Summary
A 49-year-old woman complaining of anterior chest pain underwent emergent coronary angiogram and thrombotic obstruction in the proximal left anterior descending artery was discovered. Deployment of a bare metal stent recovered good coronary flow and congestive heart failure was soon relieved. However, on day 3 of hospitalization, chest radiography suddenly showed newly emergent bilateral pulmonary infiltration shadow mimicking congestive heart failure. Chest computed tomography and clinical findings suggested bilateral alveolar hemorrhage. The patient received dual antiplatelet therapy, aspirin 100 mg/day and clopidogrel 75 mg/day and continuous 15,000 U/day heparin infusion, after percutaneous coronary intervention. Therapies that minimize bleeding risk while maintaining an antithrombotic effect are required for patients with acute coronary syndrome (ACS). Due to concern about the increased risk of early stent thrombosis induced by discontinuation of antiplatelet therapy, we continued to administer dual antiplatelet therapy. Pulmonary hemorrhage complicated with ACS without abciximab is a rare clinical entity, and we successfully overcame this potentially life-threatening complication with conservative therapy.
Keywords: Anticoagulants, Complications, Coronary artery disease
Introduction
Currently percutaneous coronary intervention (PCI) is widely performed all over the world, and multiple antiplatelet drugs have become standard therapy for preventing thrombotic events after PCI. However, bleeding complications during the treatment for acute coronary syndrome (ACS) is a relatively frequent non-cardiac event and sometimes associated with a poor hospital prognosis. Although pulmonary hemorrhage can be easily misdiagnosed as congestive heart failure on chest radiogram, we have to investigate the pathological entity as accurately as possible to achieve a better outcome for these patients.
Case report
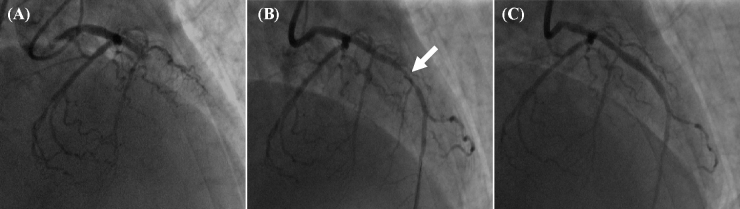
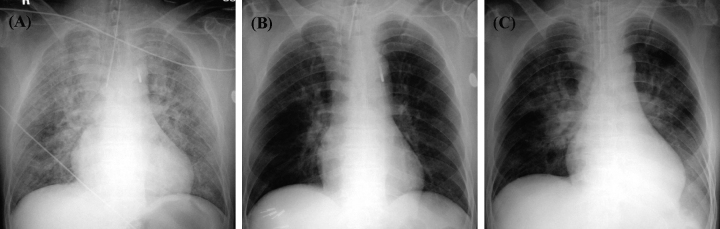
A 49-year-old medium-sized woman (body mass index = 21.4) who had been receiving medication therapy for diabetes mellitus (DM) consulted the emergency room complaining of sudden onset anterior chest pain in the early morning. Her only coronary risk factor was DM. Her blood pressure was 145/92 mmHg, and the pulse rate was 54/min with regular rhythm. A 12-lead electrocardiography demonstrated an elevated ST-segment in a wide range of anterior chest leads and ultrasound cardiography showed akinesis of broad apico-anterior wall of left ventricle. Laboratory study showed typical ACS findings of acute phase (Table 1). She was highly suspected of having acute apico-anterior myocardial infarction and underwent emergent coronary angiogram. Proximal left anterior descending artery (LAD) was totally occluded by thrombus (Fig. 1A) and PCI was continuously performed. During the PCI procedure, acute pulmonary congestion worsened rapidly and cardiogenic shock developed (Fig. 2A). The patient was intubated and artificial ventilation was started. Successful aspiration of red thrombus achieved LAD recanalization and demonstrated moderate LAD stenosis (Fig. 1B, Arrow). Then, bare metal stent deployment promptly achieved thrombolysis in myocardial infarction grade 3 flow under intra-aortic balloon pumping (IABP) support (Fig. 1C).
Table 1.
Laboratory data on admission.
| WBC | 10610/μl | LDH | 297 U/l |
| RBC | 3.95 × 106/μl | ALP | 655 U/l |
| Hgb | 11.7 g/dl | T-Bil | 0.2 mg/dl |
| Hct | 36.5% | CRP | 0.1 mg/dl |
| PLT | 25.3 × 104/μl | BS | 195 mg/dl |
| BUN | 26.4 mg/dl | TP | 6.8 g/di |
| Cre | 1.17 mg/dl | Alb | 3.6 g/di |
| Na | 138 mequiv./l | TG | 52 mg/dl |
| K | 3.9 mequiv./l | HDL-C | 39.4 mg/dl |
| Cl | 106 mequiv./l | LDL-C | 104.0 mg/dl |
| Amy | 78 IU/l | TropT | Positive |
| CPK | 217 U/l | PT | 113% |
| AST | 74 U/l | APTT | 24.9 s |
| ALT | 84 U/l | Fibrinogen | 440 mg/dl |
Alb, albumin; Amy, amylase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; ALT, alanine aminotransferase; APTT, activated partial thromboplastin time; BS, blood sugar; BUN, blood urea nitrogen; CPK, creatine phosphokinase; Cre, serum creatinine; CRP, c-reactive protein; Hct, hematocrit; HDL-C, high density lipoprotein cholesterol; Hgb, hemoglobin; LDH, lactate dehydrogenase; LDL-C, low density lipoprotein cholesterol; PLT, platelet count; PT, ptothrombin time; RBC, red blood cell count; T-Bil, total bilirubin; TG, triglyceride; TP, total protein; TropT, troponin T; WBC, white blood cell count.
Figure 1.
Emergent coronary angiogram showed obstruction of proximal left anterior descending artery (A). After aspiration of thrombus, stenotic lesion was shown in the mid-left anterior descending artery (B, arrow). Deployment of bare metal stent recovered thrombolysis in myocardial infarction grade 3 coronary flow and the procedure was successfully finished (C).
Figure 2.
Transition of images on chest radiogram. Severe pulmonary congestion was seen on coronary care unit admission (A). Pulmonary congestion quickly recovered on day 2 of hospitalization (B). Bilateral infiltration shadow appeared on day 3 (C).
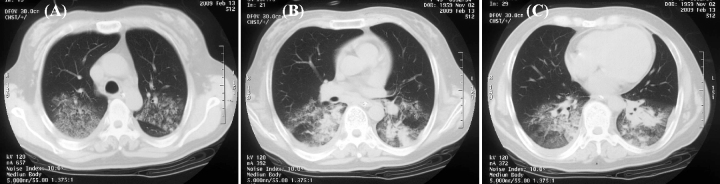
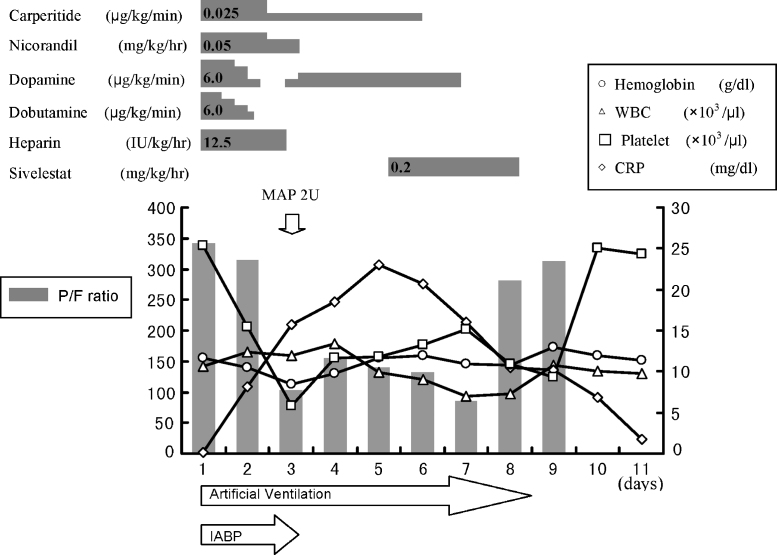
The patient was admitted to the coronary care unit. She received aspirin 200 mg and clopidogrel 300 mg loading dose in the emergency room. After admission, she received aspirin 100 mg/day and clopidogrel 75 mg/day from the stomach tube. Unfractionated heparin 15,000 U/day was also continuously dripped. Medication for congestive heart failure effectively improved her respiratory state. Chest radiography on day 2 of hospitalization showed remarkable improvement of pulmonary congestion compared with that on admission (Fig. 2B). However, on day 3 of hospitalization her blood oxygenation suddenly decreased and chest radiography demonstrated newly emergent bilateral pulmonary infiltration shadow (Fig. 2C). Chest computed tomography showed a ground-glass appearance with partial consolidation at the bilateral posterior lung field (Fig. 3). At the same time, some fresh blood was aspirated through the intubated tube, and her hemoglobin decreased from 10.5 mg/dl to 8.4 mg/dl. Findings suggested that her clinical pathology was derived from pulmonary hemorrhage rather than worsening of congestive heart failure. The activated coagulation time was measured as 170 s and platelet number was decreased to 58,000/μl. Therefore, we ceased continuous heparin infusion and discontinued IABP mechanical support. We then tried conservative treatment for pulmonary hemorrhage with continuous infusion of carbazochrome and tranexamic acid, and transfusion with 2 units of red cell concentrates mannitol adenine phosphate. Considering the patient's cardiac state, we continued dual antiplatelet therapy. Because of the persistence of a low PaO2/FiO2 (P/F ratio) score, we started sivelestat infusion and her respiratory state dramatically improved. She was extubated on day 8 of hospitalization (Fig. 4). Thereafter, she progressed well without relapse of either pulmonary hemorrhage or congestive heart failure. Cardiac rehabilitation after acute myocardial infarction gradually progressed, and she was finally discharged on day 30 of hospitalization.
Figure 3.
Chest computed tomography demonstrated bilateral ground-glass appearance with partial consolidation predominantly at the lower posterior lung field on day 3 of hospitalization. Images show the horizontal section just above the carina (A), below the carina (B), and at the level of mid-left ventricle (C).
Figure 4.
Changes in the medical treatment and clinical course during the early stage of hospitalization. CRP, C-reactive protein; IABP, intra-aortic balloon pumping; MAP, mannitol adenine phosphate; P/F ratio, PaO2/FiO2 ratio; WBC, white blood cells.
Discussion
In most cases of PCI in the modern era, stent deployment is a fundamental and very useful strategy. However, once stent thrombosis occurs, catastrophic results often follow. As reported by Schomig et al. [1] and Leon et al. [2], potent antiplatelet therapy is very useful for preventing stent thrombosis. Dual antiplatelet therapy has been reported to reduce the incidence of stent thrombosis to less than 1%. Currently dual antiplatelet therapy is a common strategy for interventional cardiologists after stent deployment, but we must remember that hemorrhagic complications caused by dual antiplatelet therapy occur as frequently as stent thrombosis.
Also in cases of ACS, a strategy of clopidogrel pretreatment followed by long-term therapy is reported to be beneficial in reducing major cardiovascular events [3]. That study also reported that there was less need for glycoprotein IIb/IIIa inhibitor in the clopidogrel group and there was no increase in major or life-threatening bleeding with clopidogrel use. However, when PCI is performed, we must always consider the risk of hemorrhagic complication. Major bleeding is a relatively frequent non-cardiac complication of contemporary therapy for ACS and it is associated with a poor hospital prognosis. Advanced age, female sex, history of bleeding, and renal insufficiency were independently associated with a higher risk of bleeding [4]. The GUSTO (Global Use of Strategies To Open Occluded Coronary Arteries) bleeding classification identifies patients who are at risk for short- and long-term adverse events [5]. The reason for the increased occurrence of cardiovascular events related to bleeding complication is that these patients show common risk factors such as advanced age or renal insufficiency as indicated above. Furthermore, to cope with those bleeding complications, we sometimes have to discontinue antiplatelet or anticoagulant drugs, which consequently lead to more frequent thrombotic events. Therapies that minimize bleeding risk while maintaining an anticoagulant effect may improve the outcomes of patients with ACS.
Bleeding problems from the gastrointestinal and genitourinary tract or arterial access are easily recognized. However, we must carefully monitor other possible but infrequent hemorrhagic complications. Pulmonary hemorrhage appears as a bilateral alveolar infiltration shadow on chest radiography and can be easily mistaken for acute pulmonary edema in the context of ACS [6]. When the infiltrates do not resolve with administration of drugs for congestive heart failure, cardiologists must be aware of the possibility of pulmonary hemorrhage because early treatment can increase the probability of patient survival.
Diffuse pulmonary hemorrhage is a rare event, which has mostly been reported in patients receiving glycogen IIb/IIIa inhibitors in combination with other antiplatelet drugs, such as aspirin, ticlopidine, and clopidogrel. Kalra et al. reported that severe pulmonary hemorrhage was identified in 0.27% patients who received abciximab, while there were no cases of pulmonary hemorrhage among 5412 patients who underwent coronary procedures without abciximab infusion [7].
Clopidogrel use related to alveolar hemorrhage without glycogen IIb/IIIa inhibitors has been infrequently reported to date. In the first report of this type of pathology, alveolar hemorrhage was controlled by ceasing clopidogrel use [8]. In the other case, the patient developed severe pulmonary hemorrhage and could not be resuscitated [9].
We successfully used the elastase inhibitor sivelestat that is usually applied for the treatment of acute lung injury (ALI). Although our patient did not strictly correspond to the criteria of ALI [10], she showed lower P/F ratio which is often applied for an index of respiratory dysfunction. From that point of view, we hoped the effect of this drug to improve her respiratory state.
We presented a case of pulmonary hemorrhage complicated with ACS. Multifactorial causes such as dual antiplatelet therapy, heparin infusion, thrombocytopenia, increased alveolar pressure induced by mechanical ventilation, and assumed pulmonary hypertension due to left ventricular dysfunction, were thought to be involved in the occurrence of pulmonary hemorrhage in our patient. Thrombocytopenia may be related to the pathophysiology of heparin-induced thrombocytopenia (HIT). However, no more information is available because further examination about HIT was not performed. Because our patient overcame her hemorrhagic complication without stopping antiplatelet use, strictly speaking, we cannot determine the direct correlation between antiplatelet therapy and the hemorrhagic event. However, there is no doubt that the use of multiple antiplatelet and anticoagulant drugs is involved in the increased risk of hemorrhagic events. Our patient is a case of relatively broader anterior myocardial infarction with lower cardiac function, which indicated that recurrent infarction caused by early stent thrombosis is quite capable of being fatal. Deciding to stop antiplatelet medicines in such a clinical setting could be fatal. Therefore, we continued dual antiplatelet therapy and were still able to achieve a better outcome. Making a quick and accurate diagnosis of the clinical pathology is of course important, and moreover, we have to fully consider the patient's background and current condition to determine an appropriate treatment policy.
References
- 1.Schomig A., Neumann F.J., Kastrati A., Schuhlen H., Blasini R., Hadamitzky M., Walter H., Zitzmann-Roth E.M., Richardt G., Alt E., Schmitt C., Ulm K. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996;334:1084–1089. doi: 10.1056/NEJM199604253341702. [DOI] [PubMed] [Google Scholar]
- 2.Leon M.B., Baim D.S., Popma J.J., Gordon P.C., Cutlip D.E., Ho K.K., Giambartolomei A., Diver D.J., Lasorda D.M., Williams D.O., Pocock S.J., Kuntz R.E. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. Stent Anticoagulation Restenosis Study Investigators. N Engl J Med. 1998;339:1665–1671. doi: 10.1056/NEJM199812033392303. [DOI] [PubMed] [Google Scholar]
- 3.Mehta S.R., Yusuf S., Peters R.J., Bertrand M.E., Lewis B.S., Natarajan M.K., Malmberg K., Rupprecht H., Zhao F., Chrolavicius S., Copland I., Fox K.A., Clopidogrel in Unstable angina to prevent Recurrent Events trial (CURE) Investigators Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001;358:527–533. doi: 10.1016/s0140-6736(01)05701-4. [DOI] [PubMed] [Google Scholar]
- 4.Moscucci M., Fox K.A., Cannon C.P., Klein W., Lopez-Sendon J., Montalescot G., White K., Goldberg R.J. Predictors of major bleeding in acute coronary syndromes: the Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2003;24:1815–1823. doi: 10.1016/s0195-668x(03)00485-8. [DOI] [PubMed] [Google Scholar]
- 5.Rao S.V., O’Grady K., Pieper K.S., Granger C.B., Newby L.K., Van de Werf F., Mahaffey K.W., Califf R.M., Harrington R.A. Impact of bleeding severity on clinical outcomes among patients with acute coronary syndromes. Am J Cardiol. 2005;96:1200–1206. doi: 10.1016/j.amjcard.2005.06.056. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez-Perez G.C., Vazquez M., Delgado C., Velasco M., Vazquez-Lima A., Rodriguez-Perez J. Pulmonary hemorrhage in a patient with acute coronary syndrome. Am J Roentgenol. 2007;189:W135–W137. doi: 10.2214/AJR.05.0786. [DOI] [PubMed] [Google Scholar]
- 7.Kalra S., Bell M.R., Rihal C.S. Alveolar hemorrhage as a complication of treatment with abciximab. Chest. 2001;120:126–131. doi: 10.1378/chest.120.1.126. [DOI] [PubMed] [Google Scholar]
- 8.Kilaru P.K., Schweiger M.J., Kozman H.A., Weil T.R. Diffuse alveolar hemorrhage after clopidogrel use. J Invasive Cardiol. 2001;13:535–537. [PubMed] [Google Scholar]
- 9.Gill D.S., Ng K., Ng K.S. Massive pulmonary haemorrhage complicating the treatment of acute coronary syndrome. Heart. 2004;90:e15. doi: 10.1136/hrt.2003.028589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernard G.R., Artigas A., Brigham K.L., Carlet J., Falke K., Hudson L., Lamy M., Legall J.R., Morris A., Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]