclerosis. Current atherosclerosis reports 12:291–300. [DOI] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. 2010. Particulate matter air pollution and cardiovascular disease an update to the scientific statement from the american heart association. Circulation 121:2331–2378. [DOI] [PubMed] [Google Scholar]
- Buchanan AL, Hudgens MG, Cole SR, Lau B, Adimora AA. 2014. Worth the weight: Using inverse probability weighted cox models in aids research. AIDS research and human retroviruses 30:1170–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley JP, Keil AP, McGrath LJ, Edwards JK. 2015. Evolving methods for inference in the presence of healthy worker survivor bias. Epidemiology [DOI] [PubMed] [Google Scholar]
- Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. 2001. Validation of death certificate diagnosis for coronary heart disease: The atherosclerosis risk in communities (aric) study. Journal of clinical epidemiology 54:40–50. [DOI] [PubMed] [Google Scholar]
- Cole SR, Hernán MA. 2004. Adjusted survival curves with inverse probability weights. Computer methods and programs in biomedicine 75:45–49. [DOI] [PubMed] [Google Scholar]
- Cole SR, Hernan MA. 2008. Constructing inverse probability weights for marginal structural models. American journal of epidemiology 168:656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox DR. 1992. Regression models and life-tables. In: Breakthroughs in statistics: Springer, 527–541. [Google Scholar]
- Gould DW, Teich JL, Pemberton MR, Pierannunzi C, Larson S. 2015. Behavioral health in the gulf coast region following the deepwater horizon oil spill: Findings from two federal surveys. The journal of behavioral health services & research 42:6–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S, Pearl J, Robins JM. 1999. Causal diagrams for epidemiologic research. Epidemiology 10:37–48. [PubMed] [Google Scholar]
- Gwack J, Lee JH, Kang YA, Chang KJ, Lee MS, Hong JY. 2012. Acute health effects among military personnel participating in the cleanup of the hebei spirit oil spill, 2007, in taean county, korea. Osong public health and research perspectives 3:206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe CJ, Cole SR, Chmiel JS, Munoz A. 2011. Limitation of inverse probability-of-censoring weights in estimating survival in the presence of strong selection bias. American journal of epidemiology 173:569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJ Jr., 2016. Selection bias due to loss to follow up in cohort studies. Epidemiology 27:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok RK, Engel LS, Miller AK, Blair A, Curry MD, Jackson WB, et al. 2017a. The gulf study: A prospective study of persons involved in the deepwater horizon oil spill response and clean-up. Environmental health perspectives 125:570–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok RK, McGrath JA, Lowe SR, Engel LS, Jackson WBN, Curry MD, et al. 2017b. Mental health indicators associated with oil spill response and clean-up: Cross-sectional analysis of the gulf study cohort. The Lancet Public health 2:e560–e567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesko CR, Lau B. 2017. Bias due to confounders for the exposure-competing risk relationship. Epidemiology 28:20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middlebrook AM, Murphy DM, Ahmadov R, Atlas EL, Bahreini R, Blake DR, et al. 2012. Air quality implications of the deepwater horizon oil spill. Proceedings of the National Academy of Sciences of the United States of America 109:20280–20285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nance E, King D, Wright B, Bullard RD. 2016. Ambient air concentrations exceeded health-based standards for fine particulate matter and benzene during the deepwater horizon oil spill. J Air Waste Manag Assoc 66:224–236. [DOI] [PubMed] [Google Scholar]
- Peres LC, Trapido E, Rung AL, Harrington DJ, Oral E, Fang Z, et al. 2016. The deepwater horizon oil spill and physical health among adult women in southern louisiana: The women and their children’s health (watch) study. Environmental health perspectives [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters A 2005. Particulate matter and heart disease: Evidence from epidemiological studies. Toxicology and applied pharmacology 207:477–482. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, Kaplan J. 1999. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 99:2192–2217. [DOI] [PubMed] [Google Scholar]
- Shultz JM, Walsh L, Garfin DR, Wilson FE, Neria Y. 2015. The 2010 deepwater horizon oil spill: The trauma signature of an ecological disaster. The journal of behavioral health services & research 42:58–76. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Kivimaki M. 2012. Stress and cardiovascular disease. Nature reviews Cardiology 9:360–370. [DOI] [PubMed] [Google Scholar]
- Stewart PA, Stenzel MR, Ramachandran G, Banerjee S, Huynh TB, Groth CP, et al. 2018. Development of a total hydrocarbon ordinal job-exposure matrix for workers responding to the deepwater horizon disaster: The gulf study. Journal of exposure science & environmental epidemiology 28:223–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibshirani R 1996. Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society Series B (Methodological):267–288. [Google Scholar]
- Westreich D 2012. Berkson’s bias, selection bias, and missing data. Epidemiology 23:159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson EJ, Forbes A, White IR. 2014. Variance reduction in randomised trials by inverse probability weighting using the propensity score. Statistics in medicine 33:721–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan M, Lin Y. 2006. Model selection and estimation in regression with grouped variables. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 68:49–67. [Google Scholar]
- Zock J- P, Rodríguez-Trigo G, Rodríguez-Rodríguez E, Espinosa A, Pozo-Rodríguez F, Gómez F, et al. 2012. Persistent respiratory symptoms in clean-up workers 5 years after the prestige oil spill. Occupational and environmental medicine 69:508–513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


