Abstract
BACKGROUND:
We aimed to describe the current practice of emergency physicians and anaesthesiologists in the selection of drugs for rapid-sequence induction (RSI) among trauma patients.
METHODS:
A prospective survey audit was conducted based on a self-administered questionnaire among two intubating specialties. The preferred type and dose of hypnotics, opioids, and muscle relaxants used for RSI in trauma patients were sought in the questionnaire. Data were compared for the use of induction agent, opioid use and muscle relaxant among stable and unstable trauma patients by the intubating specialties.
RESULTS:
A total of 102 participants were included; 47 were anaesthetists and 55 were emergency physicians. Propofol (74.5%) and Etomidate (50.0%) were the most frequently used induction agents. Significantly higher proportion of anesthesiologist used Propofol whereas, Etomidate was commonly used by emergency physicians in stable patients (P=0.001). Emergency physicians preferred Etomidate (63.6%) and Ketamine (20.0%) in unstable patients. The two groups were comparable for opioid use for stable patients. In unstable patients, use of opioid differed significantly by intubating specialties. The relation between rocuronium and suxamethonium use did change among the anaesthetists. Emergency physicians used more suxamethonium (55.6% vs. 27.7%, P=0.01) in stable as well as unstable (43.4 % vs. 27.7%, P=0.08) patients.
CONCLUSION:
There is variability in the use of drugs for RSI in trauma patients amongst emergency physicians and anaesthesiologists. There is a need to develop an RSI protocol using standardized types and dose of these agents to deliver an effective airway management for trauma patients.
Keywords: Rapid-sequence induction, Trauma, Emergency physicians, Anaesthetists, Drugs
INTRODUCTION
Rapid-sequence induction (RSI) is an established airway management technique for emergency endotracheal intubation in trauma patients. However, exception may be anticipated for difficult airway.[1] This technique is being utilized by anaesthesiologists and physicians, in the emergency situation at the scene, upon arrival to emergency department (ED) and in the intensive care unit.[2] There is considerable heterogeneity in the pathophysiology of trauma patients, involvement of different specialities (operators) and availability of various induction agents which introduces complexity in the RSI procedure.[3] It is crucial to avoid pharmacological as well as physiological (hypotension and hypoxia) derangements during early resuscitation in brain injury patients to prevent haemorrhage or secondary insults.[4] Trauma-induced hypotension during RSI might aggravate brain injury and ischemia. Particularly, in brain injury patients, a significant drop in the mean arterial pressure could be detrimental resulting in poor outcomes.[5]
An ideal RSI agent must have wider prospects of safety and the dose regimen should be straightforward; would not require reconstitution or dilution.[4] Several induction agents, analgesics, and muscle relaxants are available to use. However, the selection of the best combination of induction agents, muscle relaxant and opioid remains controversial. Fentanyl and morphine are the most frequently used opioid analgesics in the operating room and in intensive care unit.[6] A disadvantage of morphine is its long onset time limiting its use in RSI.[7] Remifentanil is a selective µ-opioid receptor agonist which is an ideal drug for RSI due to its rapid onset and cessation of its effect. Also, there is no need for dose adjustment in the presence of organ dysfunction, and it is metabolised into inactive products. However, the time required for reconstitution of the drug and the lack of familiarity of non-anaesthetists make remifentanil a second-line drug for RSI.[8] There is a lack of consensus on the factors affecting the choice or preference of healthcare providers toward induction agents for RSI in trauma settings. The current literature suggest that the existing diversity regarding choice of drugs for RSI might be at least country specific.[8,9] Therefore, the aim of the present study is to describe the current practice of emergency physicians and anaesthesiologists with respect to the selection of drugs for RSI in trauma patients in a single institute with a level I trauma centre.
METHODS
Study design and setting
A prospective survey audit was conducted among the emergency physicians and anaesthesiologists involved in emergency RSI of adult trauma patients at the only level I trauma centre, Hamad General Hospital, Doha between 15 June 2017 and 15 July 2017.
Selection of participants
All anaesthesiologists and emergency physicians who are potentially involved in intubating level I trauma patients were included in this audit. The survey was carried out during normal working hours. Forty-seven residents, specialists, consultants and senior consultants of the anaesthesia department and 55 emergency physicians participated in the study.
Methods and measurements
During working hours, a self-administered questionnaire was distributed to all the physicians and anaesthesiologists who volunteer to participate at the Hamad General Hospital. The questionnaire was based on a previous online survey (SurveyMonkey, San Mateo, CA, USA) and modified for the purpose of our study to enable comparison of RSI protocol introduced recently in the United Kingdom with that of Emergency Medical Service (EMS) in Qatar. Before the interview, all participants were informed that their participation was voluntary and their responses were kept anonymous and kept confidential. The data variables in the questionnaire included the preferred type and dose of hypnotics, opioids, and muscle relaxants used for RSI in trauma patients. RSI was strictly defined as the administration of a potent intravenous sedative or anesthetic agent (including thiopentone, etomidate, propofol and ketamine with or without adjunctive opioids such as fentanyl or alfentanil), immediately followed by the administration of an intravenous neuromuscular blocking agent, usually suxamethonium, to perform emergency endotracheal intubation.[10] RSI was performed with recommended doses of induction agents such as midazolam, etomidate, ketamine, propofol, followed by the administration of neuromuscular depolarizing blocker (succinylcholine 1–2 mg/kg) and/or non-depolarizing neuromuscular blocking agent (Rocuronium 0.9–1.2 mg/kg). This audit has been granted approval from the Medical Research Centre at Hamad Medical Corporation (MRC #16404/16 quality improvement/audit study).
Statistical analysis
Data were presented as proportions, medians (range), or mean (± standard deviation; SD) as appropriate. Comparison for the use of induction agent, opioid use and muscle relaxant among stable and unstable trauma patients by anaesthetists and emergency physicians were analysed using chi-square test. A significant difference was considered when the 2-tailed P value was < 0.05. Data analysis was carried out using the Statistical Package for Social Sciences version 18 (SPSS Inc., Chicago, IL).
RESULTS
A total of 102 participants from two intubating specialties were included; of which 47 questionnaires were responded by the anaesthesiologist and 55 questionnaires were completed by the emergency physicians. Table 1 shows the comparison for the use of induction agent in trauma patients by the two intubating specialties. In stable trauma patients, Propofol (74.5%) was the most frequently used induction agent (hypnotic) followed by Etomidate (20.6%), Ketamine (2.9%) and Midazolam (2.0%). Significantly higher proportion of anesthesiologist used Propofol (95.7% vs. 56.4%) whereas, Etomidate (36.4% vs. 2.1 %, P=0.001) was commonly used by emergency physicians. On the other hand, Etomidate (50.0%) was the preferred hypnotic drug of choice used in unstable pateints choosen by the two intubating specialties. Moreover, choice among the emergency physicians was in favour of Etomidate (63.6%) and Ketamine (20.0%) in unstable patients while, anesthesiologist preferred equally propofol and ketamine as the drug of choice for induction of anaesthesia.
Table 1.
Comparison for the use of induction agent in trauma patients (n, %)
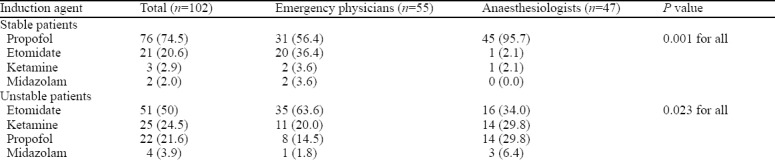
Table 2 shows the use of opioid in trauma patients by the two intubating specialties. In stable trauma patients, Fentanyl was used by 93% of the participants. The two groups were comparable for opioid use, as 97.8% anaesthetists and 89.1% of the emergency physicians used fentanyl. One anesthesiologist preferred remifentanil, whereas one (1.8 %) emergency physician did not use opioids at all and 5 (9.1%) preferred morphine (P=0.09).
Table 2.
Comparison for the use of opioid in trauma patients (n, %)
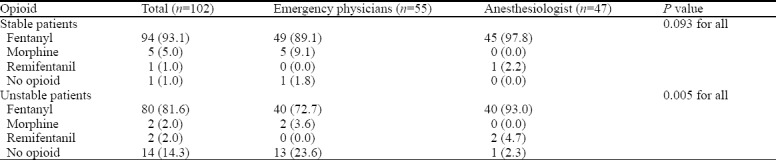
In unstable trauma patients, the use of opioid differed significantly by intubating specialties, as 93% of the anaesthetists preferred fentanyl, 2.3% preferred intubation without any opioid and 4.7% preferred remifentanil (P=0.005 for all). Also 72.7% of the emergency physicians would use fentanyl but none of them used remifentanil. However, 23.6% would intubate without any opioid and 3.6% would choose morphine over all other opioids.
Table 3 compares the use of muscle relaxant in trauma patients by the two intubating specialties. The majority of the anaesthetists used rocuronium (70.2%) as the preferred choice of muscle relaxant for RSI followed by suxamethonium (27.7%). Emergency physicians preferred suxamethonium (55.6%) over rocuronium (44.4%).
Table 3.
Comparison for the use of muscle relaxant in trauma patients (n, %)
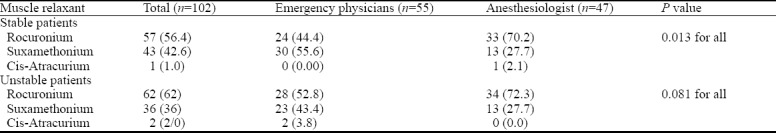
Except one, all anaesthetists choose the same muscle relaxant for stable and unstable trauma patients. With one exception, the relation between rocuronium and suxamethonium did not change among the anaesthetists in stable and unstable trauma patients. In contrast, emergency physicians used more suxamethonium (55.6% vs. 27.7%, P=0.01) in stable as well as unstable (43.4 % vs. 27.7%, P=0.08) trauma patients as compared to anaesthetists.
DISCUSSION
The present survey supports findings in the literature indicating that most participants choose fentanyl as the preferred opioid in RSI for stable and unstable trauma patients. The dosages used were around 30% less in unstable trauma patients than in stable trauma patients. Only one anaesthetist chose to use remifentanil in stable trauma patients, while two anaesthetists chose to use remifentanil in unstable trauma patients. Morphine was not chosen at all. Compared to our findings, a recent national survey from the United Kingdom revealed that a larger variety of opioids was used for RSI.[8] In this survey, 64.3% of the consultants and 35.6% of the trainees chose fentanyl followed by alfentanil, remifentanil and morphine.
Even though there is no common agreement on the use of specific drugs for RSI in trauma patients there seems to be a common trend. There is a general tendency towards the use of fentanyl, more ketamine since resolution of the myth not to use ketamine in traumatic brain injury and rocuronium since introduction of its antagonist sugammadex (a selective relaxant binding agent). These findings clearly support our survey. More than 90% of the physicians involved in the airway management care of stable trauma patients choose fentanyl, and in unstable trauma patients a shift away from propofol in favour of ketamine could be detected. Even though in the ED the use of suxamethonium is still widespread in stable trauma patients there is a slight shift towards rocuronium visible in unstable trauma patients catching up with most of the interviewed anaesthetists, the majority of whom prefer rocuronium.
However, guidelines with more detailed drug recommendations particularly from the Scandinavian society[11] or parts of Australia[12] are still inconsistent. In Qatar, for instance, opioids such as alfentanil and sufentanil are not available and therefore not a choice, even though alfentanil would be a suitable option according to several studies.[13,14] The drugs mentioned in the Scandinavian and the Australian guidelines are thought to cover a much broader spectrum of pre-hospital patients requiring intubation. However, our survey was mainly focused on trauma patients.
Concerning the use of opioids the Scandinavian guidelines, comprising the agreement between Denmark, Finland, Iceland, Norway and Sweden proposed by the Clinical Practice Committee of the Scandinavian Society of Anaesthesiology and Intensive Care Medicine state that an opioid should be used to blunt the hemodynamic response to the endotracheal intubation (Grade C recommendation).[11] According to these recommendations, either alfentanil 15–40 µg/kg[15] or remifentanil 1 µg/kg is suitable to avoid hemodynamic complications to blunt hemodynamic response and to avoid intubation pain-related rise in the blood pressure. The committee summarized the hemodynamic response to tracheal intubation depending on the combination used with the hypnotics. Studies showed that depending on the combination of hypnotic and opioid, around 2–3 µg/kg will attenuate but not abolish the hemodynamic response to intubation.[16]
The muscle relaxant, suxamethonium, has been used for decades and remains popular. Rocuronium was introduced in the market from 1994 in the United States. Since then, it has gained worldwide popularity in RSI. Since its antagonist sugammadex has been approved for the reversal of neuromuscular blockade induced by rocuronium, it is increasingly becoming the preferred drug for indication. The fact that introduction of sugammadex as a reversal of rocuronium onto the market pushed the use of rocuronium in RSI was supported by a study amongst German anaesthetists.[17] This survey showed a massive shift to the use of rocuronium, from suxamethonium from a 20:1 ratio in 2003 to a 2:1 ratio in 2013 which is contradictory to our findings. The majority of anaesthetists use rocuronium and the relation to suxamethonium (approximately 2:1) remains the same in stable and unstable trauma patients. In our study, the emergency physicians choose both drugs almost equally often with a tendency towards suxamethonium in stable trauma patients and rocuronium in unstable trauma patients. An explanation for this shift is not clear. However, the introduction of sugammadex may have contributed to a general change in practice.[18] In 2008, there was an increasing evidence for the use of high-dose rocuronium, which provided as good intubating conditions as suxamethonium.[19] A Cochrane systematic review concluded that suxamethonium created superior intubation conditions as compared to rocuronium.[20] However, this Cochrane review included also studies in which rocuronium dosage of 0.6 mg/kg has been used which is not the recommended dosage for RSI. That might be the reason why some studies indicated that the intubating conditions produced by rocuronium 1.2 mg/kg are as good as those using suxamethonium. Sugammadex at a dose of 16 mg/kg however, antagonizes the neuromuscular block of rocuronium more predictably than spontaneous recovery from suxamethonium.[21,22] The assumption that greater predictability of the reversal of neuromuscular block could be the reason for the increased use of rocuronium was addressed by Lyon et al.[4] These investigators clearly showed the superiority of rocuronium over suxamethonium with respect to laryngoscopic view and higher first-attempt intubation success.
A national survey for the current practice of RSI throughout the United Kingdom revealed that consultant anaesthetists are more likely to choose rocuronium as compared to trainees.[8] The authors indicated that rocuronium would be chosen for elective patients with an aspiration risk, for patients with an anticipated difficult airway, and in situations in which suxamethonium is contraindicated. That survey also revealed a slight tendency towards suxamethonium use. A minority (18%) of respondents of the survey used only suxamethonium for all patients and 6% used only rocuronium for all patients. Most anaesthetists (56%) used suxamethonium, and rocuronium was used in selected patients. Fifty-two (20%) respondents usually use rocuronium, but they chose to use suxamethonium in selected patients.
A recent study from India for RSI in patients with head injury revealed the predominant use of rocuronium over suxamethonium.[9] However, the ratio was less impressive as compared to the other study from Germany.[17] In the Indian study, most of the anaesthetists used rocuronium (44%), followed by suxamethonium (39%). The overall trend towards rocuronium is also supported by our survey; however, the lack of earlier data unfortunately reduces the comparability to other countries. Irrespective of the country of RSI training, most anaesthetists used rocuronium. Contradicting the findings from the United Kingdom, trainees and more-experienced anaesthetists in survey used rocuronium at nearly the same frequency.
It is possible to conduct a modified RSI technique using non-depolarising muscle relaxants such as atracurium and cis-atracurium.[23] There is no enough evidence to support the benefit of using this technique.[24] However, the Scandinavian countries are using guidelines concerning the clinical practice on general anaesthesia for emergency settings which recommend the use of suxamethonium.[11] In case of contraindications to succinylcholine, rocuronium 0.9–1.2 mg/kg is recommended as an appropriate alternative.
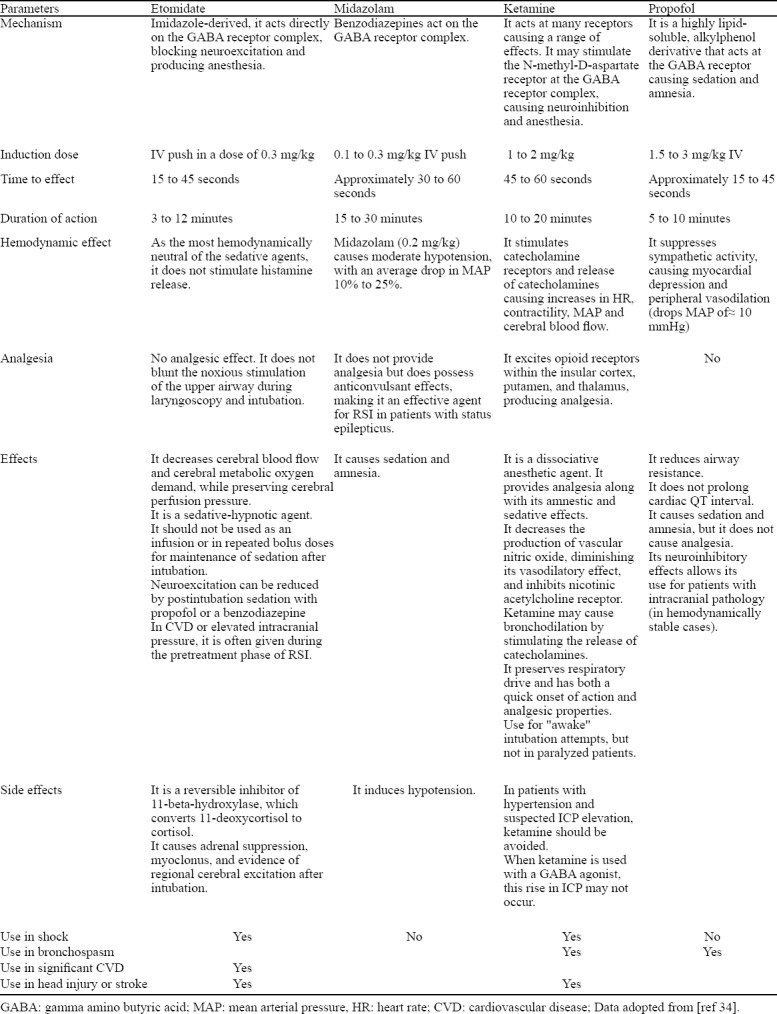
The most commonly used hypnotics are propofol, etomidate, thiopentone, and ketamine. Historically, thiopentone was the drug of choice in early 1930s and later etomidate was introduced followed by propofol.[25] Ketamine is an induction agent with analgesic properties but it is contraindicated in patients with traumatic brain injury. In this survey, 70% of anaesthetists chose propofol alone as the induction agent, followed by a mixture of propofol and ketamine among stable trauma patients. Only one anaesthetist chose the combination of propofol and midazolam, or etomidate or ketamine as a single drug. This distribution attributed to the fact that pharmacodynamics of propofol is well suited for RSI. The high degree of lipophilicity allows it to cross the blood-brain barrier rapidly, resulting in a rapid onset of action. Propofol quickly redistributes into the peripheral tissues and is rapidly metabolised, causing short duration of action. Propofol decreases the intracranial pressure; so it is suitable for induction of anaesthesia in patients with increased intracranial pressure.[26] In patients with bronchospasm, propofol is an appropriate induction agent because of its mild bronchodilating effects.[27] In unstable trauma patients, the anaesthestists use, almost equally distributed, propofol (29.8%) and ketamine (29.8%) and etomidate (34%). The anaesthetists are primarily categorized with a trend towards ketamine alone (30%), followed by a combination of propofol and ketamine (28%), etomidate (28%), and a combination of ketamine and etomidate (6%), ketamine/midazolam (4%), midazolam/etomidate (2%), and propofol only (2%). The reason for the use of propofol in combination with other drugs is likely due to its hypotensive and bradycardia effect attributed to calcium channel and ß-adrenergic receptor antagonist properties.[28,29] Caution should be exercised in patients with volume depletion, hypotension, or a reduced ejection fraction.[30] The reason that a higher percentage of anaesthetists use ketamine as the single induction agent or in combination with small dosages of propofol might be the fact the myth not to use ketamine in patients with a suspected head injury has been revised.[31,32] The superiority of ketamine compared to etomidate has also been proven in a cohort study from Lyon and colleagues.[4] However, other studies have shown superiority of propofol in combination with ketamine over the propofol alone.[33] Table 4 shows the main differences among 4 sedative agents used for RSI.[34] Nearly one-third of the participants of the current study used etomidate for RSI in trauma patients. This practice may be explained in part by etomidate being associated with better cardiovascular stability. However, its use is not recommended for critically ill patients, as indicated in a systematic review[35] and meta-analysis.[36] Furthermore, etomidate causes suppression of the adrenal cortex, even after a single dose.[37]
Table 4.
Sedative agents for RSI
Limitations
There are some limitations of the present audit survey. This is a single center study with relatively small number of participants, so the statistical interpretation of the data is limited. Moreover, our survey was mainly limited to the use of drugs and experience of the operator of RSI. The survey did not cover the strategies for management and rescue for failed intubation during RSI. Furthermore, Hamad General Hospital has the only national level I trama center in Qatar, so the number of physicians dealing with intubation of trauma patients is limited.
CONCLUSIONS
Propofol, fentanyl, and rocuronium were the most frequently used drugs for RSI. Despite the small number of participants the results reflect the current RSI practice. The results are comparable to similar international surveys and indicate a clear shift toward rocuronium as a muscle relaxant and the use of fentanyl and ketamine on the other hand. There is a persistent variability in the use of drugs for RSI in trauma patients amongst the emergency physicians and anesthesiologists that reflects the lack of agreement in clinical practice. There is a need to develop an RSI protocol using standardized types and dose of these agents to deliver an effective airway management for trauma patients.
ACKNOWLEDGMENT
We thank the participants of trauma surgery and anesthesia of Hamad General Hospital in Doha, Qatar for their kind cooperation.
Footnotes
Funding: None.
Ethics approval: This audit has been granted approval from the Medical Research Centre at Hamad Medical Corporation (MRC #16404/16 quality improvement/audit study).
Competing interests: The authors have no conflict of interest, no financial issues to disclose.
Contribution: All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published.
REFERENCES
- 1.Mayglothling J, Duane TM, Gibbs M, McCunn M, Legome E, Eastman AL, et al. Eastern Association for the Surgery of Trauma. Emergency tracheal intubation immediately following traumatic injury:an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S333–40. doi: 10.1097/TA.0b013e31827018a5. [DOI] [PubMed] [Google Scholar]
- 2.Kovacs G, Law JA, Ross J, Tallon J, MacQuarrie K, Petrie D, et al. Acute airway management in the emergency department by non-anesthesiologists. Can J Anaesth. 2004;51(2):174–80. doi: 10.1007/BF03018780. [DOI] [PubMed] [Google Scholar]
- 3.Leeuwenburg T. Airway management of the critically ill patient:modifications of traditional rapid sequence induction and intubation. Critical Care Horizons. 2015;1:1–10. [Google Scholar]
- 4.Lyon RM, Perkins ZB, Chatterjee D, Lockey DJ, Russell MQ Kent Surrey & Sussex Air Ambulance Trust. Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia. Crit Care. 2015;19:134. doi: 10.1186/s13054-015-0872-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on management of major bleeding and coagulopathy following trauma:fourth edition. Crit Care. 2016;20:100. doi: 10.1186/s13054-016-1265-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zöllner C, Schäfer M. Opioids in anesthesia. Anaesthesist. 2008;57(7):729–40. doi: 10.1007/s00101-008-1408-9. quiz 741-2. [DOI] [PubMed] [Google Scholar]
- 7.Fleischman RJ, Frazer DG, Daya M, Jui J, Newgard CD. Effectiveness and safety of fentanyl compared with morphine for out-of-hospital analgesia. Prehosp Emerg Care. 2010;14(2):167–75. doi: 10.3109/10903120903572301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sajayan A, Wicker J, Ungureanu N, Mendonca C, Kimani PK. Current practice of rapid sequence induction of anaesthesia in the UK - a national survey. Br J Anaesth. 2016;117(Suppl 1):i69–i74. doi: 10.1093/bja/aew017. [DOI] [PubMed] [Google Scholar]
- 9.Parida S, Varadharajan R, Bidkar PU, Mishra SK, Balachander H, Badhe AS, et al. A survey of a population of anaesthesiologists from South India regarding practices for rapid sequence intubation in patients with head injury. Indian J Anaesth. 2016;60(4):258–63. [Google Scholar]
- 10.Walls RM. Rapid sequence intubation. In: Walls RM, Luten RC, Murphy MF, Schneider RE, editors. Manual of Emergency Airway Management. Philadelphia: Lippincott Williams & Wilkins; 2000. pp. 8–15. [Google Scholar]
- 11.Jensen AG, Callesen T, Hagemo JS, Hreinsson K, Lund V, Nordmark J, et al. Scandinavian clinical practice guidelines on general anaesthesia for emergency situations. Acta Anaesthesiol Scand. 2010;54(8):922–50. doi: 10.1111/j.1399-6576.2010.02277.x. [DOI] [PubMed] [Google Scholar]
- 12.Ross W, Ellard L, Baitch L Rapid Sequence Induction. ATOTW 331 – Rapid Sequence Induction (24th May 2016) [acceseed on March 14, 2018]. Retrieved from http://anaesthesiology.gr/media/File/pdf/-Rapid-Sequence-Induction.pdf .
- 13.Abou-Arab MH, Feiner JR, Spigset O, Heier T. Alfentanil during rapid sequence induction with thiopental 4 mg/kg and rocuronium 0.6 mg/kg:tracheal intubation conditions. Acta Anaesthesiol Scand. 2015;59(10):1278–86. doi: 10.1111/aas.12584. [DOI] [PubMed] [Google Scholar]
- 14.Pouraghaei M, Moharamzadeh P, Soleimanpour H, Rahmani F, Safari S, Mahmoodpoor A, et al. Comparison between the effects of alfentanil, fentanyl and sufentanil on hemodynamic indices during rapid sequence intubation in the emergency department. Anesth Pain Med. 2014;4(1):e14618. doi: 10.5812/aapm.14618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller DR, Martineau RJ, O'Brien H, Hull KA, Oliveras L, Hindmarsh T, et al. Effects of alfentanil on the hemodynamic and catecholamine response to tracheal intubation. Anesth Analg. 1993;76(5):1040–6. doi: 10.1213/00000539-199305000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Gindre S, Ciais JF, Levraut J, Dellamonica J, Guerin JP, Grimaud D. Rapid sequence intubation in emergency:is there any place for fentanyl? Ann Fr Anesth Reanim. 2002;21(10):760–6. doi: 10.1016/s0750-7658(02)00795-5. [DOI] [PubMed] [Google Scholar]
- 17.Rohsbach C, Wirth S, Lenz K, Priebe H. Survey on the current management of rapid sequence induction in Germany. Minerva Anestiolol. 2013;79(7):716–26. [PubMed] [Google Scholar]
- 18.Srivastava A, Hunter JM. Reversal of neuromuscular block. Br J Anaesth. 2009;103(1):115–29. doi: 10.1093/bja/aep093. [DOI] [PubMed] [Google Scholar]
- 19.Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid-sequence induction intubation. Cochrane Database Syst Rev. 2008;2:CD002788. doi: 10.1002/14651858.CD002788.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Tran DT, Newton EK, Mount VA, Lee JS, Wells GA, Perry JJ. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015;10:CD002788. doi: 10.1002/14651858.CD002788.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sørensen MK, Bretlau C, Gätke MR, Sørensen AM, Rasmussen LS. Rapid sequence induction and intubation with rocuronium-sugammadex compared with succinylcholine:a randomized trial. Br J Anaesth. 2012;108(4):682–9. doi: 10.1093/bja/aer503. [DOI] [PubMed] [Google Scholar]
- 22.Lee C, Jahr JS, Candiotti KA, Warriner B, Zornow MH, Naguib M. Reversal of profound neuromuscular block by sugammadex administered three minutes after rocuronium:a comparison with spontaneous recovery from succinylcholine. Anesthesiology. 2009;110(5):1020–5. doi: 10.1097/ALN.0b013e31819dabb0. [DOI] [PubMed] [Google Scholar]
- 23.Teymourian H, Samet MA, Mohajerani SA, Jafari A. Comparison of modified and high dose of cisatracurium for rapid-sequence intubation. Asian J Pharm Nurs Med Sci. 2014;2:110–5. [Google Scholar]
- 24.Abrishami A, Ho J, Wong J, Yin L, Chung F. Cochrane corner:sugammadex, a selective reversal medication for preventing postoperative residual neuromuscular blockade. Anesth Analg. 2010;110(4):1239. doi: 10.1213/ANE.0b013e3181ce8d5e. [DOI] [PubMed] [Google Scholar]
- 25.Mir AH, Shah NF, Din MU, Langoo SA, Reshi FA. Effectiveness of sodium thiopentone, propofol, and etomidate as an ideal intravenous anesthetic agent for modified electroconvulsive therapy. Saudi J Anaesth. 2017;11(1):26–31. doi: 10.4103/1658-354X.197339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vahidi E, Hemati R, Momeni M, Jahanshir A, Saeedi M. Comparison of sedative effectiveness of thiopental versus midazolam in reduction of shoulder dislocation. World J Emerg Med. 2018;9(2):125–9. doi: 10.5847/wjem.j.1920-8642.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zou Y, Xin X, Zhao J. The protective effect of propofol on airway in asthmatic patients. Journal of Perioperative Science. 2014;1:5. [Google Scholar]
- 28.Vinson DR, Kea B. Understanding the effect of propofol and electrical cardioversion on the systolic blood pressure of emergency department patients with atrial fibrillation. World J Emerg Med. 2018;9(1):76–6. doi: 10.5847/wjem.j.1920-8642.2018.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kassam SI, Lu C, Buckley N, Lee RM. The mechanisms of propofol-induced vascular relaxation and modulation by perivascular adipose tissue and endothelium. Anesth Analg. 2011;112(6):1339–45. doi: 10.1213/ANE.0b013e318215e094. [DOI] [PubMed] [Google Scholar]
- 30.Stollings JL, Diedrich DA, Oyen LJ, Brown DR. Rapid-sequence intubation:a review of the process and considerations when choosing medications. Ann Pharmacother. 2014;48(1):62–76. doi: 10.1177/1060028013510488. [DOI] [PubMed] [Google Scholar]
- 31.Filanovski Y, Miller P, Kao J. Myth:ketamine should not be used as an induction agent for intubation in patients with head injury. CJEM. 2010;12(2):154–7. doi: 10.1017/s1481803500012197. [DOI] [PubMed] [Google Scholar]
- 32.Sehdev RS, Symmons DA, Kindl K. Ketamine for rapid sequence induction in patients with head injury in the emergency department. Emerg Med Australas. 2006;18(1):37–44. doi: 10.1111/j.1742-6723.2006.00802.x. [DOI] [PubMed] [Google Scholar]
- 33.Smischney NJ, Beach ML, Loftus RW, Dodds TM, Koff MD. Ketamine/propofol admixture (ketofol) is associated with improved hemodynamics as an induction agent:a randomized, controlled trial. J Trauma Acute Care Surg. 2012;73(1):94–101. doi: 10.1097/TA.0b013e318250cdb8. [DOI] [PubMed] [Google Scholar]
- 34.David C. Induction agents for rapid sequence intubation in adults outside the operating room. [accessed at 21 September 2018]. Available from https://www.uptodate.com/contents/induction-agents-for-rapid-sequence-intubation-in-adults-outside-the-operating-room .
- 35.Albert SG, Ariyan S, Rather A. The effect of etomidate on adrenal function in critical illness:a systematic review. Intensive Care Med. 2011;37(6):901–10. doi: 10.1007/s00134-011-2160-1. [DOI] [PubMed] [Google Scholar]
- 36.Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis:a meta-analysis. Crit Care Med. 2012;40(11):2945–53. doi: 10.1097/CCM.0b013e31825fec26. [DOI] [PubMed] [Google Scholar]
- 37.Vinclair M, Broux C, Faure P, Brun J, Genty C, Jacquot C, et al. Duration of adrenal inhibition following a single dose of etomidate in critically ill patients. Intensive Care Med. 2008;34(4):714–9. doi: 10.1007/s00134-007-0970-y. [DOI] [PubMed] [Google Scholar]


