Abstract
Background
Chlamydia trachomatis is the most prevalent bacterial sexually transmitted infection (STI) in the world. Approximately 80% of infected women are asymptomatic, although this infection can lead to serious complications in the female reproductive tract. Few data on Chlamydia infection are available in rural Amazonian communities.
Objectives
To evaluate the prevalence of sexual C. trachomatis infection in women from Marajó Archipelago communities in the Amazon region of Brazil and to identify associated factors and genotypes.
Methods
We utilized amplification of the ompA gene by nested PCR. Positive samples were genotyped by sequencing. Study participants completed a questionnaire on social, epidemiological, and reproductive health variables. A Poisson regression was used to evaluate the degree of association of these variables with the infection.
Results
The sexual infection by C. trachomatis was observed in 4% (16/393) of the subjects, and was more often found in women aged ≤25 (14.3%; 95% CI = 2.83–35.47; p <0.001), and in women with a household income of less than one Brazilian monthly minimum wage (5.2%; 95% CI = 1.33–11.37; p = 0.014). The ompA gene was sequenced in 13 samples, revealing F genotypes (38.4%, n = 5), D (23%, n = 3), E (15.3%, n = 2), Ia (7.6%, N = 1), J (7.6%, n = 1) and B (7.6%, n = 1).
Conclusions
We recorded a high prevalence of sexual infection by C. trachomatis in young and poor women from the interior of the Brazilian Amazon. This high prevalence and the frequencies of the main genotypes were similar to those found in major Brazilian urban centers. Our results reinforce the importance of the screening of this neglected infection, and the prevention of later sequelae in young women from rural and urban areas of Brazil.
Introduction
Chlamydia trachomatis is the most prevalent bacterial Sexually Transmitted Infection (STI) in the world [1], with about 128 million cases being diagnosed annually [2]. The infection is asymptomatic in approximately 80% of the infected women, going completely unnoticed by most women. The lack of an early diagnosis may make it impossible to treat the disorder adequately, with serious consequences for the female reproductive tract, such as salpingitis, Pelvic Inflammatory Disease (PID), ectopic pregnancy and tubal infertility, with an annual cost of up to four billion dollars [3–6]. This infection is the most common cause of preventable infertility in sexually active women and is a risk factor for other STIs [7–10].
The ompA gene of C. trachomatis has 19 genotypes, which are associated with a range of pathologies in humans [11]. The A, B, Ba and C genotypes are associated with trachoma [12], while the D, Da, E, F, G, Ga, H, I, Ia, J and K genotypes are associated with non-invasive urogenital infections [13], and the L1, L2, L2a and L3 genotypes cause lymphogranuloma venereum [14]. In Brazil, the actual prevalence of this infection and the genotypes present in different populations are still unclear, making it difficult to understand the dynamics of infection and preventing the creation of effective C. trachomatis screening programs by Brazilian public health agencies. Previous studies using nucleic acid amplification techniques have demonstrated that C. trachomatis infection rates range from 5% to 31% in Brazilian youths and adults, and that the most frequent genotypes in the country are the E, F and D types [15–19].
In the Brazilian Amazon region, many communities are located far from major urban centers, and have little access to public healthcare services or other resources [19, 20]. Understanding the diversity and distribution of the genotypes is essential for the monitoring of the infection, although few studies are available on the genotypes of sexual C. trachomatis infections in Brazil, and only one has focused on an urban Amazonian population [18]. The vast Marajó Archipelago is located at the mouth of the Amazon River, in the Brazilian state of Pará, and is inhabited by a largely rural population, living in small communities with few public healthcare services or even basic programs focusing on reproductive health [21, 22]. The present study aimed to determine the prevalence of C. trachomatis and its genotypes in the endocervical infections of women that have limited access to public health services, resident in four communities of the Marajó Archipelago, and to describe the potential. Study participants completed a questionnaire on social, epidemiological, and reproductive health variables associated with the prevalence of this disease.
Methods
Study population and data collection
This cross-sectional study was conducted between March 2013 and May 2015. The target population included autochthonous women (n = 393), from four small communities [São Sebastião da Boa Vista (n = 113), Anajás (n = 96), Portel (n = 60) and Chaves (n = 124)] of the Marajó Archipelago in Pará, in the Brazilian Amazon region. This archipelago is considered to be one of Pará’s main tourist destinations. Its principal islands are Marajó, Caviana, Mexiana and Gurupá, with 16 municipalities and a large network of rivers, creeks, lakes, and marshlands that criss-cross the islands and impede terrestrial access to most communities.
During the study period, the multidisciplinary team travelled from Belém (Pará state capital) to the communities for the collection of data. The sexually-active women in each community were informed of the periodicity of the health exams and asked to seek gynecological care during the home visits of the designated municipal health agents.
We investigated a non-probabilistic, intentional, and conventional sample, composed of women 18 to 79 years old, who had either never had a Pap smear or who had last had one more than one year previously. Exclusion criteria were pregnancy, menstruation, and not wishing to participate in the study or not signing the informed consent form. The participants were asked to answer a questionnaire, and were made aware of the importance of providing reliable answers, in order to minimize possible bias. The following variables were investigated: age, conjugal status, occupation/education, household income, age at fist sexual intercourse, lifetime number of sexual partners, number of sexual partners in the past year, use of condoms, use of contraceptives, previous pregnancies, natural childbirth, miscarriage, and whether the Pap test was taken.
Cervical secretions were collected during routine pelvic examinations using an endocervical brush, and the samples were stored in cryogenic tubes containing 1 ml Tris-EDTA buffer (TE) [10 mM Tris-HCl pH 8.5; 1 mM EDTA] at a temperature of -20°C for testing.
Ethics statement
This study was part of the "Epidemiological Markers in the Healthcare of the Marajó Archipelago" project, which was approved by the Ethics Committee for Research of the State Foundation for Hemotherapy, with authorization number 0003.0.324.000–10. All participants signed up to be adults, with no participants below the age of 18. Free and informed consent for participation in the study was obtained in writing before the collection of samples and epidemiological data. All the data were analyzed with complete anonymity.
Extraction of the DNA
The DNA was extracted using a pureLink Genomic DNA Purificationkit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions and stored at -20°C until analysis. A Polymerase Chain Reaction (PCR) of the human β globin gene was conducted prior to the detection of C. trachomatis to confirm the suitability of the samples [23].
Detection of the ompA gene of C. trachomatis
Detection of C. trachomatis was performed using a nested PCR protocol modified by Jalal et al. 2007 [24], which amplified 394bp of the ompA gene of C. trachomatis. The first reaction used 6.0 μL of GoTaqGreen Master Mix (Promega, Madison, WI, USA), 0.5 μL (containing 20 pmol/μL of each primer) of the primers P1 (A) (5'GACTTTGTTTTCGACCGTGTT-3 ') and P2 (5'AGCRTATTGGAAAGAAGCBCCTAA-3 '), 2 μL genomic DNA, and 3 μL sterile water for a final volume of 12 μL. The second reaction used 0.5 μL of the solution of the first reaction, 6.0 μL Go Taq Green Master Mix (Promega, Madison, WI, USA), 4.5 μL of sterile water, 0.5 μL (20 pmol/μL) of the primers P3 (5'-AAACWGATGTGAATAAAGARTT-3') and P4 (5'-TCCCASARAGCTGCDCGAGC-3'). In the two steps of the nested PCR, a negative and a positive control was used to optimize the result. In the first and second stages of the nested PCR, the initial activation was at 95°C for 5 min and 1 min, respectively, followed by 35 cycles of denaturation at 94°C for 40 s, annealing at 54°C for 30 s, and elongation at 72°C for 90 s, with a final extension step at 72°C for 7 min. The amplified products were visualized after electrophoresis in 1% agarose gel with ethidium bromide (0.5mg/mL) staining.
DNA sequencing
The Sanger method of nucleotide sequencing was used. An approximately 990bp fragment of the ompA gene was amplified by nested PCR using primers P1(B) (5′-ATGAAAAAACTCTTGAAATCGG-3′) and OMP2 (5′-ACTGTAACTGCGTATTTGTCTG-3′), and whenever re-amplification was necessary, the inner primers MOMP87 (5′-TGA ACC AAG CCT TAT GAT CGA CGG A-3′) and RVS1059 (5′-GCA ATA CCG CAA GAT TTT CTA GAT TTC ATC-3′) were used [25]. The first step of the nested PCR was run in a 0.5 μL volume containing 20 pmol/μL of each primer P1(B) and OMP2 and 5.0 μL of the DNA extracted from the endocervical secretion, 14 μL of sterile water, 1.0 μL of MgCl2, 1.0 μL deoxynucleoside triphosphate (10mM), 2.5 μL of 10x buffer, and 0.5 μL of Hotstar Taq DNA Polymerase 1.5U (Qiagen). Amplification was run in a final reaction volume of 25 μl [25]. In the two steps of nested PCR a negative and a positive control was used to optimize the result, but these controls were not used in the sequencing.
In the initial step of the nested PCR, amplification conditions were 95°C for 5 min, followed by 40 cycles of 94°C for 30 s, 55°C for 30 s, and 72°C for 90 s, and a final extension at 72°C for 7 min. In the nested PCR, the MOMP87-RVS 1059 primer pair was used with 1.5 μl of the product of the first stage of the nested PCR, which was added to a final volume of 25 μl. The conditions of the second step of the nested PCR were the same as those described above, except for the annealing temperature which was 60°C, and the addition of 17.5 μl of sterile water [25].
The amplified products were visualized by ethidium bromide (0.5 mg/mL) staining after electrophoresis in 1% agarose gel. The products obtained by the nested PCR were purified using a BigDye Xterminator Purification kit (Applied Biosystems, Foster City, CA, USA) to sequence both strands. A BigDyeTerminator Cycle kit (Foster City, CA, USA) was used for the sequencing reaction, according to the manufacturer's instructions. The reaction mixtures were sequenced in an ABI 3130 (Applied Biosystems, Foster City, CA, USA).
Phylogenetic analysis and Genotyping
The sequences were assembled using the CAP3 software, aligned in MAFFT v 7.221 and edited in Bioinformatic Geneious v 8.1.7. The consensus sequences were compared with known C. trachomatis lineages [26] using the BLAST search tool in the National Center for Biotechnological Information (www.ncbi.nlm.nih.gov). The residues that correspond to the flanking primers were excluded from the analyses.
The phylogenetic analysis was run in three stages. The first stage involved the use of IQ-TREE v 1.3.2 for the selection of the most adequate evolutionary model for the maximum likelihood analysis. The phylogenetic reconstruction was also run in IQ-TREE. The standard error was obtained using a bootstrap value of 0.03 for 2000 repetitions. In the third stage, FigTree v 1.4.2 was used to edit the phylogenetic tree produced by the analyses.
Statistical analysis
The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 21.0 (SPSS, Chicago, illinois, EUA). A Poisson regression was used to examine the unadjusted and adjusted associations between the Prevalence Ratio (PR) and the different variables. A 95% confidence interval (CI) was estimated and a critical p value of 0.05 was considered in all analyses.
Results
The ages of the 393 women investigated in the present study ranged from 18 to 79 years. The median (interquartile range) age was 40.0 (29.0–52.0) years, and 82.2% (n = 323) of the participants were older than 25 years. Most of the women (n = 68.7%) were married, 75.9% (n = 259) were employed informally, and 55.7% (n = 219) had a family income of no more than the Brazilian minimum wage (U$250–300/month). Just over half 51.1% of the women (n = 201) were not using oral contraceptives, 90.6% (n = 356) were already mothers, and 90.4% (n = 355) of these mothers reported having had a vaginal delivery. Around one third, 32.6% (n = 128), reported having suffered at least one miscarriage, and 81.4% regularly have Pap tests.
The total prevalence of sexual infection by C. trachomatis was 4.1% (16/393). The infection was detected in 14.3% of the women that were 25 years old or younger, with an adjusted prevalence 10 times higher (95% CI = 2.83–35.47; p <0.001) than in women older than 25 years. The prevalence of infection was also 3.88 times higher in women from low-income households (below minimum wage) in comparison with those from higher income households (95% CI = 1.33–11.37; p = 0.014). No other variables were associated statistically with C. trachomatis infection (Table 1).
Table 1. Social, epidemiological, and reproductive health variables characteristics, with raw and adjusted prevalence ratios, in women from communities in Marajó Archipelago, Pará, Brazil.
| Social Variables |
Total (n = 393) |
C. trachomatis positive 4.1% (16/393) |
RP Ajusted (CI95%) |
p-value | ||||
| n | % | n | % | |||||
| Age (years)a | ≤25 | 70 |
17.8 |
10 |
14.3 |
10.01(2.83–35.47) |
<0.001* | |
| >25 | 323 | 82.2 | 6 | 1.8 | 1 | |||
| Not answered | 0 | 0 | ||||||
| Conjugal statusa | Single | 96 | 24.4 | 7 | 7.3 | 1.72(0.54–5.53) | 0.383 | |
| Married | 270 | 68.7 | 6 | 2.2 | 1 | |||
| Not answered | 27 | 6.9 | ||||||
| Occupationa | Informal | 259 | 65.9 | 8 | 3.1 | 0.59(0.21–1.65) | 0.312 | |
| Student | 105 | 26.7 | 6 | 5.7 | 1 | |||
| Not answered | 29 | 7.4 | ||||||
| Household incomea (number of Brazilian minimum wages) |
<1 | 154 | 39.2 | 8 | 5.2 | 3.88(1.33–11.37) | 0.014* | |
| ≥1 | 219 | 55.7 | 8 | 3.7 | 1 | |||
| Not answered | 20 | 5.1 | ||||||
| Epidemiological variables | Age at fist sexual intercourse (years)b | <15 | 127 | 32.3 | 9 | 7.1 | 2.93(0.91–9.47) | 0.073 |
| ≥15 | 239 | 60.8 | 7 | 2.9 | 1 | |||
| Not answered | 27 | 6.9 | ||||||
| Sexual partnera | Yes | 285 | 72.5 | 9 | 3.1 | 2.78(0.74–10.49) | 0.132 | |
| No | 94 | 23.9 | 7 | 7.4 | 1 | |||
| Not answered | 14 | 3.6 | ||||||
| Sexual partners in the last yearb | >1 | 100 | 25.4 | 2 | 2 | 1.03(0.13–7.95) | 0.974 | |
| 1 | 238 | 60.6 | 10 | 4.2 | 1 | |||
| Not answered | 55 | 14.0 | ||||||
| Condom usea b | Yes | 59 | 15.0 | 4 | 6.8 | 1.33(0.28–6.25) | 0.715 | |
| No | 321 | 81.7 | 12 | 3.7 | 1 | |||
| Not answered | 13 | 3.3 | ||||||
| Number of sexual partners in lifeb | >3 | 75 | 19.1 | 6 | 8.0 | 1.94(0.51–7.44) | 0.329 | |
| ≤3 | 239 | 60.8 | 8 | 3.3 | 1 | |||
| Not answered | 79 | 20.1 | ||||||
| Reproductive health variables | Contraceptive usea | Yes | 188 | 47.9 | 7 | 3.7 | 0.92(0.31–2.76) | 0.891 |
| No | 201 | 51.1 | 9 | 4.4 | 1 | |||
| Not answered | 4 | 1 | ||||||
| Previous pregnancyb | Yes | 356 | 90.6 | 13 | 3.7 | 0.59(0.13–2.58) | 0.484 | |
| No | 32 | 8.1 | 2 | 6.5 | 1 | |||
| Not answered | 5 | 1.3 | ||||||
| Natural childbirthb | Yes | 355 | 90.3 | 13 | 3.7 | 0.63(0.14–2.79) | 0.543 | |
| No | 34 | 8.7 | 2 | 5.9 | 1 | |||
| Not answered | 4 | 1.0 | ||||||
| Miscarriage b | Yes | 128 | 32.6 | 3 | 2.3 | 0.53(0.15–1.90) | 0.328 | |
| No | 260 | 66.1 | 12 | 4.6 | 1 | |||
| Not answered | 5 | 1.3 | ||||||
| Pap smear testb | Yes | 320 | 81.4 | 12 | 3.8 | 0.85(0.21–3.38) | 0.818 | |
| No | 69 | 17.6 | 3 | 4.3 | 1 | |||
| Not answered | 4 | 1.0 | ||||||
RP Adjusted (ratio of adjusted prevalence): variables adjusted to each other in each group—multiple analysis. 95% CI: 95% Confidence Interval.
*: Statistically significant p value
a:Current variables
b:Anamnesis variables.
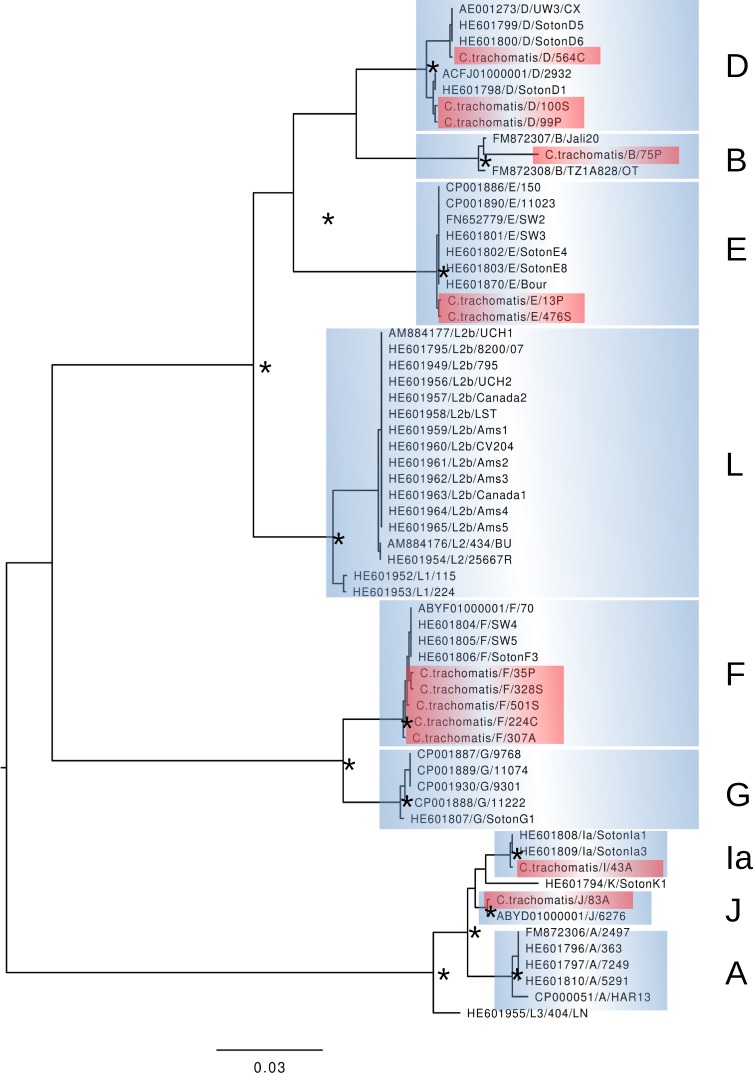
The ompA gene was sequenced in 13 of the 16 positive samples. Six genotypes were detected F (38.4%, n = 5), D (23%, n = 3), and E (15.3%, n = 2), with one sample each (7.6%) of the Ia, J, and B genotypes. The phylogenetic analysis revealed the evolutionary relationship among the C. trachomatis genotypes from the present study, with 99–100% similarity among the lineages, and 87.9% of similarity with the C. trachomatis reference lineage (Fig 1). The nucleotide sequences of the different C. trachomatis lineages identified in the present study were deposited in GenBank (NCBI) under access codes KU295204–KU295216. (Figs 1 and S1)
Fig 1. Results of the phylogenetic analysis of the ompA gene sequences of C. trachomatis detected in the endocervical samples of women from the Marajó Archipelago, Pará, Brazil.
The samples analyzed in the present study are shown in red, and all other were obtained from GenBank (https://www.ncbi.nlm.nih.gov/genbank).
Discussion
This preliminary study presented a molecular approach for the diagnosis of C. trachomatis infection in women who are socially deprived, residents in communities with little or no access to health care and laboratory procedures, which not only identified infection rates, but also the genotypes involved. The study participants completed a questionnaire on social, epidemiological, and reproductive health variables associated with the prevalence of this disease.
The low prevalence (4.1%) of C. trachomatis sexual infection identified in these communities may be related to the maturity of the women surveyed (mean age of 41 years and 82.2% more than 25 years old). On the other hand, we identified a significantly higher prevalence (14.3%) of C. trachomatis infection in young women (≤ 25 years old). High prevalence (11%) [18] and (18%) [19] were also identified in young women from the region’s largest city (Belém).
Access to health services is precarious in some parts of northern Brazil, such as Marajó Island, mainly due to its geographical characteristics [20,21]. In addition to being more common in younger women, the infection was also associated with a low family income.
In urban areas of other Brazil regions, infection rates vary from 9.6% to 31.0% [17, 27–32].
Even at such high prevalence rates, the association with risk variables is not easily identified, but there is evidence linking prevalence to young age and sexual conduct [29], as well as low income [30]. Precarious social conditions, a lack of economic opportunities, and risky sexual behavior are all closely associated with the incidence of STIs in young people [32].
High rates of sexual infection by C. trachomatis were recorded in Spain (8.5%) [33] and Great Britain (12.3%) [34]. Monitoring urogenital C. trachomatis infection by DNA amplification in women of less than 25 years of age should be a priority in most of these countries [35–38].
Although three samples could not be sequenced, six genotypes were identified in the remaining 13 samples. In general, our findings confirmed a higher prevalence of C. trachomatis genotypes F, D, E in sexual infections, as already described in an urban study in northern Brazil, together with genotype J [18]. Previous serological studies in the Amazon have shown that the distribution of C. trachomatis serotypes is similar to that observed in the present study [22]. Similar C. trachomatis genotypes have also been found in other regions of the Brazil [15–16] and the world [39–42].
The present study identified the occurrence of the B genotype of C. trachomatis in sexual infections of women from rural communities in the Brazilian Amazon region. The presence of the B genotype of C. trachomatis, an ocular genotype, is not unusual in the genital samples and has been reported in other studies [43–45]. Trachoma infection is another prominent clinical feature of C. trachomatis infection that has been reported from the Marajó Archipelago [46, 47]. However, it is still too early to confirm that this finding is related to cross-infection or gene recombination, which were not investigated specifically in the present study.
The lack of a public health program for the screening of this STI in Brazil is a major obstacle to the understanding of the epidemiology of C. trachomatis in this country. This favors the onset of reproductive problems, which can develop slowly and silently [48, 49].
The molecular screening for C. trachomatis infection is not yet included in the National Strategic Plan for STDs and AIDS in Brazil [50]. However, it would be important to include techniques with high sensitivity and specificity for the primary screening of active infection by C. trachomatis. More studies on the molecular prevalence, cross-infection, gene recombination, and genotypes of C. trachomatis will also be important, especially in young women, to elucidate the epidemiological network of this neglected STI.
The principal limitations of this study may be related to the relatively reduced sample size in comparison with the vast universe of communities in the Brazilian Amazon region, together with possible social biases in the responses of the women to the questionnaire. In the context of these considerations, this preliminary study is part of a larger project that aims to identify potential indicators that will support effective strategies for the improvement of the quality of life of the populations of the Marajó Archipelago. While it should be possible to extrapolate these findings to other, similar Amazonian communities, further research will be important to elucidate the exact nature of this infection and the distribution of the sexual and ocular genotypes of C. trachomatis in the region.
Conclusions
We report a high prevalence of sexual infection by C. trachomatis in young and poor women from the interior of the Brazilian Amazon region. This prevalence and the diversity of C. trachomatis genotypes identified in this study were similar to that found in other Brazilian regions. Our results reinforce the importance of the adequate screening of this infection for the prevention of late sequelae in the young population of rural and urban areas of Brazil.
Supporting information
The 13 samples sequenced in this study are shown in the tree in red letters.
(DOCX)
Acknowledgments
We thank the women volunteers that participated the study and wish them the best of health.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The present study was fully supported by grants from the Fundação Amazônia Paraense de Amparo a Pesquisa (FAPESPA – ICAAF 014/2012) and Ministério da Saúde do Brasil (MS). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (WHO). Prevalence and incidence of selected sexually transmitted infections. Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis and Trichomonas vaginalis. Methods and results used by WHO to generate 2005 estimates; 2005. [Google Scholar]
- 2.Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, Stevens G, Gottlieb S, Kiarie J, Temmerman M. Global estimates of the prevalence and incidence of curable Sexually Transmitted Infections in 2012 based on systematic review and global reporting. PLoS One. 2015. December 8; 10(12):e0143304 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stamm WE.Chlamydia trachomatis infections: progress and problems. The Journal of Infectious Diseases. 1999;179, (Suppl) 2:S380–3 10081511. [DOI] [PubMed] [Google Scholar]
- 4.Eleutério RMN, Junior JE, Giraldo PC, Muniz AMV. Chlamydia trachomatis Cervicitis in Sexual Actives Women From a Private Gynecologic Service, in Fortaleza City, Role-based access control, vol. 2007; 39(4): 287–290. [Google Scholar]
- 5.Gottlieb SL, Berman SM, Low N. Screening and treatment to prevent sequelae in women with Chlamydia trachomatis genital infection: how much do we know? The Journal of Infectious Diseases. 2010; 201(suppl 2): S156–67. [DOI] [PubMed] [Google Scholar]
- 6.Mania-Pramanik J, Kerkar S, Sonawane S, Mehta P, Salvi V. Current Chlamydia trachomatis infection, a major cause of infertility. Journal of Reproduction and Infertility. 2012. 13(4): 204–210. [PMC free article] [PubMed] [Google Scholar]
- 7.Samoff E, Koumans EH, Markowitz LE, Sternberg M, Sawyer MK, Swan D, et al. Association of Chlamydia trachomatis with persistence of high-risk types of human papillomavirus in a cohort of female adolescents. American Journal of Epidemiology. 2005;162(7):668–75. 10.1093/aje/kwi262 [DOI] [PubMed] [Google Scholar]
- 8.Nakashima K, Shigehara K, Kawaguchi S, Wakatsuki A, Kobori Y, Nakashima K, Ishii Y, Shimamura M, Sasagawa T, Kitagawa Y, Mizokami A, Namiki M. Prevalence of human papillomavirus infection in the oropharynx and urine among sexually active men: a comparative study of infection by papillomavirus and other organisms, including Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma spp., and Ureaplasma spp. BMC Infectious Diseases. 2014; 27: 14–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdella RM, Abdelmoaty HI, Elsherif RH, Sayed AM, Sherif NA, Gouda HM, El Lithy A, Almohamady M, Abdelbar M, Hosni AN, Magdy A, Ma Y. Screening for Chlamydia trachomatis in Egyptian women with unexplained infertility comparing real-time PCR techniques to standard serology tests case control study. BMC Womens Health. 2015; 2;15:45 10.1186/s12905-015-0202-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cunha CB, Friedman RK, de Boni RB, Gaydos C, Guimarães MR, Siqueira BH, Cardoso SW, Chicayban L, Coutinho JR, Yanavich C, Veloso VG, Grinsztejn B. Chlamydia trachomatis, Neisseria gonorrhoeae and syphilis among men who have sex with men in Brazil. BMC Public Health. 2015;15:686 10.1186/s12889-015-2002-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaltenboeck B, Kousoulas KG, Storz J. Structures of and allelic diversity and relationships among the major outer membrane protein (ompA) genes of the four chlamydial species. Jounal of Bacteriology. 1993; 175:487–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burton MJ, Mabey DC. The global burden of trachoma: A review. PLoS Neglected Tropical Diseases. 2009; 3:e 460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millman K,Black CM,Johnson RE,Stamm WE,Jones RB,Hook EW,Martin DH, Bolan G, Tavaré S, Dean D. Population-based genetic and evolutionary analysis of Chlamydia trachomatis urogenital strain variation in the United States. Journal of Bacteriology. 2004; 186:2457–2465. 10.1128/JB.186.8.2457-2465.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manavi K. A review on infection with Chlamydia trachomatis. Best Practice & Research Clinical Obstretics & Gynaecology. 2006;20:941–51. [DOI] [PubMed] [Google Scholar]
- 15.Lima H E, Oliveira MB, Valente BG, Afonso DAF, Darocha WD, Souza MCM, Alvim TC, Barbosa-Stancioli EF, Noronha FSM. Genotyping of Chlamydia trachomatis From Cervical Specimens in Brazil. Sexually Transmitted Diseases. Vol. 34, No. 9, p.709–717, 2007. 10.1097/01.olq.0000258399.27873.d9 [DOI] [PubMed] [Google Scholar]
- 16.Machado ACS, Bandea CI, Alves MFC, Joseph K, Igietseme J, Miranda AE, Guimarães EMB, Turchi, MD, Black CM. Distribution of Chlamydia trachomatis genovars among youths and adults in Brazil. Journal of Medical Microbiology. 2011; 60; 472–476. 10.1099/jmm.0.026476-0 [DOI] [PubMed] [Google Scholar]
- 17.Machado MSC, Silva BFBC, Gomes ILC, Santana IU, Grassi MFR. Prevalence of cervical Chlamydia trachomatis infection in sexually active adolescents from Salvador, Brazil. The Brazilian Journal of Infectious Diseases, v. 16, n. 2, 2012; 188–191. [DOI] [PubMed] [Google Scholar]
- 18.Brasiliense DM, Borges BN, Ferreira WA. Genotyping and prevalence of Chlamydia trachomatis infection among women in Belém, Pará, northern Brazil. J Infect Dev Ctries. 2016; 10(2):134–7. 10.3855/jidc.6474 [DOI] [PubMed] [Google Scholar]
- 19.Santos Ulian WL, Trindade JQ, Sousa FDM, Oliveira JFG, Pereira CCC, Brasiliense DM, Prazeres BA, Tsutsumi MY, Ishikawa EAY, Sousa MS. Prevalência da infecção endocervical de Chlamydia trachomatis em universitárias do Estado do Pará, região Amazônica, Brasil. Revista Pan-Amazônica de Saúde (Online), V. 8, P. 27–33, 2017. 10.5123/s2176-62232017000300004 [Google Scholar]
- 20.Santos LM, Souza IRA, Holanda LHC, Vaz JO, Tsutsumi MY, Ishikawa EAY, Sousa MS. Alta incidência da infecção urogenital por Chlamydia trachomatis em mulheres parturientes de Belém, Estado do Pará, Brasil. Revista Pan-Amazônica de Saúde (Online), v. 7, p. 101–106, 2016. 10.5123/s2176-62232016000400012 [Google Scholar]
- 21.Fonseca MG, Bastos FI. Twenty-five years of the AIDS epidemic in Brazil: principal epidemiological findings, 1980–2005. Cadernos de Saúde Pública, 23 (Suppl. 3) (2007), pp. S333–S344 [DOI] [PubMed] [Google Scholar]
- 22.Ishak MO, Costa MM, de Almeida NC,Santiago AM,Brito,Vallinoto AC,Azevedo VN,Ishak R. Chlamydia trachomatis serotype A infections in the Amazon region of Brazil: prevalence, entry and dissemination. Revista da Sociedade Brasileira de Medicina Tropical. 2015; 48(2):170–4. 10.1590/0037-8682-0038-2015 [DOI] [PubMed] [Google Scholar]
- 23.Greer CE, Lund J. K, Manos MM. PCR amplification from paraffin- embedded tissues: recommendations on fixatives for Long-term Storage and prospective Studies. PCR Methods Appl. v.1, 1991; 46–50. [DOI] [PubMed] [Google Scholar]
- 24.Jalal H,Stephen H, Alexander S, Carne C,Sonnex C. Development of real-time PCR assays for genotyping of Chlamydia trachomatis. Journal of Clinical and Microbiology. 2007; 45(8):2649–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lysén M,Osterlund A,Rubin CJ,Persson T,Persson I,Herrmann B. Characterization of ompA Genotypes by Sequence Analysis of DNA from All Detected Cases of Chlamydia trachomatis Infections during 1 Year of Contact Tracing in a Swedish County. Journal of Clinical Microbiology. 2004, 42(4):1641–7. 10.1128/JCM.42.4.1641-1647.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris SR,Clarke IN,Seth-Smith HM, Solomon AW, Cutcliffe LT, Marsh P, Skilton RJ, Holland MJ, Mabey D, Peeling RW, Lewis DA, Spratt BG, Unemo M, Persson K, Bjartling C, Brunham R, de Vries HJ, Morré SA, Speksnijder A, Bébéar CM, Clerc M, de Barbeyrac B, Parkhill J, Thomson NR. Whole-genome analysis of diverse Chlamydia trachomatis strains identifies phylogenetic relationships masked by current clinical typing. Nature Genetics. 2012. March 11;44(4):413–9, S1. 10.1038/ng.2214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magalhães PA, Miranda CA, Lima ÉG, Moizéis RN, de Lima DB, Cobucci RN, de Medeiros Fernandes TA, de Azevedo JC, de Azevedo PR, de Araújo JM, Fernandes JV. Genital tract infection with Chlamydia trachomatis in women attended at a cervical cancer screening program in Northeastern from Brazil. Archives of Gynecology and Obstetrics. 2015; 291(5):1095–102. 10.1007/s00404-014-3514-z [DOI] [PubMed] [Google Scholar]
- 28.de Abreu AL, Nogara PR, Souza RP, da Silva MC, Uchimura NS, Zanko RL, Ferreira EC, Tognim MC, Teixeira JJ, Gimenes F, Consolaro ME. Molecular detection of HPV and Chlamydia trachomatis infections in Brazilian women with abnormal cervical cytology. The American Journal of Tropical Medicine and Hygiene. 2012; 87(6):1149–51. 10.4269/ajtmh.2012.12-0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lima YA,Turchi MD,Fonseca ZC,Garcia FL,Cardoso FAB, Reis MNG, Guimarães EMB,Alves RRF,Carvalho NR,Alves MFC. Sexually transmitted bacterial infections among young women in Central Western Brazil. International Journal of Infectious Diseases. 2014; 25:16–21. 10.1016/j.ijid.2014.03.1389 [DOI] [PubMed] [Google Scholar]
- 30.Garcês AX, Martinez AM, Gonçalves CV, Germano FN, Barral MF, Vieira VC Prevalence of Chlamydia trachomatis and risk factors associated with infection detected in endocervical sample. Revista Brasileira de Ginecologia e Obstetrícia. 2013; 35(8):379–83. [DOI] [PubMed] [Google Scholar]
- 31.Tavares MCM, Macêdo JL, Lima Júnior SF, Heráclio SA, Amorim MM, Maia MMD, Souza PRE. Chlamydia trachomatis infection and human papillomavirus in women with cervical neoplasia in Pernambuco-Brazil. Molecular Biology Reports. 2014; 41:865–874. 10.1007/s11033-013-2927-2 [DOI] [PubMed] [Google Scholar]
- 32.Sheringham J, Mann S, Simms I, Stafford M, Hart G J, Raine R. It matters what you measure: a systematic literature review examining whether young people in poorer socioeconomic circumstances are more at risk of Chlamydia. Sexually Transmitted Infections. 2013;89: 175–180. 10.1136/sextrans-2011-050223 [DOI] [PubMed] [Google Scholar]
- 33.López-Corbeto E,González V,Casabona J;Grupo de estudio CT/NG-ASSIR. Prevalence and re-infection rate of C. trachomatis genital infections in young people under 25 years in Catalonia. Enfermidades Infecciosas y Microbiology Clinic. 2015; S0213-005X (15)00286-4. [DOI] [PubMed] [Google Scholar]
- 34.Woodhall SC, Nichols T, Alexander S, Silva FC, Mercer CH, Ison C, Gill ON, Soldan K Can we use postal surveys with anonymous testing to monitor chlamydia prevalence in young women in England? Pilot study incorporating randomised controlled trial of recruitment methods. Sexually Transmitted Infections. 2015; 91(6):412–4. 10.1136/sextrans-2015-052067 [DOI] [PubMed] [Google Scholar]
- 35.European Centre for Disease Prevention and Control, Chlamydia control in Europe, ISBN 978-92-9193-165-1. Stockholm, 2009.
- 36.Preventive Services US. Task Force. Screening for chlamydial infection: U.S. Preventive Services Task Force recommendation statement. Annais of Internal Medicine. 2007;147:128–134. [DOI] [PubMed] [Google Scholar]
- 37.Hocking J S, Walker J, Regan D, Chen M Y, Fairley C K. Chlamydia screening: Australia should strive to achieve what others have not. Medical Journal of Australia. 2008; 188 (2): 106–108. [DOI] [PubMed] [Google Scholar]
- 38.Lanjouw E, Ossewaarde JM, Stary A, Boag F, van der Meijden WI. European guideline for the management of Chlamydia trachomatis infections. International Journal of DST AIDS.2010; 21 (11): 729–37. [DOI] [PubMed] [Google Scholar]
- 39.CDC. Recommendations for the Laboratory-Based Detection of Chlamydia trachomatis and Neisseria gonorrhoeae—2014. Morbidity and Mortality Weekly Report (MMWR). Recommendations and Reports. 2014, Vol. 63, No. 2. [PMC free article] [PubMed] [Google Scholar]
- 40.Fernández-Benítez C, Mejuto-López P, Otero-Guerra L, Margolles-Martins MJ, Suárez-Leiva P, Vazquez F. Prevalence of genital Chlamydia trachomatis infection among young men and women in Spain. BMC Infectious Diseases. 2013; 13:388 10.1186/1471-2334-13-388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fieser N, Simnacher U, Tausch Y, Werner-Belak S, Ladenburger-Strauss S, von Baum H, Reischl U, Essig A. Chlamydia trachomatis prevalence, genotyping and identification of the new Swedish variant in Southern Germany. Infection. 2013; 41 (1): 159–66. 10.1007/s15010-012-0301-2 [DOI] [PubMed] [Google Scholar]
- 42.Haro-Cruz MJ, Deleón-Rodriguez I, Escobedo-Guerra MR, López-Hurtado M, Arteaga-Troncoso G, Ortiz-Ibarra FJ, Guerra-Infante FM. Genotyping of Chlamydia trachomatis from cervical specimens of infertile Mexican women. Enfermidades Infecciosas y Microbiology Clinic. 2011; 29(2):102–108. [DOI] [PubMed] [Google Scholar]
- 43.Piñeiro L, Montes M, Gil-Setas A, Camino X, Echeverria MJ, Cilla G. Genotyping of Chlamydia trachomatis in an area of northern Spain. Enfermidades Infecciosas y Microbiology Clinic. 2009;27(8):462–4. [DOI] [PubMed] [Google Scholar]
- 44.Herrmann B, Isaksson J, Ryberg M, Tångrot J, Saleh I, Versteeg B, Gravningen K, Bruisten S. Global Multilocus Sequence Type Analysis of Chlamydia trachomatis Strains from 16 Countries. J Clin Microbiol. 2015. July;53(7):2172–9. 10.1128/JCM.00249-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yamazaki T, Matsumoto M, Matsuo J, Abe K, Minami K, Yamaguchi H. Frequency of Chlamydia trachomatis in Ureaplasma-positive healthy women attending their first prenatal visit in a community hospital in Sapporo, Japan. BMC Infectious Diseases. 2012; 12:82 10.1186/1471-2334-12-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reilly LA, Favacho J, Garcez LM, Courtenay O. Preliminary evidence that synanthropic flies contribute to the transmission of trachoma- causing Chlamydia trachomatis in Latin America. Cadernos de Saúde Pública. 2007; 23, n.7, 1682–1688. [DOI] [PubMed] [Google Scholar]
- 47.Favacho J, Alves da Cunha AJL, Gomes STM, Freitas FB, Queiroz MAF, Vallinoto ACR, Ishak R, Ishak MOG. Prevalence of trachoma in school children in the Marajó Archipelago, Brazilian Amazon, and the impact of the introduction of educational and preventive measures on the disease over eight years. PLoS Negl Trop Dis. 2018. February 15;12(2):e0006282 10.1371/journal.pntd.0006282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Greydanus DE,Dodich C. Pelvic inflammatory disease in the adolescent: a poignant, perplexing, potentially preventable problem for patients and physicians. Current Opinion in Pediatrics. 2015. February;27(1):92–9. 10.1097/MOP.0000000000000183 [DOI] [PubMed] [Google Scholar]
- 49.Silva LD,Miranda A,Batalha R,Ferreira L,Santos M,Talhari S. High-risk human papillomavirus and cervical lesions among women living with HIV/AIDS in Brazilian Amazon, Brazil. The Brazillian Journal of Infectious Diseases. 2015. Nov-Dec;19(6):557–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.BRASIL. Ministério da Saúde: PROJETO AIDS-SUS (AIDS-SUS Project–National AIDS Program and National Health Services)- RELATÓRIO DE PROGRESSO N° 01. 2012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The 13 samples sequenced in this study are shown in the tree in red letters.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.