Summary
This report presents the case of a 48-year-old male with acute congestive heart failure caused by paroxysmal supraventricular tachycardia. The patient showed no structural heart disease with normal echocardiography parameters of the left ventricle. The pulmonary capillary wedge pressure (PCWP) was continuously monitored during the electrophysiological study. The PCWP and the plasma B-type natriuretic peptide increased from the normal range during ongoing tachycardia. The tachycardia was diagnosed as orthodromic atrioventricular reciprocating tachycardia and it was successfully eliminated by radiofrequency catheter ablation.
Keywords: Paroxysmal supraventricular tachycardia, Congestive heart failure, B-type natriuretic peptide, Catheter ablation
Introduction
Persistent or incessant supraventricular and ventricular tachycardia may cause reversible left ventricular (LV) dysfunction, known as tachycardia-induced cardiomyopathy, and congestive heart failure [1], [2], [3]. Hemodynamic changes occur as soon as 24 h after rapid pacing, with continued deterioration in ventricular function for up to 3–5 weeks, thus resulting in end-stage heart failure in experimental animal models [4], [5]. However, the acute cardiovascular collapse induced by paroxysmal supraventricular tachycardia rarely occurs in patients with a normal ventricular function. This report presents a case with acute congestive heart failure caused by orthodromic atrioventricular reciprocating tachycardia (AVRT) in a heart with a normal LV systolic function.
Case report
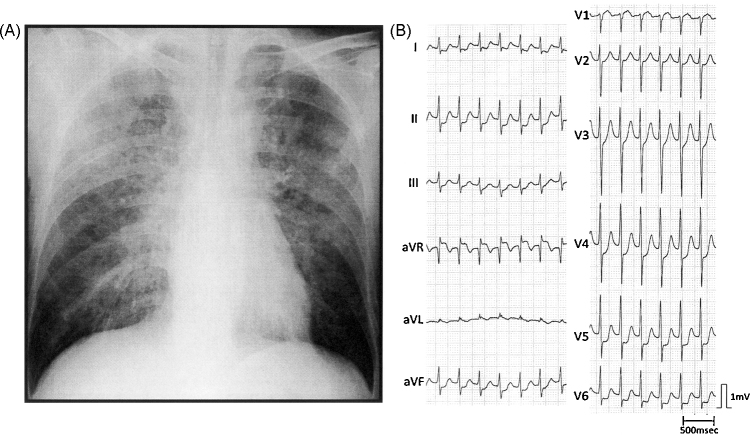
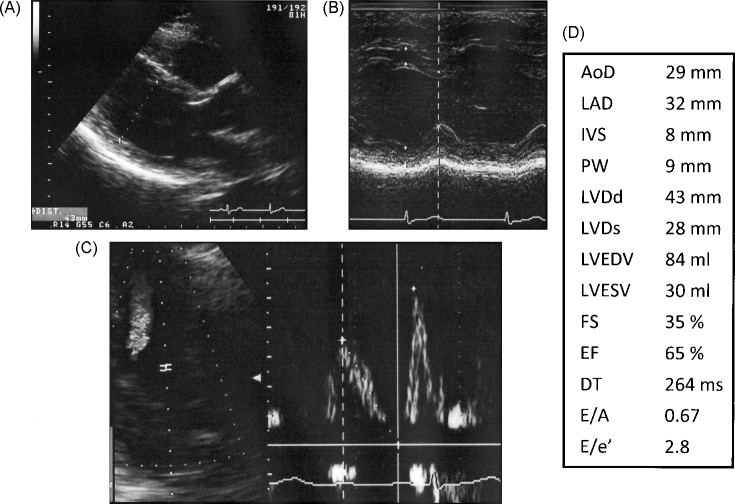
A 48-year-old male with dyspnea and palpitation was hospitalized. He had been diagnosed with congestive heart failure and had been treated by the venous administration of diuretics several times at another hospital. He had no history of hypertension and diabetes mellitus, or smoking. The family history was negative. A chest X-ray at the time of hospitalization showed a butterfly shadow indicating pulmonary edema without evidence of cardiomegaly (cardiothoracic ratio 41%, Fig. 1A), while echocardiography revealed a normal heart with the following data: LV ejection fraction (LVEF) of 64%, interventricular septum of 9 mm, LV posterior wall of 10 mm and an LV diastolic dimension of 40 mm during tachycardia. Twelve-lead electrocardiogram recorded on admission demonstrated a regular narrow QRS tachycardia at a rate of 185 beats/min (Fig. 1B). Rapid venous injection of adenosine 5′-triphosphate terminated the tachycardia. During sinus rhythm the 12-lead electrocardiogram presented no pre-excitation. While the normal size of the LV and preserved systolic function (LVEF 65%) were demonstrated by the echocardiogram during sinus rhythm, a transmitral early-to-late flow velocity ratio of 0.67 suggested a possible mild LV diastolic dysfunction (Fig. 2). The deceleration time and the ratio of the peak early diastolic velocity of transmitral flow to the peak early diastolic velocity of mitral annulus were also within the normal range (Fig. 2D). The dyspnea and the butterfly shadow in his chest X-ray disappeared following the tachycardia termination and treatment with 20 mg of furosemide venous injection. The findings of both coronary computed tomography angiography and cardiovascular magnetic resonance imaging were normal.
Figure 1.
A chest X-ray and electrocardiogram at the admission. (A) A chest X-ray (anteroposterior view) at the time of admission shows diffuse bilateral pulmonary edema with a 42% cardiothoracic ratio. (B) The 12-lead electrocardiogram demonstrates regular narrow QRS tachycardia.
Figure 2.
Echocardiogram during sinus rhythm. Long axis (A) and M-mode (B) of the left ventricle are shown. (C) Pulse Doppler recording was obtained at the mitral annulus. (D) Echocardiographical parameters. AoD, aortic diastolic diameter; LAD, left atrial dimension; IVSd, interventricular septum; PW, posterior wall; LVDd, left ventricular internal dimension in diastole; LVDs, left ventricular internal dimension in systole; LVEDV, left ventricular end-diastolic volume; LVESV, left ventricular end-systolic volume; FS, fractional shortening; EF, ejection fraction; DT, deceleration time; E/A, peak early diastolic LV filling velocity/peak atrial filling velocity ratio; E/e′, the ratio of the peak early diastolic velocity of transmitral flow to the peak early diastolic velocity of the mitral annulus.
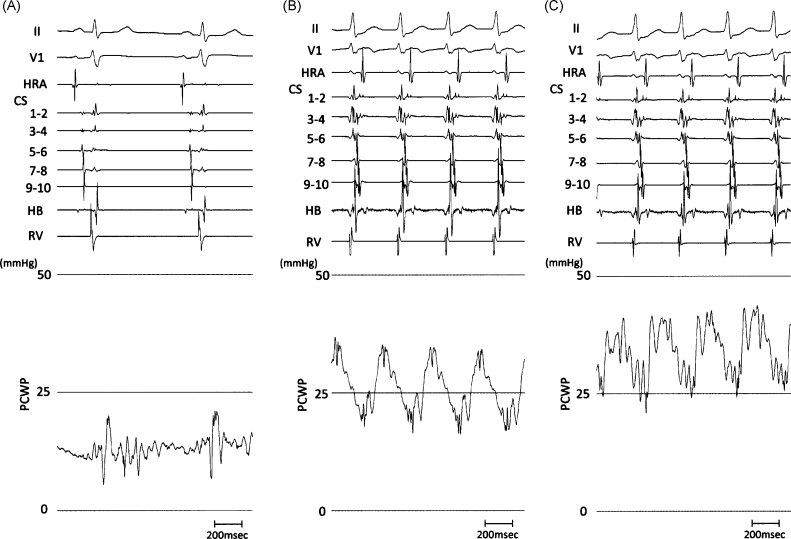
An electrophysiological study and catheter ablation were conducted after the patient provided his informed consent. A decapolar electrode catheter was inserted into the coronary sinus via a subclavian vein approach. The catheters were placed into the right atrium, His-bundle region, and right ventricle through the femoral veins. A Swan-Ganz catheter was also inserted and positioned in the pulmonary artery so that pulmonary capillary wedge pressure (PCWP) recordings were continuously obtained upon balloon inflation. The plasma B-type natriuretic peptide (BNP) level and PCWP were within the normal range (3.0 pg/ml and 13 mmHg, respectively; Fig. 3A) at the beginning of the procedure. The atrio-His and the His-ventricular conduction interval during sinus rhythm were 50 and 45 ms, respectively. Retrograde conduction was observed during pacing from the right ventricle with the earliest atrial activation on the postero-lateral left atrium. The regular narrow QRS tachycardia was then induced by programmed stimulation without isoproterenol administration. Interestingly, the plasma BNP level and the PCWP elevated immediately after the induction of the tachycardia (Fig. 3B). The plasma BNP concentration 5, 10, 15, and 20 min after the induction of the tachycardia were 3.2, 29.6, 28.5, and 32.2 pg/ml, respectively. After 20 min, tachycardia was terminated by burst pacing from the right ventricle because the patient complained of dyspnea and the PCWP increased to 32 mmHg (Fig. 3C). The tachycardia was diagnosed to be orthodromic AVRT using the accessory pathway located postero-lateral of the mitral annulus. A 4-mm-tip steerable ablation catheter was then inserted via the femoral artery retrogradely through the aortic valve. Radiofrequency application along the 4 O’clock position on the mitral annulus resulted in the elimination of the accessory pathway during pacing from the ventricle. The BNP level returned to the normal range (4.6 pg/ml) by 1 day after the procedure. During the 6-month follow-up period following the ablation procedure, the patient was free from both tachycardia and heart failure without taking any medication.
Figure 3.
The increase in pulmonary capillary wedge pressure (PCWP) by tachycardia. (A) Intracardiac recordings and PCWP at the beginning of the procedure. The PCWP during sinus rhythm was within normal range (13 mmHg). (B) The endocardial electrograms and the PCWP 5 min after the induction of the supraventricular tachycardia. The earliest atrial activation during tachycardia was observed in the bipolar electrogram of the coronary sinus 5–6. The PCWP increased markedly to 24 mmHg. (C) Twenty minutes after the initiation of the tachycardia. The PCWP was 32 mmHg. HRA, high right atrium; CS, coronary sinus (1–2 = most distal pair, 9–10 = most proximal pair); HB, His bundle; RV, right ventricle; PCWP, pulmonary capillary wedge pressure; II and V1 represent recordings from 12-lead surface electrocardiogram.
Discussion
This report described a patient presenting acute progression of congestive heart failure due to orthodromic AVRT with a normal heart. There was a real time elevation of the PCWP and the plasma BNP concentration due to supraventricular tachycardia. Although either persistent or incessant supraventricular tachycardia induces congestive heart failure following LVEF reduction and LV dilatation [1], an acute collapse of the hemodynamic status by paroxysmal narrow QRS tachycardia is rarely observed in patients without LV systolic dysfunction or structural heart disease. Recurrent congestive heart failure was presented in this case with narrow QRS tachycardia, but the symptoms and 24-h electrocardiogram recordings show that it was neither the persistent nor incessant form. Tachycardia-induced cardiomyopathy is defined as atrial or ventricular dysfunction with LV dilatation and reduction in the LVEF, which reverse with the abolition of the tachycardia or appropriate ventricular rhythm control. However, the LV size and contraction were preserved both during the ongoing tachycardia and sinus rhythm even immediately after the termination of tachycardia in the present case, indicting the absence of tachycardia-induced cardiomyopathy.
The induction of AVRT produces an acute and marked rise in plasma atrial natriuretic peptide concentrations, which rapidly return to normal when the sinus rhythm is restored [6]. They suggested that the acute increase in atrial natriuretic peptide probably does not mediate a sudden change in the hemodynamics, but induces the acute natriuretic effect of paroxysmal tachycardia [6]. On the other hand, Tada et al. [7] demonstrated that the plasma BNP concentration exceeds the normal range in 56% of patients with idiopathic ventricular arrhythmia. In their study, the BNP concentration correlated with the frequency of premature ventricular contractions, thus suggesting that secretion of BNP is regulated mainly by wall tension, and an increase in the plasma BNP concentration may reflect ventricular structural and functional abnormalities. In this case, the marked elevation of the plasma BNP concentration was observed only during tachycardia. Moreover the PCWP was also within normal range at baseline and was simultaneously raised during tachycardia. These observations suggested that at least the AVRT played an important role in the collapse of the cardiovascular system in the present case, and was the main or possibly an independent factor in the congestive heart failure.
It is not clear whether the AVRT was an independent cause of congestive heart failure in this case. Although the unremarkable echocardiography parameters and the normal level of the plasma BNP during sinus rhythm at baseline could demonstrate the absence of any disorder of the cardiovascular system, the slightly elevated PCWP (13 mmHg) might indicate that this patient may have had heart disease with a normal LVEF including either tachycardia-induced cardiomyopathy with an improved LV function or early phase dilated cardiomyopathy. Furthermore, while the normal deceleration time and the ratio of the peak early diastolic velocity of transmitral flow to the peak early diastolic velocity of the mitral annulus suggested the absence of a severe diastolic dysfunction of the LV, the decrease in the transmitral early-to-late flow velocity ratio possibly indicated mild LV diastolic dysfunction. In the present case, no significant structural heart disease was detected by using non-invasive examination. However, tachycardia-induced cardiomyopathy, which usually results in LV dilatation or systolic dysfunction, could lead only to diastolic dysfunction by rapid arrhythmia. A further clinical follow-up should therefore be carried out to timely identify any hidden heart disease or unexpected cardiac events even after the elimination of tachycardia.
Acknowledgment
We are grateful to Dr. Brian Quinn (Department of Linguistic Environment, Kyushu University) for linguistic comments on the manuscript.
References
- 1.Cruz F.E., Cheriex E.C., Smeets J.L., Atié J., Peres A.K., Penn O.C., Brugada P., Wellens H.J. Reversibility of tachycardia-induced cardiomyopathy after cure of incessant supraventricular tachycardia. J Am Coll Cardiol. 1990;16:739–744. doi: 10.1016/0735-1097(90)90368-y. [DOI] [PubMed] [Google Scholar]
- 2.Shinbane J.S., Wood M.A., Jensen D.N., Ellenbogen K.A., Fitzpatrick A.P., Scheinman M.M. Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol. 1997;29:709–715. doi: 10.1016/s0735-1097(96)00592-x. [DOI] [PubMed] [Google Scholar]
- 3.Omichi C., Tanaka T., Kakizawa Y., Yamada A., Ishii Y., Nagashima H., Kanmatsuse K., Endo M. Improvement of cardiac function and neurological remodeling in a patient with tachycardia-induced cardiomyopathy after catheter ablation. J Cardiol. 2009;54:134–138. doi: 10.1016/j.jjcc.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Wilson J.R., Douglas P., Hickey W.F., Lanoce V., Ferraro N., Muhammad A., Reichek N. Experimental congestive heart failure produced by rapid ventricular pacing in the dog: cardiac effects. Circulation. 1987;75:857–867. doi: 10.1161/01.cir.75.4.857. [DOI] [PubMed] [Google Scholar]
- 5.Moe G.W., Grima E.A., Angus C., Wong N.L., Hu D.C., Howard R.J., Armstrong P.W. Response of atrial natriuretic factor to acute and chronic increases of atrial pressures in experimental heart failure in dogs. Role of changes in heart rate, atrial dimension, and cardiac tissue concentration. Circulation. 1991;83:1780–1787. doi: 10.1161/01.cir.83.5.1780. [DOI] [PubMed] [Google Scholar]
- 6.Burch M., Till J.A., Rigby M.L., Shinebourne E.A., Carter N.D., Jeffery S., Smith A. Plasma concentration of atrial natriuretic peptide in spontaneous atrioventricular re-entrant tachycardias of childhood. Br Heart J. 1990;64:317–320. doi: 10.1136/hrt.64.5.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tada H., Ito S., Shinbo G., Tadokoro K., Ito I., Hashimoto T., Miyaji K., Kaseno K., Naito S., Nogami A., Oshima S., Taniguchi K. Significance and utility of plasma brain natriuretic peptide concentrations in patients with idiopathic ventricular arrhythmias. Pacing Clin Electrophysiol. 2006;29:1395–1403. doi: 10.1111/j.1540-8159.2006.00553.x. [DOI] [PubMed] [Google Scholar]