Summary
Idiopathic recurrent pericarditis (IRP) impairs quality of life. Although its precise etiology is not certain, it is believed to be immunologically mediated. Its optimal treatments are unknown. Initial therapy is with non-steroidal anti-inflammatory drugs and colchicine. Steroids, which are often used, however may promote recurrences. European guidelines advocate azathioprine or cyclophosphamide in refractory cases despite limited evidence. We report two adults with IRP successfully treated with the interleukin-1 antagonist, anakinra. We combine this experience with the first systematic literature review of immunosuppression in IRP. A total of 8 papers were included in the review, which alongside our patients described 18 cases. The best treatments comprised anakinra and intravenous immunoglobulin, with respective remission rates of 100% and 67%. Cyclophosphamide and azathioprine were less efficacious. The unprovoked inflammatory episodes in our patients alongside their prompt response to anakinra indicate that in some instances IRP may represent an autoinflammatory condition. We suggest that in IRP refractory to initial treatment, anakinra should be considered as a potential therapy. Clinical trials are required to confirm its benefits in IRP.
Keywords: Recurrent pericarditis, Anakinra, Immunosuppression, Autoinflammatory
Introduction
Idiopathic recurrent pericarditis (IRP) complicates 30% of acute pericarditis cases. Although rarely life-threatening, IRP is painful and significantly impairs quality of life. Its etiology is uncertain; it may follow an initial viral infection that triggers further immunologically mediated episodes.
Initial treatment involves non-steroidal anti-inflammatory drugs (NSAIDs) and colchicine. Corticosteroids are effective in the short-term, however as they may increase the risk of recurrence other immunosuppressants are often required. Current European guidelines advocate azathioprine or cyclophosphamide as first-line agents despite limited supporting evidence. More recently the interleukin-1 (IL-1) receptor antagonist, anakinra has been successfully used in 3 children with IRP, suggesting this cytokine has a key pathogenic role [1].
We provide further evidence for the efficacy of anakinra in IRP by reporting its use in two adult patients. Given the uncertainty regarding the optimal treatment of this condition, we combined our experience with the first systematic literature review of immunosuppression in IRP.
Case report 1
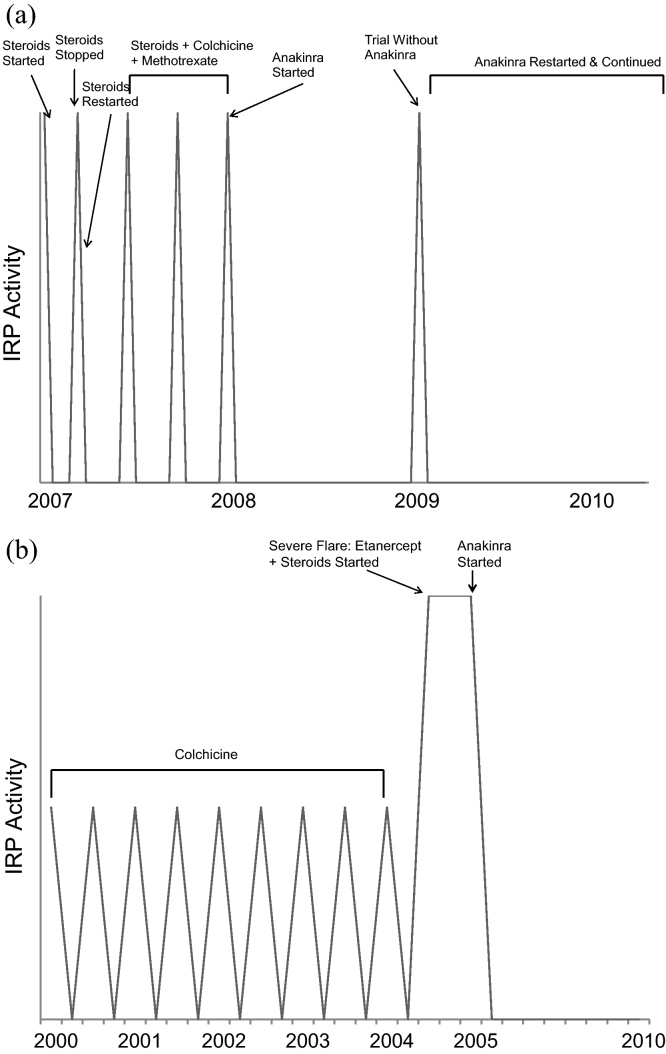
A 33-year-old female presented in 2007 with 2 weeks of pericarditic pain. She reported several previous milder episodes. Her C-reactive protein (CRP) was raised at 221 mg/l. Immunological tests (antinuclear antibodies, antineutrophil cytoplasmic antibodies, dsDNA, rheumatoid factor, lupus anticoagulant, antiphospholipid antibodies) and infection screens (blood cultures and serology for mycoplasma, legionella, cytomegalovirus, hepatitis, and human immunodeficiency virus) were negative. She had neither recurrent fevers nor features of a rheumatic disease and genetic sequencing of MEFV and TNFRSF1A – responsible for familial Mediterranean fever (FMF) and tumor necrosis factor (TNF) receptor associated periodic syndrome, respectively – were normal. Prednisolone was initiated with a prompt clinical response; her CRP fell to 83 mg/l within 36 h. Two weeks later she was asymptomatic. On discontinuing steroids she immediately relapsed (CRP 358 mg/l); steroids were restarted. Despite the addition of regular colchicine and methotrexate, her pericarditis relapsed on three further occasions over 3 months.
Treatment with anakinra was commenced in 2008 enabling prednisolone and methotrexate withdrawal without disease recurrence. In 2009 she was completely well on anakinra and colchicine. A trial of anakinra withdrawal was followed within one week by florid pericarditis that promptly resolved after restarting anakinra. Eighteen months later she remains in remission on anakinra and colchicine.
Case report 2
A 28-year-old male presented in August 2000 with acute pericarditis. Over the following 4 years he had numerous further attacks characterized by typical pain, pericardial effusions and a marked acute phase response, which responded little to NSAIDs. His autoimmune serology and MEFV genotype were normal. A diagnosis of IRP was made and colchicine initiated, with minimal benefit. In December 2004 he became acutely unwell with severe pericarditic pain, arthralgia, anemia, and thrombocytopenia that responded to prednisolone. Etanercept was introduced with the hope it might facilitate prednisolone tapering, but this prompted further IRP flares. In February 2005, etanercept was replaced by anakinra with dramatic efficacy. Steroids were completely withdrawn and he has had no further flares.
The clinical courses of our two patients alongside their treatment responses are outlined in Fig. 1.
Figure 1.
Clinical course and treatment responses of two patients with idiopathic recurrent pericarditis (IRP). (a) Case 1 and (b) Case 2.
Literature review
We searched Pubmed, EMBASE, and MEDLINE up to October 2010 using the following search terms: recurrent or chronic idiopathic or relapsing and pericarditis and immunosuppression or IL-1 or interleukin-1 or anakinra or anti-TNF or biologic or cyclosporin or methotrexate or azathioprine or cyclophosphamide or mycophenolate. We excluded papers not in English or dealing with alternative diagnoses.
We identified 96 citations and fully reviewed 20 reports; 12 were excluded (8 were duplicate publications, 4 dealt with alternative diagnoses). Finally, 8 were included (see Table 1 [1], [2], [3], [4], [5], [6], [7], [8]), comprising 3 case reports and 5 case series.
Table 1.
Immunosuppressants used in idiopathic recurrent pericarditis.
| Study | Year | Cases | Age (years) | Sex | Follow-up (months) | Immunosuppression | Outcome |
|---|---|---|---|---|---|---|---|
| Bird and Mustchin [2] | 1987 | 1 | 32 | M | 60 | Azathioprine | Remission |
| Marcolongo et al. [3] | 1995 | 2 | 56 | F | 21 | Azathioprine | Remission |
| 19 | M | 7 | Azathioprine | Remission | |||
| Lessio et al. [4] | 1999 | 1 | 44 | M | 24 | Cyclosporin | Remission |
| Tona et al. [5] | 2003 | 2 | 30 | M | 42 | a. Azathioprine/Cyclosporin | a. No response |
| b. Cyclophosphamide | b. Improved | ||||||
| c. IVIG | c. Remission | ||||||
| 19 | F | 32 | a. Cyclophosphamide/Cyclosporin/MTX | a. No response | |||
| b. IVIG | b. Remission | ||||||
| Peterlana et al. [6] | 2005 | 4 | 29 | M | 32 | IVIG | Remission |
| 28 | M | – | IVIG | Remission | |||
| 21 | M | – | IVIG | Improved | |||
| 11 | M | – | a. MTX/Cyclosporin/Azathioprine | a. No response | |||
| b. IVIG | b. Improved | ||||||
| Imazio et al. [7] | 2007 | 1 | 45 | F | 63 | a. Azathioprine | a. Improved |
| b. MTX/Cyclosporin | b. Improveda | ||||||
| Dalla Pozza et al. [8] | 2007 | 2 | 12 | F | 12 | Azathioprine/MTX | Improved |
| 7 | F | 68 | Azathioprine/MTX/Anti-TNF | No response | |||
| Picco et al. [1] | 2009 | 3 | 14 | F | 15 | Anakinra | Remissionb |
| 12 | M | 9 | Anakinra | Remissionb | |||
| 13 | F | 44 | a. MTX | a. No response | |||
| b. Anakinra | b. Remissionb | ||||||
Patient died.
All 3 cases relapsed on stopping anakinra with remission on restarting. IVIG, intravenous immunoglobulin; Anti-TNF, anti-tumor necrosis factor; MTX, methotrexate.
Along with our patients there were 18 reported cases of IRP treated with immunosuppression. These comprised 10 males and 8 females (mean age 25 years; mean follow-up 39 months). Nine patients received more than one immunosuppressant given sequentially.
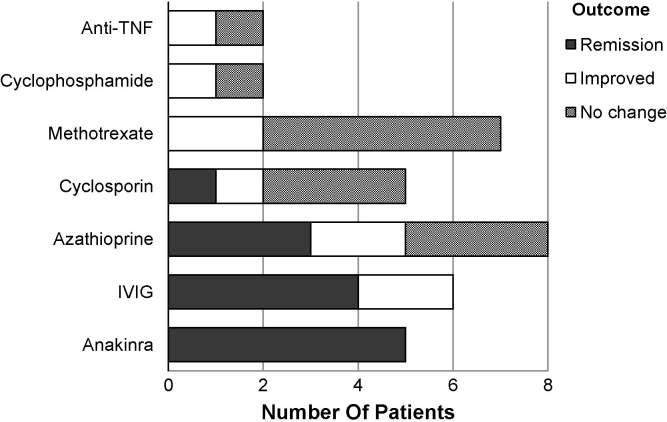
Thirteen patients achieved remission, 4 improved and 1 showed no response. Their treatments and outcomes are shown in Table 1 and Fig. 2. The treatments and their remission rates comprised azathioprine (8 cases, 38% remission), methotrexate (7 cases, no remission), intravenous immunoglobulin (IVIG) (6 cases, 67% remission), cyclosporin (5 cases, 20% remission), anakinra (5 cases, 100% remission), cyclophosphamide (2 cases, no remission), and anti-TNF (2 cases, no remission). Methotrexate was least efficacious; 71% of patients did not improve.
Figure 2.
Outcome of immunosuppression in idiopathic recurrent pericarditis. TNF, tumor necrosis factor; IVIG, intravenous immunoglobulin.
Discussion
IRP is a debilitating condition with a predilection for younger patients. Several immunosuppressants have been used with variable success. Although current European guidelines recommend azathioprine and cyclophosphamide as first-line therapies, published data identified from our review suggest these agents have limited efficacy (remission rates of 38% and 0%, respectively). IVIG and anakinra were most efficacious with high remission rates of 67% and 100%, respectively. We suggest that current guidance requires reappraisal.
The etiology of IRP remains unknown. It is probably a heterogeneous condition arising from several distinct pathological mechanisms. There is evidence for an auto-immune process involving the adaptive immune system, with Imazio et al. finding anti-nuclear antibodies in 43% of 145 cases of recurrent pericarditis [9]. Our review supports an autoimmune process with multiple immune modulating treatments reducing recurrences. The excellent response to anakinra however suggests that at least some cases may be autoinflammatory in nature.
Autoinflammatory syndromes are a heterogeneous group of disorders that are characterized by episodes of apparently unprovoked inflammation due to activation of the innate immune system. Because the adaptive immune system is not involved patients do not exhibit auto-antibodies. The underlying defect in these disorders appears to be aberrancies in pathways that regulate the inflammasome. The inflammasome is an intracellular complex, which on detection of foreign pathogens by pathogen-recognition receptors results in an immune response via activation of the proinflammatory cytokine, IL-1β. It is regulated by several different proteins, examples of which include pyrin (the variant protein in FMF) and cryopyrin (the variant protein in cryopyrin-associated periodic syndromes). The importance of IL-1β production in these diseases explains their response to IL-receptor blockade with anakinra. The unprovoked inflammatory episodes in our two patients, the absence of auto-antibodies, and their dramatic response to anakinra supports the view of Picco et al. that at least a subset of patients with IRP have an autoinflammatory disease [1] and suggests such cases result from deficient inflammasome regulation. Further support for this concept comes from the report of anakinra responsive pericarditis in a patient with a variant of cryopyrin associated periodic syndrome [10].
Our review has several limitations. All publications are case reports or series, with no clinical trials available. There is clinical heterogeneity between patients, varying with regards to age, disease duration, and previous treatments. Finally the follow-up period is short with long-term outcomes unknown.
In conclusion our findings support a role for anakinra in IRP resistant to initial treatment with NSAIDs and colchicine. Anakinra provided the best chance of remission in published cases and should be considered as a potential treatment in refractory IRP. Its benefits however require formal assessments in clinical trials of IRP patients.
Acknowledgments
This data was presented at the British Society of Rheumatology annual conference (2010).
References
- 1.Picco P., Brisca G., Traverso F., Loy A., Gattorno M., Martini A. Successful treatment of idiopathic recurrent pericarditis in children with interleukin-1β receptor antagonist (anakinra). An unrecognized autoinflammatory disease? Arthritis Rheum. 2009;60:264–268. doi: 10.1002/art.24174. [DOI] [PubMed] [Google Scholar]
- 2.Bird A.G., Mustchin C.P. Immunological studies in a case of idiopathic relapsing pericarditis. Eur Heart J. 1987;8:199–201. [Google Scholar]
- 3.Marcolongo R., Rosario R., Laveder F., Noventa F., Agostini C. Immunosuppressive therapy prevents recurrent pericarditis. J Am Coll Cardiol. 1995;26:1276–1279. doi: 10.1016/0735-1097(95)00302-9. [DOI] [PubMed] [Google Scholar]
- 4.Lessio S., Laveder F., Marcolongo R., Rigoli A., Tona F., Cyclosporin A in the treatment of idiopathic recurrent pericarditis: a case report. J Clin Basic Cardiol. 1999;2:130–131. [Google Scholar]
- 5.Tona F., Bellotto F., Laveder F., Meneghin A., Sinagra G., Marcolongo R. Efficacy of high-dose intravenous immunoglobulins in two patients with idiopathic recurrent pericarditis refractory to previous immunosuppressive treatment. Ital Heart J. 2003;4:64–68. [PubMed] [Google Scholar]
- 6.Peterlana D., Puccetti A., Simeoni S., Tinazzi E., Corrocher R., Lunardi C. Efficacy of intravenous immunoglobulin in chronic idiopathic pericarditis: report of four cases. Clin Rheumatol. 2005;24:18–21. doi: 10.1007/s10067-004-0959-7. [DOI] [PubMed] [Google Scholar]
- 7.Imazio M., Cecchi E., Correndo L., Antonielli E., D’Oulx A., Doronzo B., Trinchero R. Treatment of refractory recurrent pericarditis. J Cardiovasc Med. 2007;8:748–753. doi: 10.2459/JCM.0b013e3280101e24. [DOI] [PubMed] [Google Scholar]
- 8.Dalla Pozza R., Hartl D., Bechtold S., Urschel S., Kozlik-Feldmann R., Pankuweit S., Belohradsky B., Netz H. Recurrent pericarditis in children: elevated cardiac autoantibodies. Clin Res Cardiol. 2007;96:168–175. doi: 10.1007/s00392-007-0471-6. [DOI] [PubMed] [Google Scholar]
- 9.Imazio M., Cecchi E., Demichelis B., Ierna S., Demarie D., Ghisio A., Pomari F., Coda L., Belli R., Trinchero R. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739–2744. doi: 10.1161/CIRCULATIONAHA.106.662114. [DOI] [PubMed] [Google Scholar]
- 10.Murphy G., Daly M., O'Sullivan M., Stack J., Rowczenio D., Lachmann H., Shanahan F., Harney S., Hawkins P., Molloy M. An unusual phenotype in Muckle-Wells syndrome associated with NLRP3 E311K. Rheumatology (Oxford) 2011;50:419–420. doi: 10.1093/rheumatology/keq280. [DOI] [PubMed] [Google Scholar]