Abstract
BACKGROUND:
The objective of this study was to evaluate an ongoing initiative to improve colorectal cancer (CRC) screening uptake in the New York State (NYS) Medicaid managed care population.
METHODS:
Patients aged 50 to 75 years who were not up to date with CRC screening and resided in 2 NYS regions were randomly assigned to 1 of 3 cohorts: no mailed reminder, mailed reminder, and mailed reminder + incentive (in the form of a $25 cash card). Screening prevalence and the costs of the intervention were summarized.
RESULTS:
In total, 7123 individuals in the Adirondack Region and 10,943 in the Central Region (including the Syracuse metropolitan area) were included. Screening prevalence in the Adirondack Region was 7.2% in the mailed reminder + incentive cohort, 7.0% in the mailed reminder cohort, and 5.8% in the no mailed reminder cohort. In the Central Region, screening prevalence was 7.2% in the mailed reminder cohort, 6.9% in the mailed reminder + incentive cohort, and 6.5% in the no mailed reminder cohort. The cost of implementing interventions in the Central Region was approximately 53% lower than in the Adirondack Region.
CONCLUSIONS:
Screening uptake was low and did not differ significantly across the 2 regions or within the 3 cohorts. The incentive payment and mailed reminder did not appear to be effective in increasing CRC screening. The total cost of implementation was lower in the Central Region because of efficiencies generated from lessons learned during the first round of implementation in the Adirondack Region. More varied multicomponent interventions may be required to facilitate the completion of CRC screening among Medicaid beneficiaries.
INTRODUCTION
Of the approximately 6.1 million New York State (NYS) residents covered by Medicaid, approximately 4.7 million (77%) are enrolled in Medicaid Managed Care (MMC) (Byun C, personal communication). The NYS MMC program is a mandatory program operating under a 1115 waiver granted by the Centers for Medicare and Medicaid Services. With the exception of those who are eligible for both Medicare and Medicaid, and select populations who are institutionalized, very few Medicaid patients are excluded from mandatory MMC, making it 1 of the largest and most demo-graphically diverse programs in the country. The NYS MMC program has a comprehensive benefit package to meet the many health care needs of the covered population, including a focus on preventive care and screening.
It has been demonstrated that colorectal cancer (CRC) screening substantially reduces CRC mortality, and it is recommended for all individuals aged 50 to 75 years.1 In 2015, the CRC screening rate among the NYS MMC population was 61%, versus 63% for the commercial health maintenance organization population.2,3 Both rates are below the Healthy People 2020 goal of 70.5% and below the self-reported NYS population rate of 70.5%.4,5
Because 4 of every 10 MMC patients are not up to date with CRC screening, the NYS Department of Health (NYSDOH), building on past successful collaborations with managed care organizations (MCOs) to better understand patient-specific barriers to cancer screening and communicate findings to MCO staff and providers, sought to promote CRC screening among this population. In June 2015, the NYSDOH successfully competed for support from the Centers for Disease Control and Prevention’s (CDC) Colorectal Cancer Control Program to implement evidence-based interventions (eg, provider reminders, patient reminders) and supporting activities (eg, patient navigation and small media) as recommended by the Community Preventive Services Task Force.6 The NYSDOH focused its efforts on mailing reminder letters about CRC screening to MMC patients and randomly assigned a cohort of these patients to receive letters containing the offer of a $25 incentive (in the form of a cash card) for the completion of CRC screening. Because the Community Preventive Services Task Force has determined that there is insufficient evidence regarding the effectiveness of client incentives in the promotion of CRC screening, we sought to measure the effect of incentives in the MMC population.6 Partnering MCOs mailed notifications to providers to inform them of project activities and encourage them to recommend CRC screening to their patients.
In this report, we describe CRC screening promotion activities that were completed in 2016 among intervention cohorts residing in 2 different regions of NYS. The impact on screening prevalence and the associated costs are presented.
MATERIALS AND METHODS
Given the size of the NYS MMC population and the desire to reach as many patients as possible, CRC screening promotion focused on relatively low-cost patient reminder letters. In addition, the effectiveness of offering a $25 incentive for completion of CRC screening was evaluated among a sample of MMC patients. MMC patients could choose fecal occult blood tests, sigmoidoscopies, or colonoscopies in discussion with their providers. An ancillary Medicaid provider outreach activity, as described below (see Provider Outreach), was designed to inform providers of all patients who were identified as not up to date with CRC screening about project activities and to provide a brief review of CRC screening test options. Provider outreach preceded the patient-level interventions but was not included in the cost analysis.
Target Demographic/Region
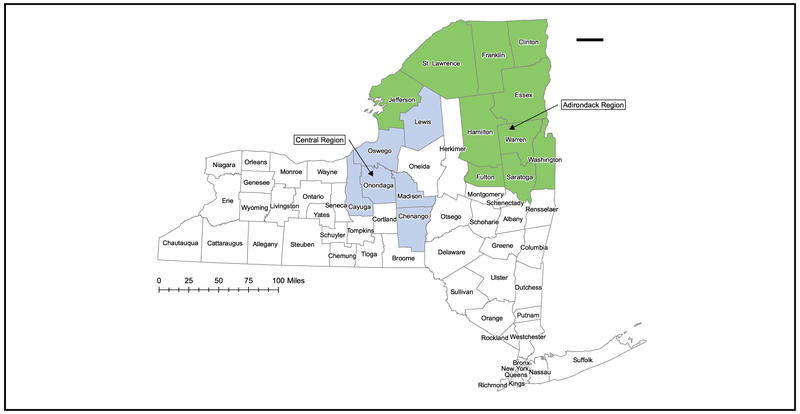
The Adirondack Region, located in the northeastern corner of NYS (Fig. 1), has multiple Medically Underserved Population designations and Health Professional Shortage Area designations for primary care, mental health, and dental services.7 This region was selected as the focus of round 1 activities because of its high proportion of age-eligible MMC patients, its population size (large enough to evaluate the effectiveness of patient reminders, but not so large that a significant proportion would be excluded from outreach because of the limited resources available for the intervention), and because MMC enrollment in this region is concentrated in 2 MCOs, which simplifies collaboration. Round 2 of the project focused on a second priority region in Central NYS that borders the Adirondack Region to the west and an additional (third) MCO serving that region. The Central Region was selected for its low screening rates, for its geographic proximity to the Adirondack Region, and to test the effectiveness of patient reminders and incentives in the urban setting of Syracuse, New York.
Figure 1.
This is a map of the Adirondack and Central Regions of New York State.
Managed Care Organization Partners
MCOs were included early on as key partners for several reasons. MCOs have a unique understanding of regional health systems, including the providers with whom they contract to provide CRC screening and their knowledge of patient-level barriers to care, including those that exist for patients living in rural NYS areas. Quality-improvement staff from partnering MCOs attended biweekly conference calls with the NYSDOH, provided feedback on patient reminders and incentives, and conducted provider outreach activities.
Provider Outreach
Panel data, which are submitted quarterly by MCOs to the NYSDOH, crosswalk MMC patients to their assigned primary care providers (PCPs). The NYSDOH used these data to identify the assigned PCP for each MMC patient who was in need of CRC screening. Lists of identified providers were shared with partner MCOs, which then collaborated to ensure that providers common to 2 or more MCOs received only 1 letter. Letters were printed on MCO letterhead and signed by the medical director at each MCO. Before mailing patient reminder letters, the MCOs sent letters to 592 PCPs in the Adirondack Region and 689 PCPs in the Central Region informing them of the CRC project, advising them that patient reminders were being sent to a subset of their patients, and encouraging them to continue to act as strong advocates for screening. Letters were sent to all identified PCPs regardless of the cohort assignment of their patients, as described below (see Patient Selection and Assignment). A version of the letter also was sent to 126 colonoscopists in the Adirondack Region and 119 colonoscopists in the Central Region.
Patient Selection and Assignment
Medicaid enrollment, claims, and encounter data were used to identify patients aged 50 to 75 years residing in the priority regions who were not up to date with CRC screening according to Healthcare Effectiveness Data and Information Set (HEDIS) CRC measure specifications.2 In addition, according to HEDIS CRC exclusion criteria, any patient who had a CRC diagnosis or who underwent total colectomy was not included in any of our outreach cohorts. Patients who were dually eligible for both Medicaid and Medicare were excluded from outreach, because Medicare is the primary payer of CRC screenings for these patients, and project staff do not have access to Medicare claims data. Eligible patients were clustered by reported address of residence (household), and a single stage cluster sampling was performed to assign them to 1 of 3 cohorts: no-mailed reminder, mailed reminder, or mailed reminder + incentive (Table 1). The size of each cohort was determined by available resources (informational brochures and funding for the cost of mailings and incentives). If 2 or more eligible patients shared the reported address of residence (household), then they were assigned to the same cohort. Chi-square tests were conducted to ensure that the random assignment of patients resulted in similar proportions of key demographic variables in each cohort.
TABLE 1.
Medicaid Patient Cohorts: Adirondack and Central New York State Regions, 2016-2017
| Patient Cohort, Reminder | Region, No. (%) |
||
|---|---|---|---|
| Intervention Received | Adirondack | Central | |
| No mailed | Usual care (Medicaid coverage of screenings and transportation); provider outreach | 1123 (15.8) | 2861 (26.1) |
| Mailed | Usual care, postal reminder and brochure; provider outreacha | 4000 (56.2) | 4582 (41.9)b |
| Mailed + incentive | Usual care, postal reminder, brochure, and offer of $25 for completed screening; provider outreacha | 2000 (28.1) | 3500 (32.0) |
The Centers for Disease Control and Prevention brochure Screen for Life was used in the Adirondack Region, and the NY State brochure Get the Facts About Colon Cancer was used in the Central Region.
Eighty-two patients with the same address were excluded from the random assignment and included in the mailed reminder cohort.
Patient Outreach and Data Monitoring
Customized patient reminders on NYSDOH letterhead were mailed to MMC patients in the mailed reminder and mailed reminder + incentive cohorts. Each letter referenced the patient’s MCO, provided information about CRC and the benefits of screening, and included the assurance that screening was free, as was transportation to most medical services. The language used in the patient reminder did not exceed a fifth-grade reading level, and the information provided used tested messages from the National Colorectal Cancer Roundtable/American Cancer Society’s publication 80% by 2018 Communications Guidebook: Recommended Messaging to Reach the Unscreened.8 The Adirondack Region reminder included the CDC’s Screen for Life brochure, which has since been revised but, at the time of mailing, was the most up-to-date version from 2010.9 Reminders sent to patients in the Central Region included a different brochure, Get the Facts about Colon Cancer,10 which was developed by the NYSDOH in 2016 using the National Colorectal Cancer Roundtable guidebook referenced above. For both regions, the letter to MMC patients in the mailed reminder + incentive cohort offered a $25 incentive for completing screening by a specified date and advised patients to allow at least 12 weeks from the time of screening for delivery of the incentive. Medicaid encounter data were extracted weekly by staff at the NYSDOH to identify screenings, calculate cohort-level screening uptake, and identify patients who earned the $25 incentive. The implementation period in the Adirondack Region was 5 months (from February to June 2016) and, in the Central Region, it was 4 months (from September to December 2016).
Data Collection
Several process measures were collected to track the interventions: the number of patient reminders mailed (including re-mailings), the number of incentives paid, and the number of provider letters mailed. We report screening uptake, defined as the increase in screening during the study timeframe after the interventions were implemented for each region, to evaluate the change in screening prevalence. Screening prevalence was calculated as the number of distinct patients who were screened, as determined by a Current Procedural Terminology or Healthcare Common Procedure Coding System procedure code for a fecal occult blood test, flexible sigmoidoscopy, or colonoscopy (numerator, according to HEDIS specifications), residing in the priority region and enrolled in a partnering MCO at the time of screening, divided by the number of distinct patients eligible for screening (denominator) who were, as of the end of the implementation phase, residents of the priority region and enrolled in a partnering MCO.2
Cost data were collected using a project-specific, Excel-based instrument. The instrument is based on previously published methods of collecting cost data for program evaluation and previously tested and validated approaches to collect resource use and cost data from CRC screening programs.11 The purpose of the instrument was for the NYSDOH and partner MCOs to report data on costs related to the development and implementation of the interventions used in this project. The instrument included data collection on activities related to mailing patient letters, implementing the patient incentives program, and coordinating with MCOs.
The instrument was completed for 2 time periods: 1) for activities related to the implementation of interventions in the Adirondack Region and 2) for activities related to the Central Region. For both time periods, the NYSDOH reported on activities related to intervention development (eg, the process to select interventions), intervention implementation (eg, contacting MMC patients), administration (eg, hiring staff, attending meetings), and evaluation (eg, collecting and reporting data) of the outcome of the interventions.
Details collected in the instrument included annual staff salary, full-time equivalent (FTE) status, and the number of hours staff spent working on each activity. Staff costs were aggregated by activity. Nonlabor costs also were collected related to printing, mailings, and travel. The labor and nonlabor costs were allocated to appropriate activities and aggregated into the project components of intervention development, intervention implementation, administration, and evaluation. We report both the total cost and the FTEs for each project component.
RESULTS
Patient demographics, stratified by region and cohort, are presented in Table 2. In total, 7123 patients in the Adirondack Region and 10,943 in the Central Region (which includes the Syracuse metropolitan area) were included in the initiative. There were no significant differences in demographics by cohort. In both regions and across all cohorts, most patients were women, aged <60 years, white, non-Hispanic, and did not receive Supplemental Security Income (monthly payments paid by the federal government to low-income individuals aged ≥ 65 years or those who are blind or disabled).12 In both regions, the cohorts were nearly evenly divided between those who received cash assistance (state-funded financial support) and those who did not.
TABLE 2.
Patient Demographics by New York State Region and Cohort, 2016-2017a
| Reminder, No. (%) |
||||
|---|---|---|---|---|
| Cohort | No Mailed | Mailed | Mailed + Incentive | P |
| Adirondack region | ||||
| Sample size | 1123 | 4000 | 2000 | |
| Sex | ||||
| Men | 552 (49.2) | 1956 (48.9) | 984 (49.2) | .9719 |
| Women | 571 (50.9) | 2044 (51.1) | 1016 (50.8) | |
| Age, y | ||||
| 50-54 | 501 (44.6) | 1719 (43.0) | 866 (43.3) | .8765 |
| 55-59 | 398 (35.4) | 1450 (36.3) | 713 (35.7) | |
| ≥60 | 224 (20.0) | 831 (20.8) | 421 (21.1) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 967 (86.1) | 3373 (84.3) | 1709 (85.5) | .2486 |
| Other | 156 (13.9) | 627 (15.7) | 291 (14.6) | |
| Medicaid/Medicaid category | ||||
| SSI | 174 (15.5) | 690 (17.3) | 327 (16.4) | .3303 |
| Non-SSI | 949 (84.5) | 3310 (82.8) | 1673 (83.7) | |
| Poverty indicator | ||||
| Cash assistance | 562 (50.0) | 2008 (50.2) | 993 (49.7) | .9224 |
| No cash assistance | 561 (50.0) | 1992 (49.8) | 1007 (50.4) | |
| Central region | ||||
| Sample size | 2861 | 4500 | 3500 | |
| Sex | ||||
| Men | 1391 (48.6) | 2222 (49.4) | 1716 (49.0) | .8165 |
| Women | 1470 (51.4) | 2278 (50.6) | 1784 (51.0) | |
| Age, y | ||||
| 50-54 | 1086 (38.0) | 1709 (38.0) | 1369 (38.1) | .1991 |
| 55-59 | 978 (34.2) | 1599 (35.5) | 1247 (35.6) | |
| ≥60 | 797 (27.9) | 1192 (26.5) | 884 (25.3) | |
| Race/ethnicity | ||||
| White, non-Hispanic | 1972 (68.9) | 3156 (70.1) | 2414 (69.0) | .4197 |
| Other | 889 (31.1) | 1344 (29.9) | 1086 (31.0) | |
| Medicaid/Medicaid category | ||||
| SSI | 563 (19.7) | 973 (21.6) | 703 (20.1) | .0853 |
| Non-SSI | 2298 (80.3) | 3527 (78.4) | 2797 (79.9) | |
| Poverty indicator | ||||
| Cash assistance | 1611 (56.3) | 2568 (57.1) | 1971 (56.3) | .7366 |
| No cash assistance | 1250 (43.7) | 1932 (42.9) | 1529 (43.7) | |
Abbreviations: SSI, Supplemental Security Income.
Source: Analyses of program data.
Other includes black, non-Hispanic, Hispanic, Asian/Pacific Islander, Native American, unknown, missing, biracial, and multiracial patients.
Process measures and the percentage screened by region are presented in Table 3. Overall, 6000 patient reminder letters were mailed in the Adirondack Region, and 8000 were mailed in the Central Region. In both regions, the proportion of patient letters that were resent or undelivered was <7%. After the implementation period, screening prevalence was similar across the 3 cohorts in both the Adirondack and Central Regions. In the Adirondack Region, after the 5-month implementation period, the screening prevalence was 7.2% in the mailed reminder + incentive cohort, 7.0% in the mailed reminder cohort, and 5.8% in the no-mailed reminder cohort. After the 4-month implementation period, Central Region patients in the mailed reminder cohort had a screening prevalence of 7.2%, whereas those in the mailed reminder + incentive cohort had a screening prevalence of 6.9%. Patients who did not receive a mailed reminder or incentive had a prevalence of 6.5%. In neither region were the differences in screening rates between cohorts statistically different.
TABLE 3.
Process Measures and Screening Uptake
| Reminder | No. of Letters |
Numerator, No. Screeneda |
Denominator, No. Eligible for Screeningb |
Percentage Screened | P | ||
|---|---|---|---|---|---|---|---|
| Mailed | Re-Sent | Undelivered | |||||
| Adirondack Region: February to June 2016 | |||||||
| No mailed | — | — | 55 | 946 | 5.8 | .3648 | |
| Mailed | 4000 | 29 | 119 | 235 | 3343 | 7.0 | |
| Mailed + incentive | 2000 | 17 | 57 | 118 | 1645 | 7.2 | |
| Central Region: September to December 2016 | |||||||
| No mailed | — | — | 149 | 2279 | 6.5 | .6647 | |
| Mailed | 4500 | 73 | 210 | 249 | 3480 | 7.2 | |
| Mailed + incentive | 3500 | 51 | 163 | 186 | 2698 | 6.9 | |
The number screened were distinct patients residing in the priority region and enrolled in a partnering managed care organization at the time of screening.
Those eligible for screening were distinct patients who, as of the end of the implementation phase, resided in the priority region and enrolled in a partnering managed care organization.
Total costs of developing and implementing the program by region are provided in Table 4. The Adirondack Region had a total cost of $176,005, including both partners (NYSDOH and MCOs), ranging from $15,753 for implementation activities to $86,224 for administration and management activities. Activities in the Central Region had a total cost of $82,521. Costs in the Central Region ranged from $11,983 for evaluation and reporting activities to $28,215 for activities during the development phase. The implementation cost included incentive payments ($25 per eligible patient) in both regions. In the Adirondack Region, 118 gift cards were provided for a total of $3416.10, including a $3.95 processing fee for each $25 gift card imposed by the bank and paid by the NYSDOH. In the Central Region, 186 incentives were paid at a cost of $5384.70. The total cost per incentive provided was $47.48 in the Adirondack Region and $32.28 in the Central Region, a difference of 32% because of the lower cost of processing and mailing the incentives.
TABLE 4.
Total Cost and Full Time Equivalents by Category and New York State Region
| Variable | Region |
Difference | Percentage Decrease | |
|---|---|---|---|---|
| Adirondack: February to June 2016 |
Central: September to December 2016 |
|||
| Total cost by category, $ | ||||
| Intervention development phase | 52,154 | 28,215 | (23,939) | 45.9 |
| Intervention implementation phase | 15,753 | 14,116 | (1636) | 10.4 |
| Administration and management | 86,224 | 28,206 | (58,018) | 67.3 |
| Evaluation and reporting | 21,874 | 11,983 | (9890) | 45.2 |
| Total | 176,005 | 82,521 | (93,484) | 53.1 |
| Incentives, $a | ||||
| Cost of incentivesb | 3416.10 | 5384.70 | 1968.60 | 57.6 |
| Cost of processing and mailing incentives | 2186.65 | 619.19 | (1567.46) | 71.7 |
| Total cost per incentive provided | 47.48 | 32.28 | (15.20) | 32.0 |
| Full-time equivalent by category | ||||
| Intervention development phase | 0.53 | 0.30 | 0.22 | 42.2 |
| Intervention implementation phase | 0.12 | 0.05 | 0.06 | 56.3 |
| Administration and management | 0.68 | 0.24 | 0.44 | 65.1 |
| Evaluation and reporting | 0.18 | 0.10 | 0.07 | 41.8 |
| Total | 1.50 | 0.70 | 0.80 | 53.6 |
These costs were included in intervention implementation phase.
These costs included a $3.95 fee per card.
The total program cost for the Central Region was approximately 53.1% less than that for the Adirondack Region. The largest cost decreases were in administration and management activities (67.3%), followed by intervention development (45.9%), and evaluation and reporting activities (45.2%). There also were differences in FTEs between the 2 regions: the Adirondack Region used 1.50 FTEs compared with 0.70 FTEs in the Central Region, for a difference of 53.6%.
DISCUSSION
The current report presents results from 2 rounds of interventions implemented to increase CRC screening among MMC patients in 2 NYS regions. Our findings indicate that, during the 4-month to 5-month implementation period, screening prevalence increased from 0% at baseline in all study cohorts in both regions. With no patient-level intervention (no mailed reminder, no incentive; ie, usual care), 5.8% of the Adirondack Region cohort underwent screening compared with 6.5% of the Central Region cohort. We observed similar increases in screening uptake, ranging from 0.4% to 1.4% above the usual care cohorts, after the reminder mailings; these differences were not statistically significant. We also observed no consistent positive motivation to undergo screening among those who were offered the $25 incentive. Although our evaluation sought to determine the effectiveness of patient-level interventions, the provider mailings may have contributed to an increase in screening rates that would be expected to be similar across the intervention cohorts and may be an area for future study.
Prior CRC interventions using mailed fecal immunochemical tests and automated and tailored telephone calls in NYS populations have demonstrated increases in screening uptake that range from 6% to 21% during 6 to 18 months of follow-up.13,14 These findings are not directly comparable to the current study because of the differences in the interventions used, follow-up time-frames, and targeted populations. In 1 study involving 3 MMC plans in New York City, cancer screening telephone support by MMC staff, patient education, and support to overcome screening barriers (eg, competing priorities, misconceptions, and worry) resulted in mixed findings among eligible women. The intervention effect varied substantially across the MMC plans, with an absolute difference in screening rates between intervention and usual care ranging from 1% to 14% during the 18-month intervention. Indeed, 2 of the MMC plans did not achieve statistically significant rate increases in the intent-to-treat analysis, which was performed to compare intervention with usual care cohorts.14 Our study cohort in rural upstate NYS comprised of 16 counties, 9 of which had an Urban Influence Code of 5 (“micropolitan adjacent to a small metro area”) or greater (indicating greater rurality), is likely different from cohorts targeted in New York City, because rural individuals may face more barriers related to the availability of services and longer travel times to health centers.15,16
In response to low screening uptake after our initial rounds of mailings, in subsequent mailings to the Adirondack and Central Regions (implementation and evaluation of which are ongoing), changes were made to increase screening outcomes. The project dropped the no-mailed reminder cohort, so all eligible patients were assigned to either the reminder cohort or the reminder + incentive cohort. Both patient and provider communications were edited to more strongly promote screening options; and, in the patient reminder letter, messages were modified to be more actionable rather than just informational (eg, patients were encouraged to, “Make an appointment with your physician to talk about colon cancer testing and the questions below to find out which test is right for you...”). In addition, in the second phase of interventions, a proportion of patients received a reminder telephone call after receipt of the letter. Telephone calls were made to both the reminder cohort and the reminder + incentive cohort. Additional provider outreach activities included an in-person provider education meeting and direct provider outreach detailing efforts delivered by the 3 partner MCOs. In addition, at the tail end of Adirondack Region round 1, and ending just before the second phase of interventions in the Central Region, a statewide mass media campaign promoting CRC screening was underway. We plan to evaluate the impact of these changes to the interventions and implement additional changes to further improve CRC screening uptake in these regions.
The economic evaluation performed in the current study revealed that the cost incurred in round 2 (Central Region) was much lower than that in round 1 (Adirondack Region). The implementation in round 2 benefitted from the procedures and lessons learned from the implementation of the interventions in round 1. The costs associated with intervention development, administration, and evaluation declined substantially, because these activities are expected to incur high start-up planning costs. Surprisingly, despite the cost reduction, round 2 delivered more mailed reminders than in round 1. Thus, efficiencies can be gained to reduce implementation costs, largely in administering the reminder mailings and patient tracking procedures. Prior studies on the economics of CRC screening programs have highlighted the high start-up costs required to initiate screening promotion interventions, but this is the first study to empirically evaluate the magnitude of the start-up costs. The substantial decrease in cost is important to consider in economic evaluations, because future rounds of intervention implementation are likely to be far less expensive than the initial round of the intervention. Therefore, it is important to consider initial planning or start-up costs when evaluating CRC interventions.
The current study has many strengths, including the availability of high-quality screening uptake data from the NYSDOH Office of Quality and Patient Safety, the collaboration achieved with major MCOs serving the priority regions, and engagement of the MCOs in working to improve CRC screening rates. Despite these strengths, there were limitations to this study. The implementation period during which CRC screenings were assessed may not have been long enough for patients to get screened, especially if they encountered long waiting times in scheduling a colonoscopy. This will be addressed in future rounds of the planned intervention by assessing the long-term impact of the interventions during a 12-month to 18-month period after the patient reminder letters are mailed. The expected wait time of at least 12 weeks for delivery of the incentive, as specified in the patient reminder letter, may have diminished its effectiveness, because previous research indicates that immediate incentives are more effective for promoting healthy behavior.17 In addition, Medicaid data do not include information on screenings that occurred before enrollment in Medicaid (MMC or fee-for-service). However, because the cohorts were randomly assigned, we would expect the proportion of patients with prior screenings to be similar in each of the 3 cohorts. Patient letters were created on NYSDOH letterhead and, although they referenced the member’s MCO by name, were signed by an NYSDOH staff member. It is possible that communications directly from the MCO or from the patient’s PCP would have more impact. MMC patients also are more likely to encounter barriers to screenings, such as low health literacy and limited English language competency, which can affect screening uptake.18,19
Through this CDC-supported initiative, the NYSDOH performed a systematic assessment of patient reminders to increase CRC screening. The phased approach, involving several rounds of interventions in 2 regions, allows lessons learned to be incorporated continuously to improve the implementation of future patient reminder interventions. This process will ensure that optimal, tailored, and cost-effective interventions are adopted to increase CRC screening among MMC patients in NYS.
Acknowledgments
FUNDING SUPPORT
Support for the New York State Department of Health was provided by the Centers for Disease Control and Prevention by a Cooperative Agreement (award 1NU58DP6102). Support for RTI International also was provided by the Centers for Disease Control and Prevention (contract 200-2014-61,263 Task 4, to RTI International).
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315: 2564–2575. [DOI] [PubMed] [Google Scholar]
- 2.National Committee for Quality Assurance (NCQA). HEDIS Technical Specifications. Washington, DC: NCQA; 2014. [Google Scholar]
- 3.New York State Department of Health. eQARR 2014—An Online Report on Quality Performance Results for Health Plans in New York State. Albany, NY: New York State Department of Health; Available at: https://www.health.ny.gov/health_care/managed_care/reports/. Accessed August 3, 2018. [Google Scholar]
- 4.HealthyPeople.gov. 2020 Topics and Objectives: Cancer. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/can-cer/objectives#4054. Accessed June 21, 2017.
- 5.New York State Department of Health. Behavioral Risk Factor Surveillance System (BRFSS) Brief 1702: Colorectal Cancer Screening, New York State Adults, 2015. Albany, NY: New York State Department of Health; 2015. Available at: https://www.health.ny.gov/statistics/brfss/reports/docs/1702_brfss_colorectal_cancer_screening.pdf. Accessed March 5, 2018. [Google Scholar]
- 6.Community Preventive Services Task Force. Cancer Screening: Multicomponent Interventions—Colon Cancer. Atlanta, GA: Community Guide Branch; Division of Public Health Information Dissemination; Center for Surveillance, Epidemiology, and Laboratory Services; Office of Public Health Science Services; Centers for Disease Control and Prevention; 2017. Available at: https://www.thecommunityguide.org/findings/cancer-screening-multicompo-nent-interventions-colorectal-cancer. Accessed June 6, 2017. [Google Scholar]
- 7.Department of Health and Human Services, Health Resources and Services Administration (HRSA). HRSA Data Warehouse: Shortage Areas. Rockville, MD: Department of Health and Human Services, HRSA; 2017. Available at: https://datawarehouse.hrsa.gov/topics/shortageAreas.aspx. Accessed June 30, 2017. [Google Scholar]
- 8.National Colorectal Cancer Roundtable, American Cancer Society. 80% by 2018 Communications Guidebook: Recommended Messaging to Reach the Unscreened. Atlanta, GA: National Colorectal Cancer Roundtable, American Cancer Society; 2017. Available at: https://nccrt.org/tools/80-percent-by-2018/80-by-2018-communications-guidebook/. Accessed June 30, 2017. [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC). Colorectal (Colon) Cancer: Screen for Life Campaign Brochures. Atlanta, GA: CDC; 2017. Available at: https://www.cdc.gov/cancer/colorectal/sfl/publications/brochures.htm. Accessed June 30, 2017. [Google Scholar]
- 10.New York State Department of Health. Get the Facts About Colon Cancer. Albany, NY: New York State Department of Health; Available at: https://www.health.ny.gov/publications/0416.pdf. Accessed June 30, 2017. [Google Scholar]
- 11.Subramanian S, Ekwueme DU, Gardner JG, Trogdon J. Developing and testing a cost-assessment tool for cancer screening programs. Am JPrev Med. 2009;37:242–247. [DOI] [PubMed] [Google Scholar]
- 12.Social Security Administration. Supplemental Security Income (SSI). Publication No. 05–111000. Woodlawn, MD: Social Security Administration; 2017; Available at: https://www.ssa.gov/pubs/EN-05-11000.pdf. Accessed June 30, 2017. [Google Scholar]
- 13.Basch CE, Wolf RL, Brouse CH, et al. Telephone outreach to increase colorectal cancer screening in an urban minority population. Am J Public Health. 2006;96:2246–2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dietrich AJ, Tobin JN, Robinson CM, et al. Telephone outreach to increase colon cancer screening in Medicaid managed care organizations: a randomized controlled trial. Ann Fam Med. 2013;11:335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Economic Research Service, US Department of Agriculture. Urban Influence Codes. Washington, DC: US Department of Agriculture; 2013. Available at: https://www.ers.usda.gov/data-products/ur-ban-influence-codes.aspx. Accessed February 27, 2018. [Google Scholar]
- 16.Gupta S, Sussman DA, Doubeni CA, et al. Challenges and possible solutions to colorectal cancer screening for the underserved [serial online]. J Natl Cancer Inst. 2014;106:dju032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meredith SE, Jarvis BP, Raiff BR, et al. The ABCs of incentive-based treatment in health care: a behavior analytic framework to inform research and practice. Psychol Rese Behav Manag. 2014;7: 103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weiss JM, Smith MA, Pickhardt PJ, et al. Predictors of colorectal cancer screening variation among primary-care providers and clinics. Am J Gastroenterol. 2013;108:1159–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ojinnaka CO, Choi Y, Kum HC, Bolin JN. Predictors of colorectal cancer screening: does rurality play a role? J Rural Health. 2015;31:254–268. [DOI] [PubMed] [Google Scholar]