Abstract
BACKGROUND:
This report details the cost effectiveness of a non-nurse patient navigation (PN) program that was implemented at the University of Chicago Medical Center to increase colonoscopy-based colorectal cancer (CRC) screening.
METHODS:
The authors investigated the impact of the PN intervention by collecting process measures. Individuals who received navigation were compared with a historic cohort of non-navigated patients. In addition, a previously validated data-collection instrument was tailored and used to collect all costs related to developing, implementing, and administering the program; and the incremental cost per patient successfully navigated (the cost of the intervention divided by the change in the number who complete screening) was calculated.
RESULTS:
The screening colonoscopy completion rate was 85.1% among those who were selected to receive PN compared with 74.3% when no navigation was implemented. With navigation, the proportion of no-shows was 8.2% compared with 15.4% of a historic cohort of non-navigated patients. Because the perceived risk of noncompletion was greater among those who received PN (previous no-show or cancellation, poor bowel preparation) than that in the historic cohort, a scenario analysis was performed. Assuming no-show rates between 0% and 50% and using a navigated rate of 85%, the total incremental program cost per patient successfully navigated ranged from $148 to $359, whereas the incremental intervention-only implementation cost ranged from $88 to $215.
CONCLUSIONS:
The current findings indicate that non-nurse PN can increase colonoscopy completion, and this can be achieved at a minimal incremental cost for an insured population at an urban academic medical center.
Keywords: cancer screening, Chicago, cost effectiveness, patient navigation
INTRODUCTION
Individuals between ages 50 and 75 years who comply with colorectal cancer (CRC) screening recommendations could substantially reduce their risk of CRC.1 In 2014, CRC ranked third in cancer incidence among men and women, with a rate of 38.4 per 100,000, and had the second highest mortality rate (14.1 per 100,000) among cancers diagnosed in men and women.2 Although screening for CRC is highly effective, it is underused, with 62.4% of individuals between ages 50 and 75 years having completed guideline-specific screening.3 CRC screening prevalence among racial/ethnic minority groups is even lower and is lowest among the uninsured and those without a usual source of care.3–6
It has been demonstrated that patient navigation (PN) is an effective, evidence-based intervention that reduces barriers to screening.7–9 However, despite the success of PN services in improving both CRC screening and the quality of screening,10 the current payment models do not cover PN services.11 Furthermore, very few studies to date have reported the resource requirements and cost effectiveness of PN interventions.12–14 To develop the business case and determine appropriate payment models for PN services, we need cost and cost-effectiveness studies on a broad spectrum of PN interventions applied across varied patient cohorts and health care settings.
Between 2013 and 2014, the University of Chicago Medical Center (UCMC) participated in a State of Illinois PN program to enhance CRC screening among uninsured Illinois residents. This pilot project suggested that PN was effective in increasing CRC screening and resulted in improved quality indicators compared with non-navigated patients.15,16 In 2015, the UCMC was funded as a Centers for Disease Control and Prevention Colorectal Cancer Control Program grantee, supporting the opportunity to implement an onsite UCMC, non-nurse–facilitated PN program in August 2016. Non-nurse PN could offer a less expensive approach to implementing navigation for the successful completion of CRC screening than a nurse-based navigation program. The current study was designed to assess the effectiveness of a non-nurse PN intervention in increasing colonoscopy completion and to evaluate the cost effectiveness of this intervention at an urban academic medical center serving primarily racial/ethnic minority groups. It is noteworthy that the PN intervention was implemented within the real-world practice at the UCMC; therefore, challenges and facilitators of the introduction of the PN services can be identified, and lessons learned can be shared with other implementation teams.
MATERIALS AND METHODS
Patient Navigation Intervention
We present findings from an observational study of a patient-navigated CRC screening colonoscopy program at UCMC between August 2016 and April 2017. UCMC is located on the Southside of Chicago, with a catchment area of 95 square miles that includes 34 of Chicago’s 77 community areas and 1 of the nation’s largest, contiguous, urban, African American communities. The University of Chicago Institutional Review Board approved the study protocol.
UCMC operates a state-of-the-art gastroenterology (GI) unit that performs approximately 12,000 endoscopic procedures each year. Approximately 65% of patients are referred from the University of Chicago primary care clinic, and the remainder include referrals from the GI clinic and open-access, nonuniversity patients. Most referrals are processed through an electronic referral system. There are 15 gastroenterologists performing screening colonoscopies with over 160 procedures performed per week. The GI unit is staffed by a nurse manager, an operations manager, procedure nurses, and technicians. Beginning in July 2016, the UCMC hired and trained 1 non-nurse navigator to address the high number of no-shows and cancellations in the GI procedure unit. Qualifications for the non-nurse navigator position included previous navigation experience, ideally in a specialty care setting; a college education; and residence within the geographic service areas of the hospital. Before initiation of the PN services, all patients received up to 2 GI procedure nurse calls to remind patients of their procedure time and place and to field any questions about the process. After the initiation of PN, patients who were identified as requiring PN services did not continue to receive nurse preprocedure calls.
The UCMC PN program was modeled on the American Cancer Society and the New York City Department of Health and Mental Hygiene’s Colonoscopy Patient Navigator Program.15–17 PN training took place for a 2-month period before initiation of the PN program and focused on the following topics: CRC and CRC screening methods, the follow-up process after a positive fecal test, quality metrics, data management, navigator roles and responsibilities, common patient barriers, communication skills with health care providers and other health professionals, cultural competency, and local community resources. In addition, the navigator had the opportunity to rotate through the colonoscopy suite at the UCMC as part of the patient experience process. The goal of this activity was to create an interactive environment to gain knowledge through direct experience. The navigator met with the GI procedure management staff and faculty directors on a biweekly basis to discuss cases, share information, and address issues associated with their roles and responsibilities.
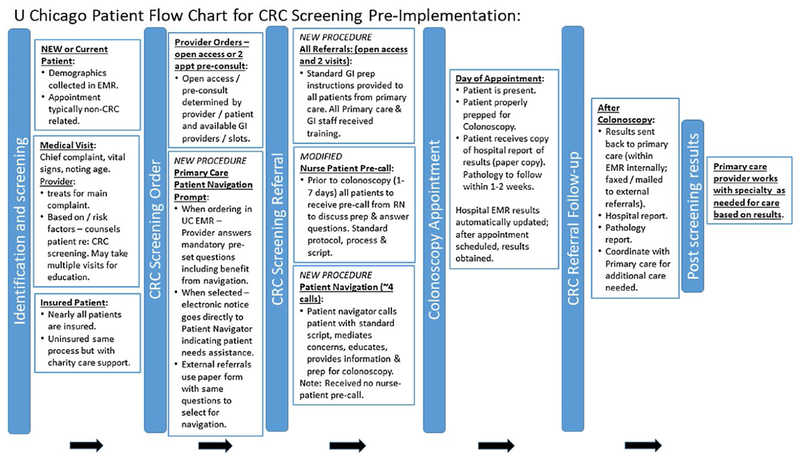
An essential component of the PN program was leveraging the intraorganizational capacity in the GI section. This included GI clinical and primary care coordinators as well as the GI procedure unit staff. PN introduction within the UCMC setting promoted an internal quality-review process, and multiple procedural modifications were implemented to support the PN program. These modifications, including updated bowel preparation instructions, nurse preprocedure calls, data and documentation of PN interactions, integration of PN with existing process, primary care physician referral process, PN management protocol, and primary care physician training and awareness to improve coordination and efficiency, were completed during the preimplementation process (from July 2015 to June 2016). See Fig. 1 for details on changes implemented for the PN program.
Figure 1.
This is a patient flow chart for implementing colorectal cancer (CRC) patient navigation. EMR indicates electronic medical record; GI, gastrointestinal.
All patients between ages 50 and 75 years who underwent a screening colonoscopy between August 2016 and April 2017 were eligible for referral to PN services. Patients with a previous CRC diagnosis, inflammatory bowel disease, or undergoing a diagnostic colonoscopy were excluded from this study. Two provider educational sessions were conducted and included information on the PN program, the process for referral, and the PN prompt. Physicians provided feedback on risk stratification for PN services, and a consensus was reached based on supporting literature and clinical experiences. Given this input, patients who were selected for navigation services included those with a prior history of a no-show, poor bowel preparation, previous cancellation, and/or multiple comorbidities, based on provider assessment. Patients who received PN services were referred by several mechanisms: recommendation by primary care or GI faculty; through prerecorded telephone-based bowel preparation instructions, which allowed patients to self-refer; and identification through a nurse preprocedure call. (Direct referral through an electronic medical record [EMR] PN prompt was initiated in May 2017 and was not evaluated in the current study.) Most patients were referred by physicians. All patients who received PN were contacted 4 times on average to provide the following: introduction to the PN process, basic CRC screening facts, bowel preparation procedures, and support for any barriers identified. Most PN encounters were by telephone, and <5% of patients received face-to-face communication. All encounters were entered and tracked in a password-protected database. Once an encounter was initiated, the patient navigator followed the patient until he or she completed the examination.
Cost-Effective Analysis
We updated and tailored a previously validated cost data-collection instrument to obtain resource use information specific to the development and implementation of the navigation program.18–23 We defined the intervention development period as starting when internal discussions and procedures were initiated to plan the PN program and ending when the implementation began. The intervention implementation period then continued to the end of the last reporting period, April 31, 2017. For both the intervention development and implementation periods, we collected labor and nonlabor resources on tasks related to: administration and management; evaluation, research and reporting; and data quality assessment. For each of these broad categories, we developed a specific list of activities pertinent to the PN program. For example, activities under intervention development included the process of identifying eligible patients, developing tracking forms and databases, and providing staff and navigator training. Implementation activities included recruiting patients, providing navigation, and tracking patients.
Cost data metrics were collected from all staff working on PN implementation through interviews and Excel data sheet inputs. Cost and resource use data collection began in March 2017, with information collected retrospectively from the start of implementation development (July 2015) and prospectively through the end of the reporting period on April 30, 2017. Labor hours were collected retrospectively to minimize staff burden using a previously tested, standardized approach to yield high-quality data.18,19 The project staff were requested to review meeting calendars and other internal reporting systems to identify the hours expended as accurately as possible. We collected salaries and the percentage of time worked to accurately account for part-time employment. Nonlabor costs related to equipment, supplies, and software purchases were catalogued for each activity.
We estimated labor costs by activity using the annual staff salary, the number of hours worked by staff by activity, and the percentage of time staff worked overall. We calculated hourly rates and, using hours spent per activity, calculated the staff cost of each activity. We aggregated all labor and nonlabor costs by activity and then further aggregated the costs into the broad categories of intervention development phase, intervention implementation phase, administration procedures, evaluation, and data quality assessment.
A selected number of PN process and outcome measures were collected. We tracked the number of patients referred for PN through multiple referral sources. We also collected the no-show rate, which was defined as missing the colonoscopy appointment or canceling with 48 hours of the scheduled time. The main outcome to assess the effectiveness of the PN intervention was the number of colonoscopies completed. Data for these measures were obtained from multiple sources, including the UCMC EMR data, patient navigator logs, and GI unit databases, which track patient colonoscopy appointments and the status of scheduled procedures.
Because this was an observational study of PN implementation in a real-world setting (which involved referral of patients for PN services among those likely to fail to complete the screening colonoscopy procedure) and was based largely on physicians’ perception of the risk of noncompletion, we did not design the study with a comparison cohort. We compared the navigated patients with a historic cohort of patients from the UCMC who were scheduled to receive screening colonoscopies during the period from January to December 2016 and did not receive any navigation services. Patients in the navigated and non-navigated cohorts were similar in their characteristics. In both cohorts, most patients were women (approximately 60%), African American (approximately 65%), and had private insurance or Medicare (>80%). Because we relied on EMR data for these demographic variables, large proportions of data were missing for these measures, and there may have been other uncontrolled differences.
For both cohorts we present the proportion of no-shows and colonoscopy completions. Because we anticipated that the proportion of patients who would have completed colonoscopies in the navigated cohort (these individuals were specifically selected for navigation because they were not likely to complete the procedure) would have been much lower than of those in the historic cohort who were available for comparison, we performed a scenario analysis. We present scenarios under 4 different levels of completion rates (0%, 25%, 50%, and 75% rates of screening colonoscopy completion) that could have been achieved without navigation services for the cohort referred for services. The patients referred for PN were likely in the range <50%. We present the cost per patient successfully navigated, which is the incremental cost of the PN intervention. The incremental cost per patient successfully navigated is calculated by dividing the cost of the navigation intervention by the additional number of patients who complete colonoscopy screening because of the navigation provided. This intermediate cost-effectiveness measure provides the estimated economic cost of having 1 more patient complete their scheduled colonoscopy among those selected for navigation.
RESULTS
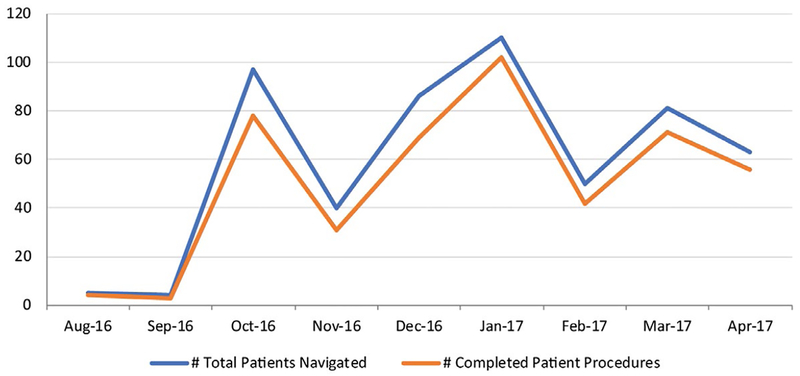
In Fig. 2, we present the total number of patients navigated compared with the total number of completed procedures. PN began in August 2016; and, by October 2016, there had been a substantial increase in patients served (from 5 to 97 patients). Overall, 536 patients were navigated between August 2016 and April 2017.
Figure 2.
The total numbers of patients navigated and completed procedures are illustrated.
There were 536 patients who received navigation and 2713 who did not (Table 1). The completion rate was significantly higher for patients who were navigated (85.1% vs 73.4%), and the no-show rate was significantly lower for patients who were navigated (8.2% vs 15.4%) compared with patients who were not navigated.
TABLE 1.
Effectiveness of the Patient Navigation Intervention
| Navigationa | ||
|---|---|---|
| Variable | No | Yes |
| No. of patients | 2713 | 536 |
| No. who completed colonoscopy | 1990 | 456 |
| Completion rate, % | 73.4 | 85.1b |
| No-show rate, % | 15.4 | 8.2b |
The cohort of patients who did not receive navigation underwent colonoscopies from January to December 2016. Navigated patients were scheduled for colonoscopies between August 2016 and April 2017.
P < .05.
Total costs of the PN intervention by program category are provided in Table 2. In total, the cost to develop and implement the program was $67,278. The largest costs were attributed to the intervention implementation phase ($40,261), followed by costs for the intervention development phase ($13,728), and administration and management ($6999). The remaining the costs were for evaluation, research, and reporting ($3609) and for data quality assessment ($2680).
TABLE 2.
Total Costs by Program Category
| Program Category | Cost, $ |
|---|---|
| Intervention development phase | 13,727.91 |
| Intervention implementation phase | 40,261.23 |
| Administration and Management | 6999.21 |
| Evaluation, research, reporting | 3609.44 |
| Data, quality, assessment | 2680.25 |
| Total | 67,278.04 |
In Table 3, we present the incremental cost per patient successfully navigated. We also report the incremental cost of a 1% increase in successfully navigated patients. Assuming a 0% to 50% no-show rate and using the navigated rate of 85%, the total cost per patient successfully navigated ranged from $147.54 to $358.62. If we use only the implementation costs (because these costs are expected to continue, whereas other costs are expected to decrease), we calculate that the total cost per patient successfully navigated ranges from $88.29 to $214.61. Because the assumed no-show rate without navigation increases, the total costs and implementation-only costs per successfully navigated patient increase.
TABLE 3.
Cost per Patient Navigated
| Incremental Cost Per Patient Successfully Navigated, $ | |||
|---|---|---|---|
| No-Show Rate, % | Navigated Rate, % | Total Cost, $ | Implementation Only, $ |
| 0 | 85 | 147.54 | 88.29 |
| 25 | 85 | 209.20 | 125.19 |
| 50 | 85 | 358.62 | 214.61 |
| 75 | 85 | 1255.19 | 751.14 |
DISCUSSION
Our current results add to the growing body of literature on the efficacy and cost effectiveness of PN services in increasing colonoscopy completion for CRC screening. We report an increase in the overall percentage of completed colonoscopies of almost 11 percentage points among navigated patients compared with patients who did not receive PN (historic controls) within 1 year of initiating the PN program. Our findings are within the range of previously reported increases, from 8 percentage points to 40 percentage points, in studies conducted among low-income populations who received PN services to increase colonoscopy completion.24–26 These studies revealed a large range in the effectiveness of PN programs and likely reflect differences in the populations navigated and the intensity of navigation services.27 It is also important to note that, in our study, only a selected cohort of individuals received navigation; these individuals were referred for PN because they were considered most likely not to complete the colonoscopy procedure as recommended. Thus, the true impact of the navigation program is likely higher, because the projected colonoscopy completion rate among navigated patients was anticipated to be lower than the completion rate among average patients (<73.4% reported before the initiation of navigation).
Moreover, the frequency of no-shows among navigated patients was reduced by >47%, a significant finding given the fixed cost of maintaining endoscopy units.28 Endoscopy units often experience a high rate of no-shows,29,30 which result in idle endoscopy capacity and loss of revenue. Therefore, our PN program may result in significant long-term improvements in both screening prevalence and efficiency gains because endoscopy capacity is used more optimally.
In addition to an overall increase in CRC screening uptake among navigated patients, our current study demonstrates that this increase is balanced by a reasonable incremental cost to support the process. A unique aspect of this study is our analysis of the preimplementation costs associated with the initiation of a new PN program. The total cost includes the steps required to successfully implement a new PN program. These included the total costs to develop and implement the program ($67,278). The largest costs were attributed to the intervention implementation phase, followed by costs for intervention development and administration and management. Other costs included evaluation, research and reporting, and data quality assessment. In contrast to the total cost amount, implementation costs of the PN alone were significantly lower. The additional cost per person screened ranged from $148 to $359 based on the finding that 0% to 50% of those navigated otherwise would have failed to show up for their appointment, as reported. In contrast, the implementation cost of PN alone is significantly more cost effective, ranging from $88 to $215 per successfully navigated patient; we anticipate that a large portion of the costs not directly related with PN patient interaction will reduce substantially in the future because the high start-up and on-the-job training and supervision costs will no longer be incurred. We plan to continue to monitor the cost of the PN activities to track potential efficiencies after the initial 9-month period of implementation reported here. In this study, we relied on providers to identify patients for navigation based on specific criteria, including a history of poor bowel preparation, multiple comorbidities, and a requirement for assistance because of low literacy. On the basis of lessons learned from this study, we will be testing a direct referral system using an EMR PN prompt.
Our current findings support a generally favorable balance between the cost of PN and the increase in screening uptake compared with other similar studies. Because there is no specific benchmark for the intermediate cost-effectiveness measure reported in this study, we offer a comparison with other estimates reported in the peer-reviewed literature. In a nonrandomized evaluation comparing PN implementation in public hospitals, the PN program cost varied from $50 to $300 per patient referred to a navigator, and incremental cost-effectiveness varied from $200 to $700 per additional procedure completed.14 Another study that used a randomized design to evaluate navigated interventions to increase CRC screening in the primary care setting estimated that the average cost per patient ranged from $167 to $289, and the cost per additional patient screened ranged from $906 to $1958.13
Our study does have several limitations. First, our results are from a single academic medical center. However, we report findings across a large urban center with a high percentage of insured patients providing data, which may inform a broader population-based approach to navigation services. This is particularly important because >50% of those who remain unscreened are insured.31 Second, we included no-show rates in our analysis, and it is possible that other mitigating strategies may have influenced our findings, such as comorbidities and quality of bowel preparation. Third, we used a historic comparison cohort. This cohort may not have been an appropriate comparison population, as the navigated cohort was specifically referred for PN services because they were unlikely to complete the colonoscopy procedure. We used scenario analysis in an attempt to evaluate the likely true impact of the PN program. Fourth, before the implementation of the PN services, several process changes were implemented to support the PN navigation activities. Although these changes impacted both the control and navigated groups, these changes also may have contributed to the improvements in the colonoscopy completion rates. Finally, we collected cost data retrospectively, and staff relied on individual recall to determine the specific time allocated to planning and implementing PN services. We believe this resulted in minimal bias, because the recall period for implementation was within 12 months, the UCMC received technical support to maintain good resource use records, and the process for labor and nonlabor data collection was consistent with other reported methodological approaches for assessing cost.18–23,32
These results support the finding that PN can increase colonoscopy completion and can significantly reduce no-shows. A direct implication of this finding is that endoscopy suites can increase their revenue if no-show rates are reduced and providers are able to use the available facilities optimally to perform colonoscopies that result in additional reimbursement. This can serve as an incentive to fund and implement PN interventions because, currently, there is no direct reimbursement for navigation services. Furthermore, our study indicates that PN services in an urban academic medical center can be implemented at a reasonable additional cost per individual screened. Finally, there are important policy implications supported by this study. Serious consideration should be given to formalizing the reimbursement of PN services to enhance CRC screening uptake as we shift away from pay for performance to a value-based model for population health that rewards outcomes.
Acknowledgments
FUNDING SUPPORT
Support for this study was provided by the Centers for Disease Control and Prevention to RTI International (contract 200-2014-61263 Task 4) and to the Center for Asian Health Equity (grant 5NU58DP006079-03-0).
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the Division of Cancer Prevention and Control.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:2564–2575. [DOI] [PubMed] [Google Scholar]
- 2.US Cancer Statistics Working Group. United States Cancer Statistics: 1999–2014 Incidence and Mortality Web-Based Report. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2017. https://www.cdc.gov/uscs. Accessed January 4, 2018. [Google Scholar]
- 3.White A, Thompson TD, White MC, et al. Cancer screening test use—United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.List DT, Baker DW. Understanding current racial/ethnic disparities in colorectal cancer screening in the United States: the contribution of socioeconomic status and access to care. Am J Prev Med. 2014;46:228–236. [DOI] [PubMed] [Google Scholar]
- 5.Gupta S, Tong L, Allison JE, et al. Screening for colorectal cancer in a safety-net health care system: access to care is critical and has implications for screening policy. Cancer Epidemiol Biomarkers Prev. 2009;18:2373–2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klabunde CN, Cronin KA, Breen N, Waldron WR, Ambs AH, Nadel MR. Trends in colorectal cancer test use among vulnerable populations in the United States. Cancer Epidemiol Biomarkers Prev. 2011;20:1611–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf L. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008;100:278–284. [DOI] [PubMed] [Google Scholar]
- 8.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized controlled trial. J Gen Intern Med. 2009;24:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma GX, Shive S, Tan Y, et al. Community-based colorectal cancer intervention in underserved Korean Americans. Cancer Epidemiol. 2009;33:381–386. [DOI] [PubMed] [Google Scholar]
- 10.Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2014;109:1528–1545. [DOI] [PubMed] [Google Scholar]
- 11.Jandorf L, Stossel LM, Cooperman JL, et al. Cost analysis of a patient navigation system to increase screening colonoscopy adherence among urban minorities. Cancer. 2013;119:612–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ladabaum U, Mannalithara A, Jandorf L, Itzkowitz SH. Cost-effectiveness of patient navigation to increase adherence with screening colonoscopy among minority individuals. Cancer. 2015;121:1088–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lairson DR, Dicarlo M, Deshmuk AA, et al. Cost-effectiveness of a standard intervention versus a navigated intervention on colorectal cancer screening use in primary care. Cancer. 2014;120:1042–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elkin EB, Shapiro E, Snow JG, Zauber AG, Krauskopf MS. The economic impact of a patient navigator program to increase screening colonoscopy. Cancer. 2012;118:5982–5988. [DOI] [PubMed] [Google Scholar]
- 15.Naylor K, Fritz C, Polite B, Kim K. Evaluating screening colonoscopy quality in an uninsured urban population following patient navigation. Prev Med Rep. 2017;5:194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fritz C, Naylor K, Kim K. Knowledge of polyp history and recommended follow-up among a predominately African American patient population and the impact of patient navigation. J Racial Ethn Health Disparities. 2016;3:403–412. [DOI] [PubMed] [Google Scholar]
- 17.Lebwohl B, Neugut AI, Stavsky E, et al. Effect of a patient navigator program on the volume and quality of colonoscopy. J Clin Gastroenterol. 2011;45:e47–e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Subramanian S, Tangka FK, Hoover S, et al. Costs of planning and implementing the CDC’s Colorectal Cancer Screening Demonstration Program. Cancer. 2013;119(suppl 15):2855–2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subramanian S, Tangka FK, Hoover S, DeGroff A, Royalty J, Seeff LC. Clinical and programmatic costs of implementing colorectal cancer screening: evaluation of 5 programs. Eval Program Plann. 2011;34:147–153. [DOI] [PubMed] [Google Scholar]
- 20.Subramanian S, Tangka FKL, Hoover S, Royalty J, DeGroff A, Joseph D. Costs of colorectal cancer screening provision in CDC’s Colorectal Cancer Control Program: comparisons of colonoscopy and FOBT/FIT based screening. Eval Program Plann. 2017;62:73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tangka FK, Subramanian S, Bapat B, et al. Cost of starting colorectal cancer screening programs: results from 5 federally funded demonstration programs [serial online]. Prev Chronic Dis. 2008;5:A47. [PMC free article] [PubMed] [Google Scholar]
- 22.Tangka FK, Subramanian S, Beebe MC, Hoover S, Royalty J, Seeff LC. Clinical costs of colorectal cancer screening in 5 federally funded demonstration programs. Cancer. 2013;119(suppl 15):2863–2869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tangka FKL, Subramanian S, Hoover S, et al. Costs of promoting cancer screening: evidence from CDC’s Colorectal Cancer Control Program (CRCCP). Eval Program Plann. 2017;62:67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeGroff A, Schroy PC 3rd, Morrissey KG, et al. Patient navigation for colonoscopy completion: results of an RCT. Am J Prev Med. 2017;53:363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reuland DS, Brenner AT, Hoffman R, et al. Effect of combined patient decision aid and patient navigation vs usual care for colorectal cancer screening in a vulnerable patient population: a randomized clinical trial. JAMA Intern Med. 2017;177:967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen LA, Santos S, Jandorf L, et al. A program to enhance completion of screening colonoscopy among urban minorities. Clin Gastroenterol Hepatol. 2008;6:443–450. [DOI] [PubMed] [Google Scholar]
- 27.Jean-Pierre P, Hendren S, Fiscella K, et al. Understanding the processes of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. J Cancer Educ. 2011;26:111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berg BP, Murr M, Chermak D, et al. Estimating the cost of no-shows and evaluating the effects of mitigation strategies. Med Decis Making. 2013;33:976–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tibble JA, Forgacs I, Bjarnason I, Przemioslo R. The effects of a pre-assessment clinic on nonattendance rates for day-case colonoscopy. Endoscopy. 2000;32:963–965. [DOI] [PubMed] [Google Scholar]
- 30.Adams LA, Pawlik J, Forbes GM. Nonattendance at outpatient endoscopy. Endoscopy. 2004;36:402–404. [DOI] [PubMed] [Google Scholar]
- 31.Shires DA, Divine G, Schum M, et al. Colorectal cancer screening use among insured primary care patients. Am J Manag Care. 2011;17:480–488. [PubMed] [Google Scholar]
- 32.Subramanian S, Ekwueme DU, Gardner JG, Trogdon J. Developing and testing a cost-assessment tool for cancer screening programs. Am J Prev Med. 2009;37:242–247. [DOI] [PubMed] [Google Scholar]