Abstract
With the accelerated aging of human society Alzheimer’s disease (AD) has become one of the most threatening diseases in the elderly. However, there is no efficient therapeutic agent to combat AD. Berberine is a natural isoquinoline alkaloid that possesses a wide range of pharmacological effects. In the present paper, we review the multiple activities of berberine, including antioxidant, acetylcholinesterase and butyrylcholinesterase inhibitory, monoamine oxidase inhibitory, amyloid-b peptide level-reducing and cholesterol-lowering activities, which suggest that berberine may act as a promising multipotent agent to combat AD.
Keywords: Alzheimer’s disease, berberine, multipotent agent
1. Introduction
As the most common form of dementia, Alzheimer’s disease (AD) has been one of the most threatening diseases in the elderly with the accelerated aging of human society [1,2,3,4]. Multiple factors have been recognized to be implicated in the pathogenesis of AD, which provide diverse targets, including oxidative stress, acetylcholinesterase enzyme (AChE), butyrylcholinesterase (BChE), monoamine oxidase (MAO), amyloid-b peptide (Ab) aggregation, etc. [5,6,7,8,9,10], to screen drugs to treat this disease. Although much effort has been devoted to the anti-AD drug discovery in recent years, there are no efficient therapeutic agents for AD at present.
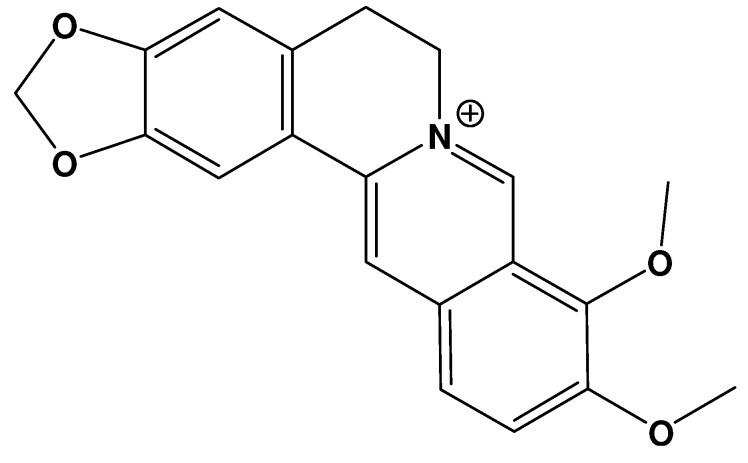
Berberine (Figure 1) is a natural isoquinoline alkaloid isolated from the Chinese herb Rhizoma coptidis, which has been widely used in Chinese herbal medicine. Berberine has gained much attention in recent years owing to its multiple biochemical and pharmacological effects, including anticancer, antiviral, and antibacterial activities [11,12,13,14,15,16]. Accumulating evidences indicate that berberine also possesses potential to treat AD [17,18]. For instance, it was demonstrated that intragastric administration of berberine (50 mg/kg) once daily for 14 days significantly ameliorated the spatial memory impairment in the rat model of AD [18]. In the present review, it is suggested that berberine may act as a promising multipotent agent to combat AD on the basis of the natural product’s multiple activities, such as antioxidant, AChE and BChE inhibitory, MAO inhibitory, Ab level-reducing and cholesterol-lowering activities.
Figure 1.
Molecular structure of berberine.
2. Antioxidant Activity
It has been widely recognized that oxidative damage plays an important role in the pathogenesis of AD [5,19,20,21,22]. Cellular oxidative stress and/or nitrosative stress, including augmentation of protein oxidation, protein nitration, glycoloxidation, and lipid peroxidation are involved in AD pathogenesis [5,19,20,21,22]. The antioxidant activity of berberine has been widely demonstrated [17,23,24,25,26,27,28]. First, it was reported that berberine can scavenge reactive oxygen species (ROS) and reactive nitrogen species (RNS) [17,23,24,25,26,27]. For instance, among the RNS, peroxynitrites (ONOO−) generated through the reaction between nitric oxide (NO·) and superoxide anion radical in vivo has been implicated in Aβ formation and accumulation. Previous studies showed that berberine can scavenge both NO·and ONOO− [17,25]. Secondly, berberine can inhibit lipid peroxidation and show protective effects against low-density lipoprotein (LDL) oxidation [23,27,28]. In addition, it was found that berberine can also bind catalyzing metal ions, which can reduce the concentration of metal ions in lipid peroxidation [28].
3. AChE and BChE Inhibitory Activity
AChE is mainly present in the central nervous system and its principle role is to catalyze the hydrolysis of the neurotransmitter acetylcholine (ACh) to choline. This process can return an activated cholinergic neuron to its resting state. The pathogenesis of AD is linked to a deficiency in the brain ACh [6]. Thus, AChE is an important pathogenic factor of AD and most pharmacological study to screen agent to combat AD has focused on AChE inhibitors to alleviate cholinergic deficit and improve neurotransmission [6,29]. In addition, BChE also plays an important role in the aetiology and disease progression of AD beyond regulation of synaptic ACh levels [30]. It has been found that Aβ neurotoxicity is amplified when BChE is added to Aβ in tissue culture [31]. Gene studies found a potential allelic link between K-variant of BChE (BChE-K) and development AD [32]. These findings support a potential therapeutic role for BChE inhibition in AD.
Many studies proved that berberine exerts inhibitory effect against AChE [17,33,34,35,36,37]. Jung and co-workers reported that berberine can inhibit AChE with an IC50 of 0.44 μM [17] and a close value of 0.58 μM and 0.37 μM was reported by Ingkaninan et al. [34] and Huang et al. [37], respectively. Xiang et al. have explored the molecular mechanisms underlying the inhibition of berberine with AChE [38]. They proposed that the binding of berberine to AChE is principally driven by a favorable entropy increase and the inhibition of AChE with berberine consists of the main contributions of interaction as well as minor conformation change of AChE induced by berberine [38]. In addition, berberine is also found to be a BChE inhibitor and the corresponding IC50 was estimated to be 3.44 μM [17]. Thus, berberine acts as dual inhibitors of AChE and BChE.
4. MAO Inhibitory Activity
There are two isoforms of MAO in humans, designated as MAO-A and MAO-B. MAO-A inhibitors have been proven to be effective antidepressantn, while MAO-B inhibitors are potential agents to combat neurodegenerative diseases, including AD and Parkinson’s disease [39]. The mechanisms underlying the neuroprotective effects in AD of MAO-B inhibitors have been reviewed by Riederer et al. [40]. Berberine has been demonstrated to inhibit both MAO-A and MAO-B [41,42,43,44]. Berberine is reported to exhibit inhibitory activity on MAO-A with an IC50 value of 126 μM [41]. The inhibitory effect of berberine against MAO-B has also been observed [42,44]. Castillo and coworkers reported the IC50 for the inhibition of berberine against MAO-B using benzylamine (substrate) method and direct fluorescence method, and the IC50 was estimated to be 98.4 μM and 90 μM, respectively [44]. These values are in agreement with that obtained by Lee et al., 98.2 μM [42].
5. Aβ Level-Reducing Activity
The accumulation and aggregation of Ab is a central event in the pathogenesis of AD [1,2,3]. Ab is generated from amyloid precursor protein (APP). Therefore, the inhibition of Ab generation should be a promising therapeutic strategy in treating AD. It is interesting to find that berberine can reduce Aβ levels [45]. Asai and coworkers reported that berberine can reduce Aβ levels by altering APP processing in human neuroglioma H4 cells that stably express Swedish-type of APP at the range of berberine concentration (0.1–100 μM) without cellular toxicity [45].
6. Cholesterol-Lowering Activity
Previous epidemiologic study indicated that there is a decreased prevalence of AD associated with the supplement of cholesterol-lowering drugs [46]. Simons et al. investigated how cholesterol might modulate Aβ deposit formation and proposed that decreased neuronal cholesterol levels can inhibit the Aβ-forming amyloidogenic pathway possibly by removing APP from membrane microdomains and reduce the ability of Aβ to act as a seed for further fibril formation [47]. Moreover, Puglielli et al. and Wolozin also reviewed the molecular mechanisms underlying the cholesterol-AD relationship and proposed that cholesterol-lowering drugs have great potential to combat AD [48,49]. Kong et al. found that oral administration of berberine can effectively reduce serum cholesterol and LDL-cholesterol levels in hyperlipidemic hamsters and human hypercholesterolemic patients and the mechanism of cholesterol-lowering action of berberine is different from that of the statin drugs [50].
7. Other Activities
There are other activities of berberine which may be involved in its anti-AD potential. Accumulating evidences indicate diabetes act as a risk factor for AD, most likely associated with an impairment of insulin signaling in the brain [51]. In a recent experiment the diabetes drug liraglutide is proved to prevent key neurodegenerative developments in a mouse model of AD [52]. The efficacy and safety of berberine in the treatment of type 2 diabetes have been reported [53,54], which reinforces the anti-AD potential of berberine. This is further supported by the recently reported beneficial effect of berberine in ameliorating memory dysfunction in a rat model of streptozotocin-induced diabetes [55]. Moreover, glucagon-like peptide-1 (GLP-1) is an endogenous insulinotropic peptide and has been recognized as an attractive agent to treat type 2 diabetes. GLP-1 has been proved to protect neurons from toxic effects and proposed as a novel therapeutic target for intervention in AD [56,57]. Previous studies found that berberine treatment can increase GLP-1 (7–36) amide secretion in streptozotocin-induced diabetic rats [58] and berberine can modulate GLP-1 release as demonstrated both in vivo and in vitro experiments [59]. The effects of berberine on GLP-1 may also contribute its anti-AD potential.
In addition, mitochondria have been found to be central players in mediating neuronal stress relevant to the pathogenesis of AD [60]. Mitochondrial dysfunction and energy deficiency are recognized to be the early feature of AD [60]. The mitochondrial effects of berberine have been investigated [61,62]. Pereira et al. reported the interaction of berberine with mitochondria both in situ and in isolated mitochondrial fractions and found that berberine is accumulated by mitochondria of a mouse melanoma cell line, leading to mitochondrial fragmentation and dysfunction, while in isolated mitochondrial fractions, berberine is toxic to mitochondria [62]. Whether the mitochondrial effect of berberine is beneficial to AD treatment or not needs to be further studied.
8. Conclusions
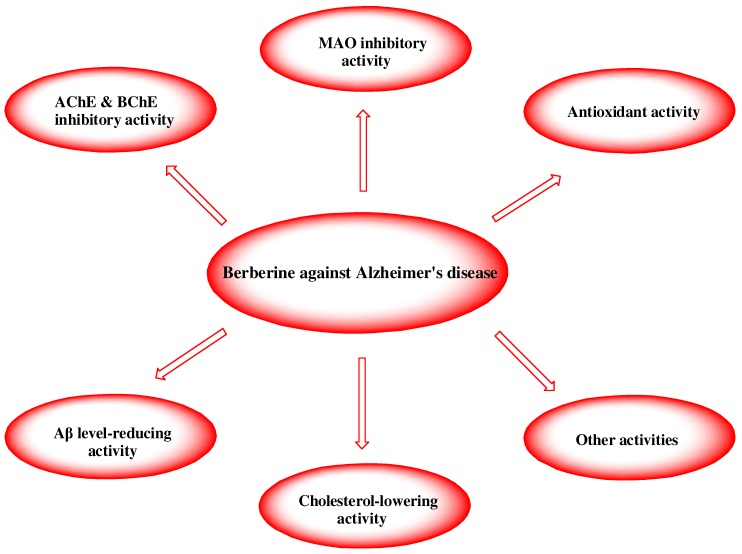
In summary, berberine possesses multiple activities which may be involved in anti-AD potential, including antioxidant activity, AChE and BChE inhibitory activity, MAO inhibitory activity, and its abilities to reduce Aβ level and to lower cholesterol (Figure 2). In addition, there is fruitful information on berberine’s safety profile [63,64]. Berberine is generally considered to be non-toxic at doses used in clinical situations and lacks genotoxic, cytotoxic or mutagenic activity [64,65,66]. Berberine can be administered orally [67] and pass through the blood-brain barrier [68]. Therefore, it is suggested that berberine is a potential multipotent agent to combat AD.
Figure 2.
Potential mechanisms rendering berberine a multiotent agent to combat AD.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 30800184).
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Cummings J.L. Alzheimer’s disease. N. Engl. J. Med. 2004;351:56–67. doi: 10.1056/NEJMra040223. [DOI] [PubMed] [Google Scholar]
- 2.Ballard C., Gauthier S., Corbett A., Brayne C., Aarsland D., Jones E. Alzheimer’s disease. Lancet. 2011;377:1019–1031. doi: 10.1016/S0140-6736(10)61349-9. [DOI] [PubMed] [Google Scholar]
- 3.Blennow K., de Leon M.J., Zetterberg H. Alzheimer’s disease. Lancet. 2006;368:387–403. doi: 10.1016/S0140-6736(06)69113-7. [DOI] [PubMed] [Google Scholar]
- 4.Plassman B.L., Langa K.M., Fisher G.G., Heeringa S.G., Weir D.R., Ofstedal M.B., Burke J.R., Hurd M.D., Potter G.G., Rodgers W.L., et al. Prevalence of dementia in the United States: The aging, demographics, and memory study. Neuroepidemiology. 2007;29:125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnham K.J., Masters C.L., Bush A.I. Neurodegenerative diseases and oxidative stress. Nat. Rev. Drug. Discov. 2004;3:205–214. doi: 10.1038/nrd1330. [DOI] [PubMed] [Google Scholar]
- 6.Muñoz-Torrero D. Acetylcholinesterase inhibitors as disease-modifying therapies for Alzheimer’s disease. Curr. Med. Chem. 2008;15:2433–2455. doi: 10.2174/092986708785909067. [DOI] [PubMed] [Google Scholar]
- 7.Brown D.R., Kozlowski H. Biological inorganic and bioinorganic chemistry of neurodegeneration based on prion and Alzheimer diseases. Dalton Trans. 2004:1907–1917. doi: 10.1039/b401985g. [DOI] [PubMed] [Google Scholar]
- 8.Hardy J., Allsop D. Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends Pharmacol. Sci. 1991;12:383–388. doi: 10.1016/0165-6147(91)90609-V. [DOI] [PubMed] [Google Scholar]
- 9.Hashimoto M., Rockenstein E., Crews L., Masliah E. Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer’s and Parkinson’s diseases. Neuromolecular Med. 2003;4:21–36. doi: 10.1385/NMM:4:1-2:21. [DOI] [PubMed] [Google Scholar]
- 10.Benson A. Alzheimer’s disease: A tangled issue. Drug Discov. Today. 2005;10:749–751. doi: 10.1016/S1359-6446(05)03482-3. [DOI] [PubMed] [Google Scholar]
- 11.Imanshahidi M., Hosseinzadeh H. Pharmacological and therapeutic effects of Berberis vulgaris and its active constituent, berberine. Phytother. Res. 2008;22:999–1012. doi: 10.1002/ptr.2399. [DOI] [PubMed] [Google Scholar]
- 12.Kuo C.L., Chi C.W., Liu T.Y. The anti-inflammatory potential of berberine in vitro and in vivo. Cancer Lett. 2004;203:127–137. doi: 10.1016/j.canlet.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Kettmann V., Kosfálová D., Jantová S., Cernáková M., Drímal J. In vitro cytotoxicity of berberine against HeLa and L1210 cancer cell lines. Pharmazie. 2004;59:548–551. [PubMed] [Google Scholar]
- 14.Stermitz F.R., Lorenz P., Tawara J.N., Zenewicz L.A., Lewis K. Synergy in a medicinal plant: Antimicrobial action of berberine potentiated by 5-methoxyhydrocarpin, a multidrug pump inhibitor. Proc. Natl. Acad. Sci. USA. 2000;97:1433–1437. doi: 10.1073/pnas.030540597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Racková L., Májeková M., Kost'álová D., Stefek M. Antiradical and antioxidant activities of alkaloids isolated from Mahonia aquifoliu. Structural aspects. Bioorg. Med. Chem. 2003;12:4709–4715. doi: 10.1016/j.bmc.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 16.Iwasa K., Kamigauchi M., Ueki M., Taniguchi M. Antibacterial activity and structure-activity relationships of berberine analogs. Eur. J. Med. Chem. 1996;31:469–478. doi: 10.1016/0223-5234(96)85167-1. [DOI] [Google Scholar]
- 17.Jung H.A., Min B.S., Yokozawa T., Lee J.H., Kim Y.S., Choi J.S. Anti-Alzheimer and antioxidant activities of Coptidis Rhizoma alkaloids. Biol. Pharm. Bull. 2009;32:1433–1438. doi: 10.1248/bpb.32.1433. [DOI] [PubMed] [Google Scholar]
- 18.Zhu F., Qian C. Berberine chloride can ameliorate the spatial memory impairment and increase the expression of interleukin-1beta and inducible nitric oxide synthase in the rat model of Alzheimer’s disease. BMC Neurosci. 2006;7:78. doi: 10.1186/1471-2202-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jomova K., Vondrakova D., Lawson M., Valko M. Metals, oxidative stress and neurodegenerative disorders. Mol. Cell Biochem. 2010;345:91–104. doi: 10.1007/s11010-010-0563-x. [DOI] [PubMed] [Google Scholar]
- 20.Markesbery W.R. Oxidative stress hypothesis in Alzheimer’s disease. Free Radic. Biol. Med. 1997;23:134–147. doi: 10.1016/S0891-5849(96)00629-6. [DOI] [PubMed] [Google Scholar]
- 21.Agostinho P., Cunha R.A., Oliveira C. Neuroinflammation, oxidative stress and the pathogenesis of Alzheimer’s disease. Curr. Pharm. Des. 2010;16:2766–2778. doi: 10.2174/138161210793176572. [DOI] [PubMed] [Google Scholar]
- 22.Butterfield D.A., Reed T., Newman S.F., Sultana R. Roles of amyloid beta-peptide-associated oxidative stress and brain protein modifications in the pathogenesis of Alzheimer’s disease and mild cognitive impairment. Free Radic. Biol. Med. 2007;43:658–677. doi: 10.1016/j.freeradbiomed.2007.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Racková L., Májeková M., Kost'álová D., Stefek M. Antiradical and antioxidant activities of alkaloids isolated from Mahonia aquifolium. Structural aspects. Bioorg. Med. Chem. 2004;12:4709–4715. doi: 10.1016/j.bmc.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 24.Yokozawa T., Satoh A., Cho E.J., Kashiwada Y., Ikeshiro Y. Protective role of Coptidis Rhizoma alkaloids against peroxynitrite-induced damage to renal tubular epithelial cells. J. Pharm. Pharmacol. 2005;57:367–374. doi: 10.1211/0022357055470. [DOI] [PubMed] [Google Scholar]
- 25.Yokozawa T., Ishida A., Kashiwada Y., Cho E.J., Kim H.Y., Ikeshiro Y. Coptidis Rhizoma: Protective effects against peroxynitrite-induced oxidative damage and elucidation of its active components. J. Pharm. Pharmacol. 2004;56:547–556. doi: 10.1211/0022357023024. [DOI] [PubMed] [Google Scholar]
- 26.Sarna L.K., Wu N., Hwang S.Y., Siow Y.L., Karmin O. Berberine inhibits NADPH oxidase mediated superoxide anion production in macrophages. Can. J. Physiol. Pharmacol. 2010;88:369–378. doi: 10.1139/Y09-136. [DOI] [PubMed] [Google Scholar]
- 27.Hsieh Y.S., Kuo W.H., Lin T.W., Chang H.R., Lin T.H., Chen P.N., Chu S.C. Protective effects of berberine against low-density lipoprotein (LDL) oxidation and oxidized LDL-induced cytotoxicity on endothelial cells. J. Agric. Food Chem. 2007;55:10437–10445. doi: 10.1021/jf071868c. [DOI] [PubMed] [Google Scholar]
- 28.Shirwaikar A., Shirwaikar A., Rajendran K., Punitha I.S. In vitro antioxidant studies on the benzyl tetra isoquinoline alkaloid berberine. Biol. Pharm. Bull. 2006;29:1906–1910. doi: 10.1248/bpb.29.1906. [DOI] [PubMed] [Google Scholar]
- 29.Scarpini E., Scheltens P., Feldman H. Treatment of Alzheimer’s disease: Current status and new perspectives. Lancet Neurol. 2003;2:539–547. doi: 10.1016/S1474-4422(03)00502-7. [DOI] [PubMed] [Google Scholar]
- 30.Greig N.H., Utsuki T., Yu Q., Zhu X., Holloway H.W., Perry T., Lee B., Ingram D.K., Lahiri D.K. A new therapeutic target in Alzheimer’s disease treatment: Attention to butyrylcholinesterase. Curr. Med. Res. Opin. 2001;17:159–165. doi: 10.1185/0300799039117057. [DOI] [PubMed] [Google Scholar]
- 31.Barber K., Mesulam M.M., Kraft G.A., Klein W.L. Butyrylcholinesterase alters the aggregation state of β-amyloid. Proc. Soc. Neurosci. 1996;72:1172. [Google Scholar]
- 32.Lehmann D., Johnston C., Smith A.D. Synergy between the genes for butyrylcholinesterase K variant apolipoprotein E4 in late-onset confirmed Alzheimer’s disease. Hum. Mol. Genet. 1997;6:933–935. doi: 10.1093/hmg/6.11.1933. [DOI] [PubMed] [Google Scholar]
- 33.Hung T.M., Na M., Dat N.T., Ngoc T.M., Youn U., Kim H.J., Min B.S., Lee J., Bae K. Cholinesterase inhibitory and anti-amnesic activity of alkaloids from Corydalis turtschaninovii. J. Ethnopharmacol. 2008;119:74–80. doi: 10.1016/j.jep.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 34.Ingkaninan K., Phengpa P., Yuenyongsawad S., Khorana N. Acetylcholinesterase inhibitors from Stephania venosa tuber. J. Pharm. Pharmacol. 2006;58:695–700. doi: 10.1211/jpp.58.5.0015. [DOI] [PubMed] [Google Scholar]
- 35.Huang L., Shi A., He F., Li X. Synthesis, biological evaluation, and molecular modeling of berberine derivatives as potent acetylcholinesterase inhibitors. Bioorg. Med. Chem. 2010;18:1244–1251. doi: 10.1016/j.bmc.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 36.Kim D.K., Lee K.T., Baek N.I., Kim S.H., Park H.W., Lim J.P., Shin T.Y., Eom D.O., Yang J.H., Eun J.S. Acetylcholinesterase inhibitors from the aerial parts of Corydalis speciosa. Arch. Pharm. Res. 2004;27:1127–1131. doi: 10.1007/BF02975117. [DOI] [PubMed] [Google Scholar]
- 37.Huang L., Luo Z., He F., Shi A., Qin F., Li X. Berberine derivatives, with substituted amino groups linked at the 9-position, as inhibitors of acetylcholinesterase/butyrylcholinesterase. Bioorg. Med. Chem. Lett. 2010;20:6649–6652. doi: 10.1016/j.bmcl.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 38.Xiang J., Yu C., Yang F. Conformation-activity studies on the interaction of berberine with acetylcholinesterase: Physical chemistry approach. Prog. Nat. Sci. 2009;19:1721–1725. doi: 10.1016/j.pnsc.2009.07.010. [DOI] [Google Scholar]
- 39.Riederer P., Lachenmayer L., Laux G. Clinical applications of MAO-inhibitors. Curr. Med. Chem. 2004;11:2033–2043. doi: 10.2174/0929867043364775. [DOI] [PubMed] [Google Scholar]
- 40.Riederer P., Danielczyk W., Grünblatt E. Monoamine oxidase-B inhibition in Alzheimer’s disease. Neurotoxicology. 2004;25:271–277. doi: 10.1016/S0161-813X(03)00106-2. [DOI] [PubMed] [Google Scholar]
- 41.Kong L.D., Cheng C.H., Tan R.X. Monoamine oxidase inhibitors from rhizoma of Coptis chinensis. Planta Med. 2001;67:74–76. doi: 10.1055/s-2001-10874. [DOI] [PubMed] [Google Scholar]
- 42.Lee S.S., Kai M., Lee M.K. Effects of natural isoquinoline alkaloids on monoamine oxidase activity in mouse brain: Inhibition by berberine and palmatine. Med. Sci. Res. 1999;27:749–751. [Google Scholar]
- 43.Kulkarni S.K., Dhir A. On the mechanism of antidepressant-like action of berberine chloride. Eur. J. Pharmacol. 2008;589:163–172. doi: 10.1016/j.ejphar.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 44.Castillo J., Hung J., Rodriguez M., Bastidas E., Laboren I., Jaimes A. LED fluorescence spectroscopy for direct determination of monoamine oxidase B inactivation. Anal. Biochem. 2005;343:293–298. doi: 10.1016/j.ab.2005.05.027. [DOI] [PubMed] [Google Scholar]
- 45.Asai M., Iwata N., Yoshikawa A., Aizaki Y., Ishiura S., Saido T.C., Maruyama K. Berberine alters the processing of Alzheimer’s amyloid precursor protein to decrease Abeta secretion. Biochem. Biophys. Res. Commun. 2007;352:498–502. doi: 10.1016/j.bbrc.2006.11.043. [DOI] [PubMed] [Google Scholar]
- 46.Wolozin B., Kellman W., Ruosseau P., Celesi G.G., Siegel G. Decreased prevalence of Alzheimer disease associated with 3-hydroxy-3-methyglutaryl coenzyme A reductase inhibitors. Arch. Neurol. 2000;57:1439–1443. doi: 10.1001/archneur.57.10.1439. [DOI] [PubMed] [Google Scholar]
- 47.Simons M., Keller P., Dichgans J., Schulz J.B. Cholesterol and Alzheimer’s disease: Is there a link? Neurology. 2001;57:1089–1093. doi: 10.1212/WNL.57.6.1089. [DOI] [PubMed] [Google Scholar]
- 48.Puglielli L., Tanzi R.E., Kovacs D.M. Alzheimer’s disease: The cholesterol connection. Nat. Neurosci. 2003;6:345–351. doi: 10.1038/nn0403-345. [DOI] [PubMed] [Google Scholar]
- 49.Wolozin B. Cholesterol and the biology of Alzheimer’s disease. Neuron. 2004;41:7–10. doi: 10.1016/S0896-6273(03)00840-7. [DOI] [PubMed] [Google Scholar]
- 50.Kong W., Wei J., Abidi P., Lin M., Inaba S., Li C., Wang Y., Wang Z., Si S., Pan H., et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat. Med. 2004;10:1344–1351. doi: 10.1038/nm1135. [DOI] [PubMed] [Google Scholar]
- 51.Akter K., Lanza E.A., Martin S.A., Myronyuk N., Rua M., Raffa R.B. Diabetes mellitus and Alzheimer’s disease: Shared pathology and treatment? Br. J. Clin. Pharmacol. 2011;71:365–376. doi: 10.1111/j.1365-2125.2010.03830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McClean P.L., Parthsarathy V., Faivre E., Hölscher C. The diabetes drug liraglutide prevents degenerative processes in a mouse model of Alzheimer’s disease. J. Neurosci. 2011;31:6587–6594. doi: 10.1523/JNEUROSCI.0529-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang Y., Li X., Zou D., Liu W., Yang J., Zhu N., Huo L., Wang M., Hong J., Wu P., et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J. Clin. Endocrinol. Metab. 2008;93:2559–2565. doi: 10.1210/jc.2007-2404. [DOI] [PubMed] [Google Scholar]
- 54.Yin J., Xing H., Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57:712–717. doi: 10.1016/j.metabol.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bhutada P., Mundhada Y., Bansod K., Tawari S., Patil S., Dixit P., Umathe S., Mundhada D. Protection of cholinergic and antioxidant system contributes to the effect of berberine ameliorating memory dysfunction in rat model of streptozotocin-induced diabetes. Behav. Brain Res. 2011;220:30–41. doi: 10.1016/j.bbr.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 56.Chen J.X., Yan S.S. Role of mitochondrial amyloid-beta in Alzheimer’s disease. J. Alzheimer’s Dis. 2010;20:S569–S578. doi: 10.3233/JAD-2010-100357. [DOI] [PubMed] [Google Scholar]
- 57.Hölscher C. The role of GLP-1 in neuronal activity and neurodegeneration. Vitam. Horm. 2010;84:331–354. doi: 10.1016/B978-0-12-381517-0.00013-8. [DOI] [PubMed] [Google Scholar]
- 58.Perry T., Greig N.H. The glucagon-like peptides: A new genre in therapeutic targets for intervention in Alzheimer’s disease. J. Alzheimer’s Dis. 2002;4:487–496. doi: 10.3233/jad-2002-4605. [DOI] [PubMed] [Google Scholar]
- 59.Lu S.S., Yu Y.L., Zhu H.J., Liu X.D., Liu L., Liu Y.W., Wang P., Xie L., Wang G.J. Berberine promotes glucagon-like peptide-1 (7-36) amide secretion in streptozotocin-induced diabetic rats. J. Endocrinol. 2009;200:159–165. doi: 10.1677/JOE-08-0419. [DOI] [PubMed] [Google Scholar]
- 60.Yu Y., Liu L., Wang X., Liu X., Liu X., Xie L., Wang G. Modulation of glucagon-like peptide-1 release by berberine: In vivo and in vitro studies. Biochem. Pharmacol. 2010;79:1000–1006. doi: 10.1016/j.bcp.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 61.Pereira C.V., Machado N.G., Oliveira P.J. Mechanisms of berberine (natural yellow 18)-induced mitochondrial dysfunction: Interaction with the adenine nucleotide translocator. Toxicol. Sci. 2008;105:408–417. doi: 10.1093/toxsci/kfn131. [DOI] [PubMed] [Google Scholar]
- 62.Pereira G.C., Branco A.F., Matos J.A., Pereira S.L., Parke D., Perkins E.L., Serafim T.L., Sardão V.A., Santos M.S., Moreno A.J., et al. Mitochondrially targeted effects of berberine [Natural Yellow 18, 5,6-dihydro-9,10-dimethoxybenzo(g)-1,3-benzodioxolo(5,6-a) quinolizinium] on K1735-M2 mouse melanoma cells: Comparison with direct effects on isolated mitochondrial fractions. J. Pharmacol. Exp. Ther. 2007;323:636–649. doi: 10.1124/jpet.107.128017. [DOI] [PubMed] [Google Scholar]
- 63.Rabbani G.H., Butler T., Knight J., Sanyal S.C., Alam K. Randomized controlled trial of berberine sulfate therapy for diarrhea due to enterotoxigenic Escherichia coli and Vibrio cholerae. J. Infect. Dis. 1987;155:979–984. doi: 10.1093/infdis/155.5.979. [DOI] [PubMed] [Google Scholar]
- 64.Birdsall T.C., Kelly G.S. Berberine: Therapeutic potential of an alkaloid found in several medicinal plants. Altern. Med. Rev. 1997;2:94–103. [Google Scholar]
- 65.Diogo C.V., Machado N.G., Barbosa I.A., Serafim T.L., Burgeiro A., Oliveira P.J. Berberine as a promising safe anti-cancer agent - is there a role for mitochondria? Curr. Drug Targets. 2011;12:850–859. doi: 10.2174/138945011795528930. [DOI] [PubMed] [Google Scholar]
- 66.Imanshahidi M., Hosseinzadeh H. Pharmacological and therapeutic effects of Berberis vulgaris and its active constituent, berberine. Phytother. Res. 2008;22:999–1012. doi: 10.1002/ptr.2399. [DOI] [PubMed] [Google Scholar]
- 67.Ye M., Fu S., Pi R., He F. Neuropharmacological and pharmacokinetic properties of berberine: A review of recent research. J. Pharm. Pharmacol. 2009;61:831–837. doi: 10.1211/jpp/61.07.0001. [DOI] [PubMed] [Google Scholar]
- 68.Wang X., Wang R., Xing D., Su H., Ma C., Ding Y., Du L. Kinetic difference of berberine between hippocampus and plasma in rat after intravenous administration of Coptidis rhizoma extract. Life Sci. 2005;77:3058–3067. doi: 10.1016/j.lfs.2005.02.033. [DOI] [PubMed] [Google Scholar]