Abstract
A significant proportion of youth engage in health risk behaviors, which are of concern, as they are associated with adverse health consequences across development. Two factors associated with engagement in such behaviors are emotion dysregulation and impulsivity. Dialectical Behavioral Therapy (DBT) is an effective intervention that enhances emotion regulation skills to reduce problem behaviors among adolescent populations; however limited research has been conducted implementing the program within school settings. The current study was a 9-week DBT skills group conducted among 80 middle school youth, with pre-posttest data among 53 students. Findings indicated feasibility to implement the program in schools and preliminary evidence of efficacy in decreasing youth’s likelihood to engage in risky, particularly among youth high on an emotion-based impulsivity trait. Brief DBT skills group may be an effective program to be utilized by school nurses and health care teams to reduce health risk behaviors among school-aged youth.
Keywords: health risk behaviors, adolescents, Dialectical Behavioral Therapy, schools, school nursing
Significant proportions of youth have tried alcohol, marijuana, and have engaged in sexual intercourse (Kann et al., 2016). Moreover, nearly a third of youth report being in at least one physical fight during the past year (Kann et al., 2016). Engagement in such high-risk behaviors is of concern, as they are associated with the leading causes of death among persons aged 10–24 in the United States (Eaton et al., 2012). Moreover, even experimentation in such behaviors, particularly substance use, during adolescence is of concern, as it is predictive of problematic use and adverse health consequences into adulthood (DeWit, Adlaf, Offord, & Ogborne, 2000; Tucker, Ellickson, Collins, & Klein, 2006). Thus prevention programs are needed to mitigate engagement in such behaviors during adolescence.
Although adolescence is characterized by a normative increase in risk taking behavior, with 80 percent of 11 to 15 year olds exhibiting at least one reckless act within the past month (Maggs et al., 1995), there are some characteristics that place youth at higher risk. Two factors that have garnered much attention are emotion dysregulation and impulsivity. Emotion dyregulation is conceptualized as the inability to modulate one’s emotional state. During adolescence, psychosocial capacities that help with regulating emotions are not fully developed (Larson, Moneta, Richards, & Wilson, 2002; Steinberg, 2007), which increases the likelihood of adolescents engaging in health risk behaviors (Brown, Houck, Lescano, Donenberg, Tolou-Shams, & Mello, 2012; McLaughlin, Hatzenbuehler, Mennin, & Nolen-Hoeksema, 2011; Raffaelli & Crockett, 2003; Tarter, 2002). For example, Hessler and Katz (2010) found that youth with poor emotional regulation had a higher likelihood of using hard drugs, having more sexual partners, and experiencing more behavioral problems.
Impulsivity is a complex construct that can be broadly defined as a disposition to engage in rash action. Over the past few decades, researchers have worked to disaggregate impulsivity into five specific traits (i.e., sensation seeking, lack of planning, lack of perseverance, negative urgency, and positive urgency), that, though associated, differentially predict behavior among youth populations, which has been since been replicated by other researchers (Tomko, Prisciandaro, Falls, & Magid, 2016; Zapolski, Stairs, Settles, Combs, & Smith, 2010). Among such studies, the impact of the emotion-based traits (i.e., negative and positive urgency) has been shown to have the strongest effect on health risk behaviors among adolescents.
Negative and positive urgency can be defined as the tendency to engage in rash acts when experiencing intense negative and positive emotions, respectively. There is strong evidence for elevated risk for engagement in drinking, smoking, marijuana use, and binge eating among youth who exhibit elevations in these emotion-based personality traits (Combs, Spillane, Caudill, Stark, & Smith, 2012; Pearson, Zapolski, & Smith, 2015; Robinson, Ladd, & Anderson, 2014; Zapolski, Cyders, & Smith, 2009; Zapolski et al, 2010). For example, Riley, Rukavina, & Smith (2016) found that urgency predicted subsequent drinking among youth followed from 5th grade to 8th grade. Moreover, Tomko and colleagues (2016) found among treatment seeking adolescent that positive urgency was associated with frequency of binge drinking and negative urgency was associated with marijuana use and substance use problems.
It thus appears important to focus on emotion-based rash action among adolescents. By addressing emotion regulation during adolescence, we may be able to reduce engagement in such health risk behaviors earlier in development, the likelihood of progression to more severe behaviors, and the occurrence of associated negative health outcomes (Eaton et al., 2012; Kann et al., 2016). One of the leading treatments for addressing poor emotion regulation is Dialectical Behavioral Therapy (DBT). DBT is cognitive behavioral treatment program, but differs from traditional cognitive behavioral programs by the inclusion of dialectical philosophy, radical behaviorism, and mindfulness. DBT was originally developed for chronically suicidal adults with Borderline Personality Disorder (BPD), which comprised of a 12-month commitment for individual therapy and concurrent group-based skills training that taught modules on emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness (Linehan, 1993). To date, five randomized controlled trials have been conducted on DBT for BPD. A meta-analysis based on these studies by Panos et al. (2014) found a benefit of DBT compared to treatment as usual in decreasing suicidal attempts. DBT has been adapted for a variety of disorders including substance abuse, depression, and attention-deficit/hyperactivity disorder among adult populations (MacPherson, Cheavens, & Fristad, 2013), as well as self-injurious behavior, oppositional defiant disorder, and externalizing disorders among adolescents (MacPherson et al., 2013). A recent meta-analysis examining the efficacy of DBT for adolescents found a large effect in reducing non-suicidal self-injury and a small effect on depression (Cook & Gorraiz, 2016).
Studies have also documented the efficacy of the DBT skills group as a stand-alone treatment (Chugani, Ghali, & Brunner, 2013; Meaney-Tavares & Hasking, 2013). Blackford and Love (2011) conducted a weekly DBT skills group for a six-month period in a community mental health setting, finding a significant decrease in depression scores, with greater improvements on depression and other outcome variables (i.e., symptom severity, quality of life, and community functioning) based on number of sessions attended. Rizvi and Steffel (2014) conducted a shorter eight-week DBT skills group of the emotion regulation and mindfulness components among college students, finding significant improvements on measures of emotion regulation, positive and negative affect, use of coping skills in daily life, mindfulness skills, and work and social functioning.
To date, only a few studies have examined the use of the DBT skills group among adolescent populations (e.g., Memel, 2012; Nelson-Gray, Keane, Hurst, Mitchell, Warburton, Chok, & Cobb, 2006), with only one conducted in a school setting (Ricard, Lerma, & Heard, 2013). Specifically, Ricard and colleagues (2013) conducted a 4-week skills group among a sample of adolescents attending a Disciplinary Alternative Education Program. Pre-post test comparisons reveals improvements in both student and parent-reported indicators of behavioral distress compared to youth who did not receive the intervention. However, more evidence to support the efficacy of DBT skills groups among adolescent populations in school settings is needed, and is consistent with a recent call from the American Psychological Associations Division of School Psychology requesting 1) more studies documenting the efficacy of DBT as a prevention and treatment tool in school settings, even among youth not diagnosed with a disorder, and 2) further research exploring shorter treatment sequences of the program from the current 1 year program (Fiorillo & Long, 2012).
The aims of this study were to: examine whether (1) a brief 9-week adaptation of DBT could be successfully implemented as a preventative intervention program in a school-based setting for middle-school youth (i.e., ability to recruit participants and administer all sessions of the 9-week program), (2) the program would show evidence of reducing risk for engagement in health risk health behaviors among participants, and (3) this program was particularly effective for youth exhibiting heightened urgency traits, such that decrease in likelihood to engage in health risk behaviors would be stronger for those with high scores on the urgency traits.
Methods
The current study is a one sample pre-post design of a 9-week DBT skills group. Participants were recruited into the study based on referrals from school staff and administration of youth who had been experiencing behavioral or academic problems within the school setting, in order to increase power to detect engagement in risk-taking behaviors and potential changes in behaviors post-intervention. The inclusion criteria for the study were youth who attended the designated school, were currently enrolled 7th or 8th grade, and could read and understand English. There were no exclusion criteria based on psychiatric diagnosis or treatment.
Study participants were 80 students from 4 urban middle schools in the Southeastern United States. Of the 80 participants, 20 did not complete the post-treatment questionnaire due to early dropout (retention rate=75%). Another 7 participants were excluded from analysis due to not completing study measures. The final sample for data analysis was 53 participants. The majority of participants were in 7th grade (64%; mean age = 12.7) and female (51%). Most participants identified themselves as African American (47%), followed by White (42%), Multiracial (9%), and Hispanic (2%). See Figure 1 for flow chart on recruitment and retention.
Figure 1.
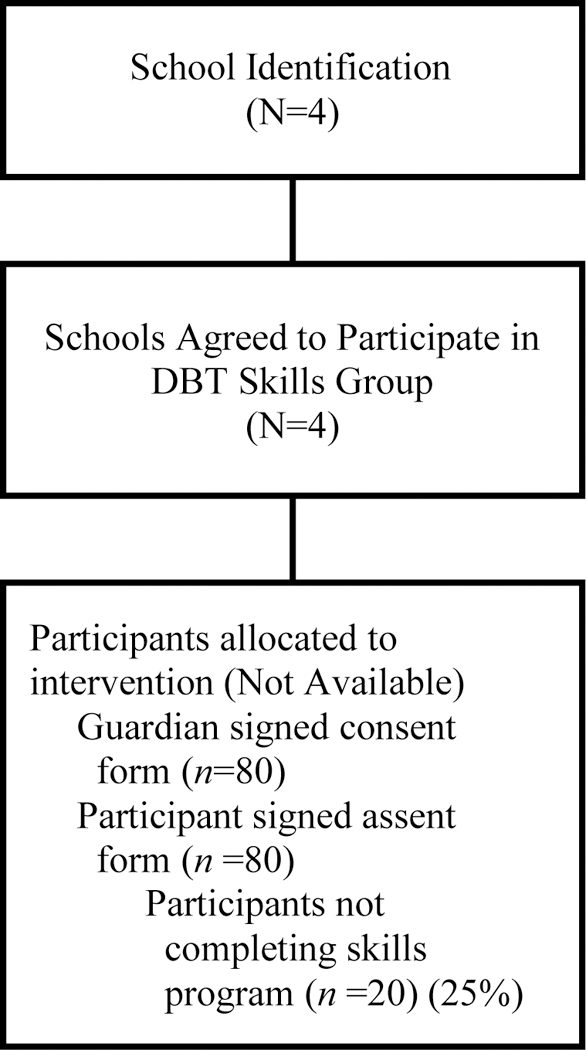
Flow Diagram of Participant Recruitment and Retention.
Procedures.
As approved by the university IRB, participants were recruited through 4 local public middle schools based on referrals from the guidance counselors, staff, and administration at the school. All participants were be told that the group would address factors that hinder reaching goals, such as stress, anger, sadness, and interpersonal difficulties, and will teach participants skills on how to manage those factors. A description of the group and a consent form was sent home to the guardians of the child participants by the school administration on behalf of the research team. The guardians were required to return a signed consent to the school administration or guidance counselor prior to the first day of the group in order for the student to be eligible to participate. The student also received information about the group and signed an assent form.
Each skills group consisted of 5–10 students with a mixture of boys and girls, co-led by two clinical psychology doctoral students who were trained by a licensed psychologist with intensive professional training in DBT. Sessions occurred during school hours, primarily during elective class periods, and were located on school campus in an unoccupied classroom or conference room. The program lasted for nine weeks, with one session a week. Each session ran for approximately 45 minutes (the length of a class period) and included a review of homework from the previous session, presentation of new material, in-session activities related to the topic, and assignment of homework for the following session. Session topics corresponded with the DBT modules on emotion regulation, distress tolerance, and interpersonal skills (see Table 1 for more details on content for each session). The content of the groups followed closely to that of the original manual (Linehan, 1993), but was modified to provide examples that were developmentally appropriate for school-aged youth. To measure efficacy of the program, participants completed pre-post measures assessing the urgency traits, lifetime engagement in risky behaviors, and intentions to engage in risky behaviors at the first and final group session.
Table 1.
| Session | DBT Module Adaptation |
Activities |
|---|---|---|
| Session 1: Introduction and Pre- Treatment Assessment |
||
| Session 2: Understanding Emotions | Emotion Regulation | Model for observing and describing emotions |
| Session 3: Reducing Vulnerability to Extreme Emotions |
Emotion Regulation | PLEASE Master: importance of taking care of your body |
| Session 4: Managing Emotions/Opposite Action |
Emotion Regulation | Opposite action skills: how to change or reduce intensity of emotions |
| Session 5: Review Session | ||
| Session 6: Distress Tolerance/Relaxation |
Distress Tolerance | Self talk, self-soothe, use of distractions, relaxation skills |
| Session 7: Perspective Taking, Problem Solving, & Pros/Cons |
Interpersonal Effectiveness |
Perspective taking, STEPS skills for problem solving, pros/Cons list |
| Session 8: Application of Skills to Real-Life Problems |
Interpersonal Effectiveness |
Asking for what you need, handling disagreements, dealing with peer pressure |
| Session 9: Review Session and Post- Treatment Assessment |
Measures
Demographic Measure.
A series of demographic questions where included to assess the participant’s age, year in school, race/ethnicity, and gender.
The UPPS-P-Child Version (UPPS-P-C; Zapolski et al., 2010).
The UPPS-P-C is a 40-item Likert-type scale self-report measure designed to assess five impulsivity-related traits (negative urgency, lack of planning, lack of perseverance, sensation seeking, and positive urgency). Items are rated from 1 (not at all like me) to 4 (very much like me). Scale scores were calculated as the sum of item responses, with higher scores indicating more impulsive tendencies. For the current study, we were only interested in examining the moderating effect of the emotion-based impulsivity traits, negative and positive urgency, on the program outcome variables. Thus, only those trait scales were included in the study analyses. Consistent with past work, the two scales appear to be internally consistent (α = .78 and .92 for negative and positive urgency, respectively).
Mood-Based Questionnaire (MBQ-C; Zapolski et al., 2010).
The MBQ-C is a self-report measure that assesses lifetime endorsement and current likelihood to engage in 24 risky behaviors while being in either an unusually negative mood or an unusually positive mood. Lifetime endorsement is measured on a dichotomous, yes-no scale. Likelihood to engage in in risky behaviors is measured on a 5-point Likert scale, with 1 (not at all), 3 (maybe) and 5 (will definitely try). Behaviors assessed on the measure include drank alcohol, broke the law, smoked a cigarette or cigar, kissed someone romantically, urinated outside, shoplifted, started a fight, trespassed, cheated on a test, disobeyed your parent. In previous research with adolescents, good evidence was reported for the MBQ-C’s reliability and validity (Zapolski et al., 2010). In the current sample, there was good internal consistency (negative: α = .86-.89; positive: α = .85-.92).
Data Analysis
Approximately 1 percent of the data among the 53 participants was missing. Little’s MCAR analysis was conducted with a non-significant effect, indicating that data in our sample was missing at random. Data were imputed using multiple imputation (Buuren & Groothuis-Oudshoorn, 2011) on pre and post scale items for the urgency traits and intentions to engage in risky behaviors. A majority of these participants (91%) had three or fewer missing data points. All subsequent analyses were performed using SPSS 23.0. Correlations were conducted between the urgency traits, baseline risk-taking behavior, and baseline intentions to engage in risky behavior. To examine the effect of the intervention on intentions to engage in risky behavior paired t-tests were conducted. To examine whether changes in intentions to engage in risky behavior based on pre and post-treatment assessment were stronger for youth higher on the urgency traits, Pearson correlations and linear regression analysis were conducted.
Results
Consistent with previous studies, most youth reported engaging in risky behaviors (mean = 5). The types of behaviors engaged in did vary based on mood state. Approximately half of youth reported breaking/throwing something, starting a fight, and disobeying their parent/teacher while in an extremely negative mood. Moreover, nearly one-third of youth reported hurting themselves/someone else and one-quarter reported trespassing or cheating on a test/homework due to a negative mood. As for positive mood, approximately half of youth reported that they had kissed someone romantically and ate a large amount of food. One-third of youth had broken or thrown something, did something they normally would not do, and disobeyed their parent/teacher due to being in a positive mood. Also consistent with previous literature, the urgency traits were significantly correlated with pre-treatment measures of lifetime risk-taking (negative urgency (NU): r = 0.43, p < .01; positive urgency (PU): r = 0.49, p < .001) and likelihood to engage in risky behaviors (NU: r = 0.52, p < .001; PU: r = 0.49, p < .001) while in intense negative and positive moods, respectively.
Pre- and post-treatment assessments were compared to examine changes in likelihood to engage in such behaviors due to mood states. There was a significant decrease in intentions to engage in risky behaviors due to positive mood (t(52) = −2.65, p < .01), and marginally significant changes for negative mood (t(52) = −1.59, p = .06). Moreover, an effect based on impulsivity was found, with elevations in negative urgency associated with steeper decreases in the likelihood of engaging in risky behaviors due to negative mood by the end of treatment (r = −0.27, p < .05). This relationship was also significant based on regression analysis (b = −.745, p < .05). See Tables 2 and 3 for complete details.
Table 2.
Descriptive Statistics
| Variable | Mean (SD) |
|---|---|
| Negative Urgency | 2.50 (.69) |
| Positive Urgency | 2.30 (.90) |
| Lifetime Risk-Taking (Negative Mood) | 5.21 (4.53) |
| Lifetime Risk-Taking (Positive Mood) | 4.58 (3.87) |
| Pre-Treatment Intentions for Risk-Taking (Negative Mood) |
1.75 (.64) |
| Pre-Treatment Intentions for Risk-Taking (Positive Mood) |
1.75 (.68) |
| Post-Treatment Intentions for Risk-Taking (Negative Mood) |
1.61 (.56) |
| Post-Treatment Intentions for Risk-Taking (Positive Mood) |
1.52 (.46) |
Table 3.
Relationship between negative urgency and outcome variables
Note: NU: negative urgency; PU: positive urgency; RB_1: pre-treatment risky behavior due to intense negative or positive mood state, respectively; RBI_1: pre-treatment risky behavior intentions due to intense negative or positive mood state, respectively; Δ RBI: change in risky behaviors from pre to post treatment based on negative or positive mood, respectively.
p < .05
p < .01; **p < .001
Discussion
There is robust evidence for DBT as an effective treatment program for a variety of adolescent problem behaviors (MacPherson et al., 2012). Moreover, studies have documented the efficacy of the DBT skills group as a stand-alone treatment of problem behaviors (Blackford & Love, 2011; Chugani et al., 2013; Meaney-Tavares & Hasking, 2013; Rizvi & Steffel, 2014). However, to date, only one study has been published using the DBT skills modules as a stand-alone program within a school setting. The current pilot study aimed to expand upon this work by providing evidence on the feasibility of conducting a 9-week DBT skills group among middle school youth in a school-based setting and providing preliminary indication of its efficacy at reducing intentions to engage in risky behaviors.
This pilot study provided evidence for the feasibility of implementing the brief DBT skills program in a school setting, as all school administration who were provided information regarding the pilot program agreed to participate. Moreover, we were able to successfully recruit 80 youth to participate in the program and retained 66% throughout the 9 weeks of the intervention. It is possible that the timing of the intervention was related to drop out of some participants, as the end of the nine weeks was toward the end of each school semester. Moreover, we were able to document preliminary evidence on the efficacy of the program to reduce the likelihood of engagement in risk-taking behaviors among middle school students. Study findings also suggest that though the program can be useful for all youth, it can be particularly beneficial for high-risk youth who exhibit elevations in negative urgency. Although the association between negative urgency and changes in risk was significant, the effect was weak in magnitude. It is possible that a stronger effect may be observed with a larger sample size.
Study limitations should be noted. Given that the current study was a pilot, the lack of a control group provides threats to internal validity, limiting interpretation that reductions in risk was due to participation in the intervention. Additionally, recruitment was based on referral by school staff and we did not assess participant’s diagnostic history or history of treatment. Obtaining such information would be beneficial to assess the impact of the intervention for a particular subgroup of youth, as well as the impact of the intervention above prior treatment exposure. Lastly, changes in emotion regulation skills and reduction in health risk behaviors were not assessed. Inclusion of such measures would allow for the assessment of mechanisms within the intervention to reduce risk-taking and specific behavioral outcomes.
In sum, implementing prevention programs, such as DBT, in school-based setting, is critical as it provides the opportunity to reach youth at earlier stages of risk, thus reducing the likelihood of progression to more severe behaviors and diagnosable levels of dysfunction. School nurses are particularly well suited to deliver such services, given their role within schools in promoting adaptive health behaviors. School nurses provide important resources to students, such as preventive and screening services, health education, and intervention programming (Broussard, 2004; Council of School Health, 2008; Krause-Parello & Samms, 2010; National Association of School Nurses, 2016). Moreover, there is strong evidence to support the role of nurses in the areas of smoking cessation (Pbert et al., 2011), reducing obesity (Gellar, Druker, Osganian, Gapinski, LaPelle, & Pbert, 2012), and teaching health curricula more broadly (Krause-Parello & Samms, 2010) within school settings. Thus, it is plausible to extend upon this work to interventions focused on emotion regulation as an indicated intervention for at-risk youth or provided as part of health curricula, which can be coordinated by school nurses and delivered alongside teachers or collaboratively with school health service teams (Broussard, 2004; Council on School Health, 2008; Denehy, 2004). Training and consultation for DBT skills group could also be obtained through collaborations with trained local health professionals or by attending workshops provided by the Linehan Institute.
References
- Blackford JU, & Love R (2011). Dialectical behavior therapy group skills training in a community mental health setting: A pilot study. International Journal of Group Psychotherapy, 61(4), 645–57. doi:http://dx.doi.org.proxy.ulib.uits.iu.edu/101521ijgp2011614645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broussard L (2004). School Nursing: Not Just Band‐Aids Any More!. Journal for Specialists in Pediatric Nursing, 9(3), 77–83. [DOI] [PubMed] [Google Scholar]
- Brown LK, Houck C, Lescano C, Donenberg G, Tolou-Shams M, & Mello J (2012). Affect regulation and HIV risk among youth in therapeutic schools. AIDS and Behavior, 16(8), 2272–2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buuren S, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. Retrieved from http://www.jstatsoft.org/v45/i03/. [Google Scholar]
- Chugani CD, Ghali MN, & Brunner J (2013). Effectiveness of short term dialectical behavior therapy skills training in college students with cluster B personality disorders. Journal of College Student Psychotherapy, 27(4), 323–336. [Google Scholar]
- Combs JL, Spillane NS, Caudill L, Stark B, & Smith GT (2012). The acquired preparedness risk model applied to smoking in 5th grade children. Addictive Behaviors, 37(3), 331–334. doi:10.1016/j.addbeh.2011.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook NE, & Gorraiz M (2016). Dialectical behavior therapy for nonsuicidal self‐injury and depression among adolescents: Preliminary meta‐analytic evidence. Child And Adolescent Mental Health, 21(2), 81–89. doi:10.1111/camh.12112 [DOI] [PubMed] [Google Scholar]
- Council of School Health. (2008). Role of the school nurse in providing school health services. Pediatrics, 121(5), 1052–1056. doi: 10.1542/peds.2008-0382 [DOI] [PubMed] [Google Scholar]
- Denehy J (2001). Health education: An important role for school nurses. The Journal of School Nursing, 17(5), 233–238. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, & Ogborne AC (2000). Age at first alcohol use: A risk factor for the development of alcohol disorders. American Journal of Psychiatry, 157(5), 745–750. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, … & Wechsler H (2012). Youth risk behavior surveillance-United States, 2011. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, DC: 2002), 61(4), 1–162. [PubMed] [Google Scholar]
- Fiorillo J, & Long J (2012). Dialectical behavior therapy skills groups in schools: A review of empirical findings. From Science to Practice July 2012 Retrieved from http://www.apadivisions.org/division-16/publications/newsletters/science/2012/07/empirical-findings.aspx.
- Gellar L, Druker S, Osganian SK, Gapinski MA, LaPelle N, & Pbert L (2012). Exploratory research to design a school nurse-delivered intervention to treat adolescent overweight and obesity. Journal of Nutrition Education and Behavior, 44(1), 46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessler DM, & Katz LF (2010). Brief report: Associations between emotional competence and adolescent risky behavior. Journal of Adolescence, 33(1), 241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, et al. (2016). Youth Risk Behavior Surveillance — United States, 2015. Morbidity and Mortality Weekly Report, 65(No. SS-6), 1–174. DOI: http://dx.doi.org/10.15585/mmwr.ss6506a1 [DOI] [PubMed] [Google Scholar]
- Krause‐Parello CA, & Samms K (2010). School nurses in New Jersey: A quantitative inquiry on roles and responsibilities. Journal for Specialists in Pediatric Nursing, 15(3), 217–222. [DOI] [PubMed] [Google Scholar]
- Larson RW, Moneta G, Richards MH, & Wilson S (2002). Continuity, stability, and change in daily emotional experience across adolescence. Child Development, 1151–1165. Retrieved from http://www.jstor.org/stable/3696277 [DOI] [PubMed]
- Linehan M (1993). Cognitive-behavioral treatment of borderline personality disorder Guilford Press: New York, NY. [Google Scholar]
- MacPherson HA, Cheavens JS, & Fristad MA (2013). Dialectical behavior therapy for adolescents: Theory, treatment adaptations, and empirical outcomes. Clinical Child and Family Psychology Review, 16(1), 59–80. [DOI] [PubMed] [Google Scholar]
- Maggs JL, Almeida DM, & Galambos NL (1995). Risky business: The paradoxical meaning of problem behavior for young adolescents. Journal of Early Adolescence, 15, 344–362. [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, & Nolen-Hoeksema S (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy, 49(9), 544–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaney-Tavares R, & Hasking P (2013). Coping and regulating emotions: A pilot study of a modified dialectical behavior therapy group delivered in a college counseling service. Journal of American College Health, 61(5), 303–309. [DOI] [PubMed] [Google Scholar]
- Memel B (2012). A quality improvement project to decrease the length of stay on a psychiatric adolescent partial hospital program. Journal Of Child And Adolescent Psychiatric Nursing, 25(4), 207–218. doi:10.1111/jcap.12005 [DOI] [PubMed] [Google Scholar]
- National Association of School Nurses. (2016). The role of the 21st century school nurse (Position Statement). Silver Spring, MD: Author [Google Scholar]
- Nelson-Gray RO, Keane SP, Hurst RM, Mitchell JT, Warburton JB, Chok JT, & Cobb AR (2006). A modified DBT skills training program for oppositional defiant adolescents: Promising preliminary findings. Behaviour Research and Therapy, 44(12), 1811–1820. doi:10.1016/j.brat.2006.01.004 [DOI] [PubMed] [Google Scholar]
- Panos PT, Jackson JW, Hasan O, & Panos A (2014). Meta-analysis and systematic review assessing the efficacy of dialectical behavior therapy (DBT). Research on Social Work Practice, 1049731513503047. [DOI] [PMC free article] [PubMed]
- Pearson CM, Zapolski TC, & Smith GT (2015). A longitudinal test of impulsivity and depression pathways to early binge eating onset. International Journal Of Eating Disorders, 48(2), 230–237. doi:10.1002/eat.22277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pbert L, Druker S, DiFranza JR, Gorak D, Reed G, Magner R, … & Osganian S (2011). Effectiveness of a school nurse–delivered smoking-cessation intervention for adolescents. Pediatrics, 128, 926–936. doi:10.1542/peds.2011-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffaelli M, & Crockett LJ (2003). Sexual risk taking in adolescence: the role of self-regulation and attraction to risk. Developmental Psychology, 39(6), 1036–1046. [DOI] [PubMed] [Google Scholar]
- Ricard RJ, Lerma E, & Heard CC (2013). Piloting a dialectical behavioral therapy (DBT) infused skills group in a disciplinary alternative education program (DAEP). The Journal for Specialists in Group Work, 38(4), 285–306. [Google Scholar]
- Riley EN, Rukavina M, & Smith GT (2016). The reciprocal predictive relationship between high-risk personality and drinking: An 8-wave longitudinal study in early adolescents. Journal of Abnormal Psychology, 125(6), 798–804. doi:10.1037/abn0000189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, & Steffel LM (2014). A pilot study of 2 brief forms of dialectical behavior therapy skills training for emotion dysregulation in college students. Journal Of American College Health, 62(6), 434–439. doi:10.1080/07448481.2014.907298 [DOI] [PubMed] [Google Scholar]
- Robinson JM, Ladd BO, & Anderson KG (2014). When you see it, let it be: Urgency, mindfulness and adolescent substance use. Addictive Behaviors, 39(6), 1038–1041. doi:10.1016/j.addbeh.2014.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence new perspectives from brain and behavioral science. Current Directions in Psychological Science, 16(2), 55–59. [Google Scholar]
- Tarter RE (2002). Etiology of adolescent substance abuse: A developmental perspective. The American Journal on Addictions, 11(3), 171–191. [DOI] [PubMed] [Google Scholar]
- Tomko RL, Prisciandaro JJ, Falls SK, & Magid V (2016). The structure of the UPPS-R-Child impulsivity scale and its relations with substance use outcomes among treatment-seeking adolescents. Drug And Alcohol Dependence, 161276–283. doi:10.1016/j.drugalcdep.2016.02.010 [DOI] [PMC free article] [PubMed]
- Tucker JS, Ellickson PL, Collins RL, & Klein DJ (2006). Are drug experimenters better adjusted than abstainers and users?: a longitudinal study of adolescent marijuana use. Journal of Adolescent Health, 39(4), 488–494. doi:10.1016/j.jadohealth.2006.03.012 [DOI] [PubMed] [Google Scholar]
- Zapolski TCB, Cyders MA, & Smith GT (2009). Positive urgency predicts illegal drug use and risky sexual behavior. Psychology of Addictive Behaviors, 23, 348–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TC, Stairs AM, Settles RF, Combs JL, & Smith GT (2010). The measurement of dispositions to rash action in children. Assessment, 17(1), 116–125. [DOI] [PMC free article] [PubMed] [Google Scholar]


