Summary
Brain abscesses have cardiac etiology in 5% of cases with valvular heart disease and endocarditis being the most common. Congenital heart disease with the risk of right to left shunt and paradoxical embolization is also a culprit. Our case describes a young patient with a prior undiagnosed patent foramen ovale (PFO), who presented with solitary brain abscess without any underlying primary source of infection. Since there was no evidence of contiguous spread of infection by computed tomography or magnetic resonance imaging scans, hematogenous spread of the streptococcal species was the most likely etiology. Transesophageal echocardiography (TEE) revealed no evidence of valvular endocarditis but did show intracardiac right-to-left shunting via a PFO. We suggest that all patients with a brain abscess of an unclear etiology caused be screened for a PFO with a TEE and bubble study.
Keywords: Brain abscess, PFO, Streptococcus intermedius
Introduction
A young man presented with seizure activity initially thought to be caused by alcohol intoxication. Further evaluation revealed an unexpected and serious condition.
A 20-year-old Caucasian male had a witnessed episode of seizure 2 h after an alcohol binge. On arrival to the hospital the patient was uncooperative, combative, and oriented only to person. His temperature was 98 °F (36.7 °C), blood pressure 132/94 mmHg, pulse 94 beats/min, and respiratory rate 14 breaths/min. As the patient's mentation improved he reported no significant past medical history, no recent dental work, no exposure to sick contacts, and no intravenous drug use.
Case report
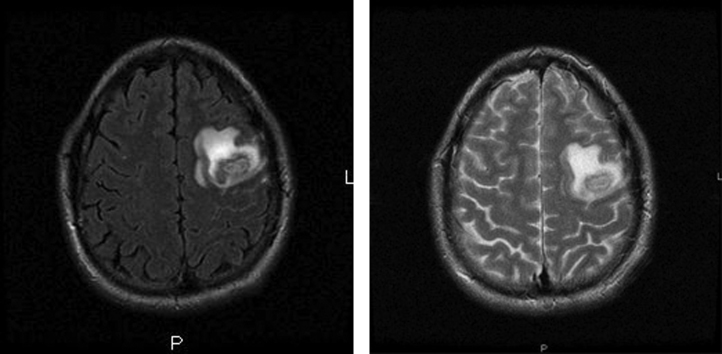
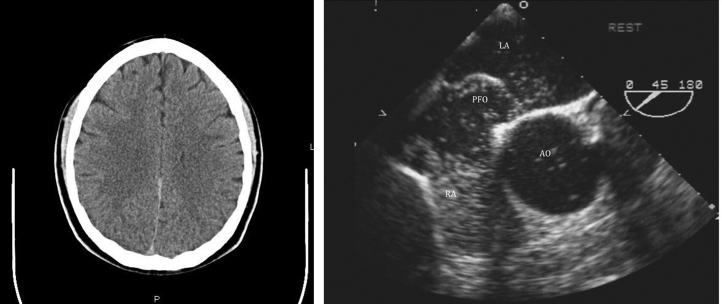
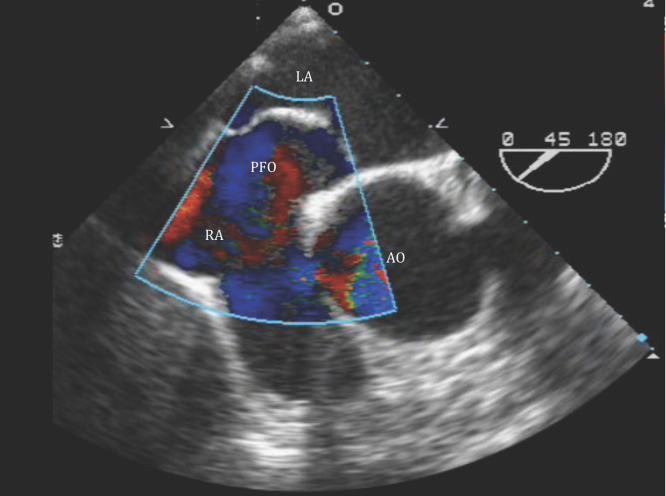
Laboratory work up: white blood cells (WBC) 20,600/dl (92% neutrophils). Two sets of blood cultures, urinalysis, and chest X-ray were negative. Cerebrospinal fluid analysis showed WBC 1/mm3, 120 red blood cells 120/mm3, glucose 76 mg/dl, protein 38 mg/dl, a negative Gram stain, and negative herpes simplex virus by polymerase chain reaction. A human immunodeficiency virus test was negative. The urinary toxicology was positive only for cannabis. A noncontrast computed tomography (CT) revealed focal low attenuation in the posterior left frontal lobe consistent with contusion. However, during his first day of hospitalization the patient developed three episodes of generalized tonic–clonic seizures and a temperature of 100.5 °F (38.1 °C). Broad antimicrobial coverage with cefepime and vancomycin were started. The magnetic resonance imaging (MRI) of the brain demonstrated a ring enhancing lesion and high signal on diffusion series suggestive of abscess (Fig. 1). A transesophageal echocardiogram (TEE) including a bubble study demonstrated air bubbles that crossed from the right to the left atrium within the first three cardiac cycles indicating the presence of a right-to-left shunt from a large patent foramen ovale (PFO) (maximum separation 8 mm) and an atrial septal aneurysm (ASA) (Fig. 2).
Figure 1.
Ring enhancing lesion noted within the posterior left frontal lobe. Non-enhancing central portion of the lesion is bright on the diffusion series.
Figure 2.
Patent foramen ovale as shown in transesophageal echocardiogram.
The patient underwent a stereotactic-CT-guided biopsy of the brain lesion which revealed a purulent aspirate. The Gram stain showed no organisms, but the culture showed Streptococcus intermedius (minimal inhibitory concentration to ceftriaxone ≤0.25). He completed six weeks of antibiotic treatment with ceftriaxone and metronidazole. Six months after the hospitalization, the patient had no episode of seizures and the primary lesion had completely resolved in the CT scan (Fig. 3).
Figure 3.
Computed tomography of the brain with intravenous contrast. There is no abnormal intracranial enhancement.
Discussion
Brain abscesses have cardiac etiology in about 5% of cases, valvular heart disease with endocarditis being the most common (2–4%), but congenital heart disease with possibility of right-to-left shunt and risk of paradoxical embolization is also a possible cause. The most likely cause for the brain abscess in our patient is paradoxical septic embolization through the ASA from an unknown infectious focus.
Seven cases in the literature have described the association of a PFO and a brain abscess in adults. All of them have been in middle-aged individuals with poor dentition [1]. It seems that healthy individuals as in our case, develop transient bacteremia from microaerophilic flora normally found in oropharynx even after simple procedures as tooth brushing. Right-to-left shunts would allow microorganisms to enter the arterial circulation, bypassing the oxygen-rich pulmonary circulation and the lymphatic system.Streptococcus intermedius is a member of the Streptococcus anginosus group (SAG), also known as the “Streptococcus milleri” group. The SAG, one of five groups collectively known as viridans group streptococci, consists of the species S. intermedius, S. anginosus, and S. constellatus. These organisms are commonly associated with purulent infections, primarily of the brain and liver, with abscess formation and less commonly are the cause of endocarditis than other viridans streptococci. An underlying condition, such as diabetes, cirrhosis, or cancer, is associated with the majority of patients [2].
PFO is detected in 20–35% of the general population at autopsy and in 10–26% of normal individuals by contrast TEE. In studies of patients with cryptogenic stroke, PFOs are consistently overrepresented. In the past, case–control studies employing TEE with intravenous contrast provided evidence of the association of PFO with ischemic stroke by finding PFOs in 40–50% of young or cryptogenic stroke patients versus 10–15% of controls. One meta-analysis of 9 case–control studies showed that young patients with cryptogenic stroke had an odds ratio of 6.0 for having a PFO versus patients with a known stroke cause [3]. However, a recent meta-analysis of 23 case–control studies reported that one third of PFOs discovered in patients with cryptogenic stroke are likely to be incidental and unrelated to the stroke [4]. PFO has been found to be more likely to be associated with cryptogenic stroke in patients who were younger and did not have classic stroke risk factors. In addition to age and conventional stroke risk factors, morphological features (PFO diameter, right-to-left shunt, higher septal wall motion) of a PFO and particularly the presence of ASA may influence the association between PFO and cryptogenic stroke [4]. Recently, the American Heart Association/American Stroke Association (AHA/ASA) [5] guidelines have recommended antiplatelet therapy for patients with ischemic stroke or transient ischemic attack and PFO, unless other indications exist for vitamin K antagonist therapy (e.g. atrial fibrillation, hypercoagulable state). The AHA/ASA guidelines for secondary stroke prevention state that “insufficient data exist to make a recommendation about PFO closure in patients with a first stroke and a PFO.” PFO closure may be considered for patients with recurrent CS despite optimal medical therapy.
Conclusion
Our case describes a patient diagnosed with solitary brain abscess with a PFO without any underlying primary source of infection or thrombus. Since there was no evidence of contiguous spread of infection by CT or MRI scans, hematogenous spread of the cultured streptococcal species was the most likely etiology. TEE revealed no evidence of valvular endocarditis but did show intracardiac right-to-left shunting via a PFO.
We suggest that all patients with a brain abscess caused by traditional flora commonly found in the oropharynx be screened for a PFO with a TEE and bubble study. Only a prospective, randomized trial would determine the optimal strategy about whether PFO closure versus conservative therapy is more effective in preventing recurrence, but the low incidence of brain abscess in the population may make such studies unfeasible.
References
- 1.Khouzam R.N., El-Dokla A.M., Menkes D.L. Undiagnosed patent foramen ovale presenting as a cryptogenic brain abscess: case report and review of the literature. Heart Lung. 2006;35:108–111. doi: 10.1016/j.hrtlng.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Bert F., Bariou-Lancelin M., Lambert-Zechovsky N. Clinical significance of bacteremia involving the “Streptococcus milleri” group: 51 cases and review. Clin Infect Dis. 1998;27:385–387. doi: 10.1086/514658. [DOI] [PubMed] [Google Scholar]
- 3.Overell J.R., Bone I., Lees K.R. Interatrial septal abnormalities and stroke: a meta-analysis of case–control studies. Neurology. 2000;55:1172–1179. doi: 10.1212/wnl.55.8.1172. [DOI] [PubMed] [Google Scholar]
- 4.Alsheikh-Ali A.A., Thaler D.E., Kent D.M. Patent foramen ovale in cryptogenic stroke: incidental or pathogenic? Stroke. 2009;40:2349–2355. doi: 10.1161/STROKEAHA.109.547828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Gara P.T., Messe S.R., Tuzcu E.M., Catha G., Ring J.C. Percutaneous device closure of patent foramen ovale for secondary stroke prevention: a call for completion of randomized clinical trials: a science advisory from the AHA/ASA/ACC/AAN affirms the value of this science advisory. Circulation. 2009;119:2743–2747. doi: 10.1161/CIRCULATIONAHA.109.192272. [DOI] [PubMed] [Google Scholar]