Abstract
Background
Our randomized trial found that pictorial cigarette pack warnings elicited more quit attempts than text-only warnings.
Purpose
In the current study, we sought to identify psychological mechanisms that explain why pictorial cigarette pack warnings change behavior.
Methods
In 2014 and 2015, we recruited 2,149 adult smokers in NC and CA, USA. We randomly assigned smokers to receive on their cigarette packs for 4 weeks either a text-only warning (one of the USA’s current warnings on the side of cigarette packs) or a pictorial warning (one of the USA’s proposed text warnings with pictures on the top half of the front and back of cigarette packs).
Results
Pictorial warnings increased attention to, reactions to, and social interactions about cigarette pack warnings (all p < .05). However, pictorial warnings changed almost no belief or attitude measures. Mediators of the impact of pictorial warnings included increased attention, negative affect, social interactions, thinking about the warning and harms of smoking, and intentions to quit (all p < .05). Analyses also found that pictorial warnings led to greater avoidance of the warnings, which was associated with more quit attempts (p < .05).
Conclusions
Pictorial warnings increased quit attempts by eliciting aversive reactions and by keeping the message vividly in smokers’ minds. Contrary to predictions from several theories of health behavior, the warnings exerted little of their influence through changes in beliefs and attitudes and none of their influence through changes in risk perception. We propose the Tobacco Warnings Model based on these findings.
Clinical Trial information
ClinicalTrials.gov identifier: NCT02247908; https://clinicaltrials.gov/ct2/show/NCT02247908.
Keywords: pictorial warnings, cigarettes, smoking, quit attempts, mediation analysis, randomized controlled trial
Pictorial cigarette pack warnings increased quit attempts by eliciting aversive reactions and by keeping the message vividly in smokers’ minds.
Introduction
Tobacco is the leading cause of preventable death worldwide, accounting for nearly 6 million deaths per year mostly due to cancer and cardiovascular disease [1]. Pictorial cigarette pack warnings are a promising solution for curbing the tobacco epidemic. More than 100 countries, with nearly 60% of the world’s population, have policies that require pictorial warnings on cigarette packs [2]. A systematic review [3] and a large randomized clinical trial [4] demonstrate that pictorial cigarette pack warnings promote cessation behavior, including quit attempts, across a wide range of samples and cultural contexts.
The psychological mechanisms through which pictorial warnings change behavior are largely unknown, although health behavior theories and empirical models have identified many possibilities [3, 5–8]. The Elaboration Likelihood Model [9] suggests that pictorial warnings could increase attention [10–13] and cognitive elaboration (e.g., thinking about the warning and harms of smoking) [14–17], which should lead to persuasion (i.e., attitude change [18, 19]) and then behavior change. Expectancy value theories—including the Health Belief Model [20], the Theory of Planned Behavior [21], and the Tripartite Model of Risk Perceptions [22]—suggest that pictorial warnings could exert their effects by changing risk perceptions and attitudes. The Extended Parallel Process Model [23] suggests that pictorial warnings may change behavior by eliciting fear [24–27] and adaptive responding, or they may instead elicit maladaptive coping in the form of message reactance and avoidance to dispel fear [28–33]. These psychological mechanisms share the insight that pictorial warnings generate deeper engagement with the messages.
To establish which of these mechanisms has empirical support, researchers can measure the candidate constructs and use mediation analyses. Several researchers have done this work using observational study data or non-behavioral outcomes [14, 34, 35]. Our study contributes by examining a comprehensive set of mediators in a single prospective, randomized clinical trial with a behavioral endpoint. Thus, our study aimed to identify psychological mechanisms that explain why pictorial cigarette pack warnings increase quit attempts. Understanding these mechanisms will help tobacco control programs design better warnings and will advance a deeper understanding of why pictorial cigarette pack warnings change behavior.
Methods
Study Design and Population
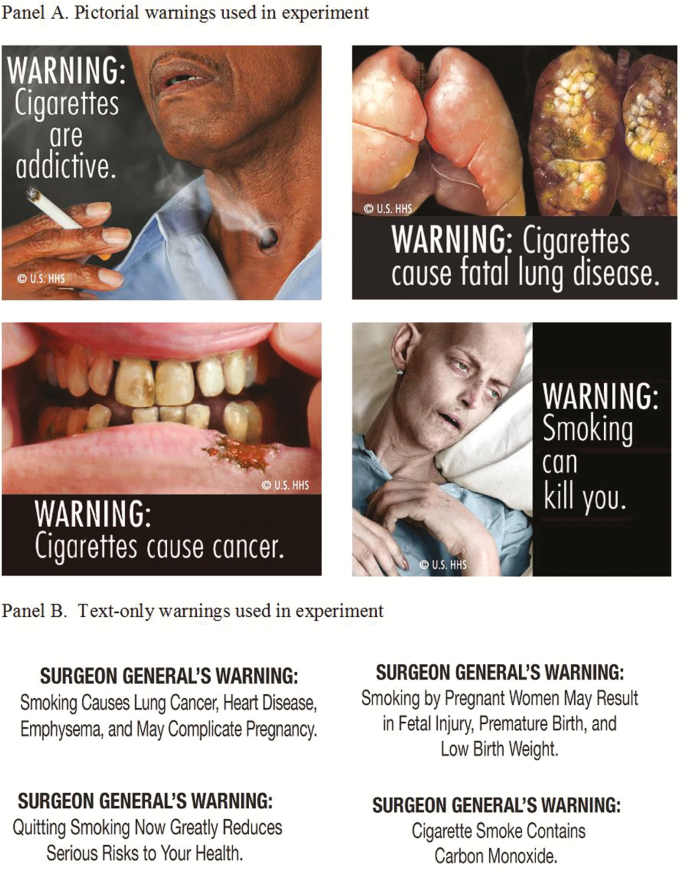
We used longitudinal data from a randomized clinical trial with 2,149 adult smokers living in North Carolina and California. Details of the trial including study protocols, questionnaire development, and participant recruitment have been previously published [4]. Other papers using this dataset have explored the frequency and content of social interactions [36], reactance to warnings [37], and trajectories of pictorial warnings’ impact [38], as well as attitudes toward regulation of tobacco products [39, 40]. From September 2014 to August 2015, we recruited English-speaking current smokers over the age of 18 to participate in the trial (see Table 1 for participant characteristics). Smokers brought in an eight-day supply of their own cigarettes weekly and received warnings on their packs for four weeks [4, 41]. Participants were randomly assigned to have one of four pictorial warnings applied to the top half of the front and back panels of their cigarette packs (Fig. 1), or one of four text-only warnings applied to the side of their cigarette packs placed over the current Surgeon General’s warning, for the duration of the study. Randomization created arms that did not differ on key demographic characteristics (all p > .05) [4]. Participants completed two computer surveys at the first study visit (i.e., baseline and immediately after seeing their assigned warning) and one survey at each visit thereafter. Participants provided written informed consent before enrollment. The University of North Carolina Institutional Review Board approved the study procedures.
Table 1.
Participant characteristics (N = 2,149)
| n | (%) | |
|---|---|---|
| Demographics | ||
| Study site | ||
| California | 1,186 | (55.2) |
| North Carolina | 963 | (44.8) |
| Age | ||
| 18–24 years | 323 | (15.3) |
| 25–39 years | 775 | (36.7) |
| 40–54 years | 642 | (30.4) |
| ≥55 years | 371 | (17.6) |
| Mean (SD) | 39.7 | (13.5) |
| Gender | ||
| Male | 1,039 | (48.7) |
| Female | 1,060 | (49.7) |
| Transgender | 34 | (1.6) |
| Gay, lesbian, or bisexual | 368 | (17.5) |
| Hispanic | 181 | (8.6) |
| Race | ||
| American Indian or Alaska Native | 18 | (0.9) |
| Asian | 70 | (3.3) |
| Black or African American | 994 | (47.3) |
| Native Hawaiian or other Pacific Islander | 17 | (0.8) |
| White | 751 | (35.7) |
| Other/multiracial | 251 | (11.9) |
| Education | ||
| High school graduate or less | 677 | (31.8) |
| Some college | 1,021 | (47.9) |
| College graduate | 312 | (14.6) |
| Graduate degree | 121 | (5.7) |
| Household income, annual | ||
| $0–$24,999 | 1,155 | (54.5) |
| $25,000–$49,999 | 538 | (25.4) |
| $50,000–$74,999 | 202 | (9.5) |
| ≥$75,000 | 224 | (10.6) |
| Low income (≤150% of federal poverty level) | ||
| No | 983 | (45.9) |
| Yes | 1,159 | (54.1) |
| Cigarettes smoked per day, mean (SD) | 8.7 | (7.0) |
| Smoking frequency | ||
| Daily | 1,730 | (80.5) |
| Non-daily | 418 | (19.5) |
| Primary trial outcome at baseline | ||
| Made quit attempt in last month | 545 | (26.5) |
Study characteristics and outcomes at baseline did not differ by trial arm. Missing demographic data ranged from 0.7% to 2.2%. SD = standard deviation.
Fig. 1.
Warnings used in the trial
Measures
The primary trial outcome was attempting to quit smoking during the study. At each of the follow-up visits, smokers answered the following survey question: “During the last week, did you stop smoking for 1 day or longer because you were trying to quit smoking?” The survey at Week 4 follow-up also asked, “Since you started the study, did you stop smoking for 1 day or longer because you were trying to quit smoking?” We considered participants to have made a quit attempt if they answered “yes” to any of the quit attempt questions.
Surveys assessed psychological constructs from all stages of the Message Impact Framework to serve as potential mediators (see Supplementary Material 1) [8]. The categories of variables were attention/noticing, warning reactions, social interactions, attitudes and beliefs, intentions to quit smoking, and perceived effectiveness of the warnings (see Table 2 for a full list of variables and measurement time points). Cronbach’s alpha was .70 or greater for all multi-item scales, except for two reactance subscales (discounting and government), which were both greater than .60.
Table 2.
Effects of pictorial warnings on mediators (N = 2,149)
| Mediator (# of items) | Week 0 | Week 1 | Week 2 | Week 3 | Week 4 |
|---|---|---|---|---|---|
| d (95% CI) | d (95% CI) | d (95% CI) | d (95% CI) | d (95% CI) | |
| Attention/noticing (3) | — | 10.02 (0.92, 10.11)* | 0.82 (0.73, 0.91)* | 0.74 (0.64, 0.83)* | 0.82 (0.73, 0.91)* |
| Warning reactions | |||||
| Cognitive elaboration (4) | — | 0.44 (0.35, 0.53)* | 0.38 (0.29, 0.47)* | 0.38 (0.29, 0.47)* | 0.38 (0.30, 0.47)* |
| Thinking about the warning message (2) | — | 0.63 (0.54, 0.73)* | 0.56 (0.47, 0.65)* | 0.56 (0.47, 0.65)* | 0.55 (0.46, 0.64)* |
| Thinking about the harms of smoking (2) | — | 0.14 (0.05, 0.23)* | 0.11 (0.02, 0.20)* | 0.10 (0.02, 0.19)* | 0.12 (0.04, 0.21)* |
| Negative affect (15) | 0.85 (0.76, 0.94)* | 0.76 (0.67, 0.84)* | 0.66 (0.57, 0.75)* | 0.63 (0.55, 0.72)* | 0.59 (0.51, 0.68)* |
| Anxiety (3) | 0.84 (0.75, 0.93)* | 0.72 (0.63, 0.80)* | 0.64 (0.56, 0.73)* | 0.60 (0.51, 0.69)* | 0.56 (0.48, 0.65)* |
| Disgust (3) | 10.04 (0.95, 10.13)* | 0.92 (0.83, 10.01)* | 0.81 (0.72, 0.89)* | 0.75 (0.66, 0.84)* | 0.75 (0.66, 0.84)* |
| Fear (3) | 0.71 (0.63, 0.80)* | 0.64 (0.56, 0.73)* | 0.58 (0.50, 0.67)* | 0.56 (0.48, 0.65)* | 0.52 (0.44, 0.61)* |
| Guilt (3) | 0.59 (0.51, 0.68)* | 0.56 (0.48, 0.65)* | 0.50 (0.42, 0.59)* | 0.50 (0.41, 0.59)* | 0.46 (0.38, 0.55)* |
| Sadness (3) | 0.72 (0.63, 0.80)* | 0.61 (0.53, 0.70)* | 0.52 (0.43, 0.60)* | 0.54 (0.45, 0.62)* | 0.46 (0.37, 0.54)* |
| Negative cigarette pack attitudes (6) | — | — | — | — | 0.49 (0.40, 0.58)* |
| Perceived understandability (1) | 0.10 (0.01, 0.18)* | — | — | — | 0.10 (0.02, 0.19)* |
| Reactance, brief form (3) | 0.44 (0.35, 0.52)* | 0.38 (0.29, 0.46)* | — | — | 0.30 (0.21, 0.38)* |
| Reactance, long form subscales | — | — | |||
| Anger (3) | 0.46 (0.37, 0.55)* | 0.40 (0.32, 0.49)* | — | — | 0.32 (0.24, 0.41)* |
| Common knowledge (3) | −0.25 (−0.34, −0.17)* | −0.16 (−0.24, −0.07)* | — | — | −0.13 (−0.22, −0.05)* |
| Derogation (3) | −0.10 (−0.19, −0.02)* | −0.11 (−0.20, −0.03)* | — | — | −0.11 (−0.19, −0.02)* |
| Discounting (3) | 0.32 (0.23, 0.40)* | 0.25 (0.17, 0.34)* | — | — | 0.22 (0.14, 0.31)* |
| Exaggeration (3) | 0.29 (0.21, 0.38)* | 0.23 (0.15, 0.32)* | — | — | 0.20 (0.11, 0.28)* |
| Government (3) | 0.32 (0.24, 0.41)* | 0.25 (0.17, 0.34)* | — | — | 0.20 (0.11, 0.28)* |
| Manipulation (3) | 0.41 (0.33, 0.50)* | 0.36 (0.28, 0.45)* | — | — | 0.29 (0.21, 0.38)* |
| Personal attack (3) | 0.37 (0.28, 0.45)* | 0.33 (0.24, 0.41)* | — | — | 0.31 (0.22, 0.39)* |
| Self-relevance (3) | 0.06 (−0.03, 0.14) | 0.04 (−0.04, 0.13) | — | — | 0.02 (−0.06, 0.11) |
| Warning avoidance (3) | — | 0.75 (0.65, 0.84)* | 0.61 (0.51, 0.70)* | 0.59 (0.50, 0.68)* | 0.56 (0.47, 0.65)* |
| Worry about consequences of smoking (4) | 0.09 (0.00, 0.17)* | 0.08 (−0.00, 0.17) | 0.09 (0.00, 0.17)* | 0.07 (−0.02, 0.15) | 0.08 (−0.00, 0.17) |
| Social interactions (3) | — | 0.41 (0.32, 0.49)* | 0.28 (0.19, 0.36)* | 0.21 (0.12, 0.29)* | 0.21 (0.12, 0.29)* |
| Attitudes and beliefs | |||||
| Anticipated regret of quitting smoking (3) | — | — | −0.08 (−0.16, 0.01) | — | −0.05 (−0.13, 0.04) |
| Anticipated regret of smoking (3) | — | — | −0.11 (−0.19, −0.02)* | — | −0.08 (−0.17, 0.00) |
| Negative consequences of smoking (4) | 0.00 (−0.08, 0.09) | −0.01 (−0.09, 0.08) | 0.03 (−0.05, 0.12) | 0.04 (−0.05, 0.12) | 0.02 (−0.07, 0.10) |
| Perceived benefits of quitting smoking (4) | — | −0.02 (−0.10, 0.07) | 0.04 (−0.05, 0.12) | 0.01 (−0.08, 0.09) | 0.03 (−0.05, 0.12) |
| Perceived costs of quitting smoking (4) | — | −0.07 (−0.15, 0.02) | −0.02 (−0.10, 0.07) | −0.02 (−0.10, 0.07) | −0.01 (−0.08, 0.09) |
| Perceived likelihood of harm from smoking (3) | — | — | 0.04 (−0.04, 0.13) | — | 0.03 (−0.05, 0.11) |
| Perceived severity of harm from smoking (3) | — | — | 0.00 (−0.09, 0.08) | — | −0.01 (−0.10, 0.07) |
| Perceived threat (PL*PS) | — | — | 0.04 (−0.05, 0.14) | — | 0.02 (−0.07, 0.11) |
| Perceived severity of negative consequences of quitting smoking (3) | — | — | 0.00 (−0.09, 0.08) | — | −0.01 (−0.09, 0.08) |
| Perceived efficacy (8) | — | — | 0.12 (0.03, 0.22)* | — | 0.11 (0.02, 0.20)* |
| Self-efficacy to quit smoking (5) | — | — | 0.10 (0.02, 0.19)* | — | 0.12 (0.03, 0.20)* |
| Response efficacy of quitting smoking: lower risk of health problems (3) | — | — | 0.05 (−0.04, 0.13) | — | 0.03 (−0.05, −0.12)* |
| Perceived efficacy*Threat | — | — | 0.09 (−0.01, 0.18) | — | 0.07 (−0.02, 0.16) |
| Response efficacy of quitting smoking: cause negative consequences (3) | — | — | −0.03 (−0.12, 0.05) | — | −0.01 (−0.09, 0.08) |
| Smoker prototypes (8) | 0.03 (−0.06, 0.11) | 0.03 (−0.05, 0.12) | 0.00 (−0.09, 0.08) | −0.01 (−0.09, 0.08) | −0.08 (−0.16, 0.01) |
| Negative (4) | 0.05 (−0.03, 0.13) | 0.05 (−0.03, 0.14) | 0.09 (0.01, 0.18)* | 0.10 (0.01, 0.18)* | 0.16 (0.08, 0.25)* |
| Positive (4) | 0.10 (0.01, 0.18)* | 0.11 (0.02, 0.19)* | 0.11 (0.03, 0.20)* | 0.11 (0.02, 0.19)* | 0.09 (0.01, 0.17)* |
| Smoking reinforcement attitudes – negative (4) | −0.03 (−0.11, 0.06) | −0.06 (−0.14, 0.03) | −0.04 (−0.120. 0.05) | −0.01 (−0.09, 0.08) | −0.03 (−0.12, 0.05) |
| Smoking reinforcement attitudes – positive (4) | 0.02 (−0.07, 0.10) | 0.01 (−0.08, 0.09) | −0.01 (−0.09, 0.08) | 0.00 (−0.09, 0.08) | −0.02 (−0.10, 0.07) |
| Subjective norms of quitting smoking (4) | — | −0.02 (−0.10, 0.07) | 0.01 (−0.08, 0.09) | 0.02 (−0.06, 0.11) | −0.01 (−0.10, 0.07) |
| Intentions | |||||
| Quit intentions (3) | 0.26 (0.18, 0.35)* | 0.19 (0.10, 0.27)* | 0.20 (0.11, 0.28)* | 0.15 (0.07, 0.24)* | 0.16 (0.07, 0.24)* |
| Quit stage (1) | 0.15 (0.07, 0.24)* | 0.13 (0.05, 0.22)* | 0.14 (0.05, 0.22)* | 0.11 (0.03, 0.20)* | 0.14 (0.05, 0.22)* |
| Perceived effectiveness of warnings (3) | 0.71 (0.63, 0.80)* | — | — | — | — |
Table reports Cohen’s d, which is the difference between intervention and control, divided by the pooled standard deviation. Intent-to-treat analyses included all participants randomized. Sample sizes after carrying the last value forward range from 2,122 to 2,149 at Week 0, 1,821 to 2,149 at Week 1, 1,908 to 2,149 at Week 2, 1,930 to 2,149 at Week 3, and 1,997 to 2,149 at Week 4. Week 0 refers to survey at first visit, immediately after smokers saw their labeled cigarette packs. CI = confidence interval. — = not assessed. * designates an interaction term. Numbers in parentheses indicate the number of items in the scale. PL*PS = perceived likelihood * perceived severity.
*p < .05
Statistical Analysis
Analyses used an intent-to-treat approach, including all participants randomized in the trial, using the last observation available for missing data [42]. First, we compared trial arms on each potential mediator at each time point using t-tests. We characterized the associations using Cohen’s d, calculated using PROC TTEST in SAS v9.4 (SAS Institute Inc., Cary, NC). To facilitate use of our findings in future meta-analyses as well as interpretation of the relative size of the effects, we report the effect sizes (Cohen’s d) for scales and subscales at all times we had data available.
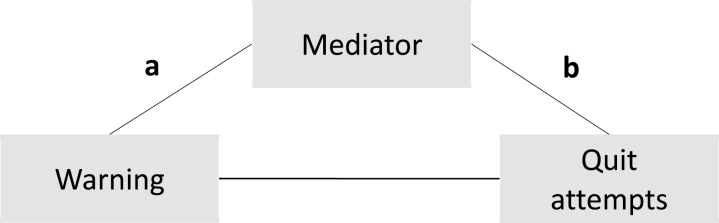
Second, we conducted mediation analyses to identify variables that could explain the association between pictorial warnings and quit attempts (i.e., mediation). We characterized associations using standardized regression coefficients (β). The MacKinnon approach [43] to mediation is to (a) examine the association of trial arm to mediator (a pathway), (b) examine the association of mediator to quit attempt outcome, adjusting for trial arm (b pathway), and (c) examine the product of the two (a*b pathway) (Fig. 2). Mediation exists if βa*βb is larger or smaller than 0. Mediation analyses used a separate structural equation model for each potential mediator, at the earliest observation available, in Mplus version 7.4 (Muthén & Muthén, Los Angeles, CA). We parceled the mediator variables in the model based on theoretical grounds, high correlations between items, and to simplify model specification [44]. To allow use of the full sample, analyses accounted for missing data by employing full information maximum likelihood estimation available in Mplus. Mediation analyses used bootstrapped 95% confidence intervals with 1,000 repetitions, as this approach does not assume that indirect effects are normally distributed [45]. All models had acceptable fit statistics (CFI > 0.95 and RMSEA < 0.05).
Fig. 2.
Mediation model
Finally, based on our findings, we identified the most active variables in the Message Impact Framework to create a parsimonious empirical model of the process through which warnings exert their influence. The model included variables that had relatively large mediated pathways (statistically significant and larger than .02) and that did not assess conceptually similar constructs (e.g., we did not include intentions and perceived message effectiveness). We evaluated the model using structural equation modeling, using the same methods described above.
Results
Attention to the warnings was greater for pictorial than text warnings at all four of the follow-up time points it was measured (median d = .82, all p < .05, Table 2). Pictorial warnings elicited stronger effects at all time points for most of the eight warning reactions measures (median d = .43, most p < .05). The exceptions were worry, which showed differences at two of the five time points, the reactance self-relevance subscale, which showed no difference at any time point, and the common knowledge and derogation reactance subscales, which were higher in the text arm. Among warning reactions, the largest effect size was for the disgust subscale of negative affect (median d = .81, all p < .05). Pictorial warnings led to more social interactions about the warnings at all follow-up time points (median d = .25, all p < .05). However, pictorial warnings affected only two of the 18 belief and attitude measures (median d = .03, few p < .05). Belief and attitude constructs affected in at least two time points were self-efficacy and positive and negative prototypes. Finally, pictorial warnings led to higher intentions (median d = .15, all p < .05) and perceived message effectiveness (d = .71, p < .05) at all time points measured.
The two largest mediation effects were for attention/noticing and thinking about the warnings (both βa*βb = .15, p < .05), in simple mediation analyses (Table 3). Other larger mediation effects were for avoidance, perceived effectiveness, negative affect, and negative cigarette pack attitudes (βa*βb = .12, .11, .09 and .07, p < .05). Constructs with smaller path coefficients were quit intentions, self-efficacy, social interactions, worry, self-efficacy, and quit stage. Reactance suppressed the impact of pictorial warnings, although this effect was one of the smallest we identified (βa*βb = −.02, p < .05).
Table 3.
Mediation of pictorial warnings’ effect on quit attempts, single mediator analyses (N = 2,149)
| Mediator | a pathway | b pathway | a*b pathway | |
|---|---|---|---|---|
| Week | β a | β b | β a*βb | |
| Attention/noticing | 1 | .45* | .32* | .15* |
| Warning reactions | ||||
| Cognitive elaboration | 1 | .22* | .37* | .08* |
| Thinking about the warning message | 1 | .30* | .38* | .12* |
| Thinking about the harms of smoking | 1 | .07* | .27* | .02* |
| Negative affect | 0 | .39* | .23* | .09* |
| Anxiety | 0 | .39* | .20* | .08* |
| Disgust | 0 | .46* | .20* | .09* |
| Fear | 0 | .34* | .23* | .08* |
| Guilt | 0 | .29* | .22* | .06* |
| Sadness | 0 | .34* | .21* | .07* |
| Negative cigarette pack attitudes | 4 | .24* | .27* | .07* |
| Perceived understandability | 0 | .05* | −.05 | .00 |
| Reactance, brief form | 0 | .21* | −.07* | −.02* |
| Reactance, long form subscales | ||||
| Anger | 0 | .22* | −.04 | −.01 |
| Common knowledge | 0 | −.13* | −.15* | .02* |
| Derogation | 0 | −.05* | −.09* | .00 |
| Discounting | 0 | .16* | .03 | .00 |
| Exaggeration | 0 | .14* | .00 | .00 |
| Government | 0 | .16* | −.09* | −.01* |
| Manipulation | 0 | .20* | −.07* | −.01* |
| Personal attack | 0 | .18* | −.01 | .00 |
| Self-relevance | 0 | .03 | −.01 | .00 |
| Warning avoidance | 1 | .35* | .34* | .12* |
| Worry about consequences of smoking | 0 | .04* | .24* | .01* |
| Social interactions | 1 | .20* | .19* | .04* |
| Attitudes and beliefs | ||||
| Anticipated regret of quitting smoking | 2 | −.04 | −.22* | .01 |
| Anticipated regret of smoking | 2 | −.05* | .03 | .00 |
| Negative consequences of smoking | 0 | .00 | .03 | .00 |
| Perceived benefits of quitting smoking | 1 | −.01 | −.02 | .00 |
| Perceived costs of quitting smoking | 1 | −.04 | −.21* | .01 |
| Perceived likelihood of harm from smoking | 2 | .02 | .10* | .00 |
| Perceived severity of harm from smoking | 2 | .00 | −.05* | .00 |
| Perceived threat (PL*PS) | 2 | .02 | .08* | .00 |
| Perceived severity of negative consequences of quitting smoking | 2 | .00 | −.12* | .00 |
| Perceived efficacy | 2 | .06* | .34* | .02* |
| Self-efficacy to quit smoking | 2 | .05* | .37* | .02* |
| Response efficacy of quitting smoking: lower risk of health problems | 2 | .02 | .10* | .00 |
| Perceived efficacy*Perceived threat | 2 | .04 | .21* | .01 |
| Response efficacy of quitting smoking: cause negative consequences | 2 | −.02 | −.15* | .00 |
| Smoker prototypes | 0 | .01 | −.10* | .00 |
| Negative | 0 | .03 | .12* | .00 |
| Positive | 0 | .05* | .01 | .00 |
| Smoking reinforcement attitudes—negative | 0 | −.01 | −.15* | .00 |
| Smoking reinforcement attitudes—positive | 0 | .01 | −.17* | .00 |
| Subjective norms of quitting smoking | 1 | −.01 | .12* | .00 |
| Intentions | ||||
| Quit intentions | 0 | .13* | .39* | .05* |
| Quit stage | 0 | .08* | .32* | .02* |
| Perceived effectiveness of warnings | 0 | .34* | .32* | .11* |
Outcome variable was having reported a quit attempt during the 4-week trial. Table reports β, the standardized path coefficient. Analyses used a single mediator. Week 0 refers to survey at first visit, immediately after smokers saw their labeled cigarette packs. To allow use of the full sample, analyses accounted for missingness by employing full information maximum likelihood estimation available in Mplus. * designates an interaction term. PL*PS = perceived likelihood * perceived severity.
*p < .05
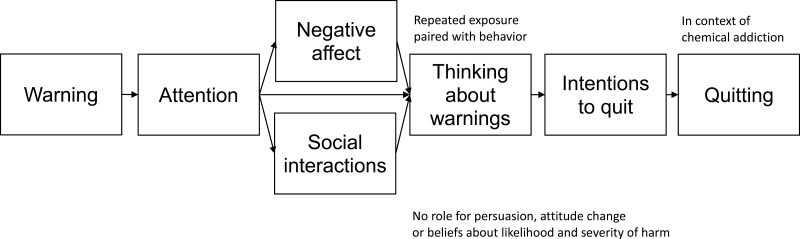
Based on our findings, we built the Tobacco Warnings Model, shown in Fig. 3. The model showed acceptable fit: χ2 [13] = 172, p < .001; RMSEA = .076 (90% CI: .066 to .086); CFI = .934. When respecifying the model, we added a correlation between attention and quit intentions to account for the theoretical supposition that people intending to quit pay more attention to the warnings (Supplementary Fig. 4). The revised model showed good fit: χ2 [12] = 118, p < .001; RMSEA = .064 (90% CI: .054 to .075); CFI = .956. All pathways in the models were statistically significant, (p < .05).
Fig. 3.
Tobacco Warnings Model
Discussion
Pictorial warnings on cigarette packs increase quit attempts and quitting [3, 4], but why they do so is poorly understood. This large gap hampers cancer and cardiovascular disease prevention efforts that focus on smoking. Our large trial with U.S. smokers showed that pictorial warnings increased quit attempts by eliciting aversive reactions and by keeping the message vividly in smokers’ minds. The warnings exerted little of their influence through changes in beliefs and attitudes and none of their influence through changes in risk perception. Given the emphasis in past research on these factors in eliciting behavior change, this pattern of findings was unexpected. Pictorial warnings kept the risk messages in people’s minds without increasing perceived risk. They increased negative affect and anger (a part of reactance [28, 46, 47]), yet negative affect motivated quit attempts even as anger had the opposite effects. They increased social interactions but not subjective norms. They increased avoidance of the warning, which was associated with more quit attempts.
Taken together, these findings do not conform to existing models of health behavior. To come to this conclusion, we compared our findings with the predictions of six widely used health behavior change theories in the first three columns of Table 4. As additional background on pictorial warnings, the table also includes findings on the warning-to-mediator pathways (a) from our trial [4], a meta-analysis of experiments [8], and systematic reviews of the impact of warning policy change as documented in observational studies [3, 5]. One of the oldest and most widely used theories, the Health Belief Model [20], did not fit our findings. Support was modest at best for the Theory of Planned Behavior [21], mostly due to the lack of impact that the warnings had on behavioral attitudes, which are a central construct in the model. Support was modest for the Elaboration Likelihood Model [9]; its central pathway to persuasion through attitude change was not well supported but other aspects of the model related to gaining people’s attention and increasing cognitive elaboration garnered some support. Finally, the Extended Parallel Process Model [23], which was specifically designed to understand fear communication, had modest support. The risk predictions failed [8, 34, 35, 48], but the pathways through fear (and other negative emotions) received clear support. An important shortcoming of the Extended Parallel Process Model in this context is that warning avoidance—in the model as a defensive reaction—acted as a marker for motivation to quit, not an undermining factor. Similarly, several observational studies have found that avoidance does not hinder smoking cessation [31, 32] and may in fact be associated with more quit attempts [33].
Table 4.
Support for theories of health behavior
| Analysis of support | Additional information | ||||
|---|---|---|---|---|---|
| Support for theory | Findings from RCT a*b pathway |
Findings from RCT a pathway |
Meta-analysis of experiments [8] a pathway |
Systematic reviews of observational studies [3, 5] a pathway |
|
| Theory | |||||
| Construct (measure in RCT) | |||||
| Health Belief Model [20] | No support | ||||
| Perceived likelihood | ◯ | ◯ | ◯ | ◯ | |
| Perceived severity | ◯ | ◯ | ● 1 | ● 1 | |
| Perceived threat (PL*PS) | ◯ | ◯ | — | — | |
| Perceived benefit of quitting | ◯ | ◯ | — | — | |
| Perceived costs of quitting | ◯ | ◯ | — | — | |
| Transtheoretical Model [52] | Modest support | ||||
| Perceived benefits (pros of quitting) | ◯ | ◯ | — | — | |
| Perceived costs (cons of quitting) | ◯ | ◯ | — | — | |
| Processes of change | — | — | — | — | |
| Self efficacy | ● | ● | ◯ | — | |
| Stage of change (quit stage) | ● | ● | — | — | |
| Theory of Planned Behavior [21] | Modest support | ||||
| Attitudes (attitudes toward smoking) | ◯ | ◯ | ● | ● 1 | |
| Subjective norms | ◯ | ◯ | — | — | |
| Perceived behavioral control (SE+RE) | ● | ● | ◯SE | — | |
| Intentions (quit intentions) | ● | ● | ● | ⌾ | |
| Constructs added to theory | No support | ||||
| Anticipated regret | ◯ | ◯ | — | — | |
| Smoker prototypes | ◯ | ⌾ | — | — | |
| Behavioral willingness | — | — | — | — | |
| Tripartite Model of Risk Perceptions [22] | Modest support | ||||
| Deliberative risk (perceived likelihood) | ◯ | ◯ | ◯ | ◯ | |
| Affective risk (negative affect) | ● | ● | ● | ⌾ 1 | |
| Experiential risk | — | — | — | — | |
| Elaboration Likelihood Model (9) | |||||
| Attention/noticing | Modest support | ● | ● | ● | ● |
| Recall/recognition | — | — | ● | ⌾ | |
| Perceived understandability | ◯ | ● | — | — | |
| Cognitive processing (cognitive elaboration) | ● | ● | ● | ● | |
| Attitude change | ◯ | ◯ | ● | ● | |
| Extended Parallel Process Model [23] | Modest support | ||||
| Perceived threat (PL*PS) | ◯ | ◯ | — | — | |
| Perceived efficacy (SE+RE) | ● | ● | ◯SE | — | |
| Perceived threat*Perceived efficacy | ◯ | ◯ | — | — | |
| Protection motivation (quit intentions) | ● | ● | ● | ⌾ | |
| Fear (negative affect) | ● | ● | ● | ⌾ 1 | |
| Defensive motivation (reactance) | ● | ● | ● | — | |
| Maladaptive changes (avoidance) | ◯* | ● | — | ● | |
Analysis for support of the theory is based largely on the mediational findings from the trial (a*b pathway). ○ = no support for prediction. ⌾ = mixed support for prediction. ● = support for prediction. — = mediator not assessed. 1 = based on only 1 study in the reviews. SE = self-efficacy. RE = response efficacy of quitting smoking to lower risk of health problems. *Path goes in the opposite direction predicted (prediction from theory: avoidance undermines effect of warnings; finding in RCT: avoidance reinforces/mediates impact of warnings). PL*PS = perceived likelihood * perceived severity.
We make several other observations that can inform future theorizing and may explain the existing theories’ limitations in accounting for pictorial warnings’ effects. First, smoking is a special type of health behavior in that it involves addiction to nicotine. If smokers cannot change their behavior, they may shift their beliefs or attitudes to be consistent with the undesired behavior, and these beliefs and attitudes may change only after the smoker has successfully quit [49]. It is worth noting that while smokers’ attitude toward the pack was a mediator of quit attempts, attitudes and beliefs about the act of smoking were not, and our data suggest these do not change in response to pictorial warnings. Similarly, smokers routinely underestimate their health risks relative to nonsmokers, and the general idea that smoking is a harmful behavior is familiar to many smokers [50, 51]. It is also true that warnings typically address severity but not the likelihood of disease. Also, repeated exposures to the warnings are paired directly with the repeated behavior of smoking, allowing their effects to accumulate over time. Thus, even if warnings do not shift risk beliefs and smoking attitudes, the constant presence of the warnings on the packs may act as a risk reminder that counteracts smokers’ active minimization of risk, and people motivated to quit by the warnings may increase their attention to the warnings.
Building on our trial findings and previous work including the Message Impact Framework [3–5, 8], we propose the Tobacco Warnings Model (Fig. 3) as a way to advance our theoretical understanding of why tobacco warnings exert their effects on behavior. The model proposes that tobacco product warnings increase noticing of and attention to the message. This processing leads to greater negative affect including fear and more conversations with other people about the warnings. Though smokers, most of whom are addicted to nicotine, will generally not change their risk perceptions, the repeated exposure to the warnings keeps the warnings on their mind. The next step is an increase in motivation to quit smoking, as evidenced by greater intentions to quit smoking. Finally, warnings will increase quit attempts and quitting. The model focuses on mediators shown to be important in our trial and other studies. However, future studies should confirm the model given the post hoc nature of our proposal. A strength of the model is its parsimony, but additional constructs such as message reactance, avoidance, and pack attitudes may also play small but important roles [33].
Study strengths include a large and diverse sample, a successful trial with respect to the primary trial outcome of behavior, and a large number of potential mediators. Study limitations include the imperfect comparison of existing text warnings with the novel text of the pictorial warnings. For this reason, the trial did not have an adequate assessment of message recall, another potential mediator. The trial also did not assess knowledge, which may be especially relevant to policymakers, but knowledge is rarely a motivator of behavior change. The trial provided data for people’s responses in the weeks after first exposure, but the generalizability to responses over the longer term remains to be established. As warnings wear out over time, the relative strength of the pathways may change. Finally, as this trial was in a country with text-only warnings currently on cigarette packs, the generalizability of the findings will need to be established for countries that have already adopted pictorial warnings.
Future studies should examine whether warnings designed to target the Tobacco Warnings Model’s five core constructs (attention, negative affect, social interactions, thinking about the warnings, and motivation) are more effective than those targeting other potential mediators. Pictorial cigarette warning studies have yet to examine some additional relevant constructs, including experiential perceived risk (e.g., feeling concerned about harms of smoking) [22]. Studies could also examine the value of the Tobacco Warnings Model in other cancer prevention contexts. The model may be helpful for understanding the impact of warnings on other tobacco products such as e-cigarettes, cigarillos, and hookah, and warnings to reduce other behaviors that contribute to obesity such as consumption of sugar-sweetened beverages and unhealthy snack foods.
Supplementary Material
Acknowledgments
The authors thank the research participants for taking part in our trial. The authors also thank staff at the Pacific Institute for Research and Evaluation, staff at Ewald and Wasserman, Laura Bach, Trent Johnson, and Jennifer MacKinnon for assistance with the trial. Research reported in this publication was supported by The National Cancer Institute and FDA Center for Tobacco Products (CTP) under Award Number P30CA016086-38S2. R25CA057726 from The National Cancer Institute and T32ES007018 from The National Institute of Environmental Health Sciences supported HP’s time writing the manuscript. F31CA196037 and T32-CA057726 from the National Cancer Institute of the National Institutes of Health and P50CA180907 from the National Cancer Institute and the FDA Center for Tobacco Products supported MGH’s time writing the paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Drs. Brewer and Ribisl have served as paid expert consultants in litigation against tobacco companies. The other authors declare no conflicts of interest.
Ethical Approval The University of North Carolina at Chapel Hill Institutional Review Board approved our study protocol.
Informed Consent Participants provided informed consent prior to enrolling in the trial.
References
- 1. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2013: Enforcing Bans on Tobacco Advertising, Promotion and Sponsorship. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2. Canadian Cancer Society. Cigarette Package Health Warnings: International Status Report. 4th ed. Ontario, Canada: Canadian Cancer Society; 2016. [Google Scholar]
- 3. Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brewer NT, Hall MG, Noar SM et al. . Effect of pictorial cigarette pack warnings on changes in smoking behavior: A randomized clinical trial. JAMA Intern Med. 2016;176:905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Noar SM, Francis DB, Bridges C et al. . Effects of strengthening cigarette pack warnings on attention and message processing: A systematic review. Journal Mass Commun Q. 2017;94:416–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fong GT, Cummings KM, Borland R et al. . The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15(Suppl 3):iii3–iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention, Tobacco Control. Vol. 12 Lyon, France: Methods for evaluating tobacco control policies; 2008. [Google Scholar]
- 8. Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tob Control. 2016;25:341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. Adv Exp Soc Psychol. 1986;19:123–205. [Google Scholar]
- 10. Borland R. Tobacco health warnings and smoking-related cognitions and behaviours. Addiction. 1997;92:1427–1435. [PubMed] [Google Scholar]
- 11. Borland R, Wilson N, Fong GT et al. . Impact of graphic and text warnings on cigarette packs: Findings from four countries over five years. Tob Control. 2009;18:358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: Findings from the international tobacco control four country study. Am J Prev Med. 2007;32:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thrasher JF, Pérez-Hernández R, Arillo-Santillán E, Barrientos-Gutiérrez I. Towards informed tobacco consumption in Mexico: Effect of pictorial warning labels in smokers. Salud Publica Mex. 2012;54:242–253. [PMC free article] [PubMed] [Google Scholar]
- 14. Yong HH, Borland R, Thrasher JF et al. . Mediational pathways of the impact of cigarette warning labels on quit attempts. Health Psychol. 2014;33:1410–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moodie C, Mackintosh AM, Hastings G. Adolescents’ response to pictorial warnings on the reverse panel of cigarette packs: A repeat cross-sectional study. Tob Control. 2015;24:e93–97. [DOI] [PubMed] [Google Scholar]
- 16. White V, Webster B, Wakefield M. Do graphic health warning labels have an impact on adolescents’ smoking-related beliefs and behaviours?Addiction. 2008;103:1562–1571. [DOI] [PubMed] [Google Scholar]
- 17. Wardle H, Pickup D, Lee L et al. . Evaluating the Impact of Picture Health Warnings on Cigarette Packets. London, UK: Public Health Research Consortium; 2010. [Google Scholar]
- 18. Peters E, Romer D, Slovic P et al. . The impact and acceptability of Canadian-style cigarette warning labels among U.S. smokers and nonsmokers. Nicotine Tob Res. 2007;9:473–481. [DOI] [PubMed] [Google Scholar]
- 19. Golmier I, Chebat JC, Gélinas-Chebat C. Can cigarette warnings counterbalance effects of smoking scenes in movies?Psychol Rep. 2007;100:3–18. [DOI] [PubMed] [Google Scholar]
- 20. Rosenstock IM. Historical origins of the health belief model. Health Educ Behav. 1974;2:328–335. [Google Scholar]
- 21. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991; 50:179–211. [Google Scholar]
- 22. Ferrer RA, Klein WM, Persoskie A, Avishai-Yitshak A, Sheeran P. The Tripartite Model of Risk Perception (TRIRISK): Distinguishing deliberative, affective, and experiential components of perceived risk. Ann Behav Med. 2016;50:653–663. [DOI] [PubMed] [Google Scholar]
- 23. Witte K. Putting the fear back into fear appeals: The extended parallel process model. Commun Monogr. 1992;59:329–349. [Google Scholar]
- 24. Kees J, Burton S, Andrews JC, Kozup J. Understanding how graphic pictorial warnings work on cigarette packaging. J Pub Pol Mark. 2010;29:265–276. [Google Scholar]
- 25. Kees J, Burton S, Andrews JC, Kozup J. Tests of graphic visuals and cigarette package warning combinations: Implications for the framework convention on tobacco control. J Pub Pol Mark. 2006;25:212. [Google Scholar]
- 26. Nonnemaker JM, Choiniere CJ, Farrelly MC, Kamyab K, Davis KC. Reactions to graphic health warnings in the United States. Health Educ Res. 2015;30:46–56. [DOI] [PubMed] [Google Scholar]
- 27. O’Hegarty M, Pederson LL, Nelson DE, Mowery P, Gable JM, Wortley P. Reactions of young adult smokers to warning labels on cigarette packages. Am J Prev Med. 2006;30:467–473. [DOI] [PubMed] [Google Scholar]
- 28. Hall MG, Sheeran P, Noar SM, Ribisl KM, Bach LE, Brewer NT. Reactance to health warnings scale: Development and validation. Ann Behav Med. 2016;50:736–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Erceg-Hurn DM, Steed LG. Does exposure to cigarette health warnings elicit psychological reactance in smokers?J Appl Soc Psychol. 2011;41:219–237. [Google Scholar]
- 30. LaVoie NR, Quick BL, Riles JM, Lambert NJ. Are graphic cigarette warning labels an effective message strategy? A test of psychological reactance theory and source appraisal. Communic Res. 2017;44:416–436. [Google Scholar]
- 31. Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: Evidence from Canadian smokers. Am J Public Health. 2004;94:1442–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Borland R, Yong HH, Wilson N et al. . How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey. Addiction. 2009;104:669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cho YJ, Thrasher JF, Swayampakala K et al. . Does reactance against cigarette warning labels matter? Warning label responses and downstream smoking cessation amongst adult smokers in Australia, Canada, Mexico and the United States. PLoS ONE. 2016;11:e0159245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Emery LF, Romer D, Sheerin KM, Jamieson KH, Peters E. Affective and cognitive mediators of the impact of cigarette warning labels. Nicotine Tob Res. 2014;16:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Evans AT, Peters E, Strasser AA, Emery LF, Sheerin KM, Romer D. Graphic warning labels elicit affective and thoughtful responses from smokers: Results of a randomized clinical trial. PLoS ONE. 2015;10:e0142879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Morgan JC, Southwell BG, Noar SM et al. . Frequency and content of conversations about pictorial warnings on cigarette packs. Nicotine Tob Res. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hall MG, Sheeran P, Noar SM et al. . Negative affect, message reactance and perceived risk: How do pictorial cigarette pack warnings change quit intentions?Tob Control. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Parada H Jr., Hall MG, Boynton MH, Brewer NT. Trajectories of responses to pictorial cigarette pack warnings. Nicotine Tob Res. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kowitt SD, Goldstein AO, Schmidt AM, Hall MG, Brewer NT. Attitudes toward FDA regulation of newly deemed tobacco products. Tob Regul Sci. 2017;3:504–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hall MG, Marteau TM, Sunstein CR et al. . Public support for pictorial warnings on cigarette packs: An experimental study of US smokers. J Behav Med. 2018;41:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brewer NT, Hall MG, Lee JG, Peebles K, Noar SM, Ribisl KM. Testing warning messages on smokers’ cigarette packages: A standardised protocol. Tob Control. 2016;25:153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brody T: Clinical Trials: Study Design, Endpoints and Biomarkers, Drug Safety, and FDA and ICH Guidelines. London, UK: Academic Press; 2011. [Google Scholar]
- 43. MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kline RB. Principles and Practice of Structural Equation Modeling. New York, NY: Guilford Press; 2011. [Google Scholar]
- 45. Hayes AF. Beyond baron and kenny: Statistical mediation analysis in the new millennium. Commun Monogr. 2009;76:408–420. [Google Scholar]
- 46. Hall MG, Sheeran P, Noar SM, Ribisl KM, Boynton MH, Brewer NT. A brief measure of reactance to health warnings. J Behav Med. 2017;40:520–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Dillard JP, Shen L. On the nature of reactance and its role in persuasive health communication. Commun Monogr. 2005;72:144–168. [Google Scholar]
- 48. Peebles K, Hall MG, Pepper JK, Byron MJ, Noar SM, Brewer NT. Adolescents’ responses to pictorial warnings on their parents’ cigarette packs. J Adolesc Health. 2016;59:635–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Festinger L. A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press; 1957. [Google Scholar]
- 50. Weinstein ND. Accuracy of smokers’ risk perceptions. Ann Behav Med. 1998;20:135–140. [DOI] [PubMed] [Google Scholar]
- 51. Weinstein ND, Marcus SE, Moser RP. Smokers’ unrealistic optimism about their risk. Tob Control. 2005;14:55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Prochaska JO, DiClemente CC.. Toward a comprehensive model of change. In Miller WR, Heather N, eds. Treating Addictive Behaviors. New York: Plenum Press; 1986:3–27. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.