Abstract
BACKGROUND:
Whether cooking with solid fuels, as occurs widely in developing countries, including Nepal, is a risk factor for pulmonary tuberculosis (PTB) is uncertain. Epidemiologic studies have produced variable results. This case-control study sought to resolve this issue with a large sample size and a population-based control group.
METHODS:
PTB cases (N = 581), aged 18 to 70 were recruited from diagnostic centers in Kaski and neighboring districts of Nepal. Population-based controls (N = 1,226) were recruited. Persons who had previously been diagnosed with TB were excluded. Questionnaires were administered at participants’ homes.
RESULTS:
Using liquefied petroleum gas (LPG) as the cookstove reference fuel, for women the odds ratio (OR) for having a primary cookstove that used wood was 0.21 (95% CI: 0.08,0.52); for men the corresponding OR was 0.80 (0.37, 1.74). For biogas, the OR for women was 0.24 (0.06,0.87) and for men, 1.41 (0.61, 3.23).
CONCLUSIONS:
The unexpected finding of a higher risk for women using LPG cookstoves, relative to wood or biogas-burning cookstoves, may be attributable to excluding persons with prior TB. A possible explanation is that emissions, such as ultrafine particles, formed during LPG combustion promote PTB manifestation in infected people who have not previously had PTB. The damage from the initial PTB leaves them susceptible to the PTB-promoting effects of smoke from wood fires. Further studies, excluding participants who have previously had TB are needed to confirm these findings. Use of exhaust hoods to the outdoors for all stoves, well-ventilated kitchens, and gas stoves raised above ground would reduce exposures.
Keywords: biogas, biomass, cooking, heating, liquefied petroleum gas
Introduction and background
Tuberculosis (TB) remains one of the world’s most intractable diseases, with an estimated 2 billion people (http://www.who.int/tb/publications/global_report/en/) infected with Mycobacterium tuberculosis complex. This is particularly so in South Asia, including India, Nepal, Pakistan and Bangladesh, where latent TB infection (LTBI) prevalence in the population can be as much as 40%(Pai and Rodrigues 2015). At any one time only a small proportion of the infected population have manifest TB disease. This makes it important to identify modifiable risk factors for the occurrence of the disease.
Household air pollution in South Asia is largely a result of combustion of fuels for cooking, heating and lighting. Worldwide, about 3 billion people still use solid fuels for heating and cooking(WHO 2014) and about 1.5 billion use kerosene for lighting(Mills 2005). Several health impacts of biomass burning have been identified, including chronic obstructive pulmonary disease, pneumonia, low birthweight and cataracts(Mortimer et al. 2012; Gordon et al. 2014; West et al. 2013; Amegah et al. 2014; Apte and Salvi 2016).
Previous studies have produced equivocal results concerning the relationship between household cooking fuel combustion and tuberculosis. Two recent reviews of this topic reached different conclusions about the relationship between biomass burning and pulmonary TB—one considered that a relationship between biomass smoke and tuberculosis had been demonstrated by the cumulative evidence from studies(Kurmi et al. 2014); the other, relying on a similar set of studies, concluded that the association had not been demonstrated, but the quality of evidence was low and insufficient for a judgement to be made(Lin et al. 2014).
A previous study carried out in Kaski District, Nepal, provided little evidence that cooking with biomass was associated with pulmonary TB, but biomass for heating appeared to be a risk factor(Pokhrel et al. 2010). The same study suggested that kerosene use, both for cooking and lighting, was associated with TB.
A limitation of that study was that most cases were recruited from a TB diagnostic center, whereas all controls and only about 10% of the cases were selected from the outpatient department of a nearby hospital. More of the cases (28%) were resident in districts outside of Kaski than were controls (6%). This raised the possibility of a selection bias influencing the results.
The lack of consensus from previous studies in general and, in particular, the uncertainty in interpretation of the Kaski study, were major impetuses for the present study using a populationbased control selection method. Its main objective was to investigate whether household fuel uses for cooking, heating or lighting are pulmonary TB risk factors.
Materials and methods
This was a case-control study of pulmonary TB disease in both men and women, recruited mainly from the Western Regional TB Center (WRTC) in Pokhara, Nepal. Although women are the adult family members generally most exposed to cooking smoke, men were also included as participants, as they are also exposed to smoke, particularly from heating and lighting fuels.
Before any field work was carried out, ethical approval was obtained from the Center for Protection of Human Subjects at the University of California, Berkeley, and the Nepal Health Research Council. The work described was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). Informed consent was obtained from all subjects before they participated in the study.
Recruitment of cases
Recruitment of pulmonary TB cases began in May 2013 and concluded in February 2017. Eligible for recruitment as cases were all patients, aged 18–70, with newly diagnosed active pulmonary TB by chest x-ray and sputum smear positivity (at least one of two sputum specimens positive for acidfast bacilli by microscopy), using methods recommended by the World Health Organization(Getahun et al. 2007). Later in the study, cases diagnosed using GeneXpert (Cepheid Inc.) were included after the TB Center acquired a GeneXpert device. Excluded as cases were:
Anyone with known immunosuppressive conditions or taking immunosuppressive drugs (e.g., corticosteroids, cancer chemotherapy) to minimize effect modification, as exploration of this was not an objective of the investigation.
Anyone with a history of TB.
Although informed consent was obtained at the time of diagnosis, collection of data for the study did not begin until at least 4 weeks of treatment had occurred, as a precautionary measure for the field staff.
Although the original intention had been to collect all cases mainly from Kaski District, where the WRTC, is located, towards the end of the field data collection, since recruitment of cases from the WRTC was slower than anticipated, cases were also obtained from TB diagnostic centers in districts neighboring Kaski, namely Tanahun, Syanja and Parbat.
Control recruitment
To achieve a suitable population-based control group for this study, we used the geographic distribution of residences of pulmonary TB cases mainly in Kaski District diagnosed by the WRTC in the previous 3 years. We sought to obtain a geographic distribution of controls (2:1, control to case ratio) that reflected the previous distribution of cases, on the assumption that the distribution of such cases during the period of study data collection would be similar.
At the time of the study, rural areas of districts in Nepal were divided into political units called Village Development Committees (VDCs) and metropolitan areas were divided into wards. For example, the Kaski district comprised 47 VDCs and two metropolitan areas (Pokhara and Lekhnath). Each VDC had a population of around 3,000–12,000 (Bern et al., 2000). Pokhara city had a population of more than 200,000, divided among 18 wards; Lekhnath’s population was about 70,000 in 15 wards. Based on statistical power calculations and on the expected gender ratio for cases, our goal was to obtain 1,300 controls, proportionately selected on the previous distribution of cases from VDCs and metropolitan wards. Houses were randomly selected from the 2008 voter registration list provided by the Nepal Government Electoral Commission in Kathmandu, with each residence in a VDC or ward having a probability of being selected proportionate to the number of registered voters in the household. If more than one person in a household was eligible, a methodology was used that randomly selected from among those eligible, with a 2:1 ratio of males to females, reflecting the expected ratio among cases. We did not obtain historical data for the diagnostic centers in other districts, but for each case recruited from those centers, two controls were selected from the same VDC/ward using a similar procedure with the voter lists for those other districts—a procedure designed to be equivalent to the use of historical case data in Kaski District.
For efficiency, rather than individually matching controls to cases as cases arose, the anticipated necessary number of controls was recruited on a frequency basis, ward by ward and VDC by VDC. Recruitment of controls was made by visits to selected residences in the VDCs. Residences in each ward/VDC were visited in the order of their random selection. If a house contained no person eligible to be a control or a selected potential control was unwilling to participate, then the next household was approached following the random order. Exclusion criteria for controls were the same as for cases— no TB history, nor on immunosuppressive medication. All participation refusals were recorded.
Data collection
Apart from TB case diagnostic data, all study data for both cases and controls were collected during the field visit to the current residence.
The questionnaire
The study questionnaire was developed in English and team-translated into Nepali for administration. It was set up on laptop computers using CasicBuilder Software (West Portal Software Corporation, San Francisco, CA). After extensive field testing to ensure cultural and linguistic appropriateness and correct functioning of skip patterns, data were directly entered on the laptop during the interview. Modules in the questionnaire covered means of cooking, heating and lighting in the household, personal history of tobacco use and alcohol consumption, socio-economic factors (education, income, type of work), housing type, health history, household history of TB, food availability, use of mosquito coils and incense, number of people in the household, presence of other household members who were smokers, number of rooms, kitchen configuration and ventilation features.
Diabetes screening test
We obtained from both cases and controls a finger-prick blood sample, which we tested in the field for Hemoglobin A1c (HbA1c) using the In2it (Bio-Rad Laboratories, Hercules, CA, U.S.A), a pointof-care device operated on batteries. This test measures the presence of glycated hemoglobin, an adduct of hemoglobin and glucose, and provides a measure of the average level of blood glucose over about the last 4 months. Uncontrolled diabetics have higher levels of HbA1c than nondiabetics. Towards the end of the study, manufacture and sales of the In2it machines and their cartridges were discontinued by the manufacturer. We then switched to collecting a 0.5 ml blood sample from each participant using sterile venipuncture technique. This was put into a CBC vial containing the anti-coagulent EDTA. Blood samples were collected by trained phlebotomists, kept cool and taken to the Fishtail Laboratory and Diagnostic Centre, Pokhara, where they were analyzed for their HbA1c concentration using a MISPA I2 automated analyzer (Agappe Diagnostics, Switzerland).
Conclusion of participation
Each participant received 300 Nepali rupees (about US$3.00) as compensation for their time and effort. Participants were also advised of their HbA1c results and, if the reading was above 6.5%, advised to seek medical advice.
Data analysis
The initial analysis involved a descriptive analysis, comparing distributions of key variables, mainly collected by questionnaire, but also from the HbA1c analysis, across cases and controls, with calculation of bivariate odds ratios and confidence intervals using conditional logistic regression, with the linking variable being the VDC or urban ward from which controls were selected. Conditional regression was used because of the large number of VDCs and wards on which cases and controls were frequency matched, causing small numbers of participants in many of the data cells(Hosmer and Lemeshow 2000). For selection of the main kitchen in households with two kitchens (none had more than two), we used the following procedure: (1) if one of the kitchens was used in more seasons than the other, then we selected that kitchen; (2) if seasonal use was equal, we selected the kitchen first in the following sequence: inside the main house, attached to the main house, separate building from the main house. This sequence reflects the descending frequency of main kitchens in single kitchen households.
Most households contained more than one stove. Although one of these stoves was designated by the interviewee as the primary stove, we coded all secondary stoves with a series of dichotomous variables denoting presence or absence of each stove type in a household. For this purpose, any additional stove in a household that was the same type as the primary stove was not coded as present with the secondary stove variables.
For diabetes, we coded as diabetic anyone who fell into either of two categories; those who reported a doctor’s diagnosis of diabetes and those who had HbA1c levels of 7% or greater.
The descriptive analysis by case and control status was followed by a descriptive analysis of how the same set of variables distributed according to the three primary fuel types used in study participant homes—LPG, biogas and wood.
Multivariate analysis was carried out using conditional logistic regression, with the matching variable being VDC or urban ward. For the main model we included all likely household sources of household air pollution exposure, including cooking, heating and lighting fuels, mosquito coils and incense burning, as well as tobacco smoking. Potential confounders were selected by examining whether covariates were independently associated with the outcome and with cooking fuel use, the main exposure of interest, as well as individually testing whether each variable affected the main result of interest—for primary cookstoves. Variables that altered any of the main outcomes by 10% or more were included in the final model, after excluding possible colliders or variables on the causal pathway (e.g., kitchen ventilation and use of fume hoods). Most models were based on stratification by the effect modifier, sex, and some models investigated the influence of kitchen characteristics, and urban or rural residence.
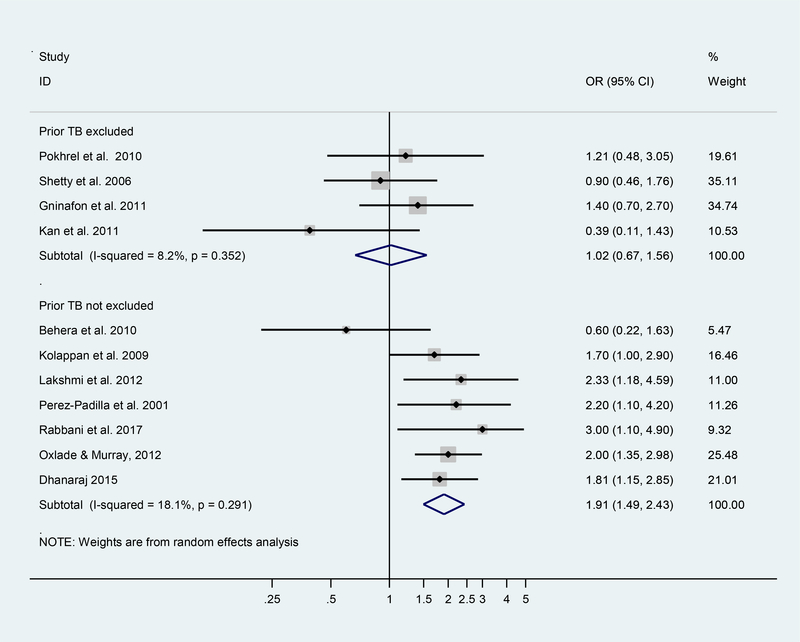
Meta-analysis of previous studies using a random-effects model was carried out to compare results of previous studies of pulmonary TB and cooking fuels that had excluded cases who had a history of TB with those that had not applied such an exclusion criterion. The basis for this was studies that had been used in two recently published (2014) meta-analyses and a few more recently published studies(Rabbani et al. 2017; Dhanaraj et al. 2015; Woldesemayat et al. 2014). Studies were excluded if they did not include a comparison of biomass with gas or where there was little variation in cooking fuel type across the study population.
Results
We obtained informed consent and study data from a total of 581 cases and 1,226 controls. Sixteen cases died before we could interview them, 7 went abroad, contact was lost with 8 cases after they returned to their homes after attending the diagnostic center, 14 were excluded for reasons to do with their living circumstances (e.g., homeless or living in a hotel or hostel), 1 because of deafness, and 2 were excluded for interviewer-safety reasons, because they had multidrug resistant TB. Ten cases refused to participate with no particular reason given. Of the controls, 24 refused to participate with no particular reason provided and 10 were excluded because they refused to provide a blood sample. Considering only the numbers refusing to participate, this gives participation rates of 98.3% and 97.3% for cases and controls, respectively.
Table 1 shows basic descriptive data for cases and controls, separately for males and females, with bivariate odds ratios (OR) and 95% confidence intervals. Most houses had only one kitchen; two kitchens were present in 140 households. For women, results in Table 1 suggest a protective association for both biogas and wood primary stoves, relative to LPG stoves; for males also a protective association for biogas, but a slightly elevated OR for wood stoves. The ORs for pulmonary TB declines with age, particularly in women; wealthier people have generally lower ORs; higher education appears protective in men, but has relatively little association in women; literacy and owning land appear protective in both sexes, but again more so in men. Using either kerosene or candles for lighting during periods of electricity blackout appears to be a risk factor, and having others in the household who are smokers appears to be a risk factor. There is no clear relationship with religion, but higher caste appears protective in both sexes. There is some suggestion that, relative to having a kitchen inside the house, having an attached kitchen or an outside kitchen building may have a protective effect. Strong pulmonary TB risk factors appear to be not owning one’s house, having a more crowded house (>2 people per room), being a smoker (men only), heavier alcohol consumption, having been diagnosed with diabetes, and having had a family member with TB in the last few years. Generally, with the exception of results for the cookstoves, these patterns are consistent with TB risk factors found in other populations. Two widely established risk factors for TB, malnutrition (as judged by self-reported days of going without food) and physician-diagnosed HIV infection, were present at only very low levels in this population.
Table 1.
Socio-demographic and household fuel use characteristics of study participants, by sex and case or control status (N = 1,807).
| Females (N = 840) | Males (N= 967) | |||||
|---|---|---|---|---|---|---|
| Cases N (col. %) | Controls N (col. %) | Bivariate Analysis OR (95% CI) | Case s N (col. %) | Controls N (col. %) | Bivariate Analysis OR (95% CI) | |
| Total participants Primary stove, main kitchen | 191 (100) | 649 (100) | 390 (100) | 577 (100) | ||
| LPG | 142 (74.3) | 341 (52.5) | 1.00 | 245 (62.8) | 362 (62.7) | 1.00 |
| Biogas | 7 (3.7) | 70 (10.8) | 0.26 (0.10– 0.65) |
21 (5.4) | 61 (10.6) | 0.56 (0.30– 1.05) |
| Wood | 42 (22.0) |
234 (36.1) |
0.53 (0.29– 0.98) |
121 (31.0) |
152 (26.3) |
1.24 (0.78– 1.98) |
| Other | 0 (0.0) | 4 (0.6) | 1.00 | 3(0.8) | 2 (0.3) | 2.22 (0.34–14.45) |
| LPG | ||||||
| No | 181 (94.8) | 570 (87.8) | 1.00 | 364 (93.3) | 513 (88.9) | 1.00 |
| Yes | 10 (5.2) | 79 (12.2) | 0.48 (0.22–1.03) | 26 (6.7) | 64 (11.1) | 0.60 (0.35–1.02) |
| Biogas | ||||||
| No | 188 (98.4) | 609 (93.8) | 1.00 | 367 (94.1) | 543 (94.1) | 1.00 |
| Yes | 3 (1.6) | 40 (6.2) | 0.37 (0.11– 1.26) | 23 (5.9) | 34 (5.9) | 0.92 (0.51– 1.68) |
| Wood | ||||||
| No | 178 (93.2) | 572 (88.1) | 1.00 | 347 (89.0) | 512 (88.7) | 1.00 |
| Yes | 13 (6.8) | 77 (11.9) | 0.62 (0.32–1.21) | 43 (11.0) | 65 (11.3) | 0.96 (0.61–1.51) |
| Kerosene | ||||||
| No | 187 (97.9) | 639 (98.5) | 1.00 | 373 (95.6) | 568 (98.4) | 1.00 |
| Yes | 4 (2.1) | 10 (1.5) | 0.93 (0.27–3.28) | 17 (4.4) | 9 (1.6) | 2.80 (1.19–6.57) |
| Electric | ||||||
| No | 188 (98.4) | 628 (96.8) | 1.00 | 383 (98.2) | 550 (95.3) | 1.00 |
| Yes | 3 (1.6) | 21 (3.2) | 0.39 (0.11–1.39) | 7 (1.8) | 27 (4.7) | 0.28 (0.11– 0.70) |
| Rice Cooker (electric) | ||||||
| No | 93 (48.7) | 299 (46.1) | 1.00 | 208 (53.3) | 203 (35.2) | 1.00 |
| Yes | 98 (51.3) | 350 (53.9) | 0.57 (0.38–0.85) | 182 (46.7) | 374 (64.8) | 0.40 (0.29–0.56) |
| Other sec. stove type | ||||||
| No | 187 (97.9) | 618 (95.2) | 1.00 | 378 (96.9) | 544 (94.3) | 1.00 |
| Yes | 4 (2.1) | 31 (4.8) | 0.57 (0.18–1.82) | 12 (3.1) | 33 (5.7) | 0.58 (0.27–1.25) |
| Residential areaa | ||||||
| Urban | 120 (62.8) | 343 (52.9) | 226 (57.9) | 344 (59.6) | ||
| Rural | 71 (37.2) | 306 (47.1) | 164 (42.1) | 233 (40.4) | ||
| Age Categories (years) | ||||||
| 18 to <28 | 84 (44.0) | 125 (19.3) | 1.00 | 83 (21.3) | 118(20.5) | 1.00 |
| 28 to <38 | 41 (21.5) | 156 (24.0) | 0.36 (0.23–0.59) | 81 (20.8) | 97 (16.8) | 1.25 (0.81–1.93) |
| 38 to <48 | 24 (12.6) | 123 (19.0) | 0.30 (0.17–0.54) | 69(17.7) | 109 (18.9) | 0.88 (0.57–1.37) |
| 48 to <58 | 17 (8.9) | 118 (18.2) | 0.24 (0.13–0.44) | 73 (18.7) | 120 (20.8) | 0.81 (0.52–1.25) |
| 58 to 70 | 25 (13.1) | 127(19.6) | 0.32 (0.18–0.56) | 84 (21.5) | 133 (23.1) | 0.91 (0.59–1.40) |
| Marital Status | ||||||
| Married | 131 (68.6) | 521 (80.3) | 1.00 | 287 (73.6) | 467 (80.9) | 1.00 |
| Single | 41 (21.5) | 56 (8.6) | 2.31 (1.42–3.77) | 64 (16.4) | 95 (16.5) | 1.20 (0.82–1.75) |
| Widow(er) | 15 (7.9) | 62 (9.6) | 1.02 (0.53– 1.94) | 23 (5.9) | 10 (1.7) | 3.09 (1.41–6.78) |
| Divorced | 4 (2.1) | 10 (1.5) | 1.10 (0.33–3.70) | 16 (4.1) | 5 (0.9) | 4.96 (1.75–14.04) |
| Monthly Income (NR) | ||||||
| < Rs 8K | 32 (16.8) | 94 (14.5) | 1.00 | 92 (23.6) | 65 (11.3) | 1.00 |
| Rs 8 to <16K | 42 (22.0) | 134 (20.6) | 0.83 (0.45– 1.52) | 92 (23.6) | 110 (19.1) | 0.54 (0.34–0.86) |
| Rs 16 to <32K | 52 (27.2) | 166 (25.6) | 0.82 (0.46–1.46) | 99 (25.4) | 166 (28.8) | 0.37 (0.23–0.59) |
| Rs 32 To <64K | 34 (17.8) | 121 (18.6) | 0.50 (0.27–0.93) | 57 (14.6) | 130 (22.5) | 0.26 (0.16–0.43) |
| > Rs 64K | 13 (6.8) | 57 (8.8) | 0.48 (0.22– 1.04) | 19 (4.9) | 62 (10.7) | 0.18 (0.09–0.35) |
| Refuse/DNK | 18 (9.4) | 77 (11.9) | 0.56 (0.27–1.16) | 31 (7.9) | 44 (7.6) | 0.44 (0.24–0.82) |
| Worked Overseas |
||||||
| No | 185 (96.9) | 638 (98.3) | 1.00 | 273 (70.0) | 456 (79.0) | 1.00 |
| Yes | 6 (3.1) | 11 (1.7) | 1.49 (0.47–4.72) | 117 (30.0) | 121 (21.0) | 1.52 (1.11–2.08) |
| Education | ||||||
| No formal Ed | 67 (35.1) | 243 (37.4) | 1.00 | 81 (20.8) | 52 (9.0) | 1.00 |
| Any Primary | 32 (16.8) | 118 (18.2) | 1.17 (0.69–1.97) | 112 (28.7) | 120 (20.8) | 0.61 (0.38–0.98) |
| Any Secondary | 39 (20.4) | 170 (26.2) | 0.80 (0.50–1.29) | 138 (35.4) | 213 (36.9) | 0.36 (0.23–0.57) |
| Any Intermediate or vocational qualification. | 33 (17.3) | 73 (11.2) | 1.24 (0.72–2.13) | 42 (10.8) | 104 (18.0) | 0.22 (0.13–0.38) |
| Any College | 20 (10.5) | 45 (6.9) | 1.34 (0.70–2.58) | 17 (4.4) | 88 (15.3) | 0.11 (0.05–0.21) |
| Read & Write Nepali | ||||||
| No | 74 (38.7) | 230 (35.4) | 1.00 | 89 (22.8) | 56 (9.7) | 1.00 |
| Yes | 117 (61.3) | 419 (64.6) | 0.72 (0.50–1.05) | 301 (77.2) | 521 (90.3) | 0.37 (0.25–0.55) |
| Religion | ||||||
| Hindu | 157 (82.2) | 570 (87.8) | 1.00 | 313 (80.3) | 495 (85.8) | 1.00 |
| Buddhist | 18 (9.4) | 52 (8.0) | 0.94 (0.51–1.74) | 57 (14.6) | 64 (11.1) | 1.38 (0.91–2.08) |
| Muslim | 3 (1.6) | 3 (0.5) | 2.83 (0.43–18.78) | 2 (0.5) | 5 (0.9) | 0.58 (0.11–3.19) |
| Christian | 12 (6.3) | 19 (2.9) | 1.94 (0.88–4.29) | 12 (3.1) | (1.7) | 2.22 (0.90–5.47) |
| Other | 1 (0.5) | 5 (0.8) | 0.46 (0.05–4.09) | 6 (1.5) | 3 (0.5) | 4.00 (0.95–16.85) |
| Caste | ||||||
| Dalit | 37 (19.4) | 101 (15.6) | 1.00 | 88 (22.6) | 65 (11.3) | 1.00 |
| Disadvantaged Janajati | 50 (26.2) | 117 (18.0) | 1.19 (0.67–2.10) | 105 (26.9) | 99 (17.2) | 0.72 (0.44–1.15) |
| Religious Minority | 7 (3.7) | 14 (2.2) | 1.04 (0.34–3.15) | 9 (2.3) | 16 (2.8) | 0.37 (0.14–0.98) |
| Relative Adv. Janajatis | 51 (26.7) | 145 (22.3) | 0.81 (0.46–1.43) | 103 (26.4) | 153 (26.5) | 0.44 (0.28–0.71) |
| Upper Caste | 46 (24.1) | 272 (41.9) | 0.43 (0.25–0.74) | 85 (21.8) | 244 (42.3) | 0.21 (0.13–0.33) |
| Own Land | ||||||
| No | 20 (10.5) | 47 (7.2) | 1.00 | 54 (13.8) | 34 (5.9) | 1.00 |
| Yes | 162 (84.8) |
599 (92.3) | 0.74 (0.41–1.34) | 334 (85.6) | 540 (93.6) | 0.39 (0.24–0.64) |
| Refuse/DNK | 9 (4.7) | 3 (0.5) | - | 2 (0.5) | 3 (0.5) | - |
| Kitchen Location | ||||||
| Kitchen inside house | 135 (70.7) | 409 (63.0) | 1.00 | 268 (68.7) | 367 (63.6) | 1.00 |
| Attached Kitchen | 35 (18.3) | 149 (23.0) | 0.82 (0.52–1.30) | 66 (16.9) | 141 (24.4) | 0.68 (0.47–0.98) |
| Unattached Kitchen | 16 (8.4) | 78 (12.0) | 0.81 (0.43–1.54) | 38 (9.7) | 64 (11.1) | 0.66 (0.41–1.09) |
| Outside Kitchen | 5 (2.6) | 13 (2.0) | 1.47 (0.41–5.30) | 18 (4.6) | 5 (0.9) | 5.01 (1.64–15.33) |
| House ownership | ||||||
| Yes | 106 (55.5) | 563 (86.7) | 1.00 | 241 (61.8) | 505 (87.5) | 1.00 |
| No | 85 (44.5) | 86 (13.3) | 3.96 (2.59–6.05) | 149 (38.2) | 72 (12.5) | 6.78 (4.59–10.00) |
| Household Crowding |
||||||
| ≤ 2/room | 148 (77.5) | 606 (93.4) | 1.00 | 284 (72.8) | 527 (91.3) | 1.00 |
| > 2/room | 43 (22.5) | 43 (6.6) | 3.16 (1.92–5.19) | 106 (27.2) | 50 (8.7) | 3.82 (2.58- 5.64) |
| Has transportation15 | ||||||
| No | 123 (64.4) | 407 (62.7) | 1.00 | 272 (69.7) | 253 (43.8) | 1.00 |
| Yes | 68 (35.6) | 242 (37.3) | 0.61 (0.42–0.90) | 118 (30.3) | 324 (56.2) | 0.24(0.17- 0.34) |
| Lighting when electricity not available | ||||||
| Kerosene Lamp | ||||||
| No | 180 (94.2) | 620 (95.5) | 1.00 | 361 (92.6) | 553 (95.8) | 1.00 |
| Yes | 11 (5.8) | 29 (4.5) | 2.04 (0.85–4.88) | 29 (7.4) | 24 (4.2) | 1.87 (1.03–3.41) |
| Candles | ||||||
| No | 120 (62.8) | 497 (76.6) | 1.00 | 235 (60.3) | 428 (74.2) | 1.00 |
| Yes | 71 (37.2) | 152 (23.4) | 1.62 (1.11–2.36) | 155 (39.7) | 149 (25.8) | 2.02 (1.49–2.74) |
| Solar Lamp | ||||||
| No | 166 (86.9) | 484 (74.6) | 1.00 | 344 (88.2) | 395 (68.5) | 1.00 |
| Yes | 25 (13.1) | 165 (25.4) | 0.47 (0.28–0.79) | 46 (11.8) | 182 (31.5) | 0.27 (0.18–0.41) |
| Battery Lights | ||||||
| No | 82 (42.9) | 268 (41.3) | 1.00 | 153 (39.2) | 300 (52.0) | 1.00 |
| Yes | 109 (57.1) | 381 (58.7) | 0.86 (0.59–1.23) | 237 (60.8) | 277 (48.0) | 1.82 (1.35–2.45) |
| Oil Lamp | ||||||
| No | 183 (95.8) | 622 (95.8) | 1.00 | 375 (96.2) | 564 (97.7) | 1.00 |
| Yes | 8 (4.2) | 27 (4.2) | 1.30 (0.54–3.14) | 15 (3.8) | 13 (2.3) | 1.27 (0.54–3.00) |
| Generator for Lights | ||||||
| No | 191 (100.0) | 648 (99.8) | 387 (99.2) | 574 (99.5) | 1.00 | |
| Yes | 0 (0.0) | 1 (0.2) | 3 (0.8) | 3 (0.5) | 1.48 (0.27–8.19) | |
| Burn Mosquito Coils | ||||||
| No | 129 (67.5) | 478 (73.7) | 1.00 | 224 (57.4) | 411 (71.2) | 1.00 |
| Yes | 62 (32.5) | 171 (26.3) | 1.15 (0.78–1.69) | 166 (42.6) | 166 (28.8) | 1.92 (1.42–2.59) |
| Burn Incense | ||||||
| No | 86 (45.0) | 188 (29.0) | 1.00 | 162 (41.5) | 158 (27.4) | 1.00 |
| Yes | 105 (55.0) | 461 (71.0) | 0.42 (0.28–0.61) | 228 (58.5) | 419 (72.6) | 0.49 (0.36–0.67) |
| Heat Home | ||||||
| No | 164 (85.9) | 555 (85.5) | 1.00 | 354 (90.8) | 501 (86.8) | 1.00 |
| Yes | 27 (14.1) | 94 (14.5) | 0.82 (0.49–1.39) | 36 (9.2) | 76 (13.2) | 0.61 (0.39–0.97) |
| Smoking status | ||||||
| Non Smoker | 145 (75.9) | 515 (79.4) | 1.00 | 142(36.4) | 339(58.8) | 1.00 |
| ≤ 8 pack-years | 14 (7.3) | 48 (7.4) | 1.36 (0.68–2.70) | 88 (22.6) | 113 19.6) | 1.81 (1.25–2.64) |
| > 8 pack-years | 32 (16.8) | 86 (13.3) | 1.38 (0.85–2.25) | 160 (41.0) | 125 (21.7) | 3.17 (2.28–4.42) |
| Other Household Smoker | ||||||
| No | 130 (68.1) | 483 (74.4) | 1.00 | 287 (73.6) | 471 (81.6) | 1.00 |
| Yes | 61 (31.9) | 166 (25.6) | 1.47 (1.00–2.17) | 103 (26.4) | 106 (18.4) | 1.63 (1.17–2.27) |
| Ventilation/Windows | ||||||
| Open Windows | 126 (66.0) | 460 (70.9) | 1.00 | 256 (65.6) | 434 (75.2) | 1.00 |
| < 4 Walls | 18 (9.4) | 44 (6.8) | 2.15 (1.08–4.31) | 36 (9.2) | 31 (5.4) | 1.95 (1.12–3.40) |
| Closed/No Windows | 47 (24.6) | 145 (22.3) | 1.26 (0.83–1.92) | 98 (25.1) | 112 (19.4) | 1.52 (1.09–2.13) |
| Use Smoke Hood | ||||||
| No | 169 (88.5) | 560 (86.3) | 1.00 | 351 (90.0) | 465 (80.6) | 1.00 |
| Yes | 22 (11.5) | 89 (13.7) | 0.58 (0.33–1.02) | 39 (10.0) | 112 (19.4) | 0.46 (0.30–0.69) |
| Days with insufficient food in last 6 months | ||||||
| No | 188 (98.4) | 645 (99.4) | 1.00 | 381 (97.7) | 573 (99.3) | 1.00 |
| Some Days | 3 (1.6) | 4 (0.6) | 1.92 (0.36–10.20) | 9 (2.3) | 4 (0.7) | 2.88 (0.83–10.00) |
| Drink Alcohol | ||||||
| Don't drink | 117 (61.3) | 457 (70.4) | 1.00 | 43 (11.0) | 112 (19.4) | 1.00 |
| Occasional Drink | 40 (20.9) | 136 (21.0) | 1.10 (0.72–1.70) | 75 (19.2) | 191 (33.1) | 1.07 (0.67–1.70) |
| 1+/wk for 6+Month | 34 (17.8) | 56 (8.6) | 2.12 (1.25–3.59) | 272 (69.7) | 274 (47.5) | 2.39 (1.57–3.64) |
| Family member with TB in last 10 Years | ||||||
| No | 149 (78.0) | 558 (86.0) | 1.00 | 309 (79.2) | 497 (86.1) | 1.00 |
| Yes | 32 (16.8) | 33 (5.1) | 4.11 (2.24–7.55) | 59 (15.1) | 22 (3.8) | 4.64 (2.69–8.01) |
| Refuse/DNK | 10 (5.2) | 58 (8.9) | 1.22 (0.54–2.77) | 22 (5.6) | 58 (10.1) | 0.49 (0.27–0.88) |
| Diabetes | ||||||
| No | 148 (77.5) | 570 (87.8) | 1.00 | 298 (76.4) | 484 (83.9) | 1.00 |
| Dr.-diagnosed diabetes | 12 (6.3) | 19 (2.9) | 2.31 (1.02– 5.25) | 32 (8.2) | 41 (7.1) | 1.02 (0.60–1.73) |
| HbA1c2265 7 | 31 (16.2) | 60 (9.2) | 2.05 (1.16–3.61) | 60 (15.4) | 52 (9.0) | 1.63 (1.05–2.54) |
| HIV doctor diagnosis | ||||||
| No | 188 (98.4) |
648 (99.8) |
1.00 | 382 (97.9) |
576 (99.8) | 1.00 |
| Yes | 3 (1.6) | 1 (0.2) | 7.58 (0.77–74.55) | 8 (2.1) | 1 (0.2) | - |
Matching factor (rural VDCs, urban wards): no OR calculation.
Transportation: family has bicycle, bullock cart, motorcycle, motorscooter, tractor or motor vehicle.
Table 2 shows how the study population (cases and controls combined) was distributed according to whether the primary household cooking fuel was LPG, biogas or wood. That is to say that it shows whether variables are associate with the primary exposure of interest—a key consideration for confounding to be present. Most of the demographic covariates were differentially distributed according to the primary household fuel type. In general, urban, younger, wealthier, bettereducated and higher caste people were more likely to use LPG, and rural, older, poorer, less educated and lower caste people to use wood for cooking. Participants with kitchens inside the main house were more likely to use LPG and those with other types of kitchen, particularly kitchens in unattached buildings and outdoors, to use wood. Home ownership was associated with being more likely to use wood than people who did not own, who were more likely to use LPG. People who used kerosene lamps for lighting when there was no electricity supply were more likely to use wood for cooking; non-smokers were more likely to be LPG users. The overall general picture is that participants who fell into higher socio-economic groups were more likely to be LPG users.
Table 2.
Socio-demographic characteristics of study participants, by sex and primary cooking fuel type (N = 1,799).
| Variable Primary stoves in main kitchen | Number of participants -cases and controls (row %)a | |||||||
|---|---|---|---|---|---|---|---|---|
| Female Subjects (N = 836) | Male Subjects (N = 963) | |||||||
| LPG | Biogas | Wood | Χ2 p-value | LPG | Biogas | Wood | Χ2 p-value | |
| Total participants | 483 (57.7%) | 77 (9.2%) | 276 (33.0%) | 607 (62.1%) | 82 (8.5%) | 273 (28.4%) | ||
| Secondary stovesb LPG | ||||||||
| LPG | ||||||||
| No | - | 30 (4%) | 235 (31%) | - | 34 (4%) | 231 (26%) | ||
| Yes | - | 47 (53%) | 41 (47%) | 0.000 | - | 48 (53%) | 42 (47%) | 0.000 |
| Biogas | ||||||||
| No | 452 (57%) | - | 264 (33%) | 573 (63%) | - | 250 (28%) | ||
| Yes | 31 (72%) | - | 12 (28%) | 0.046 | 34 (60%) | - | 23 (40%) | 0.015 |
| Wood | ||||||||
| No | 420 (56%) | 53 (7%) | - | 534 (62%) | 50 (6%) | - | ||
| Yes | 63 (72%) | 24 (28%) | - | 0.000 | 73 (70%) | 32 (30%) | - | 0.000 |
| Kerosene | ||||||||
| No | 470 (57%) | 77 (9%) | 276 (34%) | 584 (62%) | 82 (9%) | 273 (29%) | ||
| Yes | 13 (100%) | 0 (0%) | 0 (0%) | 0.008 | 23 (100%) | 0 (0%) | 0 (0%) | 0.001 |
| Electric | ||||||||
| No | 464 (57%) | 76 (9%) | 273 (34%) | 573 (62%) | 82 (9%) | 273 (29%) | ||
| Yes | 19 (83%) | 1 (4%) | 3 (13%) | 0.050 | 34 (100%) | 0 (0%) | 0 (0%) | 0.000 |
| Rice Cooker | ||||||||
| No | 134 (34%) | 36 (9%) | 220 (56%) | 150 (37%) | 35 (9%) | 221 (54%) | ||
| Yes | 349(78%) | 41 (9%) | 56 (13%) | 0.000 | 457 (82%) | 47 (8%) | 52 (9%) | 0.000 |
| Other | ||||||||
| No | 475 (59%) | 72 (9%) | 254 (32%) | 595 (65%) | 75 (8%) | 247 (27%) | ||
| Yes | 8 (23%) | 5 (14%) | 22 (63%) | 12 (27%) | 7 (16%) | 26 (58%) | ||
| Age Categories (years) | ||||||||
| 18 to <28 | 141 (67%) | 13 (6) | 56 (28) | 140 (73) | 16 (8) | 35 (18) | ||
| 28 to <38 | 120 (63) | 9 (5) | 62 (32) | 129 (73) | 12 (7) | 36 (20) | ||
| 38 to <48 | 85 (57) | 10 (7) | 55 (37) | 119 (68) | 9 (5) | 48 (27) | ||
| 48 to <58 | 68 (51) | 21 (16) | 45 (34) | 113 (61) | 17 (9) | 55 (30) | ||
| 58 to 70 | 75 (47) | 23(14) | 62 (39) | 0.000 | 99 (42) | 28 (12) | 107 (46) | 0.000 |
| Marital Status | ||||||||
| Married | 362 (56) | 62 (10) | 227 (35) | 453 (60) | 67 (9) | 232 (31) | ||
| Single | 73 (76) | 8 (8) | 15 (16) | 116 (73) | 12 (8) | 31 (19) | ||
| Widow(er) | 35 (45) | 6 (8) | 36 (47) | 19 (58) | 1 (3) | 13 (39) | ||
| Divorced | 10 (83) | 0 (0) | 2 (17) | 0.000 | 12 (63) | 2 (11) | 5 (26) | 0.058 |
| Monthly Income | ||||||||
| < Rs 8K | 41 (33) | 11 (9) | 74 (59) | 58 (37) | 7 (4) | 92 (59) | ||
| Rs 8 to <16K | 92 (53) | 14 (8) | 68 (39) | 107 (54) | 18 (9) | 73 (37) | ||
| Rs 16 to <32K | 136 (62) | 24 (11) | 58 (27) | 186 (70) | 25 (9) | 54 (20) | ||
| Rs 32 To <64K | 119 (77) | 10 (6) | 26 (17) | 149 (80) | 16 (9) | 22 (12) | ||
| ≥ Rs 64K | 49 (71) | 4 (6) | 16 (23) | 66 (81) | 6 (7) | 9 (11) | ||
| Refuse/DNK | 43 (46) | 13 (14) | 38 (40) | 0.000 | 34 (45) | 10 (13) | 31 (41) | 0.000 |
| Worked Overseas | ||||||||
| No | 470 (57%) | 76 (9%) | 273 (33%) | 467 (64%) | 63 (9%) | 197 (27%) | ||
| Yes | 13 (76%) | 1 (6%) | 3 (18%) | 0.287 | 140 (60%) | 19 (8%) | 76 (32%) | 0.301 |
| Education | ||||||||
| No formal Ed | 139 (45%) | 39 (13%) | 129 (42%) | 58 (44%) | 6 (5%) | 67 (51%) | ||
| Any Primary | 78 (52%) | 9 (6%) | 63 (42%) | 111 (48%) | 16 (7%) | 102 (45%) | ||
| Any Secondary | 133 (64%) | 11 (5%) | 65 (31%) | 242 (69%) | 35 (10%) | 74 (21%) | ||
| Any Intermediate or vocational qualification | 82 (78%) | 11(10%) | 12 (11%) | 109 (75%) | 14 (10%) | 23 (16%) | ||
| Any College | 51 (78%) | 7 (11%) | 7 (11%) | 87 (83%) | 11 (10%) | 7 (7%) | 0.000 | |
| Read & Write Nepali | ||||||||
| No | 126 (42%) | 34 (11%) | 141 (47%) | 58 (41%) | 7 (5%) | 77 (54%) | ||
| Yes | 357 (67%) | 43 (8%) | 135 (25%) | 0.000 | 549 (67%) | 75 (9%) | 196 (24%) | 0.000 |
| Religion | ||||||||
| Hindu | 397 (55%) | 75 (10%) | 251 (35%) | 489 (61%) | 75 (9%) | 239 (30%) | ||
| Buddhist | 59 (84%) | 2 (3%) | 9 (13%) | 91 (75%) | 4 (3%) | 26 (21%) | ||
| Muslim | 5 (83%) | 0 (0%) | 1 (17%) | 5 (71%) | 0 (0%) | 2 (29%) | ||
| Christian | 19 (61%) | 0 (0%) | 12 (39%) | 16 (73%) | 1 (5%) | 5 (23%) | ||
| Other | 3 (50%) | 0 (0%) | 3 (50%) | 0.000 | 6 (67%) | 2 (22%) | 1 (11%) | 0.05 |
| Caste | ||||||||
| Dalit | 55 (40%) | 7 (5%) | 76 (55%) | 63 (41%) | 7 (5%) | 82(54%) | ||
| Disad. Janajatis | 94 (57%) | 13 (8%) | 59 (36%) | 126 (62%) | 9 (4%) | 67 (33%) | ||
| Religious Minority | 14 (67%) | 1 (5%) | 6 (29%) | 14 (56%) | 3 (12%) | 8 (32%) | ||
| Relative Adv. Janajat | 147 (76%) | 5 (3%) | 42 (22%) | 194 (76%) | 12 (5%) | 50 (20%) | ||
| Upper Caste | 173 (55%) | 51 (16%) | 93 (29%) | 0.000 | 210 (64%) | 51 (16%) | 66 (20%) | 0.000 |
| Residential Location | ||||||||
| Urban | 383 (83%) | 34 (7%) | 44 (10%) | 490 (86%) | 32 (6%) | 45 (8%) | ||
| Rural | 100 (27%) | 43 (11%) | 232 (62%) | 0.000 | 117 (30%) | 50 (13%) | 228 (58%) | 0.000 |
| Own Land | ||||||||
| No | 42 (63%) | 2 (3%) | 23 (34%) | 64 (74%) | 2 (2%) | 20 (23%) | ||
| Yes | 431 (57%) | 75 (10%) | 251 (33%) | 540 (62%) | 80 (9%) | 251 (29%) | ||
| Refuse/DNK | 10 (83%) | 0 (0%) | 2 (17%) | 0.133 | 3 (60%) | 0 (0%) | 2 (40%) | 0.101 |
| Kitchen Location | ||||||||
| Inside Kitchen | 369 (68%) | 47 (9%) | 125 (23%) | (72%) | 452 | 52 (8%) | 127(20%) | |
| Attached Kitchen | 89 (49%) | 21 (11%) | 73 (40%) | (58%) | 120 (10%) | 21 (32%) | 65 | |
| Unattached Kitchen | 23 (24%) | 9 (10%) | 62 (66%) | 31 (30%) | 9 (9%) | 62 (61%) | ||
| Outside Kitchen | 2 (11%) | 0 (0%) | 16 (89%) | 0.000 | 4 (17%) | 0 (0%) | 19 (83%) | 0.000 |
| Owns House | ||||||||
| Yes | 330 (50%) | 77 (12%) | 258 (39%) | 414 (56%) | 80 (11%) | 250 (34%) | ||
| No | 153 (89%) | 0 (0%) | 18 (11%) | 0.000 | 193 (89%) | 2 (1%) | 23 (11%) | 0.000 |
| Household | ||||||||
| Crowding | ||||||||
| <= 2/room | 426 (57%) | 74 (10%) | 250 (33%) | 502 (62%) | 80 (10%) | 226 (28%) | ||
| > 2/room | 57 (66%) | 3 (3%) | 26 (30%) | 0.089 | 105 (68%) | 2 (1%) | 47 (31%) | 0.002 |
| Has Transportation | ||||||||
| No | 229 (43%) | 51 (10%) | 248 (47%) | 236 (45%) | 48 (9%) | 236 (45%) | ||
| Yes | 254 (82%) | 26 (8%) | 28 (9%) | 0.000 | 371 (84%) | 34 (8%) | 37 (8%) | 0.000 |
| Lighting during electricity blackouts | ||||||||
| Kerosene Lamp | ||||||||
| No | 476 (60%) | 74 (9%) | 246 (31%) | 592 (65%) | 80 (9%) | 237 (26%) | ||
| Yes | 7 (18%) | 3 (8%) | 30 (75%) | 0.000 | 15 (28%) | 2 (4%) | 36 (68%) | 0.000 |
| Candles | ||||||||
| No | 337 (55%) | 60 (10%) | 218 (35%) | 384 (58%) | 67 (10%) | 210 (32%) | ||
| Yes | 146 (66%) | 17 (8%) | 58 (26%) | 0.014 | 223 (74%) | 15 (5%) | 63 (21%) | 0.000 |
| Solar Lamp | ||||||||
| No | 375 (58%) | 51 (8%) | 221 (34%) | 480 (65%) | 39 (5%) | 217 (29%) | ||
| Yes | 108 (57%) | 26 (14%) | 55 (29%) | 0.036 | 127 (56%) | 43 (19%) | 56 (25%) | 0.000 |
| Battery Lights | ||||||||
| No | 212 (61%) | 35 (10%) | 100 (29%) | 296 (66%) | 44 (10%) | 110 (24%) | ||
| Yes | 271 (55%) | 42 (9%) | 176 (36%) | 0.091 | 311 (61%) | 38 (7%) | 163 (32%) | 0.028 |
| Oil Lamp | ||||||||
| No | 474 (59%) | 73 (9%) | 255 (32%) | 598 (64%) | 80 (9%) | 256 (27%) | ||
| Yes | 9 (26%) | 4 (12%) | 21 (62%) | 0.001 | 9 (32%) | 2 (7%) | 17 (61%) | 0.001 |
| Generator for Lights | ||||||||
| No | 482 (58%) | 77 (9%) | 276 (33%) | 601 (63%) | 82 (9%) | 273 (29%) | ||
| Yes | 1 (100%) | 0 (0%) | 0 (0%) | 0.694 | 6 (100%) | 0 (0%) | 0 (0%) | 0.171 |
| Burn Mosquito | ||||||||
| Coils | ||||||||
| No | 329 (54%) | 53 (9%) | 222 (37%) | 367 (58%) | 52 (8%) | 213 (34%) | ||
| Yes | 154 (66%) | 24 (10%) | 54 (23%) | 0.001 | 240 (73%) | 30 (9%) | 60 (18%) | 0.000 |
| Burn Incense | ||||||||
| No | 139 (51%) | 7 (6%) | 115 (42%) | 169 (53%) | 25 (8%) | 123 (39%) | ||
| Yes | 344 (61%) | 60 (11%) | 161 (28%) | 0.000 | 438 (68%) | 57 (9%) | 150 (23%) | 0.000 |
| Heat Home | ||||||||
| No | 418 (58%) | 69 (10%) | 229 (32%) | 533 (63%) | 70 (8%) | 247 (29%) | ||
| Yes | 65 (54%) | 8 (7%) | 47 (39%) | 0.234 | 74 (66%) | 12 (11%) | 26 (23%) | 0.353 |
| Smoking status | ||||||||
| Non Smoker | 399 (61%) | 54 (8%) | 204 (31%) | 317 (66%) | 50 (10%) | 112 (23%) | ||
| <= 8 pack-years | 38 (61%) | 3 (5%) | 21 (34%) | 145 (71%) | 12 (6%) | 48 (23%) | ||
| > 8 pack-years | 46 (39%) | 20 (17%) | 51 (44%) | 0.000 | 145 (52%) | 20 (7%) | 113 (41%) | 0.000 |
| Other Household | ||||||||
| Smoker | ||||||||
| No | 376 (62%) | 55 (9%) | 179 (29%) | 496 (66%) | 70 (9%) | 186 (25%) | ||
| Yes | 107 (48%) | 22 (10%) | 96 (43%) | 0.001 | 111 (53%) | 12 (6%) | 86 (41%) | 0.000 |
| Ventilation/Windows | ||||||||
| Open Windows | 378 (65%) | 63 (11%) | 142 (24%) | 480 (70%) | 60 (9%) | 149 (22%) | ||
| < 4 Walls | 7 (11%) | 1 (2%) | 54 (87%) | 9 (14%) | 5 (8%) | 52 (79%) | ||
| Closed/No Windows | 98 (51%) | 13 (7%) | 80 (42%) | 0.000 | 118 (57%) | 17 (8%) | 72 (35%) | 0.00 |
| Use Smoke Hood | ||||||||
| No | 383 (53%) | 69 (10%) | 274 (38%) | 468 (58%) | 75 (9%) | 268 (33%) | ||
| Yes | 100 (91%) | 8 (7%) | 2 (2%) | 0.000 | 139 (92%) | 7 (5%) | 5 (3%) | 0.000 |
| Miss/no food in 6 months | ||||||||
| No | 478 (58%) | 77 (9%) | 274 (33%) | 603 (64%) | 82 (9%) | 264 (28%) | ||
| Some Days | 5 (71%) | 0 (0%) | 2 (29%) | 0.631 | 4 (31%) | 0 (0%) | 9 (69%) | 0.004 |
| Drink Alcohol | ||||||||
| Don't drink | 313 (55%) | 65 (11%) | 194 (34%) | 101 (65%) | 21 (14%) | 33 (21%) | ||
| Occasional Drink | 121 (70%) | 6 (3%) | 47 (27%) | 194 (73%) | 23 (9%) | 49 (18%) | ||
| 1+/wk for 6+Month | 49 (54%) | 6 (7%) | 35 (39%) | 0.001 | 312 (58%) | 38 (7%) | 191 (35%) | 0.000 |
| Family w/ TB last 10 Years | ||||||||
| No | 427 (61%) | 70 (10%) | 208 (30%) | 513 (64%) | 77 (10%) | 212 (26%) | ||
| Yes | 34 (52%) | 3 (5%) | 28 (43%) | 62 (78%) | 1 (1%) | 17 (21%) | ||
| Refuse/DNK | 22 (33%) | 4 (6%) | 40 (61%) | 0.000 | 32 (40%) | 4 (5%) | 44 (55%) | 0.000 |
| Diabetes | ||||||||
| No | 403 (56%) | 70 (10%) | 242 (34%) | 478 (62%) | 66 (8%) | 233 (30%) | ||
| Dr. diag diabetes | 22 (73%) | 1 (3%) | 7 (23%) | 56 (77%) | 6 (8%) | 11 (15%) | ||
| HbA1c>= 7 | 58 (64%) | 6 (7%) | 27 (30%) | 0.245 | 73 (65%) | 10 (9%) | 29 (26%) | 0.089 |
| HIV Doctor diagnosis | ||||||||
| No | 481 (58%) | 77 (9%) | 274 (33%) | 601 (63%) | 81 (8%) | 271 (28%) | ||
| Yes | 2 (50%) | 0 (0%) | 2 (50%) | 0.683 | 6 (67%) | 1 (11%) | 2 (22%) | 0.900 |
Eight participants excluded because they used other main cooking fuel types (kerosene, electricity, coal)
Secondary stoves when different to the primary stove.
The results of the multivariate analysis for the sources of household air pollution are shown in Table 3. The only strong associations with pulmonary tuberculosis in which the confidence interval excludes the null are for primary stove type in women (using either a wood or biogas cookstove is protective relative to using an LPG stove), tobacco smoking by both sexes, and burning incense for women. The latter is in a protective direction. Relative to the bivariate results in Table 1, the protective directive of the relationship for primary stoves cooking with wood has strengthened for women. Among men, the association with wood has moved in the direction of a protective relationship; with biogas the OR has moved to above the null, but both confidence intervals include 1.00. The pattern with secondary stoves generally reflects the pattern with primary stoves, particularly for women: having a secondary LPG cookstove was associated with higher risk, while having either a biogas or wood-burning secondary cookstove was associated with reduced risk.
Table 3.
Multivariate conditional logistic regression analysis of pulmonary tuberculosis and sources of household air pollution, in and around Kaski district, Nepal, by sex.
| OR (95% confidence interval)a | ||
|---|---|---|
| Females | Males | |
| OR (95% CI) | OR (95% CI) | |
| Primary stove type in main kitchen | ||
| LPG | 1.00 | 1.00 |
| Biogas | 0.24 (0.06, 0.87) | 1.41 (0.61, 3.23) |
| Wood | 0.21 (0.08, 0.52) | 0.80 (0.37, 1.74) |
| Secondary, fuel-using stovesb | ||
| LPG | ||
| No | 1.00 | 1.00 |
| Yes | 1.49 (0.47, 4.70) | 0.69 (0.32, 1.45) |
| Biogas | ||
| No | 1.00 | 1.00 |
| Yes | 0.46 (0.13, 1.65) | 1.83 (0.83, 4.04) |
| Wood | ||
| No | 1.00 | 1.00 |
| Yes | 0.89 (0.39, 2.03) | 0.82 (0.36, 1.86) |
| Kerosene | ||
| No | 1.00 | 1.00 |
| Yes | 0.77 (0.06, 9.38) | 1.26 (0.45, 3.49) |
| During electricity blackouts, use: Kerosene Lamp | ||
| No | 1.00 | 1.00 |
| Yes | 2.24 (0.81, 6.21) | 1.61 (0.76, 3.42) |
| Candles | ||
| No | 1.00 | 1.00 |
| Yes | 1.21 (0.71, 2.05) | 0.94 (0.62, 1.44) |
| Oil Lamp | ||
| No | 1.00 | 1.00 |
| Yes | 1.62 (0.50, 5.27) | 0.58 (0.23, 1.44) |
| Burn Mosquito Coils | ||
| No | 1.00 | 1.00 |
| Yes | 0.77 (0.49, 1.19) | 1.31 (0.87, 1.97) |
| Burn Incense | ||
| No | 1.00 | 1.00 |
| Yes | 0.64 (0.41, 0.98) | 0.73 (0.51, 1.04) |
| Heat Home | ||
| No | 1.00 | 1.00 |
| Yes | 0.83 (0.41, 1.68) | 0.73 (0.46, 1.15) |
| Tobacco smoking | ||
| Never | 1.00 | 1.00 |
| <8 pack-years | 1.56 (0.52, 4.63) | 1.06 (0.66, 1.70) |
| >8 pack-years | 2.26 (1.12, 4.56) | 2.88 (1.81, 4.59) |
| Other Household Smoker(s) | ||
| No | 1.00 | 1.00 |
| Yes | 1.38 (0.77, 2.48) | 1.31 (0.87, 1.99) |
Adjusted for age (continuous), income, education, literacy, home ownership, use of electric stoves and rice cookers, solar lamps or battery lights, alcohol consumption, and family member with TB in last 10 years.
Secondary stoves that are different to the primary stove in household.
In both sexes, tobacco smoking was associated with TB. None of the other sources of household air pollution—lighting, heating, mosquito coils, other household members who smoked—showed clear evidence of an association with pulmonary TB, although small numbers (e.g., for kerosene lamps) may have made it difficult to identify associations if they were present.
To examine possible effect modifiers, Table 4 shows fully adjusted results, similar to those in Table 3, but just for primary cookstoves, subsetted by various kitchen situations—households with only one kitchen, households with only a 4-walled kitchen, and urban and rural households separately. The most striking differences are for residential location, where for women the apparent protective associations, relative to LPG, for both biogas and woodstove kitchen households are much stronger in rural than in urban settings. Somewhat anomalously, biogas cooking appears to be a strong risk factor for men in urban settings, but not in rural areas.
Table 4.
Multivariate conditional logistic regression analysis results for primary biogas and wood cookstoves, relative to primary LPG cookstoves (OR = 1.00), subsetted for various kitchen situations and settings, separately by sex.
| Kitchen settings | Females | Males | ||||
|---|---|---|---|---|---|---|
| n | Biogas stove | Wood stove | N | Biogas stove | Wood stove | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||
| All Kitchens (as in Table 3) | 645 | 0.24 (0.06, 0.87) | 0.21 (0.08, 0.52) | 918 | 1.41 (0.61, 3.23) | 0.80 (0.37, 1.74) |
| Single kitchen households | 588 | 0.18 (0.04, 0.72) | 0.26 (0.09, 0.71) | 839 | 1.66 (0.62, 4.43) | 0.79 (0.34, 1.83) |
| 4-wall kitchen households | 595 | 0.15 (0.04, 0.65) | 0.10 (0.03, 0.29) | 855 | 1.43 (0.57, 3.59) | 0.45 (0.19, 1.06) |
| Urban households | 399 | 0.36 (0.05, 2.55) | 0.52 (0.13, 2.06) | 550 | 5.65 (1.30, 24.60) | 1.29 (0.44, 3.81) |
| Rural households | 246 | 0.11 (0.01, 1.03) | 0.08 (0.02, 0.25) | 368 | 0.37 (0.10, 1.40) | 0.31 (0.11, 0.90) |
Adjusted for age (continuous), income, education, literacy, home ownership, secondary stoves, lighting types used when electricity was unavailable, home heating, use of incense and mosquito coils, cigarette smoking, alcohol consumption, other household member who smokes, and family member with TB in last 10 years.
Adjusted for age (continuous), income, education, literacy, home ownership, secondary stoves, lighting types used when electricity was unavailable, home heating, use of incense and mosquito coils, cigarette smoking, alcohol consumption, other household member who smokes, and family member with TB in last 10 years.
To investigate whether exclusion of participants with a history of TB could explain the disparity of previous results, we conducted a stratified, random-effects model meta-analysis. Studies of adults were stratified into (i) those for which either at least cases explicitly excluded those with a prior TB history, and (ii) those for which there is no evidence of such a limitation on eligibility of both cases and controls, or for which only control eligibility included a requirement for no prior TB history. We treated case exclusions and control exclusions differently because prior TB histories will be much more common in cases than in controls, since TB in the general population is a relatively rare condition. For the studies to include in our meta-analysis we relied on searches carried out for previous recent meta-analyses of adult TB(Kurmi et al. 2014; Lin et al. 2014), and included a few more recently published studies, but not our present study.
We excluded studies for which the comparison was not between biomass and gas (i.e., LPG, natural gas or biogas) as the reference category. Those excluded were studies involving comparisons of the extent of biomass use (Crampin et al. 2004; Garcia-Sancho et al. 2009), studies where virtually everyone used solid fuels(Woldesemayat et al. 2014), and studies using solid fuels or kerosene in the comparison group(Mishra et al. 1999; Gupta et al. 1997). We used results for females only when they were available(Pokhrel et al. 2010; Rabbani et al. 2017; Kan et al. 2011; Lakshmi et al. 2012; Gninafon et al. 2011), but when results only for males and females combined were available, we used those (Dhanaraj et al. 2015; Perez-Padilla et al. 2001; Oxlade and Murray 2012; Shetty et al. 2006; Kolappan and Subramani 2009). Figure 1 shows a Forest plot from the meta-analysis. There is a clear difference in the summary estimates for the two categories of study, with the estimate for studies when prior TB cases were not excluded being higher than the estimate for studies with the exclusion of at least cases with prior TB. Based on the I2 values, results of neither group of studies was significantly heterogeneous.
Figure 1.
Random-effects meta-analysis of previous epidemiologic studies investigating the relationship between biomass cooking (relative to gas) and pulmonary TB, stratified according to whether cases with prior TB were excluded or not.
Discussion
This case-control study sought to provide clear evidence of an association between household air pollution from solid fuel use and pulmonary TB. As illustrated by two recent systematic reviews/meta-analyses of the existing evidence, studies to date have provided, at most, only weak and somewhat inconsistent evidence of an association with solid fuel use(Kurmi et al. 2014; Lin et al. 2014).
The present study was a follow-up to a small, clinic-based, case-control study in the same district of Nepal. That study provided little evidence for an association of solid fuel use for cooking with pulmonary TB, but did provide evidence of an association of TB with solid fuel use for heating and also, at the time unexpectedly, evidence of an association of TB with kerosene use, both for cooking and lighting(Pokhrel et al. 2010). The present study was prompted particularly because most cases and controls in that previous study were obtained from different institutions—leading to the concern that results might be a consequence of selection bias arising from different catchment areas for cases and controls. Controls in the present study were population-based—mainly selected from areas where pulmonary TB cases attending the WRTC during the previous 3 years had lived. The underlying assumption was that the cases in the following years were likely to come from the same catchment area.
A second motivation to carry out the present study was to confirm the striking and unprecedented results for kerosene obtained in the previous Kaski study(Pokhrel et al. 2010). However, since that study, the Government of Nepal had removed the subsidy for kerosene. Probably as a consequence of this, we found few kerosene cookstove users in our study population, rendering it impossible to confirm the kerosene cookstove-related results of our previous study. The small number of kerosene lighting users made it difficult to examine with sufficient sample size the kerosene lighting result previously obtained. Elevated odds for the association with kerosene lamp use were obtained for both males and females (Table 3), but both confidence intervals included the null.
In addition to the population-based sampling frame, other strengths of this study were: it had a larger sample size than any previous case-control study that had addressed this issue in a population using a variety of fuel types; it excluded anyone, case or control, who had a prior TB diagnosis; and it collected a comprehensive range of data on fuels used for household cooking, including secondary cookstoves, heating and lighting. The focus of most other studies has been on cooking only, and then focused only on the primary cookstove.
The results for cooking fuels obtained in the present study are both surprising and concerning. They suggest that, for women, cooking with solid fuel (almost all wood) is “protective” relative to cooking with LPG. If wood had been used as the reference fuel in Table 3, the OR for LPG would have been 4.76 (95% CI: 1.92, 12.5). A similar directionality of effect, but much weaker, was found for men. Supporting the findings, particularly for women, the pattern of results for secondary stoves was broadly similar to that for primary stoves, but with weaker effect sizes. The protective association with wood stove use was much stronger for rural than for urban participants (Table 4).
With such unexpected results it is particularly important to consider whether they could be caused by confounding, information bias, or selection bias. We collected a wide range of household and socio-demographic information in our study, key items of which are shown in Table 1. Despite extensive efforts to identify confounding that could explain the apparently higher risk associated with LPG use, the cooking fuel results proved robust.
The likelihood that information bias, either of outcome or exposure, explains our results seems low: TB cases were confirmed by sputum examination or by GeneXpert. We did not, however, test controls to ensure they were free of PTB. If some controls were actually undiagnosed TB cases, they would almost certainly have been only a small proportion of the total controls and the resulting bias would have been towards the null—which could not explain our results. In terms of the possibility for misclassification of exposures, all interviews were carried out at participant residences and the field team inspected and photographed cooking devices. Thus the likelihood of misclassification of cooking devices is small.
In regard to selection bias, the participation rates of both cases and controls were very high and efforts to ensure both groups were drawn from the same population were incorporated into the study design. Controls were chosen to represent the geographic distribution of TB case residences in the 3 years before the study began. We found no evidence that the catchment area for cases had changed substantially by the time of our study.
If some form of bias or confounding is not obviously explaining our results, then why have other studies investigating this issue in adults not obtained similar results? A few other studies have suggested a protective association with biomass cooking(Crampin et al. 2004; Kan et al. 2011; Behera and Aggarwal 2010); others have provided evidence of a positive association with biomass burning(Rabbani et al. 2017; Dhanaraj et al. 2015; Mishra et al. 1999; Gupta et al. 1997; Lakshmi et al. 2012; Perez-Padilla et al. 2001; Oxlade and Murray 2012); while others have found little evidence of association between pulmonary tuberculosis and cooking with biomass(Pokhrel et al. 2010; Gninafon et al. 2011; Shetty et al. 2006).
Although issues with control selection are evident in some of the previous studies, there is another possible reason for the wide disparity in results: Our study was unusual in that it took care to exclude any case or control who had a previous TB diagnosis. The literature from previous studies shows that most studies either did not exclude people with such a history, or it is not specified in the publication that such people were excluded, which we interpret as meaning that such exclusions were not made. A few studies were based on “newly diagnosed” pulmonary TB, but this does not mean that they explicitly excluded people with a history of TB.
To test the hypothesis that exclusion of participants with prior TB could be responsible for our results, we carried out a meta-analysis, after stratifying according to whether cases with prior TB had been excluded (Figure 1). The two groups produced quite different summary estimates. The group of studies that did not exclude cases with prior TB is visually quite consistent, with the exception of one study(Behera and Aggarwal 2010), which produced a small OR. That this study did not exclude prior cases of TB is inferred from a statement in the publication that the cases were “consecutive patients” and no mention of exclusion criteria. The main analysis adjusted for respiratory symptoms while cooking, which variable was very strongly associated with the TB outcome (adjusted OR = 10.7, 95% CI: 2.9, 39.6). Since these symptoms are likely to have been a consequence of TB disease, they could not have confounded the association between cooking fuel use and TB. Hence adjustment for this variable appears to have been inappropriate and the induced bias may explain the low observed OR for the association of biomass with TB in that study. Overall, the meta-analysis results support a hypothesis that excluding participants with prior TB is the reason for our findings.
Why then should such an exclusion criterion make such a difference to results? A possible reason is that pulmonary TB, even when cured, leaves residual lung damage, including cavities and scarring. Evidence of previous TB disease is apparent, both radiologically and clinically, such as by reduced lung function, even in people who have been treated for and are considered cured of the condition. The risk of TB by new infection is higher in people who have previously had TB, even after successful treatment(Verver et al. 2005), and there is increasing evidence that the risk of COPD-like illness is much higher in people who have had previous pulmonary TB(Sarkar et al. 2017). This damage may make the lungs more susceptible to other TB risk factors or even reinfection. However, to account for our results, this would mean that LPG would need to have a higher risk of causing first pulmonary TB manifestations than biomass smoke.
There are several reasons why that may be the case. First, there is evidence from other studies that in homes where biomass is used for cooking, infants at least are less likely to spend time in the kitchen during cooking than are infants in homes where cooking is with kerosene or with gas(Bates et al. 2013; Saksena et al. 2003). This may reflect the behaviors of their mothers when using different fuels. It is possible that this accounts for the urban-rural difference apparent in Table 4. Rural-living women may have greater opportunities to leave their kitchens during cooking.
Second, depending on how it is burned, gas can produce very small particles. This is particularly the case when gas burns with a yellow flame, indicating the formation of particles, the heating of which produces the incandescent glow. Gas cookstove design can be a major determinant of burning efficiency, including the amount of particles that are produced(Basu et al. 2008). Our observations in Nepal indicate that gas is often burned with a yellow flame, whether from an effort to conserve the fuel or because of blocked gas jets, leading to inefficient combustion. Particles from gas combustion are usually in the ultra-fine range, meaning they are more likely to be inhaled deep into the respiratory tract. Arguing against that as a reason for our results is the fact that biomass, when burned, also produces ultrafine particles--in much greater quantities than from LPG combustion(Shen et al. 2017). We know, however, that biomass smoke provokes physiological responses in the lungs, such as macrophage activation(Rylance et al. 2015), which may at the same time affect, possibly enhance, macrophage protection against TB bacilli. We are unaware of evidence that ultrafines alone (as from LPG) provoke a similar physiologic response and possibly they can reach the TB bacilli in the lungs and, in some yet-unexplained way, activate them.
If some such mechanism does apply, then it must occur only at lower levels of biomass smoke exposure: in our study, tobacco smoking, a form of biomass combustion, was clearly a risk factor in both men and women (Table 3). This confirms other findings(Bates et al. 2007; Lin et al. 2007) and is likely due to the much heavier smoke exposure from direct tobacco smoking and the fact that the smoke is inhaled deeply into the lungs,
Third, it is well established that burning of LPG produces nitrogen oxides and possibly other chemicals, such as formaldehyde. Potentially, these could be responsible for TB-activating effects of LPG. Fourth, the hotter flame associated with LPG burning is also likely to generate more food or cooking oil particles than the lower heat from wood burning. All or any of these factors could have contributed to the associations found in this study.
It is notable that the results for LPG and biogas are different for women. The biogas result is not explained by primary biogas users having a biomass stove--among women most of them (61%) used LPG as a second stove and only 31% had a second stove which burned biomass (Table 2). The number of biogas users was small, with wide confidence intervals, allowing for the possibility that the biogas result may be attributable to chance. However, there are substantial differences in composition, properties and combustion characteristics between biogas and LPG. In particular, LPG is a variable mixture of propane and butane, whereas biogas is mainly methane and carbon dioxide(Surendra et al. 2014). In that sense, biogas is similar to natural gas, which is also mainly methane and burns more cleanly, with less particle formation, than LPG and with less NOx formation. Anecdotally, biogas is said in Nepal to be a cleaner burning fuel than LPG.
Possibly corroborative of the different results for these two gases, is that in an ongoing crosssectional study of eye diseases in Nepal, we asked a question about how much time a woman spends in the kitchen when cooking. Results were quite different for LPG and biogas users. Of 380 LPG users, 112 (29.5%) spent all or most of their time in the kitchen when cooking, but only 3/59 (5.1%) of biogas users did the same. Unfortunately, we did not ask the same question in our TB study, but the ocular study is being carried out among women in the same district of Nepal.
Why women cooking with biogas would spend less time in the kitchen than women cooking with LPG might have something to do with the stronger odor of biogas in some households. It could also be because biogas, having less calorific value for the same volume of gas, cooks more slowly, reducing the need for the presence of the cook in the kitchen.
Although, relative to LPG, cooking with solid fuels was not a risk factor in our study, it was perhaps more surprising that we did not find heating the house with solid fuels, relative to no heating at all, to be a risk factor. Heating the house is uncommon in Nepal, as the great majority of people simply wear more clothes inside when it gets cold. In those households which do use fuel for heating we would expect the house to be closed up and become smokier. A possible explanation, consistent with our cookstove results, is that exposures to biomass smoke that are substantially less than those experienced by a tobacco smoker are a weaker risk factor in those who have not already experienced pulmonary TB disease.
Although relatively few households used kerosene for lighting when the electricity supply was unavailable, many more used candles. In some ways, candles are like kerosene lamps in that they produce fine particles, although they emit at a lower rate than kerosene lamps. However, although we found limited evidence that kerosene lamps were a risk factor for TB (Table 3), the results did not suggest this for candles.
Since the results of our study are radically different to what was anticipated, at least for cookstoves, they should be confirmed by other studies. We recommend that such studies incorporate several features: (i) an exclusion criterion for both cases and controls of no prior history of TB, pulmonary or extra-pulmonary (or at least collecting information on whether each participant had previous TB disease); (ii) a population-based control group, with care to ensure that controls are representative of the population that generated the cases; (iii) detailed collection of data on cooking practices, including different kitchens, time spent in kitchen while cooking, and stove types used in each; and (iv) a sample size large enough for examination of specific cooking fuels, including (depending on fuels used at the study location) biogas and LPG separately, and wood and cow dung separately. Many previous studies of this issue have stratified combinations of fuels into “clean” and “dirty” or “solid” and “not solid”. As our results show, LPG and biogas, which, to the best of our knowledge in previous studies of household cooking fuel use have always been combined as “gas”, may have quite different associations with pulmonary TB. Commonly also, wood and dung have been combined into a “biomass” category. In our study population virtually no-one used cow dung as a fuel and so we were not able to examine its association with TB. Cow dung is a widely used fuel in the southern part of Nepal (the Terai) and other parts of South Asia. The difference may be important as, for example, cow dung smoke has been shown to have much higher levels of endotoxin than wood smoke(Semple et al. 2010) and the consequent impact on pulmonary TB risk may be different.
If the results of our study are confirmed, they have serious policy implications. There has been a big move internationally to move less-developed countries up the “energy ladder”, away from solid fuel use for cooking(Jose et al. 2018). Because in most developing countries, electricity connection and supply is largely unaffordable, LPG and, to a lesser extent, biogas are the cooking fuels available to replace biomass. However, the World Health Organization has highlighted that there have been few studies evaluating the safety of LPG and it is important that such studies be carried out(WHO 2014). In general, gas stoves are perceived to be much cleaner than biomass stoves, although levels of ultrafine particulates and low levels of NOx are not generally detectable by people.
Related to this, the results of our study may throw some light on concerns expressed in a recent major publication from the Global Burden of Disease Study 2015 (GBD Tuberculosis Collaborators 2017). Some countries, including in South Asia, were found to have a burden of TB higher than would be predicted based on their socioeconomic development. The attributable TB burden for household fuel use was not calculated both because of insufficient evidence for a causal relationship with HAP and because of concerns about recall bias in case-control studies, as none of them measured air pollution levels. If the results of the present study hold up, it may provide a reason for the apparent inconsistency with expectations based on economic development, as such development is often accompanied by a move from biomass-burning to LPG stoves. It could also overcome previous concerns about the basis for calculating a HAP-related burden of TB: our study provides an explanation for inconsistency of past results and, even though this is a case-control study, recall bias should not be a problem because household stove types were verified by inspection. Objective household air pollution measurements would not necessarily provide more clarity as there is a much smaller mass of PM2.5 released by gas stoves than biomass stoves, even if the number of particles released and their ability to penetrate deep into the lungs may be much greater.
Irrespective of whether LPG is confirmed as a TB risk factor, this should not be taken to suggest there is no problem with biomass burning. The fact that, as the meta-analysis suggests, biomass was a stronger risk factor than gas in studies with no prior TB exclusions suggests that it may be a risk factor for TB recurrence, whether from reactivation of existing infections or new infections. Also, there are many other health outcomes that have been clearly associated with biomass burning, the studies of which have not produced the variable range of results seen across the studies focused on pulmonary TB(Kurmi et al. 2014; Lin et al. 2014). Efforts to reduce or eliminate exposure to biomass smoke need to continue unchecked.
Conclusions
The results of our study, particularly when taking into account the results of other studies of household fuel use and PTB, provide a plausible explanation for why the results of those other studies have appeared heterogeneous and insufficient to confirm the widely held, but unverified, assumption that biomass smoke is a risk factor for pulmonary TB. Collectively, the results of all of the studies do suggest that biomass burning is a pulmonary TB risk factor, but this appears more likely to be the case if a person has previously suffered from pulmonary TB.
The most important finding of this study is that cooking with LPG gas appears to be a strong PTB risk factor, relative to cooking with wood or biogas, particularly in people who have not manifested TB previously. This may be mostly people newly infected with the M. tuberculosis bacillus, as evidence shows that the risk of manifest TB is highest in the first year after infection(Esmail et al. 2014).
More studies that exclude previous TB cases are desirable to confirm the findings of the present study. At the same time, re-analysis of existing data from well-conducted epidemiology studies that permit separation of pulmonary TB cases into those who have previously had TB and those who have not had it may help elucidate the present results. Despite the present lack of confirmatory studies, the evidence at this time is sufficient for advocacy of at least the use of hoods for all stoves, including gas stoves, ensuring that the kitchen is well-ventilated during their use, providing more efficiently burning LPG stoves with gas jets less likely to clog, minimizing time in the kitchen during cooking, and ensuring gas stoves are kept raised above the ground--to help reduce exposures to their emissions. The latter precaution is appropriate also for fire safety reasons.
Highlights.
Liquefied petroleum gas (LPG) emissions appear to be a stronger risk factor for pulmonary tuberculosis (PTB) than wood smoke in people who have not had prior TB
Biogas (methane) appears to be a lesser risk factor for PTB than LPG (propane and butane)
The difference in risk may be because of ultrafine particles formed when LPG burns inefficiently
Wood smoke appears to be a PTB risk factor in people who have had prior TB, possibly because of lung damage
Acknowledgements
The authors thank Drs. Prakash Mishra and Mukunda Prasad Acharya, Directors of the Western Regional Tuberculosis Center in Pokhara, Nepal, for providing access to cases, and the following members of the Nepal field team for data collection: Ambika Baniya, Avash Bhandari, Anjana Dhakal, Kabita Dhamala, Bina Gurung, Birendra Kunwar, Madhu Maya Pahari, Bhawani Prasad Pandey, Suraj Pant, Nabaraj Poudel, Pradip Poudel, Ramesh Kumar Rijal, Sharada Thapa, Sujata Thapa, and Subash Timilsina. Thanks also to Ellen Eisen, Laura Flores, Dirgha Ghimire, the late Krishna J. Ghimire, Maria-Theresa Hernandez, Drew Hill, Phil Hopewell, Nicholas Jewell, Midori Kato-Maeda, Lee Riley, Kirk Smith, and Nancy Smith for assistance with various aspects of the investigation.
Funding
This work was supported by the National Institute of Environmental Health Sciences of the National Institutes of Health (grant number R01ES019624). The funding source had no involvement in the study design or collection, analysis or interpretation of the data, in the writing of the publication or the decision to submit the article for publication.
Footnotes
The authors declare they have no actual or potential competing financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amegah AK, Quansah R, Jaakkola JJ. 2014. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis of the empirical evidence. PLoS One 9(12): e113920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apte K, Salvi S. 2016. Household air pollution and its effects on health. F1000Res 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu D, Saha R, Ganguly R, Datta A. 2008. Performance improvement of LPG cook stoves through burner and nozzle modifications. Journal of the Energy Institute 81(4): 218–225. [Google Scholar]
- Bates MN, Chandyo RK, Valentiner-Branth P, Pokhrel AK, Mathisen M, Basnet S, et al. 2013. Acute lower respiratory infection in childhood and household fuel use in Bhaktapur, Nepal. Environ Health Perspect 121(5): 637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates MN, Khalakdina A, Pai M, Chang L, Lessa F, Smith KR. 2007. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch Intern Med 167(4): 335–342. [DOI] [PubMed] [Google Scholar]
- Behera D, Aggarwal G. 2010. Domestic cooking fuel exposure and tuberculosis in Indian women. Indian J Chest Dis Allied Sci 52(3): 139–143. [PubMed] [Google Scholar]
- Crampin AC, Glynn JR, Floyd S, Malema SS, Mwinuka VK, Ngwira BM, et al. 2004. Tuberculosis and gender: exploring the patterns in a case control study in Malawi. Int J Tuberc Lung Dis 8(2): 194–203. [PubMed] [Google Scholar]
- Dhanaraj B, Papanna MK, Adinarayanan S, Vedachalam C, Sundaram V, Shanmugam S, et al. 2015. Prevalence and risk factors for adult pulmonary tuberculosis in a metropolitan city of South India. PLoS One 10(4): e0124260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esmail H, Barry CE 3rd, Young DB, Wilkinson RJ 2014. The ongoing challenge of latent tuberculosis. Philos Trans R Soc Lond B Biol Sci 369(1645): 20130437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Sancho MC, Garcia-Garcia L, Baez-Saldana R, Ponce-De-Leon A, Sifuentes-Osornio J, Bobadilla-Delvalle M, et al. 2009. Indoor pollution as an occupational risk factor for tuberculosis among women: a population-based, gender oriented, case-control study in Southern Mexico. Rev Invest Clin 61(5): 392–398. [PubMed] [Google Scholar]
- GBD Tuberculosis Collaborators. 2017. The global burden of tuberculosis: results from the Global Burden of Disease Study 2015. Lancet Infect Dis. 18(3):261–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getahun H, Harrington M, O’Brien R, Nunn P. 2007. Diagnosis of smear-negative pulmonary tuberculosis in people with HIV infection or AIDS in resource-constrained settings: informing urgent policy changes. Lancet 369(9578): 2042–2049. [DOI] [PubMed] [Google Scholar]
- Gninafon M, Ade G, Ait-Khaled N, Enarson DA, Chiang CY. 2011. Exposure to combustion of solid fuel and tuberculosis: a matched case-control study. Eur Respir J 38(1): 132–138. [DOI] [PubMed] [Google Scholar]
- Gordon SB, Bruce NG, Grigg J, Hibberd PL, Kurmi OP, Lam KB, et al. 2014. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med 2(10): 823–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta BN, Mathur N, Mahendra PN, Srivastava AK, Swaroop V, Agnihortri MS. 1997. A study of household environmental risk factors pertaining to respiratory diseases. Energy Environ Monitor 13: 61–67. [Google Scholar]
- Hosmer DW, Lemeshow S. 2000. Applied Logistic Regression. Second ed. New York: John Wiley & Sons, Inc. [Google Scholar]
- Jose G, Javier M-G, Ambuj S, Kirk RS. 2018. Household air pollution, health, and climate change: cleaning the air. Environmental Research Letters 13(3): 030201. [Google Scholar]
- Kan X, Chiang CY, Enarson DA, Chen W, Yang J, Chen G. 2011. Indoor solid fuel use and tuberculosis in China: a matched case-control study. BMC Public Health 11: 498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolappan C, Subramani R. 2009. Association between biomass fuel and pulmonary tuberculosis: a nested case-control study. Thorax 64(8): 705–708. [DOI] [PubMed] [Google Scholar]
- Kurmi OP, Sadhra CS, Ayres JG, Sadhra SS. 2014. Tuberculosis risk from exposure to solid fuel smoke: a systematic review and meta-analysis. J Epidemiol Community Health 68(12): 1112–1118. [DOI] [PubMed] [Google Scholar]
- Lakshmi PV, Virdi NK, Thakur JS, Smith KR, Bates MN, Kumar R. 2012. Biomass fuel and risk of tuberculosis: a case-control study from Northern India. J Epidemiol Community Health 66(5): 457–461. [DOI] [PubMed] [Google Scholar]
- Lin HH, Ezzati M, Murray M. 2007. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med 4(1): e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin HH, Suk CW, Lo HL, Huang RY, Enarson DA, Chiang CY. 2014. Indoor air pollution from solid fuel and tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung Dis 18(5): 613–621. [DOI] [PubMed] [Google Scholar]
- Mills E 2005. The Specter of Fuel-Based Lighting. Science 308(5726): 1263–1264. [DOI] [PubMed] [Google Scholar]
- Mishra VK, Retherford RD, Smith KR. 1999. Cooking with biomass fuels increases the risk of tuberculosis. Natl Fam Health Surv Bull(13): 1–4. [PubMed] [Google Scholar]
- Mortimer K, Gordon SB, Jindal SK, Accinelli RA, Balmes J, Martin WJ 2nd. 2012. Household air pollution is a major avoidable risk factor for cardiorespiratory disease. Chest 142(5): 1308–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxlade O, Murray M. 2012. Tuberculosis and poverty: why are the poor at greater risk in India? PLoS One 7(11): e47533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai M, Rodrigues C. 2015. Management of latent tuberculosis infection: An evidence-based approach. Lung India 32(3): 205–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Padilla R, Perez-Guzman C, Baez-Saldana R, Torres-Cruz A. 2001. Cooking with biomass stoves and tuberculosis: a case control study. Int J Tuberc Lung Dis 5(5): 441–447. [PubMed] [Google Scholar]
- Pokhrel AK, Bates MN, Verma SC, Joshi HS, Sreeramareddy CT, Smith KR. 2010. Tuberculosis and Indoor Biomass and Kerosene Use in Nepal: 
A Case–Control Study. Environ Health Perspect 118(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabbani U, Sahito A, Nafees AA, Kazi A, Fatmi Z. 2017. Pulmonary Tuberculosis Is Associated With Biomass Fuel Use Among Rural Women in Pakistan: An Age- and Residence-Matched Case-Control Study. Asia Pac J Public Health 29(3): 211–218. [DOI] [PubMed] [Google Scholar]
- Rylance J, Fullerton DG, Scriven J, Aljurayyan AN, Mzinza D, Barrett S, et al. 2015. Household air pollution causes dose-dependent inflammation and altered phagocytosis in human macrophages. Am J Respir Cell Mol Biol 52(5): 584–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saksena S, Singh P, Prasad RK, Prasad R, Malhotra P, Joshi V, et al. 2003. Exposure of infants to outdoor and indoor air pollution in low-income urban areas [mdash] a case study of Delhi. J Expo Anal Environ Epidemiol 13(3): 219–230. [DOI] [PubMed] [Google Scholar]
- Sarkar M, Srinivasa, Madabhavi I, Kumar K 2017. Tuberculosis associated chronic obstructive pulmonary disease. Clin Respir J 11(3): 285–295. [DOI] [PubMed] [Google Scholar]
- Semple S, Devakumar D, Fullerton DG, Thorne PS, Metwali N, Costello A, et al. 2010. Airborne endotoxin concentrations in homes burning biomass fuel. Environ Health Perspect 118(7): 988–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen G, Gaddam CK, Ebersviller SM, Vander Wal RL, Williams C, Faircloth JW, et al. 2017. A Laboratory Comparison of Emission Factors, Number Size Distributions, and Morphology of Ultrafine Particles from 11 Different Household Cookstove-Fuel Systems. Environ Sci Technol 51(11): 6522–6532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shetty N, Shemko M, Vaz M, D’Souza G. 2006. An epidemiological evaluation of risk factors for tuberculosis in South India: a matched case control study. Int J Tuberc Lung Dis 10(1): 80–86. [PubMed] [Google Scholar]
- Surendra KC, Takara D, Hashimoto AG, Khanal SK. 2014. Biogas as a sustainable energy source for developing countries: Opportunities and challenges. Renewable and Sustainable Energy Reviews 31: 846–859. [Google Scholar]
- Verver S, Warren RM, Beyers N, Richardson M, van der Spuy GD, Borgdorff MW, et al. 2005. Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med 171(12): 1430–1435. [DOI] [PubMed] [Google Scholar]
- West SK, Bates MN, Lee JS, Schaumberg DA, Lee DJ, Adair-Rohani H, et al. 2013. Is household air pollution a risk factor for eye disease? Int J Environ Res Public Health 10(11): 5378–5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. 2014. WHO Indoor Air Quality Guidelines: Household Fuel Combustion. 2015/01/13 ed. Geneva: Switzerland. [PubMed]
- Woldesemayat EM, Datiko DG, Lindtjorn B. 2014. Use of biomass fuel in households is not a risk factor for pulmonary tuberculosis in South Ethiopia. Int J Tuberc Lung Dis 18(1): 67–72. [DOI] [PubMed] [Google Scholar]