Abstract
BACKGROUND:
Rapid and effective pain relief in acute traumatic limb injuries (ATLI) is one of the most important roles of emergency physicians. In these situations, opioid addiction is an important concern because of the dependency on opioids. The study aims to compare the effectiveness of intravenous (IV) fentanyl versus morphine in reducing pain in patients with opioid addiction who suffered from ATLI.
METHODS:
In this double-blind randomized clinical trial, 307 patients with ATLI, who presented to the emergency department (ED) from February 2016 to April 2016, were randomly divided into two groups. One group (152 patients) received 0.1 mg/kg IV morphine. The other group (155 patients) received 1 mcg/kg IV fentanyl. Patients’ demographic data, pain score at specific intervals, vital signs, side effects, satisfaction and the need for rescue analgesia were recorded.
RESULTS:
Eight patients in the morphine group and five patients in the fentanyl group were excluded. Pain score in the fentanyl group had a significant decrease at 5-minute follow-up (P value=0.00). However, at 10, 30, and 60-minute follow-ups no significant differences were observed between the two groups in terms of pain score reduction. The rescue analgesia was required in 12 (7.7%) patients in the fentanyl group and in 48 (31.6%) patients in the morphine group (P value=0.00). No significant difference was observed regarding side effects, vital signs and patients’ satisfaction between the two groups.
CONCLUSION:
Fentanyl might be an effective and safe drug in opioid addicts suffering from ATLI.
Keywords: Fentanyl, Morphine, Opioid addiction, Acute traumatic limb injury, Pain score
INTRODUCTION
Pain is an unpleasant feeling and experience which is the result of acute or chronic injury to tissues. If not controlled appropriately, this unpleasant feeling can lead to adverse behavioral responses by the patient that will affect his/her quality of life in long-term (like its effect on sleep [insomnia], mood [fear and anxiety], brain [decrease in grey matter and memory problems] and sexual function [decreased libido] or cardiovascular health [hypertension and ischemic heart diseases]). Rapid and effective pain relief is considered as a humanistic action and is one of the basic rights of every patient.[1,2]
In the recent years, considerable amount of attention has been paid to narcotics for the purpose of pain alleviation, either acute or chronic. Use of these medications in their recommended dosages is routine in most emergency department (ED)s.[1,3] It should be noted that if such analgesics are used in more than their recommended dosages or used illegally, they could lead to opioid dependency. Opioid addicted patients are a special population in the field of pain management. Such patients are resistant to narcotic analgesics at standard dosages and thus they do not show appropriate response.[4, 5]
Intravenous (IV) morphine sulfate has a rapid onset of action near 1–2 minutes and it reaches a peak of action in 5–15 minutes; it has a half-life of 1.5–2 hours with a duration of action near 3–4 hours. The appropriate loading dose for acute sever pain is 0.1 mg/kg and this dose can be repeated as half the initial dose every 5–15 minutes.[6,7] Some studies have recommended that in addicts, it should be administered at higher doses; 10–15 mg for initial doses and continuous infusion thereafter.[4,5] Each morphine ampule contains 10 mg/mL and is diluted by 10 cc of distilled water to reach a dose of 1 mg/mL. For moderate to severe pain in an average adult who weighs 70 kg, 2–10 mg is routinely administered over 4–5 minutes. Its side effects include hypotension, bradycardia, seizures, confusion, itching, rash, and respiratory depression. Contraindications to its administration include allergy to morphine, asthma, upper airway obstruction, signs of overdose such as cold skin, respiratory depression, stupor, coma, and death.[6,7]
Besides morphine, another appropriate medication for pain relief and also induction of sedation, is fentanyl. Fentanyl has been used in anesthesiology since 1960. Different routes of administration make fentanyl a good choice in emergency situations.[7] Its onset of action is less than 60 seconds with a half-life of 90 minures and duration of action near 30–60 minutes. Its peak effect is 2–5 minutes. For deep sedation, fentanyl is administered at doses of 1–2 mcg/kg. For moderate sedation, it is used with midazolam and its dose is titrated. Fentanyl usually exerts its analgesic effect at 1–1.5 mcg/kg.[6,7] However, this dosage can be adjusted by the physician considering sedation and analgesia. Rarely, glottis spasm and chest tightness occur with dosages used in sedation. Most of the side effects of fentanyl can be reversed by naloxone.
Trans-mucosal fentanyl with a-10 to 30-minute onset of action, in the form of candy lollipop, has been used in children anesthesia (with maximum dose of 10–15 mcg/kg). However, this form has not been used extensively in sedation due to the high risk of nausea (20%–40%).[8,9]
IV fentanyl has an appropriate effectiveness in acute pain relief and suitable doses have comparable effects to morphine with shorter onset of action.[10,11] Acceptable pain relief of fentanyl has been reported in many studies.[12,13]
The objective of this study aims to compare the analgesic effect of IV fentanyl versus morphine in patients with severe pain induced by acute traumatic limb injury (ATLI) who were opioid addicted.
METHODS
Participants and drug administration
This was a double blind randomized clinical trial with block randomization. The study population included patients who were addicted to opioids and presented with acute pain of traumatic limb injury. They were admitted to the EDs of Shariati and Sina hospitals in Tehran, from February 2016 to April 2016. The study was approved by the ethics committee of Tehran University of Medical Sciences and the IRCT registration number was IRCT201601308872N10.
Inclusion criteria were all patients older than 18 years with pain score more than 5, who suffered from ATLI and were addicted to opioids. Addiction to opioids is a primary condition manifesting as uncontrollable cravings, inability to control opioid use, compulsive use and use despite doing harm to oneself or others. Our criterion for addiction was daily compulsive usage of opioids (daily dependency on opium). Pain severity index was documented using the numerical rating scale (NRS) which is a 10-cm scale from 0 to 10. Sore of 0 means no pain and score of 10 means most severe pain. Our exclusion criteria included history of allergic reactions to fentanyl or morphine, Glasgow Coma Scale (GCS) score less than 14, pain severity score less than 5 (based on NRS), unstable hemodynamic status (systolic blood pressure [SBP] <90 mmHg) at the time of entrance to the study.
After getting written informed consent and description of our study objectives, patients were asked to score their pain level based on the NRS. Then the patients were randomly assigned to one of the two study groups. One group received IV morphine sulfate with a dose of 0.1 mg/kg (Morphine, ampule of 10 mg/1 cc, Darou Pakhsh Co., Tehran, Iran). The other group received IV fentanyl hydrochloride with dosage of 1 mcg/kg (Fentanyl, ampule of 0.5 mg in 10 cc, Abu Raihan Co., Tehran, Iran). The treating emergency physician confirmed diagnosis and contacted the chief investigator. Based on the code in block randomization, patients entered either group and only the chief investigator and the triage nurse were aware of the assignment and group. The specified drug and dose were provided by the triage nurse based on the code and it was injected slowly to the patient by the treating emergency physician who was blinded to the study.
Heart rate (HR), SBP, diastolic blood pressure (DBP), respiratory rate (RR), and oxygen saturation (O2sat) were documented before and after the intervention. Patients’ pain score, vital signs, satisfaction and drugs’ side effects were reported at 5, 15, 30 and 60 minutes after the intervention. If the patients’ pain score did not decrease to less than 3 cm or if the pain did not decrease to less than 50% of the initial score after 60 minutes, rescue analgesia with IV ketorolac 60 mg was administered. Patients’ satisfaction of pain relief was recorded by a Likert scale from 1 to 5 “completely satisfied”, “partially satisfied”, “neither satisfied nor dissatisfied”, “partially dissatisfied”, and “completely dissatisfied”. Major drugs’ adverse effects on cardiopulmonary or cerebrovascular system (respiratory or cardiac arrest, symptomatic bradycardia or loss of consciousness) were closely monitored and managed appropriately if occurred. Naloxone or atropine was ready to use in these situations. Standard cardiopulmonary resuscitation steps were taken when necessary.
Primary and secondary outcomes
Our primary outcome was to compare pain score (NRS) changes during the study time intervals. Our secondary outcomes were comparison of vital signs, side effects, patients’ satisfaction and the need for rescue analgesia.
Statistical analysis and sample size calculation
Based on Smith et al[14] study, we calculated a sample size of 307 (d=0.8, power=80%, SD1=2.4, SD2=2.7). After gathering all data, they were inserted into SPSS software (ver. 22.0). The descriptive indices such as frequency (percentage) and mean (standard deviation, SD) were used to express the results. To compare the two groups regarding pain scores, analysis of variance (ANOVA) or t-test for data with normal distribution was used and in case of data without normal distribution, non-parametric tests were used. To compare the qualitative variables, Chi-squared test or Fischer’s exact test was used. The level of significance was 0.05. In order to compare mean scores of the data in follow-ups, ANOVA test with repeated measures was used.
RESULTS
In the morphine group 8 patients were excluded: 4 did not have desire to continue, 2 used opium after receiving morphine, and 2 had depressed level of consciousness. In the fentanyl group 5 patients were excluded: 2 had depressed level of consciousness and 3 did not have desire to continue. Finally, 152 cases remained in the morphine group and 155 cases were studied in the fentanyl group (Figure 1).
Figure 1.
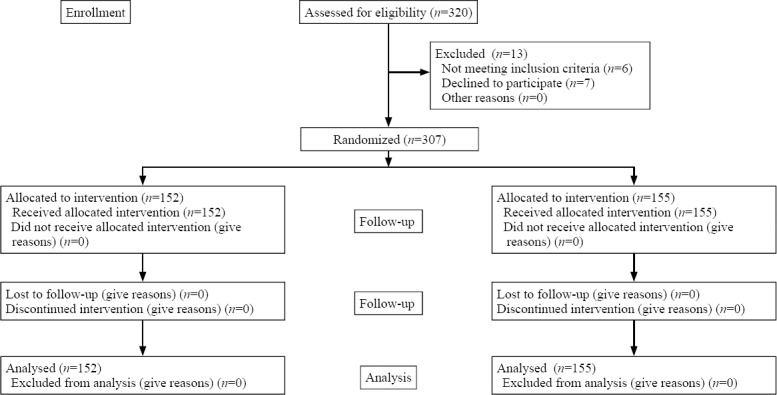
Flow diagram of the patient selection.
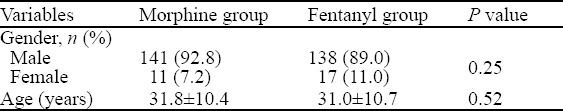
Mean±SD age of the participants was 31.45±10.57 years old (most were between 18–66). There were 279 (90.9%) males and 28 (9.1%) females. Age and gender distributions showed no significant differences between the two groups. Data were shown in Table 1.
Table 1.
Demographic data distribution between the two groups
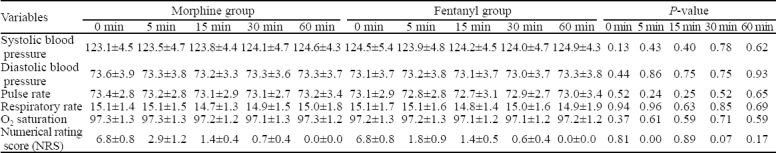
Vital signs had no significant differences between the two groups at the beginning of the study and also during different time intervals. Regarding pain severity, a significant difference was observed only at 5-minute follow-up (P value=0.00) which showed patients in the fentanyl group had less pain perception at 5 minutes compared to the morphine group. However, at 10-, 30-, and 60-minute follow-ups no significant differences were noted between the two groups. Data were shown in Table 2.
Table 2.
Comparison of the vital signs and pain scores between the two groups
All of our patients were carefully monitored. No cardiac or respiratory adverse events were observed but the only side effects happened were nausea and vomiting, 28 (18.4%) patients in the morphine group and 17 (11.0%) patients in the fentanyl group with no statistically significant difference (P value=0.06). At the end of our study, 83.5% patients in the morphine group and 87.5% in the fentanyl group reported that they were totally satisfied with the amount of pain reduction. We also noticed that 2.6% patients in the morphine group and 0.7% in the fentanyl group were totally dissatisfied with the medication. Patients’ satisfaction showed no significant difference between the two groups (P value=0.13). The rescue analgesia, 60 mg IV ketorolac was administered in 60 patients in our study. After 60 minutes of opioid administration, pain was not controlled in 12 (7.7%) patients in the fentanyl group and in 48 (31.6%) patients in the morphine group. This rate had a significant difference between the two groups (P value=0.00).
DISCUSSION
Pain relief is an important priority for emergency physicians, particularly in trauma patients suffering from severe pain. Most of ATLIs are the result of traffic accidents, falls or assaults. Pain and long waiting times for diagnostic and therapeutic interventions are major causes of dissatisfaction among trauma patients. Using analgesics such as narcotics is a routine measure to alleviate pain of such patients. In addicted patients, routine and standard administration of morphine may not lead to significant pain relief. Yet, higher doses may lead to adverse events. Therefore, it seems a good idea to consider other analgesics like fentanyl in such patients.
Addiction put patients at high risk of incorrect management of their pain. Three items are important in managing these patients. Firstly, issues related to the addicted person such as the method of abusing illegal drugs, changes in pain perception, and the method of administering analgesics and subsequent follow-ups. Secondly, drug interactions between the administered analgesics and the abused illegal drug are important. For example, the mortality risk can be increased when opioids are prescribed for patients on alcohol, sedatives, hypnotics or anxiolytics. Thirdly, many diseases and complications develop as the result of prolonged drug abuse such as psychiatric disturbances, chronic physical diseases (cancer), ischemic heart disease and chronic obstructive pulmonary disease.[15]
Mehta et al[16,17] in 2006 revealed that, in general, addicted patients experienced less pain decrease compared to other patients. Most pain managements done for such patients were based on the type of drug abused, background status of the patient, and duration of drug abusing. It was suggested to use bolus opioids with higher therapeutic dosages at specified intervals. Trans-dermal opioid patches as well as implantable pumps could provide gradual release of medication. Some especial drug delivery systems were introduced to deliver more appropriate short-acting opioids to these patients.
Fentanyl has been administered for acute pain relief since long ago. Furyk et al[18] compared inhalational fentanyl versus IV morphine in pediatric patients suspected of having broken limbs in emergency department in Australia. They revealed that there were no significant differences between the two groups regarding decrease in pain scores, vital signs or side effects.
In a study by Smith et al,[14] the analgesic effectiveness and side effects of the two medications were assessed in traumatic patients transferred by helicopter to hospitals. They concluded that no significant differences were observed in the amount of pain relief, nausea and vomiting between the two groups.
In our study, a substantial number of patients were young adults. This can be expected regarding demographics of the addicted patients in our country. Since age and gender were distributed evenly between the two groups, no statistically significant differences were observed in these variables between the two groups. We found that pain severity index was decreased gradually during the study intervals within each group. The only significant change observed in our study was more pain reduction at 5 minutes by fentanyl. Patients in the morphine group required more frequent doses of rescue analgesia (12 [7.7%] patients in the fentanyl group versus 48 [31.6%] patients in the morphine group; P value=0.00). We concluded that both morphine and fentanyl’s side effects were unremarkable.
Galinski et al[19] compared the analgesic effectiveness of fentanyl versus morphine in traumatic and non-traumatic patients in pre-hospital setting. Their results showed that no significant difference in the pain reduction was found between the two groups. In their study about 62% patients in the morphine group and 76% in the fentanyl group reported satisfactory pain management. Side effects showed no significant difference between the two groups. The authors concluded that fentanyl had comparable effects to morphine and they suggested to use fentanyl in acute severe pain in pre-hospital setting.
One of the concerns in administering fentanyl might be its cardiovascular and respiratory effects.[10,20,21] The current findings showed that fentanyl caused no considerable changes in cardiovascular or respiratory system. Our study showed that there was no significant difference in the side effects between the two groups.
As more opioid addicted patients nowadays are resistant to morphine analgesic effects, fentanyl might be a good alternative in case of morphine failure to control severe pain.
Limitation
Some of addict patients concealed their addiction in the first visit because of the negative social impact on their caretakers. One limitation of our study was that we did not follow patients after 60 minutes. Fentanyl is a short acting opioid while morphine is a long acting one. Our sample size was not sufficient to detect the exact drugs’ effects and adverse events. Further clinical trials with larger sample sizes and longer follow-up should therefore be performed to identify adverse events.
CONCLUSION
Our study showed that fentanyl can decrease pain more rapidly than morphine in opioid addicted patients with less adverse effects. More patients in the morphine group (48 [31.6%] patients) needed rescue analgesia.
Footnotes
Funding: None.
Ethical approval: The study was approved by the ethics committee of Tehran University of Medical Sciences.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: HSMV proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.No authors listed. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–226. [PubMed] [Google Scholar]
- 2.Somerville MA. Opioids for chronic pain of non-malignant origin--coercion or consent? Health Care Anal. 1995;3(1):12–4. doi: 10.1007/BF02197188. [DOI] [PubMed] [Google Scholar]
- 3.Collett BJ. Chronic opioid therapy for non-cancer pain. Br J Anaesth. 2001;87(1):133–43. doi: 10.1093/bja/87.1.133. [DOI] [PubMed] [Google Scholar]
- 4.Shao E, Hughes J, Eley R. The presenting and prescribing patterns of migraine in an Australian emergency department:A descriptive exploratory study. World J Emerg Med. 2017;8(3):170–6. doi: 10.5847/wjem.j.1920-8642.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta V, Langford RM. Acute pain management for opioid dependent patients. Anaesthesia. 2006;61(3):269–76. doi: 10.1111/j.1365-2044.2005.04503.x. [DOI] [PubMed] [Google Scholar]
- 6.Miner JR. Pain management. In: Marx JA, editor. Rosen's emergency medicine. Philadelphia: Elsevier Saunders; 2014. pp. 31–49. [Google Scholar]
- 7.Ducharme J. Acute pain management. In: Tintinalli JE, editor. Tintinalli's emergency medicine. McGraw-Hill; 2016. pp. 231–8. [Google Scholar]
- 8.Fine PG, Streisand JB. A review of oral transmucosal fentanyl citrate:potent, rapid and noninvasive opioidanalgesia. J Palliat Med. 1998;1(1):55–63. doi: 10.1089/jpm.1998.1.55. [DOI] [PubMed] [Google Scholar]
- 9.Schechter NL, Weisman SJ, Rosenblum M, Bernstein B, Conard PL. The use of oral transmucosal fentanyl citratefor painful procedures in children. Pediatrics. 1995;95(3):335–9. [PubMed] [Google Scholar]
- 10.Shrestha R, Pant S, Shrestha A, Batajoo KH, Thapa R, Vaidya S. Intranasal ketamine for the treatment of patients with acute pain in the emergency department. World J Emerg Med. 2015;7(1):19–24. doi: 10.5847/wjem.j.1920-8642.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Streisand JB, Stanley TH, Hague B, van Vreeswijk H, Ho GH, Pace NL. Oral transmucosal fentanyl citrate premedication in children. Anesth Analg. 1989;69(1):28–34. [PubMed] [Google Scholar]
- 12.Borland M, Jacobs I, King B, O'Brien D. A randomized controlled trial comparing intranasal fentanyl to intravenous morphine for managing acute pain in children in the emergency department. Acute Pain. 2007;9(2):100. doi: 10.1016/j.annemergmed.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 13.Mercadante S, Villari P, Ferrera P, Casuccio A, Mangione S, Intravaia G. Transmucosal fentanyl vs. intravenous morphine in doses proportional to basal opioid regimen for episodic-breakthrough pain. Br J Cancer. 2007;96(12):1828–33. doi: 10.1038/sj.bjc.6603811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith MD, Wang Y, Cudnik M, Smith DA, Pakiela J, Emerman CL. The effectiveness and adverse events of morphine versus fentanyl on a physician-staffed helicopter. J Emerg Med. 2012;43(1):69–75. doi: 10.1016/j.jemermed.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 15.Oliver J, Coggins C, Compton P, Hagan S, Matteliano D, Stanton M, et al. American Society for Pain Management nursing position statement:pain management in patients with substance usedisorders. J Addict Nurs. 2012;23(3):210–22. doi: 10.1097/JAN.0b013e318271c123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehta V, Langford RM. Acute pain management for opioid dependent patients. Anaesthesia. 2006;61(3):269–76. doi: 10.1111/j.1365-2044.2005.04503.x. [DOI] [PubMed] [Google Scholar]
- 17.Compton P, Charuvastra VC, Ling W. Pain intolerance in opioid-maintained former opiate addicts:effect of long-acting maintenance agent. Drug Alcohol Depend. 2001;63(2):139–46. doi: 10.1016/s0376-8716(00)00200-3. [DOI] [PubMed] [Google Scholar]
- 18.Furyk JS, Grabowski WJ, Black LH. Nebulized fentanyl versus intravenous morphine in children with suspected limb fractures in the emergency department:a randomized controlled trial. Emerg Med Australas. 2009;21(3):203–9. doi: 10.1111/j.1742-6723.2009.01183.x. [DOI] [PubMed] [Google Scholar]
- 19.Galinski M, Dolveck F, Borron SW, Tual L, Van Laer V, Lardeur JY, et al. A randomized, double-blind study comparing morphine with fentanyl in prehospital analgesia. Am J Emerg Med. 2005;23(2):114–9. doi: 10.1016/j.ajem.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Curtis KM, Henriques HF, Fanciullo G, Reynolds CM, Suber F. A fentanyl-based pain management protocol provides early analgesia for adult trauma patients. J Trauma. 2007;63(4):819–26. doi: 10.1097/01.ta.0000240979.31046.98. [DOI] [PubMed] [Google Scholar]
- 21.Claxton AR, McGuire G, Chung F, Cruise C. Evaluation of morphine versus fentanyl for postoperative analgesia after ambulatory surgical procedures. Anesth Analg. 1997;84(3):509–14. doi: 10.1097/00000539-199703000-00008. [DOI] [PubMed] [Google Scholar]


